22 Homeostatic Maintenance
You have read about general and specific examples of homeostasis, including positive and negative feedback, and have learned the terminology that is used to describe parts of the feedback loops. It is important to become comfortable with the terminology since it will be used to introduce new concepts in upcoming sections of this course.
Maintaining homeostasis within the body is important for proper physiological function. It is important to recognize the mechanisms of homeostasis in the body, as well as the consequences of homeostasis dysfunction.
In the following examples, you will learn to identify homeostasis at different levels of organization, such as how the body maintains tight control over small molecules, and the importance of maintaining cell number.
Homeostasis of Ions
Body functions such as regulation of the heartbeat, contraction of muscles, activation of enzymes, and cellular communication require tightly regulated calcium levels. Normally, we get a lot of calcium from our diet. The small intestine absorbs calcium from digested food.
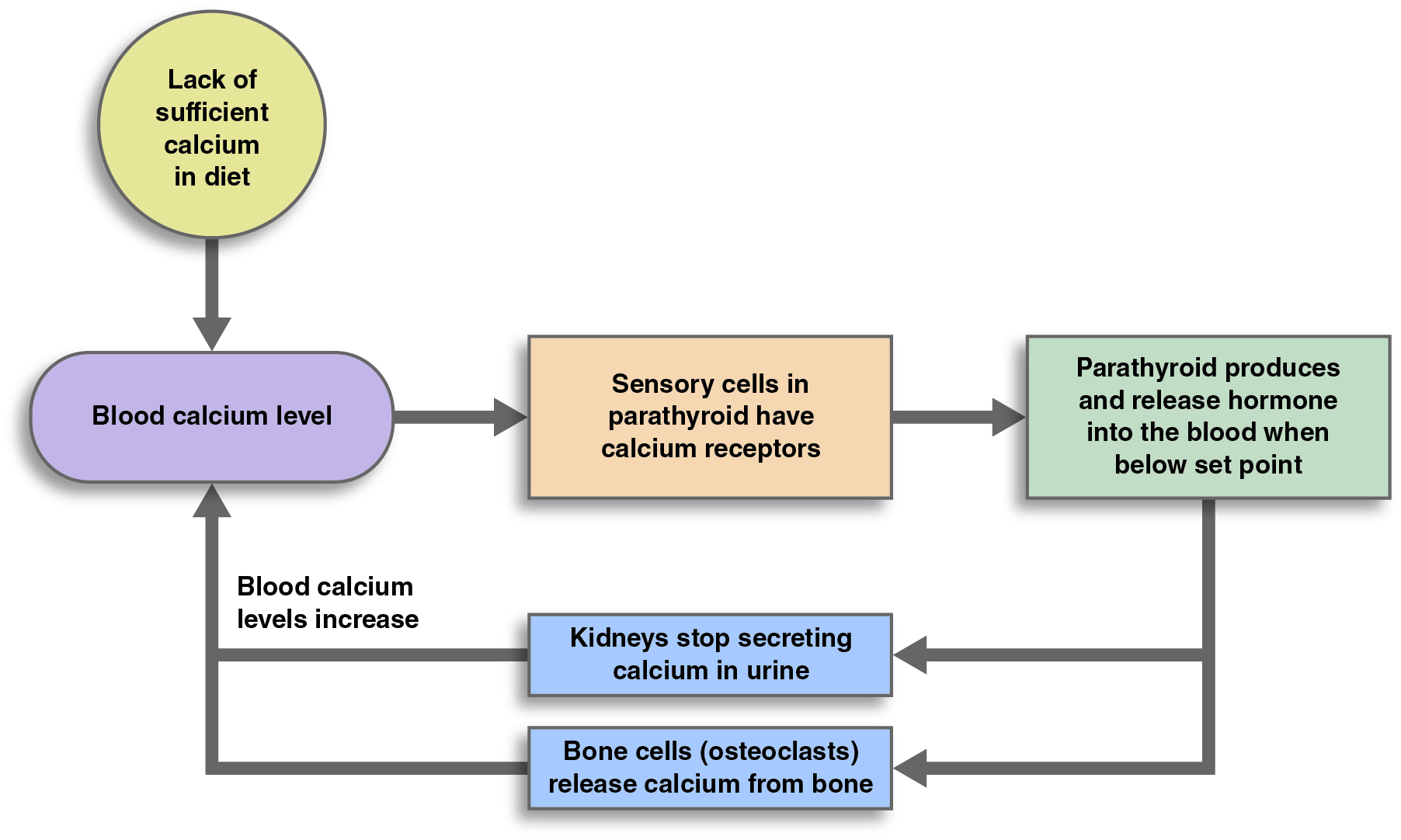
The endocrine system is the control center for regulating blood calcium homeostasis. The parathyroid and thyroid glands contain receptors that respond to levels of calcium in the blood. In this feedback system, blood calcium level is the variable, because it changes in response to the environment. Changes in blood calcium level have the following effects:
When blood calcium is low, the parathyroid gland secretes parathyroid hormone. This hormone causes effector organs (the kidneys and bones) to respond. The kidneys prevent calcium from being excreted in the urine. Osteoclasts in bones breakdown bone tissue and release calcium. When blood calcium levels are high, less parathyroid hormone is released. Parathyroid hormone is the main controller of blood plasma calcium levels in adults.
A second hormone that contributes to calcium regulation is called calcitonin. It is released from the thyroid gland when blood calcium levels are high. Calcitonin prevents bone breakdown and causes the kidneys to reabsorb less calcium from the filtrate, allowing excess calcium to be removed from the body in urine.
Calcium imbalance in the blood can lead to disease or even death. Hypocalcemia refers to low blood calcium levels. Signs of hypocalcemia include muscle spasms and heart malfunctions. Hypercalcemia occurs when blood calcium levels are higher than normal. Hypercalcemia can also cause heart malfunction as well as muscle weakness and kidney stones.
Homeostasis of Molecules
Glucose is an important energy source used by most cells in the body, especially muscles. Without glucose, the body “starves”, but if there is too much glucose, problems occur in the kidneys, eyes, and even with the immune response. Insulin is a hormone produced by the pancreas in response to increased blood glucose levels. When the pancreas releases insulin, it acts as a key to open passageways for glucose to enter all body cells, where it is used for energy production. The liver also plays an important role in this feedback loop. Excess glucose is used by liver and muscle cells to synthesize glycogen for storage. The pancreas also produces the hormone glucagon. Glucagon is released when blood glucose levels decrease and stimulates liver cells to catabolize glycogen back to glucose, which is then released into the blood to bring blood glucose levels back up.
Control of Cell Number
Although homeostasis is often carried out by a negative feedback loop with an identifiable receptor, control center and effectors, it more broadly means maintaining variables in a range suitable for optimal function. This includes the regulation of cell number in our tissues so that we don’t have too few or too many. It may be hard to identify specific components of a feedback loop, but it is clear that there are at least negative feedback cycles that help maintain cell numbers. This negative feedback is known to occur through cell-to-cell communications of neighboring cells and an ability to sense the levels of nutrients and matrix in the area they are growing in. Normally cells will stop dividing when there is an appropriate number of cells in a tissue or space. If a neighboring cell is lost or if there is an inadequate number of cells, cells may be stimulated to divide. Cells with too many neighbors trigger an internal response to die in a regulated programmed way called apoptosis. When cells sense they have no neighbors, signals in the nucleus cause division of the cell.
Homeostasis Integration of Systems
Each organ system performs specific functions for the body, and each organ system is typically studied independently. However, the organ systems also work together to help the body maintain homeostasis.
Example: Water Levels
For example, the cardiovascular, urinary, and lymphatic systems all help the body control water balance. The cardiovascular and lymphatic systems transport fluids throughout the body and help sense both solute and water levels and regulate pressure. If the water level gets too high, the urinary system produces more dilute urine (urine with a higher water content) to help eliminate the excess water. If the water level gets too low, more concentrated urine is produced so that water is conserved. The digestive system also plays a role with variable water absorption. Water can be lost through the integumentary and respiratory systems, but that loss is not directly involved in maintaining body fluids and is usually associated with other homeostatic mechanisms.
Internal Temperatures
Similarly, the cardiovascular, integumentary, respiratory, and muscular systems work together to help the body maintain a stable internal temperature. If body temperature rises, blood vessels in the skin dilate, allowing more blood to flow near the skin’s surface. This allows heat to dissipate through the skin and into the surrounding air. The skin may also produce sweat if the body gets too hot; when the sweat evaporates, it helps to cool the body. Rapid breathing can also help the body eliminate excess heat. Together, these responses to increased body temperature explain why you sweat, pant, and become red in the face when you exercise hard. (Heavy breathing during exercise is also one way the body gets more oxygen to your muscles, and gets rid of the extra carbon dioxide produced by the muscles.)
Conversely, if your body is too cold, blood vessels in the skin contract, and blood flow to the extremities (arms and legs) slows. Muscles contract and relax rapidly, which generates heat to keep you warm. The hair on your skin rises, trapping more air, which is a good insulator, near your skin. These responses to decreased body temperature explain why you shiver, get “goose bumps,” and have cold, pale extremities when you are cold.
Development of a fever is an interesting situation. Although it may appear that fever is caused by a disrupted feedback loop, it is actually a situation in which the temperature set point of the body changes and the feedback loop continues to operate normally. This causes body temperature to increase similar to the way that the temperature in your home will increase if you turn up the thermostat.
In extreme cases, a fever can be a medical emergency; but fever is an adaptive physiological response of our body to certain infectious agents. Pyrogens are molecules that cause the temperature set point to change. These pyrogens can come from microorganisms that infect you, or they can be produced by your body cells in response to an infection of some sort.
Fuel for Body Functions
As you have learned, blood glucose homeostasis is regulated by two hormones from the pancreas. This glucose provides the fuel for ATP production by all body cells. But the endocrine system is not the only system involved.
Many body cells respond to insulin and glucagon, but the liver of the digestive system plays in important role in ensuring the availability of fuel in-between meals. Under the influence of insulin, the anabolic process of glycogenesis (-genesis means “origin” or “birth”) in the liver converts excess glucose entering liver cells to polymerize into glycogen for storage. Under the influence of glucagon, the reverse catabolic reaction of glycogenolysis (-lysis means “break up”) will convert the glycogen back into glucose for release into the blood stream. The liver cells can also perform gluconeogenesis (-neo means “new”), which creates glucose from non-carbohydrate sources, mainly from specific amino acids.
The nervous system also plays a role in maintaining blood glucose levels. When the stomach is empty and blood glucose levels are low, the digestive system receptors and the brain respond by making you feel hungry—your stomach may “growl,” and you may feel pain or discomfort in your midsection. These sensations prompt you to eat, which provides new nutrient sources to raise blood glucose levels. The exocrine part of the pancreas is also part of the digestive system. It produces enzymes that help digest the nutrients you have eaten so they can be absorbed by the small intestine into the blood. The circulatory system is important in transporting the glucose and pancreatic hormones in blood to all body cells.
Blood Calcium Levels
As you have learned, proper calcium levels are important for normal function of several systems. Calcium ions are used for blood clotting, the contraction of muscles, the activation of enzymes, and cellular communication. The parathyroid gland of the endocrine system is the main receptor and control center for blood calcium levels. When the parathyroid glands detect low blood calcium levels, they communicate with several organ systems and alter their function to restore blood calcium levels back to normal. The skeletal, urinary, and digestive systems all act as effectors to achieve this goal through negative feedback.
The release of parathyroid hormone from the endocrine system triggers osteoclasts of the skeletal system to breakdown (resorb) bone and release calcium into the blood. Similarly, this hormone causes the kidneys of the urinary system to reabsorb calcium and return it to the blood instead of excreting calcium into the urine. Through altered function of the kidneys to form active vitamin D, the small intestine of the digestive system increases the absorption of calcium.
When blood calcium levels are elevated, the parathyroid gland senses that as well. But in this case, instead of increasing its secretion of parathyroid hormone, it decreases secretion of the hormone. This decreases bone resorption, increases calcium levels in the urine and decreases calcium absorption in the intestines.

