65 Urinary Structures and Functions
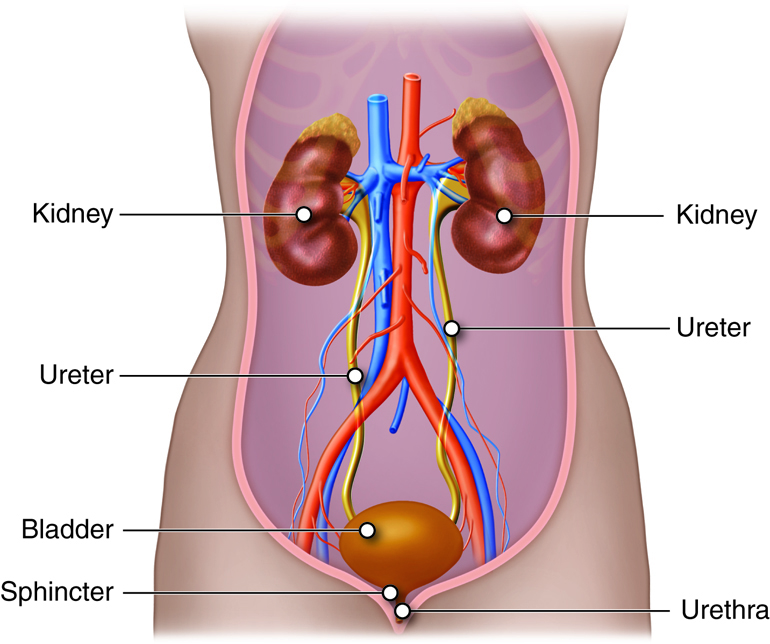
Urinary Tract Anatomy
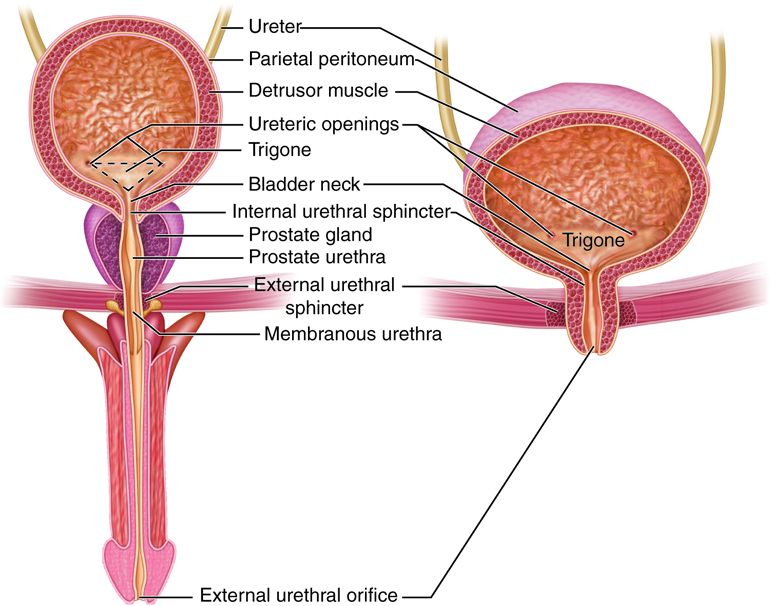
As noted above, much of the maintenance of proper chemical balance, or homeostasis, is the function of the kidneys, which are located towards the lower back. The process begins with waste carrying blood entering each of the two kidneys through the renal artery. Urine is produced by the nephrons in the kidneys. Once filtered, the blood exits through the renal vein. Urine leaves each kidney through a ureter. Each ureter transports the urine via peristalsis to the urinary bladder (a hollow, muscular chamber that collects and stores urine). A single urethra transports the urine from the urinary bladder to the outside of the body. This process through the smooth muscles is otherwise known as: peristalsis. An internal urethral sphincter muscle and an external urethral sphincter muscle help keep the urine in the bladder until the process of urination. The internal urethral sphincter muscle, surrounds the neck of the urinary bladder at the juncture of the bladder with the urethra. It opens reflexively when the bladder muscle contracts and builds up pressure. The external urethral sphincter muscle is part of the urogenital diaphragm and is located at the external opening of the urethra. It is under voluntary control, and as a result of the voluntary control, urination can be delayed for a time. Micturition is the entire process of urination.
The process of urination is known as micturition which begins with blood carrying various wastes that enter each of the two kidneys through the renal artery and ends when urine exits out of the body through the urethra.
Anatomy of the Kidney
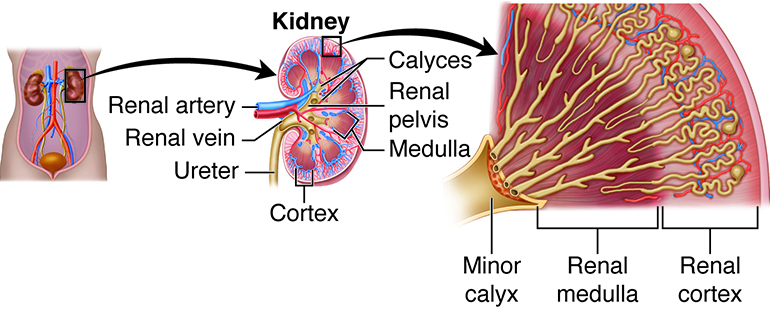
There are six organs in the urinary system: two kidneys, two ureters, the urinary bladder, and the urethra.The kidneys are the body’s main purification system. They remove wastes, some of which are toxic, from the blood. The kidneys also help to regulate blood composition and volume. By manipulating blood volume, the kidneys contribute to the regulation of blood pressure. The kidneys are about the size of your fist and are shaped like beans. The nephron is the structural and functional unit of the kidney. The average number of nephrons in each kidney is about one million, although this number can vary from about half a million to two million. Nephrons are so good at what they do that it only takes about one fourth of them to be functional to meet the needs of the body. Still, a low number of functioning nephrons has been linked to a greater risk of developing kidney disease and high blood pressure (hypertension).
Kidney Location
The kidneys lie between the parietal peritoneum and the posterior abdominal wall, just above waist level. The location posterior to the parietal peritoneum means they are retroperitoneal. These reddish, paired organs are offered some protection by the eleventh and twelfth rib pairs. The right kidney lies slightly lower than the left kidney. This asymmetry occurs due to the increases space required by the liver on the right side of the abdominal cavity superior to the kidney.
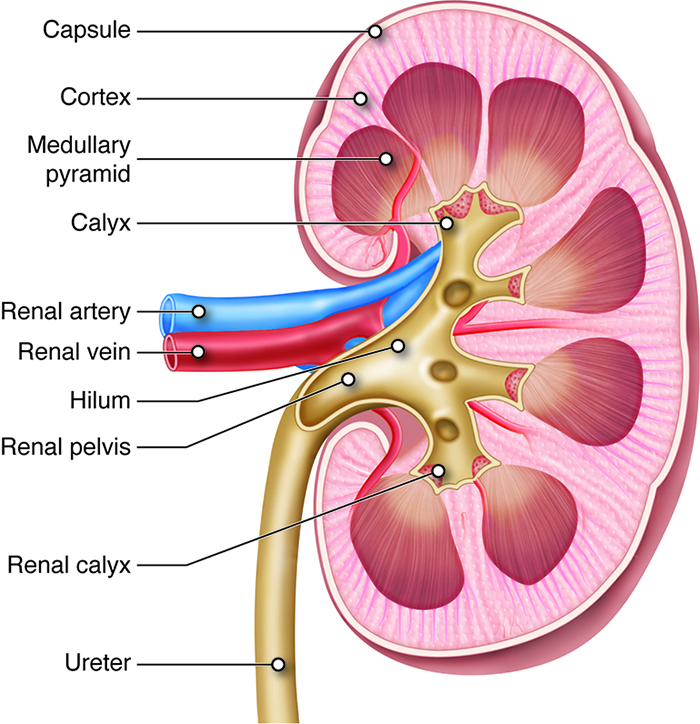
External Anatomy
In adults, the kidney is approximately four to five inches long, two to three inches wide, and one inch thick (10 cm long, 5 cm wide and 2 cm thick). On average, each kidney weighs just under five ounces. The kidneys have a concave medial border that faces the vertebral column. There is a depression near the middle of the concave border called the renal hilum, where the renal artery enters the kidney and the renal vein, and ureters leave it.
Each kidney is enshrouded in four tissue layers. The innermost layer, the renal capsule, is composed of fibrous connective tissue. It preserves the form of the kidney while protecting it from damage due to trauma. The adipose capsule or perinephric fat is the middle tissue layer. This fatty tissue mass encircles the renal capsule, offering another layer of protection from trauma and fixing the kidney in place. The renal fascia is the third tissue layer. The renal fascia is a slim layer of dense irregular connective tissue. This layer tethers each kidney to neighboring structures and to the abdominal wall. The paranephric fat forms the superficial layerand provides additional cushion and support for the kidney.
Renal Ptosis
The position of the kidneys is in part maintained by the layers of fat surrounding them. People who lose a lot of weight in a short period of time can also lose some of the fat that surrounds their kidneys. Very thin people may not have a sufficient layer of fat around their kidneys. In either case, one or both kidneys may drop down into the pelvis when a person stands up, a condition called renal ptosis (ptosis: “to fall”). For the majority of cases, people are without symptoms. However, in some cases health problems ranging from acute pain and vomiting to kinking of the ureter can occur.
If renal ptosis creates a kink in the ureter, the kink can prevent the drainage of urine. Urine can then back up into the kidney, creating pressure that may damage renal tissue.
Diagnosis is controversial but may be confirmed by a patient experiencing relief from abdominal pain upon lying in a supine position and/or by imaging tests.
Treatment for severely symptomatic patients usually involves a laproscopic surgical procedure called nephropexy. This procedure affixes the kidney to the retroperitoneal tissue, closer to its usual position.
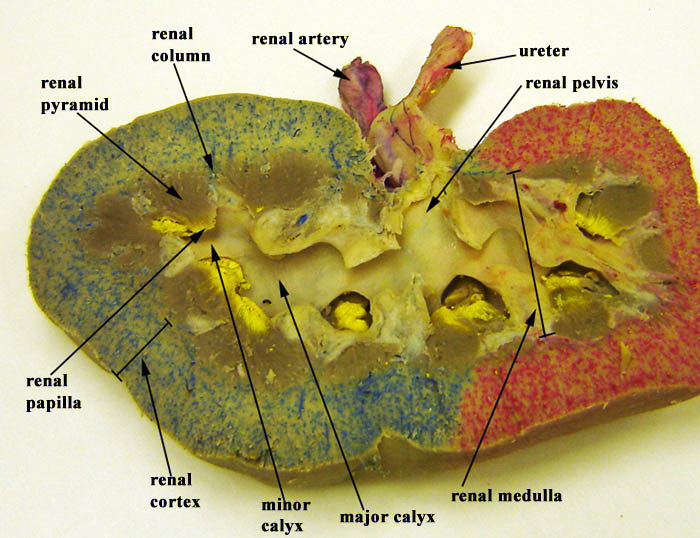
Internal Anatomy
Two structures dominate the internal anatomy of the kidney: a deep reddish-brown area called the renal medulla, and a superficial pinkish area called the renal cortex. The renal medulla is made up of cone-shaped structures called renal pyramids and its primary purpose is to maintain the proper balance of salt and water in the blood. The bases of the pyramids border the renal cortex, and their apexes (renal papillae) face the renal hilum. The smooth-textured renal cortex runs from the renal capsule to the renal pyramid bases and extends towards the pelvis in the spaces between the pyramids. The renal cortex has an outer cortical zone and an inner juxtamedullary zone. The areas of renal cortex lying between renal pyramids are called renal columns. A renal lobe consists of one renal pyramid with its surrounding renal cortex, including one half of both adjacent renal columns.
The parenchyma refers to the functional part of any organ. In the case of the kidney, the parenchyma includes the renal cortex and the renal pyramids. The actual functional units of the kidneys are microscopic structures called nephrons. Recall that there are about a million of nephrons per kidney. A low nephron number is associated with an increased risk of kidney disease and high blood pressure (hypertension).
One of the nephrons’ main roles is to create urine. Urine produced by nephrons empties into large papillary ducts. These ducts run through the renal papillae of the pyramids. From the papillary ducts, urine flows into cup-like structures called the minor and major calyces (calyces: “cups”). Each kidney contains two or three major calyces and several minor calyces. The papillary ducts of one renal papilla drains into a minor calyx. As minor calyces join together, they form a major calyx. All major calyces join together to form one large chamber called the renal pelvis. Urine that collects in the renal pelvis is transported out of the pelvis through the ureters and to the urinary bladder.
Within the kidney, the hilum opens up into a cavity called the renal sinus, which includes a portion of the renal pelvis, the calyces, and renal blood vessel and nerve branches. These structures are held in place in the renal sinus by adipose tissue.
Blood and Nerve Supply
The kidneys’ generous supply of blood vessels reflects their roles in the removal of wastes from the plasma and regulators of the volume and ionic composition of blood. Despite the kidneys accounting for less than 0.5 percent of total body mass, the right and left renal arteries transport approximately one fourth of total cardiac output (approximately1.2 quarts or 1 liter) to these organs every minute.
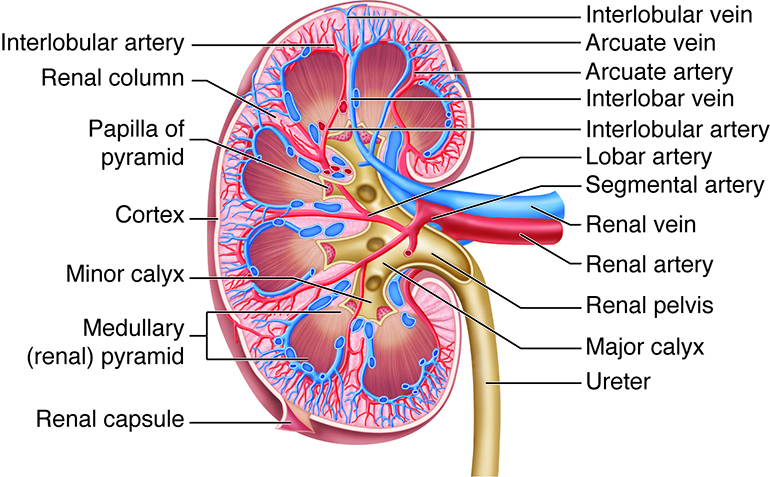
The large renal artery divides into several segmental arteries within the kidney that supply different areas or segments of the kidney. The segmental arteries branch into a number of interlobar arteries within the renal column. At the corticomedullary junction, the interlobar arteries branch to form the arcuate arteries (arcuate means curved). The arcuate arteries divide into smaller cortical radiate arteries (also called interlobular arteries) that supply the cortical tissue. The cortical radiate arteries divide into afferent arterioles, which supply nephrons. The renal cortex receives more than 90 percent of the renal blood supply.
Veins generally follow the same courses as arteries, but in reverse. From the renal cortex, blood drains first into the cortical radiate (interlobular) veins and then the arcuate, interlobar, and renal veins; there are no segmental veins. The renal veins drain into the inferior vena cava, which is located to the right of the vertebral column. Because of the position of the inferior vena cava, the left renal vein is about twice as long as the right renal vein.
Innervation of the kidneys and their ureters is supplied from an outgrowth of the celiac plexus called the renal plexus. This complex of autonomic nerve fibers and ganglia is primarily supplied by sympathetic vasomotor fibers. Their motor function is to adjust the diameter of renal arterioles to help regulate renal blood flow. This includes regulation of blood flow in the affrent and efferent arterioles and thus in the glomerulus. These fibers also innervate the juxtaglomerular apparatus.
The Nephron
The functional units of the kidneys are called nephrons. To understand how different regions of the nephron are able to have unique, spatial functions, we will first discuss how the multicellular epithelial structures found in these structures are organized for specific functions.
Nephrons are made up of epithelial cells with an underlying non-cellular layer or basement membrane that separates the filter in the lumen fluid from the interstitial space. These epithelial cells differ in cellular anatomy along the length of the nephrons according to the filtering and processing functions of the epithelial cells.
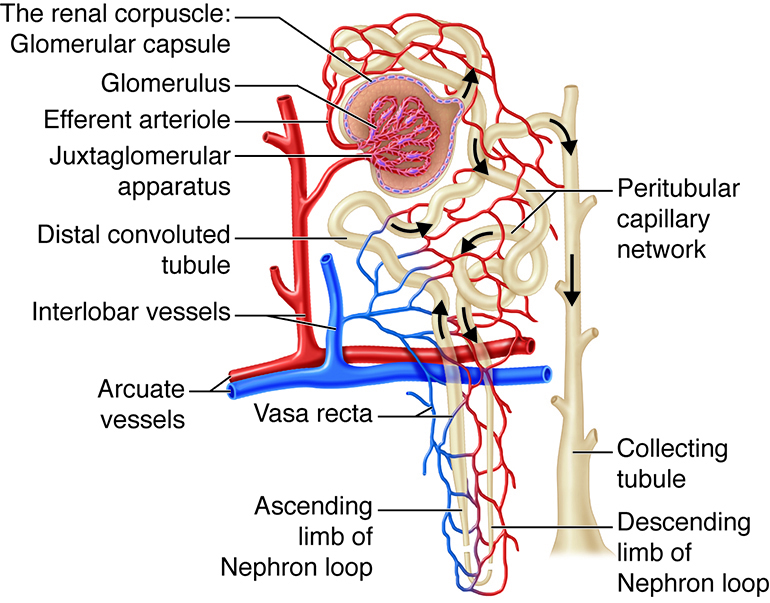
As the chief functional organ in the urinary system, the kidneys excrete nitrogenous wastes and are involved in regulating the volume, composition, and pH of the blood. The kidneys receive one fourth of total cardiac output, a reflection of their function as blood processors. Each kidney contains about one million nephrons, the structural and functional units of the kidneys. Each nephron is made up of a high-pressure capillary bed called a glomerulus and a renal tubule, segments of which included a proximal convoluted tubule, nephron loop (loop of Henle), and distal convoluted tubule. The distal convoluted tubules from multiple nephrons join a common collecting duct. The nephrons are involved in three functions: filtration, reabsorption, and secretion.
Overview of Nephron Structure
The structure within each nephron that actually filters blood plasma is the renal corpuscle containing the glomerulus and glomerular capsule. Another nephron structure called the renal tubule receives the filtered fluid, called glomerular filtrate. Very thin and a little over an inch long, the renal tubule has three major consecutive segments that the filtrate flows through: a proximal convoluted tubule the nephron loop(loop of Henle), and a distal convoluted tubule.
| Nephron Structure | Function | Description |
|---|---|---|
| Glomerulus | Filtration | The glomerulus is a capillary network found in close proximity to the nephron that filters plasma into the nephron. Proteins and blood cells are retained in the glomerular capillary. |
| Tubules and nephron loop (loop of Henle) | Reabsorption | Epithelial cells actively transport some substances from the tubular fluid back into blood. Other substances, such as water, are passively reabsorbed in some segments. |
| Capillaries specifically Peritubular | Secretion | Epithelial cells actively secrete certain substances from the blood into the tubular lumen. |
| Collecting duct | Collection | Accumulates any material that is not returned to blood in the preceding segments. Secretes or reabsorbs H+, HCO3+, and K+ ions. Reabsorbs water under the influence of anti-diuretic hormone. Anything left in the distal end of the collecting duct will l be excreted as urine |
The Glomerulus
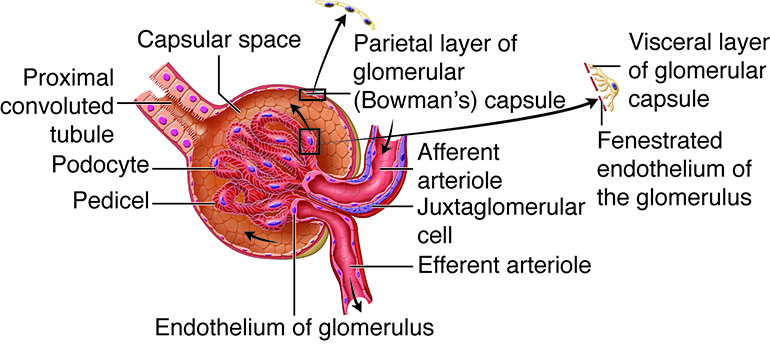
The renal corpuscle is made up of a tangled capillary network called a glomerulus and a cup-shaped structure called the glomerular capsule (Bowman’s capsule) surrounding the glomerulus. The glomerular capsule has an external parietal layer made of simple squamous epithelium. Although this layer is not involved in the production of filtrate, it helps to maintain the shape of the capsule. An inner visceral layer adheres to the glomerular capillaries and is composed of a special type of simple squamous epithelial cells called podocytes. These podocytes have multiple projections called pedicels or foot processes. The pedicels of one podocyte interlock with the pedicels of adjacent podocytes. Filtrate from the glomerulus passes through filtration slits, the openings between the foot pedicels, to enter the capsular space(Bowman’s space), the area between the visceral and parietal layers of the glomerular capsule.
The Proximal Convoluted Tubule
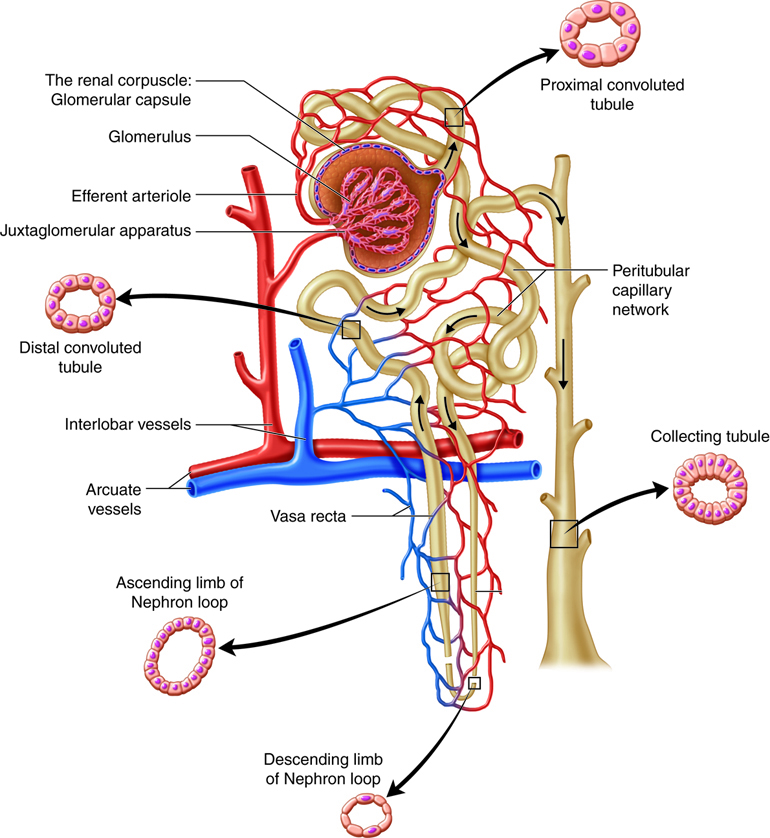
The proximal convoluted tubule (convoluted refers to the coiled shape) tubule connects the glomerular capsule to the nephron loop. The apical surface of the simple cuboidal epithelial cells making up the proximal convoluted tubule are covered in microvilli producing a brush border. The brush border and the length of the proximal convoluted tubule dramatically increase the luminal surface area available for reabsorbing water and solutes and for secreting substances into the filtrate.
The Nephron Loop
The renal corpuscle, the proximal convoluted tubule, and the juncture between the proximal convoluted tubule and the nephron loop are located in the renal cortex. The first part of the nephron loop, the descending limb of the nephron loop, drops into the renal medulla. In the renal medulla, the loop makes a sharp, almost 180-degree turn back toward the renal cortex as the ascending limb of the nephron loop. The ascending limb is continuous with the distal convoluted tubule. The ascending and descending limbs of the nephron loop have two distinct parts: a thin section of the limb and a thick section of the limb. In the thin section of the limb, the diameter of the tubule is distinctly smaller than the diameter of the rest of the nephron tubules. In the thin sections of the limbs, the epithelium is thinner simple squamous epithelium that is permeable to water. In the thick sections of the limbs, the epithelium is simple cuboidal epithelium that is highly impermeable to water. Regardless of being in the thin or the thick segments, the lumen is the same size as the lumen in the rest of the renal tubule.
The Distal Convoluted Tubule
The final segment of the nephron is the distal convoluted tubule. As the ascending limb of the nephron loop reaches the renal cortex, it becomes the distal convoluted tubule. The distal convoluted tubule extends to the collecting tubule, the short connection with a collecting duct. The distal convoluted tubule is composed of simple cuboidal epithelium with very few microvilli and no brush border.
Capillaries of the Nephron
The glomerulus is not the only capillary bed associated with nephrons. Peritubular capillaries are branches of the efferent arterioles that drain the glomeruli and recover most of the filtrate produced in the renal corpuscle. Glomerular capillaries differ from other capillary beds in the body, because they are both supplied by and drained by arterioles. The feeder afferent arterioles are branches of the cortical radiate arteries. The draining efferent arterioles branch into the peritubular capillary network around the proximal and distal convoluted tubules or the vasa recta around the nephron loop. The diameter of the draining efferent arterioles is smaller than that of the afferent arterioles, giving the efferent arterioles higher resistance. Because of this, the glomerulus has a high blood pressure that allows it to filter high volumes of fluid and solutes out of the blood and into the glomerular capsule. The nephrons segments reabsorb approximately 99 percent of this filtrate. The peritubular capillaries adhere to neighboring convoluted tubules and drain into neighboring venules. These low-pressure and porous capillaries easily reabsorb the water and solutes that the tubule recovers from the filtrate. In some nephrons, rather than breaking up into peritubular capillaries, the efferent arterioles form clusters of thin-walled vasa recta. Important for the formation of concentrated urine, the vasa recta are long, straight capillaries that reach deep into the medulla alongside the longest nephron loops where they can collect reabsorbed substances from the loop segments.
Because blood in the renal circulation flows through two arterioles (where a majority of the manipulation of vascular resistance is found), renal blood pressure drops from about 95 mm Hg in the renal arteries to less than 10 mm Hg in the renal veins. Resistance in the afferent arterioles fluctuates in order to help maintain a relatively constant glomerular capillary hydrostatic pressure even if there are substantial changes in systemic blood pressure. The resistance of the efferent arterioles also contributes to maintenance of glomerular capillary hydrostatic pressure and also contributes to a low hydrostatic pressure in the peritubular capillaries.
Specialized Cells Associated with the Nephron
In all nephrons, the last part of the ascending limb of the nephron loop transitions into the distal convoluted tubule and comes in contact with the afferent arteriole supplying the renal corpuscle. In this region the columnar epithelial cells at the beginning of the distal convoluted tubule are very crowded, leading to the name macula densa (“dense spot”). The macula densa is believed to monitor sodium chloride concentration of the filtrate entering the distal convoluted tubule. The wall of the afferent arteriole that is adjacent to the macula densa contains granular cells (also known as juxtaglomerular cells ). The granular cells produce and secrete the enzyme renin and are also capable of contracting when stimulated. These cells and the macular densa make up the juxtaglomerular apparatus. The action of the juxtaglomerular apparatus helps control glomerular hydrostatic pressure by sending signals to the afferent arteriole. There are also special smooth muscle cells called intraglomerular mesangial cells in in the spaces between the loops of the glomerulus. These cells help regulate blood flow through the glomerulus.
Collecting Ducts
As the functional units of the kidneys, the primary role of the nephrons is to filter plasma, reabsorb what the body would like to keep, and excrete the rest. Any substances not reabsorbed in the tubules of the nephrons flows into one of thousands of collecting ducts in the kidney. A short collecting tubule forms the juncture between a distal convoluted tubule and a collecting duct. Each collecting duct receives fluid from several nephrons and then transports it to the renal pelvis. The collecting tubules and ducts have two types of cells: intercalated cells, cuboidal cells with plentiful microvilli, and the more populous principal cells, cuboidal cells with limited, short microvilli. Principal cells help maintain water and sodium and potassium ion balance in the body. Intercalated cells help regulate the acid-base balance of the blood.
The Ureters, Bladder, and Urethra
The ureters are a pair of thin, muscular tubes that transport urine from the kidneys to the bladder. Beginning at the level of the second lumbar vertebra, the location of the ureters is retroperitoneal. Each ureter runs inferiorly and enters the posterolateral wall of the urinary bladder. This angle of entry is important, because it helps prevent urine from flowing back into the ureters when the bladder fills with urine. In addition, accumulating urine increases the internal pressure of the bladder, and this pressure compresses and seals the distal portion of the ureters.
There are three layers in the ureter wall. The innermost mucosa lining contains transitional epithelium capable of stretching but is impermeable to urine. The ability to stretch allows the ureter wall to accommodate changing volumes of urine. The middle muscularis layer is composed of two layers of smooth muscle: an inner longitudinal layer and outer circular layer. In the lower third of the ureter, the muscularis has a third outer layer of longitudinal muscle fibers. The muscularis layer is responsible for the peristaltic contractions needed to move urine through the ureters and into the bladder. The external layer of the ureter wall, the adventitia, is made of fibrous connective tissue and helps anchor the ureter to the abdominal wall.
When urine enters and distends the ureters, stretch receptors are stimulated. Reflexive action results in the contraction of the muscularis and, movement of the urine into the bladder. The power and frequency of peristalsis is directly related to the rate of urine formation. Although the ureters are innervated by both sympathetic and parasympathetic fibers, the nervous system does not appear to have major involvement in the transport of urine in these organs.
The Urinary Bladder
The urinary bladder is a hollow, collapsible muscular sac that serves as a temporary storage facility for urine. It is located in the pelvic cavity, just posterior to the pubic symphysis. In females, the bladder lies anterior to the vagina and inferior to the uterus. In males, it is immediately anterior to the rectum. Peritoneal folds hold the bladder in place.
The bladder can hold up to about a liter of urine, although this amount varies from person to person. Despite its capacity to enlarge, an overfull bladder can burst but it is more likely that excess urine will leak out of the urethra. When empty, the bladder collapses into a pyramidal shape. When a small amount of urine accumulates, it is spherical. When a larger volume of urine accumulates, the bladder becomes pear-shaped and ascends in the abdominal cavity. There are three openings in the bladder: two for the ureters and one for the urethra. These openings frame a triangular region at the base of the bladder called the trigone.
The bladder wall is made up of a mucosa with transitional epithelium, a submucosa, a thick muscularis called the detrusor muscle, and a fibrous adventitia. The adventitia is on the inferior surface only. In contrast, the peritoneum covers the superior surface. The detrusor muscle is composed of inner and outer layers of longitudinal smooth muscle fibers and an intermediate layer of circular muscle fibers.
The Urethra
The urethra is a small muscular tube that transports urine from the bladder out of the body. The urethra is five times longer in males (8 inches, 20 cm) than in females (1.6 inches, 4 cm). In males, the urethra is also part of the reproductive system, providing a passageway for semen as well as urine. The course of the urethra also differs between the sexes. In females, fibrous connective tissue binds it to the anterior vaginal wall, and its external urethral orifice (external opening) is located anterior to the vaginal opening and posterior to the clitoris. In males, the urethra is divided into three regions. The prostatic urethra is surrounded by the prostate. The membranous urethra passes through the urogenital diaphragm. The spongy urethra runs through the penis and ends at the external urethral orifice.
At the bladder-urethra junction, the circular fibers of the bladder’s detrusor muscle form the internal urethral sphincter. When urine is not draining from the bladder, this involuntary sphincter closes off the urethra to prevent the leakage of urine when you are not voiding. At the point where the urethra passes through the urogenital diaphragm, it is surrounded by the external urethral sphincter, a skeletal muscle. The external sphincter is voluntarily controlled and is kept contracted until voiding.
Urinary Tract Infections
Urinary tract infections (UTIs) are the most common type of bacterial infection. Women are predisposed to UTIs because their urethras are shorter than those of men. Moreover, the urethra’s external opening in women is closer to the anus than it is in men. Over 50 percent of women will have a UTI at some point during their lifetime. Fecal bacteria such as Escherichia coli (E. coli) can easily travel up the urethra. This is why women should never wipe the anus in a forward direction after defecation. However, most UTIs in women occur as a result of sexual activity. During intercourse, bacteria from the external genital area and the vagina can be pushed up the short urethra toward the bladder. The use of spermicides actually increases the risk of UTIs, because spermicides kill bacteria that would otherwise help destroy infectious fecal bacteria in the vagina. Drinking plenty of water and urinating immediately after sexual activity can help prevent UTIs by flushing bacteria out of the urethra. Infection of the urethra (urethritis) can easily spread to the urinary bladder (cystitis) and sometimes to the kidneys (pyelitis or pyelonephritis). Symptoms of a UTI include pain during urination (dysuria), frequent urination or an urgent need to urinate, cloudiness or blood in the urine (hematuria), urine with a strong odor, nausea, and fever. Fortunately, most UTIs respond to antibiotics. Analgesics may also be prescribed to reduce discomfort. Unfortunately, having a UTI increases the chances of having subsequent UTIs. UTIs are also common in infants, particularly in uncircumcised male infants.
Summary of Urinary Anatomy
There are six organs in the urinary system: two kidneys, two ureters, the urinary bladder, and the urethra.
- The two kidneys, perform the following functions:
- Remove wastes from the blood.
- Help regulate blood composition and volume.
- Contributing to the regulation of blood pressure.
- External Anatomy of the kidneys include:
- A renal hilum, renal vein, ureter, and nerves either enter or exit the kidney.
- A renal capsule that preserves the form of the kidney.
- The perinephric fat that encircles the renal capsule, offering another layer of protection.
- The renal fascia that tethers each kidney to neighboring structures and to the abdominal wall.
- The paranephric fat that comprises the outermost layer, and provides another layer of protection.
- Internal Anatomy of the kidneys include:
- Therenal medulla that maintains the proper balance of salt and water in the blood
- The renal cortex is the outer layer of the kidney. It also extends as renal columns between the renal pyramids.
- The renal pyramids make up the renal medulla Included as part of the functional part of the kidney.
- The renal papillae are located at the apex of the renal pyramids.
- The renal columns are part of the renal lobes.
- The renal lobes consist of one renal pyramid with its surrounding renal cortex, including one half of both adjacent renal columns.
- The functional units of the kidneys are called nephrons, which are made up of epithelial cells sitting on top of a non-cellular layer or basement membrane.
- Each kidney contains about one million nephrons, which are made up of:
- A renal corpuscle made up of a glomerulus within a glomerular capsule
- A renal tubule comprised of a proximal convoluted tubule, nephron loop, and distal convoluted tubule.
- Collecting ducts that receive tubular filtrate from multiple nephrons and transport the fluid to the calyces and renal pelvis.
- The nephrons are involved in three functions: filtration, reabsorption, and secretion.
- The other organs of the urinary system include:
- The ureters:
- The innermost mucosa lining allows the ureter wall to accommodate changing volumes of urine.
- The middle muscularis layer is composed of two layers of smooth muscle: an inner longitudinal layer and outer circular layer. The muscularis is responsible for moving urine through the ureters and into the bladder.
- The outer layer of adventitia.
- The urinary bladder:
- The trigone.
- The internal urethral sphincter At the bladder-urethra junction, involuntarily sphincter closes off the urethra and prevents the leakage of urine when you are not voiding.
- The external urethral sphincter at the distal end of the urethra at the orifice closes off the urethra and prevents the leakage of urine when you are not voiding.
- The urethra is a small muscular tube that transports urine from the bladder out of the body. The urethra is five times longer in males (8 inches, 20 cm) than in females (1.6 inches, 4 cm). The course of the urethra also differs between the sexes. At the bladder-urethra junction, the internal urethral sphincter involuntarily sphincter closes off the urethra and prevents the leakage of urine when you are not voiding.

