47 Lymphatic Structures and Functions
Major Functions of the Lymphatic System
The lymphatic system is essential for our survival. This system has three main functions:
- To collect and recycle the excess interstitial fluid and its dissolved substances
- To absorb fats and other substances from the digestive tract (this topic will be discussed in the Digestive System Unit)
- To initiate and coordinate an immune response to remove cellular debris, bacteria, toxins, fungi, parasites, and viruses that accumulate in our bodies
Because this system has the two very different functions of maintaining the proper fluid balance in the body and protecting the body from harmful infections, we will begin its study by 1) investigating the lympathic vessels and lymph which function in fluid balance and then 2) investigate how these structures along with lymphatic cells, tissues and organs function in protecting the body from infections. Infection can be viewed as the invasion and multiplication of microorganisms that are not normally present within the body. An infection may remain at the location where it entered the body, or it may spread through the body via blood or lymphatic vessels. Immunity is the state of having sufficient defenses (resistance) against infections that might disrupt homeostasis. Immunity involves both non-specific, inherent components (innate immunity) and specific, acquired from previous exposure components (adaptive immunity).
It is important to realize that although immunity will be considered here in the context of human anatomy and physiology, it is not restricted to humans or animals. The ability to defend itself from “non-self” invaders appears as early as in bacteria defending themselves from viral attacks, and it is an inherent homeostatic mechanism present in all types of cells, plants, and animals. As organisms evolved, so did the immune system. Thus, while the innate system is present in all animals, only vertebrates present the adaptive response.
Lymph Tissue and Lymphatic Vessels
Like the circulatory system that carries blood throughout the body, the lymphatic system is made of a series of vessels, capillaries, and organs. These structures collect excess fluid and cellular debris from the tissues and return them back to the blood.
In the circulatory system, blood flows from arteries, through capillaries and into veins to be returned to the heart. On its way through the capillaries, some of the fluid passes out across the capillary wall and into the interstitial fluid in a process called capillary filtration. This filtration tends to occur across the arterial end of the capillary, with most of the filtered fluid being reabsorbed at the venous end of the capillary. This leaves a small amount of fluid that remains in the interstitial spaces between cells. This filtered fluid is mostly plasma plus any plasma proteins that might have leaked from the blood vessel as well. This excess interstitial fluid is collected by the lymphatic system. The fluid flows through the lymphatic vessels until it is returned to the circulatory system to again become a component of blood. Once interstitial fluid passes into lymphatic vessels, it is called lymph. Lymph is a clear, pale-yellow fluid connective tissue.
The lymphatic system consists of many different tissues and organs that are found throughout the body. Some organs provide the environment for the development and maturation of leukocytes. Other tissues and organs trap pathogen and are the sites where leukocytes can interact with the pathogen. The circulatory and lymphatic systems interact to connect these organs and tissues.
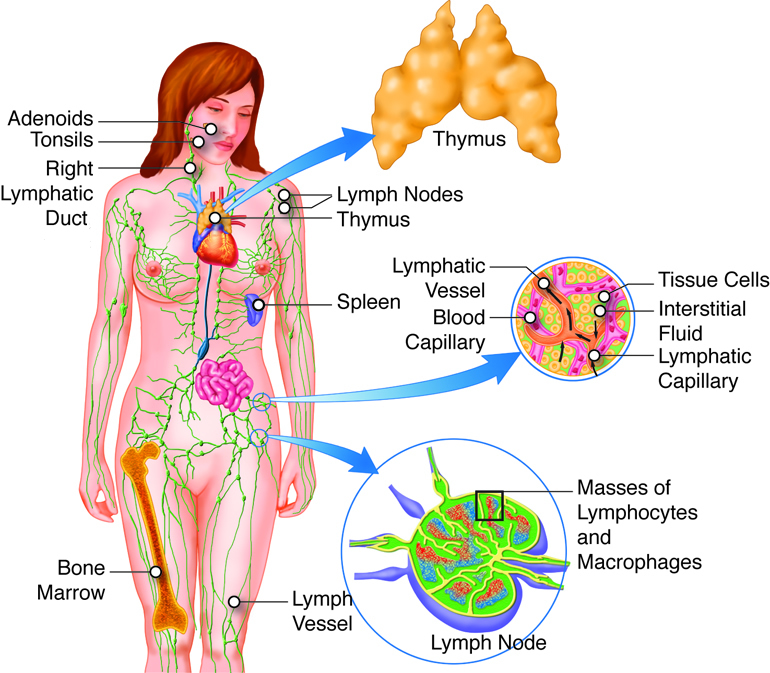
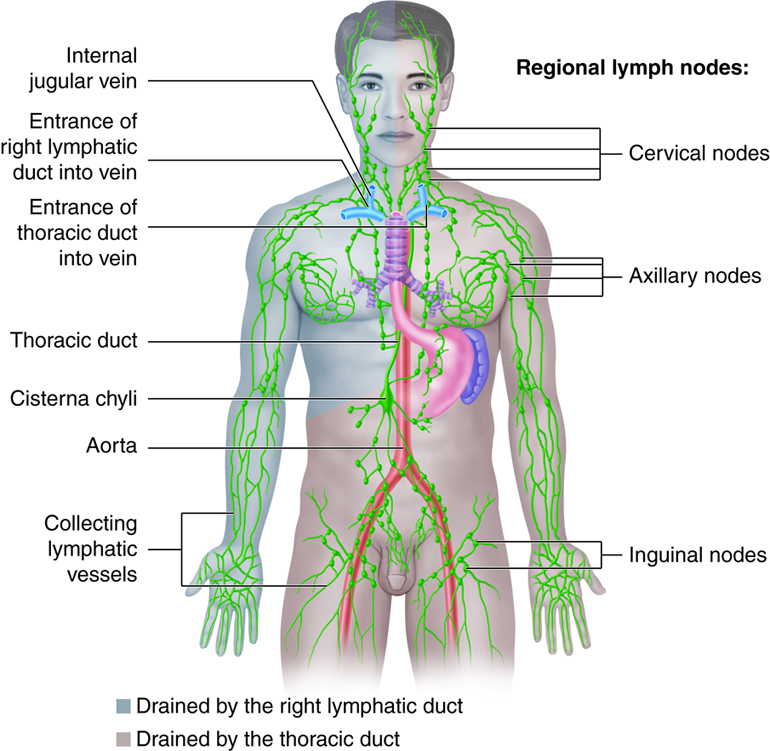
Fluid moves from blood capillaries into the interstitial spaces. Most of the fluid returns to the blood, but some of the fluid moves from the interstitial spaces into lymphatic capillaries to become lymph. To collect the lymph from the interstitial space, lymph capillaries originate in the blood capillary beds, and lymph vessels run parallel to the veins. At intervals along the lymphatic vessels, lymph flows through lymph nodes. Fluid collected in the lymph system is returned to the heart via veins in the chest. Unlike the circulatory system, the lymphatic system does not flow through a closed, circular system. There are no lymph arteries. Lymph fluid is not pumped around the body. Instead, the lymph system collects the lymph into vein-like structures called lymph vessels and returns it to the bloodstream.
Lymph Vessels and Capillaries
The lymphatic system contains both capillaries and vessels. Lymphatic vessels begin as capillaries. Both of these structures are thin walled, which allows lymph to be transported across the membrane and collected in the vessels. Lymphatic capillaries have greater permeability than blood capillaries and can absorb large molecules such as proteins and lipids. The endothelial cells that make up the wall of a lymphatic capillary lack a basement membrane, loosely attach to each other and slightly overlap. Interstitial fluid enters the lymphatic vessel when the pressure is greater in the interstitial fluid than in lymph and nothing in the interstitial fluid is excluded from entering the lymphatic capillaries. When pressure is greater inside the lymphatic capillary, the endothelial cells prevent lymph from passing back into the interstitial spaces by acting like a one-way swinging door. Lymphatic capillaries are found wherever blood capillaries are located except in the central nervous system and bone marrow.
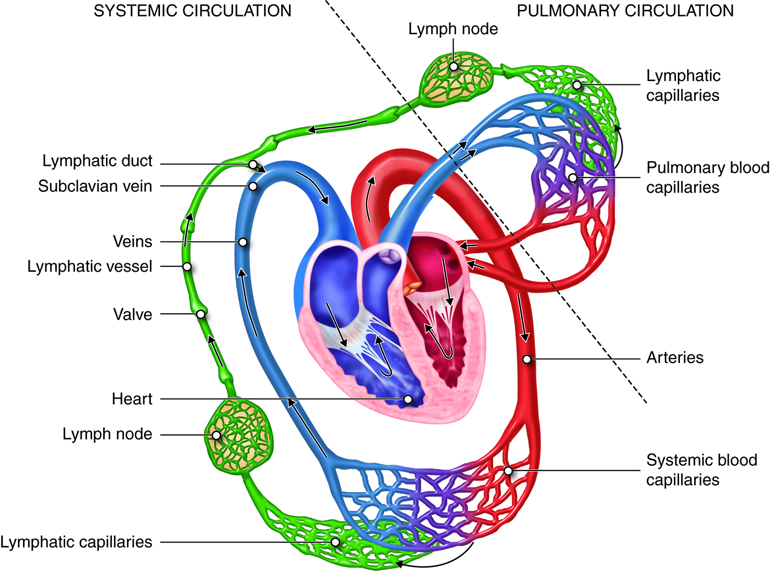
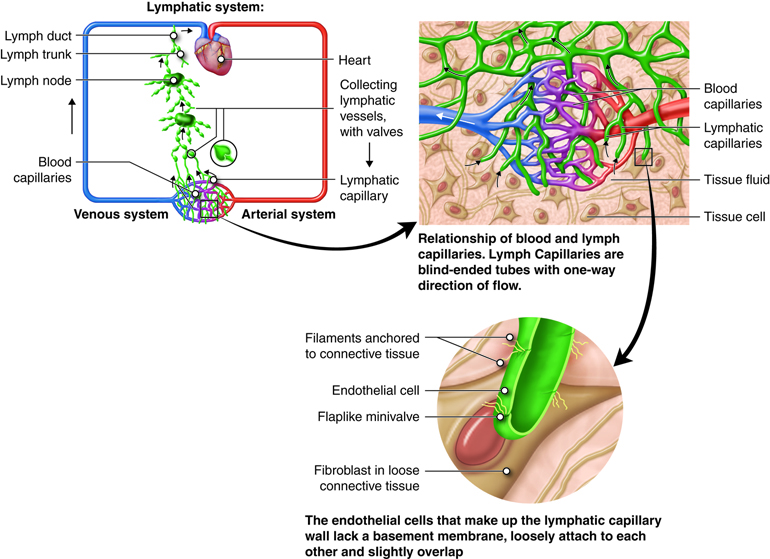
Lymphatic capillaries unite to form larger lymphatic vessels. Structurally, lymphatic vessels are similar to veins because they also have one way valves that function like gates to ensure the lymph only flows in one direction. Like veins, skeletal muscle contraction exerts pressure on the lymph vessels and forces the lymph forward through them. Lymph vessels are like one-way roads, with the lymph being collected at the capillary beds and travels through the body into the thoracic cavity. Lymph is deposited in one of two large ducts in the chest region: the right lymphatic duct and the thoracic duct. The lymph then travels from these ducts into venous circulation via the subclavian and jugular veins.
Unlike the cardiovascular circulation, the lymphatic circulation lacks a pump like the heart. Lymphatic vessels are low pressure vessels similar to veins and the same muscle pump and respiratory pump that promote venous return also facilitate lymph flow. Therefore, even though there is some smooth muscle in lymphatic vessels, movement of the body is important to lymph circulation.
Common Dysfunctions of the Lymphatic Circulation
Anything that would disrupt the flow of lymph could contribute to significant swelling of tissues (edema). Lymphedema is a condition of localized fluid retention and a tissue swelling caused by a compromised lymphatic system. Lymphedema can be primarily caused genetically or secondarily due to injury or obstruction of lymphatic vessels. It is most frequently seen after lymph node dissection, surgery and/or radiation, in which lymphatic system damage is caused during the treatment of cancer, usually breast cancer. Lymphedema may also be associated with parasitic infections in which parasites obstruct lymph vessels. Symptoms may include fatigue, a swollen limb or localized fluid accumulation in other body areas, including the head and neck, discoloration of the skin overlying the swollen tissue and eventually deformity (elephantiasis).
Immunity
Historical Perspective and Overview of Immunity
In relative terms, the study of immunity is a new science that started with Edward Jenner’s discovery in 1796, that individuals exposed to cowpox were often resistant to human smallpox. He also observed that people who had recovered from even a mild case of smallpox were seldom infected a second time. Jenner experimented with placing weakened (attenuated) strains of disease-causing agents into otherwise healthy individuals to provide protection from disease. He called his procedure vaccination. Adding to Jenner’s work, in the 1880s, Robert Koch and Louis Pasteur showed that most infectious diseases were caused by microorganisms. Today it is generally accepted that these disease-causing agents (pathogens) may be microscopic like viruses, bacteria, protozoa and yeast or larger like molds and helminths. Scientists discovered a substance in the serum of vaccinated individuals, which they termed antibodies, that could bind to the pathogen that was used in the vaccination. It was shown that antibodies could be generated against a variety of substances and the term antigen was created to describe these substances. As we will learn shortly, not all antigens stimulate the immune system to produce antibodies so a more general use of the term antigen refers to any substance capable of being recognized during the immune response.

Basically the immune system, as part of the lymphatic system, can be viewed as may subsystems constantly guarding its host against microbial invasion. These systems may be viewed both as an armory (chemical substances), with it tools and weapons, and as an army (cells) capable of using these tools and weapons in defense of the host. Immunity (resistance) has an innate component and an adaptive component. Both of these components depend on the responses of white blood cells (leukocytes).
Innate immunity is the natural resistance with which a person is born and is the result of actions of both external and internal systems. First lines of defense against infection include mechanical and chemical barriers, such as skin and saliva, the effectiveness of which is enhanced by antimicrobial substances. Microbes that succeed in passing the external barriers next encounter the second line of defense, the internal systems. The internal system includes antimicrobial substances and subsets of leukocytes called granulocytes and macrophages. Granulocytes contain an arsenal of cytoplasmic granules that can be released during an immune response. Several of these granulocytes and the macrophages are phagocytic which means they are able to ingest and destroy pathogens. They use pattern-recognition receptors (PRRs) to recognize pathogens. These receptors recognize and bind to molecules found on a wide variety of microbial cells and on damaged or infected host cells. Thus they recognize in a broad and general way the presence of harmful microbes and can quickly attack and usually prevent the spread of the microbes. In addition, the innate immune system includes complement, a set of soluble molecules that can bind to certain molecules common to microbial cells. This binding can lead to the direct destruction of the microbe and can also trigger increased activity of phagocytic cells against the microbe.
A bridge between the innate and the adaptive components is the inflammatory response. Although many soluble factors, blood proteins and cells participate in this response, the main purpose of all of the factors is to enable phagocytic leukocytes and plasma components to leave the blood circulation and enter into damaged and/or infected tissues. The phagocytes in the tissue carry out an array of activities at the inflamed site, the main one being to rid the area of microorganisms and damaged tissue and thus to set the stage for healing. As will be described more completely in a later module, all events between the initial damage and the final restoration of the tissue may be considered parts of the inflammatory response.
Sometimes, however, the innate immune components cannot quickly eliminate the infectious agents especially viral infections. In such instances, cells of the innate system interact with T lymphocytes (T cells) and B lymphocytes (B cells) to initiate adaptive immune responses against the threatening pathogens. The lymphocytes of the adaptive immune response have receptors that are generated by random rearrangement of DNA segments. Such receptors are able to identify and bind a far greater range of substances than can be detected by the PRRS of the innate response. Lymphocytes can detect, with great specificity, threats and proliferate rapidly to act against them in a targeted manner.
The interaction between the innate and adaptive immune responses begins when macrophages and dendritic cells process pathogens and display them in a way that leads to activation of a subset of T lymphocytes (helper T cells). The activated T helper cells can then interact with a variety of other cells, including another subset of T lymphocytes (cytotoxic T cells) and the B lymphocytes. Some cytotoxic T cells become directly involved in attacks against the infection, while the B lymphocytes produce antigen-specific antibodies. The function of antibodies in the immune system is to recognize and neutralize microbes. Once inititated by cells of the innate response, adaptive responses lead to an expansion of the numbers of lymphocytes able to recognize and bind the pathogen in question. In responding to the pathogen, the lymphocytes not only act directly on the substance providing the threat, but may also recruit cells, for example phagocytic cells, and molecules, for example complement, from the innate system and together both the innate and the adaptive immune responses focus their destructive capabilities on removing the threat. Unlike the innate response that operates at a relatively constant level, adaptive immune responses generate memory B and T lymphocytes that produce more vigorous responses upon subsequent encounters with the same microbe.
One essential component of the immune response is that it must be able to distinguish self, which belongs in the body, from nonself (foreign). Agents or molecules classified as nonself may enter the body from the outside or represent an unacceptable change within the body (for example, a virus infected self-cell or a self-cell becoming cancerous). B lymphocyte receptors recognize foreign molecules not associated with self-cells (for example bacterial cells or their toxins). However, T lymphocyte receptors recognize foreign molecules only in association with self-cells (for example a virus-infected cell). Therefore, this recognition involves two considerations: self versus nonself and threat versus nonthreat. Immune cells distinguish self from nonself through cell-surface receptors. All nucleated cells of the body express major histocompatibility complex (MHC) molecules. MHC molecules associated with foreign proteins allow T lymphocytes to recognize self that is threatened and needs to be removed by immune responses.
In summary, because of the wide variety of pathogens located within the body and at its surfaces, host defense requires a wide variety of recognition and defense mechanisms. Innate immunity serves the first line of defense, but is unable to recognize certain pathogens and unable to provide improved defenses that prevents re-infection. Adaptive immunity is based on lymphocytes with receptors that can potentially recognize any foreign antigen. In addition to the adaptive immune response that can eliminate a pathogen, memory lymphocytes are generated that can produce a more rapid and effective response on re-infection.
Common Dysfunctions of the Immune Response
The immune system works remarkably well. Unfortunately, at times it breaks down and fails to function properly. Autoimmune diseases, such as systemic lupus erythematosus (SLE), celiac disease and diabetes mellitus type I, arise from an inappropriate immune response against components normally present in the body. Allergies arise from an exaggerated immune reaction to agents that are not normally harmful and lead to release of chemicals such as histamine. Acquired Immunodeficiency Syndrome (AIDS) is caused by the human immunodeficiency virus (HIV). HIV infects a subset of T cells in the body, thus compromising the immune system. Cancers that affect either T or B cells are collectively called lymphomas. Some are aggressive and fast-growing lymphomas, while others are non-aggressive and slow growing. In a later module we’ll take a closer look at these immune problems of clinical significance.

