44 Cardiovascular Homeostasis
Local Control of Blood Flow
Autoregulation refers to a tissue’s ability to meet its metabolic needs by automatically altering its blood flow. Autoregulation is particularly important in organs such as the heart and skeletal muscles, whose need for oxygen, nutrients, and the removal of wastes during exercise can be up to 10 times higher than when the body is at rest. In addition to increasing perfusion in the heart and muscles during physical activity, autoregulation manages regional blood flow to other tissues as well, including the brain. Individual mental and physical tasks require significantly different patterns of blood distribution. When a person is on the telephone, for example, motor speech areas of the brain receive more blood when talking, and auditory areas get more blood flow when listening. Autoregulatory changes in blood flow occur in response to local signaling molecules that cause constriction or dilation of local arterioles.
Vasoconstrictors and Vasodilators
The diameter of blood vessels can be changed by chemicals secreted by various cells, such as white blood cells, smooth muscle cells, platelets, endothelial cells, and macrophages. Metabolically active tissue cells can release vasodilating chemicals such as potassium ions, hydrogen ions, lactic acid, and adenosine. Endothelial cells can also release the vasodilator nitric oxide. Tissue that is injured or inflamed secrete vasodilating compounds of the prostaglandin family. Chemicals that cause vasoconstriction include serotonin (released from platelets) and endothelins (from endothelial cells).
Changes in local oxygen concentrations elicit two very different autoregulatory reactions in the pulmonary and systemic circulations. In the systemic circulation, decreased oxygen levels in the tissues cause blood vessels to dilate, increasing the delivery of oxygen. In the pulmonary circulation, low oxygen levels in poorly ventilated alveoli cause the blood vessels feeding those alveoli to constrict. As a result, blood avoids most of the alveoli in the lungs that have poor ventilation. Instead, most blood flows to well-ventilated alveoli.
Heart Attack and Congestive Heart Failure
Cardiac output is homeostatically maintained throughout our lifetime so that it constantly meets the needs of the body’s tissues. When the heart becomes damaged, such as after a heart attack, it may not be able to maintain adequate flow. This causes blood pressure to fall, initiating homeostatic feedback loops to try to bring blood pressure (and cardiac output) back to normal.
One way that the heart can become damaged is through a heart attack. This occurs when coronary blood vessels, which supply the cells of the heart itself with oxygen and nutrients, become significantly narrowed or completely blocked with a combination of plaque and thrombus (clot). During a heart attack, cells lack oxygen, causing them to die. If enough heart muscle cells die, the heart weakens so that it can’t pump as much blood, leading to the various negative effects associated with this condition.
Congestive heart failure is another common condition affecting cardiac output. It may develop after someone has a heart attack, or as a consequence of many other cardiac conditions. The problem with congestive heart failure is that the heart muscle is weakened to the point that it doesn’t do a good job pumping out the blood that is flowing into it (the blood flowing into the heart is called venous return). In fact, one of the main feedback loops that regulates blood pressure does so by adjusting the amount of blood in the body. This is because the more blood we have, the greater our venous return, and the higher the cardiac output – assuming a healthy heart. With the weakened heart associated with congestive heart failure, more venous return can actually lead to less cardiac output. A lowered cardiac output decreases blood pressure, signaling the body to increase blood volume, increasing venous return, and making cardiac output lower still. Because this loop continually makes the problem with cardiac output and blood pressure worse, it is a positive feedback loop – and not one we want to experience. Treatment focuses on preventing further progression and easing symptoms with methods such as oxygen delivery, medications, and palliative care.
Aging and The Circulatory System
Arterial walls change with age. Arteries that undergo significant changes include the large elastic vessels such as the aorta, the coronary arteries, and the carotid arteries. Arteriosclerosis refers to conditions that make arteries less elastic (commonly referred to as hardening of the arteries). This commonly occurs as we age because of calcium deposition in the walls of vessels (calcific arteriosclerosis), or degenerative loss of elastic fibers with age (senile arteriosclerosis).
Atherosclerosis is a specific type of arteriosclerosis that involves the formation of plaques on arterial walls that make them stiffer. Plaques are made of fatty material containing cholesterol. This fatty substance may eventually be replaced with connective tissue and deposits of calcium. Plaques can rupture, initiating a blood clot at the site. Both arteriosclerosis and atherosclerosis increase resistance to blood flow. Atherosclerosis in blood vessels that supply the brain can reduce blood flow to the brain, causing brain cells to malfunction or die if the reduction in flow is severe enough. Arteriosclerosis and atherosclerosis can also lead to poor wound healing. These conditions are usually firmly diagnosed with vascular imaging methods.
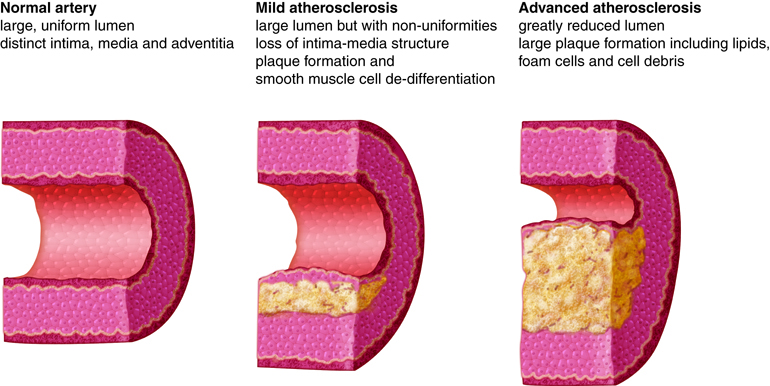
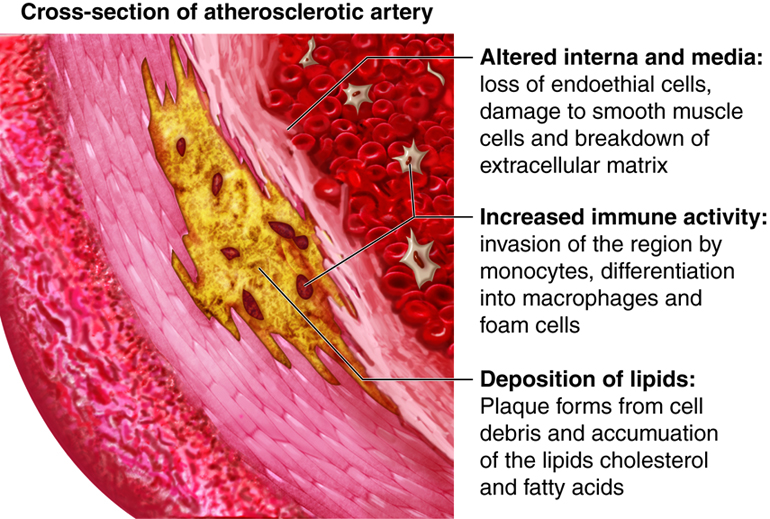
A main contributor to the development of atherosclerosis is high levels of low density lipoprotein (LDL or “bad” cholesterol) in the bloodstream. LDL typically rises with increased dietary saturated fat and decreased exercise. Because atherosclerosis is the main culprit of coronary artery disease, which is a leading cause of heart disease and death in the elderly, it is recommended that cholesterol levels be monitored with lipid profiles conducted every five years beginning at the age of 20.
Other Homeostatic Imbalances of the Cardiovascular System
We have discussed mechanisms within the heart that regulate cardiac output. For example, an increased heart muscle contraction will increase with an increase in venous return. Thus the healthy heart can pump more blood when there is more blood to pump.
There are other controls of heart function and cardiac output from the nervous system and endocrine system, which we will discuss in the integration of systems. It is important to note that we do not consciously change our heart rate or cardiac output. Instead we can indirectly adjust the nervous and endocrine feedback loops by initiating activities such as exercise or relaxation techniques.
Homeostatic Imbalances of the Plasma Constituents
Although most people realize the importance of red blood cells in distributing oxygen to the body’s tissues, it is important to realize that the plasma (non-cellular) fraction of blood is also critically important. One function of the plasma is to form blood clots when blood vessels are cut or torn in order to prevent excessive blood loss. Blood clotting needs to be limited to the vessels that are damaged in order for the system to function appropriately. Disseminated intravascular coagulation (DIC) is a serious condition in which the clotting cascade becomes activated in many non-injured blood vessels at one time. This occurs secondary to a significant insult to the body such as burns, cancer, infections, etc. With this generalized activation of the clotting cascade, small blood clots are formed, some of which limit or block off the flow of blood within vessels. This cuts off the flow of oxygen to organs, and if prolonged, can results in tissue necrosis (cell death), and the organ may stop functioning altogether. The random coagulation throughout the body leads to the coagulation proteins, as well as platelets, being used up, lowering the concentration of the essential clotting factors in the plasma. Once the coagulation process is disrupted, the patient suffers from abnormal bleeding from GI tract, respiratory tracts, and from the tiniest wounds in the body.
Homeostatic Imbalances of Red Blood Cell Concentration
Red blood cell concentration is sensitive to changes in oxygen levels. Prolonged exposure to low oxygen causes increased production of RBCs, raising the concentration of red blood cells in the blood (known as hematocrit), in order to maintain homeostatic oxygenation of the tissues. However, hematocrit levels that get too high can also lead to dysfunction, leading to a condition called polycythemia. With polycythemia, the blood will have increased viscosity, making it thicker and harder for the heart to pump this blood through the body. This can lead to heart failure in severe cases. Polycythemia can either be primary, where it is associated with an abnormality in the bone marrow that causes overproduction of red blood cells, or secondary, where red blood cell production is normally stimulated, but continues to the point of developing polycythemia.
An example of secondary polycythemia is chronic mountain sickness (Monge’s disease), which is an uncommon condition that occurs in certain people living at high altitudes (above 12,000 feet) for months or years. At higher altitudes, the atmospheric pressure decreases, resulting in less oxygen availability due to lower partial pressure of oxygen in the atmosphere. This stimulates RBC production to bring people to a slightly higher hematocrit, which then levels off. In those that develop polycythemia, their RBC production continues over time, making their hematocrit very high. As mentioned previously, as their hematocrit increases, so does blood viscosity. An increase in viscosity makes it more difficult for blood to move through blood vessels and results in the heart pumping vigorously to get blood circulating through the body. This increased resistance of blood places an excessive strain on the heart that may lead to inadequate pumping of blood and decreased oxygenation of tissue. This can lead to cardiac ischemia and hypertension due to the body’s effort to return to homeostasis. Treating chronic altitude illness requires the removal of blood (about a pint) as a form of temporary relief. However, the only effective form of treatment is to descend to a lower altitude.
Homeostatic Imbalances Caused by Vessel Dysfunction
The tissues throughout the body regulate flow to themselves by sending signals that can constrict or dilate the blood vessels that “feed” them. If these vessels don’t have an ability to make the adjustments, the tissues won’t be able to appropriately match blood flow with their metabolic activity.
One example of this is stable angina, where people experience chest pain on exertion. Stable angina is associated with atherosclerotic plaque that has developed in the main coronary arteries, which deliver flow to the cardiac muscle. Because of the plaque, these vessels can’t dilate appropriately when the needs of the heart muscle increases. Any type of increase in physical activity is not met with the normal coronary artery vasodilation in these individuals. This leads to low oxygen levels in their tissues, which can cause pain, as well as prevent the heart from functioning optimally, limiting their activity level.

