Chapter 14: Analysis of skeletal Trauma
THE ROLE OF THE FORENSIC ANTHROPOLOGIST IN TRAUMA ANALYSIS
Within the medicolegal system, forensic anthropologists are often called upon by the medical examiner, forensic pathologist, or coroner to assist with an interpretation of trauma.3 Trauma interpretation is arguably one of the most valuable services a forensic anthropologist can perform to assist criminal investigative proceedings. This is evidenced by the consistent theme of trauma-focused research in the forensic anthropology literature, spanning several decades.5 The forensic anthropologist’s main focus in any trauma analysis is the underlying skeletal system—as well as, sometimes, cartilage. Analysis and interpretation of soft tissue injuries fall within the purview of the medical examiner or pathologist. It is also important to note that the main role of the forensic anthropologist is to provide information pertaining to skeletal injury to assist the medical examiner/pathologist in their final interpretation of injury. Forensic anthropologists do not hypothesize as to the cause of death of an individual. Instead, a forensic anthropologist’s report should include a description of the injury (e.g., trauma mechanism, number of injuries, location, timing of injury); documentation of the injury, which may be utilized in court testimony (e.g., photographs, radiographs, measurements); and, if applicable, a statement as to the condition of the body and state of decomposition, which may be useful for understanding the depositional context (e.g., how long has the body been exposed to the elements; was it moved or in its original location; are any of the alterations to bone due to environmental or faunal exposure instead of intentional human modification).3
Bone Biomechanics
Although the variables influencing trauma interpretation differ from case to case, and even across elements of the same skeleton, the laws of bone biomechanics that guide these analyses stay constant. The main consideration is that wet or living bone will respond to slow loading force (e.g., blunt force) by first absorbing the force through elastic deformation (temporary alteration that disappears once force is no longer applied), moves to plastic deformation (bone begins to change permanently)when more force is applied, and when the force overloads the bone strength this causes it to fail (e.g., break). 2, 5 Plastic deformation is expressed in the bone as crushing of the cortical layer into the internal cancellous region, as the bone slowly absorbs force without exceeding its yield strength. Per contra, when a bone is exposed to rapid force, such as is seen with gunshot trauma, it will react as a more brittle material and fracture with little to no associated plastic deformation. This brittle reaction is also characteristic of postmortem dry bone breakage. Both plastic deformation and complete bone failure leave distinct signatures on the bone when observed both macro- and microscopically.5
In fracture mechanics, “fracture” refers to the separation of an object or material into two or more pieces, while a “crack” refers to the plane of separation in a structure (so a crack might be a fracture in progress). Fracture is a function of the application of enough stress (load per unit area) to cause a crack to propagate through a structure. If there is a crack in a structure but there is no stress acting on it, it will not fracture; if the stresses are large but the crack is very small, it may not propagate.1 How severe the fracture is determined by how much force is employed or the Magnitude.2 Force is defined as the action of one object on another. Loading regimes is the way forces are applied to an object.1 Bone is less able to absorb forces over a small area than a large area.2
The direction in which force is applied must also be considered as bone is better able to absorb forces in some direction than in others. Directional forces include torsion, shearing, compression, bending, and tension. Torsion occurs when bone is twisted. Shearing occurs when one part of bone is moved in one direction and another part is moved in the opposite direction. Compression occurs when bone dimensions are decreased or squeezed. Bending occurs when the dimensions of one side of the bone are increased and the other side are decreased. Finally, tension occurs when bone dimensions increase or are stretched. Bone is better at resisting compression than it is at resisting tension.2
Fracture can result from a single event that creates and propagates a crack which is caused by dynamic/ high speed forces, or it may result from a series of events involving the introduction of a crack and then subsequent loading(s) that causes it to propagate which is caused by low speed/ static forces. The fracture pattern and fracture surfaces contain clues to the intrinsic and extrinsic factors responsible for fracture morphology.1
Types of Fractures
Fractures fall into two categories: Incomplete and Complete fractures. In incomplete fractures the bone does not break into two separate parts and may involve both cracking and bending. These most often occur in children because their bones are more eleastic. There are several types of incomplete fracture including depressed, buckle, bow, and greenstick fractures. A depressed fracture is found when cranial bones have been caved in usually as a result of blunt force trauma. A buckle fracture occurs when the bone is compressed causing it to fail by expanding outward. Bow fractures occur longitudinally or down the length of the shaft and cause curvature to the bone. Greenstick fractures are partial transverse fractures which cause the bone to bend.2
In complete fractures the bone does break into at least two separate pieces. Complete fractures include comminuted, spiral, epiphyseal, oblique, and transverse fractures. Comminuted fractures occur when the bone is broken in more than two pieces. Spiral fractures occur when the fracture encircles the bone shaft. Epiphyseal fractures are fractures that cross the growth plate in unfused bones. Oblique fractures cross the bone diagonally. Finally, transverse fractures occur straight across the bone at a right angle.2
Types of Trauma
Within the field of anthropology, trauma is defined as an injury to living tissue caused by an extrinsic force or mechanism. Forensic anthropologists can assist a forensic pathologist by providing an interpretation of the course of events that led to skeletal trauma. Within this chapter the different types of trauma will be outlined. As will the timing of the injury (e.g., did trauma occur before, at or around, or after the time of death) will be discussed. Finally, the section will conclude with a discussion of how trauma interpretation is performed in the forensic anthropology laboratory.3
Typically, traumatic injury to bone is classified into one of four categories, defined by the trauma mechanism. A trauma mechanism refers to the force that produced the skeletal modification and can be classified as (1) sharp force, (2) blunt force, (3) projectile, or (4) thermal (burning). Each type of trauma, and the characteristic pattern(s) associated with that particular categorization, will be discussed below.3
Sharp-Force Trauma
Sharp-force trauma is caused by a tool that is edged, pointed, or beveled.3 The most commonly used type of weapon is a single-edged, flat-bladed kitchen, pocket or folding knife. Other weapons, tools, and objects like axes, machetes, screwdrivers, broken bottle necks, and swords can also be found.7 The patterns of injury resulting from sharp-force trauma include linear incisions created by a sharp, straight edge; punctures; and chop marks.3 Sharp weapons will leave sharply defined margins and may be observed as elongated v-shaped marks.8
Method of Tool Mark Examination
When observed under a microscope, an anthropologist can often determine what kind of tool created the bone trauma.3 The identification of a tool is possible when the surface of the tool has microscopic irregularities due to the fabrication process (e.g., grinding features) augmented by subsequent wear. These microscopic burrs, dents, and damages can be considered individual specific for one particular tool. The cutting edge of a blade produces a tool mark consisting of parallel edges and grooves produced by those irregularities. If the cutting mark shows a sufficient amount of detail, it is possible to identify that particular blade is the one that has produced the mark.7 For example, a power saw cut will be discernible from a manual saw cut.3
It is important to note that cut marks occur during excavation and also in the lab during observation. These accidental marks can be differentiated from antemortem/perimortem cut marks on the basis of color. Accidental marks will be lighter in color than the surrounding bone, while the antemortem/perimortem marks will be the same color as the surrounding bone.8
Blunt-Force Trauma
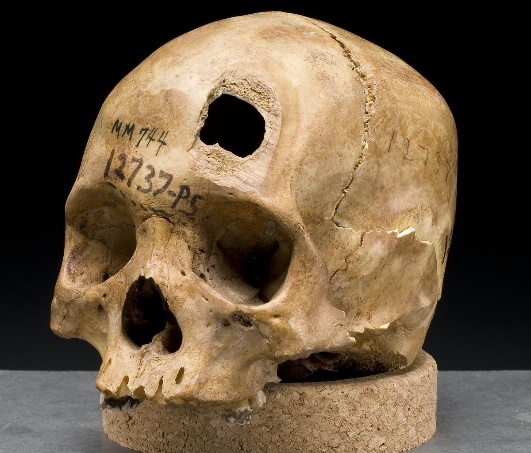
Blunt-force trauma is defined as “a relatively low-velocity impact over a relatively large surface area.” Blunt-force injuries can result from impacts from clubs, sticks, fists, and so forth. Blunt-force impacts typically leave an injury at the point of impact but can also lead to bending and deformation in other regions of the bone. Depressions, fractures, and deformation at and around the site of impact are all characteristics of blunt-force impacts (Figure 14.1). As with sharp-force trauma, an anthropologist attempts to interpret blunt-force injuries, providing information pertaining to the type of tool used, the direction of impact, the sequence of impacts, if more than one, and the amount of force applied.3
Fractures To the Skull
Approximately 30 percent of all injury-related deaths in the United States are caused by head injuries. The majority of head injuries involve falls. They are most common among young children (ages 0–4 years), adolescents (15–19 years), and the elderly (over 65 years). Additional causes vary, but prominent among these are automobile and motorcycle accidents.6
Strong blows to the brain-case portion of the skull can produce fractures. These may result in bleeding inside the skull with subsequent injury to the brain. The most common is a linear skull fracture, in which fracture lines radiate from the point of impact. Other fracture types include a comminuted fracture, in which the bone is broken into several pieces at the point of impact, or a depressed fracture, in which the fractured bone is pushed inward. In a contrecoup (counterblow) fracture, the bone at the point of impact is not broken, but instead a fracture occurs on the opposite side of the skull. Fractures of the occipital bone at the base of the skull can occur in this manner, producing a basilar fracture that can damage the artery that passes through the carotid canal.6
Fractures of Upper Limb Bones
Several types of fractures occur in the postcranial bones including, greenstick, impacted, simple, compound, comminuted, compressed, spiral, Colles’s, and parry.8 Many fractures to the upper limbs result from a hard fall onto an outstretched hand. The resulting transmission of force up the limb may result in a fracture of the humerus, radius, or scaphoid bones. These injuries are especially common in elderly people whose bones are weakened due to osteoporosis.6
Falls onto the hand or elbow, or direct blows to the arm, can result in fractures of the humerus. Following a fall, fractures at the surgical neck, the region at which the expanded proximal end of the humerus joins with the shaft, can result in an impacted fracture, in which the distal portion of the humerus is driven into the proximal portion. Falls or blows to the arm can also produce transverse or spiral fractures of the humeral shaft.6
In children, a fall onto the tip of the elbow frequently results in a distal humerus fracture. In these, the olecranon of the ulna is driven upward, resulting in a fracture across the distal humerus, above both epicondyles (supracondylar fracture), or a fracture between the epicondyles, thus separating one or both of the epicondyles from the body of the humerus (intercondylar fracture).6
Another frequent injury following a fall onto an outstretched hand is a Colles fracture (“col-lees”) of the distal radius. This involves a complete transverse fracture across the distal radius that drives the separated distal fragment of the radius posteriorly and superiorly. This injury results in a characteristic “dinner fork” bend of the forearm just above the wrist due to the posterior displacement of the hand. This is the most frequent forearm fracture and is a common injury in persons over the age of 50, particularly in older women with osteoporosis. It also commonly occurs following a high-speed fall onto the hand during activities such as snowboarding or skating.6
Projectile Trauma
Projectile trauma refers to high-velocity trauma, typically affecting a small surface area. Projectile trauma results from fast-moving objects such as bullets or shrapnel. It is typically characterized by penetrating defects or embedded materials (Figure 14.3). When interpreting injuries resulting from projectile trauma, an anthropologist can often offer information pertaining to the type of weapon used (e.g., rifle vs. handgun), relative size of the bullet (but not the caliber of the bullet), the direction the projectile was traveling, and the sequence of injuries if there are multiple present.3
The sequence of trauma can be determined by examining radiating fractures. As radiating fractures travel away from the bullet hole, they may strike another radiating fracture or suture. If they are intercepted by another radiating fracture, they will stop because the energy will be dispersed in the other radiating fracture (let’s call this radiating fracture RFA and the one mentioned earlier RFB). However, RFA must already be in place for this to occur. Which indicates that RFA occurred first and RFB occurred second in the sequence. Radiating fractures from blunt force trauma can also be used to determine the sequence of blows.2
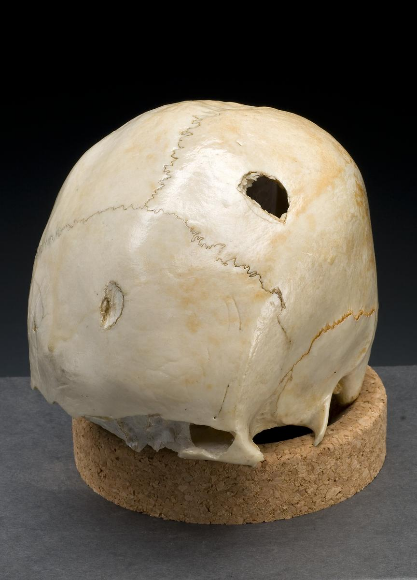
Gun shot wounds have circular holes with distinct edges. The entry wound smaller and has a beveled inner table. The exit wound is larger, has beveling of the outer table, and frequently has small fragments associated.8 A bevel is defined as the angling of fracture propagation produced by an impact creating a defect that is larger on one surface of the structure than the other.1 Fractures will likely be seen radiating away from the wound but will end at the cranial sutures. A solid diagnosis would include a use of a radiograph that should show small fragments of metal embedded in the bone.8

Bullets
When a modern-day firearm is being loaded to fire, the cartridge loaded into the gun is composed of several components. The bullet portion of the cartridge is tightly pressed into a brass tube, called the casing. At the bottom of this brass casing is a round, flat base slightly larger than the casing, and this base prevents the casing from sliding completely into the cartridge chamber of the gun when being loaded. On the bottom of this flat base of the cartridge is the primer. When the trigger is pulled, the primer is the portion of the cartridge that will be struck by the firing pin of the gun. When struck, the primer ignites the gun powder contained inside the brass casing with an explosion that causes the bullet to leave the casing, travel down the gun barrel, and exit the gun.9
Bullets fired from either a handgun or long rifle, other than a shotgun, fire a single projectile each time. This fired projectile is a lead or lead-composite bullet. When fired, this bullet travels down the barrel of the gun and begins to spin because the inside of the gun barrel has been intentionally machined with long gently turning grooves, called rifling. These grooves catch the soft-lead sides of the bullet spinning it like a football, and this spinning makes the bullet travel more straight and true to the target.9 Upon contact with bone, this spin may transmit additional stresses that may influence fracture dimension and morphology.1
Thermal Trauma
Thermal trauma is a bone alteration that results from bone exposure to extreme heat. Thermal trauma can result in cases of house or car fires, intentional disposal of a body in cases of homicidal violence, plane crashes, and so on.3 When dealing with burnt skeletal remains, bone tends to undergo a series of stages, resulting in both macro- and microstructural changes. These changes include dehydration, followed by pyrolysis of the organic component, inversion of the inorganic material, and fusion. The end product is a calcined bone which has lost structural integrity and elasticity, making it vulnerable to fracture and fragmentation, the latter which can also be influenced by recovery and transportation processes. However, it should be noted that the extent of both macro- and microstructural changes may differ due to the location, temperature, and duration of time during which the bone was exposed to heat.10
Thermal trauma is most often characterized by color changes to bone, ranging from yellow to black (charred) or white (calcined). Other bone alterations characteristic of thermal trauma include delamination (flaking or layering due to bone failure), shrinkage, fractures, and heat-specific burn patterning. When interpreting injuries resulting from thermal damage, an anthropologist can differentiate between thermal fractures and fractures that occurred before heat exposure, thereby contributing to the interpretation of burn patterning (e.g., was the individual bound or in a flexed position prior to the fire). ³ When a body is burned the loss of moisture causes the contraction of ligaments and muscles which causes the body to move into a fetal position knowing as the pugilistic posture. This does not occur if the body is bound or in a small space.2
Bodies burned slowly and are often recovered with intact skeletal or fleshed elements remaining. When bodies are exposed to fire for a significant time or at high heat will alter the bone by degrading its organic components, leaving only the mineral structure. The organic components, which are quickly dehydrated and destroyed from thermal modification, are what allow plastic deformation in living bone. Therefore, thermal fractures express features similar to bone impacted by rapid force. Due to the loss of the more pliable, organic components which allow for plasticity in bone, burning bone responds as a brittle material incapable of plastic deformation. 5 Thermally altered bone consistently exhibits a combination longitudinal, longitudinal-transverse, patina, and curved transverse fractures.5 Longitudinal- transverse or step fractures proceed longitudinally down the shaft of the bone and then turns into a transverse fractures which proceeds medially to laterally, or vice versa, across the bone. Curved transverse fractures are transverse fractures that are shaped like half-moon. Patina fractures look like mesh.2
While there are characteristic patterns associated with the four categories of bone trauma, it is also important to note that these bone alterations do not always occur independently of different trauma types. An individual’s skeleton may present with multiple different types of trauma, such as a projectile wound and thermal trauma. Therefore, it is important that the anthropologist recognize the different types of trauma and interpret them appropriately.3
Timing of Injury
Another important component of any anthropological trauma analysis is the determination of the timing of injury (e.g., when did the injury occur). Timing of injury is traditionally split into one of three categories: antemortem (before death), perimortem (at or around the time of death), and postmortem (after death). This classification system differs slightly from the classification system used by the pathologist because it specifically references the qualities of bone tissue and bone response to external forces.3
Antemortem Trauma
Of the three traumatic time-frames (ante-, peri-, and postmortem), the easiest of the traumas to detect are those that occur antemortem. The ease of determining if trauma is antemortem derives from the fact that the fractures, generally, show signs of healing. While healing begins almost immediately after the fracture, evidence of the healing processes can develop as early as one week after the injury. Between weeks one and three, the edges of the fracture will start to become remolded and rounded, and by week six, a bony callus will begin to form. These time frames, however, can only be considered a generality because a variety of factors play into the healing rates, including the overall health and nutritional status of the injured, location of the fracture, and the severity of the injury. While not pertaining to the event that transpired to cause death, antemortem fractures can and do play a major role in forensic anthropology. They can confirm the identity of an unknown decedent by using radiographic comparisons or, if the fracture was serious enough, through the presence of plates and pins, which have recorded serial numbers that are recorded in medical charts and kept by the manufacturer. Antemortem fractures can also be useful in documenting any history of abuse or accidental trauma. While motivations that may have caused a homicide or the direct reasonings behind a death (i.e. a fall) can never truly be determined through skeletal evidence, a history of abuse, in conjunction with other evidence, could be instrumental in determining whether a “suspicious fall” was accidental or homicide.4
Perimortem
Perimortem skeletal trauma is the most important in understanding and reconstructing events because it occurs around the time of the death event. By accurately understanding trauma patterns, a forensic anthropologist will have a better understanding of how the death event took place. It should be noted, however, that this category is more often used by an anthropologist than a forensic pathologist. Depending upon the pathologist, traumas in a medical sense are classified as either antemortem or postmortem by whether they were sustained before or after life functions ceased. The distinction between perimortem and antemortem trauma can really be summed up in a singular word—healing. Perimortem fractures contain biomechanics that are present in antemortem fractures, but because of death, the natural healing process never really takes place. In addition to the absence of the evidence of healing, perimortem fractures can be distinguished from those that occur after decomposition because of the same antemortem biomechanics. Green, or “living,” bone tends to be somewhat elastic, having a little bit of “give” when it bends. This elasticity results in the edges of fractures to appear irregular, as opposed to the rather jagged or angled appearance associated with terminal breaks. In addition, because of the elasticity of bone, “butterfly” or triangular fractures can also be created when the pushing force on a bone causes a radiating fracture, which follows the tension stresses exerted when force is applied on the opposite side of the bone. This appearance, however, while more common in green bone, can be seen in postmortem traumas as well. Besides the elasticity of green bone, or possibly because of it, certain types of trauma, such as gunshot wounds and blunt force traumas, will contain radiating fractures as well. Green bones also have a tendency to splinter and when cut or incised a “curling or uplifting” will also be present.4
Postmortem
Trauma Postmortem trauma is that which occurs after death and is important for determining what transpired to the remains from the time of death to the time of recovery and afterwards. The differentiation of postmortem traumas are critical in the understanding of whether they were caused intentionally by an individual attempting to conceal his or her crime, as would be the case in dismemberment, or occurred naturally because of plant, animal, and soil activity. The differentiation between perimortem and postmortem is particularly important in cases in which remains are found at the scene of a fire. In those cases, understanding fractures that were caused by heat and those that were otherwise inflicted will help to determine if the fire was set as a means of concealing a homicide, or if the fire itself was the cause of death and was otherwise accidental. Postmortem traumas vary from their peri- and antemortem counterparts in that the biomechanics of the bone have completely changed. Whereas antemortem and perimortem traumas occur in green, elastic bones which have a somewhat “wet” aspect to them, bones in the postmortem stage tend to be dry and rather brittle. This process, called plastic deformation, occurs when excessive force is applied to a bone and due to the absence of healing mechanisms, the bone does not remodel and can create a variety of changes, particularly in the fracture patterns of the bones. Where perimortem breaks tend to splinter, postmortem breaks tend to shatter. Postmortem fragments and fractures also tend to be more regular in shape, with straight sharp edges and a lack of evidence of bending. Because of the fact that perimortem fractures exist at deposition, there is also a difference in color between perimortem and postmortem traumas. The existing traumas take on the same color as that of the surrounding bone, while postmortem, a lighter, more natural color will be present. Another source of perimortem/postmortem confusion can arise from gunshot wounds to the skull. The skull, being relatively hollow, can easily be crushed during the postmortem interval, particularly in an anterior-posterior force direction or from a lateral direction. While gunshot trauma might not be confused with actual compression fractures, they can obscure gunshot traumas, making bullet trajectories difficult to discern. The size of force exhorted from a bullet, however, compared to that of compression or crushing forces is much smaller. Gunshot wounds also tend to come with radiating fractures that radiate away from the entry and exit points. By examining for these radiating fractures, the presence of a gunshot wound and the trajectory of the bullet can be ascertained and distinguished from postmortem traumas. In addition, because bullets tend to leave metal fragments, radiographs of the remains might be able to distinguish gunshot wounds if the condition of the bones is such that radiating fractures cannot be distinguished.4
Problems
While in many cases the differentiation between antemortem, perimortem, and postmortem trauma is relatively straightforward, the identification of true perimortem trauma can be problematic. While perimortem trauma is sustained around the time of death, not all of that trauma may be related to the death event itself. In particular, traumas listed as postmortem occur in bone that is denaturalized and dried, but injuries sustained while the bone is still wet but after the death of the individual may be confused with injuries that precipitated the death itself, even if they are unrelated. More importantly, while the bone does eventually dry, the duration of the drying phase is not uniform, but contingent upon many variables including environment, soil content and minerals, water tables, and even the number of bodies found within a grave (in mass graves bodies tend to dry slower than in single graves).4 For example, in cold or freezing temperatures a body can be preserved for extended periods of time increasing the perimortem interval, while in desert climates decomposition is accelerated, thereby significantly decreasing the postmortem interval.3 Likewise there can potentially be confusion with antemortem fractures that occur so close to the death event that evidence of healing has not had time to develop. This potentially could result in the misclassification of a trauma as perimortem that is, in fact, the result of an unrelated antemortem trauma, and would force any understanding of the true perimortem death event to be inaccurate.4 Taphonomic processes can introduce secondary fractures, alter fracture margins, or conceal impact sites which could also cause misclassification. ⁵ The distinction between antemortem, perimortem, and postmortem injuries can be examined on a microscopic level, however depending upon the condition of the remains, such examinations may not be possible. In addition, the procedure might also be time and cost prohibitive.4
Fractography
Fractography refers to the study of fractures and cracks in a material in order to understand the cause of failure. Even as a complex, highly hierarchical composite, bone is a material that obeys the laws of physics and mechanics, including cracking behavior. The fields of fractography and fracture mechanics therefore have much to offer in our understanding of bone’s response to loading and force. Fracture surface analysis can yield information about the mode by which the crack has propagated through the material. Analysis of fracture surfaces of human tibiae subjected to bending revealed ductile failure mechanisms along the side subjected to tension.1
Fracture surfaces may also provide information about why failure occurred at the microstructural level. Examination of fracture surface morphology in human long bones demonstrated that the fracture site contained fewer osteons, less percentage volume of osteons, and osteons with smaller cross-sectional area than bone adjacent to it. Examination of the path of the crack through the microstructures of compact bone has also been demonstrated to reveal information about strain rate (the change in strain (change in dimension relative to initial length) of a material with respect to time). At low loading rates, cracks in compact bone follow a tortuous route along paths of least resistance such as osteonal interfaces; in contrast, at higher strain rates the crack shows no preference for such weak interfaces and propagates through all microscopic components.1
More recently, principles of fractography have been applied specifically to forensic anthropological questions. Several studies have demonstrated the utility of fractography for interpreting aspects of skeletal fractures including crack propagation direction. In an assessment of femora fractured experimentally in 3-point bending, anthropologists and fractographers analyzed the presence and orientation of fracture surface features and found them to be reliable indicators of fracture origin location and propagation direction.1
Fracture Origins From Impacts
The failure modes operative during impact-related fracture are complex and depend upon a variety of intrinsic factors (target and impacting material characteristics including elastic properties, geometry, and density) and extrinsic factors (including projectile velocity, mass, striking-surface area and design). Bone presents a particularly complex material for failure analyses due to its hierarchical structure, in which failure can occur on multiple scales.1
Despite this microstructural complexity, bone typically exhibits brittle, ceramic-type behavior (undergoing little plastic deformation and having low energy absorption before failure) at high strain rates. A fracture origin refers both to the location as well as the flaw or discontinuity from which a fracture began. The term “flaw” does not necessarily refer to something negative – it is recognized that brittle materials (including bone) are imperfect and contain irregularities and inhomogeneities that can represent the site where a fracture initiates. Fracture origins are often created by sudden impacts (for example, with blunt objects, the ground, a bullet, or a blade). These impacts cause dynamic crack initiation and propagation. In skeletal trauma analyses, fracture origins are typically of interest in understanding the location where a bone was impacted (i.e., from where the force originated).1
Much work has therefore focused on the relationship between fracture patterns and impact location, such as whether fracture origins are at the impact site or elsewhere. The relationship is somewhat complex, however, and the location of the fracture origin will depend on where the tensile stresses are greatest. Fracture origin is related to a number of factors in addition to impact location including loading regime, surface area of loading, elastic properties of the two impacting materials (e.g., the bone and the projectile), stress concentrators, and structure geometry.1
Stress concentrators (a feature within a structure that results in greater stresses in its vicinity than are present in areas more remote from it) are important considerations because they may function as a crack origin in an area not otherwise expected based on overall material properties or geometry. Stress concentrators generally include voids/cavities, inclusions, compositional irregularities, and microdamage. If stress concentrators are located in the stress field created by an impactor, the crack will originate at that location. For example, a nutrient foramen opening in tubular bone creates a surface flaw that can act as a stress concentrator. Aging and disease can also significantly affect the mechanical properties of bone and increase strength limiting features including increased porosity and the accumulation of microdamage, both of which can increase the potential for failure.
Cracks do not necessarily originate at the impact site and can initiate adjacent or even remote to the impact site. Bending force can create tensile stresses on the opposite side and trigger crack growth at that location. For example, a blunt impact to the cranium will create tension on the endocranial surface, and cracks will originate endocranially. In tubular bones, it is well understood that impacts can impose bending stresses (such as the bumper of a car impacting a tibia), creating tension on the side of the bone opposite the impact, which is where the crack will originate. Identification of the fracture origin is often a relevant and informative part of the investigation into material failure. Fracture origins typically have smoother surfaces, becoming more featured with increasing crack speed and instability.1
At higher velocities, radial cracks (cracks extending outward from a point of impact, sometimes also called radiating fractures) may be generated from the impact site originating from within the zone of the contact and propagating outward. These tend to be easy to identify and interpret, as the cracks fan out away from the impact site such that the radiating crack pattern leads back to converge in the middle. If the structure is continually loaded, the segments created by the radial fractures can bend inward, causing them to break in bending, leading to circumferential cracks (arc-shaped cracks surrounding an impact site as a result of bending of a structural segment). These roughly circular, semi-circular, or arc-shaped fractures are often offset by the radial fractures confirming that the radial fractures preceded the secondary circumferential fractures.1
In lower velocity impacts, the maximum tension is on the impacted side of the material and the circumferential fracture therefore initiates ectocranially, propagating toward the endocranial surface. With highvelocity perforating impacts to crania (because the cranium is an enclosed structure), the segments produced by radial fractures may be pushed outward due to the temporary cavity created by energy transfer from the projectile, resulting in circumferential fractures that initiate on the endocranial surface. Note that the term concentric has traditionally been used interchangeably with circumferential by anthropologists and others to refer to this fracture pattern. Technically, concentric refers to multiple generations of arc-shaped fractures sharing a common center (rather than a single arc). Concentric fractures are less common but occasionally seen in high-velocity projectile impacts to bone.1
The fields of fractography and fracture mechanics can significantly inform our understanding of bone’s response to loading and force. This is becoming more widely embraced by forensic anthropologists, and the application of the science of fractography to the study and analysis of skeletal fractures in forensic contexts represents part of the shift from a typological to a mechanics- centered approach. As a relatively new method in forensic anthropology, fractography is not yet widely known or understood, and is not commonly taught as part of forensic anthropological educational or training programs. Fractography is also heavily based in engineering principles, and it is recognized that most forensic anthropologists do not possess engineering backgrounds. Importantly, failure and fracture patterns are strongly influenced by structure geometry, and within the human skeleton there is significant variation in bone shape and configuration. Therefore, the response of each bone or bone type to certain loading conditions will vary. Additional research on different loading and impacting regimes may clarify the creation and appearance of fracture patterns on various bone types.1
References:
1. Angi M. Christensen, John M. Rickman, and Hugh E. Berryman, “Forensic fractography of bone: fracture origins from impacts, and an improved understanding of the failure mechanism involved in beveling,” Forensic Anthropology 4 (2021): 57-69. https://dspace.lib.cranfield.ac.uk/bitstream/handle/1826/17151/Forensic_fractography_of_bone-2021.pdf?sequence=1&isAllowed=y
2. Angi M. Christensen, Nicholas V. Passalacqua, and Eric J. Bartelink, Forensic Anthropology: Current Methods and Practice, 2nd ed. (London: Academic Press, 2019): 38, 407-434.
3. Ashley Kendell, Alex Perrone, and Colleen Milligan, “Bioarcheology and Forensic Anthropology” In Explorations, ed. Beth Shook, Katie Nelson, Kelsie Aguilera and Lara Braff (Arlington: American Anthropological Association, 2019).
4. Ashley Smith, “Distinguishing Between Antemortem, Perimortem, and Postmortem Bone Trauma: A Short Primer,” Academia Letters (2021). https://doi.org/10.20935/AL1570.
5. Kamryn Keys and Ann H. Ross, “Identifying Blunt Force Traumatic Injury on Thermally Altered Remains: A Pilot Study Using Sus scrofa,” Biology 11 (2022). https://www.mdpi.com/2079-7737/11/1/87.
6. Layci Harrison, Anatomical Basis of Injury (Houston: University of Houston, 2019). https://uhlibraries.pressbooks.pub/atpanatomy/front-matter/about-this-book/.
7. Matthias Weber, Sibylle Banaschak and Markus Alexander Rothschild, “Sharp force trauma with two katana swords: identifying the murder weapon by comparing tool marks on the skull bone,” International Journal of Legal Medicine volume 135 (2021): 313–322. https://link.springer.com/article/10.1007/s00414-020-02372-3.
8. Roberta Hall, Kenneth Beals, Holm Neumann, Georg Neumann, and Gwyn Madden, Introduction to Human Osteology (Michigan: Grand Valley State University, 2010). https://pressbooks.gvsu.edu/introhumanosteology/.
9. Rod Gehl and Darryl Plecas, Introduction to Criminal Investigation: Processes, Practices and Thinking (New Westminster, BC: Justice Institute of British Columbia, 2017). Download this book for free at https://pressbooks.bccampus.ca/criminalinvestigation/ as follows: digital format: on every electronic page print format: on at least one page near the front of the book.
10. Vijarn Vachirawongsakorn, Nicholas Márquez-Grant and Jonathan Painter, “Survival of sharp force trauma in burnt bones: effects of environmental factors,” International Journal of Legal Medicine (2022). https://link.springer.com/article/10.1007/s00414-022-02916-9#article-info.
Figure Attributes:
Figure 14.1 Skull sword trauma by the National Institutes of Health, Health & Human Services [19th Century Collection, National Museum of Health and Medicine, Armed Forces Institute of Pathology, Washington, D.C. From exhibition “Visible Proofs: Forensic Views of the Body” U.S. National Library of Medicine] is in the public domain.
Figure 14.2 Skull hammer trauma by the National Institutes of Health, Health & Human Services [19th Century Collection, National Museum of Health and Medicine, Armed Forces Institute of Pathology, Washington, D.C. From exhibition “Visible Proofs: Forensic Views of the Body” U.S. National Library of Medicine] is in the public domain.
Figure 14.3 Trauma: Gunshot Wounds by Smithsonian [exhibit: Written in Bone, How Bone Biographies Get Written] has no known copyright restrictions.

