Chapter 7: Morphological Variation of the Human
Skeleton
Within all species individuals vary. This variation occurs because of genetics, disease, trauma, and other environmental stimuluses. This variation should be noted when analyzing human remains as it can aid in the identification of those remains. If there is a variant on the skeleton that is rare it can be used to directly id remains or used to narrow down a missing person’s list. The variant present could also have been severe enough as to have caused the death of this individual which aids in reconstructing the manner of death. Finally, skeletal variation should be understood as to not confuse it with alterations that occur after death.1
Skeletal variation falls into four types: Normal Variation, Anomalous Variation, Variation Caused by Pathology, and Musculoskeletal Stress Markers.1
Natural Variation
Normal variation is present in all humans; however, they differ between individuals. Some normal variation is unique enough to identify individuals.1 Normal variation includes:
External Bone Shapes
Most bones overall shape is the same between individuals. However, there are a few bones that show more variation than others. These include the vertebra, hyoid and clavicle.1
Trabecular Bone Patterns
Unlike the external surface of bone, the trabecular bone pattern shows so much variation that it can be used for identification. To view this variation a radiography must be taken.1
Paranasal Sinus Shape
Although, many features of the human skull display extensive variation and thus are useful for individual identification, many investigators have focused on the frontal sinus.5 The frontal sinuses are pneumatic cavities lined with mucosa situated between and internal and external cortical bone of the frontal bone. The frontal sinus is absent in only 4% of the population and presents distinctive variations in shape, area, and symmetry.16 This variation apparently reflects environmental and developmental influences as even identical twins display morphological differences in frontal sinus expression.5 The frontal sinus becomes radiologically evident at age 5–6, and are fully developed at age 10–12.16
Although most early comparative studies of frontal sinus morphology utilized in medicolegal applications featured pattern recognition, metric and more sophisticated statistical treatments have been introduced as well. Scientists have introduced a metric approach that documented the vertical and horizontal dimensions of the sinus expression. They declared a match if the comparative measurements were within 5 mm of each other.5
Cranial Suture Shape
Throughout postnatal craniofacial development, sutures function as sites of bone growth, accommodating expansion of a growing brain. As growth frontiers, cranial sutures are actively responsible for the size and shape of the cranial bones, with overall skull shape being altered by changes to both the level and time period of activity of a given cranial suture. Beyond this crucial role, sutures also function postnatally to provide locomotive shock absorption, allow joint mobility during feeding, and, in later postnatal stages, suture fusion acts to protect the developed brain. All these sutural functions have a clear impact on overall cranial function, development and morphology.7
At the microscopic level, a suture has a dense network of fibers creating a matrix of connective tissue, consisting mainly of collagen, which forms the fibrous sutural joint connection between two approaching bone fronts. The microscopic organization of these fibers has been studied using various methods including confocal laser scanning, histology, and synchrotron X-ray microtomography, all of which identify a unique fiber orientation pattern for each suture. Sutures that remain unfused, such as the sagittal suture, have a random arrangement of fibers. This variable fiber orientation across the sutures appears to be associated with minute growth, specific to the suture, thus producing a unique microscopic morphology at each suture. Moreover, the orientation of these fibers adapts throughout development creating a pattern that is specific to the suture.7
At this gross scale, suture morphology is once again highly variable, with the same suture having a very different morphology. Interestingly, there is a strong association between the microscopic fiber organization and the gross suture morphology. Mechanical constraints and pressures generated during sutural growth are thought to influence the fiber orientation which in turn shapes and modifies the developed gross suture morphology.7
Anomalous Variation
Anomalous variation may not be especially rare but are certainly not present in all humans. These can result from nutritional deficiencies, genetic conditions, or other environmental factors.1 Anomalous Variation Includes:
Accessory Bones
Accessory Bones and Foramen generally result from the failure of bones to fuse or fully fuse together when growth is complete. This is called a non-fusion anomaly.1
Bipartite patella– Division of the patella. The area of division will be porous, centrally roughened, and smooth margins. Seen at a higher frequency among males.15
Acromial Non-Fusion– Lack of fusion of the acromion, presents with rounded margins on the epiphysis and acromion.15
Spondylolysis is a defect of the neural arch of vertebrae, most commonly seen at L5 and L4. The defect is bilateral in approximately 80% of cases and can occur in more than one level. Spondylolysis diminishes the stability of the spinal motion segment and can result in the forward displacement of the upper vertebrae and separation of the anterior aspects of the vertebra from its neural arch. The incidence of spondylolysis has been reported to be 3% to 11.5% in the general population and 23% to 63% in young athletes. Spondylolysis frequently develops between 7 and 10 years of age and is very rare in patients under 5 or over 20 years of age.9
Extra Sutural Bones
Wormian Bones– Small islands of bone within the lambdoid suture.
Asterionic bone– Accessory bone located at the intersections of the lambdoidal and squamosal sutures.15
Bregma bone– Accessory bone located at the intersection of the coronal and sagittal sutures (bregma).15
Inca bone (bipartite, tripartite)- A transverse suture divided the squamous portion of the occipital, creating an accessory bone. The Inca bone is seen at a higher frequency among South American populations. The Inca bone may be singular, bipartite or tripartite. If bipartite an vertical suture will separate the bone into two pieces, if tripartite two vertical sutures will separate the bone into three pieces.15
Extra Sutures
Os japonicum– Occasionally, a suture separates the lower portion of the zygomatic.15
Infraorbital suture– accessory suture located medially, inferior to the lower margin of the orbit on the maxillary bone. May be either complete or partial.15
Metopic suture– Divides the frontal bone, located at midline. Generally, closes by eight years of age. If present, it should be scored as complete or partial.15
Accessory Foramen (Extra Holes)
Infraorbital foramen are additional foramen located medially, inferior to the lower margin of the orbit on the maxillary bone. One is always present.15
Mastoid foramina are single or multiple foramina located within the occipitomastoid suture, or near the suture on either the temporal or occipital. Number and location should always be noted during observation.15
Parietal foramen– Single foramen located on the posterior aspect of the parietal along the sagittal suture. Each parietal may display a foramen, although the foramen may be either absent or within the suture itself. Very large or misshapen parietal foramen are sometimes observed, and should be recorded.15
Supraorbital foramen– Complete foramina located along the superior margins of the orbits (anterior frontal). Number should be observed for each orbit.15
Zygomatico-facial foramen– Single or multiple foramina located on the convex surface of the zygomatics, inferior to the orbital margin. The number and size (large or small) should be noted during observation.15
Septal aperture– Perforation of the olecranon fossa of the humerus, may be large or small. Seen at a slightly higher frequency among females.15
Dental Variation
Carabelli’s cusp – Additional cusp on the mesio-lingual border of the upper molars. Seen at the highest frequency among those of European descent.15
Shovel-shaped incisors – The marginal ridges on the lingual aspect of the incisor are prominent with a deep central depression.15
Supernumerary – Additional teeth, may be seen at multiple locations within the maxillary or mandibular dentition. These teeth may be peg shaped.15 This condition is also called Hyperdontia.1
Other Non-fusion Anomalies
Neural tube defects (NTDs) are anomalies of the central nervous system (CNS) present at birth that manifest with varying subtypes and severity and are among the most common structural birth defects. In more severe NTD subtypes the neural tube fails to close, exposing the brain and cervical–thoracic spine, resulting in intrauterine or neonatal death. In contrast, spina bifida is a neural tube closure defect most often confined to the caudal spine below the level of T10. With advances in surgical repair and management, the majority of spina bifida patients will live into adulthood, but will experience lifelong physical challenges including paralysis, associated hydrocephalus requiring cerebrospinal fluid (CSF) shunting, autonomic dysfunction, orthopedic issues, and more.14
Orofacial clefts (OFC) are the most common congenital anomalies of the craniofacial complex. They can be unilateral, bilateral, complete or incomplete, and may involve the lip only, the palate only (CP) or both. Maxillofacial growth and development can be influenced by the type of cleft and by other factors, such as the degree of congenital tissue defect and the intrinsic growth potential of the craniofacial tissue.8
Variation Caused by Pathology
While there is a wide range of variation within the human skeletal system, bone development can also occur pathologically. Bone pathology can occur when there is excessive bone growth (osteoblastic activity or bone building) or bone is destroyed unnecessarily (osteoclastic activity or bone breakdown). Osteoblastic (bone building) and osteoclastic (bone destruction or breakdown) activities are normal processes of bone development, growth, and maintenance; however, when bone growth or breakdown exceeds what is necessary, the bony change can be classified as pathological, resulting in a bone pathology.2
Over activity of osteoblasts results in a type of lesion called a proliferative lesion which results in the production of too much bone. Increased osteoclast activity results in a type of lesion called lytic or bone loss. Disease can also lead to a complete change the bone’s shape, this is called a deformative lesion.1
Diseases that Cause Proliferative Lesion
Osteosarcoma
Osteosarcoma is a type of neoplastic bone pathology. Characterized by malignant tumors that begin within bone tissues, osteosarcoma is a primary bone cancer (meaning it begins directly in bone tissue, rather than spreading to bone from other body tissues). Malignant tumors associated with osteosarcoma usually occur during growth and development and are observed most often in adolescents and young adults. Tumors are most frequently observed near the ends of long bones.2
Clinically, osteosarcoma is pathologically characterized by lower limb pain, lumps, and anemia. Although the overall survival rate has been significantly ameliorated due to the early diagnosis and timely treatment, osteosarcoma still remains high mortality in children and adolescents.18
Button Osteoma
A Button osteoma is a benign tumor usually found on the parietal or frontal bone. It generally takes the form of a single small lump of bone. In rarer cases multiple button osteomas have been found.4
Diseases that Cause Lytic Lesions
Venereal Syphilis
Venereal syphilis is a disease that is transmitted through sexual contact.4 Chronic syphilis is characterized by development in three clinical stages. The first stage is identified only by a primary lesion or chancre and the second phase features a rash that affects the skin and mucous membranes. In its tertiary stage, the disease can cause serious damage to virtually all parts of the human body; for example, it can lead to hepatic cirrhosis in the liver. The skull is the most common location of tertiary syphilitic lesions. These lesions, which are called caries sicca, are considered by many authors as being pathognomonic for venereal syphilis.3 Caries Sicca can cause erosions of the cranial bone and are associated with the spread of infection to the brain and potentially with the development of neural symptoms.10 The tibia is another bone that can be affected by syphilis. Periosteal bone formation causes the cortical bone to thicken resulting in the Tibia becoming heavier.4 These lesions are rarely seen in modern populations with access to antibiotic treatment.10
Osteomyelitis
Osteomyelitis is an infection that starts in the bone marrow and mostly affects the interior surface of bone. In the vast majority of cases the infectious agent that causes osteomyelitis is a form of streptococcus called Streptococcus aureus. Strep can get into the bone either directly due to an open fracture or during surgery or indirectly from a nearby tissue. This nearby tissue is often the periosteum and if the periosteum is affected the external surface will be affected and the marrow cavity may remain unchanged.4
If osteomyelitis occurs in a postcranial bone a cloaca (hole) may be formed to facilitate the drainage of pus. Part of the bone or the entire bone shaft can become necrotic or die which is caused by lytic lesions in the spongy bone. This can result in small or large sequestration or pieces of dead bone that breaks off the rest of the bone. New bone may also be formed around the shaft by the periosteum called an involucrum. This is used by the body to repair the damage caused by this infection.4
Tuberculosis
Tuberculosis is an infectious disease that is transmitted from one human to another through breathing in the bacteria. This means that the infection will start in the lung and spread to the lymph nodes. If the infected human has a strong immune system, the lungs will heal, and the disease will not spread to other parts of the body. If the immune response is not sufficient this disease can spread to the organs and the bones.4
The vertebra, especially the lumber vertebra, are the most commonly affected area in all age groups. In children the cranial vault is also a commonly affected area. Tuberculosis results in very little new bone formation and instead will primarily destroy the spongy bone which will weaken the bone. In the vertebra this results in a weakening of the vertebral bodies which if weakened enough can result in the collapse of the body and kyphosis. The vertebral arches are generally unaffected.4
Brucellosis
Brucellosis, also known as “Mediterranean fever” or “Malta fever”, is a frequently encountered zoonotic infection in the Middle East. It is usually transmitted to humans from infected animals including cattle, sheep, goats, camels, and pigs via ingestion of food products or by contact with tissue or fluids. It is an important public health concern in many developing countries worldwide. The incidence of brucellosis has been estimated to range from one per 100,000 to 20 per 100,000 in the Middle East and North Africa (MENA) region. This may be an underestimation to actual numbers due to lack of surveillance system among many countries in the region, including Lebanon.13
Brucella infection signs and symptoms are highly variable in the majority of patients including, but not limited to fever, chills, weight loss, headaches, abdominal pain, and depression.13 The bones most commonly affected by this condition are the sacroiliac joint and vertebra. In these bones large lytic lesions are produced.1
Diseases that Cause Deformative Lesions
Rickets
Rickets is a metabolic bone pathology resulting from a Vitamin D deficiency in childhood. Vitamin D is essential to the mineralization of bone tissue and is characterized by a wide variety of cranial and postcranial changes, including the following: asymmetrical deformities of the skull, bowing of the long bones, vertebral compression fractures, and a smaller, thicker pelvis.2
Osteomalacia
Osteomalacia constitutes defective mineralization of existing (old) bone during the remodeling process and therefore always goes along with rickets in growing children (open growth plates) and occurs ubiquitously in bones of adults or adolescents (closed growth plates). Therefore, osteomalacia is not just a disease of adults, but the main reason for long bone bowing deformities and fractures in children with rickets, as poor mineralization reduces bone stiffness. Low calcium intake and/or low vitamin D (from lack of sunshine exposure) are the leading causes of body calcium deprivation worldwide and their combined deficiency accelerates bone demineralization.17
Craniosynostosis
Craniosynostosis or pathological premature closure of sutures postnatally causes profound misshaping of the skull. Numerous mutations have been associated with craniosynostosis. Although it can also be caused by other syndromes, including Apert syndrome, Carpenter syndrome, Crouzon syndrome, Muenke syndrome, and Pfeiffer syndrome. Of these syndromes, Muenke syndrome is the most common and presents with coronal suture synostosis. Aside from the coronal and sagittal sutures, the lambdoid suture is also commonly affected. In each of these examples, craniosynostosis of the suture has a resultant effect on the cranial morphology. Morphological changes in the skull can also impact on the brain. In severe cases, brain expansion becomes limited or distorted from the alterations in cranial morphology leading to cognitive deficits. The reduction in cranial size induces a physiological increase in intracranial pressure, which creates a number of functional impairments, manifesting as visual impairments, deafness, and further cognitive deficits, requiring surgical correction.7
Hydrocephaly
Hydrocephalus was defined as any increase in CSF within the intracranial compartment. Cerebrospinal fluid (CSF) is all fluid within the intracranial compartment except blood. This causes an active distension of the ventricular system of the brain resulting from inadequate passage of CSF from its point of production within the cerebral ventricles to its point of absorption into circulation.6 This causes the skull to become enlarged and serious neurological deficiencies.1
Deformation of the Vertebral Column
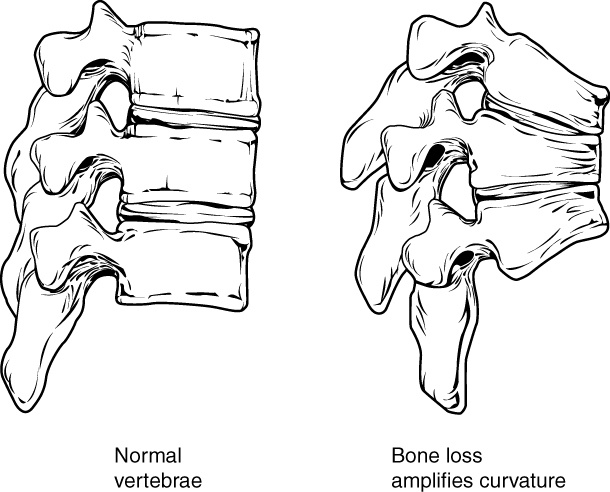
Developmental anomalies, pathological changes, or obesity can enhance the normal vertebral column curves, resulting in the development of abnormal or excessive curvatures. Kyphosis, also referred to as humpback or hunchback, is an excessive posterior curvature of the thoracic region. This can develop when osteoporosis causes weakening and erosion of the anterior portions of the upper thoracic vertebrae, resulting in their gradual collapse. Lordosis, or swayback, is an excessive anterior curvature of the lumbar region and is most commonly associated with obesity or late pregnancy. The accumulation of body weight in the abdominal region results an anterior shift in the line of gravity that carries the weight of the body. This causes in an anterior tilt of the pelvis and a pronounced enhancement of the lumbar curve.11
Scoliosis is an abnormal, lateral curvature, accompanied by twisting of the vertebral column. Compensatory curves may also develop in other areas of the vertebral column to help maintain the head positioned over the feet. Scoliosis is the most common vertebral abnormality among girls. The cause is usually unknown, but it may result from weakness of the back muscles, defects such as differential growth rates in the right and left sides of the vertebral column, or differences in the length of the lower limbs. When present, scoliosis tends to get worse during adolescent growth spurts. Although most individuals do not require treatment, a back brace may be recommended for growing children. In extreme cases, surgery may be required.11
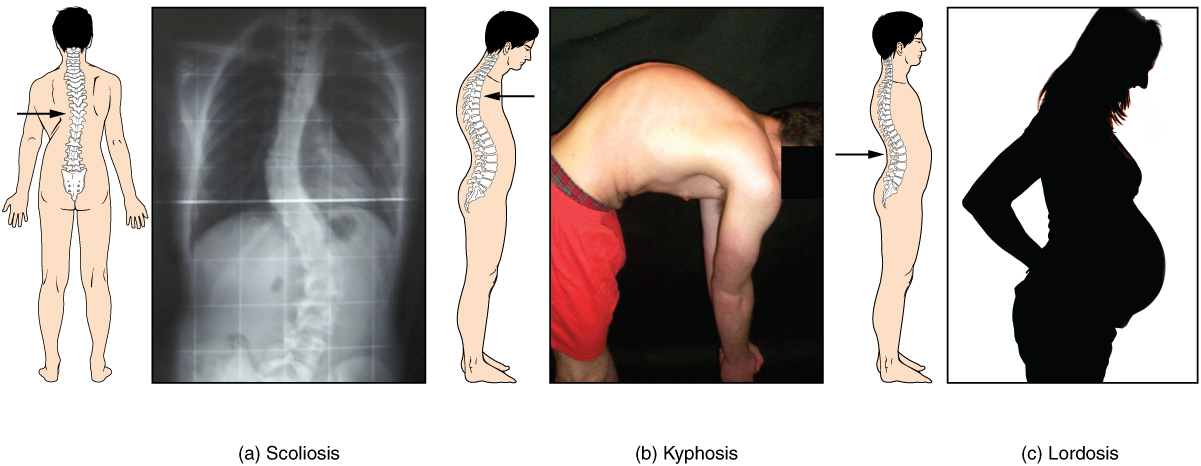
Osteoporosis is an age-related disorder that causes the gradual loss of bone density and strength. When the thoracic vertebrae are affected, there can be a gradual collapse of the vertebrae. This results in kyphosis, an excessive curvature of the thoracic region.11
Deformation Caused by Cultural Practices
Cranial deformation – Two major types of cranial deformation may be observed: artificial and accidental. Artificial deformation is practiced purposely by a number of cultures globally, and can be meant to show social status, ethnic affiliation, or beauty. Pressure may be placed on the frontal, occipital, or circumferentially. Accidental deformation occurs when an infant is strapped to a cradle board for a long period of time, or if an infant is allowed to lay flat on their back. Both accidental forms are known to create flat spots on the back of the cranium.15
Musculoskeletal Stress Markers
Sometimes cultural activities are conducted by individuals at such a frequency that they can cause changes to the bones themselves. The most common of these are alterations to the teeth and to muscle attachment sites on the bones. Alterations to the teeth usually take the form of wear to the cusps, facets, or notches in the teeth. Simply as a byproduct of chewing the cusp are going to wear down over time. However, this occurs faster with some diets than with others. With particularly abrasive diets the wear is going to occur at a faster rate. If a population uses their teeth as tools this can also cause a faster rate of wear, as well as, groves and notches in the teeth.
Hyper-development occurs when a muscle attachment site increases in size as a byproduct of a muscle increasing in size. When muscles are used a particular way routinely, usual during a sport related activity, that muscle will increase in size and because muscles attach and interact with the underlying bone, than the bone will increase in size as will at the attachment point. This can occur symmetrically or asymmetrically depending if both sides of the body are being used equally or if one side is being used more than the other.
References:
1. Angi M. Christensen, Nicholas V. Passalacqua, and Eric J. Bartelink, Forensic Anthropology: Current Methods and Practice, 2nd ed. (London: Academic Press, 2019): 38, 369-399, 477.
2. Ashley Kendell, Alex Perrone, and Colleen Milligan, “Bioarcheology and Forensic Anthropology” In Explorations, ed. Beth Shook, Katie Nelson, Kelsie Aguilera and Lara Braff (Arlington: American Anthropological Association, 2019).
3. Célia Lopes, Mary Lucas Powell, and Ana Luísa Santos, “Syphilis and cirrhosis: a lethal combination in a XIX century individual identified from the Medical Schools Collection at the University of Coimbra (Portugal),” Memórias do Instituto Oswaldo Cruz 105 (2010). https://www.scielo.br/j/mioc/a/VWRpNf45KyJZcqg3NVWvW6B/?lang=en.
4. David J. Ortner, Identification of Pathological Conditions in Human Skeletal Remains, 2nd ed. (San Diego: Academic Press, 2003), 179-183, 199, 227, 229-231, 235, 278, 285-286, 283, 422, 463, 503-504, 506, and 592.
5. Douglas H. Ubelaker, Austin Shamlou, and Amanda Kunkle, “Contributions of Forensic Anthropology to Positive Scientific Identification: A Critical Review,” Forensic Sciences Research 4 (2019): 45–50. https://academic.oup.com/fsr/article/4/1/45/6794580.
6. Harold L Rekate, “The definition and classification of hydrocephalus: a personal recommendation to stimulate debate,” Cerebrospinal Fluid Research 5 (2008). https://link.springer.com/article/10.1186/1743-8454-5-2#rightslink.
7. Heather E. White, Anjali Goswami, and Abigail S. Tucker, “The Intertwined Evolution and Development of Sutures and Cranial Morphology,” Frontiers in Cell and Developmental Biology 9 (2021). https://www.frontiersin.org/articles/10.3389/fcell.2021.653579/full?&utm_source=Email_to_authors_&utm_medium=Email&utm_content=T1_11.5e1_author&utm_campaign=Email_publication&field=&journalName=Frontiers_in_Cell_and_Developmental_Biology&id=653579.
8. Jakob Sajovic, Anina Setnikar Lesjak, Alja Plut, Andreja Eberlinc, Jasmina Primožič, Eva Drevenšek, and Martina Drevenšek, “Maxillary arch dimensions, occlusion assessment and space conditions in patients with cleft palate in the period of deciduous dentition—A retrospective study,” Journal of Stomatology, Oral and Maxillofacial Surgery 124 (2023): 101356. https://www.sciencedirect.com/science/article/pii/S246878552200369X .
9. Jeffrey H. Choi MD, Jonathan K. Ochoa MD, Ariadna Lubinus, Stephen Timon MD, Yu-po Lee MD, and Nitin N. Bhatia MD, “Management of lumbar spondylolysis in the adolescent athlete: a review of over 200 cases,” The Spine Journal 22 (2022): 1628-1633. https://www.sciencedirect.com/science/article/pii/S1529943022001681.
10. Laura Lockau, “A Question of Origins: Skeletal Evidence for the History Venereal Syphilis,” Environment & Society Portal, Arcadia (2017). doi.org/10.5282/rcc/7952. Environment & Society Portal, Arcadia (Summer 2017)
11. Layci Harrison, Anatomical Basis of Injury (Houston: University of Houston, 2019). https://uhlibraries.pressbooks.pub/atpanatomy/front-matter/about-this-book/
12. Muhammad Umair, Farooq Ahmad, Muhammad Bilal, Wasim Ahmad, and Majid Alfadhe, “Clinical Genetics of Polydactyly: An Updated Review,” Frontiers in Genetics 9 (2018). https://www.frontiersin.org/articles/10.3389/fgene.2018.00447/full.
13. Nour Youssef, Yolla Youssef, Dolly Noun, Miguel Abboud, and Ghassan Dbaibo, “Brucellosis causing bone marrow aplasia in an 11-year-old patient with complete recovery after treatment,” IDCases 29 (2022): e01531. https://www.sciencedirect.com/science/article/pii/S2214250922001597.
14. Paul Wolujewicz, Vanessa Aguiar-Pulido, Alice AbdelAleem, Vidya Nair, Gaurav Thareja, Karsten Suhre, Gary M. Shaw, Richard H. Finnell, Olivier Elemento, and M. Elizabeth Ross, “Genome-wide investigation identifies a rare copy-number variant burden associated with human spina bifida,” Genetics in Medicine 23 (2021): 1211-1218. https://www.sciencedirect.com/science/article/pii/S1098360021050322.
15. Roberta Hall, Kenneth Beals, Holm Neumann, Georg Neumann, and Gwyn Madden, Introduction to Human Osteology (Michigan: Grand Valley State University, 2010). https://pressbooks.gvsu.edu/introhumanosteology/.
16. Rhonan Ferreira da Silva, Rodrigo Naves Pinto, Geovane Miranda Ferreira, and Eduardo Daruge Júnior, “Importance of frontal sinus radiographs for human identification,” Brazilian Journal of Otorhinolaryngology 74 (2008): 798. https://www.sciencedirect.com/science/article/pii/S1808869415313963.
17. Suma Uday and Wolfgang Högler, “Nutritional Rickets and Osteomalacia in the Twenty-first Century: Revised Concepts, Public Health, and Prevention Strategies,” Current Osteoporosis Reports 15 (2017): 293–302. https://link.springer.com/article/10.1007/s11914-017-0383-y#rightslink.
18. Xiaofeng Liu, Mingyang Wang, Liwen Zhang, and Lei Huang, “LncRNA ZFAS1 contributes to osteosarcoma progression via miR-520b and miR-520e-mediated inhibition of RHOC signaling,” Clinics 78 (2023): 100143. https://www.sciencedirect.com/science/article/pii/S1807593222033440.
Figure Attributions:
Figure 1 Chapter 7: Axial Skeleton. Authored by: OpenStax College. Provided by: Rice University. Located at: http://cnx.org/contents/14fb4ad7-39a1-4eee-ab6e-3ef2482e3e22@7.1@7.1.. Project: Anatomy & Physiology. License: CC BY: Attribution. (CC BY 4.0).
Figure 2 Chapter 7: Axial Skeleton. Authored by: OpenStax College. Provided by: Rice University. Located at: http://cnx.org/contents/14fb4ad7-39a1-4eee-ab6e-3ef2482e3e22@7.1@7.1.. Project: Anatomy & Physiology. License: CC BY: Attribution. (CC BY 4.0).

