30 Skeletal Homeostasis
The skeletal system provides an excellent example of homeostasis. From the time that we are born, our skeleton must be sufficiently robust to provide stature, protect our soft internal organs and provide a mechanical resistance for our muscles to pull on. However, in addition to the constant need for the skeleton to maintain its function, it must also constantly remodel, otherwise we could not grow. Even in adulthood we constantly develop microfractures that need to be repaired.
Maintaining Calcium Levels in the Bone
The body uses the bones not only for structure and protection, but also for calcium storage. Approximately 99 percent of the body’s calcium is stored in the bone, and calcium plays an important role in most of the body’s functions. Free calcium levels must remain at a set point for proper body functions. The extracellular levels of calcium are affected by calcium intake from foods, excretion of calcium as waste, and the storage and release of calcium from the bones. Hormones regulate these processes to maintain balanced calcium levels in the extracellular fluid, which is necessary to maintain homeostasis.
Small changes in blood calcium levels can have significant effects on body function. For example, if extracellular calcium levels are too low, the nervous system becomes overexcited, resulting in tetany (rigid, locked muscles). On the other hand, if calcium levels in the body are above normal, the nervous system becomes sluggish. Muscle activity of the heart and gastrointestinal tract slows down.
Milk and dark green vegetables are rich in calcium, and an adequate supply of calcium helps maintain healthy bones. When we eat calcium-rich foods, some calcium is absorbed into the small intestinal wall, and some of the calcium becomes soluble in the blood stream. However, calcium and other divalent cations (ions that are missing two electrons) are poorly absorbed by the small intestine. For this reason, vitamin D is an important dietary supplement. Vitamin D increases calcium absorption in the small intestine.
By altering the function of the osteoblasts and osteoclasts, hormones help regulate calcium levels in the blood. There are three hormones that control osteoblast and osteoclast activity:
- parathyroid hormone or PTH, which increases bone resorption by stimulating osteoclasts, leading to increased calcium release from bone.
- calcitonin, which acts in children to decrease bone resorption, leading to less calcium entering the blood.
- calcitriol, (vitamin D) which increases absorption of dietary calcium.
Parathyroid hormone (produced in the parathyroid glands) controls extracellular calcium by regulating how calcium is reabsorbed in the intestines, excreted from the body, and exchanged between the extracellular fluid and the bone. The cells of the parathyroid gland synthesize and release parathyroid hormone in response to low blood calcium levels. To bring blood calcium levels into the normal range, the release of parathyroid hormone stimulates osteoclasts to reabsorb bone mineral, therefore releasing calcium into the blood. Parathyroid hormone also enhances calcium absorption by the intestines, and prevents calcium loss in urine to increase calcium levels in the blood. When parathyroid cells sense that blood calcium levels are above normal, cellular receptors are activated and the synthesis and release of parathyroid hormone is inhibited.
Calcitonin is produced in the thyroid gland. The function of this hormone is to decrease bone resorption and retain calcium in the bones. Therefore, the effects of calcitonin counteract the effects of parathyroid hormone. When blood calcium levels are high, the thyroid releases calcitonin into the blood. Calcitonin decreases bone resorption by decreasing the activity of osteoclasts and decreasing the formation of new osteoclasts. In this way, calcitonin shifts the bone balance in favor of bone deposition, which requires the removal of calcium from the blood and into the bone. Calcitonin also has minor effects on how the intestines and kidney tubules handle calcium. In adult humans, calcitonin has weak effects on the regulation of calcium levels. We know this because if the thyroid gland is removed, calcium levels are not adversely affected.
Other Important Regulatory Factors
Vitamin D is a group of lipid soluble compounds involved in calcium regulation. Vitamin D can be made in the skin through exposure to sunlight, or acquired from the diet and dietary supplements. Under the influence of the parathyroid hormone, vitamin D is converted to an active molecule, calcitriol. Calcitriol circulates through the blood to maintain normal blood calcium levels. When your body does not have sufficient levels of calcitriol, the intestines do not absorb as much calcium, and blood calcium levels decrease. Vitamin D also inhibits calcium loss in urine.
The activity of osteoblasts and osteoclasts in the bone is tightly regulated by the activity of the parathyroid hormone, calcitonin and vitamin D. Nutritional deficiencies in vitamin D, calcium or phosphate lead to a disease called osteomalacia.
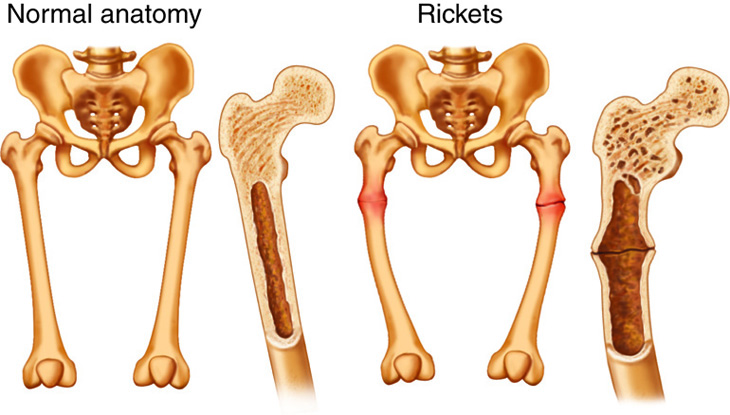
Osteomalacia (from osteo–, meaning “bone,” and mal-, meaning “bad”), also known as rickets when it occurs in children, is a disease that is most commonly caused by a lack of vitamin D in the body. Remember that vitamin D helps to increase the amount of calcium that the body absorbs and, as a result, helps the body build the mineralized extracellular matrix in bone tissue. If a person lacks sufficient vitamin D, calcium absorption is slowed, and bone growth is affected.
In children, the lack of calcium absorption prevents new bone tissue from ossifying properly. As a result, the bones become weak and rubbery. Because their bones are less able to support the body and withstand the pressure of the body’s weight, children with rickets may develop bowed legs and deformed skeletons.
In adults, osteomalacia prevents bones from healing and remodeling properly. Recall that bone tissue is being continually formed and broken down by osteoblasts and osteoclasts. If insufficient calcium is available, the new bone that forms may not calcify properly. As a result, the bones may become painful and brittle.
Osteoporosis is a condition in which the balance between calcium deposition and calcium loss in bones is disrupted. In people with osteoporosis, the bones lose more calcium than they deposit. As a result, the bones become brittle and break easily.
Osteoporosis is most common in post-menopausal women. As a woman goes through menopause, her levels of estrogen decrease significantly. Estrogen and testosterone are important hormones that affect the reproductive system, but they also can stimulate osteoblast activity. As concentrations of these hormones decrease, osteoblasts become less active, and less calcium is deposited in the extracellular matrix. In addition to resulting in weak bones, this is also an issue because there is a reduced reserve of calcium in the body for other tissues.
Osteoporosis can be affected by diet and lifestyle. People who consume very little calcium and vitamin D are at increased risk of osteoporosis. (For example, women with anorexia nervosa, who eat very little, may develop osteoporosis in their late twenties and thirties.) Weight-bearing exercise, such as running, helps to build bone mass and can reduce the chances of developing osteoporosis.
Bone Response to Force
You learned that osteocytes become embedded within bone matrix during mineralization. Within bone lamellae, osteocytes interact with each other through a network of cellular extensions. These extensions, found in a network of canals referred to as canaliculi, allow external mechanical information to be rapidly transmitted to many osteocytes. The response of osteocytes to mechanical force allows our skeletal system to maintain itself.
When bone experiences a mechanical force, this force is transmitted to the fluids and cells within the bone. The forces on the fluids are then transferred through the spaces of the canaliculi down to the osteocytes. In response to the received forces, osteocytes generate a force on the bone tissue. Therefore, the cells and bone matrix constantly respond to each other’s mechanical force input.
Osteocytes in bone tissue act as mechanical strain sensors to convert information about mechanical force into chemical messages. These chemical messages control osteoblast and osteoclast activity and can result in either bone deposition or bone resorption, also known as osteolysis. In response to mechanical force, a two-step process occurs. First, mechanically sensitive membrane proteins on the surface of the osteocytes are activated. Second, chemical pathways within the osteocytes are activated. Activation of these intracellular pathways stimulates osteoblast activity and inhibits osteoclast activity.
As you learned earlier, bone ECM (extracellular matrix) maintains the mechanical structure and functional properties of bone tissue. The collagen fibers of bone ECM are under constant tension so that the bone ECM is always ready to respond to mechanical force. Because osteocytes are attached to the ECM, the tension felt by the collagen fibers is balanced by the tension that osteocytes place on the ECM. Therefore, osteocytes sense mechanical force and transmit this force to the surrounding ECM. Bone ECM is constantly remodeled to maintain optimal strength for applied mechanical force.
Mechanical forces control osteoblast and osteoclast activity through feedback from the osteocytes and the ECM. One common type of mechanical force is physical activity. Another force that is not as obvious is body mass. With increased mechanical force, such as physical activity or weight gain, bone ECM increases to support the force. When the mechanical force applied to bone is too high, osteocytes within bone matrix signal for remodeling through bone resorption and bone deposition.
People who routinely lift heavy loads have very strong bones, but the body spends a lot of energy to maintain these stronger bones. On the other hand, sedentary individuals may lose bone density and strength. However, that can be a problem: a lack of exercise, extended bed rest and space travel (for astronauts), during which there is little or no force on bones because of inactivity or weightlessness, can cause a significant loss of bone mass.
Homeostasis of Cartilage
You have learned in relation to ossification how cartilage and bone are inherently integrated. Both tissue types are also some of the most force-responsive in the body. This is necessary to maintain stature. Chondrocytes sense force and changes in water movement—associated with the force-induced movement of water—and secrete the appropriate collagen and proteoglycan extracellular matrix proteins.
Recall that cartilage is composed primarily of a network of elastic type II collagen fibers embedded in gel-like proteoglycans. Water, electrolytes, and chondrocytes are interspersed within the network. The physical properties of collagen and proteoglycans are largely responsible for the ability of cartilage to respond flexibly to force.
Collagen fibers have significant tensile strength, which means that they can withstand a lot of tension (pulling) without damage. However, collagen fibers have very little compressive strength—that is, under compression (squeezing), they bend easily. You can think of a collagen fiber as a rubber band or string. If you pull on a rubber band, it stretches easily, and then returns to its original shape when you stop pulling. However, if you push on the ends of the rubber band, it folds up easily—it has minimal strength.
Collagen fibers are what give cartilage its strength. The cartilage in different areas of the body contains fibers that are arranged in different ways. The orientation and arrangement of the collagen fibers helps to give each region of cartilage strength to withstand specific types of stress. For example, articular cartilage—the cartilage that forms the articulating surfaces of joints, such as the knee—contains two main regions of collagen fiber orientation. At the surface of the cartilage, the fibers are arranged primarily parallel to the surface. Further from the surface, the fibers are arranged primarily perpendicular to the surface.
Proteoglycans are gel-like, elastic substances. They are highly resilient, which means that they deform easily under stress, but return to their original shape when the stress is removed. Proteoglycans give cartilage its resiliency and elasticity.
The combination of strength and elasticity allows cartilage to respond flexibly and quickly to forces placed on it. For example, the cartilage in your knee can support up to eight to 10 times your body weight for short periods without being damaged. As more force acts on the cartilage, it compresses. Its elasticity allows it to distribute the force evenly, and its strength allows it to withstand the stress without breaking or collapsing. When the stress is removed, the cartilage returns to its original shape. The physical movement of the water in the cartilage also helps to distribute the force of compression.
Cartilage is less complex in response to force than bone, which has multiple integrated cell types. Cartilage is less regulated by hormones, is difficult to overgrow, and grows extremely slowly. Part of the reason for slow growth is a limited amount of nutrients. Cartilage is avascular (a- means “none”), so there are no blood vessels or blood supply to the interior of the cartilage, so nutrient travel is limited to diffusion, and growth is limited.
Arthritis (from arthro–, meaning “joint,” and –itis, meaning “inflammation”) is any inflammation of the cartilage and/or bone tissue within a joint. The most common form of arthritis is osteoarthritis, which is caused primarily by physical damage to the cartilage that cushions many joints. The damage may be caused by a decrease in cartilage flexibility and water content as a person ages, but it may also be a secondary result of a variety of other conditions (including diabetes and mechanical injury to the joint). Osteoarthritis is most common in the elderly, but can affect younger people as well.
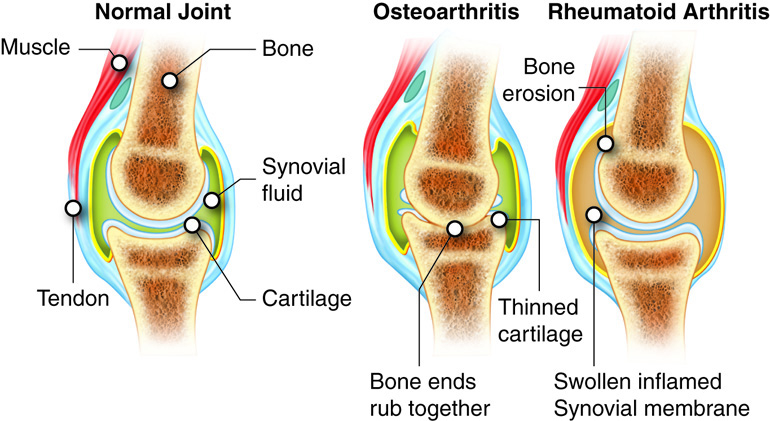
Osteoarthritis begins with physical damage to cartilage tissue in the joints. The damage may be cellular (such as damage cause by an infection), or it may occur at the tissue level. The damage causes the cartilage to break down. As the cartilage breaks down, friction within the joint increases; in severe cases, the ends of the bones themselves may rub together, causing severe pain. Loss of cartilage can also reduce the flexibility of the joint. Pain and loss of flexibility typically cause a person to move the joint less; as a result, the muscles, tendons, and ligaments near the joint may weaken. This in turn can cause additional difficulty moving the joint.
A different form of arthritis that also causes joint pain, rheumatoid arthritis, is caused by inflammation of the membranes of the synovial capsule, not the articular cartilage.

