25 Integumentary Levels of Organization
The levels of organization of the skin and its accessory structures are listed below. You will be exploring these further in the coming pages.
- Molecular level – keratin, melanin and vitamin D
- Microscopic level – stem cells and skin cells
- Tissue level – epithelial and connective tissue
- Organ level – skin, consisting of the epidermis, dermis, and hypodermis, as well as hair, nails and glands
Molecular Level
Keratin and Melanin
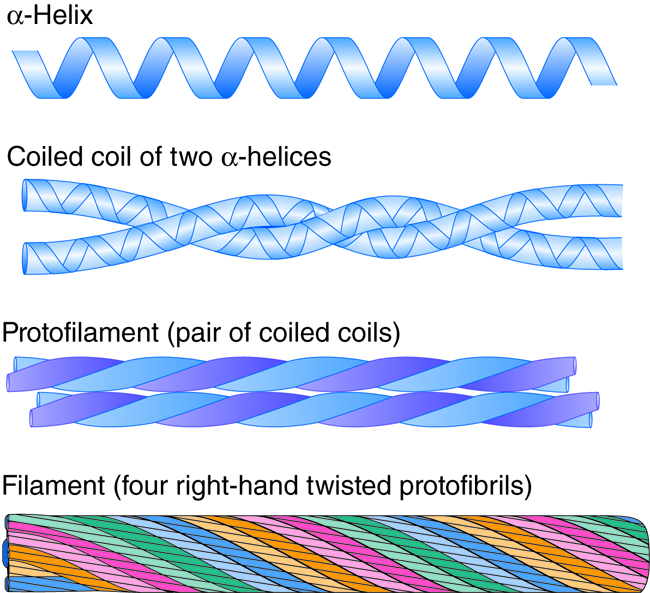
Keratin is a group of fibrous proteins that give hair, nails, and skin their tough, water-resistant properties. Keratins are filaments formed from the polymerization of intermediate filament proteins. In addition to intra- and intermolecular hydrogen bonds, keratins have large amounts of the sulfur-containing amino acid cysteine, which forms disulfide bridges that confer additional strength.
Keratins are an excellent example of protein assembly. Keratins have an alpha-helix secondary structure in the central rod domain. Two keratin proteins then come together and the helices wind around themselves to form a quaternary structure of a coiled-coil dimer. These dimers then assemble into protofilaments and then filaments. The twists of twists are similar to fibers inside of ropes. However, keratins aren’t twisted by machines; they self assemble based on their primary structure.
Melanin is a class of photopigment (“photo,” meaning “light,” and “pigment,” meaning”colored material”) with a molecular structure that allows it to absorb UV (ultraviolet) radiation from the sun. Melanin transforms the energy from the radiation into harmless heat, and melanin prevents the indirect DNA damage from the sun that is responsible for many skin cancers. Melanin also gives skin, hair and eyes their color. Melanin is produced by specialty cells called melanocytes, inside special vesicles called melanosomes. About 10 days after initial sun exposure, melanin synthesis peaks, which is why pale-skinned individuals tend to suffer sunburns of the epidermis initially.
Example; Albinism
Albinism is a genetic disorder that affects (completely or partially) the coloring of skin, hair, and eyes. The defect is primarily due to the inability of melanocytes to produce melanin. Individuals with albinism tend to appear white or very pale due to the lack of melanin in their skin and hair. Melanin protects the DNA of skin cells from the harmful effects of UV rays from the sun. Individuals with albinism need more protection from the sun and must limit their outdoor activities. Treatment of this disorder usually involves addressing the symptoms.
Molecular Level
Vitamin D
The epidermal layer of human skin synthesizes the precursor to vitamin Dwhen exposed to UV radiation. In the presence of sunlight, an isomer of vitamin D3, cholecalciferol, is synthesized from a derivative of the steroid cholesterol in the skin. The liver converts cholecalciferol to calcidiol, which is then converted to calcitriol (the active chemical form of the vitamin) in the kidneys. Vitamin D, which is really a hormone, is essential for normal absorption of calcium and phosphorous, which are required for healthy bones. In the present day, this hormone is added as a supplement to many foods including milk and orange juice, compensating for the need for sun exposure.
In addition to affecting bone health, Vitamin D is essential for general immunity against bacterial, viral and fungal infections. Recent studies are also finding a link between insufficient vitamin D and cancer.
Example: Rickets
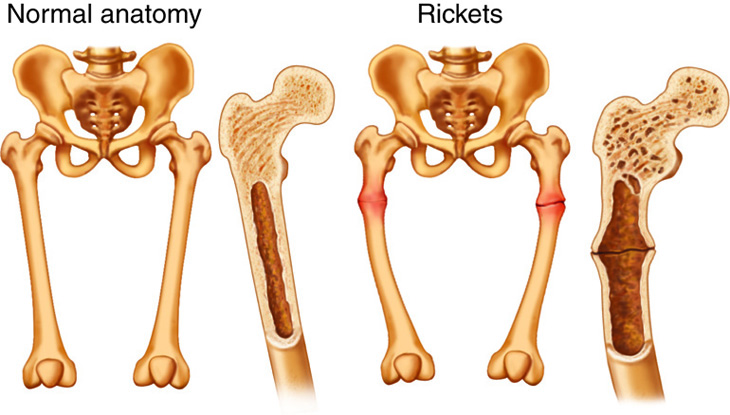
Rickets is a disease of bone deterioration often caused by insufficient vitamin D, leading to insufficient calcium absorption. Children are especially prone to effects from this vitamin deficiency due to their rapid bone turnover and formation. In adults, the deficiency of vitamin D is called osteomalacia. Typically rickets is found in developing countries where malnutrition would prevent proper supply of calcium and dietary vitamin D.
Microscopic Level – Cells of the Epidermis
The epidermis (or epithelial layer) is stratified squamous epithelia, composed of four to five layers (depending on body region) of epithelial cells. The top layers of the epidermis are made up of keratinocytes, which are cells containing the protein keratin. The keratinocytes on the most superficial layer of the epidermis are dead, and periodically slough away, being replaced by cells from the deeper layers. As keratinocytes move superficially from the deeper layers, they lose cytoplasm and become flattened, allowing for many layers in a relatively small space.
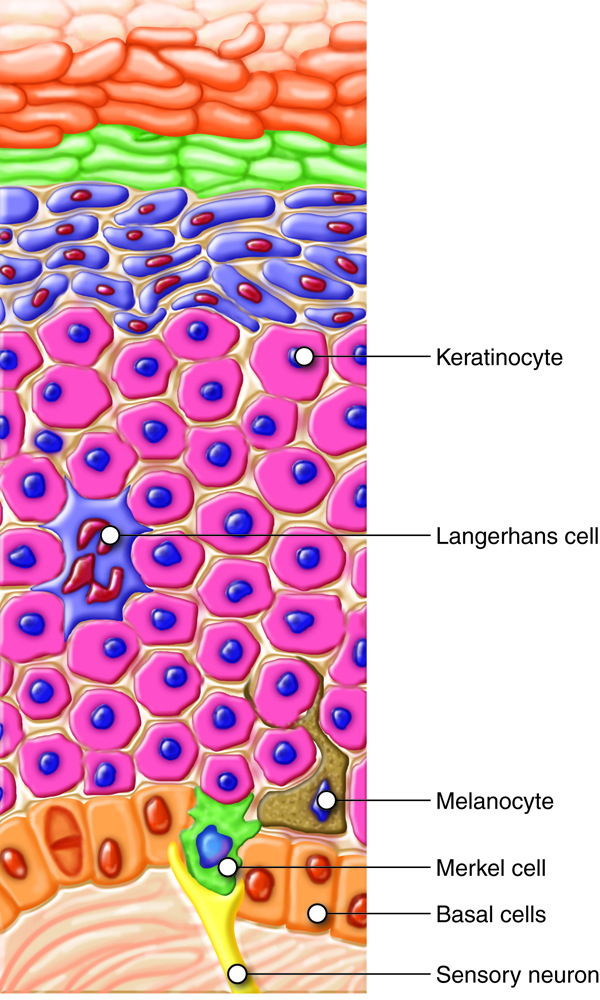
Basal cells are an example of tissue-specific stem cells, meaning they can turn into a variety of cell types found in that tissue. Under normal conditions, daughter basal cells most commonly replace lost keratinocytes.
The deepest layer of the epidermis and the most superficial layer of the dermis give out projections that interlock with each other (like Velcro) and strengthen the bond between the epidermis and the dermis. The projections originating in epithelial cells of the bottom layer of the epidermis are called desmosomes, and the ones originating in the dermis are called dermal papillae. Think of the projections as a formation of folds of cellular matter. The greater the fold, the stronger the connections made.
Merkel cells are sensory receptors that detect light touch. They form synaptic connections with sensory nerves that carry touch information to the brain. These cells are abundant on the surface of the hands and feet.
Melanocytes are cells in the bottom layer of epidermis that produce the pigment melanin, which gives hair and skin its color. Individuals whose melanocytes produce more melanin have darker skin color. Cellular extensions of the melanocytes reach up in between the keratinocytes.
Dendritic or Langerhans cells are tissue macrophages that contribute to the immune function of the skin. They engulf foreign organisms and signal to the immune system. Since the skin is in constant contact with the environment, it is important to have immune cells to help destroy any pathogens that might get past the cell barrier of the epidermis.
Example: Eczema
Eczema is an allergic reaction that manifests as dry, itchy patches of skin that resemble rashes. Normally it is useful to have immune cells in the skin, but they can also lead to dysfunction if they become overactive. In eczema, this excess activity may be accompanied by swelling of the skin, flaking, and in severe cases, bleeding. Other allergic (immune-mediated) reactions include hives. Symptoms of these conditions are usually managed with moisturizers and topically with corticosteroid or antihistamine creams that reduce the inflammatory immune response.
Some studies report that children who are raised in “overly clean” homes are more likely to develop eczema. It is theorized that if the Langerhans cells don’t experience regular contact with antigens during early childhood development they then will be more likely to become overactive and begin to attack the body’s own cells.
Skin Cancer
Cancer in general is initiated because of DNA damage that accumulates in a particular cell over time. Exposure to UV rays from the sun can ultimately lead to mutations in the genomes of various skin cells. Accumulation of genetic mutations over a period of time, in addition to other possible causes, can trigger cells to grow out of control. The normal signals that control cell divisions (even stem cells have these controls) are lost, and cells grow to form a tumor, or mass of cells. While some tumors are benign (stay in one place), some produce cells that dislodge from the tumor and establish tumors in other areas of the body. In other words, they metastasize and form secondary tumors.
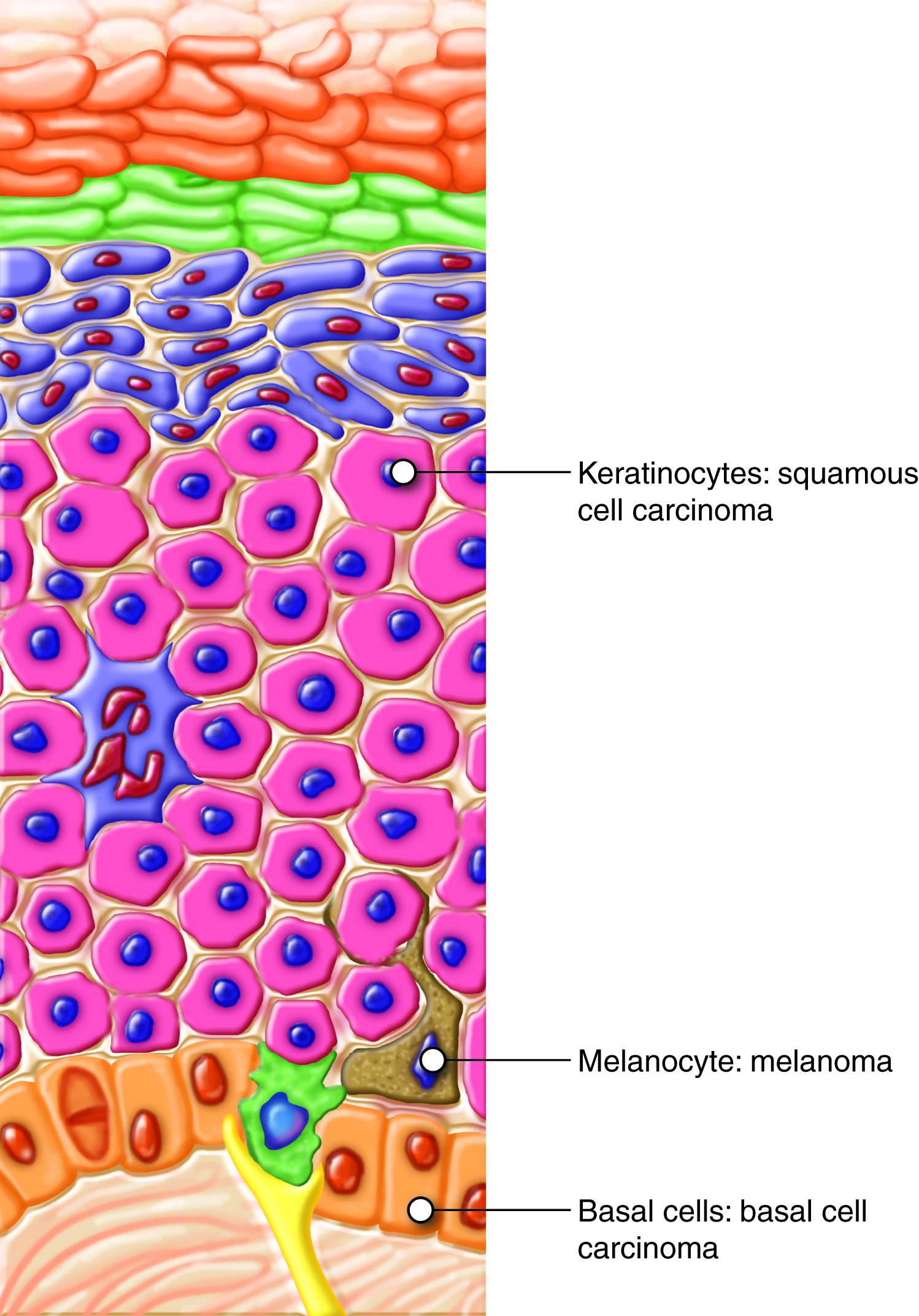
Basal Cell Carcinoma
Basal cell carcinoma is caused by mutations that lead to lack of control over the growth of stem cells located in the stratum basale. It is the most common form of all cancers that occur in the United States. The head, neck, arms, and back are most susceptible, due to long-term sun exposure. Although UV radiation is the main culprit, exposure to other agents, such as electromagnetic radiation or carcinogenic chemicals, can also lead to this type of cancer. Injury to the skin due to open sores, tattoos, burns, etc. may be predisposing factors as well. Basal cell carcinoma usually starts as an uneven patch, bump, growth, or scar on the skin surface and responds best to treatment when caught early. Complete surgical excision of the lesion usually cures this form of cancer.

Squamous Cell Carcinoma
Squamous cell carcinoma is the second most common skin cancer, and affects the keratinocytes. Lesions are usually scaly and red and are most common on the scalp, ears, and hands. If not removed, they can metastasize. Surgery and radiation are used to cure squamous cell carcinoma.

Melanoma
Melanoma affects melanocytes, the pigment-producing cells in the epidermis. It is the most fatal of all skin cancers, as it is highly metastatic and can be difficult to detect before it has spread. Melanomas usually appear as asymmetrical brown and black patches with uneven borders and a raised surface. Treatment typically involves surgical excision and immunotherapy.
Early lesions may exhibit some of the following symptoms:
- A=Asymmetry, where one side of the mass is unequal to the other side
- B=Borders are irregular and not smooth
- C=Color, where the mass has more than one color present
- D=Diameter of more than 6mm (about the size of an old wooden pencil eraser)
If you or a loved one has a mole with these symptoms, please consider visiting a dermatologist.
Part of the ABCDs for detection of melanoma. On the left side from top to bottom: melanomas showing (A) Asymmetry, (B) a border that is uneven, ragged, or notched, (C) coloring of different shades of brown, black, or tan and (D) diameter that had changed in size. The normal moles on the right side do not have abnormal characteristics (no asymmetry, even border, even color, no change in diametry). Source images:
 |
 |
 |
 |
 |
 |
 |
Source: http://visuals.nci.nih.gov
Tissue Level
Epithelial Tissue
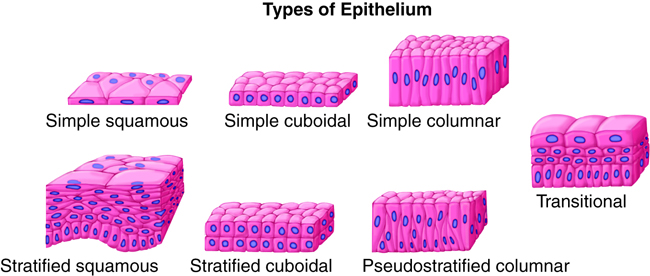
The skin contains many tissue types. The epidermis is classified as epithelial tissue composed of stratified squamous epithelia. The dermis is made of different types of connective tissues including areolar and dense irregular connective tissue, and histiocytes (tissue macrophages). The hypodermis contains areolar connective tissue, adipose tissue, and glands.
The epidermis is mainly made up of stratified (layered) squamous (flat) epithelial cells. Epithelial cells found in the different layers of the epidermis have different shapes. Stratification (layering) is important in the epithelial tissue of the integumentary system, which forms a barrier. Epithelial cells found in other systems have other surface cell shapes, including cube-like (cuboid) and column-like (columnar) in a single layer (simple) or multiple cell layers (stratified).
The epidermis contains several cell types of different origins, including keratinocytes (95 percent of the cells are keratinocytes), melanocytes, Langerhans cells and Merkel cells. The epidermis does not contain blood vessels or nerves, but Merkel cells provide signals to the sensory neurons below this layer in the dermis. Since there are no blood vessels, living cells of the epidermis are nourished by diffusion from the capillaries of the dermal papillae below.
Connective Tissue
While the epidermis is composed of epithelial cells, the dermis is composed of connective tissue. The dermis connects the epidermis to the hypodermis and provides structure and elasticity from collagen and elastin fibers. These proteins are made by fibroblasts found in the dermis. Collagen and elastin work together: collagens provide strength; elastins, as the name implies, are elastic and allow for distension. The skin must remain strong to protect you from abrasions and other cuts. However, the skin also needs to be able to deform and, hopefully, return to its original shape.
Example: Wrinkles
The permanent folds in the skin caused by a lack of “retraction” are called wrinkles. Wrinkling in the skin is caused by habitual facial expressions, aging, sun damage, smoking, poor hydration, and various other factors. Wrinkling is a surprisingly complex phenomenon. Primarily, sun or other damage to the skin causes a breakdown in collagen and elastin as well as a breakdown in the replacement of these extracellular matrix proteins in the dermis.
Example: Stretch Marks
Stretch marks usually accompany rapid weight gain during puberty and pregnancy as well as during the rapid gain of muscle associated with weight lifting. When the dermis (and possibly the hypodermis) is stretched beyond its limits of elasticity, the skin stretches to accommodate the excess pressure. In some cases, the dermis can’t adequately fill in over the stretched areas and may actually tear, causing the epidermis to become thin and making the underlying blood vessels more visible. They initially have a reddish hue, but lighten over time as the tissue repairs itself and heals. Other than for cosmetic reasons, treatment of stretch marks is not required. They occur most commonly over the hips and abdomen.
Pigmentation of the Skin
Skin contains different types of melanin, including pheomelanin, which is reddish, and eumelanin, which is dark brown. The amount and types of melanin produced is under genetic control. The combinations of the different types of melanin result in the wide range of skin colors and tones seen in humans. While the number of melanocytes do not vary too much between individuals, the skin tone depends on the amount and type of melanin produced by these cells. If a person has more eumelanin producing melanocytes, that person would have darker skin color. The predominance of pheomelanin is responsible for the reddish coloration of hair in some individuals.
Exposure to the sun causes melanin to build up, because sun exposure stimulates keratinocytes to secrete a peptide hormone that in turn stimulates melanocytes into producing melanin. The melanocytes produce and then transfer the melanin to keratinocytes. This buildup of melanin results in the darkening of the skin, or a tan. Increased melanin also protects the skin’s DNA from UV ray damage to some extent, although even very dark-skinned individuals can get skin cancer. Melanin synthesis does not peak until about 10 days after initial sun exposure, which is why pale-skinned individuals tend to suffer sunburns of the epidermis initially. Individuals with darker skin can also get sunburns, but are more protected than light-pigmented individuals.
Melanosomes, the cellular organelles that contain melanin, are temporary structures and are eventually destroyed by fusion with lysosomes, which makes tanning impermanent. Too much sun exposure can eventually lead to wrinkling of the skin due to destruction of the cellular structure of the skin, and in severe cases it can cause sufficient DNA damage to result in skin cancer. An uneven distribution of melanocytes in the skin results in the appearance of freckles.
Sunscreen and UVA and UVB Radiation
“UV” is an abbreviation for “ultraviolet.” Ultraviolet radiation is a portion of the electromagnetic spectrum between visible light and x-rays. The sun emits two ranges of ultraviolet light that penetrate earth’s atmosphere: UVA and UVB. UVB radiation is partially absorbed by the ozone layer, but some still reaches the surface of the Earth. UVA radiation is not filtered, and all of it reaches the surface of the Earth. One of the functions of our integumentary system is to protect us from this UV radiation. Exposure to this radiation can cause skin damage and cancer. Sunscreens are designed to protect our skin from UV radiation. Sunscreens with a sun protection factor (SPF) of 15 or more provide good protection from UVB radiation. To be protected from UVA radiation, you must have a “broad-spectrum” product.
Organ Level
Skin (Epidermis and Dermis)
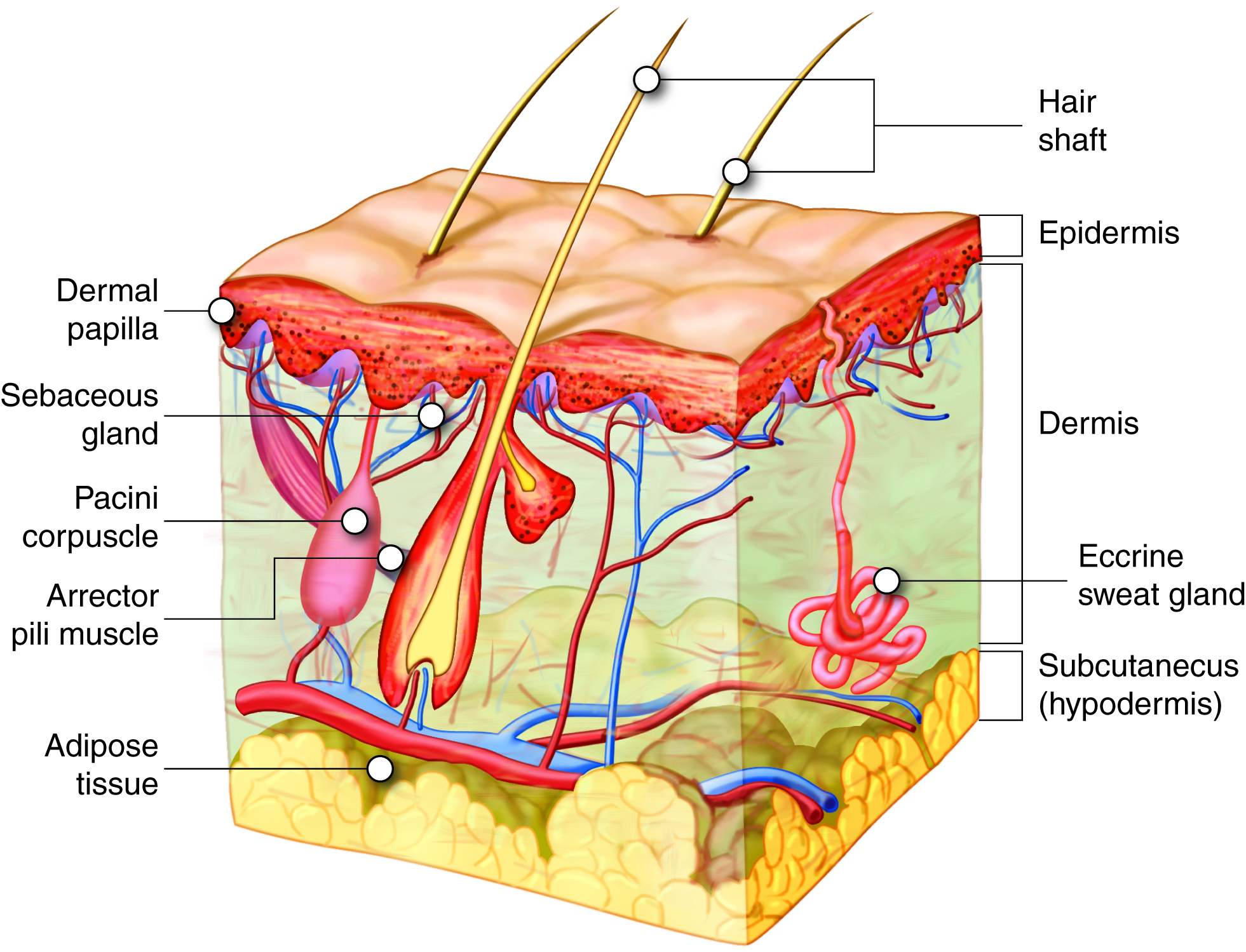
The skin, the integumentary system’s organ, is composed of the epidermis (epithelial tissue) and dermis (connective tissues), with an underlying hypodermis that is technically not part of the skin organ. Several layers of keratinocytes at the surface form the epidermis. The topmost layer is dead and sheds continuously. It is progressively replaced by stem cells that divide in the basal layer (stratum basale). The dermis connects the epidermis to the hypodermis and provides strength and elasticity due to the presence of collagen and elastin fibers. The hypodermis is the name for the layer of connective tissue that connects the dermis to the underlying organs. It also harbors adipose tissue for fat storage. Let’s look at the structure and function of these parts of the skin organ in detail.
The epidermis (or epithelial layer) is made up of four or five distinct layers (strata), depending on the region of the body. From deep to superficial, they are named the stratum basale, stratum spinosum, stratum granulosum, stratum lucidum, and stratum corneum. The stratum lucidum is unique to areas like the palms of the hand (palmar surfaces) and soles of the feet (plantar surfaces), where the skin is thicker than it is in the rest of the body. The stratum basale is made up of the many cell types already discussed, including basal cells, melanocytes, Langerhans cells and Merkel cells. As you look at the more superficial layers, you see that they become mostly (or completely) composed of keratinocytes, which protect and waterproof the body. As the cells are pushed superficially (toward the surface) they make keratin. As the cells begin to fill with keratin, they become increasingly impervious to water, and it becomes more difficult for osmosis and diffusion to occur inside the cell. In addition, as cells enter each superficial layer(further away from the dermis, which contains the blood supply), the distance across which oxygen and other nutrients must diffuse increases, making it harder for the cells to get the nutrients they need. The keratinocytes in the stratum corneum (the most superficial layer) are usually inert, or dead, and periodically slough away, being replaced by cells from the deeper layers.
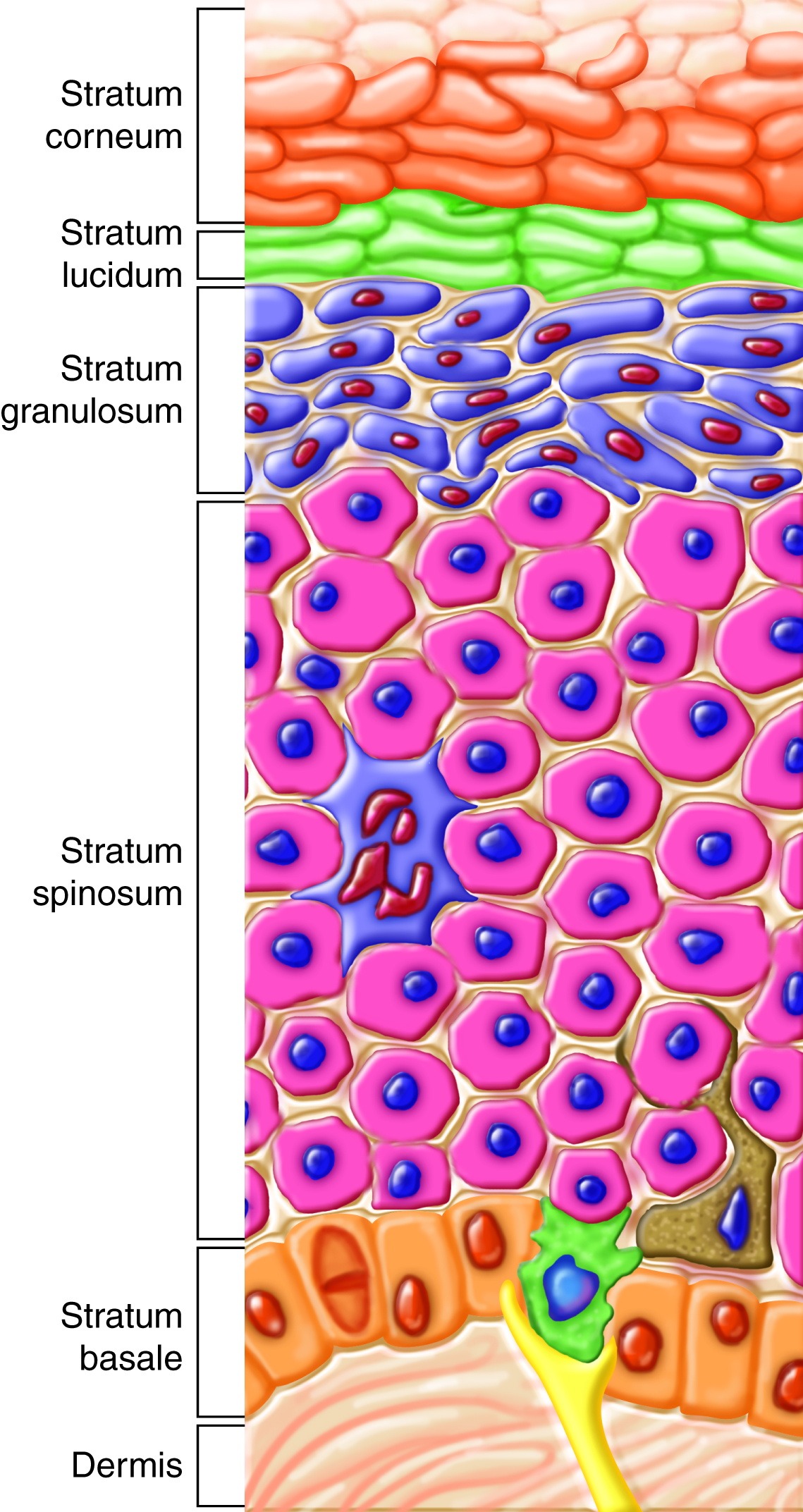
Stratum Basale
The stratum basale (also called stratum germinativum) is the deepest epidermal layer and attaches the epidermis to the basal lamina, below which lie the layers of the dermis. The stratum basale is primarily made up of a single layer of basal cells. These cells are considered to be stem cells. The function of this layer is to divide to replicate the cells that are lost from the surface. The daughter cells then differentiate into keratinocytes. Merkel cells and melanocytes are also dispersed among the basal cells in the stratum basale.
Fingerprints form in the growing fetus where the basal cells of the stratum basale meet the connective tissue of the underlying dermal layer (papillary layer). The basal cells form strong cell-to-cell junctions called desmosomes not only with adjacent cells, but also with the basal lamina between themselves and the underlying connective tissue. During development, some areas of basal cells divide at a different rate, forming epidermal ridges that extend down in the dermis, and the dermal tissue proliferates to form dermal papillae. This results in the formation of deep ridges that get transmitted through the other layers of the skin to form fingerprints on the surface. Fingerprints are unique to every individual and are used for forensic analysis because the patterns do not change with the growth and aging processes. Even identical twins with the same genes will have different fingerprints because of this random process.
Stratum Spinosum
As the name suggests, the stratum spinosum is spiny in appearance due to the polyhedral shape of the cells and desmosomes visible when tissue is prepared for microscope slides. As basal cells divide at different rates, keratinocytes get pushed up but maintain these strong cell-to-cell connections, changing cell shapes and forming a protective barrier. This stratum is composed of eight to 10 layers of keratinocytes, formed as a result of cell division in the stratum basale. Interspersed among the keratinocytes of this layer are the Langerhans cells, which help with immunity.
Stratum Granulosum
The stratum granulosum has a grainy appearance due to further changes to the keratinocytes as they move up from the stratum spinosum. The cells (three to five layers deep) become flatter, and their cell membranes thicken. At this point, the keratinocytes generate large amounts of the proteins keratin and keratohyalin in the cytoplasm and, with other lipids and enzymes, form vesicles called lamellar granules, which may be secreted by exocytosis. The cellular secretions act to retard water loss and entry of foreign materials. These two proteins eventually make up the entire mass of the keratinocytes in the stratum granulosum (the nuclei and other cell organelles disintegrate) and mark the transition between the metabolically active strata and the dead cells of the superficial strata.
Stratum Lucidum
The stratum lucidum appears lucid, or clear, and is not present throughout the body, but only on parts with thick skin, such as the surface of the palms and the soles of the feet. The stratum lucidum is a smooth, clear, thin layer, just superficial to the stratum granulosum. The keratinocytes in this layer are derived from the stratum granulosum, and mainly consist of keratin fibers. They are flat and densely packed.
Stratum Corneum
The stratum corneum is the most superficial layer of the epidermis, and is the layer that is exposed to the environment. The increased keratinization (also called “cornification”) of the cells in this layer gives it its name. There are usually 15 to 30 layers of dead cells in the stratum corneum. This dry, dead layer prevents the growth of microbes and keeps the rest of the underlying layers healthy. It is also resistant to penetration by water and protects the inner layers from environmental damage. Dead cells in this layer are shed periodically (approximately every two weeks) and are replaced by cells from the stratum granulosum (or stratum lucidum in the case of the palms and soles).
Epidermal layers
Example; Exfoliation
Exfoliation is the removal of the outermost layer of dead cells. Cosmetic procedures like microdermabrasion or chemical peels help remove some of the dry upper layer of the skin and aim to keep the skin looking “fresh” and healthy. The ancient Egyptians are credited with first discovering the beauty effects of exfoliation. Too much exfoliation can cause damage to underlying, living tissue.
Thick Versus Thin Skin
The thickness of thick skin is a function of the four upper layers of the epidermis: the stratum spinosum, stratum granulosum, stratum lucidum, and stratum corneum. The stratum corneum, consisting of keratin-packed dead cells, is substantially thicker in thick skin than in thin skin (more than 300 layers versus 15 layers of cells). The palms of your hands, soles of your feet, and your lips have thick skin. Thick skin is adapted to specialized activities, including gripping, walking and suckling, and the wear and tear that goes with those activities. Thick skin does not have hair, and has few glands.
Most of the rest of your skin is thin. The stratum lucidum isn’t even present in thin skin. The packed keratin provides most of the protective properties associated with the epidermis. Whereas the stratum corneum of thin skin may be completely shed and replaced in about a week, this replacement may take about a month in thick skin.
What is the advantage of not having oil on regions of thick skin including the hands?
Areas on the body that have thick skin require traction that would be prevented by oil, such as the hand gripping something.
Example: Calluses
When you wear shoes that do not fit well and are a constant source of abrasion on your toes, you tend to form calluses at the point of contact. This occurs because the basal stem cells in the stratum basale are triggered to divide more often. This increases the thickness of the skin at the point of abrasion so as to provide greater protection to the underlying tissue. Calluses can also form on your fingers if they are subject to constant mechanical stress like long periods of writing or playing stringed instruments or video games. The formation of calluses is an example of how tissues can adapt to a minor or local stress. Corns are a specialized form of calluses. They are formed due to the abrasion on the skin as a result of an elliptical-type motion.
Organ Level
Dermis
The skin’s dermis is made up of two distinct layers of connective tissue. The papillary layer is made up of areolar connective tissue and the underlying reticular layer is composed of dense irregular connective tissue. This dermal part of the skin (organ) is vasculated (has blood vessels) and is innervated (has nerves). As described earlier, the dermis is sparsely populated with fibroblasts that produce collagen and elastin fibers in the extracellular matrix. This leads to a strong and elastic tissue structure. The matrix can also contain mast cells involved in allergic reactions.
Papillary Layer
The fibroblasts are dispersed within the collagen and elastin fibers of the areolar tissue (loose connective tissue) of the papillary layer. This forms a loose mat, which contains an abundance of small blood vessels. The dermal papillae with blood capillaries interdigitate (become interlocked) with the epidermal ridges of the stratum basale. In addition, the papillary layer contains phagocytes — defensive cells that help fight bacteria or other infections that have breached the skin. This layer is also interspersed with lymph vessels and sensory receptors.
Reticular Layer
The reticular layer appears “reticulated” (net-like) because it is composed of a mesh of collagen fibers and elastin fibers. Fibrocytes form the bundles of collagen that extend into the papillary layer and the hypodermis, making these layers hard to distinguish. The flexible collagen provides structure and strength, while elastin lends limited elasticity to the skin. Collagen also binds with water, keeping the skin hydrated. Water is necessary to maintain the normal elasticity and resiliency (called”turgor”) of the skin. Dehydration causes a loss of turgor; if the skin of a dehydrated person is pinched it remains domed and does not immediately flatten out.
Collagen injections and Retin-A creams help restore skin turgor by introducing collagen externally in the former case or by stimulating blood flow and repair of the dermis in the latter case.Hypodermis
The hypodermis (also called the subcutis or subcutaneous layer) functions to connect the integument (epidermis and dermis) to the underlying muscles and organs. The hypodermis is not considered part of the skin, but has several important functions. Like the dermis, the hypodermis is made up of areolar tissue, collagen, and elastic fibers, providing it with some elasticity. Additionally, it contains adipose tissue, which functions as a mode of fat storage. The hypodermis is vascular and contains arteries, veins, and blood capillaries.
Adipose tissue present in the hypodermis accumulates fat, which serves as an energy reserve, insulates the body, and prevents heat loss. The fat distribution changes as our bodies mature and age. It is also hormone-dependent. Men tend to accumulate fat in different areas (neck, arms, lower back, and abdomen) than do women (breasts, hips, thighs, and buttocks). Physical inactivity due to a lack of exercise and sedentary jobs, combined with the consumption of high-calorie foods, has resulted in the highest rates of obesity ever seen in our country. While accumulation of fat provided an evolutionary advantage to our ancestors, who experienced unpredictable bouts of famine, it is now considered a major health threat. Improved diet and increased exercise are the best ways to control body fat accumulation, especially when it gets to levels that increase the risk of heart disease.
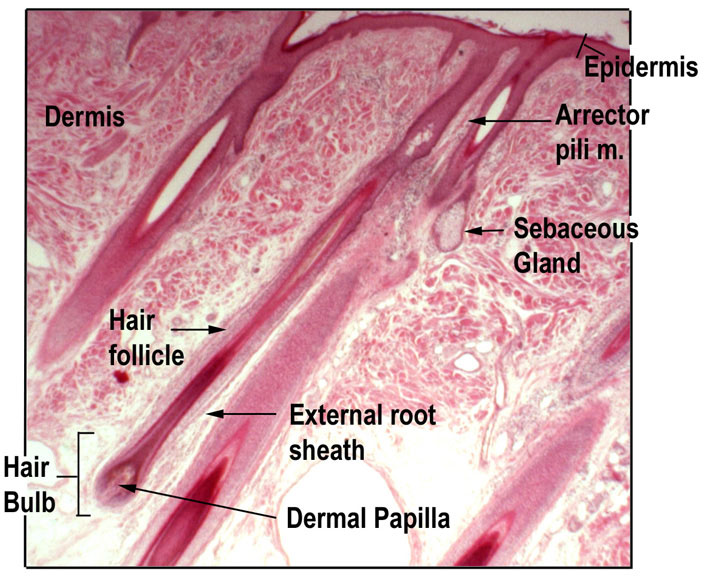
Accessory Structures
Accessory structures of the skin include hair, nails, sweat glands, and sebaceous glands. Although these structures appear to be part of the dermis, they are actually derived from the epidermis. The hair shaft is made of dead, keratinized cells and gets its color from melanin pigments. Nails are also keratinized and protect the extremities of our fingers and toes from mechanical damage. Sweat glands and sebaceous glands produce sweat and sebum, respectively. Each of these fluids has a role to play in maintaining homeostasis. Sweat helps the body remove excess fluids and electrolyte wastes and also cools down the body surface when it gets overheated. Sebum acts as a natural moisturizer of the dead, flaky outer keratin layer of skin and hair. Sebum is also known for its microbicidal and microbiostatic properties.
Hair
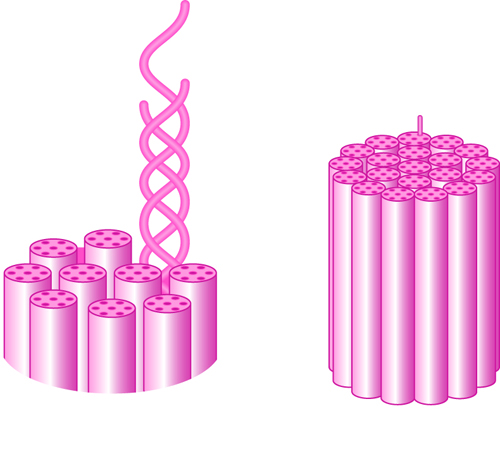
Hair is part of the integumentary system. Strands of hair originate from the base of the downward extension of living epithelial cells into the dermis that is called the hair follicle. Hair follicles are surrounded by the dermis, but the cells are part of the epidermis and are separated from the dermis by basal lamina layer. Hair forms in a manner similar to the skin: rapid division and differentiation of stem cells into keratinocytes that get pushed up and become flattened, dead, keratinized cells. The part of hair that is exposed on the skin surface is called the hair shaft, and the rest of the follicle is called the hair root. The bulge at the base of the hair root is called the hair bulb, which is made up of a layer of basal cells called the hair matrix. The hair matrix contains the cells that rapidly divide to form the hair. The hair bulb surrounds the hair papilla (made up of connective tissue, blood capillaries and nerve endings).
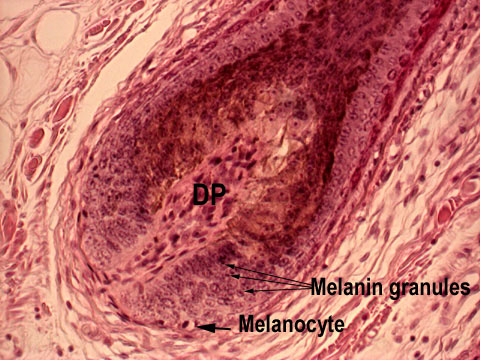 |
 |
Just as the layers of the skin form on the inner layers and get pushed out to the surface as the dead skin on the surface sheds, basal cells in the center of the hair bulb divide to form layers of keratinocytes that form the medulla, cortex, and cuticle of the hair bulb. These layers are visible in a longitudinal section of the hair follicle. Keratin formation starts in the cells of the medulla and the keratin continues to be produced in the cortex and cuticle. Keratinization is completed as the cells are pushed to the skin surface to form the shaft of hair that is externally visible. The external hair is composed entirely of keratin.
Additionally, the hair follicle is made up of three concentric layers that make up the wall of the follicle — the internal root sheath, the external root sheath, and the glassy membrane. The cells of the internal root sheath are derived from the basal cells of the hair matrix. This layer does not surround the entire hair strand, but stops short at the base of the hair shaft. The external root sheath, which encloses the hair root, is made up of basal cells at the base of the hair root and tends to be more keratinous in the upper regions. The glassy membrane is a thick, clear connective tissue sheath covering the hair root and connecting it to the tissue of the dermis.
Hair serves a variety of functions. For example, hair on the head protects it from the sun and from heat loss; and hair in the nose and ears and around the eyes (eyelashes) defends the body by trapping dust particles that may contain allergens and microbes. Hair on the eyebrows prevents sweat and other particles from bothering the eyes. Hair also has a sensory function due to innervation of the hair papilla. Hair is extremely sensitive to changes in the environment, much more so than the skin surface. The hair root is connected to smooth muscles called arrector pili that contract in response to stimuli, making the external hair shaft “stand up.” This is visible in humans as goose bumps and even more obvious in animals, such as when a frightened cat’s fur puffs out. In many animals, the puffing out makes the animal appear larger, and could possibly enable it to scare off a predator. Another advantage of this ability to cause the hair to stand up is that it can trap air and can act as an insulator, decreasing heat loss.
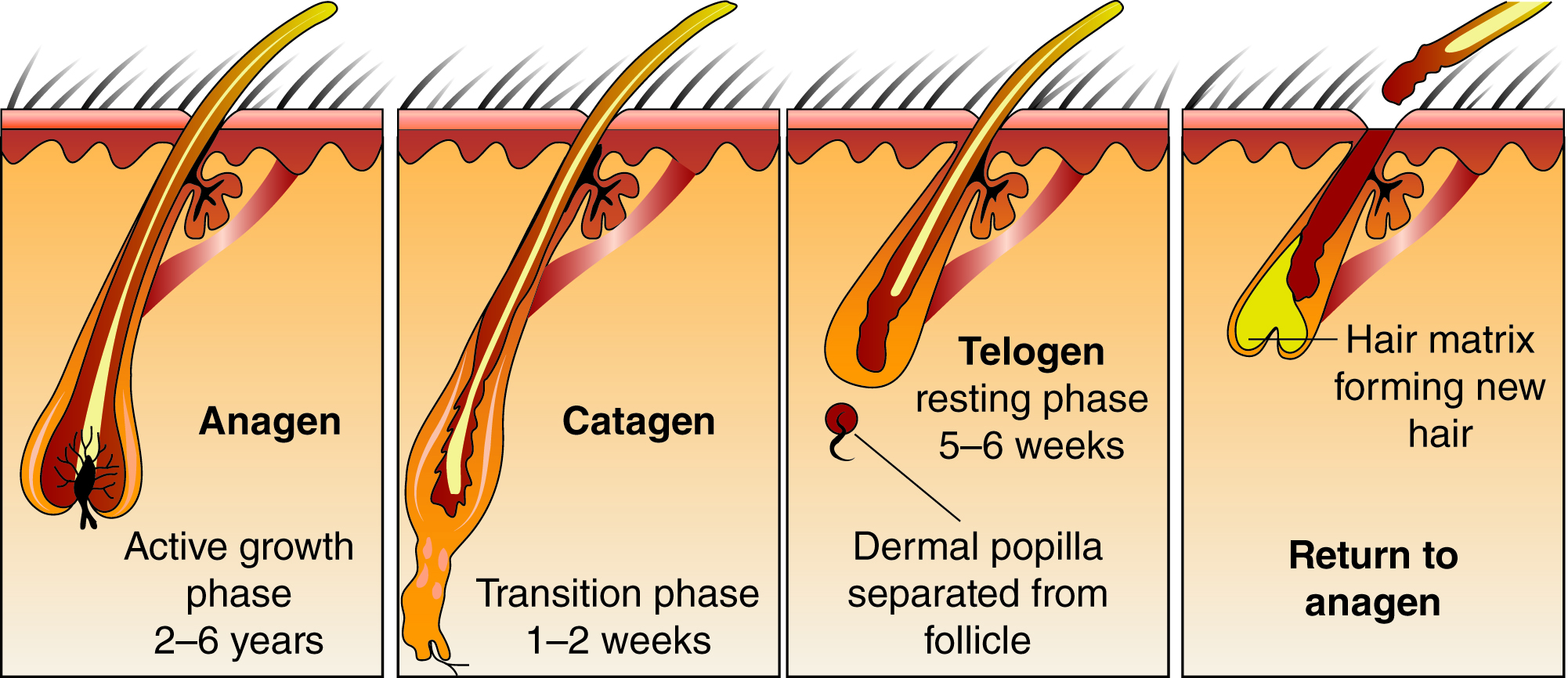
Hairs grow during a phase called anagen, and they are eventually shed, only to be replaced by newer ones. When hair is naturally ready to be shed, the follicle becomes inactive during a phase called catagen. The follicle then becomes smaller, and becomes detached from the dermal papilla at the base, during the phase called telogen. The basal cells in the hair matrix then produce a new hair follicle during anagen. Hair typically grows at the rate of 0.3 mm per day and can continue growing for two to five years before being shed. About 50 hairs may be lost and replaced per day. Hair loss occurs if there is more hair shed than what is replaced, and it can happen due to hormonal or dietary changes.
Just like the skin, hair gets its color from the pigment melanin, produced by melanocytes in the hair matrix. Different hair color results from differences in the type of melanin, which is genetically determined. As a person ages, the melanin production decreases and hair tends to lose its color, becoming gray and/or white.
Example: Alopecia
Many individuals can experience hair thinning and/or loss with advanced age. This is called alopecia. This can lead to complete hair loss, called baldness. Most baldness is caused by a genetic sensitivity of hair follicles to the androgen hormone dihydrotestosterone (DHT). DHT causes the hair follicle to receive less blood flow, so that the hair follicle begins to atrophy and any hair that is produced is thin.
A common form of baldness is male pattern baldness, which results from a mutation on the X chromosome. It is seen more often in men because men only receive one copy of the X chromosome. Many women may be carriers of this trait, having one normal X chromosome and one X chromosome that has the male pattern baldness gene. Women usually do not exhibit the balding patterns seen in men.
Nails
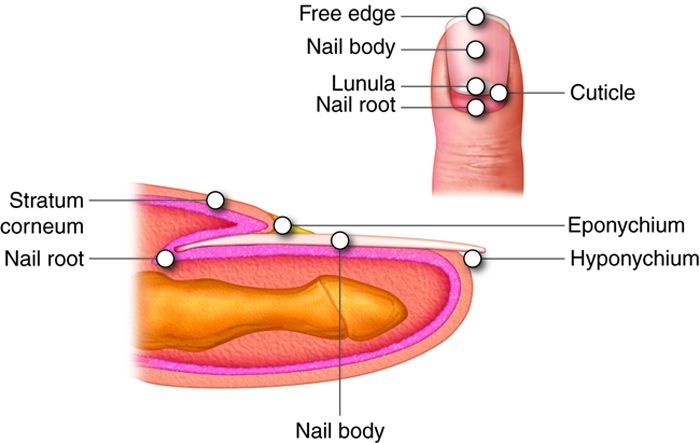
The nail is a specialized structure of the epidermis that occurs at the tips of our fingers and toes. The nail body is formed on the nail bed, and it is designed to protect the tips of our fingers and toes, as they are the farthest extremities and the parts of the body that experience the maximum mechanical stress. The epidermis in this part of the body has evolved a specialized structure upon which nails can form. The nail body forms at the nail root. Lateral nail folds, folds of skin that overlap the nail on its side, help anchor the nail body. The nail fold that meets the proximal end of the nail body forms the nail cuticle, also called the eponychium. The nail bed is rich in blood vessels, making it appear pink, except at the base, where there is a crescent-shaped region called the lunula. The nail body is composed of keratin-rich, densely packed dead keratinocytes. The area beneath the free edge of the nail, where debris gets lodged, is called the hyponychium.
Skin Glands and Secretions
Sweat (Sudoriferous Glands)
When the body becomes overheated, sweat is produced to cool the body’s temperature and prevent overheating. There are two types of sweat glands responsible for excreting sweat —eccrine (merocrine) sweat glands and apocrine sweat glands. Eccrine glands are present throughout the skin surface, especially on the palms of the hand, the soles of the feet, and the forehead. Like hair and nails, they are derived from the epidermis. They are coiled glands that lie in the dermis, with the duct opening to a pore on the skin surface, where the sweat is released(although some may open into hair follicles, like sebaceous glands). The sweat released by eccrine sweat glands is mostly water, with some salt, antibodies, traces of metabolic waste, and a microbe-killing compound called dermcidin. The main function of eccrine sweat glands is to help regulate body temperature through evaporation.
Eccrine glands are controlled by the sympathetic division of the autonomic nervous system. The sympathetic division is known as the “fight or flight” division. When you are nervous, you might notice that your palms sweat. This is because when the sympathetic division is activated, it triggers sweating.
Apocrine glands are usually associated with hair follicles and are activated in densely hairy areas like armpits and genitals. They are larger than merocrine sweat glands and lie deeper in the dermis, sometimes even reaching the hypodermis. They release a thicker fluid due to a higher concentration of fatty acids, which may give it a whitish color. These fats are often decomposed by bacteria on the skin, resulting in an unpleasant odor, commonly called body odor. Apocrine glands do not begin to function until puberty. Apocrine sweat glands are stimulated during emotional stress and sexual excitement.
Sebaceous Glands
Sebaceous glands are oil glands that are found all over the body. Most are associated with hair follicles. They generate and excrete a mixture of lipids, called sebum, onto the hair and skin surface, thereby naturally lubricating the dry and dead layer of keratinized cells of the stratum corneum and hair shaft. Sebum also has antibacterial properties, and prevents water loss from the skin in low-humidity environments. The secretion of sebum is stimulated by hormones, many of which do not become active until puberty. Thus, sebaceous glands are relatively inactive during childhood and become active only after puberty has occurred.
Example: Acne
Acne is a skin disturbance that typically occurs on areas of the skin that are rich in sebaceous glands (the face and back). It is most common during the onset of puberty due to associated hormonal changes, but can continue into adulthood. Hormones such as androgen and other sex steroid hormones stimulate the release of sebum. When sebaceous glands overproduce and get blocked with sebum, it leads to the formation of blackheads. Blackheads are the result of hyperkeratinization of the area, which causes the formation of a keratin plug and blockage of hair follicles in the area. Blackheads are prone to infection by acne-causing bacteria (i.e. Propionibacteriumand Staphylococcus), which leads to redness and swelling. In severe cases, acne can lead to scarring due to the production of scar tissue during the wound healing process.

