12.4 Muscle Contraction

Arm Wrestling
It’s obvious that a sport like arm wrestling (Figure 12.4.1) depends on muscle contractions. Arm wrestlers must contract muscles in their hands and arms, and keep them contracted in order to resist the opposing force exerted by their opponent. The wrestler whose muscles can contract with greater force wins the match.
What Is a Muscle Contraction?
A muscle contraction is an increase in the tension or a decrease in the length of a muscle. Muscle tension is the force exerted by the muscle on a bone or other object. A muscle contraction is isometric if muscle tension changes, but muscle length remains the same. An example of isometric muscle contraction is holding a book in the same position. A muscle contraction is isotonic if muscle length changes, but muscle tension remains the same. An example of isotonic muscle contraction is raising a book by bending the arm at the elbow. The termination of a muscle contraction of either type occurs when the muscle relaxes and returns to its non-contracted tension or length.
To use our arm wrestling example, if both arm wrestlers have equal strength and they are pulling with all their might, but there is no movement, that is isometric muscle contraction. However, as soon as one arm wrestler starts to win and is able to start pulling the opponents arm down, that is isotonic muscle contraction.
How a Skeletal Muscle Contraction Begins
Excluding reflexes, all skeletal muscle contractions occur as a result of conscious effort originating in the brain. The brain sends electrochemical signals through the somatic nervous system to motor neurons that innervate muscle fibres (to review how the brain and neurons function, see the chapter Nervous System). A single motor neuron with multiple axon terminals is able to innervate multiple muscle fibres, thereby causing all of them to contract at the same time. The connection between a motor neuron axon terminal and a muscle fibre occurs at a site called a neuromuscular junction. This is a chemical synapse where a motor neuron transmits a signal to a muscle fibre to initiate a muscle contraction. The process by which a signal is transmitted at a neuromuscular junction is illustrated in Figure 12.4.2 below.
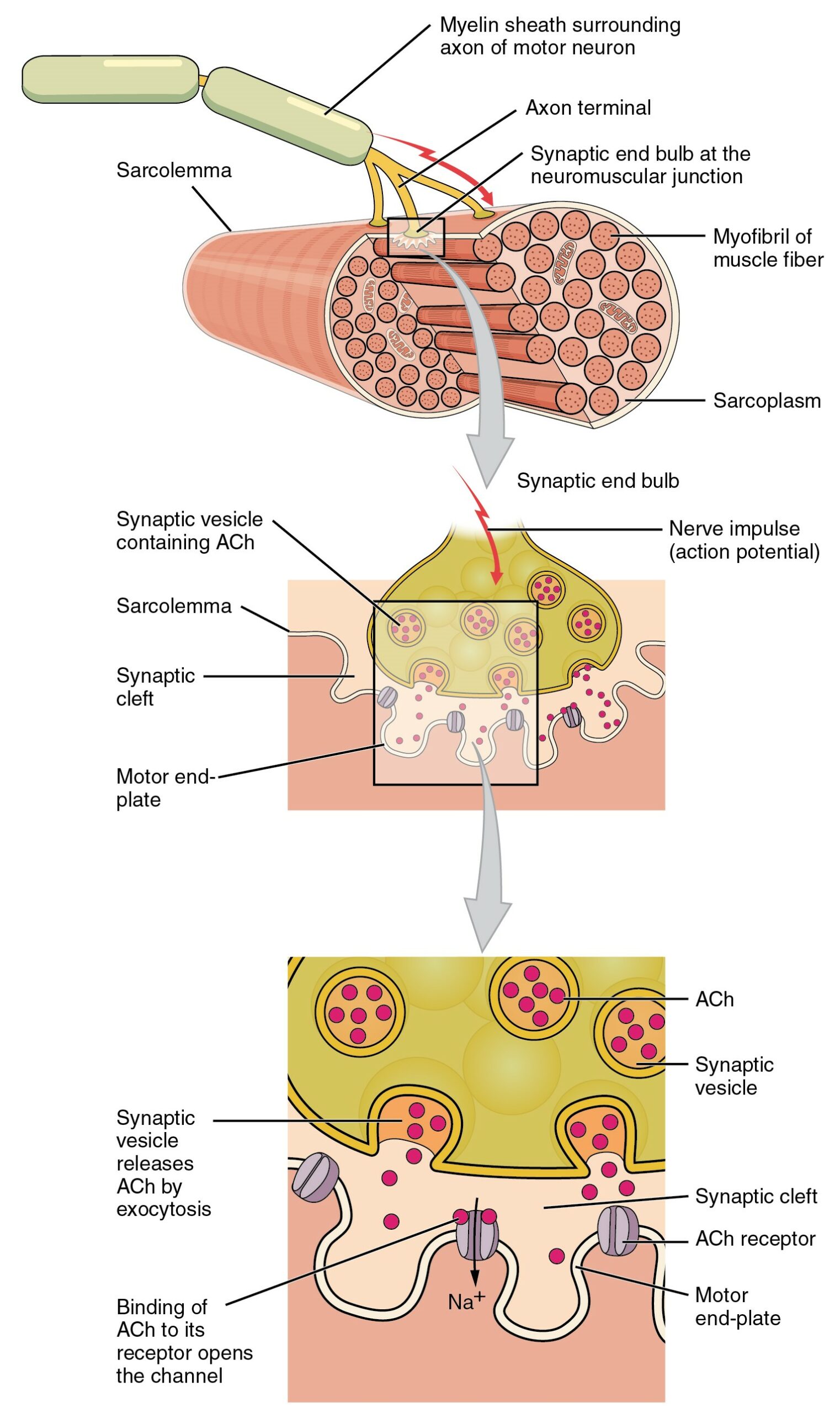
The sequence of events begins when an action potential is initiated in the cell body of a motor neuron, and the action potential is propagated along the neuron’s axon to the neuromuscular junction. Once the action potential reaches the end of the axon terminal, it causes the release of the neurotransmitter acetylcholine (ACh) from synaptic vesicles in the axon terminal. The ACh molecules diffuse across the synaptic cleft and bind to receptors on the muscle fibre, thereby initiating a muscle contraction.
Sliding Filament Theory of Muscle Contraction
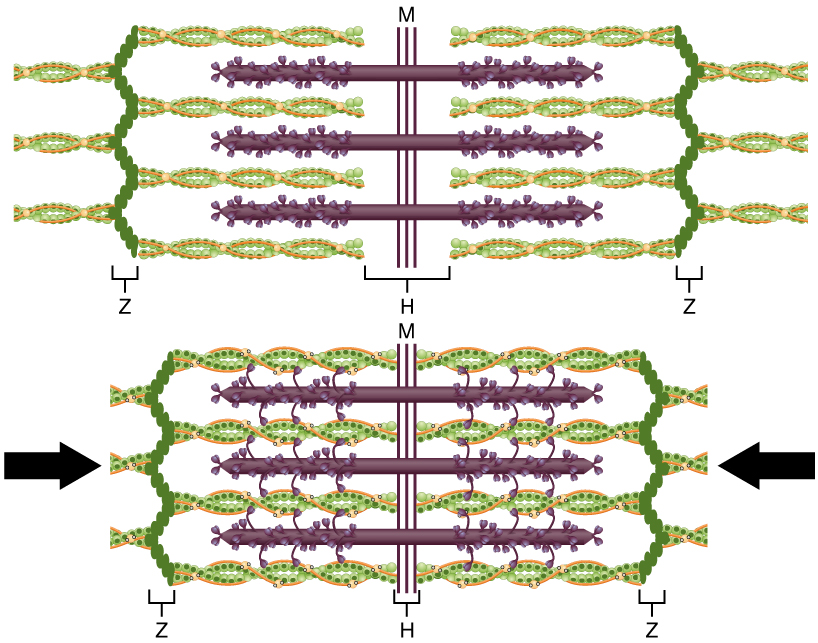
Once the muscle fibre is stimulated by the motor neuron, actin and myosin protein filaments within the skeletal muscle fibre slide past each other to produce a contraction. The sliding filament theory is the most widely accepted explanation for how this occurs. According to this theory, muscle contraction is a cycle of molecular events in which thick myosin filaments repeatedly attach to and pull on thin actin filaments, so the filaments slide over one another, as illustrated in Figure 12.4.3. The actin filaments are attached to Z discs, each of which marks the end of a sarcomere. The sliding of the filaments pulls the Z discs of a sarcomere closer together, thus shortening the sarcomere. As this occurs, the muscle contracts.
Crossbridge Cycling
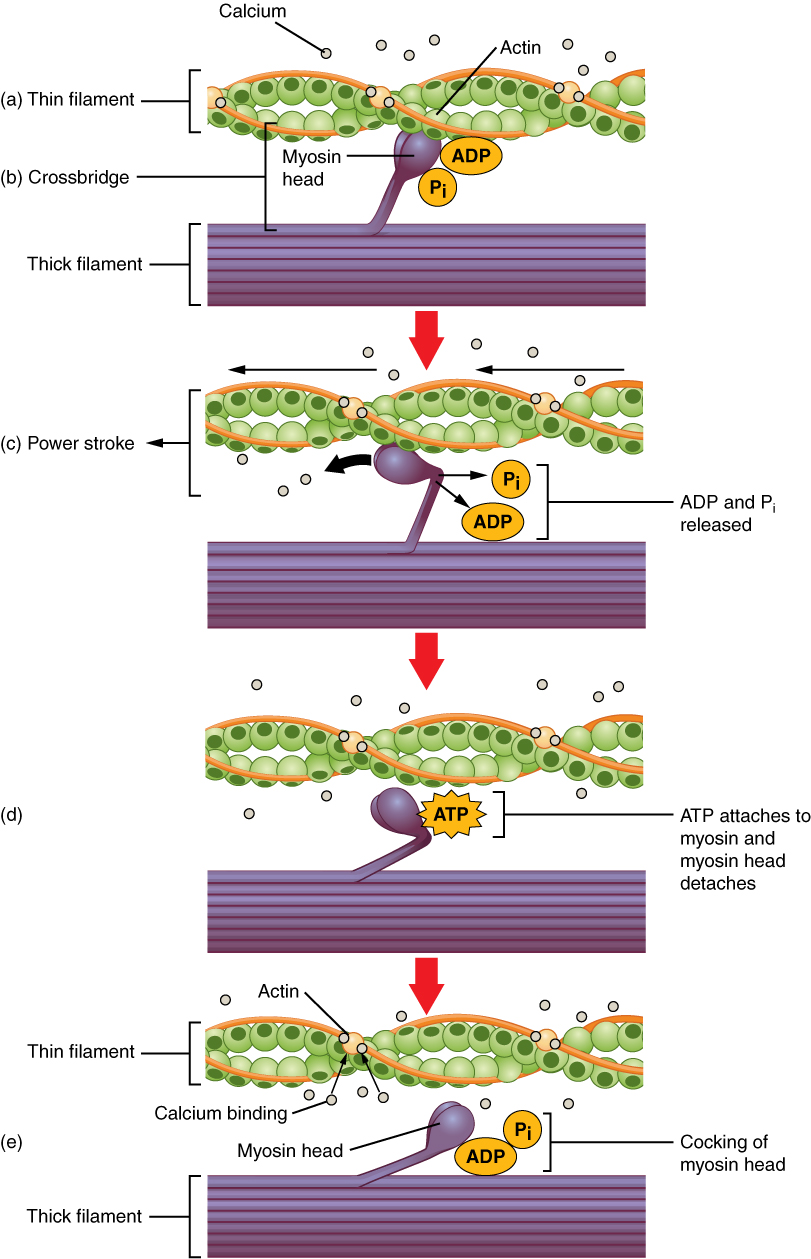
Crossbridge cycling is a sequence of molecular events that underlies the sliding filament theory. There are many projections from the thick myosin filaments, each of which consists of two myosin heads (you can see the projections and heads in Figures 12.4.3 and 12.4.4). Each myosin head has binding sites for ATP (or the products of ATP hydrolysis: ADP and Pi) and for actin. The thin actin filaments also have binding sites for the myosin heads. A crossbridge forms when a myosin head binds with an actin filament.
The process of crossbridge cycling is shown in the video “Muscle Contraction 3D” by 3DBiology (below), and in Figure 12.4.4. A crossbridge cycle begins when the myosin head binds to an actin filament. ADP and Pi are also bound to the myosin head at this stage. Next, a power stroke moves the actin filament inward toward the center of sarcomere, thereby shortening the sarcomere. At the end of the power stroke, ADP and Pi are released from the myosin head, leaving the myosin head attached just to the thin filament until another ATP binds to the myosin head. When ATP binds to the myosin head, it causes the myosin head to detach from the actin. ATP is once again split into ADP and Pi and the energy released is used to move the myosin head into a “cocked” position. Once in this position, the myosin head can bind to the actin filament again, and another crossbridge cycle begins.
Muscle Contraction 3D, 3DBiology, 2017.
Energy for Muscle Contraction
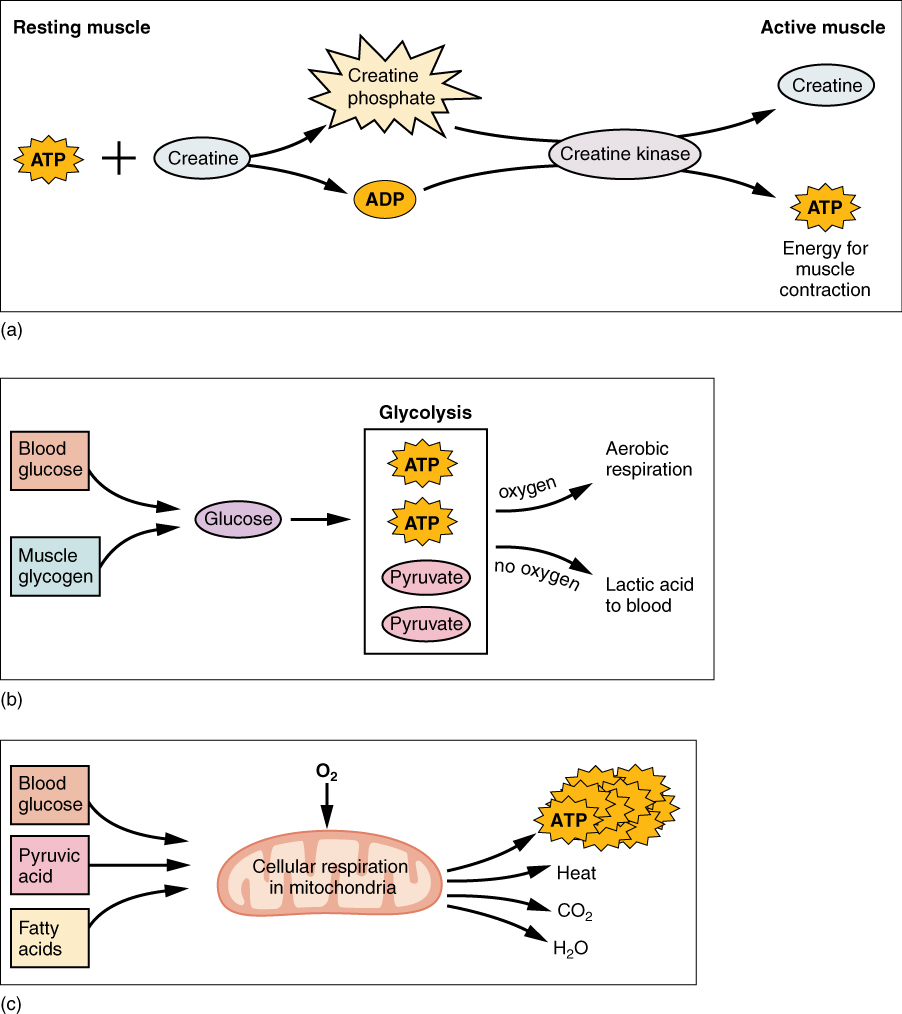
According to the sliding filament theory, ATP is needed to provide the energy for a muscle contraction. Where does this ATP come from? Actually, there are multiple potential sources, as illustrated in Figure 12.4.5 below.
- As you can see from the first diagram, some ATP is already available in a resting muscle. As a muscle contraction starts, this ATP is used up in just a few seconds. More ATP is generated from creatine phosphate, but this ATP is used up rapidly as well. It’s gone in another 15 seconds or so.
- Glucose from the blood and glycogen stored in muscle can then be used to make more ATP. Glycogen breaks down to form glucose, and each glucose molecule produces two molecules of ATP and two molecules of pyruvate. Pyruvate (as pyruvic acid) can be used in aerobic respiration if oxygen is available. Alternatively, pyruvate can be used in anaerobic respiration, if oxygen is not available. The latter produces lactic acid, which may contribute to muscle fatigue. Anaerobic respiration typically occurs only during strenuous exercise when so much ATP is needed that sufficient oxygen cannot be delivered to the muscle to keep up.
- Resting or moderately active muscles can get most of the ATP they need for contractions by aerobic respiration. This process takes place in the mitochondria of muscle cells. In the process, glucose and oxygen react to produce carbon dioxide, water, and many molecules of ATP.
Feature: Human Biology in the News
Basic research on muscle contraction, especially if it is interesting and hopeful, is often in the news, because muscle contractions are involved in so many different body processes and disorders, including heart failure and stroke.
- Heart failure is a chronic condition in which cardiac muscle cells cannot contract forcefully enough to keep body cells adequately supplied with oxygen. According to a 2016 report by the Heart and Stroke Foundation of Canada, 600,000 Canadians are living with heart failure and each year, 50,000 new cases are diagnosed. Heart failure costs the Canadian medical system more than $2.8 billion annually. In 2016, researchers at the University of Texas Southwestern Medical Center identified a potential new target for the development of drugs to increase the strength of cardiac muscle contractions in patients with heart failure. The UT researchers found a previously unidentified protein involved in muscle contraction. The protein, which is very small, turns off the “brake” on the heart so it pumps blood more vigorously. At the molecular level, the protein affects the calcium-ion pump that controls muscle contraction. The scientists also found the same protein in slow-twitch skeletal muscle fibres. Interestingly, the protein is encoded by a stretch of mRNA that had been dismissed by scientists as non-coding RNA, commonly referred to as “junk” RNA. According to one of the researchers, “We dipped into the RNA ‘junk’ pile and came up with a hidden treasure.” This result is likely to lead to searches for additional treasures that might be hiding in the RNA junk pile.
- A stroke occurs when a blood clot lodges in an artery in the brain and cuts off blood flow to part of the brain. Approximately 6% of deaths in Canada are due to stroke and while men and women experiences strokes almost equally, women are more likely to die from a stroke. Damage from the clot associated with strokes would be reduced if the smooth muscles lining brain arteries relaxed following a stroke, because the arteries would dilate and allow greater blood flow to the brain. In a recent study undertaken at the Yale University School of Medicine, researchers determined that the muscles lining blood vessels in the brain actually contract after a stroke. This constricts the vessels, reduces blood flow to the brain, and appears to contribute to permanent brain damage. The hopeful takeaway of this finding is that it suggests a new target for stroke therapy.
12.4 Summary
- A muscle contraction is an increase in the tension or a decrease in the length of a muscle. A muscle contraction is isometric if muscle tension changes, but muscle length remains the same. It is isotonic if muscle length changes, but muscle tension remains the same.
- A skeletal muscle contraction begins with electrochemical stimulation of a muscle fibre by a motor neuron. This occurs at a chemical synapse called a neuromuscular junction. The neurotransmitter acetylcholine diffuses across the synaptic cleft and binds to receptors on the muscle fibre. This initiates a muscle contraction.
- Once stimulated, the protein filaments within the skeletal muscle fibre slide past each other to produce a contraction. The sliding filament theory is the most widely accepted explanation for how this occurs. According to this theory, thick myosin filaments repeatedly attach to and pull on thin actin filaments, thus shortening sarcomeres.
- Crossbridge cycling is a cycle of molecular events that underlies the sliding filament theory. Using energy in ATP, myosin heads repeatedly bind with and pull on actin filaments. This moves the actin filaments toward the center of a sarcomere, shortening the sarcomere and causing a muscle contraction.
- The ATP needed for a muscle contraction comes first from ATP already available in the cell, and more is generated from creatine phosphate. These sources are quickly used up. Glucose and glycogen can be broken down to form ATP and pyruvate. Pyruvate can then be used to produce ATP in aerobic respiration if oxygen is available, or it can be used in anaerobic respiration if oxygen is not available.
12.4 Review Questions
- What is a skeletal muscle contraction?
-
- Explain sliding filament theory and describe crossbridge cycling.
- If the acetylcholine receptors on muscle fibres were blocked by a drug, what do you think this would do to muscle contraction? Explain your answer.
- Explain how crossbridge cycling and sliding filament theory are related to each other.
- When does anaerobic respiration typically occur in human muscle cells?
- If there were no ATP available in a muscle, how would this affect crossbridge cycling? What would this do to muscle contraction?
12.4 Explore More
The Mechanism of Muscle Contraction: Sarcomeres, Action Potential, and the Neuromuscular Junction, Professor Dave Explains, 2019.
Aerobic vs Anaerobic Difference, Dorian Wilson, 2017.
Attributions
Figure 12.4.1
Armwrestling_Championships by Jnadler1 on Wikimedia Commons is used under a CC BY-SA 3.0 (https://creativecommons.org/licenses/by-sa/3.0) license.
Figure 12.4.2
Motor_End_Plate_and_Innervation by OpenStax on Wikimedia Commons is used under a CC BY 4.0 (https://creativecommons.org/licenses/by 4.0) license.
Figure 12.4.3
Sliding_Filament_Model_of_Muscle_Contraction by OpenStax on Wikimedia Commons is used under a CC BY 4.0 (https://creativecommons.org/licenses/by 4.0) license.
Figure 12.4.4
Skeletal_Muscle_Contraction by OpenStax on Wikimedia Commons is used under a CC BY 4.0 (https://creativecommons.org/licenses/by 4.0) license.
Figure 12.4.5
Muscle_Metabolism by OpenStax on Wikimedia Commons is used under a CC BY 4.0 (https://creativecommons.org/licenses/by 4.0) license.
References
3DBiology. (2017). Muscle contraction 3D. YouTube. https://www.youtube.com/watch?v=GrHsiHazpsw
Betts, J. G., Young, K.A., Wise, J.A., Johnson, E., Poe, B., Kruse, D.H., Korol, O., Johnson, J.E., Womble, M., DeSaix, P. (2016, May 27). Figure 10.6 Motor end-plate and innervation [digital image]. In Anatomy and Physiology (Section 10.2). OpenStax. https://openstax.org/books/anatomy-and-physiology/pages/10-2-skeletal-muscle
Betts, J. G., Young, K.A., Wise, J.A., Johnson, E., Poe, B., Kruse, D.H., Korol, O., Johnson, J.E., Womble, M., DeSaix, P. (2016, May 27). Figure 10.10 The sliding filament model of muscle contraction [digital image]. In Anatomy and Physiology (Section 10.3). OpenStax. https://openstax.org/books/anatomy-and-physiology/pages/10-3-muscle-fiber-contraction-and-relaxation
Betts, J. G., Young, K.A., Wise, J.A., Johnson, E., Poe, B., Kruse, D.H., Korol, O., Johnson, J.E., Womble, M., DeSaix, P. (2016, May 27). Figure 10.11 Skeletal muscle contraction [digital image]. In Anatomy and Physiology (Section 10.3). OpenStax. https://openstax.org/books/anatomy-and-physiology/pages/10-3-muscle-fiber-contraction-and-relaxation
Betts, J. G., Young, K.A., Wise, J.A., Johnson, E., Poe, B., Kruse, D.H., Korol, O., Johnson, J.E., Womble, M., DeSaix, P. (2016, May 27). Figure 10.12 Muscle metabolism [digital image]. In Anatomy and Physiology (Section 10.3). OpenStax. https://openstax.org/books/anatomy-and-physiology/pages/10-3-muscle-fiber-contraction-and-relaxation
Dorian Wilson. (2017, March 8). Aerobic vs anaerobic difference. YouTube. https://www.youtube.com/watch?v=8Y_FdjI2v4I&feature=youtu.be
Heart and Stroke Foundation. (2016). 2016 Report on the health of Canadians: The burden of heart failure. https://www.heartandstroke.ca/-/media/pdf-files/canada/2017-heart-month/heartandstroke-reportonhealth-2016.ashx?la=en
Hill, R. A., Tong, L., Yuan, P., Murikinati, S., Gupta, S., & Grutzendler, J. (2015). Regional blood flow in the normal and ischemic brain is controlled by arteriolar smooth muscle cell contractility and not by capillary pericytes. Neuron, 87(1), 95–110. https://doi.org/10.1016/j.neuron.2015.06.001
UTSouthwestern Newsroom. (2016, January 14). Researchers find a small protein that plays a big role in heart muscle contraction [online article]. https://www.utsouthwestern.edu/newsroom/articles/year-2016/dworf-protein-olson.html
What we do. (n.d.). Heart and Stroke Foundation of Canada. https://www.heartandstroke.ca/what-we-do
Created by CK-12 Foundation/Adapted by Christine Miller

http://humanbiology.pressbooks.tru.ca/wp-content/uploads/sites/6/2019/06/human-heartbeat-daniel_simon.mp3
Lub, Dub
Lub dub, lub dub, lub dub... That’s how the sound of a beating heart is typically described. Those are also the only two sounds that should be audible when listening to a normal, healthy heart through a stethoscope, as in Figure 14.3.1. If a doctor hears something different from the normal lub dub sounds, it’s a sign of a possible heart abnormality. What causes the heart to produce the characteristic lub dub sounds? Read on to find out.
Introduction to the Heart
The heart is a muscular organ behind the sternum (breastbone), slightly to the left of the center of the chest. A normal adult heart is about the size of a fist. The function of the heart is to pump blood through blood vessels of the cardiovascular system. The continuous flow of blood through the system is necessary to provide all the cells of the body with oxygen and nutrients, and to remove their metabolic wastes.
Structure of the Heart
The heart has a thick muscular wall that consists of several layers of tissue. Internally, the heart is divided into four chambers through which blood flows. Because of heart valves, blood flows in just one direction through the chambers.
Heart Wall
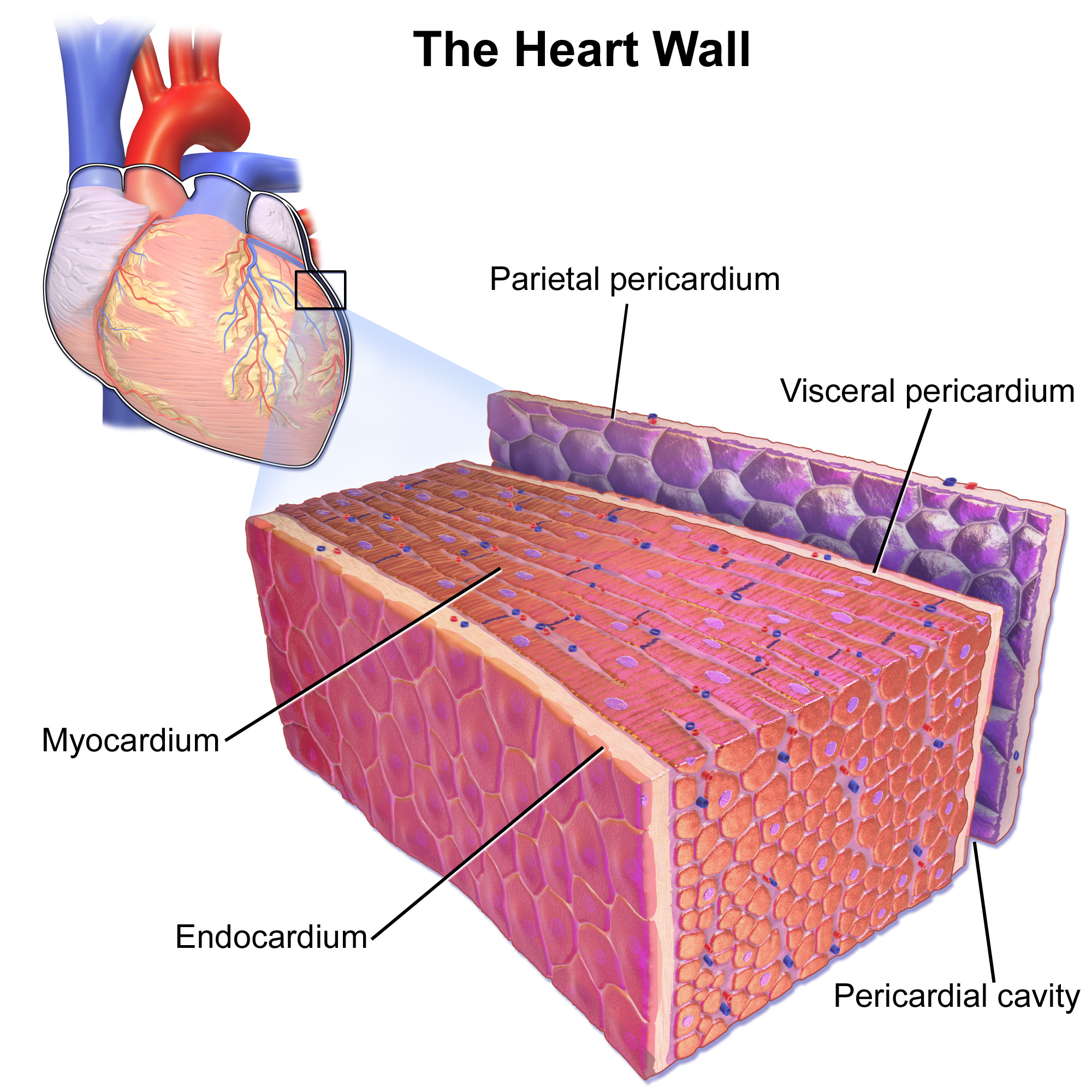
As shown in Figure 14.3.2, the wall of the heart is made up of three layers, called the endocardium, myocardium, and pericardium.
- The endocardium is the innermost layer of the heart wall. It is made up primarily of simple epithelial cells. It covers the heart chambers and valves. A thin layer of connective tissue joins the endocardium to the myocardium.
- The myocardium is the middle and thickest layer of the heart wall. It consists of cardiac muscle surrounded by a framework of collagen. There are two types of cardiac muscle cells in the myocardium: cardiomyocytes — which have the ability to contract easily — and pacemaker cells, which conduct electrical impulses that cause the cardiomyocytes to contract. About 99 per cent of cardiac muscle cells are cardiomyocytes, and the remaining one per cent is pacemaker cells. The myocardium is supplied with blood vessels and nerve fibres via the pericardium.
- The pericardium is a protective sac that encloses and protects the heart. The pericardium consists of two membranes (visceral pericardium and parietal pericardium), between which there is a fluid-filled cavity. The fluid helps to cushion the heart, and also lubricates its outer surface.
Heart Chambers
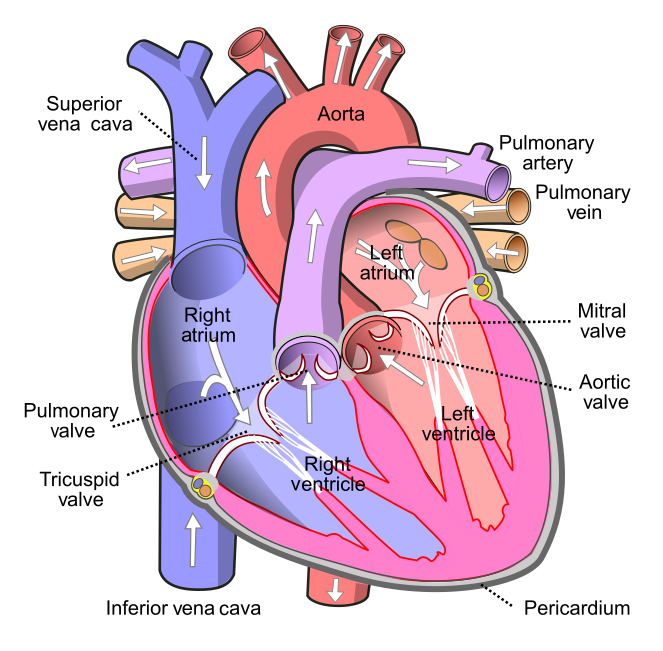
As shown in Figure 14.3.3 the four chambers of the heart include two upper chambers called atria (singular, atrium), and two lower chambers called ventricles. The atria are also referred to as receiving chambers, because blood coming into the heart first enters these two chambers. The right atrium receives deoxygenated blood from the upper and lower body through the superior vena cava and inferior vena cava, respectively. The left atrium receives oxygenated blood from the lungs through the pulmonary veins. The ventricles are also referred to as discharging chambers, because blood leaving the heart passes out through these two chambers. The right ventricle discharges blood to the lungs through the pulmonary artery, and the left ventricle discharges blood to the rest of the body through the aorta. The four chambers are separated from each other by dense connective tissue consisting mainly of collagen.
Heart Valves
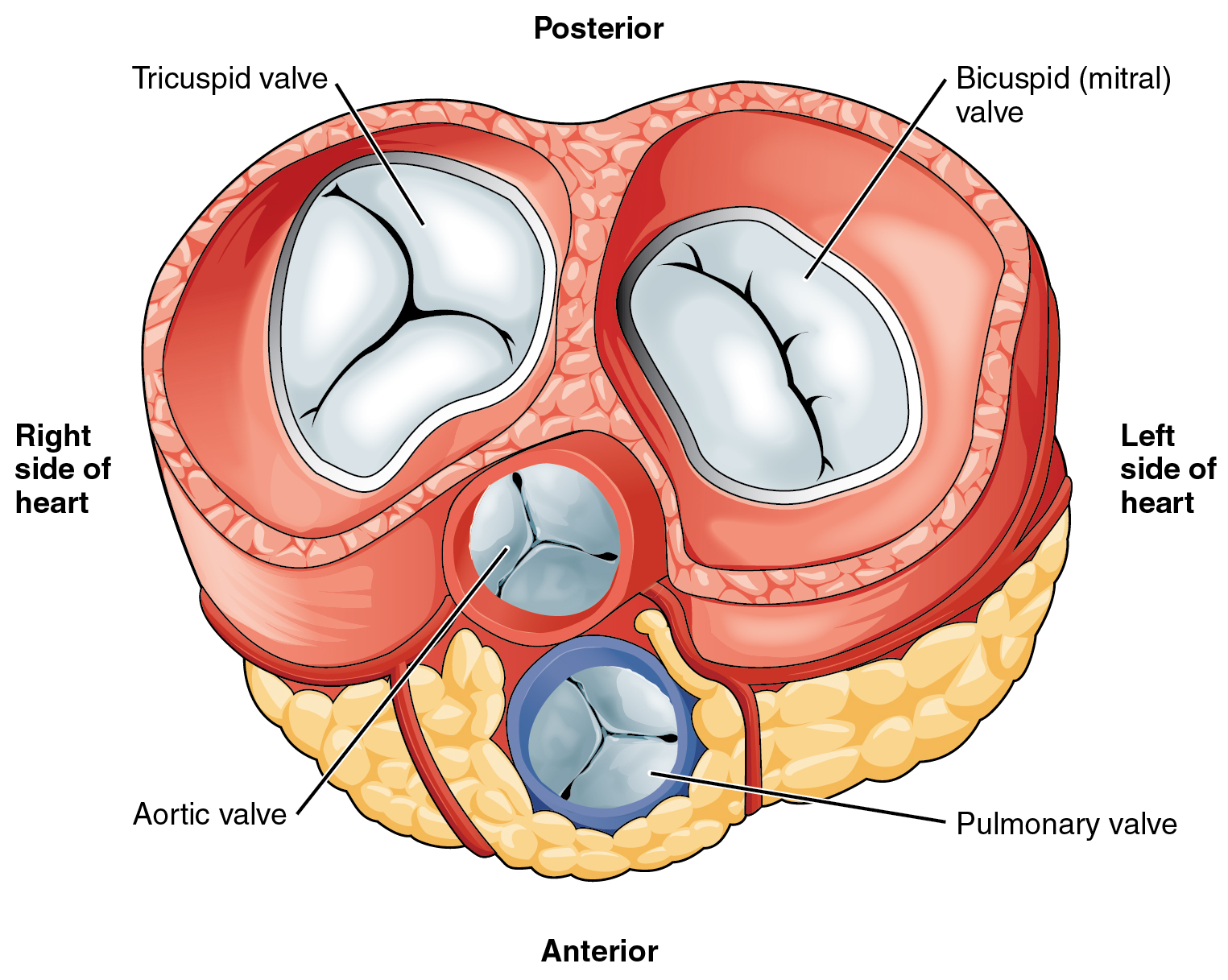
Figure 14.3.4 shows the location of the heart's four valves in a top-down view, looking down at the heart as if the arteries and veins feeding into and out of the heart were removed. The heart valves allow blood to flow from the atria to the ventricles, and from the ventricles to the pulmonary artery and aorta. The valves are constructed in such a way that blood can flow through them in only one direction, thus preventing the backflow of blood. Figure 14.3.5 shows how valves open to let blood into the appropriate chamber, and then close to prevent blood from moving in the wrong direction and the next chamber contracts. The four valves are the:
- Tricuspid atrioventricular valve, (can be shortened to tricuspid AV valve) which allows blood to flow from the right atrium to the right ventricle.
- Bicuspid atrioventricular valve (also know as the mitral valve), which allows blood to flow from the left atrium to the left ventricle.
- Pulmonary semilunar valve, which allows blood to flow from the right ventricle to the pulmonary artery.
- Aortic semilunar valve, which allows blood to flow from the left ventricle to the aorta.
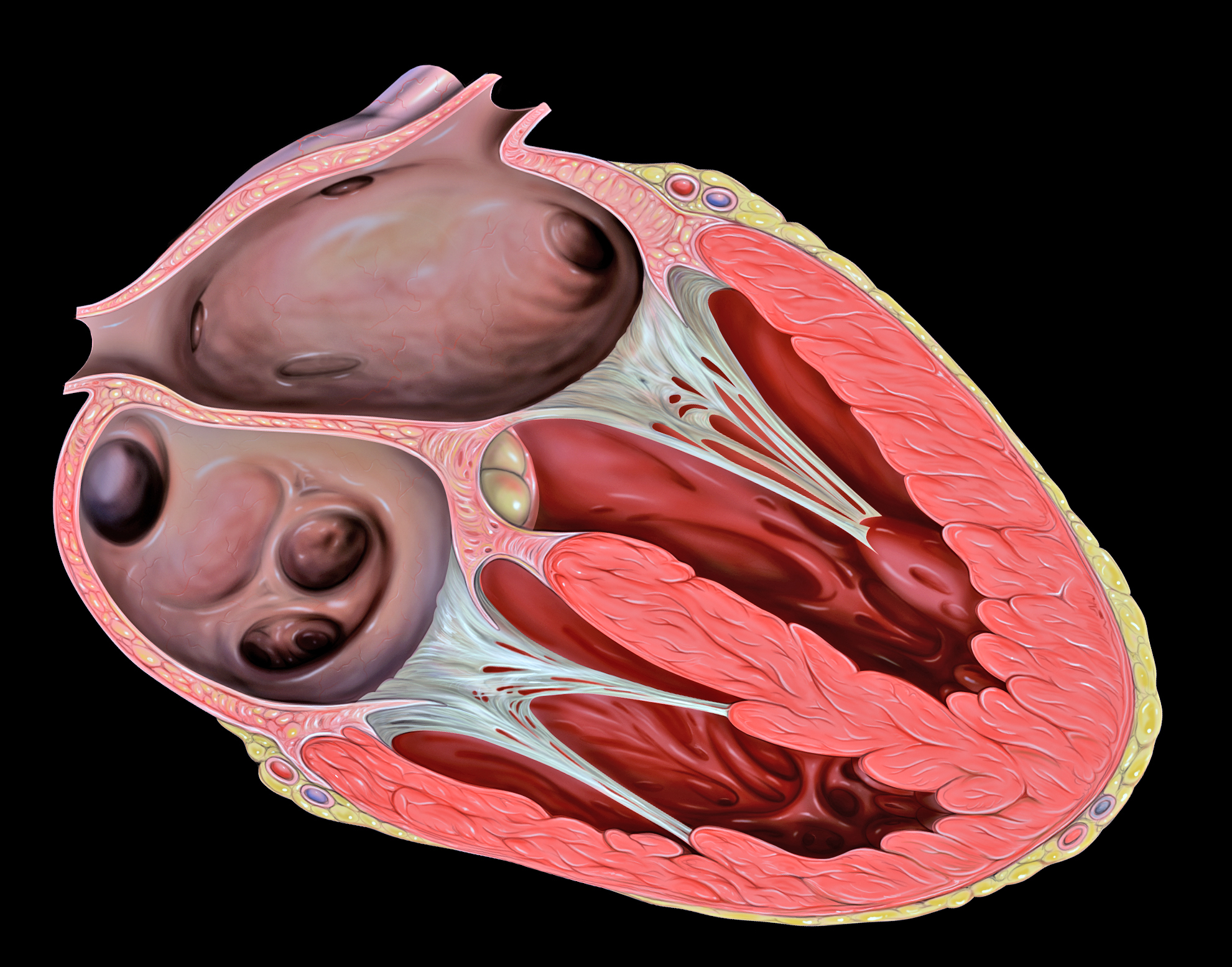
The two atrioventricular (AV) valves prevent backflow when the ventricles are contracting, while the semilunar valves prevent backflow from vessels. This means that the AV valves must withstand much more pressure than do the semilunar valves. In order to withstand the force of the ventricles contracting (to prevent blood from backflowing into the atria), the AV valves are reinforced with structures called chordae tendineae — tendon-like cords of connective tissue which anchor the valve and prevent it from prolapse. Figure 14.3.6 shows the structure and location of the chordae tendoneae.
The chordae tendoneae are under such force that they need special attachments to the interior of the ventricles where they anchor. Papillary muscles are specialized muscles in the interior of the ventricle that provide a strong anchor point for the chordae tendineae.
Coronary Circulation
The cardiomyocytes of the muscular walls of the heart are very active cells, because they are responsible for the constant beating of the heart. These cells need a continuous supply of oxygen and nutrients. The carbon dioxide and waste products they produce also must be continuously removed. The blood vessels that carry blood to and from the heart muscle cells make up the coronary circulation. Note that the blood vessels of the coronary circulation supply heart tissues with blood, and are different from the blood vessels that carry blood to and from the chambers of the heart as part of the general circulation. Coronary arteries supply oxygen-rich blood to the heart muscle cells. Coronary veins remove deoxygenated blood from the heart muscles cells.
- There are two coronary arteries — a right coronary artery that supplies the right side of the heart, and a left coronary artery that supplies the left side of the heart. These arteries branch repeatedly into smaller and smaller arteries and finally into capillaries, which exchange gases, nutrients, and waste products with cardiomyocytes.
- At the back of the heart, small cardiac veins drain into larger veins, and finally into the great cardiac vein, which empties into the right atrium. At the front of the heart, small cardiac veins drain directly into the right atrium.
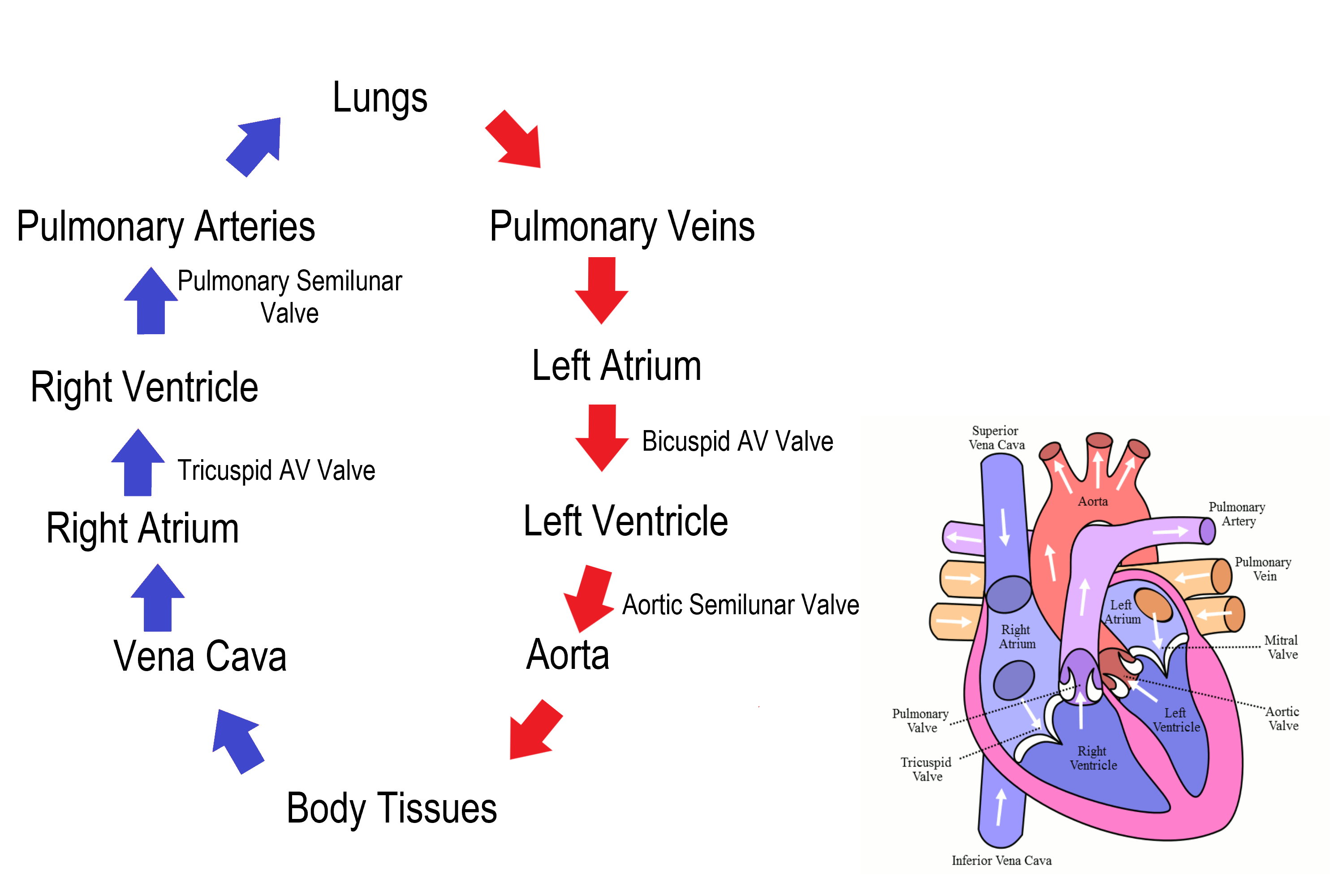
Blood Circulation Through the Heart
Figure 14.3.7 shows how blood circulates through the chambers of the heart. The right atrium collects blood from two large veins, the superior vena cava (from the upper body) and the inferior vena cava (from the lower body). The blood that collects in the right atrium is pumped through the tricuspid valve into the right ventricle. From the right ventricle, the blood is pumped through the pulmonary valve into the pulmonary artery. The pulmonary artery carries the blood to the lungs, where it enters the pulmonary circulation, gives up carbon dioxide, and picks up oxygen. The oxygenated blood travels back from the lungs through the pulmonary veins (of which there are four), and enters the left atrium of the heart. From the left atrium, the blood is pumped through the mitral valve into the left ventricle. From the left ventricle, the blood is pumped through the aortic valve into the aorta, which subsequently branches into smaller arteries that carry the blood throughout the rest of the body. After passing through capillaries and exchanging substances with cells, the blood returns to the right atrium via the superior vena cava and inferior vena cava, and the process begins anew.
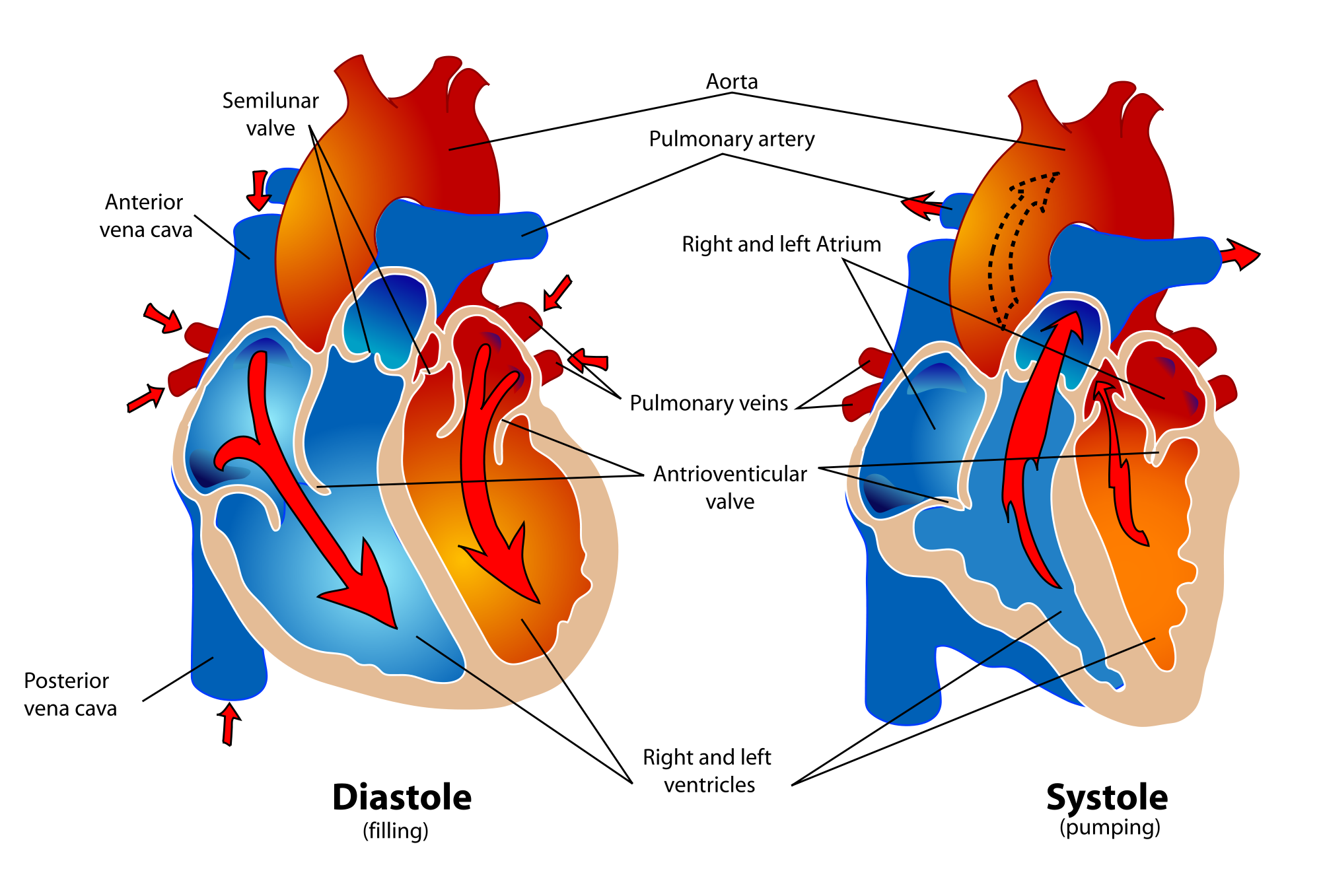
Cardiac Cycle
The cardiac cycle refers to a single complete heartbeat, which includes one iteration of the lub and dub sounds heard through a stethoscope. During the cardiac cycle, the atria and ventricles work in a coordinated fashion so that blood is pumped efficiently through and out of the heart. The cardiac cycle includes two parts, called diastole and systole, which are illustrated in the diagrams in Figure 14.3.8.
- During diastole, the atria contract and pump blood into the ventricles, while the ventricles relax and fill with blood from the atria.
- During systole, the atria relax and collect blood from the lungs and body, while the ventricles contract and pump blood out of the heart.
Electrical Stimulation of the Heart
The normal, rhythmical beating of the heart is called sinus rhythm. It is established by the heart’s pacemaker cells, which are located in an area of the heart called the sinoatrial node (shown in Figure 14.3.9). The pacemaker cells create electrical signals with the movement of electrolytes (sodium, potassium, and calcium ions) into and out of the cells. For each cardiac cycle, an electrical signal rapidly travels first from the sinoatrial node, to the right and left atria so they contract together. Then, the signal travels to another node, called the atrioventricular node (Figure 14.3.9), and from there to the right and left ventricles (which also contract together), just a split second after the atria contract.
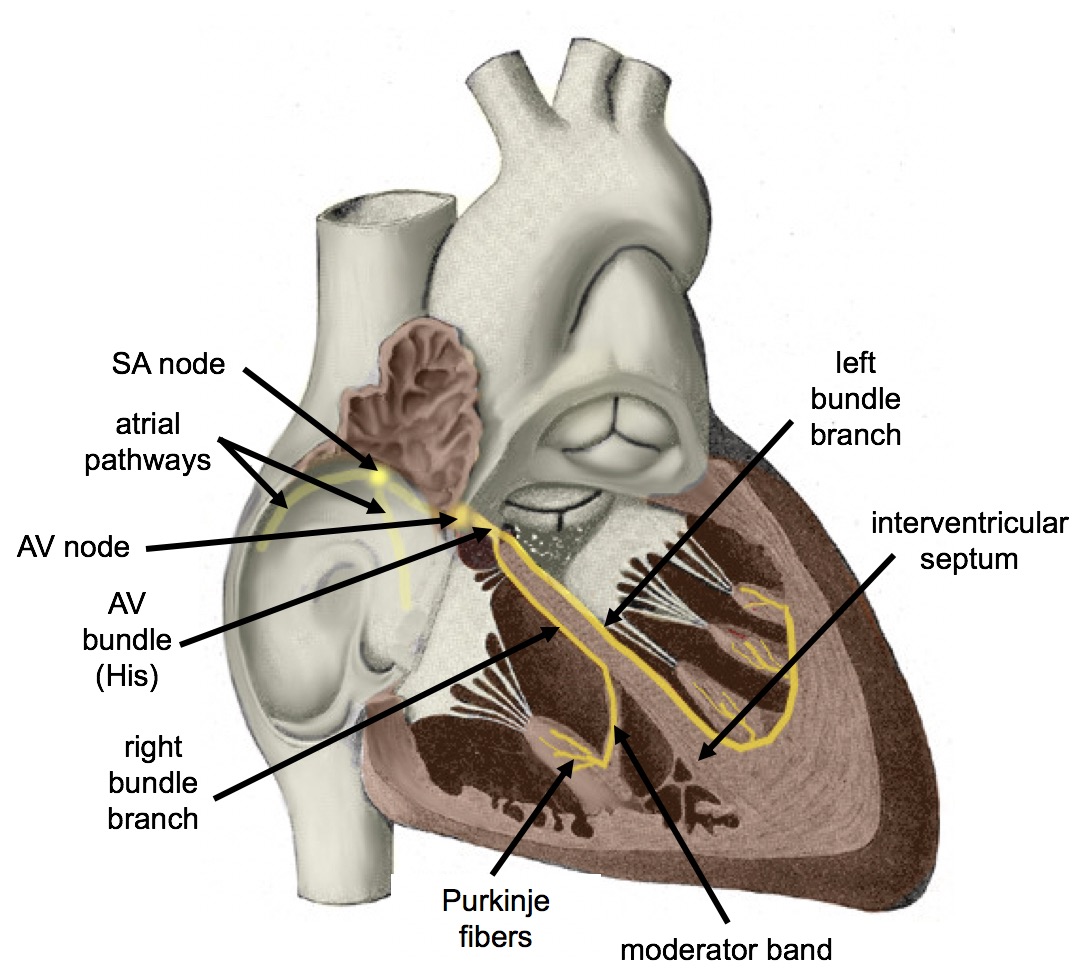
The normal sinus rhythm of the heart is influenced by the autonomic nervous system through sympathetic and parasympathetic nerves. These nerves arise from two paired cardiovascular centers in the medulla of the brainstem. The parasympathetic nerves act to decrease the heart rate, and the sympathetic nerves act to increase the heart rate. Parasympathetic input normally predominates. Without it, the pacemaker cells of the heart would generate a resting heart rate of about 100 beats per minute, instead of a normal resting heart rate of about 72 beats per minute. The cardiovascular centers receive input from receptors throughout the body, and act through the sympathetic nerves to increase the heart rate, as needed. Increased physical activity, for example, is detected by receptors in muscles, joints, and tendons. These receptors send nerve impulses to the cardiovascular centers, causing sympathetic nerves to increase the heart rate, and allowing more blood to flow to the muscles.
Besides the autonomic nervous system, other factors can also affect the heart rate. For example, thyroid hormones and adrenal hormones (such as epinephrine) can stimulate the heart to beat faster. The heart rate also increases when blood pressure drops or the body is dehydrated or overheated. On the other hand, cooling of the body and relaxation — among other factors — can contribute to a decrease in the heart rate.
Feature: Human Biology in the News
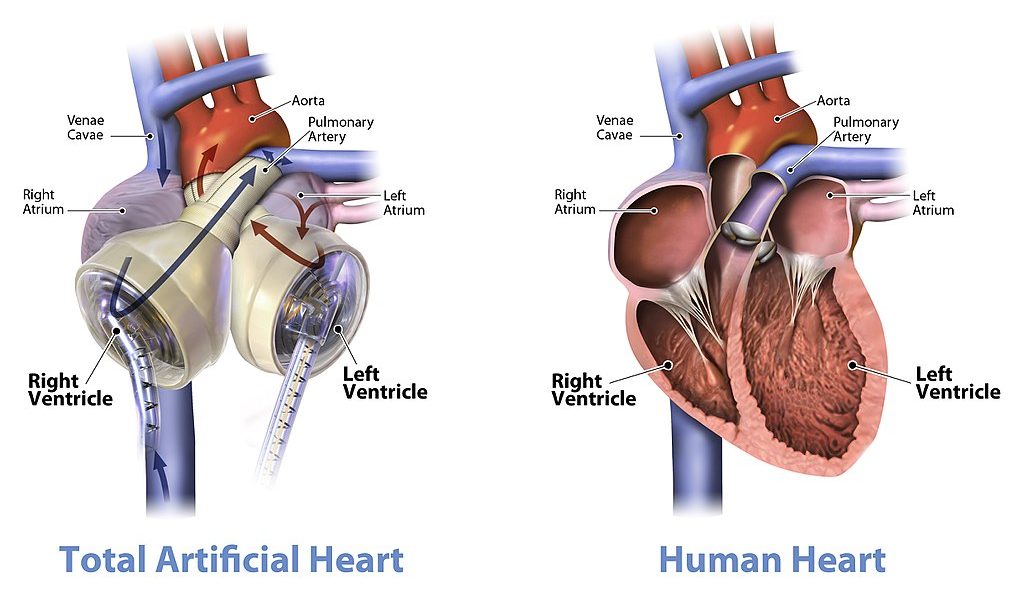
When a patient’s heart is too diseased or damaged to sustain life, a heart transplant is likely to be the only long-term solution. The first successful heart transplant was undertaken in South Africa in 1967. There are over 2,200 Canadians walking around today because of life-saving heart transplant surgery. Approximately 180 heart transplant surgeries are performed each year, but there are still so many Canadians on the transplant list that some die while waiting for a heart. The problem is that far too few hearts are available for transplant — there is more demand (people waiting for a heart transplant) than supply (organ donors). Sometimes, recipient hopefuls will receive a device called a Total Artificial Heart (see Figure 14.3.10), which can buy them some time until a donor heart becomes available.
Watch the video below "Total artificial heart option..." from Stanford Health Care to see how it works:
https://youtu.be/1PtxaxcPnGc
Total artificial heart option at Stanford (Includes surgical graphic footage), Stanford Health Care, 2014.
14.3 Summary
- The heart is a muscular organ behind the sternum and slightly to the left of the center of the chest. Its function is to pump blood through the blood vessels of the cardiovascular system.
- The wall of the heart consists of three layers. The middle layer, the myocardium, is the thickest layer and consists mainly of cardiac muscle. The interior of the heart consists of four chambers, with an upper atrium and lower ventricle on each side of the heart. Blood enters the heart through the atria, which pump it to the ventricles. Then the ventricles pump blood out of the heart. Four valves in the heart keep blood flowing in the correct direction and prevent backflow.
- The coronary circulation consists of blood vessels that carry blood to and from the heart muscle cells, and is different from the general circulation of blood through the heart chambers. There are two coronary arteries that supply the two sides of the heart with oxygenated blood. Cardiac veins drain deoxygenated blood back into the heart.
- Deoxygenated blood flows into the right atrium through veins from the upper and lower body (superior and inferior vena cava, respectively), and oxygenated blood flows into the left atrium through four pulmonary veins from the lungs. Each atrium pumps the blood to the ventricle below it. From the right ventricle, deoxygenated blood is pumped to the lungs through the two pulmonary arteries. From the left ventricle, oxygenated blood is pumped to the rest of the body through the aorta.
- The cardiac cycle refers to a single complete heartbeat. It includes diastole — when the atria contract — and systole, when the ventricles contract.
- The normal, rhythmic beating of the heart is called sinus rhythm. It is established by the heart’s pacemaker cells in the sinoatrial node. Electrical signals from the pacemaker cells travel to the atria, and cause them to contract. Then, the signals travel to the atrioventricular node and from there to the ventricles, causing them to contract. Electrical stimulation from the autonomic nervous system and hormones from the endocrine system can also influence heartbeat.
14.3 Review Questions
- What is the heart, where is located, and what is its function?
-
- Describe the coronary circulation.
- Summarize how blood flows into, through, and out of the heart.
- Explain what controls the beating of the heart.
- What are the two types of cardiac muscle cells in the myocardium? What are the differences between these two types of cells?
- Explain why the blood from the cardiac veins empties into the right atrium of the heart. Focus on function (rather than anatomy) in your answer.
14.3 Explore More
https://www.youtube.com/watch?v=1bnzVjOJ6NM
Noel Bairey Merz: The single biggest health threat women face, TED, 2012.
https://www.youtube.com/watch?v=jJm7zBcN6-M
Watch a Transcatheter Aortic Valve Replacement (TAVR) Procedure at St. Luke's in Cedar Rapids, Iowa, UnityPoint Health - Cedar Rapids, 2018.
https://www.youtube.com/watch?v=zU6mmix04PI
A Change of Heart: My Transplant Experience | Thomas Volk | TEDxUWLaCrosse, TEDx Talks, 2018.
https://www.youtube.com/watch?v=biGuwQhuAsk
Heart Transplant Recipient Meets Donor Family For The First Time, WMC Health, 2018.
Attributions
Figure 14.3.1
- Female clinician dressed in scrubs using a stethoscope by Amanda Mills, USCDCP, on Pixnio is used under a CC0 public domain certification license (https://creativecommons.org/licenses/publicdomain/).
- Human heart beating loud and strong (audio) by Daniel Simion on Soundbible.com is used under a CC BY 3.0 (https://creativecommons.org/licenses/by/3.0) license.
Figure 14.3.2
Blausen_0470_HeartWall by BruceBlaus on Wikimedia Commons is used under a CC BY 3.0 (https://creativecommons.org/licenses/by/3.0) license.
Figure 14.3.3
Diagram_of_the_human_heart_(cropped).svg by Wapcaplet on Wikimedia Commons is used under a CC BY-SA 3.0 (http://creativecommons.org/licenses/by-sa/3.0/) license.
Figure 14.3.4
Heart_Valves by OpenStax College on Wikimedia Commons is used under a CC BY 3.0 (https://creativecommons.org/licenses/by/3.0) license.
Figure 14.3.5
CG_Heart Valve Animation by DrJanaOfficial on Wikimedia Commons is used under a CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0) license.
Figure 14.3.6
Heart_tee_four_chamber_view by Patrick J. Lynch, medical illustrator from Yale University School of Medicine, on Wikimedia Commons is used under a CC BY 2.5 (https://creativecommons.org/licenses/by/2.5) license.
Figure 14.3.7
Circulation of blood through the heart by Christinelmiller on Wikimedia Commons is used under a CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0) license. [Original image in the bottom right is by Wapcaplet / CC BY-SA 3.0 (https://creativecommons.org/licenses/by-sa/3.0/)]
Figure 14.3.8
Human_healthy_pumping_heart_en.svg by Mariana Ruiz Villarreal [LadyofHats] on Wikimedia Common is released into the public domain (https://en.wikipedia.org/wiki/Public_domain).
Figure 14.3.9
Cardiac_Conduction_System by Cypressvine on Wikimedia Commons is used under a CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0) license.
References
Betts, J. G., Young, K.A., Wise, J.A., Johnson, E., Poe, B., Kruse, D.H., Korol, O., Johnson, J.E., Womble, M., DeSaix, P. (2013, June 19). Figure 19.12 Heart valves with the atria and major vessels removed [digital image]. In Anatomy and Physiology (Section 19.1). OpenStax. https://openstax.org/books/anatomy-and-physiology/pages/19-1-heart-anatomy#fig-ch20_01_04
Blausen.com Staff. (2014). Medical gallery of Blausen Medical 2014. WikiJournal of Medicine 1 (2). DOI:10.15347/wjm/2014.010. ISSN 2002-4436.
Heart and Stroke Foundation of Canada. (n.d.). https://www.heartandstroke.ca/
Sliwa, K., Zilla, P. (2017, December 7). 50th anniversary of the first human heart transplant—How is it seen today? European Heart Journal, 38(46):3402–3404. https://doi.org/10.1093/eurheartj/ehx695
Stanford Health Care. (2014, December 3). Total artificial heart option at Stanford (Includes surgical graphic footage). YouTube. https://www.youtube.com/watch?v=1PtxaxcPnGc&feature=youtu.be
TED. (2012, March 21). Noel Bairey Merz: The single biggest health threat women face. YouTube. https://www.youtube.com/watch?v=1bnzVjOJ6NM&feature=youtu.be
TEDx Talks. (2018, April 18). A change of heart: My transplant experience | Thomas Volk | TEDxUWLaCrosse. YouTube. https://www.youtube.com/watch?v=zU6mmix04PI&feature=youtu.be
UMagazine. (2015, Fall). The cutting edge: Patient first to bridge from experimental total artificial heart to transplant. UCLA Health. https://www.uclahealth.org/u-magazine/patient-first-to-bridge-from-experimental-total-artificial-heart-to-transplant
UnityPoint Health - Cedar Rapids. (2018, February 7). Watch a transcatheter aortic valve replacement (TAVR) Procedure at St. Luke's in Cedar Rapids, Iowa. YouTube. https://www.youtube.com/watch?v=jJm7zBcN6-M&feature=youtu.be
WMC Health. (2018, September 13). Heart transplant recipient meets donor family for the first time. YouTube. https://www.youtube.com/watch?v=biGuwQhuAsk&feature=youtu.be
Created by CK-12 Foundation/Adapted by Christine Miller

Bulging Veins
Why do bodybuilders have such prominent veins? Bulging muscles push surface veins closer to the skin. Combine that with a virtual lack of subcutaneous fat, and you have bulging veins, as well as bulging muscles. Veins are one of three major types of blood vessels in the cardiovascular system.
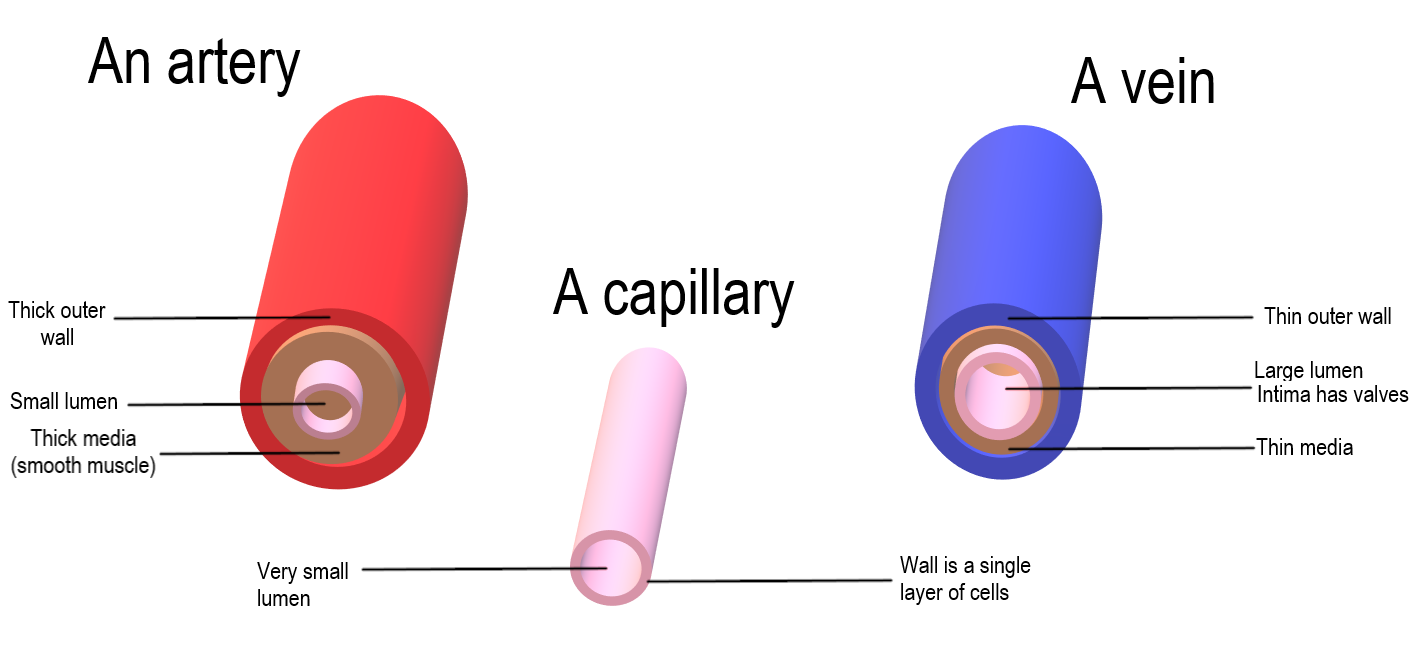
Types of Blood Vessels
Blood vessels are the part of the cardiovascular system that transports blood throughout the human body. There are three major types of blood vessels. Besides veins, they include arteries and capillaries.
Arteries
Arteries are defined as blood vessels that carry blood away from the heart. Blood flows through arteries largely because it is under pressure from the pumping action of the heart. It should be noted that coronary arteries, which supply heart muscle cells with blood, travel toward the heart, but not as part of the blood flow that travels through the chambers of the heart. Most arteries, including coronary arteries, carry oxygenated blood, but there are a few exceptions, most notably the pulmonary artery. This artery carries deoxygenated blood from the heart to the lungs, where it picks up oxygen and releases carbon dioxide. In virtually all other arteries, the hemoglobin in red blood cells is highly saturated with oxygen (95–100 per cent). These arteries distribute oxygenated blood to tissues throughout the body.
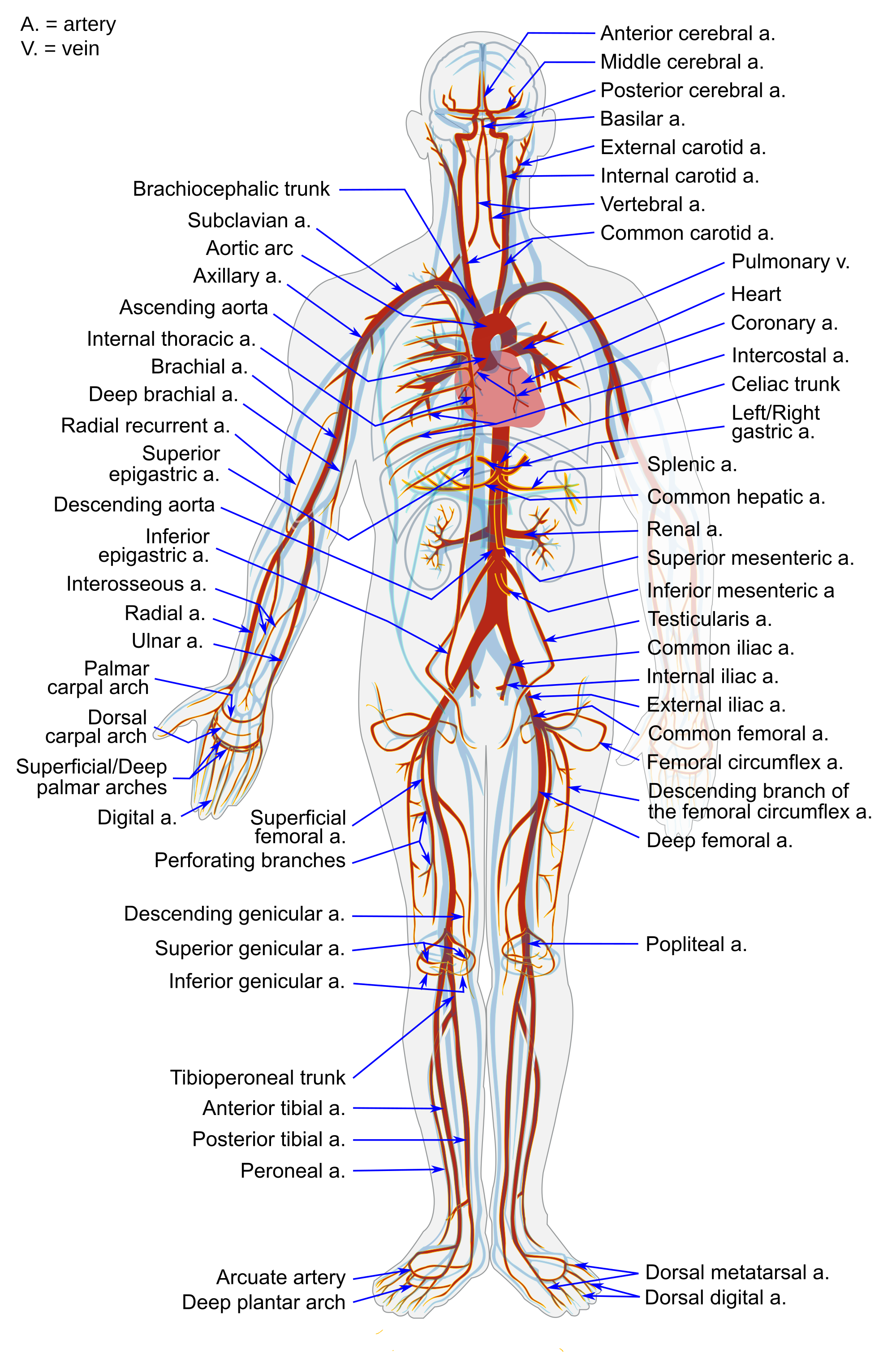
The largest artery in the body is the aorta, which is connected to the heart and extends down into the abdomen (see Figure 14.4.2). The aorta has high-pressure, oxygenated blood pumped directly into it from the left ventricle of the heart. The aorta has many branches, and the branches subdivide repeatedly, with the subdivisions growing smaller and smaller in diameter. The smallest arteries are called arterioles.
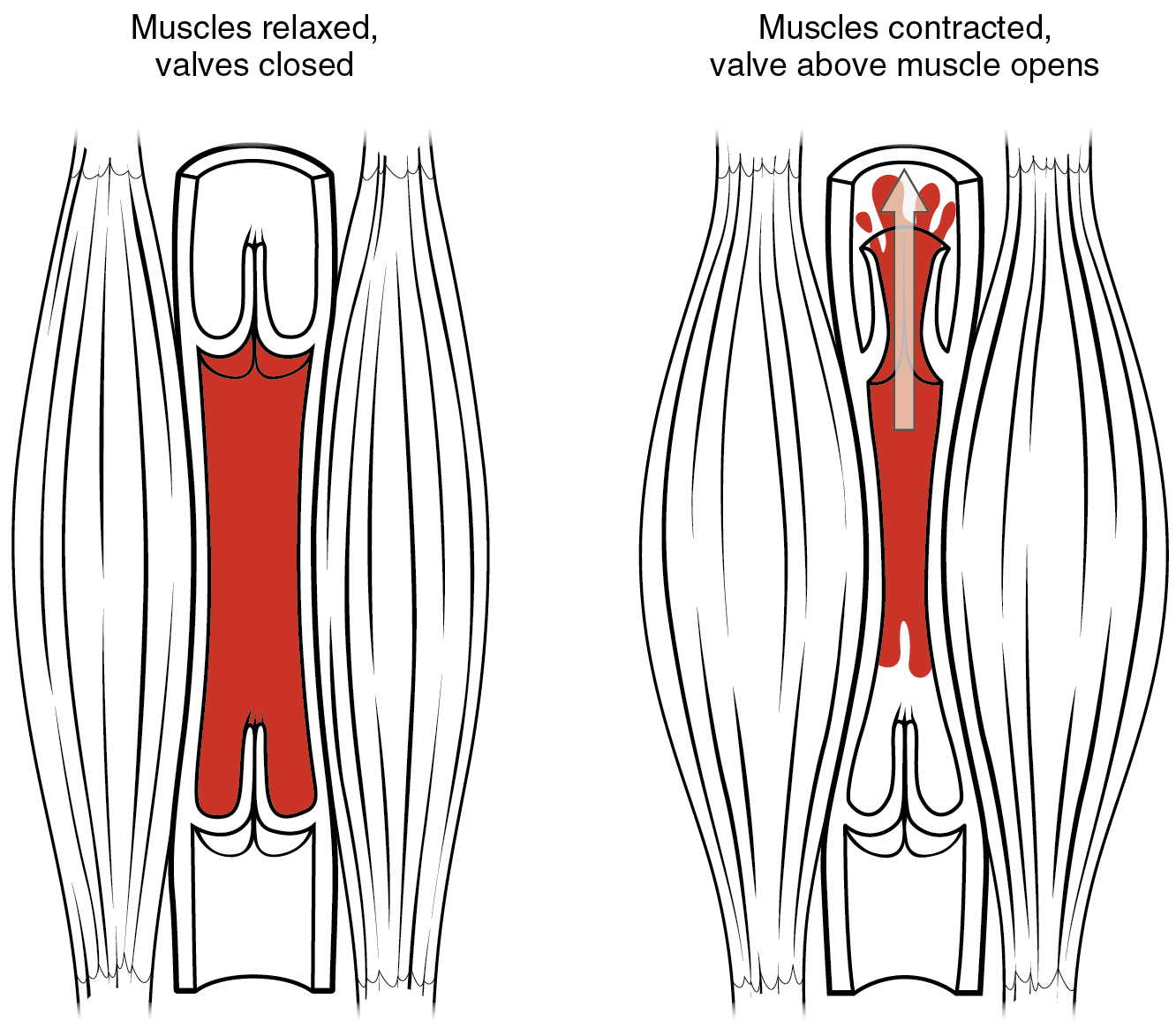
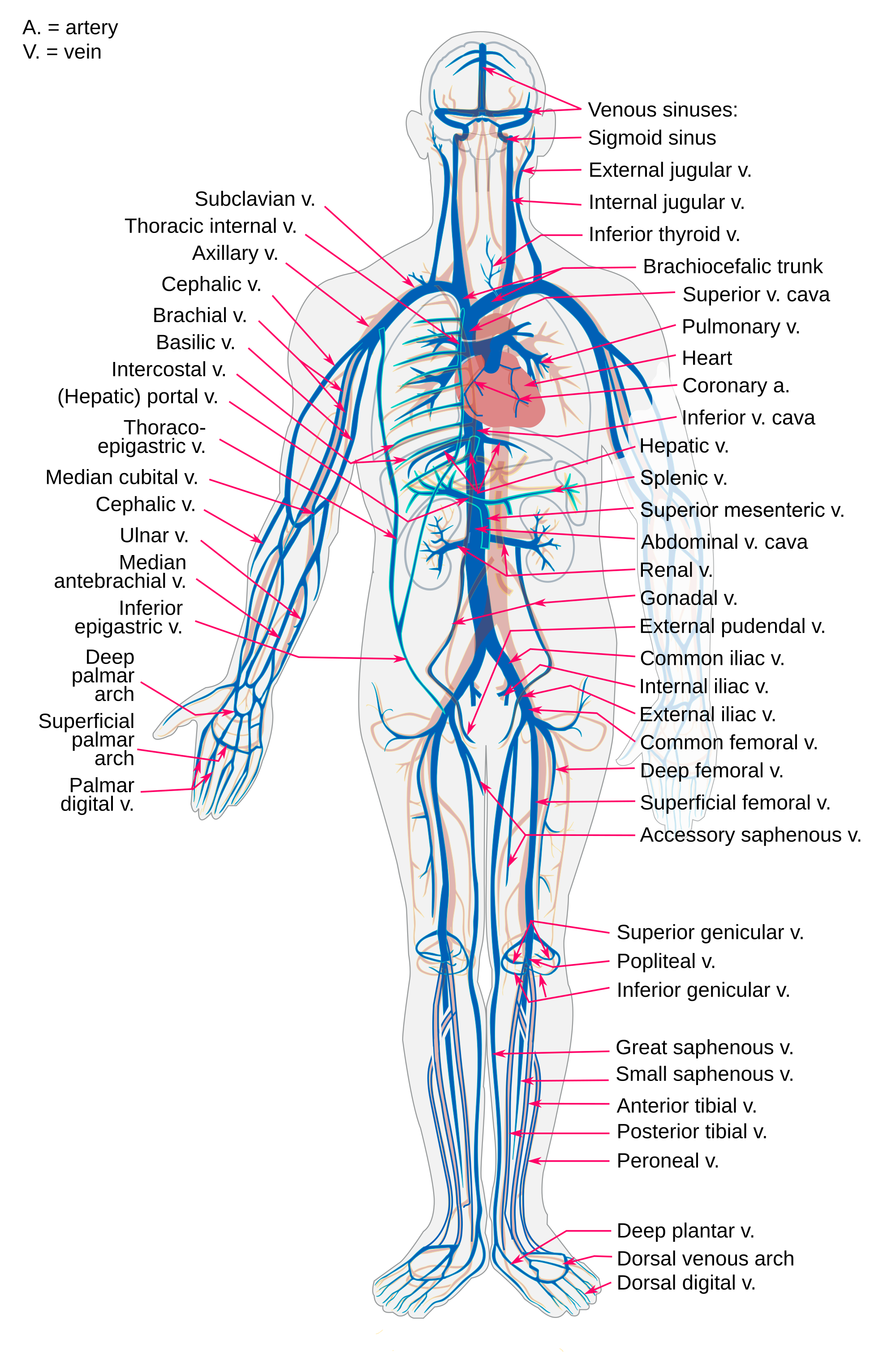
Veins
Veins are defined as blood vessels that carry blood toward the heart. Blood traveling through veins is not under pressure from the beating heart. It gets help moving along by the squeezing action of skeletal muscles, for example, when you walk or breathe. It is also prevented from flowing backward by valves in the larger veins, as illustrated in Figure 14.4.3. and as seen in the ultrasonography image in Figure 14.4.4. Veins are called capacitance blood vessels, because the majority of the body’s total volume of blood (about 60 per cent) is contained within veins.
Most veins carry deoxygenated blood, but there are a few exceptions, including the four pulmonary veins. These veins carry oxygenated blood from the lungs to the heart, which then pumps the blood to the rest of the body. In virtually all other veins, hemoglobin is relatively unsaturated with oxygen (about 75 per cent).
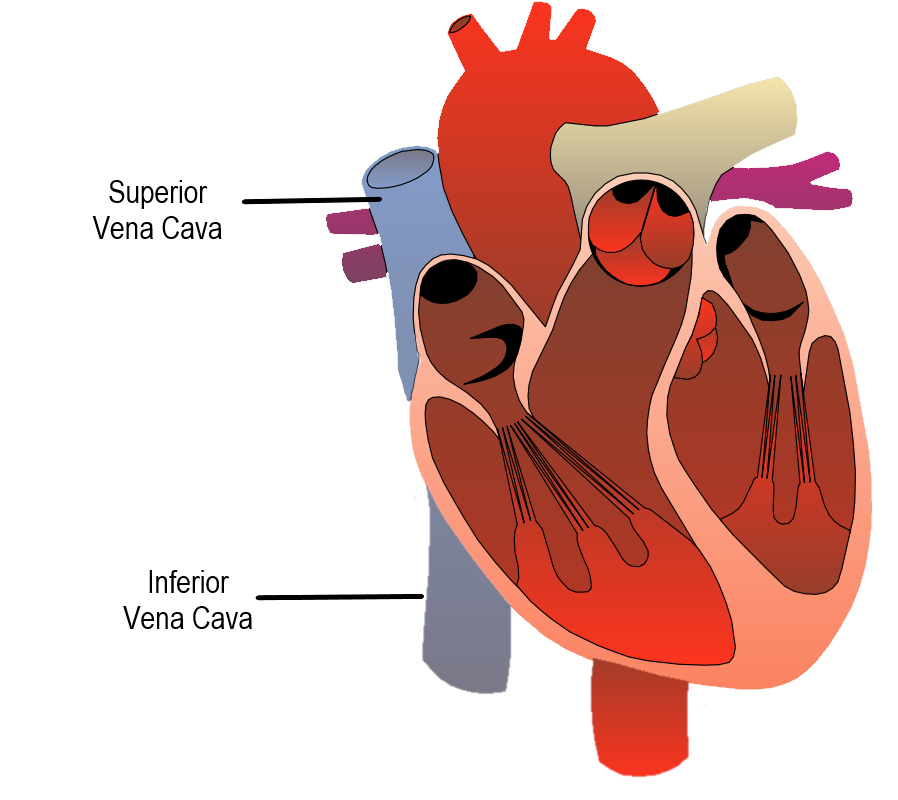
The two largest veins in the body are the superior vena cava — which carries blood from the upper body directly to the right atrium of the heart — and the inferior vena cava, which carries blood from the lower body directly to the right atrium (shown in Figure 14.4.5). Like arteries, veins form a complex, branching system of larger and smaller vessels. The smallest veins are called venules. They receive blood from capillaries and transport it to larger veins. Each venule receives blood from multiple capillaries. See the major veins of the human body in Figure 14.4.6.
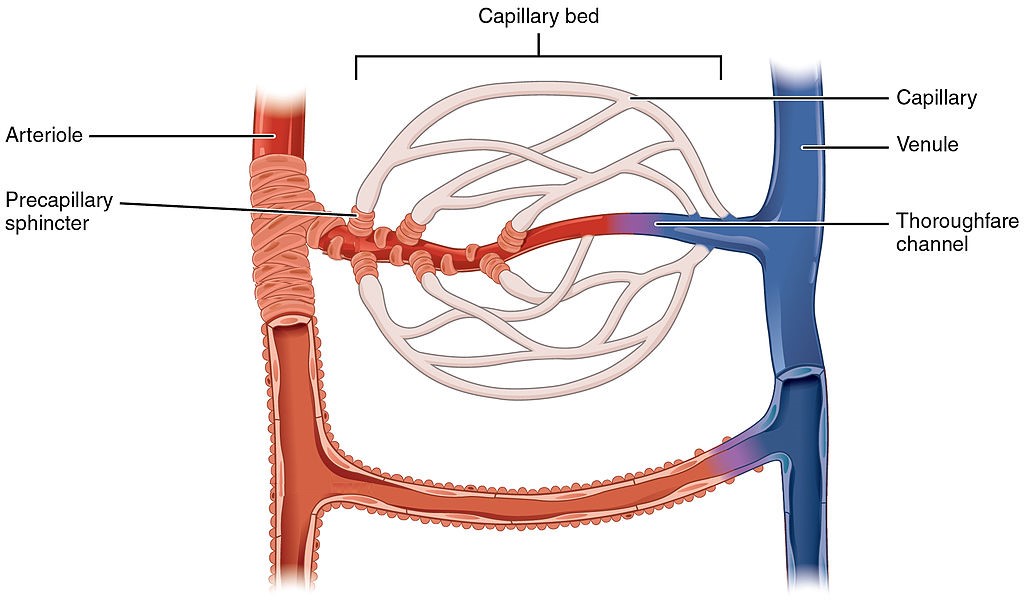
Capillaries
Capillaries are the smallest blood vessels in the cardiovascular system. They are so small that only one red blood cell at a time can squeeze through a capillary, and then only if the red blood cell deforms. Capillaries connect arterioles and venules, as shown in Figure 14.4.7. Capillaries generally form a branching network of vessels, called a capillary bed, that provides a large surface area for the exchange of substances between the blood and surrounding tissues.
Structure of Blood Vessels
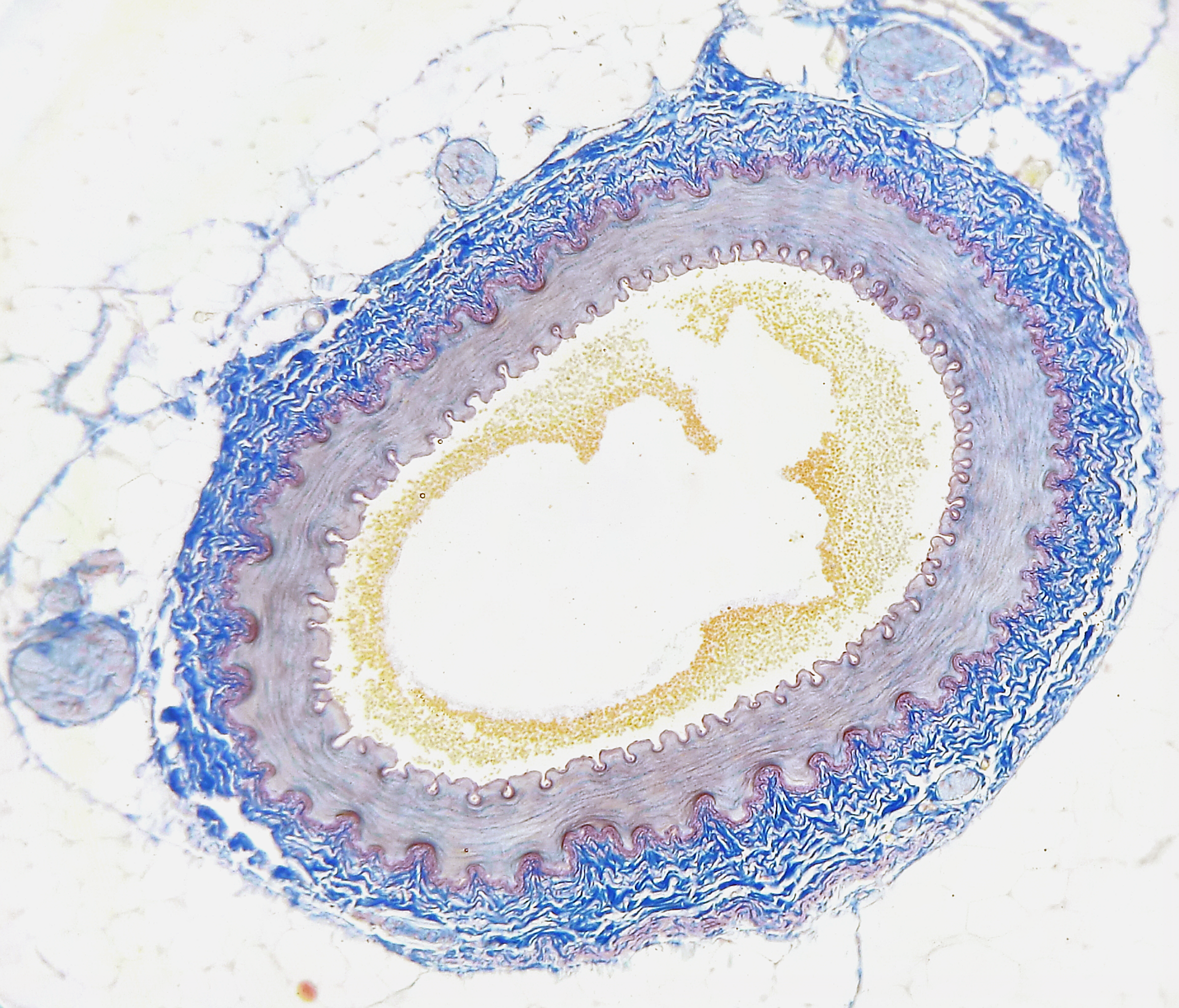
All blood vessels are basically hollow tubes with an internal space, called a lumen, through which blood flows. The lumen of an artery is shown in cross section in the photomicrograph (Figure 14.4.8). The width of blood vessels varies, but they all have a lumen. The walls of blood vessels differ depending on the type of vessel. In general, arteries and veins are more similar to one another than to capillaries in the structure of their walls.
Walls of Arteries and Veins
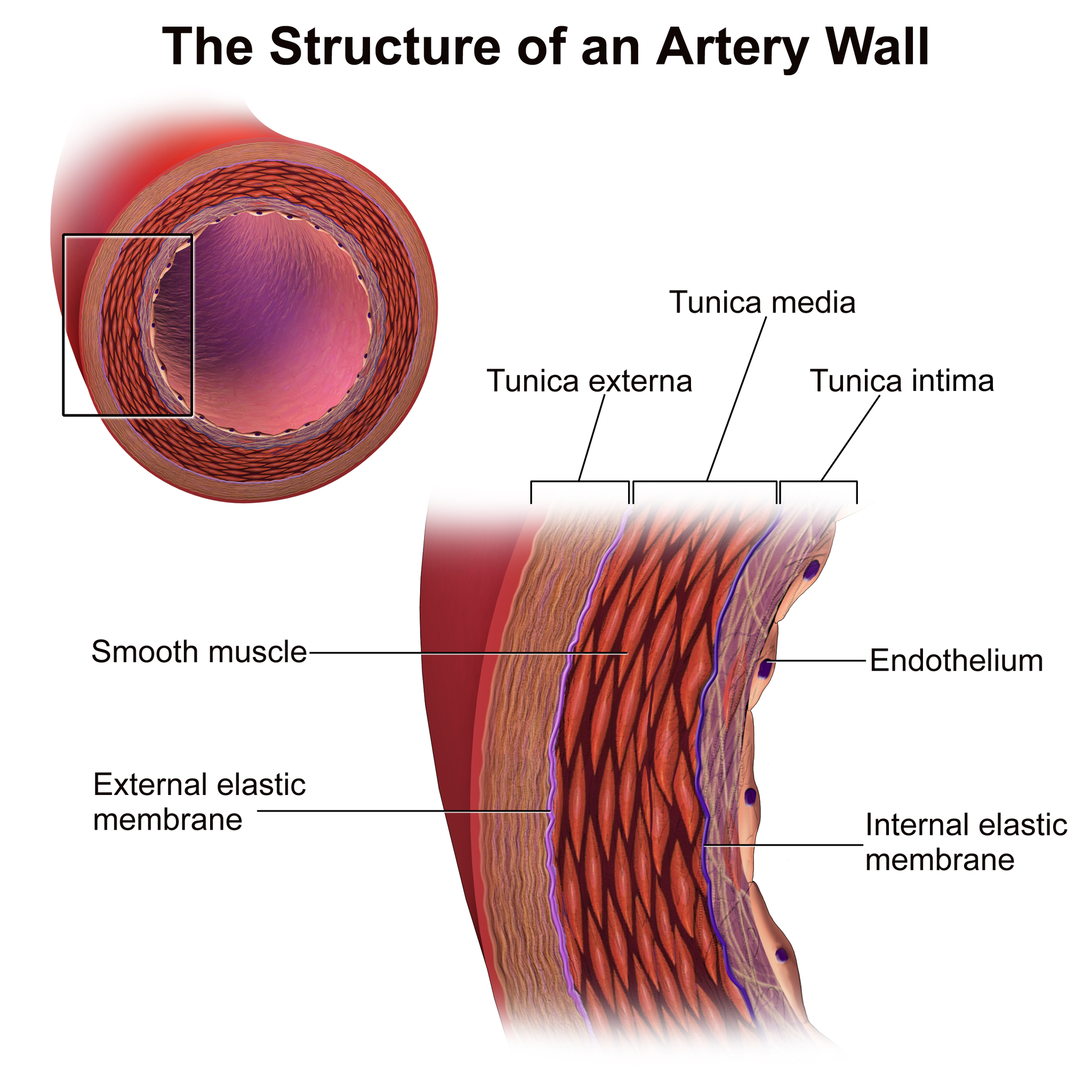
The walls of both arteries and veins have three layers: the tunica intima, tunica media, and tunica adventitia. You can see the three layers for an artery in the Figure 14.4.9.
- The tunica intima is the inner layer of arteries and veins. It is also the thinnest layer, consisting of a single layer of endothelial cells surrounded by a thin layer of connective tissues. It reduces friction between the blood and the inside of the blood vessel walls.
- The tunica media is the middle layer of arteries and veins. In arteries, this is the thickest layer. It consists mainly of elastic fibres and connective tissues. In arteries, this is the thickest layer, because it also contains smooth muscle tissues, which control the diameter of the vessels- as such, the width of the tunic media can be helpful in distinguishing arteries from veins.
- The tunica externa (also called tunica adventitia) is the outer layer of arteries and veins. It consists of connective tissue, and also contains nerves. In veins, this is the thickest layer. In general, the tunica externa protects and strengthens vessels, and attaches them to surrounding structures.
Capillary Walls
The walls of capillaries consist of little more than a single layer of epithelial cells. Being just one cell thick, the walls are well-suited for the exchange of substances between the blood inside them and the cells of surrounding tissues. Substances including water, oxygen, glucose, and other nutrients, as well as waste products (such as carbon dioxide), can pass quickly and easily through the extremely thin walls of capillaries. See figure 14.4.9 for a comparison of the structure of arteries, veins and capillaries.
Blood Pressure
The blood in arteries is normally under pressure because of the beating of the heart. The pressure is highest when the heart contracts and pumps out blood, and lowest when the heart relaxes and refills with blood. (You can feel this variation in pressure in your wrist or neck when you count your pulse.) Blood pressure is a measure of the force that blood exerts on the walls of arteries. It is generally measured in millimetres of mercury (mm Hg), and expressed as a double number — a higher number for systolic pressure when the ventricles contract, and a lower number for diastolic pressure when the ventricles relax. Normal blood pressure is generally defined as less than 120 mm Hg (systolic)/80 mm Hg (diastolic) when measured in the arm at the level of the heart. It decreases as blood flows farther away from the heart and into smaller arteries.
As arteries grow smaller, there is increasing resistance to blood flow through them, because of the blood's friction against the arterial walls. This resistance restricts blood flow so that less blood reaches smaller, downstream vessels, thus reducing blood pressure before the blood flows into the tiniest vessels, the capillaries. Without this reduction in blood pressure, capillaries would not be able to withstand the pressure of the blood without bursting. By the time blood flows through the veins, it is under very little pressure. The pressure of blood against the walls of veins is always about the same — normally no more than 10 mm Hg.
Vasoconstriction and Vasodilation
Smooth muscles in the walls of arteries can contract or relax to cause vasoconstriction (narrowing of the lumen of blood vessels) or vasodilation (widening of the lumen of blood vessels). This allows the arteries — especially the arterioles — to contract or relax as needed to help regulate blood pressure. In this regard, the arterioles act like an adjustable nozzle on a garden hose. When they narrow, the increased friction with the arterial walls causes less blood to flow downstream from the narrowing, resulting in a drop in blood pressure. These actions are controlled by the autonomic nervous system in response to pressure-sensitive sensory receptors in the walls of larger arteries.
Arteries can also dilate or constrict to help regulate body temperature, by allowing more or less blood to flow from the warm body core to the body’s surface. In addition, vasoconstriction and vasodilation play roles in the fight-or-flight response, under control of the sympathetic nervous system. Vasodilation allows more blood to flow to skeletal muscles, and vasoconstriction reduces blood flow to digestive organs.
Feature: My Human Body

The lumpy appearance of this man’s leg (Figure 14.4.10) is caused by varicose veins. Do you have varicose veins? If you do, you may wonder whether they are a sign of a significant health problem. You may also wonder whether you should have them treated, and if so, what treatments are available. As is usually the case, when it comes to your health, knowledge is power.
Varicose veins are veins that have become enlarged and twisted, because their valves have become ineffective (see Figure 14.4.11). As a result, blood pools in the veins and stretches them out. Varicose veins occur most frequently in the superficial veins of the legs, but they may also occur in other parts of the body. They are most common in older adults, females, and people who have a family history of the condition. Obesity and pregnancy also increase the risk of developing varicose veins. A job that requires standing for long periods of time, chronic constipation, and long-term alcohol consumption are additional risk factors.
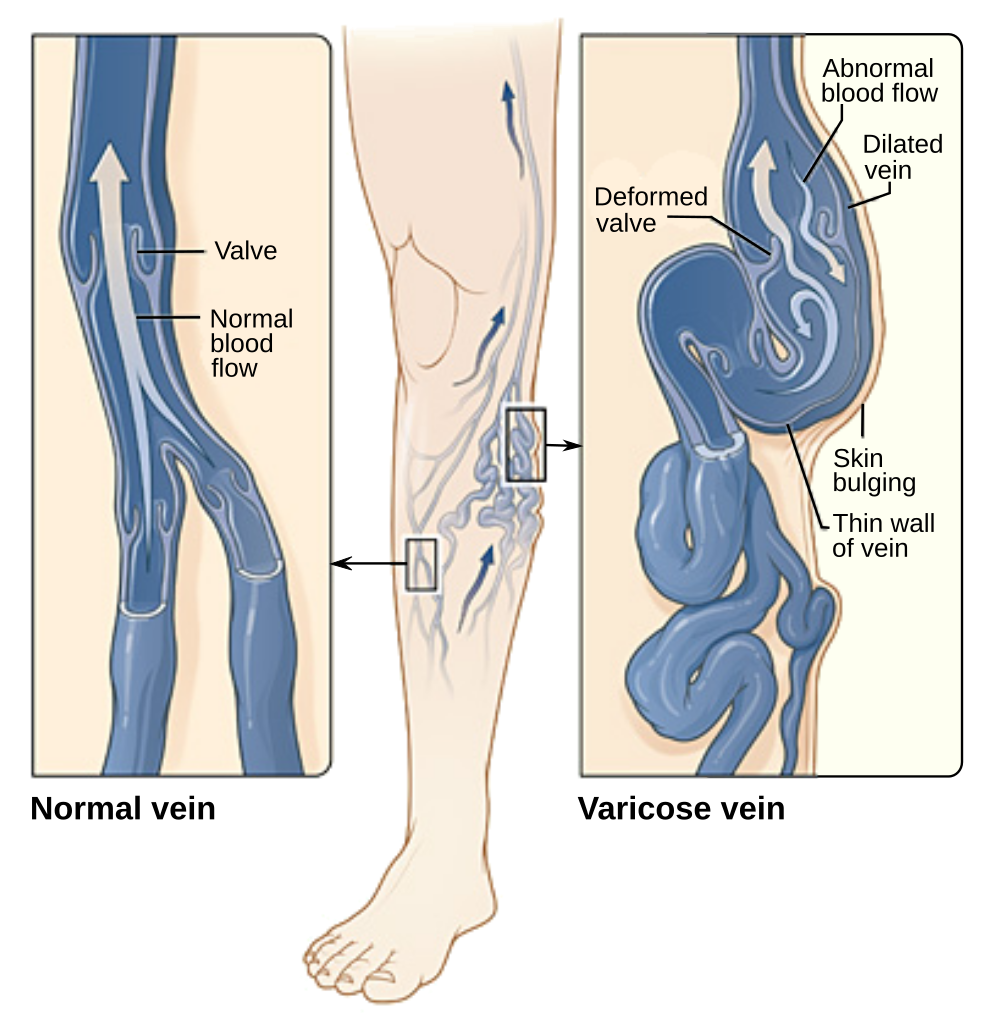
Varicose veins usually are not serious. For many people, they are only a cosmetic issue. In severe cases, however, varicose veins may cause pain and other problems. The affected leg(s) may feel heavy and achy, especially after long periods of standing. Ankles may become swollen by the end of the day. Minor injuries may bleed more than normal. The skin over the varicosity may become red, dry, and itchy. In very severe cases, skin ulcers may develop.
If you are concerned about varicose veins, call them to the attention of your doctor, who can determine the best course of action for your case. There are many potential treatments for varicose veins. Some of the treatments have potential adverse side effects, and with many of the treatments, varicose veins may return. The best treatment for a given patient depends in part on the severity of the condition.
- If varicose veins are not serious, conservative treatment options may be recommended. These include avoiding standing or sitting for long periods, frequently elevating the legs, and wearing graduated compression stockings.
- For more serious cases, less conservative, but non-surgical options may be advised. These include sclerotherapy, in which medicine is injected into the veins to make them shrink. Another non-surgical approach is endovenous thermal ablation. In this type of treatment, laser light, radio-frequency energy, or steam is used to heat the walls of the veins, causing them to shrink and collapse.
- For the most serious cases, surgery may be the best option. The most invasive surgery is vein stripping, in which all or part of the main trunk of a vein is tied off and removed from the leg while the patient is under general anesthesia. In a less invasive surgery, called ambulatory phlebectomy, short segments of a vein are removed through tiny incisions under local anesthesia.
14.4 Summary
- Blood vessels are the part of the cardiovascular system that carries blood throughout the human body. They are long, hollow,tube-like structures. There are three major types of blood vessels: arteries, veins, and capillaries.
- Arteries are blood vessels that carry blood away from the heart. Most arteries carry oxygenated blood. The largest artery is the aorta, which is connected to the heart and extends into the abdomen. Blood moves through arteries due to pressure from the beating of the heart.
- Veins are blood vessels that carry blood toward the heart. Most veins carry deoxygenated blood. The largest veins are the superior vena cava and inferior vena cava. Blood moves through veins by the squeezing action of surrounding skeletal muscles. Valves in veins prevent backflow of blood.
- Capillaries are the smallest blood vessels. They connect arterioles and venules. They form capillary beds, where substances are exchanged between the blood and surrounding tissues.
- The walls of arteries and veins have three layers. The middle layer is thickest in arteries, in which it contains smooth muscle tissue that controls the diameter of the vessels. The outer layer is thickest in veins, and consists mainly of connective tissue. The walls of capillaries consist of little more than a single layer of epithelial cells.
- Blood pressure is a measure of the force that blood exerts on the walls of arteries. It is expressed as a double number, with the higher number representing systolic pressure when the ventricles contract, and the lower number representing diastolic pressure when the ventricles relax. Normal blood pressure is generally defined as a pressure of less than 120/80 mm Hg.
- Vasoconstriction (narrowing) and vasodilation (widening) of arteries can occur to help regulate blood pressure or body temperature, or change blood flow as part of the fight-or-flight response.
14.4 Review Questions
- What are blood vessels? Name the three major types of blood vessels.
-
- Compare and contrast how blood moves through arteries and veins.
- What are capillaries, and what is their function?
- Does the blood in most veins have any oxygen at all? Explain your answer.
- Explain why it is important that the walls of capillaries are very thin.
14.4 Explore More
https://youtu.be/Ab9OZsDECZw
How blood pressure works - Wilfred Manzano, TED-Ed, 2015.
https://www.youtube.com/watch?v=9Wf8bLXVwFI
What are Varicose Veins? Cleveland Clinic, 2019.
https://www.youtube.com/watch?v=hnjMdXSyA5o
Arteries vs Veins ( Circulatory System ), MooMooMath and Science, 2018.
Attributions
Figure 14.4.1
bodybuilding_PNG24 from pngimg.com is used under a CC BY-NC 4.0 (https://creativecommons.org/licenses/by-nc/4.0/) license.
Figure 14.4.2
Arterial_System_en.svg by Mariana Ruiz Villarreal [LadyofHats] on Wikimedia Commons is in the public domain (https://en.wikipedia.org/wiki/Public_domain).
Figure 14.4.3
Skeletal_Muscle_Vein_Pump by OpenStax College on Wikimedia Commons is used under a CC BY 3.0 (https://creativecommons.org/licenses/by/3.0) license.
Figure 14.4.4
Venous_valve_00013 by Nevit Dilmen on Wikimedia Commons is used under a CC BY-SA 3.0 (https://creativecommons.org/licenses/by-sa/3.0) license.
Figure 14.4.5
Superior and Inferior Vena Cava by ArtFavor (acquired from OCAL) from Freestockphotos.biz, is used under a CC0 1.0 Universal public domain dedication license (https://creativecommons.org/publicdomain/zero/1.0/). Work adapted by Christine Miller.
Figure 14.4.6
Venous_system_en.svg by Mariana Ruiz Villarreal [LadyofHats] on Wikimedia Commons is in the public domain (https://en.wikipedia.org/wiki/Public_domain).
Figure 14.4.7
1024px-2105_Capillary_Bed by OpenStax College on Wikimedia Commons is used under a CC BY 3.0 (https://creativecommons.org/licenses/by/3.0) license.
Figure 14.4.8
Artery by Lord of Konrad on Wikimedia Commons is used under a CC0 1.0 Universal public domain dedication license (https://creativecommons.org/publicdomain/zero/1.0/).
Figure 14.4.9
Blausen_0055_ArteryWallStructure by BruceBlaus on Wikimedia Commons is used under a CC BY 3.0 (https://creativecommons.org/licenses/by/3.0) license.
Figure 14.4.10
Artery Vein Capillary Comparison by Christinelmiller on Wikimedia Commons is used under a CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0) license.
Figure 14.4.11
Varicose-veins by Jackerhack at English Wikipedia on Wikimedia Commons is used under a CC BY-SA 2.5 (https://creativecommons.org/licenses/by-sa/2.5) license.
Figure 14.4.12
Varicose_veins-en.svg by Jmarchn on Wikimedia Commons is used under a CC BY-SA 3.0 (https://creativecommons.org/licenses/by-sa/3.0) license. [Work modified from Varicose veins.jpg on Wikimedia Commons from National Heart Lung and Blood Institute (NIH)]
References
Betts, J. G., Young, K.A., Wise, J.A., Johnson, E., Poe, B., Kruse, D.H., Korol, O., Johnson, J.E., Womble, M., DeSaix, P. (2013, June 19). Figure 20.6 Capillary bed [digital image]. In Anatomy and Physiology (Section 20.1). OpenStax. https://openstax.org/books/anatomy-and-physiology/pages/20-1-structure-and-function-of-blood-vessels
Betts, J. G., Young, K.A., Wise, J.A., Johnson, E., Poe, B., Kruse, D.H., Korol, O., Johnson, J.E., Womble, M., DeSaix, P. (2013, June 19). Figure 20.15 Skeletal muscle pump [digital image]. In Anatomy and Physiology (Section 20.2). OpenStax. https://openstax.org/books/anatomy-and-physiology/pages/20-2-blood-flow-blood-pressure-and-resistance
Blausen.com Staff. (2014). Medical gallery of Blausen Medical 2014. WikiJournal of Medicine 1 (2). DOI:10.15347/wjm/2014.010. ISSN 2002-4436.
Cleveland Clinic. (2019, December 30). What are varicose veins? YouTube. https://www.youtube.com/watch?v=9Wf8bLXVwFI&feature=youtu.be
MooMooMath and Science. (2018, April 5). Arteries vs veins ( Circulatory System ). YouTube. https://www.youtube.com/watch?v=hnjMdXSyA5o&feature=youtu.be
TED-Ed. (2015, July 23). How blood pressure works - Wilfred Manzano. YouTube. https://www.youtube.com/watch?v=Ab9OZsDECZw&feature=youtu.be
Created by CK-12 Foundation/Adapted by Christine Miller

Vampires
From Bram Stoker’s famous novel about Count Dracula, to films such as Van Helsing and the Twilight Saga, fantasies featuring vampires (like the one in Figure 14.5.1) have been popular for decades. Vampires, in fact, are found in centuries-old myths from many cultures. In such myths, vampires are generally described as creatures that drink blood — preferably of the human variety — for sustenance. Dracula, for example, is based on Eastern European folklore about a human who attains immortality (and eternal damnation) by drinking the blood of others.
What Is Blood?
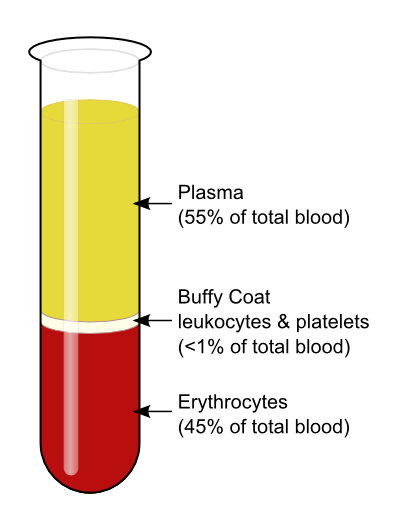
The average adult body contains between 4.7 and 5.7 litres of blood. More than half of that amount is fluid. Most of the rest of that amount consists of blood cells. The relative amounts of the various components in blood are illustrated in Figure 14.5.2. The components are also described in detail below.
Blood is a fluid connective tissue that circulates throughout the body through blood vessels of the cardiovascular system. What makes blood so special that it features in widespread myths? Although blood accounts for less than 10% of human body weight, it is quite literally the elixir of life. As blood travels through the vessels of the cardiovascular system, it delivers vital substances (such as nutrients and oxygen) to all of the cells, and carries away their metabolic wastes. It is no exaggeration to say that without blood, cells could not survive. Indeed, without the oxygen carried in blood, cells of the brain start to die within a matter of minutes.
Functions of Blood
Blood performs many important functions in the body. Major functions of blood include:
- Supplying tissues with oxygen, which is needed by all cells for aerobic cellular respiration.
- Supplying cells with nutrients, including glucose, amino acids, and fatty acids.
- Removing metabolic wastes from cells, including carbon dioxide, urea, and lactic acid.
- Helping to defend the body from pathogens and other foreign substances.
- Forming clots to seal broken blood vessels and stop bleeding.
- Transporting hormones and other messenger molecules.
- Regulating the pH of the body, which must be kept within a narrow range (7.35 to 7.45).
- Helping regulate body temperature (through vasoconstriction and vasodilation).
Blood Plasma
Plasma is the liquid component of human blood. It makes up about 55% of blood by volume. It is about 92% water, and contains many dissolved substances. Most of these substances are proteins, but plasma also contains trace amounts of glucose, mineral ions, hormones, carbon dioxide, and other substances. In addition, plasma contains blood cells. When the cells are removed from plasma, as in Figure 14.5.2 above, the remaining liquid is clear but yellow in colour.
Blood Cells
The cells in blood include erythrocytes, leukocytes, and thrombocytes. These different types of blood cells are shown in the photomicrograph (Figure 14.5.3) and described in the sections that follow.
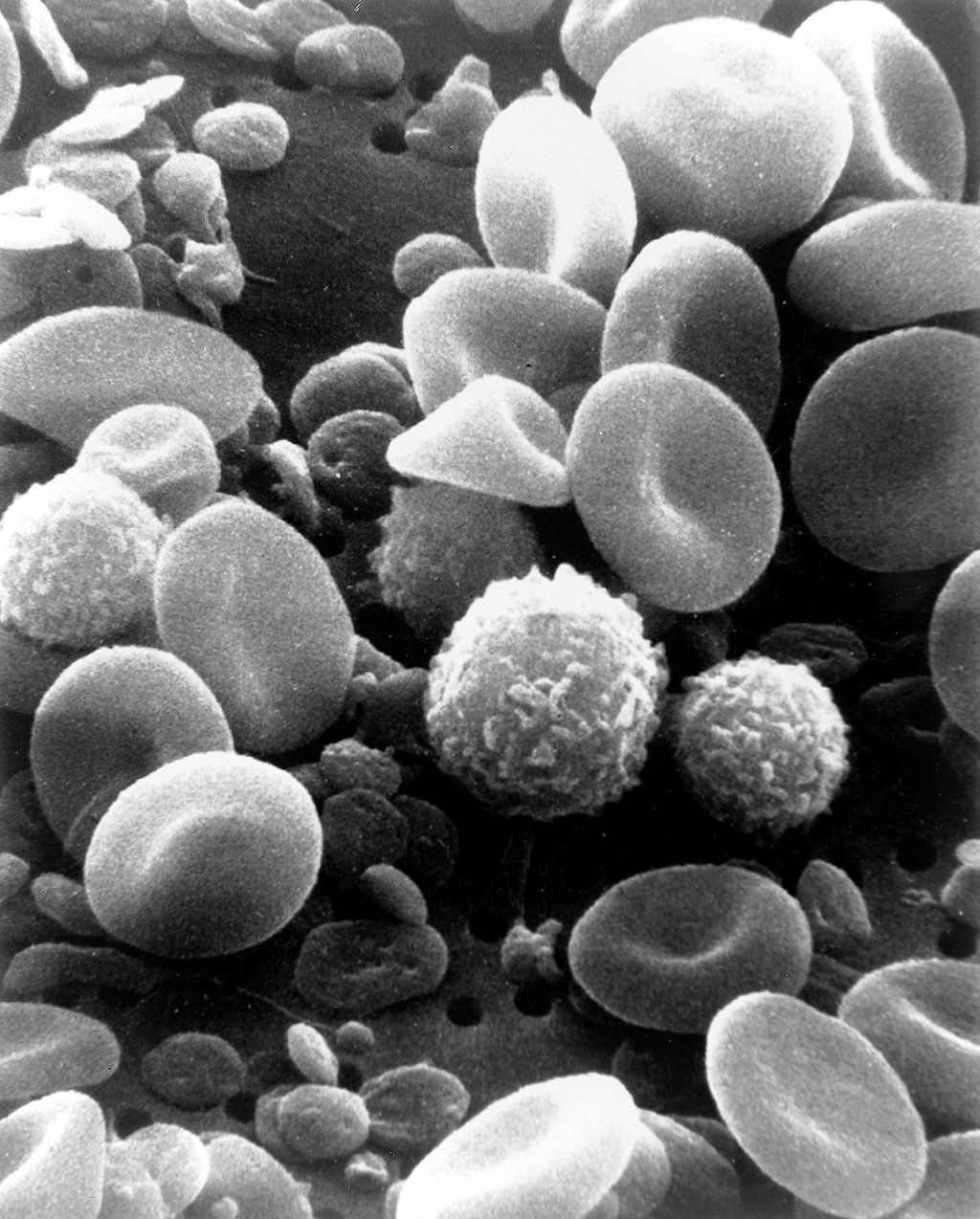
Erythrocytes
The most numerous cells in blood are red blood cells, also called erythrocytes. One microlitre of blood contains between 4.2 and 6.1 million red blood cells, and red blood cells make up about 25% of all the cells in the human body. The cytoplasm of a mature erythrocyte is almost completely filled with hemoglobin, the iron-containing protein that binds with oxygen and gives the cell its red colour. In order to provide maximum space for hemoglobin, mature erythrocytes lack a cell nucleus and most organelles. They are little more than sacks of hemoglobin.
Erythrocytes also carry proteins called antigens that determine blood type. Blood type is a genetic characteristic. The best known human blood type systems are the ABO and Rhesus systems.
- In the ABO system, there are two common antigens, called antigen A and antigen B. There are four ABO blood types, A (only A antigen), B (only B antigen), AB (both A and B antigens), and O (neither A nor B antigen). The ABO antigens are illustrated in Figure 14.5.4.
- In the Rhesus system, there is just one common antigen. A person may either have the antigen (Rh+) or lack the antigen (Rh-).
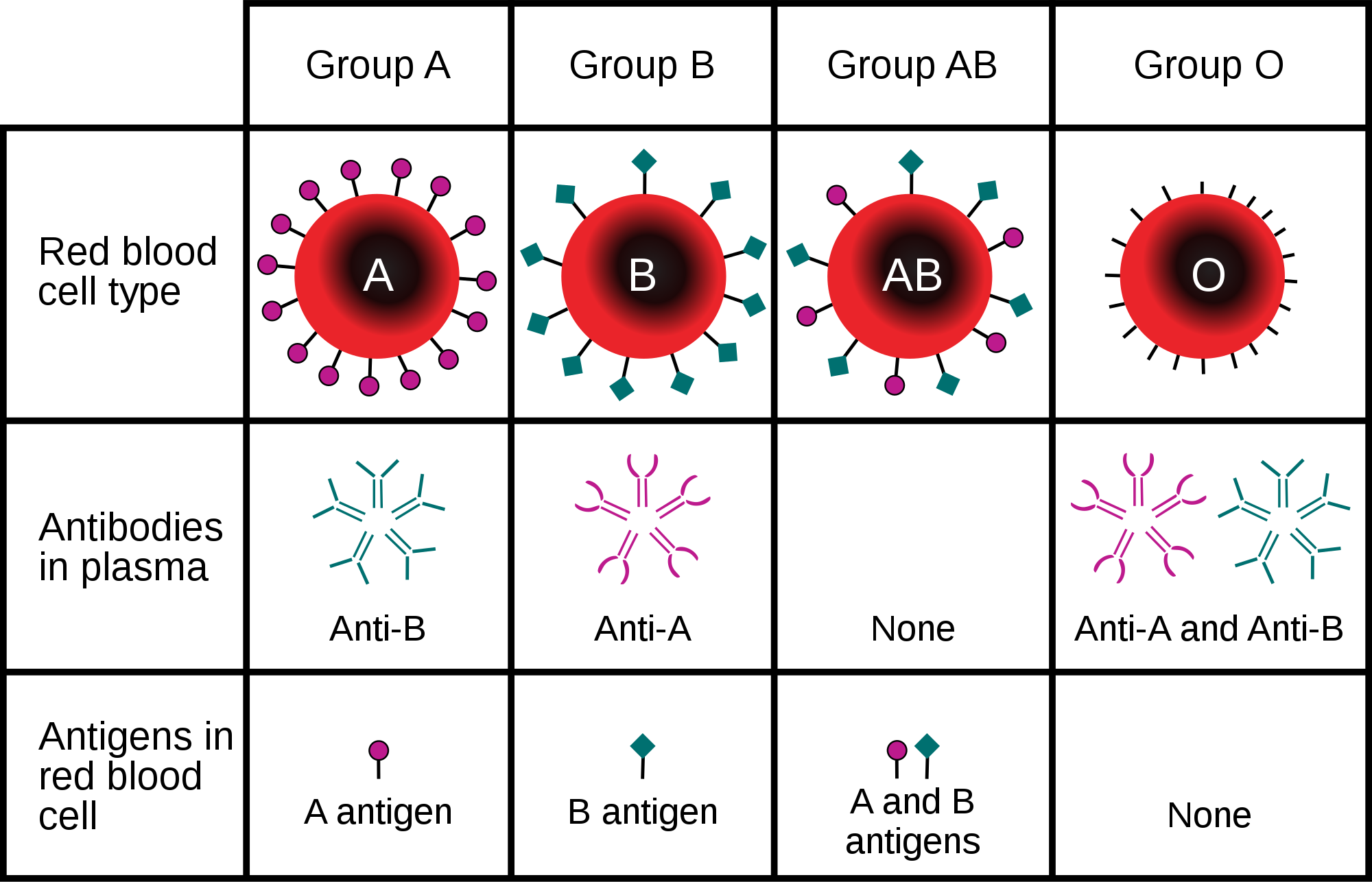
Blood type is important for medical reasons. A person who needs a blood transfusion must receive blood of a compatible type. Blood that is compatible lacks antigens that the patient's own blood also lacks. For example, for a person with type A blood (no B antigen), compatible types include any type of blood that lacks the B antigen. This would include type A blood or type O blood, but not type AB or type B blood. If incompatible blood is transfused, it may cause a potentially life-threatening reaction in the patient’s blood.
Leukocytes
Leukocytes (also called white blood cells) are cells in blood that defend the body against invading microorganisms and other threats. There are far fewer leukocytes than red blood cells in blood. There are normally only about 1,000 to 11,000 white blood cells per microlitre of blood. Unlike erythrocytes, leukocytes have a nucleus. White blood cells are part of the body’s immune system. They destroy and remove old or abnormal cells and cellular debris, as well as attack pathogens and foreign substances. There are five main types of white blood cells, which are described in Table 14.5.1: neutrophils, eosinophils, basophils, lymphocytes, and monocytes. The five types differ in their specific immune functions.
| Type of Leukocyte | Per cent of All Leukocytes | Main Function(s) |
|---|---|---|
| Neutrophil | 62% | Phagocytize (engulf and destroy) bacteria and fungi in blood. |
| Eosinophil | 2% | Attack and kill large parasites; carry out allergic responses. |
| Basophil | less than 1% | Release histamines in inflammatory responses. |
| Lymphocyte | 30% | Attack and destroy virus-infected and tumor cells; create lasting immunity to specific pathogens. |
| Monocyte | 5% | Phagocytize pathogens and debris in tissues. |
Thrombocytes
Thrombocytes, also called platelets, are actually cell fragments. Like erythrocytes, they lack a nucleus and are more numerous than white blood cells. There are about 150 thousand to 400 thousand thrombocytes per microlitre of blood.
The main function of thrombocytes is blood clotting, or coagulation. This is the process by which blood changes from a liquid to a gel, forming a plug in a damaged blood vessel. If blood clotting is successful, it results in hemostasis, which is the cessation of blood loss from the damaged vessel. A blood clot consists of both platelets and proteins, especially the protein fibrin. You can see a scanning electron microscope photomicrograph of a blood clot in Figure 14.5.5.
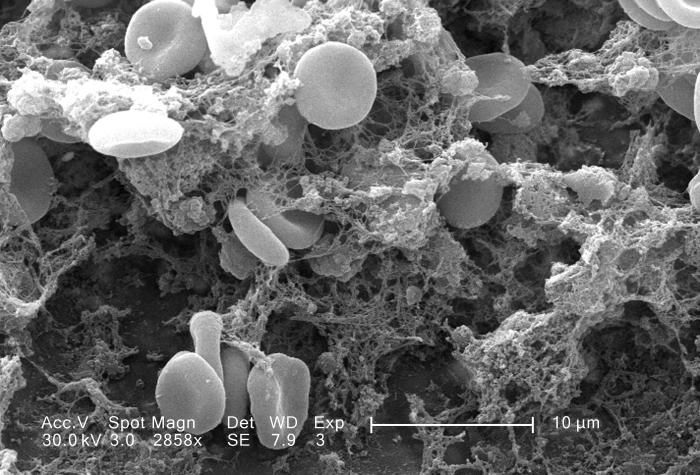
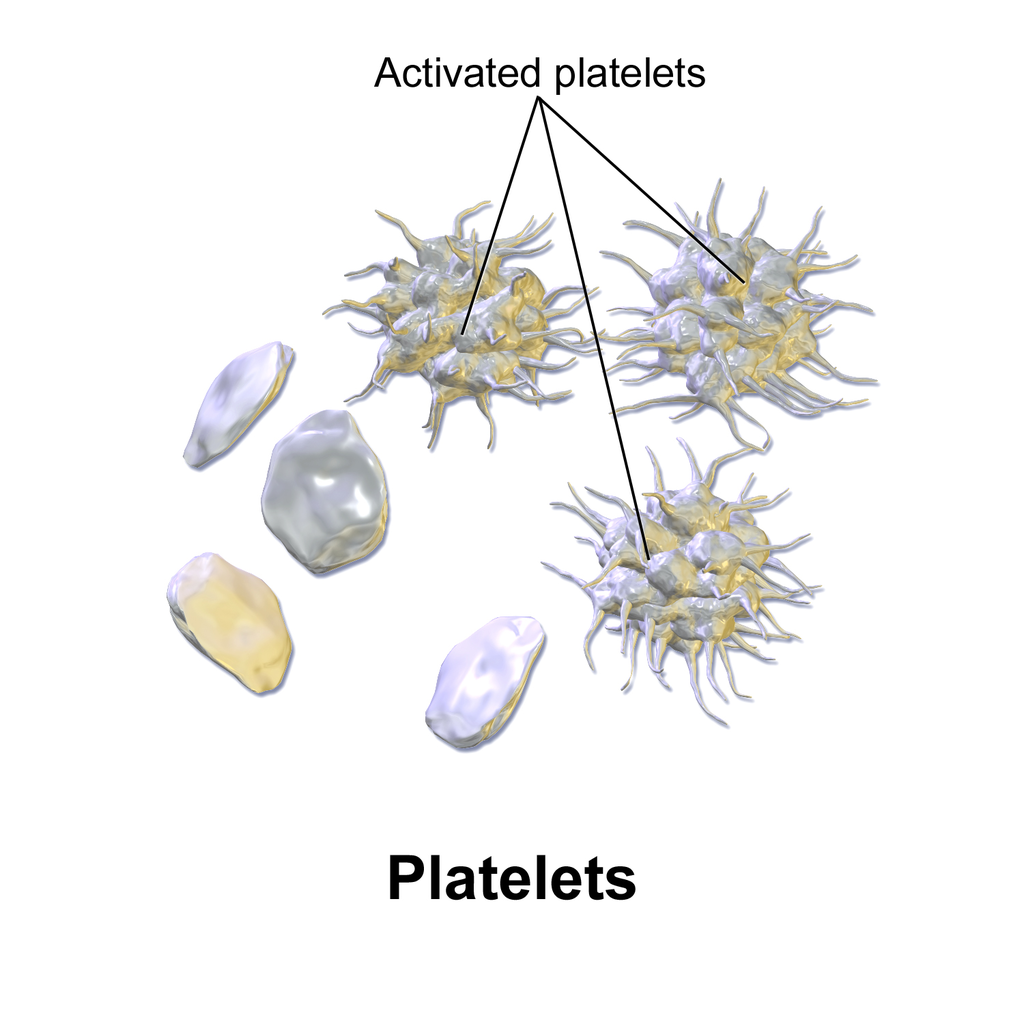
Coagulation begins almost instantly after an injury occurs to the endothelium of a blood vessel. Thrombocytes become activated and change their shape from spherical to star-shaped, as shown in Figure 14.5.6. This helps them aggregate with one another (stick together) at the site of injury to start forming a plug in the vessel wall. Activated thrombocytes also release substances into the blood that activate additional thrombocytes and start a sequence of reactions leading to fibrin formation. Strands of fibrin crisscross the platelet plug and strengthen it, much as rebar strengthens concrete.
Formation and Degradation of Blood Cells
Blood is considered a connective tissue, because blood cells form inside bones. All three types of blood cells are made in red marrow within the medullary cavity of bones in a process called hematopoiesis. Formation of blood cells occurs by the proliferation of stem cells in the marrow. These stem cells are self-renewing — when they divide, some of the daughter cells remain stem cells, so the pool of stem cells is not used up. Other daughter cells follow various pathways to differentiate into the variety of blood cell types. Once the cells have differentiated, they cannot divide to form copies of themselves.
Eventually, blood cells die and must be replaced through the formation of new blood cells from proliferating stem cells. After blood cells die, the dead cells are phagocytized (engulfed and destroyed) by white blood cells, and removed from the circulation. This process most often takes place in the spleen and liver.
Blood Disorders
Many human disorders primarily affect the blood. They include cancers, genetic disorders, poisoning by toxins, infections, and nutritional deficiencies.
- Leukemia is a group of cancers of the blood-forming tissues in the bone marrow. It is the most common type of cancer in children, although most cases occur in adults. Leukemia is generally characterized by large numbers of abnormal leukocytes. Symptoms may include excessive bleeding and bruising, fatigue, fever, and an increased risk of infections. Leukemia is thought to be caused by a combination of genetic and environmental factors.
- Hemophilia refers to any of several genetic disorders that cause dysfunction in the blood clotting process. People with hemophilia are prone to potentially uncontrollable bleeding, even with otherwise inconsequential injuries. They also commonly suffer bleeding into the spaces between joints, which can cause crippling.
- Carbon monoxide poisoning occurs when inhaled carbon monoxide (in fumes from a faulty home furnace or car exhaust, for example) binds irreversibly to the hemoglobin in erythrocytes. As a result, oxygen cannot bind to the red blood cells for transport throughout the body, and this can quickly lead to suffocation. Carbon monoxide is extremely dangerous, because it is colourless and odorless, so it cannot be detected in the air by human senses.
- HIV is a virus that infects certain types of leukocytes and interferes with the body’s ability to defend itself from pathogens and other causes of illness. HIV infection may eventually lead to AIDS (acquired immunodeficiency syndrome). AIDS is characterized by rare infections and cancers that people with a healthy immune system almost never acquire.
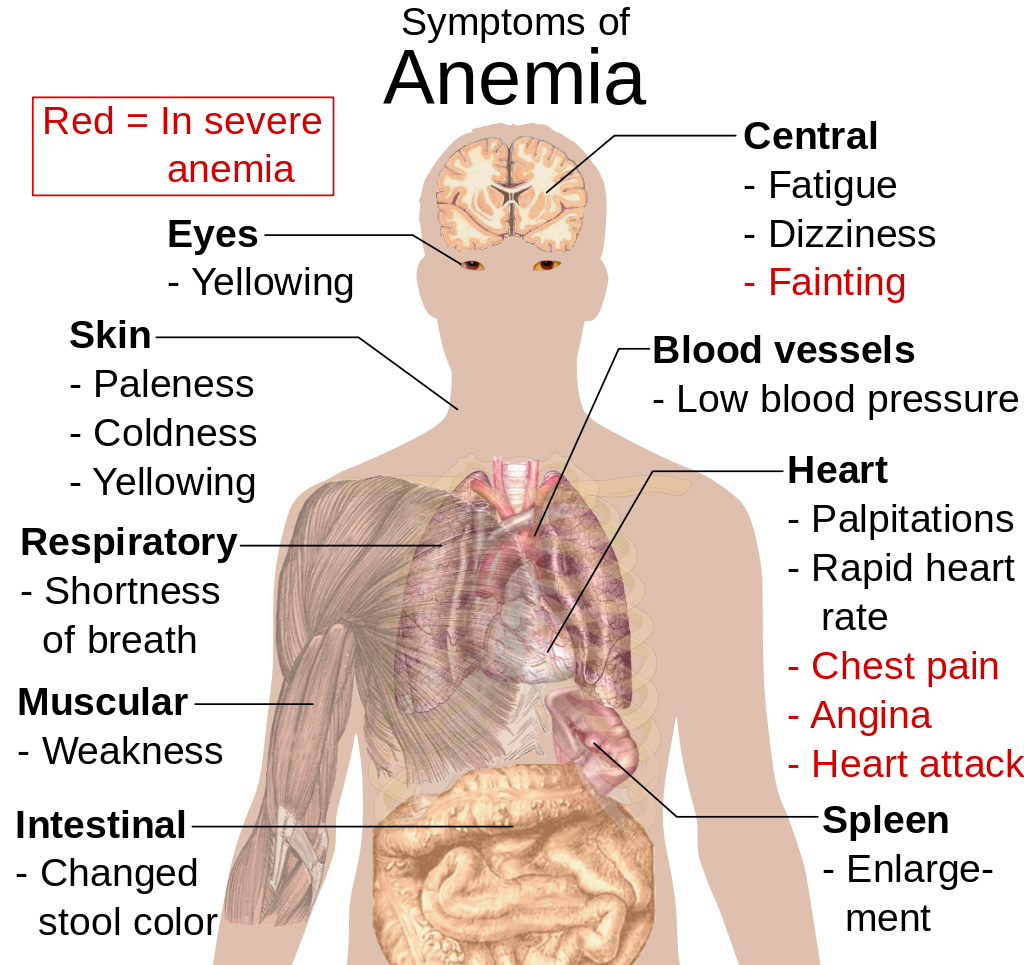
- Anemia is a disorder in which the blood has an inadequate volume of erythrocytes, reducing the amount of oxygen that the blood can carry, and potentially causing weakness and fatigue. These and other signs and symptoms of anemia are shown in Figure 14.5.8. Anemia has many possible causes, including excessive bleeding, inherited disorders (such as sickle cell hemoglobin), or nutritional deficiencies (iron, folate, or B12). Severe anemia may require transfusions of donated blood.
Feature: Myth vs. Reality
Donating blood saves lives. In fact, with each blood donation, as many as three lives may be saved. According to Government Canada, up to 52% of Canadians have reported that they or a family member have needed blood or blood products at some point in their lifetime. Many donors agree that the feeling that comes from knowing you have saved lives is well worth the short amount of time it takes to make a blood donation. Nonetheless, only a minority of potential donors actually donate blood. There are many myths about blood donation that may help explain the small percentage of donors. Knowing the facts may reaffirm your decision to donate if you are already a donor — and if you aren’t a donor already, getting the facts may help you decide to become one.
| Myth | Reality |
|---|---|
| "Your blood might become contaminated with an infection during the donation." | There is no risk of contamination because only single-use, disposable catheters, tubing, and other equipment are used to collect blood for a donation. |
| "You are too old (or too young) to donate blood." | There is no upper age limit on donating blood, as long as you are healthy. The minimum age is 16 years. |
| "You can’t donate blood if you have high blood pressure." | As long as your blood pressure is below 180/100 at the time of donation, you can give blood. Even if you take blood pressure medication to keep your blood pressure below this level, you can donate. |
| "You can’t give blood if you have high cholesterol." | Having high cholesterol does not affect your ability to donate blood. Taking cholesterol-lowering medication also does not disqualify you. |
| "You can’t donate blood if you have had a flu shot." | Having a flu shot has no effect on your ability to donate blood. You can even donate on the same day that you receive a flu shot. |
| "You can’t donate blood if you take medication." | As long as you are healthy, in most cases, taking medication does not preclude you from donating blood. |
| "Your blood isn’t needed if it’s a common blood type." | All types of blood are in constant demand. |
14.5 Summary
- Blood is a fluid connective tissue that circulates throughout the body in the cardiovascular system. Blood supplies tissues with oxygen and nutrients and removes their metabolic wastes. Blood helps defend the body from pathogens and other threats, transports hormones and other substances, and helps keep the body’s pH and temperature in homeostasis.
- Plasma is the liquid component of blood, and it makes up more than half of blood by volume. It consists of water and many dissolved substances. It also contains blood cells, including erythrocytes, leukocytes and thrombocytes.
- Erythrocytes, (also known as red blood cells) are the most numerous cells in blood. They consist mostly of hemoglobin, which carries oxygen. Erythrocytes also carry antigens that determine blood type.
- Leukocytes (also referred to as white blood cells) are less numerous than erythrocytes and are part of the body’s immune system. There are several different types of leukocytes that differ in their specific immune functions. They protect the body from abnormal cells, microorganisms, and other harmful substances.
- Thrombocytes (also called platelets) are cell fragments that play important roles in blood clotting, or coagulation. They stick together at breaks in blood vessels to form a clot and stimulate the production of fibrin, which strengthens the clot.
- All blood cells form by proliferation of stem cells in red bone marrow in a process called hematopoiesis. When blood cells die, they are phagocytized by leukocytes and removed from the circulation.
- Disorders of the blood include leukemia, which is cancer of the bone-forming cells; hemophilia, which is any of several genetic blood-clotting disorders; carbon monoxide poisoning, which prevents erythrocytes from binding with oxygen and causes suffocation; HIV infection, which destroys certain types of leukocytes and can cause AIDS; and anemia, in which there are not enough erythrocytes to carry adequate oxygen to body tissues.
14.5 Review Questions
- What is blood? Why is blood considered a connective tissue?
- Identify four physiological roles of blood in the body.
- Describe plasma and its components.
-
14.5 Explore More
https://youtu.be/e-5wqwp64MM
Joe Landolina: This gel can make you stop bleeding instantly, TED, 2014.
https://youtu.be/hgp8LtwFSBA
Can Synthetic Blood Help The World's Blood Shortage? Science Plus, 2016.
https://youtu.be/1Qfmkd6C8u8
How bones make blood - Melody Smith, TED-Ed, 2020.
Attributions
Figure 14.5.1
vampire_PNG32 from pngimg.com is used under a CC BY-NC 4.0 (https://creativecommons.org/licenses/by-nc/4.0/) license.
Figure 14.5.2
Blood-centrifugation-scheme by KnuteKnudsen at English Wikipedia on Wikimedia Commons is used under a CC BY 3.0 (https://creativecommons.org/licenses/by/3.0) license.
Figure 14.5.3
SEM_blood_cells by Bruce Wetzel and Harry Schaefer (Photographers)/ NCI AV-8202-3656 on Wikimedia Commons is in the public domain (https://en.wikipedia.org/wiki/en:Public_domain).
Figure 14.5.4
ABO_blood_type.svg by InvictaHOG on Wikimedia Commons is in the public domain (https://en.wikipedia.org/wiki/en:Public_domain).
Figure 14.5.5
Blood_clot_in_scanning_electron_microscopy by Janice Carr from CDC/ Public Health Image LIbrary (PHIL) ID #7308 on Wikimedia Commons is in the public domain (https://en.wikipedia.org/wiki/en:Public_domain).
Figure 14.5.6
Blausen_0740_Platelets by BruceBlaus on Wikimedia Commons is used under a CC BY 3.0 (https://creativecommons.org/licenses/by/3.0) license.
Figure 14.5.7
Platelet_Party_900x by Awkward Yeti (used with permission of the author) © All Rights Reserved
Figure 14.5.8
Symptoms_of_anemia.svg by Mikael Häggström on Wikimedia Commons is in the public domain (https://en.wikipedia.org/wiki/en:public_domain).
References
Blausen.com Staff. (2014). Medical gallery of Blausen Medical 2014. WikiJournal of Medicine 1 (2). DOI:10.15347/wjm/2014.010. ISSN 2002-4436.
Blood, organ and tissue donation. (2020, April 28). Government of Canada. https://www.canada.ca/en/public-health/services/healthy-living/blood-organ-tissue-donation.html#a3
Canadian Blood Services. (n.d.). There is an immediate need for blood as demand is rising. https://www.blood.ca
Science Plus. (2016, March 2). Can synthetic blood help the world's blood shortage? https://www.youtube.com/watch?v=hgp8LtwFSBA&feature=youtu.be
TED. (2014, November 20). Joe Landolina: This gel can make you stop bleeding instantly. YouTube. https://www.youtube.com/watch?v=e-5wqwp64MM&feature=youtu.be
TED-Ed. (2020, January 27). How bones make blood - Melody Smith. YouTube. https://www.youtube.com/watch?v=1Qfmkd6C8u8&feature=youtu.be
Created by CK-12 Foundation/Adapted by Christine Miller

Worm Attack!
Does the organism in Figure 17.2.1 look like a space alien? A scary creature from a nightmare? In fact, it’s a 1-cm long worm in the genus Schistosoma. It may invade and take up residence in the human body, causing a very serious illness known as schistosomiasis. The worm gains access to the human body while it is in a microscopic life stage. It enters through a hair follicle when the skin comes into contact with contaminated water. The worm then grows and matures inside the human organism, causing disease.
Host vs. Pathogen
The Schistosoma worm has a parasitic relationship with humans. In this type of relationship, one organism, called the parasite, lives on or in another organism, called the host. The parasite always benefits from the relationship, and the host is always harmed. The human host of the Schistosoma worm is clearly harmed by the parasite when it invades the host’s tissues. The urinary tract or intestines may be infected, and signs and symptoms may include abdominal pain, diarrhea, bloody stool, or blood in the urine. Those who have been infected for a long time may experience liver damage, kidney failure, infertility, or bladder cancer. In children, Schistosoma infection may cause poor growth and difficulty learning.
Like the Schistosoma worm, many other organisms can make us sick if they manage to enter our body. Any such agent that can cause disease is called a pathogen. Most pathogens are microorganisms, although some — such as the Schistosoma worm — are much larger. In addition to worms, common types of pathogens of human hosts include bacteria, viruses, fungi, and single-celled organisms called protists. You can see examples of each of these types of pathogens in Table 17.1.1. Fortunately for us, our immune system is able to keep most potential pathogens out of the body, or quickly destroy them if they do manage to get in. When you read this chapter, you’ll learn how your immune system usually keeps you safe from harm — including from scary creatures like the Schistosoma worm!
| Type of Pathogen | Description | Disease Caused | |
|---|---|---|---|
| Bacteria:
Example shown: Escherichia coli |
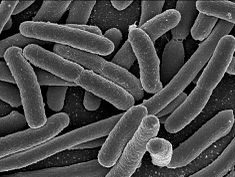 |
Single celled organisms without a nucleus | Strep throat, staph infections, tuberculosis, food poisoning, tetanus, pneumonia, syphillis |
| Viruses:
Example shown: Herpes simplex |
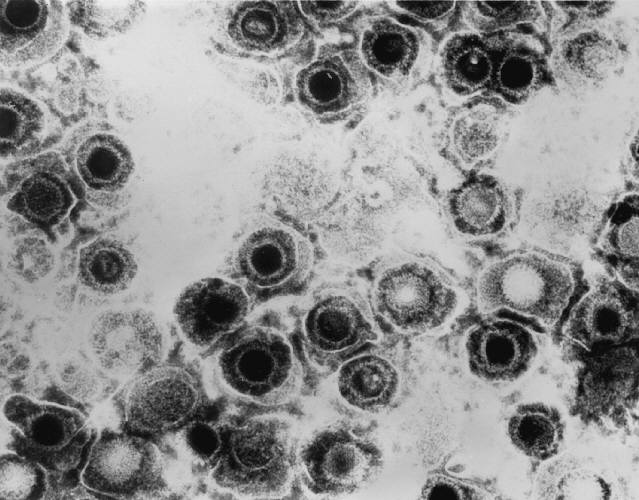 |
Non-living particles that reproduce by taking over living cells | Common cold, flu, genital herpes, cold sores, measles, AIDS, genital warts, chicken pox, small pox |
| Fungi:
Example shown: Death cap mushroom |
 |
Simple organisms, including mushrooms and yeast, that grow as single cells or thread-like filaments | Ringworm, athletes foot, tineas, candidias, histoplasmomis, mushroom poisoning |
| Protozoa:
Example shown: Giardia lamblia |
 |
Single celled organisms with a nucleus | Malaria, "traveller's diarrhea", giardiasis, typano somiasis ("sleeping sickness") |
What is the Immune System?
The immune system is a host defense system. It comprises many biological structures —ranging from individual leukocytes to entire organs — as well as many complex biological processes. The function of the immune system is to protect the host from pathogens and other causes of disease, such as tumor (cancer) cells. To function properly, the immune system must be able to detect a wide variety of pathogens. It also must be able to distinguish the cells of pathogens from the host’s own cells, and also to distinguish cancerous or damaged host cells from healthy cells. In humans and most other vertebrates, the immune system consists of layered defenses that have increasing specificity for particular pathogens or tumor cells. The layered defenses of the human immune system are usually classified into two subsystems, called the innate immune system and the adaptive immune system.
Innate Immune System
The innate immune system (sometimes referred to as "non-specific defense") provides very quick, but non-specific responses to pathogens. It responds the same way regardless of the type of pathogen that is attacking the host. It includes barriers — such as the skin and mucous membranes — that normally keep pathogens out of the body. It also includes general responses to pathogens that manage to breach these barriers, including chemicals and cells that attack the pathogens inside the human host. Certain leukocytes (white blood cells), for example, engulf and destroy pathogens they encounter in the process called phagocytosis, which is illustrated in Figure 17.2.2. Exposure to pathogens leads to an immediate maximal response from the innate immune system.
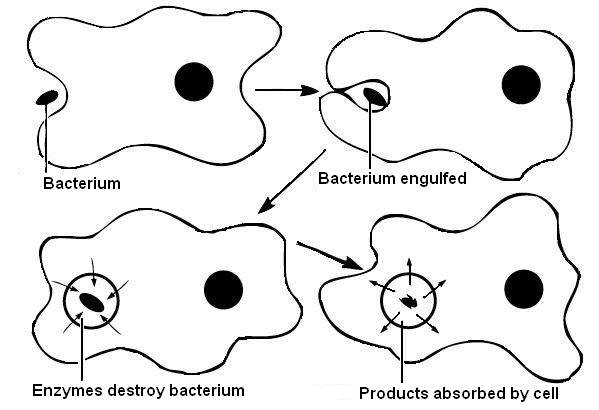
Watch the video below, "Neutrophil Phagocytosis - White Blood Cells Eats Staphylococcus Aureus Bacteria" by ImmiflexImmuneSystem, to see phagocytosis in action.
https://youtu.be/Z_mXDvZQ6dU
Neutrophil Phagocytosis - White Blood Cell Eats Staphylococcus Aureus Bacteria, ImmiflexImmuneSystem, 2013.
Adaptive Immune System
The adaptive immune system is activated if pathogens successfully enter the body and manage to evade the general defenses of the innate immune system. An adaptive response is specific to the particular type of pathogen that has invaded the body, or to cancerous cells. It takes longer to launch a specific attack, but once it is underway, its specificity makes it very effective. An adaptive response also usually leads to immunity. This is a state of resistance to a specific pathogen, due to the adaptive immune system's ability to “remember” the pathogen and immediately mount a strong attack tailored to that particular pathogen if it invades again in the future.
Self vs. Non-Self
Both innate and adaptive immune responses depend on the immune system's ability to distinguish between self- and non-self molecules. Self molecules are those components of an organism’s body that can be distinguished from foreign substances by the immune system. Virtually all body cells have surface proteins that are part of a complex called major histocompatibility complex (MHC). These proteins are one way the immune system recognizes body cells as self. Non-self proteins, in contrast, are recognized as foreign, because they are different from self proteins.
Antigens and Antibodies
Many non-self molecules comprise a class of compounds called antigens. Antigens, which are usually proteins, bind to specific receptors on immune system cells and elicit an adaptive immune response. Some adaptive immune system cells (B cells) respond to foreign antigens by producing antibodies. An antibody is a molecule that precisely matches and binds to a specific antigen. This may target the antigen (and the pathogen displaying it) for destruction by other immune cells.
Antigens on the surface of pathogens are how the adaptive immune system recognizes specific pathogens. Antigen specificity allows for the generation of responses tailored to the specific pathogen. It is also how the adaptive immune system ”remembers” the same pathogen in the future.
Immune Surveillance
Another important role of the immune system is to identify and eliminate tumor cells. This is called immune surveillance. The transformed cells of tumors express antigens that are not found on normal body cells. The main response of the immune system to tumor cells is to destroy them. This is carried out primarily by aptly-named killer T cells of the adaptive immune system.
Lymphatic System
The lymphatic system is a human organ system that is a vital part of the adaptive immune system. It is also part of the cardiovascular system and plays a major role in the digestive system (see section 17.3 Lymphatic System). The major structures of the lymphatic system are shown in Figure 17.2.3 .
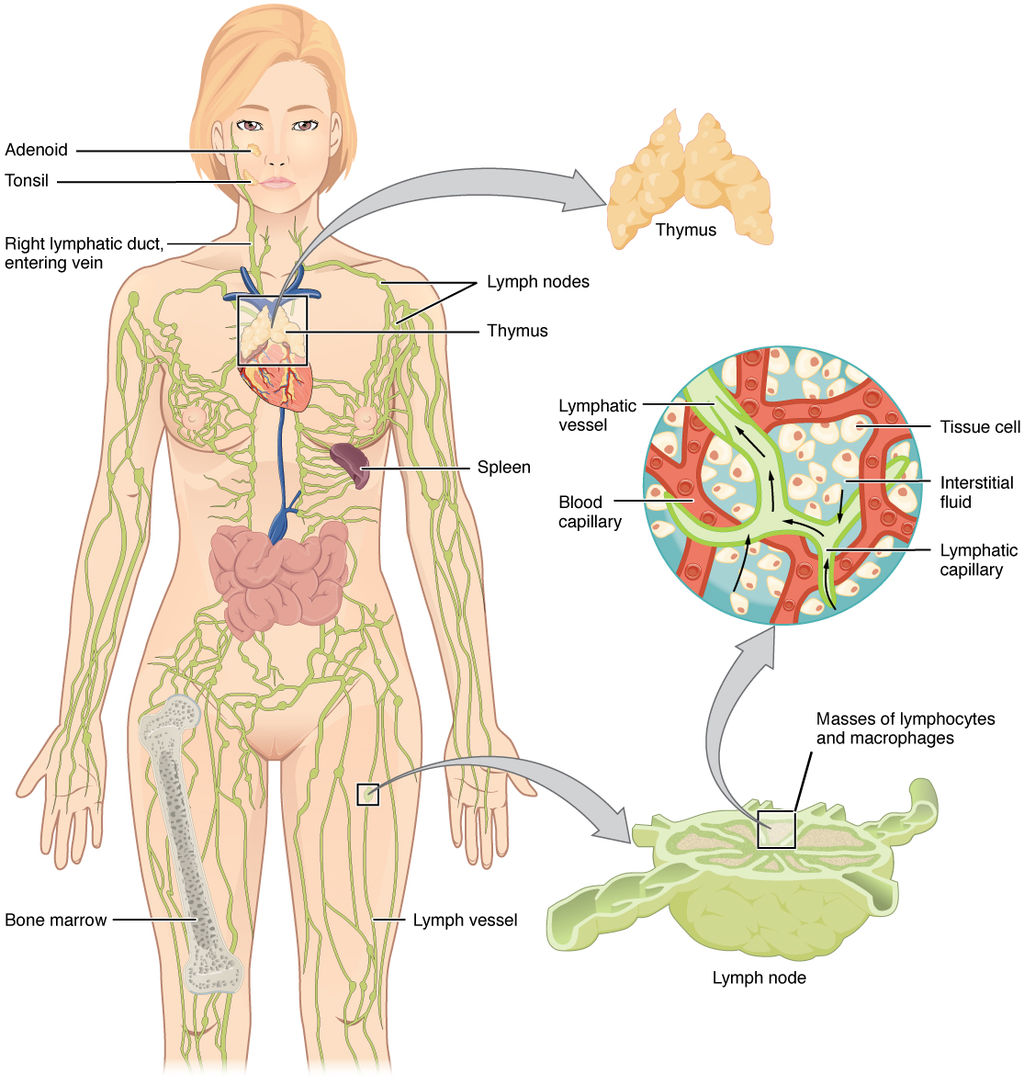
The lymphatic system consists of several lymphatic organs and a body-wide network of lymphatic vessels that transport the fluid called lymph. Lymph is essentially blood plasma that has leaked from capillaries into tissue spaces. It includes many leukocytes, especially lymphocytes, which are the major cells of the lymphatic system. Like other leukocytes, lymphocytes defend the body. There are several different types of lymphocytes that fight pathogens or cancer cells as part of the adaptive immune system.
Major lymphatic organs include the thymus and bone marrow. Their function is to form and/or mature lymphocytes. Other lymphatic organs include the spleen, tonsils, and lymph nodes, which are small clumps of lymphoid tissue clustered along lymphatic vessels. These other lymphatic organs harbor mature lymphocytes and filter lymph. They are sites where pathogens collect, and adaptive immune responses generally begin.
Neuroimmune System vs. Peripheral Immune System
The brain and spinal cord are normally protected from pathogens in the blood by the selectively permeable blood-brain and blood-spinal cord barriers. These barriers are part of the neuroimmune system. The neuroimmune system has traditionally been considered distinct from the rest of the immune system, which is called the peripheral immune system — although that view may be changing. Unlike the peripheral system, in which leukocytes are the main cells, the main cells of the neuroimmune system are thought to be nervous system cells called neuroglia. These cells can recognize and respond to pathogens, debris, and other potential dangers. Types of neuroglia involved in neuroimmune responses include microglial cells and astrocytes.
- Microglial cells are among the most prominent types of neuroglia in the brain. One of their main functions is to phagocytize cellular debris that remains when neurons die. Microglial cells also “prune” obsolete synapses between neurons.
- Astrocytes are neuroglia that have a different immune function. They allow certain immune cells from the peripheral immune system to cross into the brain via the blood-brain barrier to target both pathogens and damaged nervous tissue.
Feature: Human Biology in the News
“They’ll have to rewrite the textbooks!”
That sort of response to a scientific discovery is sure to attract media attention, and it did. It’s what Kevin Lee, a neuroscientist at the University of Virginia, said in 2016 when his colleagues told him they had discovered human anatomical structures that had never before been detected. The structures were tiny lymphatic vessels in the meningeal layers surrounding the brain.
How these lymphatic vessels could have gone unnoticed when all human body systems have been studied so completely is amazing in its own right. The suggested implications of the discovery are equally amazing:
- The presence of these lymphatic vessels means that the brain is directly connected to the peripheral immune system, presumably allowing a close association between the human brain and human pathogens. This suggests an entirely new avenue by which humans and their pathogens may have influenced each other’s evolution. The researchers speculate that our pathogens even may have influenced the evolution of our social behaviors.
- The researchers think there will also be many medical applications of their discovery. For example, the newly discovered lymphatic vessels may play a major role in neurological diseases that have an immune component, such as multiple sclerosis. The discovery might also affect how conditions such as autism spectrum disorders and schizophrenia are treated.
17.2 Summary
- Any agent that can cause disease is called a pathogen. Most human pathogens are microorganisms, such as bacteria and viruses. The immune system is the body system that defends the human host from pathogens and cancerous cells.
- The innate immune system is a subset of the immune system that provides very quick, but non-specific responses to pathogens. It includes multiple types of barriers to pathogens, leukocytes that phagocytize pathogens, and several other general responses.
- The adaptive immune system is a subset of the immune system that provides specific responses tailored to particular pathogens. It takes longer to put into effect, but it may lead to immunity to the pathogens.
- Both innate and adaptive immune responses depend on the immune system's ability to distinguish between self and non-self molecules. Most body cells have major histocompatibility complex (MHC) proteins that identify them as self. Pathogens and tumor cells have non-self antigens that the immune system recognizes as foreign.
- Antigens are proteins that bind to specific receptors on immune system cells and elicit an adaptive immune response. Generally, they are non-self molecules on pathogens or infected cells. Some immune cells (B cells) respond to foreign antigens by producing antibodies that bind with antigens and target pathogens for destruction.
- Tumor surveillance is an important role of the immune system. Killer T cells of the adaptive immune system find and destroy tumor cells, which they can identify from their abnormal antigens.
- The lymphatic system is a human organ system vital to the adaptive immune system. It consists of several organs and a system of vessels that transport lymph. The main immune function of the lymphatic system is to produce, mature, and circulate lymphocytes, which are the main cells in the adaptive immune system.
- The neuroimmune system that protects the central nervous system is thought to be distinct from the peripheral immune system that protects the rest of the human body. The blood-brain and blood-spinal cord barriers are one type of protection for the neuroimmune system. Neuroglia also play role in this system, for example, by carrying out phagocytosis.
17.2 Review Questions
-
- What is a pathogen?
- State the purpose of the immune system.
- Compare and contrast the innate and adaptive immune systems.
- Explain how the immune system distinguishes self molecules from non-self molecules.
- What are antigens?
- Define tumor surveillance.
- Briefly describe the lymphatic system and its role in immune function.
- Identify the neuroimmune system.
- What does it mean that the immune system is not just composed of organs?
- Why is the immune system considered “layered?”
17.2 Explore More
https://youtu.be/xZbcwi7SfZE
The Antibiotic Apocalypse Explained, Kurzgesagt – In a Nutshell, 2016.
https://youtu.be/Nw27_jMWw10
Overview of the Immune System, Handwritten Tutorials, 2011.
https://youtu.be/gVdY9KXF_Sg
The surprising reason you feel awful when you're sick - Marco A. Sotomayor, TED-Ed, 2016.
Attributions
Figure 17.1.1
Schistosome Parasite by Bruce Wetzel and Harry Schaefer (Photographers) from the National Cancer Institute, Visuals online is in the public domain (https://en.wikipedia.org/wiki/Public_domain).
Figure 17.1.2
Phagocytosis by Rlawson at en.wikibooks on Wikimedia Commons is used under a CC BY SA 3.0 (https://creativecommons.org/licenses/by-sa/3.0/deed.en) license. (Transferred from en.wikibooks to Commons by User:Adrignola.)
Figure 17.1.3
2201_Anatomy_of_the_Lymphatic_System by OpenStax College on Wikimedia Commons is used under a CC BY 3.0 (https://creativecommons.org/licenses/by/3.0) license.
Table 17.1.1
- EscherichiaColi NIAID [photo] by Rocky Mountain Laboratories, NIH National Institute of Allergy and Infectious Diseases (NIAID) on Wikimedia Commons is in the public domain (https://en.wikipedia.org/wiki/Public_domain).
- Herpes simplex virus TEM B82-0474 lores by Dr. Erskine Palmer/ CDC Public Health Image Library (PHIL) on Wikimedia Commons is in the public domain (https://en.wikipedia.org/wiki/Public_domain).
- Red death cap mushroom by Rosendahl on Wikimedia Commons is in the public domain (https://en.wikipedia.org/wiki/Public_domain). (Transferred from Pixnio by Fæ.)
- Scanning electron micrograph (SEM) of Giardia lamblia by Janice Haney Carr/ CDC, Public Health Image Library (PHIL) Photo ID# 8698 is in the public domain (https://en.wikipedia.org/wiki/Public_domain).
References
Barney, J. (2016, March 21). They’ll have to rewrite the textbooks [online article]. Illimitable - Discovery. UVA Today/ University of Virginia. https://news.virginia.edu/illimitable/discovery/theyll-have-rewrite-textbooks
Betts, J. G., Young, K.A., Wise, J.A., Johnson, E., Poe, B., Kruse, D.H., Korol, O., Johnson, J.E., Womble, M., DeSaix, P. (2013, June 19). Figure 21.2 Anatomy of the lymphatic system [digital image]. In Anatomy and Physiology (Section 21.1). OpenStax. https://openstax.org/books/anatomy-and-physiology/pages/21-1-anatomy-of-the-lymphatic-and-immune-systems
Handwritten Tutorials. (2011, October 25). Overview of the immune system. YouTube. https://www.youtube.com/watch?v=Nw27_jMWw10&feature=youtu.be
ImmiflexImmuneSystem. (2013). Neutrophil phagocytosis - White blood cell eats staphylococcus aureus bacteria. YouTube. https://www.youtube.com/watch?v=Z_mXDvZQ6dU
Kurzgesagt – In a Nutshell. (2016, March 16). The antibiotic apocalypse explained. YouTube. https://www.youtube.com/watch?v=xZbcwi7SfZE&feature=youtu.be
Louveau, A., Smirnov, I., Keyes, T. J., Eccles, J. D., Rouhani, S. J., Peske, J. D., Derecki, N. C., Castle, D., Mandell, J. W., Lee, K. S., Harris, T. H., & Kipnis, J. (2015). Structural and functional features of central nervous system lymphatic vessels. Nature, 523(7560), 337–341. https://doi.org/10.1038/nature14432
Mayo Clinic Staff. (n.d.). Autism spectrum disorder [online article]. MayoClinic.org. https://www.mayoclinic.org/diseases-conditions/autism-spectrum-disorder/symptoms-causes/syc-20352928
Mayo Clinic Staff. (n.d.). Multiple sclerosis [online article]. MayoClinic.org. https://www.mayoclinic.org/diseases-conditions/multiple-sclerosis/symptoms-causes/syc-20350269
Mayo Clinic Staff. (n.d.). Schizophrenia [online article]. MayoClinic.org. https://www.mayoclinic.org/diseases-conditions/schizophrenia/symptoms-causes/syc-20354443
TED-Ed. (2016, April 19). The surprising reason you feel awful when you're sick - Marco A. Sotomayor. YouTube. https://www.youtube.com/watch?v=gVdY9KXF_Sg&feature=youtu.be
Created by CK-12 Foundation/Adapted by Christine Miller

Case Study Conclusion: Trying to Conceive
The woman in Figure 18.12.1 is holding a home pregnancy test. The two pink lines in the middle are the type of result that Alicia and Victor are desperately hoping to see themselves one day — a positive pregnancy test. In the beginning of the chapter you learned that Alicia and Victor have been actively trying to get pregnant for a year, which, as you now know, is the time frame necessary for infertility to be diagnosed.
Alicia and Victor tried having sexual intercourse on day 14 of her menstrual cycle to optimize their chances of having his sperm meet her ovum. Why might this not be successful, even if they do not have fertility problems? Although the average menstrual cycle is 28 days, with ovulation occurring around day 14, many women vary widely from these averages (either consistently or variably) from month to month. Recall, for example, that menstrual cycles may vary from 21 to 45 days in length, and a woman’s cycle is considered to be regular if it varies within as many as eight days from shortest to longest cycle. This variability means that ovulation often does not occur on or around day 14, particularly if the woman has significantly shorter, longer, or irregular cycles — like Alicia does. Therefore, by aiming for day 14 without knowing when Alicia is actually ovulating, they may not be successful in helping Victor’s sperm encounter Alicia’s egg.
Lack of ovulation entirely can also cause variability in menstrual cycle length. As you have learned, the regulation of the menstrual cycle depends on an interplay of hormones from the pituitary gland and ovaries, including FSH and LH from the pituitary and estrogen and progesterone from the ovary — specifically from the follicle which surrounds the maturing egg and becomes the corpus luteum after ovulation. Shifts in these hormones and processes can affect ovulation and menstrual cycle length. This is why Alicia was concerned about her long and irregular menstrual cycles. If they are a sign that she is not ovulating, that could be the reason why she is having trouble getting pregnant.
In order to get a better idea of whether Alicia is ovulating, Dr. Bashir recommended that she take her basal body temperature (BBT) each morning before getting out of bed, and track it throughout her menstrual cycle. As you have learned, BBT typically rises slightly and stays high after ovulation. While tracking BBT is not a particularly effective form of contraception, since the temperature rise occurs only after ovulation, it can be a good way to see whether a woman is ovulating at all. Although not every woman will see a clear shift in BBT after ovulation, it is a relatively easy way to start assessing a woman’s fertility and is used as part of a more comprehensive fertility assessment by some physicians.
Dr. Bashir also recommended that Alicia use a home ovulation predictor kit. This is another relatively cheap and easy way to assess ovulation. Most ovulation predictor kits work by detecting the hormone LH in urine using test strips, like the ones shown in Figure 18.12.2. Why can this predict ovulation? Think about what you have learned about how ovulation is triggered. Rising levels of estrogen from the maturing follicle in the ovary causes a surge in the level of LH secreted from the pituitary gland, which triggers ovulation. This surge in LH can be detected by the home kit, which compares the level of LH in a woman’s urine to that of a control on the strip. After the LH surge is detected, ovulation will typically occur within one to two days.
By tracking her BBT and using the ovulation predictor kit, Alicia has learned that she is most likely ovulating, but not in every cycle, and sometimes she ovulates much later than day 14. Because frequent anovulatory cycles can be a sign of an underlying hormonal disorder, such as polycystic ovary syndrome (PCOS) or problems with the pituitary or other glands that regulate the reproductive system, Dr. Bashir orders blood tests for Alicia and sets up an appointment for a physical exam.
However, because Alicia is sometimes ovulating, the problem may not lie solely with her. Recall that infertility occurs in similar proportions in men and women, and can be due to problems in both partners. This is why it is generally recommended that both partners get assessed for fertility issues when they are having trouble getting pregnant after a year of trying.
Therefore, Victor proceeds with the semen analysis that Dr. Bashir recommended. In this process, the man provides a semen sample by ejaculating into a cup or special condom, and the semen is then examined under a microscope. The semen is then checked for sperm number, shape, and motility. Sperm with an abnormal shape or trouble moving will likely have trouble reaching and fertilizing an egg. A low number of sperm will also reduce the chances of conception. In this way, semen analysis can provide insight into the possible underlying causes of infertility. For instance, a low sperm count could indicate problems in sperm production or a blockage in the male reproductive tract that is preventing sperm from being emitted from the penis. Further testing would have to be done to distinguish between these two possible causes.
Victor had been worried that past injuries to his testes may have affected his fertility. You may remember the testes are where sperm are produced, and because they are external to the body, they are vulnerable to injury. In addition to physical damage to the testes and other parts of the male reproductive tract, a testicular injury could potentially cause the creation of antibodies against a man’s own sperm. As you have learned, Sertoli cells lining the seminiferous tubules are tightly packed so that the developing sperm are normally well-separated from the body’s immune system. However, in the case of an injury, this barrier can be breached, which can cause the creation of antisperm antibodies. These antibodies can hamper fertility by killing the sperm, or otherwise interfering with their ability to move or fertilize an egg. When infertility is due to such antibodies, it is called “immune infertility.”
Victor’s semen analysis shows that he has normal numbers of healthy sperm. Dr. Bashir recommends that while they investigate whether Alicia has an underlying medical issue, she continue to track her BBT and use ovulation predictor kits to try to pinpoint when she is ovulating. She recommends that once Alicia sees an LH surge, the couple try to have intercourse within three days to maximize their chances of conception. If Alicia is found to have a medical problem that is inhibiting ovulation, depending on what it is, they may either address the problem directly, or she can take medication that stimulates ovulation, such as clomiphene citrate (often sold under the brand name Clomid). This medication works by increasing the amount of FSH secreted by the pituitary.
Fortunately, tracking ovulation at home and timing intercourse appropriately was all Alicia and Victor needed to do to finally get pregnant! After their experience, they, like you, now have a much deeper understanding of the intricacies of the reproductive system and the complex biology that is involved in the making of a new human organism.
Chapter 18 Summary
In this chapter, you learned about the male and female reproductive systems. Specifically, you learned that:
- The reproductive system is the human organ system responsible for the production and fertilization of gametes and, in females, the carrying of a fetus.
- Both male and female reproductive systems have organs called gonads (testes in males, ovaries in females) that produce gametes (sperm or ova) and sex hormones (such as testosterone in males and estrogen in females). Sex hormones are endocrine hormones that control prenatal development of sex organs, sexual maturation at puberty, and reproduction after puberty.
- The reproductive system is the only organ system that is significantly different between males and females. A Y-chromosome gene called SRY is responsible for undifferentiated embryonic tissues developing into a male reproductive system. Without a Y chromosome, the undifferentiated embryonic tissues develop into a female reproductive system.
- Male and female reproductive systems are different at birth, but immature and nonfunctioning. Maturation of the reproductive system occurs during puberty when hormones from the hypothalamus and pituitary gland stimulate the gonads to produce sex hormones again. The sex hormones, in turn, cause the physical changes experienced during puberty.
- Male reproductive system organs include the testes, epididymis, penis, vas deferens, prostate gland, and seminal vesicles.
-
- The two testes are sperm- and testosterone-producing male gonads. They are contained within the scrotum, a pouch that hangs down behind the penis. The testes are filled with hundreds of tiny, tightly coiled seminiferous tubules, where sperm are produced. The tubules contain sperm in different stages of development, as well as Sertoli cells, which secrete substances needed for sperm production. Between the tubules are Leydig cells, which secrete testosterone.
- The two epididymides are contained within the scrotum. Each epididymis is a tightly coiled tubule where sperm mature and are stored until they leave the body during an ejaculation.
- The two vas deferens are long, thin tubes that run from the scrotum up into the pelvic cavity. During ejaculation, each vas deferens carries sperm from one of the epididymides to one of the pair of ejaculatory ducts.
- The two seminal vesicles are glands within the pelvis that secrete fluid through ducts into the junction of each vas deferens and ejaculatory duct. This alkaline fluid makes up about 70% of semen, the sperm-containing fluid that leaves the penis during ejaculation. Semen contains substances and nutrients that sperm need to survive and “swim” in the female reproductive tract.
- The prostate gland is located just below the seminal vesicles and surrounds the urethra and its junction with the ejaculatory ducts. The prostate secretes an alkaline fluid that makes up close to 30% of semen. Prostate fluid contains a high concentration of zinc, which sperm need to be healthy and motile.
- The ejaculatory ducts form where the vas deferens joins with the ducts of the seminal vesicles in the prostate gland. They connect the vas deferens with the urethra. The ejaculatory ducts carry sperm from the vas deferens, and secretions from the seminal vesicles and prostate gland that together form semen.
- The paired bulbourethral glands are located just below the prostate gland. They secrete a tiny amount of fluid into semen. The secretions help lubricate the urethra and neutralize any acidic urine it may contain.
- The penis is the external male organ that has the reproductive function of intromission, which is delivering sperm to the female reproductive tract. The penis also serves as the organ that excretes urine. The urethra passes through the penis and carries urine or semen out of the body. Internally, the penis consists largely of columns of spongy tissue that can fill with blood and make the penis stiff and erect. This is necessary for sexual intercourse so intromission can occur.
- Parts of a mature sperm include the head, acrosome, midpiece, and flagellum. The process of producing sperm is called spermatogenesis. This normally starts during puberty and continues uninterrupted until death.
-
- Spermatogenesis occurs in the seminiferous tubules in the testes, and requires high concentrations of testosterone. Sertoli cells in the testes play many roles in spermatogenesis, including concentrating testosterone under the influence of follicle stimulating hormone (FSH) from the pituitary gland.
- Spermatogenesis begins with a diploid stem cell called a spermatogonium, which undergoes mitosis to produce a primary spermatocyte. The primary spermatocyte undergoes meiosis I to produce haploid secondary spermatocytes, and these cells in turn, undergo meiosis II to produce spermatids. After the spermatids grow a tail and undergo other changes, they become sperm.
- Before sperm are able to “swim,” they must mature in the epididymis. The mature sperm are then stored in the epididymis until ejaculation occurs.
- Ejaculation is the process in which semen is propelled by peristalsis in the vas deferens and ejaculatory ducts from the urethra in the penis.
- Leydig cells in the testes secrete testosterone under the control of luteinizing hormone (LH) from the pituitary gland. Testosterone is needed for male sexual development at puberty and to maintain normal spermatogenesis after puberty. It also plays a role in prostate function and the ability of the penis to become erect.
- Disorders of the male reproductive system include erectile dysfunction (ED), epididymitis, prostate cancer, and testicular cancer.
-
- ED is a disorder characterized by the regular and repeated inability of a sexually mature male to obtain and maintain an erection. ED is a common disorder that occurs when normal blood flow to the penis is disturbed or there are problems with the nervous control of penile engorgement or arousal.
-
-
- Possible physiological causes of ED include aging, illness, drug use, tobacco smoking, and obesity, among others. Possible psychological causes of ED include stress, performance anxiety, and mental disorders.
- Treatments for ED may include lifestyle changes, such as stopping smoking and adopting a healthier diet and regular exercise. However, the first-line treatment is prescription drugs such as Viagra® or Cialis® that increase blood flow to the penis. Vacuum pumps or penile implants may be used to treat ED if other types of treatment fail.
- Epididymitis is inflammation of the epididymis. It is a common disorder, especially in young men. It may be acute or chronic and is often caused by a bacterial infection. Treatments may include antibiotics, anti-inflammatory drugs, and painkillers. Treatment is important to prevent the possible spread of infection, permanent damage to the epididymis or testes, and even infertility.
- Prostate cancer is the most common type of cancer in men and the second leading cause of cancer death in men. If there are symptoms, they typically involve urination, such as frequent or painful urination. Risk factors for prostate cancer include older age, family history, a high-meat diet, and sedentary lifestyle, among others.
-
-
-
- Prostate cancer may be detected by a physical exam or a high level of prostate-specific antigen (PSA) in the blood, but a biopsy is required for a definitive diagnosis. Prostate cancer is typically diagnosed relatively late in life, and is usually slow growing, so no treatment may be necessary. In younger patients or those with faster-growing tumors, treatment is likely to include surgery to remove the prostate, followed by chemotherapy and/or radiation therapy.
- Testicular cancer, or cancer of the testes, is the most common cancer in males between the ages of 20 and 39 years. It is more common in males of European than African ancestry. A lump or swelling in one testis, fluid in the scrotum, and testicular pain or tenderness are possible signs and symptoms of testicular cancer.
-
-
-
- Testicular cancer can be diagnosed by a physical exam and diagnostic tests, such as ultrasound or blood tests. Testicular cancer has one of the highest cure rates of all cancers. It is typically treated with surgery to remove the affected testis, and this may be followed by radiation therapy, and/or chemotherapy. Normal male reproductive functions are still possible after one testis is removed, if the remaining testis is healthy.
-
- The female reproductive system is made up of internal and external organs that function to produce haploid female gametes called ova, secrete female sex hormones (such as estrogen), and carry and give birth to a fetus.
- Female reproductive system organs include the ovaries, oviducts, uterus, vagina, clitoris, and labia.
-
- The vagina is an elastic, muscular canal that can accommodate the penis. It is where sperm are usually ejaculated during sexual intercourse. The vagina is also the birth canal, and it channels the flow of menstrual blood from the uterus. A healthy vagina has a balance of symbiotic bacteria and an acidic pH.
- The uterus is a muscular organ above the vagina where a fetus develops. Its muscular walls contract to push out the fetus during childbirth. The cervix is the neck of the uterus that extends down into the vagina. It contains a canal connecting the vagina and uterus for sperm or an infant to pass through. The innermost layer of the uterus, the endometrium, thickens each month in preparation for an embryo but is shed in the following menstrual period if fertilization does not occur.
- The oviducts extend from the uterus to the ovaries. Waving fimbriae at the ovary ends of the oviducts guide ovulated ova into the tubes where fertilization may occur as the ova travel to the uterus. Cilia and peristalsis help eggs move through the tubes. Tubular fluid helps nourish sperm as they swim up the tubes toward eggs.
- The ovaries are gonads that produce eggs and secrete sex hormones including estrogen. Nests of cells called follicles in the ovarian cortex are the functional units of ovaries. Each follicle surrounds an immature ovum. At birth, a baby girl’s ovaries contain at least a million eggs, and they will not produce any more during her lifetime. One egg matures and is typically ovulated each month during a woman’s reproductive years.
- The vulva is a general term for external female reproductive organs. The vulva includes the clitoris, two pairs of labia, and openings for the urethra and vagina. Secretions from Bartholin’s glands near the vaginal opening lubricate the vulva.
- The breasts are technically not reproductive organs, but their mammary glands produce milk to feed an infant after birth. Milk drains through ducts and sacs and out through the nipple when a baby sucks.
- Oogenesis is the process of producing eggs in the ovaries of a female fetus. Oogenesis begins when a diploid oogonium divides by mitosis to produce a diploid primary oocyte. The primary oocyte begins meiosis I and then remains at this stage in an immature ovarian follicle until after birth.
- After puberty, one follicle a month matures and its primary oocyte completes meiosis I to produce a secondary oocyte, which begins meiosis II. During ovulation, the mature follicle bursts open and the secondary oocyte leaves the ovary and enters a oviducts.
- While a follicle is maturing in an ovary each month, the endometrium in the uterus is building up to prepare for an embryo. Around the time of ovulation, cervical mucus becomes thinner and more alkaline to help sperm reach the secondary oocyte.
- If the secondary oocyte is fertilized by a sperm, it quickly completes meiosis II and forms a diploid zygote, which will continue through the oviducts. The zygote will go through multiple cell divisions before reaching and implanting in the uterus. If the secondary oocyte is not fertilized, it will not complete meiosis II, and will soon disintegrate.
- Pregnancy is the carrying of one or more offspring from fertilization until birth. The maternal organism must provide all the nutrients and other substances needed by the developing offspring, and also remove its wastes. She should also avoid exposures that could potentially damage the offspring, especially early in the pregnancy when organ systems are developing.
-
- The average duration of pregnancy is 40 weeks (from the first day of the last menstrual period) and is divided into three trimesters of about three months each. Each trimester is associated with certain events and conditions that a pregnant woman may expect, such as morning sickness during the first trimester, feeling fetal movements for the first time during the second trimester, and rapid weight gain in both fetus and mother during the third trimester.
- Labour, which is the general term for the birth process, usually begins around the time the amniotic sac breaks and its fluid leaks out. Labour occurs in three stages: dilation of the cervix, birth of the baby, and delivery of the placenta (afterbirth).
- The physiological function of female breasts is lactation, or the production of breast milk to feed an infant. Sucking on the breast by the infant stimulates the release of the hypothalamic hormone oxytocin from the posterior pituitary, which causes the flow of milk. The release of milk stimulates the baby to continue sucking, which in turn keeps the milk flowing. This is one of the few examples of positive feedback in the human organism.
- The ovaries produce female sex hormones, including estrogen and progesterone. Estrogen is responsible for sexual maturation and secondary sex characteristics at puberty. It is also needed to help regulate the menstrual cycle and ovulation after puberty until menopause. Progesterone prepares the uterus for pregnancy each month during the menstrual cycle, and helps maintain the pregnancy if fertilization occurs.
- The menstrual cycle refers to natural changes that occur in the female reproductive system each month during the reproductive years, except when a woman is pregnant. The cycle is necessary for the production of ova and the preparation of the uterus for pregnancy. It involves changes in both the ovaries and uterus and is controlled by pituitary hormones (FSH and LH) and ovarian hormones (estrogen and progesterone).
-
- The female reproductive period is delineated by menarche, or the first menstrual period, which usually occurs around age 12 or 13; and by menopause, or the cessation of menstrual periods, which typically occurs around age 52. A typical menstrual cycle averages 28 days in length but may vary normally from 21 to 45 days. The average menstrual period is five days long, but may vary normally from two to seven days. These variations in the menstrual cycle may occur both between women and within individual women from month to month.
- The events of the menstrual cycle that take place in the ovaries make up the ovarian cycle. It includes the follicular phase, when a follicle and its ovum mature due to rising levels of FSH; ovulation, when the ovum is released from the ovary due to a rise in estrogen and a surge in LH; and the luteal phase, when the follicle is transformed into a structure called a corpus luteum that secretes progesterone. In a 28-day menstrual cycle, the follicular and luteal phases typically average about two weeks in length, with ovulation generally occurring around day 14 of the cycle.
- The events of the menstrual cycle that take place in the uterus make up the uterine cycle. It includes menstruation, which generally occurs on days 1 to 5 of the cycle and involves shedding of endometrial tissue that built up during the preceding cycle; the proliferative phase, during which the endometrium builds up again until ovulation occurs; and the secretory phase, which follows ovulation and during which the endometrium secretes substances and undergoes other changes that prepare it to receive an embryo.
- Disorders of the female reproductive system include cervical cancer, vaginitis, and endometriosis.
-
- Cervical cancer occurs when cells of the cervix grow abnormally and develop the ability to invade nearby tissues, or spread to other parts of the body. Worldwide, cervical cancer is the second-most common type of cancer in females and the fourth-most common cause of cancer death in females. Early on, cervical cancer often has no symptoms; later, symptoms such as abnormal vaginal bleeding and pain are likely.
-
-
- Most cases of cervical cancer occur because of infection with human papillomavirus (HPV), so the HPV vaccine is expected to greatly reduce the incidence of the disease. Other risk factors include smoking and a weakened immune system. A Pap smear can diagnose cervical cancer at an early stage. Where Pap smears are done routinely, cervical cancer death rates have fallen dramatically. Treatment of cervical cancer generally includes surgery, which may be followed by radiation therapy or chemotherapy.
- Vaginitis is inflammation of the vagina. A discharge is likely, and there may be itching and pain. About 90% of cases of vaginitis are caused by infection with microorganisms, typically by the yeast Candida albicans. A minority of cases are caused by irritants or allergens in products such as soaps, spermicides, or douches.
-
-
-
- Diagnosis of vaginitis may be based on characteristics of the discharge, which can be examined microscopically or cultured. Treatment of vaginitis depends on the cause, and is usually an oral or topical anti-fungal or antibiotic medication.
- Endometriosis is a disease in which endometrial tissue grows outside the uterus. This tissue may bleed during the menstrual period and cause inflammation, pain, and scarring. The main symptom of endometriosis is pelvic pain, which may be severe. Endometriosis may also lead to infertility.
-
-
-
- Endometriosis is thought to have multiple causes, including genetic mutations. Retrograde menstruation may be the immediate cause of endometrial tissue escaping the uterus and entering the pelvic cavity. Endometriosis is usually treated with surgery to remove the abnormal tissue and medication for pain. If surgery is more conservative than hysterectomy, endometriosis may recur.
-
- Infertility is the inability of a sexually mature adult to reproduce by natural means. It is defined scientifically and medically as the failure to achieve a successful pregnancy after at least one year of regular, unprotected sexual intercourse.
- About 40% of infertility in couples is due to female infertility, and another 30% is due to male infertility. In the remaining cases, a couple’s infertility is due to problems in both partners or to unknown causes.
- Male infertility occurs when there are no or too few healthy, motile sperm. This may be caused by problems with spermatogenesis or by blockage of the male reproductive tract that prevents sperm from being ejaculated. Risk factors for male infertility include heavy alcohol use, smoking, certain medications, and advancing age, to name just a few.
- Female infertility occurs due to failure to produce viable ova by the ovaries or structural problems in the oviducts or uterus. Polycystic ovary syndrome is the most common cause of failure to produce viable eggs. Endometriosis and uterine fibroids are possible causes of structural problems in the oviducts and uterus. Risk factors for female infertility include smoking, stress, poor diet, and older age, among others.
- Diagnosing the cause(s) of a couple’s infertility generally requires testing both the man and the woman for potential problems. For men, semen is likely to be examined for adequate numbers of healthy, motile sperm. For women, signs of ovulation are monitored, for example, with an ovulation test kit or ultrasound of the ovaries. For both partners, the reproductive tract may be medically imaged to look for blockages or other abnormalities.
-
- Treatments for infertility depend on the cause. For example, if a medical problem is interfering with sperm production, medication may resolve the underlying problem so sperm production is restored. Blockages in either the male or the female reproductive tract can often be treated surgically. If there are problems with ovulation, hormonal treatments may stimulate ovulation.
- Some cases of infertility are treated with assisted reproductive technology (ART). This is a collection of medical procedures in which eggs and sperm are taken from the couple and manipulated in a lab to increase the chances of fertilization occurring and an embryo forming. Other approaches for certain causes of infertility include the use of a surrogate mother, gestational carrier, or sperm donation.
- Infertility can negatively impact a couple socially and psychologically, and it may be a major cause of marital friction or even divorce. Infertility treatments may raise ethical issues relating to the costs of the procedures and the status of embryos that are created in vitro but not used for pregnancy. Infertility is an under-appreciated problem in developing countries where birth rates are high and children have high economic as well as social value. In these countries, poor health care is likely to lead to more problems with infertility and fewer options for treatment.
- More than half of all fertile couples worldwide use contraception (birth control), which is any method or device used to prevent pregnancy. Different methods of contraception vary in their effectiveness, typically expressed as the failure rate, or the percentage of women who become pregnant using a given method during the first year of use. For most methods, the failure rate with typical use is much higher than the failure rate with perfect use.
- Types of birth control methods include barrier methods, hormonal methods, intrauterine devices, behavioural methods, and sterilization. Except for sterilization, all of the methods are reversible.
-
- Barrier methods are devices that block sperm from entering the uterus. They include condoms and diaphragms. Of all birth control methods, only condoms can also prevent the spread of sexually transmitted infections.
- Hormonal methods involve the administration of hormones to prevent ovulation. Hormones can be administered in various ways, such as in an injection, through a skin patch, or, most commonly, in birth control pills. There are two types of birth control pills: those that contain estrogen and progesterone, and those that contain only progesterone. Both types are equally effective, but they have different potential side effects.
- An intrauterine device (IUD) is a small T-shaped plastic structure containing copper or a hormone that is inserted into the uterus by a physician and left in place for months or even years. It is highly effective even with typical use, but it does have some risks, such as increased menstrual bleeding and, rarely, perforation of the uterus.
- Behavioural methods involve regulating the timing or method of intercourse to prevent introduction of sperm into the female reproductive tract, either altogether or when an egg may be present. In fertility awareness methods, unprotected intercourse is avoided during the most fertile days of the cycle as estimated by basal body temperature or the characteristics of cervical mucus. In withdrawal, the penis is withdrawn from the vagina before ejaculation occurs. Behavioural methods are the least effective methods of contraception.
- Sterilization is the most effective contraceptive method, but it requires a surgical procedure and may be irreversible. Male sterility is usually achieved with a vasectomy, in which the vas deferens are clamped or cut to prevent sperm from being ejaculated in semen. Female sterility is usually achieved with a tubal ligation, in which the oviducts are clamped or cut to prevent sperm from reaching and fertilizing eggs.
- Emergency contraception is any form of contraception that is used after unprotected vaginal intercourse. One method is the “morning after” pill, which is a high-dose birth control pill that can be taken up to five days after unprotected sex. Another method is an IUD, which can be inserted up to five days after unprotected sex.
In this chapter, you learned how the male and female reproductive systems work together to produce a zygote. In the next chapter, you will learn about how the human organism grows and develops throughout life — from a zygote all the way through old age.
Chapter 18 Review
-
- Which glands produce the non-sperm fluids that make up semen? What is the rough percentage of each fluid in semen?
- What is one reason why semen's alkalinity assists in reproduction?
- What are three things that pass through the cervical canal of females, going in either direction?
- Other than where the cancer originates, what is one difference between prostate and testicular cancer?
- If a woman is checking her basal body temperature each morning as a form of contraception, and today is day 12 of her menstrual cycle and her basal body temperature is still low, is it safe for her to have unprotected sexual intercourse today? Why or why not?
-
- Where is a diaphragm placed? How does it work to prevent pregnancy?
- Why are the testes located outside of the body?
- Why is it important to properly diagnose the causative agent when a woman has vaginitis?
- Describe two ways in which sperm can move through the male and/or female reproductive tracts.
Attributions
Figure 18.12.1
Pregnancy test/ Dos rayitas by Esparta Palma on Flickr is used under a CC BY 2.0 (https://creativecommons.org/licenses/by/2.0/) license.
Figure 18.12.2
1024px-Ovulatietest by Sapp on Wikimedia Commons is in the public domain (https://en.wikipedia.org/wiki/Public_domain).
Figure 18.12.3
Sperm Count by CK-12 Foundation is used under a CC BY-NC 3.0 (https://creativecommons.org/licenses/by-nc/3.0/) license.
References
Brainard, J/ CK-12 Foundation. (2016). Figure 3 Normal vs. low sperm count [digital image]. In CK-12 College Human Biology (Section 20.12) [online Flexbook]. CK12.org. https://www.ck12.org/book/ck-12-college-human-biology/section/20.12/
Created by CK-12 Foundation/Adapted by Christine Miller

Steady as She Goes
This device (Figure 7.8.1) looks simple, but it controls a complex system that keeps a home at a steady temperature — it's a thermostat. The device shows the current temperature in the room, and also allows the occupant to set the thermostat to the desired temperature. A thermostat is a commonly cited model of how living systems — including the human body— maintain a steady state called homeostasis.
What Is Homeostasis?
Homeostasis is the condition in which a system (such as the human body) is maintained in a more or less steady state. It is the job of cells, tissues, organs, and organ systems throughout the body to maintain many different variables within narrow ranges compatible with life. Keeping a stable internal environment requires continually monitoring the internal environment and constantly making adjustments to keep things in balance.
Set Point and Normal Range
For any given variable, such as body temperature or blood glucose level, there is a particular set point that is the physiological optimum value. The set point for human body temperature, for example, is about 37 degrees C (98.6 degrees F). As the body works to maintain homeostasis for temperature or any other internal variable, the value typically fluctuates around the set point. Such fluctuations are normal, as long as they do not become too extreme. The spread of values within which such fluctuations are considered insignificant is called the normal range. In the case of body temperature, for example, the normal range for an adult is about 36.5 to 37.5 degrees C (97.7 to 99.5 degrees F).
A good analogy for set point, normal range, and maintenance of homeostasis is driving. When you are driving a vehicle on the road, you are supposed to drive in the centre of your lane — this is analogous to the set point. Sometimes, you are not driving in the exact centre of the lane, but you are still within your lines, so you are in the equivalent of the normal range. However, if you were to get too close to the centre line or the shoulder of the road, you would take action to correct your position. You'd move left if you were too close to the shoulder, or right if too close to the centre line — which is analogous to our next concept, negative feedback to maintain homeostasis.
Maintaining Homeostasis
Homeostasis is normally maintained in the human body by an extremely complex balancing act. Regardless of the variable being kept within its normal range, maintaining homeostasis requires at least four interacting components: stimulus, sensor, control centre, and effector.
- The stimulus is provided by the variable being regulated. Generally, the stimulus indicates that the value of the variable has moved away from the set point or has left the normal range.
- The sensor monitors the values of the variable and sends data on it to the control centre.
- The control centre matches the data with normal values. If the value is not at the set point or is outside the normal range, the control centre sends a signal to the effector.
- The effector is an organ, gland, muscle, or other structure that acts on the signal from the control centre to move the variable back toward the set point.
Each of these components is illustrated in Figure 7.8.2. The diagram on the left is a general model showing how the components interact to maintain homeostasis. The diagram on the right shows the example of body temperature. From the diagrams, you can see that maintaining homeostasis involves feedback, which is data that feeds back to control a response. Feedback may be negative (as in the example below) or positive. All the feedback mechanisms that maintain homeostasis use negative feedback. Biological examples of positive feedback are much less common.
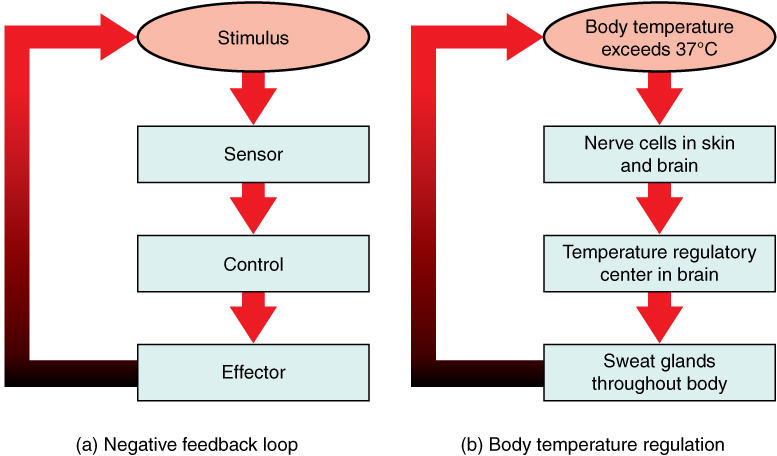
Negative Feedback
In a negative feedback loop, feedback serves to reduce an excessive response and keep a variable within the normal range. Two processes controlled by negative feedback are body temperature regulation and control of blood glucose.
Body Temperature
Body temperature regulation involves negative feedback, whether it lowers the temperature or raises it, as shown in Figure 7.8.3 and explained in the text that follows.
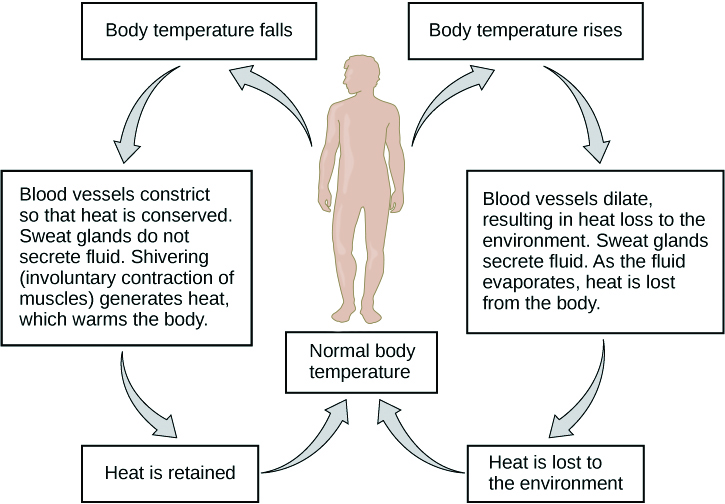
Cooling Down
The human body’s temperature regulatory centre is the hypothalamus in the brain. When the hypothalamus receives data from sensors in the skin and brain that body temperature is higher than the set point, it sets into motion the following responses:
- Blood vessels in the skin dilate (vasodilation) to allow more blood from the warm body core to flow close to the surface of the body, so heat can be radiated into the environment.
- As blood flow to the skin increases, sweat glands in the skin are activated to increase their output of sweat (diaphoresis). When the sweat evaporates from the skin surface into the surrounding air, it takes heat with it.
- Breathing becomes deeper, and the person may breathe through the mouth instead of the nasal passages. This increases heat loss from the lungs.
Heating Up
When the brain’s temperature regulatory centre receives data that body temperature is lower than the set point, it sets into motion the following responses:
- Blood vessels in the skin contract (vasoconstriction) to prevent blood from flowing close to the surface of the body, which reduces heat loss from the surface.
- As temperature falls lower, random signals to skeletal muscles are triggered, causing them to contract. This causes shivering, which generates a small amount of heat.
- The thyroid gland may be stimulated by the brain (via the pituitary gland) to secrete more thyroid hormone. This hormone increases metabolic activity and heat production in cells throughout the body.
- The adrenal glands may also be stimulated to secrete the hormone adrenaline. This hormone causes the breakdown of glycogen (the carbohydrate used for energy storage in animals) to glucose, which can be used as an energy source. This catabolic chemical process is exothermic, or heat producing.
Blood Glucose
In controlling the blood glucose level, certain endocrine cells in the pancreas (called alpha and beta cells) detect the level of glucose in the blood. They then respond appropriately to keep the level of blood glucose within the normal range.
- If the blood glucose level rises above the normal range, pancreatic beta cells release the hormone insulin into the bloodstream. Insulin signals cells to take up the excess glucose from the blood until the level of blood glucose decreases to the normal range.
- If the blood glucose level falls below the normal range, pancreatic alpha cells release the hormone glucagon into the bloodstream. Glucagon signals cells to break down stored glycogen to glucose and release the glucose into the blood until the level of blood glucose increases to the normal range.
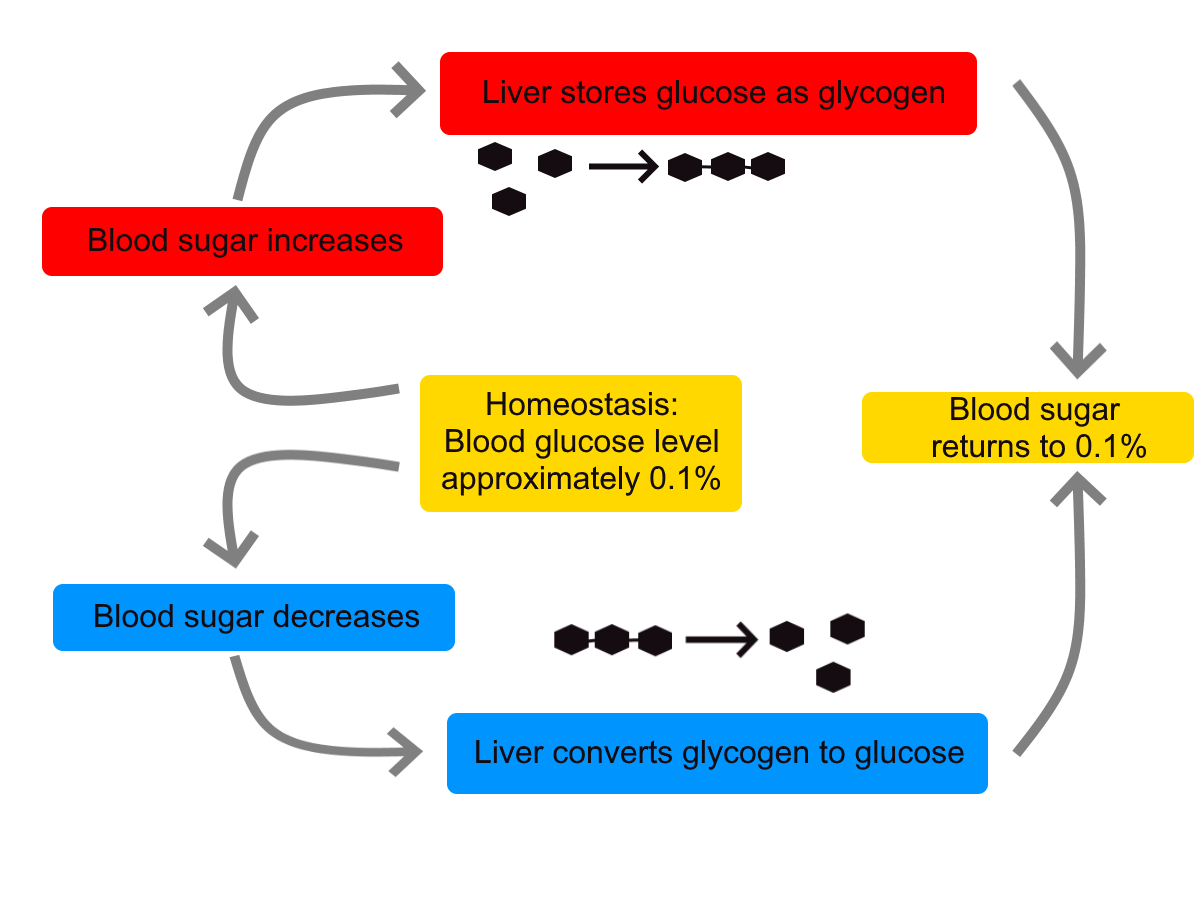
https://www.youtube.com/watch?v=Iz0Q9nTZCw4
Homeostasis and Negative/Positive Feedback, Amoeba Sisters, 2017.
Positive Feedback
In a positive feedback loop, feedback serves to intensify a response until an end point is reached. Examples of processes controlled by positive feedback in the human body include blood clotting and childbirth.
Blood Clotting
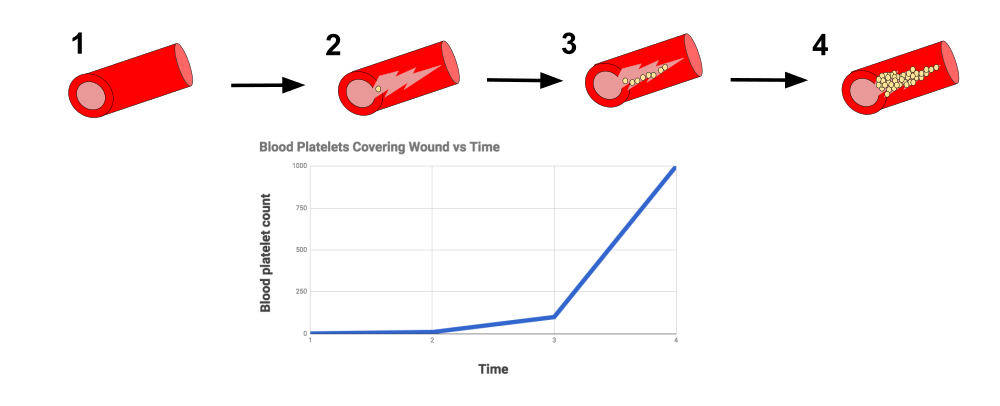
When a wound causes bleeding, the body responds with a positive feedback loop to clot the blood and stop blood loss. Substances released by the injured blood vessel wall begin the process of blood clotting. Platelets in the blood start to cling to the injured site and release chemicals that attract additional platelets. As the platelets continue to amass, more of the chemicals are released and more platelets are attracted to the site of the clot. The positive feedback accelerates the process of clotting until the clot is large enough to stop the bleeding.
Childbirth
Figure 7.8.6 shows the positive feedback loop that controls childbirth. The process normally begins when the head of the infant pushes against the cervix. This stimulates nerve impulses, which travel from the cervix to the hypothalamus in the brain. In response, the hypothalamus sends the hormone oxytocin to the pituitary gland, which secretes it into the bloodstream so it can be carried to the uterus. Oxytocin stimulates uterine contractions, which push the baby harder against the cervix. In response, the cervix starts to dilate in preparation for the passage of the baby. This cycle of positive feedback continues, with increasing levels of oxytocin, stronger uterine contractions, and wider dilation of the cervix until the baby is pushed through the birth canal and out of the body. At that point, the cervix is no longer stimulated to send nerve impulses to the brain, and the entire process stops.
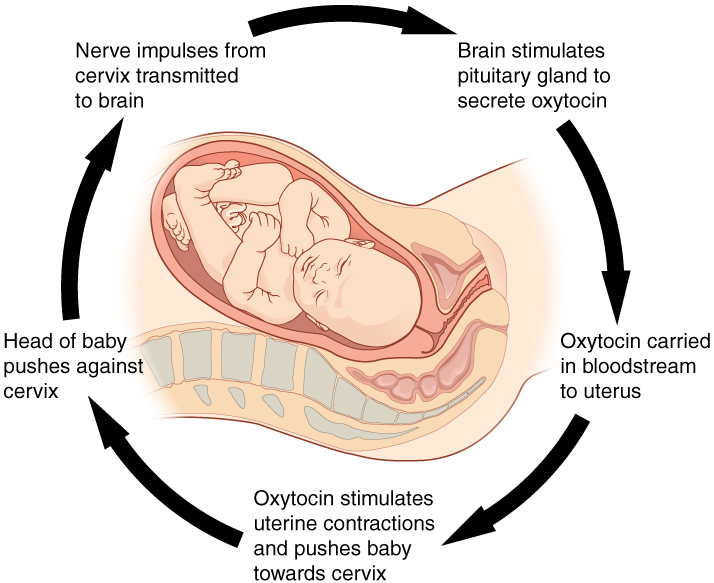
Normal childbirth is driven by a positive feedback loop. Positive feedback causes an increasing deviation from the normal state to a fixed end point, rather than a return to a normal set point as in homeostasis.
When Homeostasis Fails
Homeostatic mechanisms work continuously to maintain stable conditions in the human body. Sometimes, however, the mechanisms fail. When they do, homeostatic imbalance may result, in which cells may not get everything they need or toxic wastes may accumulate in the body. If homeostasis is not restored, the imbalance may lead to disease — or even death. Diabetes is an example of a disease caused by homeostatic imbalance. In the case of diabetes, blood glucose levels are no longer regulated and may be dangerously high. Medical intervention can help restore homeostasis and possibly prevent permanent damage to the organism.
Normal aging may bring about a reduction in the efficiency of the body’s control systems, which makes the body more susceptible to disease. Older people, for example, may have a harder time regulating their body temperature. This is one reason they are more likely than younger people to develop serious heat-induced illnesses, such as heat stroke.
Feature: My Human Body
Diabetes is diagnosed in people who have abnormally high levels of blood glucose after fasting for at least 12 hours. A fasting level of blood glucose below 100 is normal. A level between 100 and 125 places you in the pre-diabetes category, and a level higher than 125 results in a diagnosis of diabetes.
Of the two types of diabetes, type 2 diabetes is the most common, accounting for about 90 per cent of all cases of diabetes in the United States. Type 2 diabetes typically starts after the age of 40. However, because of the dramatic increase in recent decades in obesity in younger people, the age at which type 2 diabetes is diagnosed has fallen. Even children are now being diagnosed with type 2 diabetes. Today, about 3 million Canadians (8.1% of total population) are living with diabetes.
You may at some point have your blood glucose level tested during a routine medical exam. If your blood glucose level indicates that you have diabetes, it may come as a shock to you because you may not have any symptoms of the disease. You are not alone, because as many as one in four diabetics do not know they have the disease. Once the diagnosis of diabetes sinks in, you may be devastated by the news. Diabetes can lead to heart attacks, strokes, blindness, kidney failure, nerve damage, and loss of toes or feet. The risk of death in adults with diabetes is 50 per cent greater than it is in adults without diabetes, and diabetes is the seventh leading cause of death of adults. In addition, controlling diabetes usually requires frequent blood glucose testing, watching what and when you eat, and taking medications or even insulin injections. All of this may seem overwhelming.
The good news is that changing your lifestyle may stop the progression of type 2 diabetes or even reverse it. By adopting healthier habits, you may be able to keep your blood glucose level within the normal range without medications or insulin. Here’s how:
- Lose weight. Any weight loss is beneficial. Losing as little as seven per cent of your weight may be all that is needed to stop diabetes in its tracks. It is especially important to eliminate excess weight around your waist.
- Exercise regularly. You should try to exercise for at least 30 minutes, five days a week. This will not only lower your blood sugar and help your insulin work better, but it will also lower your blood pressure and improve your heart health. Another bonus of exercise is that it will help you lose weight by increasing your basal metabolic rate.
- Adopt a healthy diet. Decrease your consumption of refined carbohydrates, such as sweets and sugary drinks. Increase your intake of fibre-rich foods, such as fruits, vegetables, and whole grains. About one-quarter of each meal should consist of high-protein foods, such as fish, chicken, dairy products, legumes, or nuts.
- Control stress. Stress can increase your blood glucose and also raise your blood pressure and risk of heart disease. When you feel stressed out, do breathing exercises or take a brisk walk or jog. Try to replace stressful thoughts with more calming ones.
- Establish a support system. Enlist the help and support of loved ones, as well as medical professionals, such as a nutritionist and diabetes educator. Having a support system will help ensure that you are on the path to wellness, and that you can stick to your plan.
7.8 Summary
- Homeostasis is the condition in which a system (such as the human body) is maintained in a more or less steady state. It is the job of cells, tissues, organs, and organ systems throughout the body to maintain homeostasis.
- For any given variable, such as body temperature, there is a particular set point that is the physiological optimum value. The spread of values around the set point that is considered insignificant is called the normal range.
- Homeostasis is generally maintained by a negative feedback loop that includes a stimulus, sensor, control centre, and effector. Negative feedback serves to reduce an excessive response and to keep a variable within the normal range. Negative feedback loops control body temperature and the blood glucose level.
- Positive feedback loops are not common in biological systems. Positive feedback serves to intensify a response until an end point is reached. Positive feedback loops control blood clotting and childbirth.
- Sometimes homeostatic mechanisms fail, resulting in homeostatic imbalance. Diabetes is an example of a disease caused by homeostatic imbalance. Aging can bring about a reduction in the efficiency of the body’s control system, which makes the elderly more susceptible to disease.
7.8 Review Questions
-
-
- Compare and contrast negative and positive feedback loops.
- Explain how negative feedback controls body temperature.
- Give two examples of physiological processes controlled by positive feedback loops.
- During breastfeeding, the stimulus of the baby sucking on the nipple increases the amount of milk produced by the mother. The more sucking, the more milk is usually produced. Is this an example of negative or positive feedback? Explain your answer. What do you think might be the evolutionary benefit of the milk production regulation mechanism you described?
- Explain why homeostasis is regulated by negative feedback loops, rather than positive feedback loops.
- The level of a sex hormone, testosterone (T), is controlled by negative feedback. Another hormone, gonadotropin-releasing hormone (GnRH), is released by the hypothalamus of the brain, which triggers the pituitary gland to release luteinizing hormone (LH). LH stimulates the gonads to produce T. When there is too much T in the bloodstream, it feeds back on the hypothalamus, causing it to produce less GnRH. While this does not describe all the feedback loops involved in regulating T, answer the following questions about this particular feedback loop.
- What is the stimulus in this system? Explain your answer.
- What is the control centre in this system? Explain your answer.
- In this system, is the pituitary considered the stimulus, sensor, control centre, or effector? Explain your answer.
7.8 Explore More
https://www.youtube.com/watch?v=LSgEJSlk6W4
Homeostasis - What Is Homeostasis - What Is Set Point For Homeostasis - Homeostasis In The Human Body, Whats Up Dude, 2017.
https://www.youtube.com/watch?v=XMsJ-3qRVJM
Attributions
Figure 7.8.1
Nest_Thermostat by Amanitamano on Wikimedia Commons is used under a CC BY-SA 3.0 (https://creativecommons.org/licenses/by-sa/3.0/deed.en) license.
Figure 7.8.2
Negative_Feedback_Loops by OpenStax on Wikimedia Commons is used under a CC BY 4.0 (https://creativecommons.org/licenses/by/4.0/deed.en) license.
Figure 7.8.3
Body Temperature Homeostasis by OpenStax College, Biology is used under a CC BY 4.0 license.
Figure 7.8.4
Homeostasis_of_blood_sugar by Christinelmiller on Wikimedia Commons is used under a CC0 1.0 Universal Public Domain Dedication (https://creativecommons.org/publicdomain/zero/1.0/deed.en) license.
Figure 7.8.5
Positive_Feedback_Diagram_Blood_Clotting by Elliottuttle on Wikimedia Commons is used under a CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0) license.
Figure 7.8.6
Pregnancy-Positive_Feedback by OpenStax on Wikimedia Commons is used under a CC BY 4.0 (https://creativecommons.org/licenses/by/4.0/deed.en) license.
References
Amoeba Sisters. (2017, September 7). Homeostasis and negative/positive feedback. YouTube. https://www.youtube.com/watch?v=Iz0Q9nTZCw4&feature=youtu.be
Betts, J. G., Young, K.A., Wise, J.A., Johnson, E., Poe, B., Kruse, D.H., Korol, O., Johnson, J.E., Womble, M., DeSaix, P. (2013, April 25). Figure 1.10 Negative feedback loop [digital image/ diagram]. In Anatomy and Physiology (Section 1.5). OpenStax. https://openstax.org/books/anatomy-and-physiology/pages/1-5-homeostasis
Betts, J. G., Young, K.A., Wise, J.A., Johnson, E., Poe, B., Kruse, D.H., Korol, O., Johnson, J.E., Womble, M., DeSaix, P. (2013, April 25). Figure 1.11 Positive feedback loop normal childbirth is driven by a positive feedback loop [digital image/ diagram]. In Anatomy and Physiology (Section 1.5). OpenStax. https://openstax.org/books/anatomy-and-physiology/pages/1-5-homeostasis
Cognito. (2018, December 18). GCSE Biology - Homeostasis #38. YouTube. https://www.youtube.com/watch?v=XMsJ-3qRVJM&feature=youtu.be
Mayo Clinic Staff. (n.d.). Type 2 diabetes [online article]. MayoClinic.org. https://www.mayoclinic.org/diseases-conditions/type-2-diabetes/symptoms-causes/syc-20351193
OpenStax CNX. (2016, March 23). Figure 4 The body is able to regulate temperature in response to signals from the nervous system [digital image]. In OpenStax, Biology (Section 33.3). https://cnx.org/contents/GFy_h8cu@10.8:BP24ZReh@7/Homeostasis
Whats Up Dude. (2017, September 20). Homeostasis - What is homeostasis - What is set point for homeostasis - Homeostasis in the human body. YouTube. https://www.youtube.com/watch?v=LSgEJSlk6W4&feature=youtu.be
Image shows several baguettes laying on a counter
An organic chemical that functions in the brain and body of many types of animals (and humans) as a neurotransmitter—a chemical message released by nerve cells to send signals to other cells, such as neurons, muscle cells and gland cells.
Image shows a diagram illustrating how peristalsis pushes food through the digestive tract by squeezing just behind the food, pushing it forward.
As per caption
Created by CK-12 Foundation/Adapted by Christine Miller

Art for All Eras
Pictured in Figure 10.2.1, is Maud Stevens Wagner, a tattoo artist from 1907. Tattoos are not just a late 20th and early 21st century trend. They have been popular in many eras and cultures. Tattoos literally illustrate the biggest organ of the human body: the skin. The skin is very thin, but it covers a large area — about 2 m2 in adults. The skin is the major organ in the integumentary system.
What Is the Integumentary System?
In addition to the skin, the integumentary system includes the hair and nails, which are organs that grow out of the skin. Because the organs of the integumentary system are mostly external to the body, you may think of them as little more than accessories, like clothing or jewelry, but they serve vital physiological functions. They provide a protective covering for the body, sense the environment, and help the body maintain homeostasis.
The Skin
The skin is remarkable not only because it is the body’s largest organ: the average square inch of skin has 20 blood vessels, 650 sweat glands, and more than 1,000 nerve endings. Incredibly, it also has 60,000 pigment-producing cells. All of these structures are packed into a stack of cells that is just 2 mm thick. Although the skin is thin, it consists of two distinct layers: the epidermis and dermis, as shown in the diagram (Figure 10.2.2).
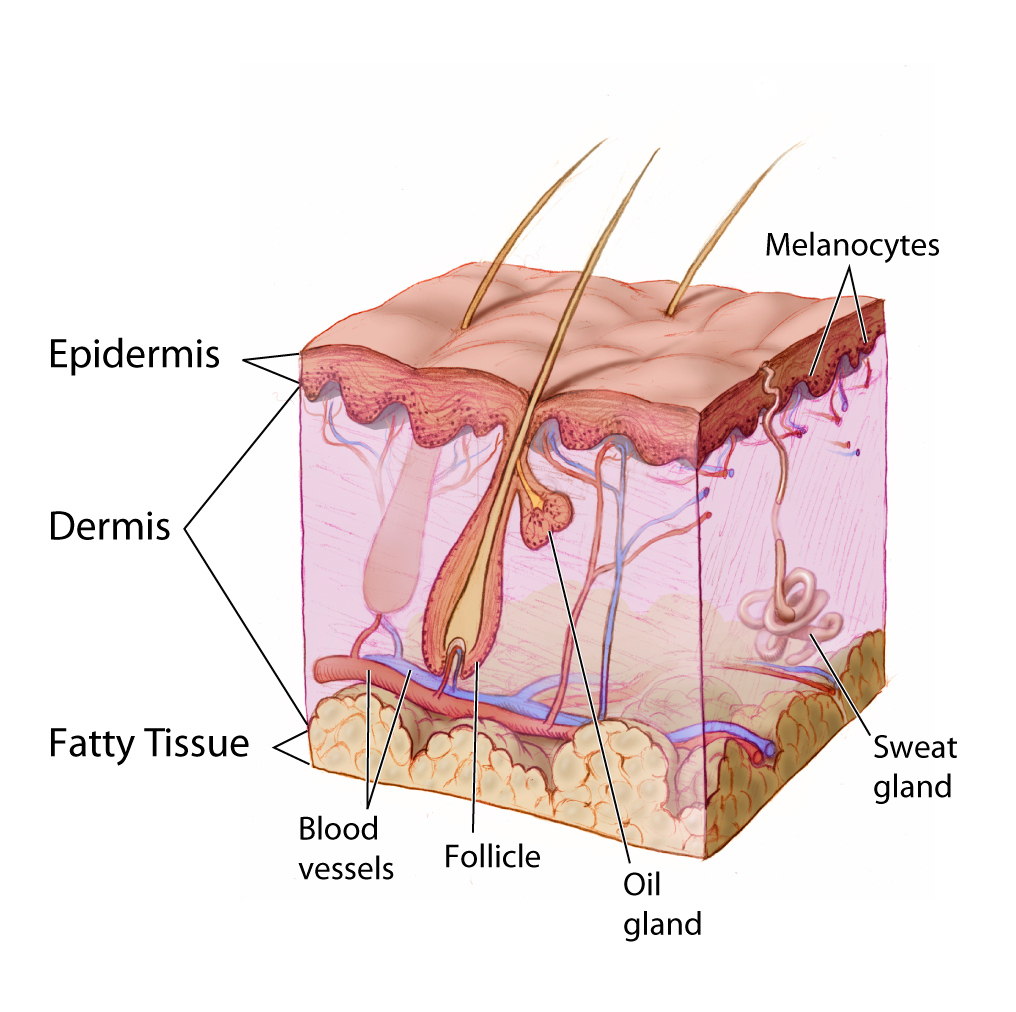
Outer Layer of Skin
The outer layer of skin is the epidermis. This layer is thinner than the inner layer (the dermis). The epidermis consists mainly of epithelial cells, called keratinocytes, which produce the tough, fibrous protein keratin. The innermost cells of the epidermis are stem cells that divide continuously to form new cells. The newly formed cells move up through the epidermis toward the skin surface, while producing more and more keratin. The cells become filled with keratin and die by the time they reach the surface, where they form a protective, waterproof layer. As the dead cells are shed from the surface of the skin, they are replaced by other cells that move up from below. The epidermis also contains melanocytes, the cells that produce the brown pigment melanin, which gives skin most of its colour. Although the epidermis contains some sensory receptor cells — called Merkel cells — it contains no nerves, blood vessels, or other structures.
Inner Layer of Skin
The dermis is the inner, thicker layer of skin. It consists mainly of tough connective tissue, and is attached to the epidermis by collagen fibres. The dermis contains many structures (as shown in Figure 10.2.2), including blood vessels, sweat glands, and hair follicles, which are structures where hairs originate. In addition, the dermis contains many sensory receptors, nerves, and oil glands.
Functions of the Skin
The skin has multiple roles in the body. Many of these roles are related to homeostasis. The skin’s main functions are preventing water loss from the body and serving as a barrier to the entry of microorganisms. Another function of the skin is synthesizing vitamin D, which occurs when the skin is exposed to ultraviolet (UV) light. Melanin in the epidermis blocks some of the UV light and protects the dermis from its damaging effects.
Another important function of the skin is helping to regulate body temperature. When the body is too warm, for example, the skin lowers body temperature by producing sweat, which cools the body when it evaporates. The skin also increases the amount of blood flowing near the body surface through vasodilation (widening of blood vessels), bringing heat from the body core to radiate out into the environment. The sweaty hair and flushed skin of the young man pictured in Figure 10.2.3 reflect these skin responses to overheating.

Hair

Hair is a fibre found only in mammals. It consists mainly of keratin-producing keratinocytes. Each hair grows out of a follicle in the dermis. By the time the hair reaches the surface, it consists mainly of dead cells filled with keratin. Hair serves several homeostatic functions. Head hair is important in preventing heat loss from the head and protecting its skin from UV radiation. Hairs in the nose trap dust particles and microorganisms in the air, and prevent them from reaching the lungs. Hair all over the body provides sensory input when objects brush against it, or when it sways in moving air. Eyelashes and eyebrows (see Figure 10.2.4) protect the eyes from water, dirt, and other irritants.
Nails
Fingernails and toenails consist of dead keratinocytes filled with keratin. The keratin makes them hard but flexible, which is important for the functions they serve. Nails prevent injury by forming protective plates over the ends of the fingers and toes. They also enhance sensation by acting as a counterforce to the sensitive fingertips when objects are handled. In addition, the fingernails can be used as tools.
Interactions with Other Organ Systems
The skin and other parts of the integumentary system work with other organ systems to maintain homeostasis.
- The skin works with the immune system to defend the body from pathogens by serving as a physical barrier to microorganisms.
- Vitamin D is needed by the digestive system to absorb calcium from food. By synthesizing vitamin D, the skin works with the digestive system to ensure that calcium can be absorbed.
- To control body temperature, the skin works with the cardiovascular system to either lose body heat, or to conserve it through vasodilation or vasoconstriction.
- To detect certain sensations from the outside world, the nervous system depends on nerve receptors in the skin.
10.2 Summary
- The integumentary system consists of the skin, hair, and nails. Functions of the integumentary system include providing a protective covering for the body, sensing the environment, and helping the body maintain homeostasis.
- The skin consists of two distinct layers: a thinner outer layer called the epidermis, and a thicker inner layer called the dermis.
- The epidermis consists mainly of epithelial cells called keratinocytes, which produce keratin. New keratinocytes form at the bottom of the epidermis. They become filled with keratin and die as they move upward toward the surface of the skin, where they form a protective, waterproof layer.
- The dermis consists mainly of tough connective tissues and many structures, including blood vessels, sensory receptors, nerves, hair follicles, and oil and sweat glands.
- The skin’s main functions are preventing water loss from the body, serving as a barrier to the entry of microorganisms, synthesizing vitamin D, blocking UV light, and helping to regulate body temperature.
- Hair consists mainly of dead keratinocytes and grows out of follicles in the dermis. Hair helps prevent heat loss from the head, and protects its skin from UV light. Hair in the nose filters incoming air, and the eyelashes and eyebrows keep harmful substances out of the eyes. Hair all over the body provides tactile sensory input.
- Like hair, nails also consist mainly of dead keratinocytes. They help protect the ends of the fingers and toes, enhance the sense of touch in the fingertips, and may be used as tools.
10.2 Review Questions
- Name the organs of the integumentary system.
- Compare and contrast the epidermis and dermis.
- Identify functions of the skin.
-
- What is the composition of hair?
- Describe three physiological roles played by hair.
- What do nails consist of?
- List two functions of nails.
- In terms of composition, what do the outermost surface of the skin, the nails, and hair have in common?
- Identify two types of cells found in the epidermis of the skin. Describe their functions.
- Which structure and layer of skin does hair grow out of?
- Identify three main functions of the integumentary system. Give an example of each.
- What are two ways in which the integumentary system protects the body against UV radiation?
10.2 Explore More
https://www.youtube.com/watch?v=OxPlCkTKhzY
The science of skin - Emma Bryce, TED-Ed, 2018.
https://www.youtube.com/watch?v=ZSJITdsTze0&feature=emb_logo
Why do we have to wear sunscreen? - Kevin P. Boyd, TED-Ed, 2013.
https://www.youtube.com/watch?time_continue=1&v=Lfhot7tQcWs&feature=emb_logo
Scarification | National Geographic, 2008.
Attributions
Figure 10.2.1
Maud_Stevens_Wagner -The Plaza Gallery, Los Angeles, 1907 from the Library of Congress on Wikimedia Commons is in the public domain (https://en.wikipedia.org/wiki/public_domain).
Figure 10.2.2
Anatomy_The_Skin_-_NCI_Visuals_Online by Don Bliss (artist) from National Cancer Institute, on Wikimedia Commons is in the public domain (https://en.wikipedia.org/wiki/public_domain).
Figure 10.2.3
shashank-shekhar-Db1J_qp_ctc [photo] by Shashank Shekhar on Unsplash is used under the Unsplash License (https://unsplash.com/license).
Figure 10.2.4
Eyelashes by aryan-dhiman-93NBu0zG_H4 [photo] by Aryan Dhiman on Unsplash is used under the Unsplash License (https://unsplash.com/license).
Reference
National Geographic. (2008). Scarification | National Geographic. YouTube. https://www.youtube.com/watch?v=Lfhot7tQcWs&t=1s
TED-Ed. (2018, March 12). The science of skin - Emma Bryce. YouTube. https://www.youtube.com/watch?v=OxPlCkTKhzY&feature=youtu.be
TED-Ed. (2013, August 6). Why do we have to wear sunscreen? - Kevin P. Boyd. YouTube. https://www.youtube.com/watch?v=ZSJITdsTze0&feature=youtu.be
Created by CK-12 Foundation/Adapted by Christine Miller

Feel the Burn
The person in Figure 10.3.1 is no doubt feeling the burn — sunburn, that is. Sunburn occurs when the outer layer of the skin is damaged by UV light from the sun or tanning lamps. Some people deliberately allow UV light to burn their skin, because after the redness subsides, they are left with a tan. A tan may look healthy, but it is actually a sign of skin damage. People who experience one or more serious sunburns are significantly more likely to develop skin cancer. Natural pigment molecules in the skin help protect it from UV light damage. These pigment molecules are found in the layer of the skin called the epidermis.
What is the Epidermis?
The epidermis is the outer of the two main layers of the skin. The inner layer is the dermis. It averages about 0.10 mm thick, and is much thinner than the dermis. The epidermis is thinnest on the eyelids (0.05 mm) and thickest on the palms of the hands and soles of the feet (1.50 mm). The epidermis covers almost the entire body surface. It is continuous with — but structurally distinct from — the mucous membranes that line the mouth, anus, urethra, and vagina.
Structure of the Epidermis
There are no blood vessels and very few nerve cells in the epidermis. Without blood to bring epidermal cells oxygen and nutrients, the cells must absorb oxygen directly from the air and obtain nutrients via diffusion of fluids from the dermis below. However, as thin as it is, the epidermis still has a complex structure. It has a variety of cell types and multiple layers.
Cells of the Epidermis
There are several different types of cells in the epidermis. All of the cells are necessary for the important functions of the epidermis.
- The epidermis consists mainly of stacks of keratin-producing epithelial cells called keratinocytes. These cells make up at least 90 per cent of the epidermis. Near the top of the epidermis, these cells are also called squamous cells.
- Another eight per cent of epidermal cells are melanocytes. These cells produce the pigment melanin that protects the dermis from UV light.
- About one per cent of epidermal cells are Langerhans cells. These are immune system cells that detect and fight pathogens entering the skin.
- Less than one per cent of epidermal cells are Merkel cells, which respond to light touch and connect to nerve endings in the dermis.
Layers of the Epidermis
The epidermis in most parts of the body consists of four distinct layers. A fifth layer occurs in the palms of the hands and soles of the feet, where the epidermis is thicker than in the rest of the body. The layers of the epidermis are shown in Figure 10.3.2, and described in the following text.
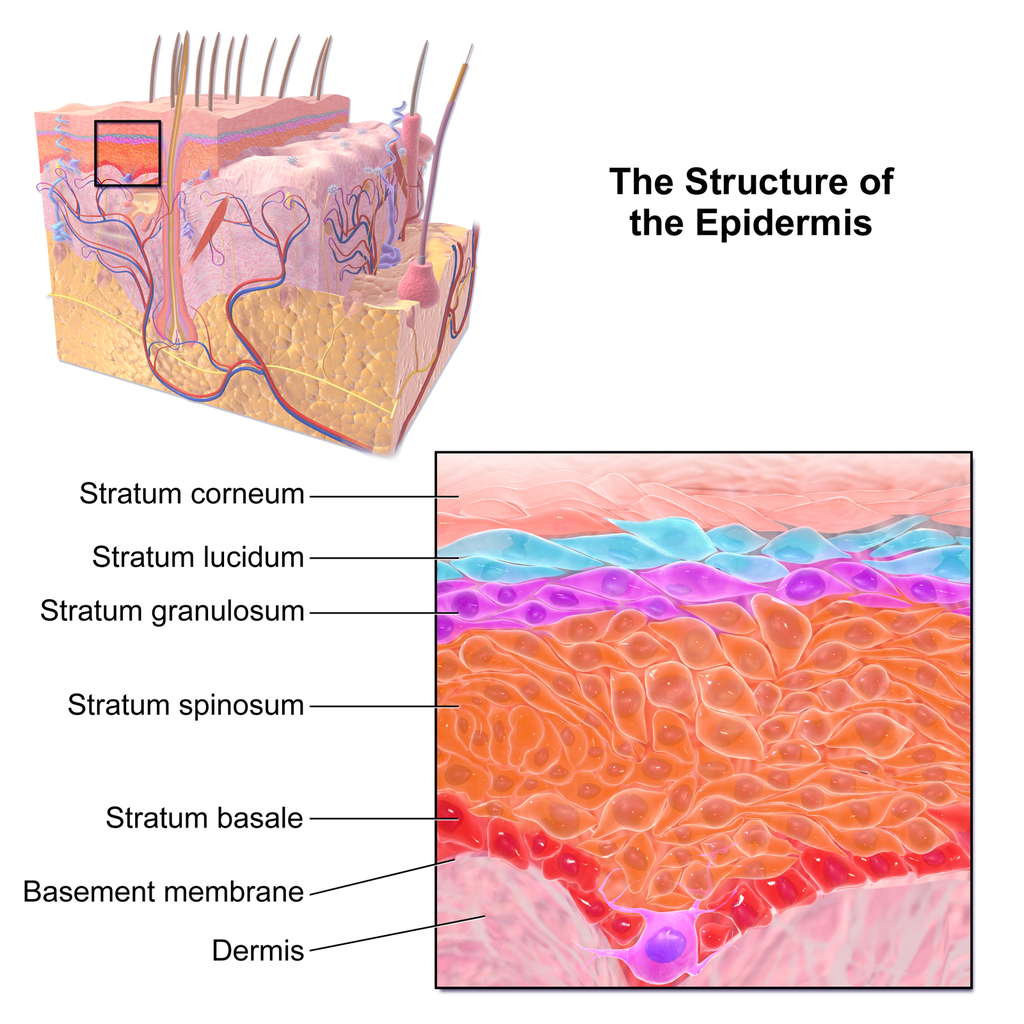
Stratum Basale
The stratum basale is the innermost (or deepest) layer of the epidermis. It is separated from the dermis by a membrane called the basement membrane. The stratum basale contains stem cells — called basal cells — which divide to form all the keratinocytes of the epidermis. When keratinocytes first form, they are cube-shaped and contain almost no keratin. As more keratinocytes are produced, previously formed cells are pushed up through the stratum basale. Melanocytes and Merkel cells are also found in the stratum basale. The Merkel cells are especially numerous in touch-sensitive areas, such as the fingertips and lips.
Stratum Spinosum
Just above the stratum basale is the stratum spinosum. This is the thickest of the four epidermal layers. The keratinocytes in this layer have begun to accumulate keratin, and they have become tougher and flatter. Spiny cellular projections form between the keratinocytes and hold them together. In addition to keratinocytes, the stratum spinosum contains the immunologically active Langerhans cells.
Stratum Granulosum
The next layer above the stratum spinosum is the stratum granulosum. In this layer, keratinocytes have become nearly filled with keratin, giving their cytoplasm a granular appearance. Lipids are released by keratinocytes in this layer to form a lipid barrier in the epidermis. Cells in this layer have also started to die, because they are becoming too far removed from blood vessels in the dermis to receive nutrients. Each dying cell digests its own nucleus and organelles, leaving behind only a tough, keratin-filled shell.
Stratum Lucidum
Only on the palms of the hands and soles of the feet, the next layer above the stratum granulosum is the stratum lucidum. This is a layer consisting of stacks of translucent, dead keratinocytes that provide extra protection to the underlying layers.
Stratum Corneum
The uppermost layer of the epidermis everywhere on the body is the stratum corneum. This layer is made of flat, hard, tightly packed dead keratinocytes that form a waterproof keratin barrier to protect the underlying layers of the epidermis. Dead cells from this layer are constantly shed from the surface of the body. The shed cells are continually replaced by cells moving up from lower layers of the epidermis. It takes a period of about 48 days for newly formed keratinocytes in the stratum basale to make their way to the top of the stratum corneum to replace shed cells.
Functions of the Epidermis
The epidermis has several crucial functions in the body. These functions include protection, water retention, and vitamin D synthesis.
Protective Functions
The epidermis provides protection to underlying tissues from physical damage, pathogens, and UV light.
Protection from Physical Damage
Most of the physical protection of the epidermis is provided by its tough outer layer, the stratum corneum. Because of this layer, minor scrapes and scratches generally do not cause significant damage to the skin or underlying tissues. Sharp objects and rough surfaces have difficulty penetrating or removing the tough, dead, keratin-filled cells of the stratum corneum. If cells in this layer are pierced or scraped off, they are quickly replaced by new cells moving up to the surface from lower skin layers.
Protection from Pathogens

When pathogens such as viruses and bacteria try to enter the body, it is virtually impossible for them to enter through intact epidermal layers. Generally, pathogens can enter the skin only if the epidermis has been breached, for example by a cut, puncture, or scrape (like the one pictured in Figure 10.3.3). That’s why it is important to clean and cover even a minor wound in the epidermis. This helps ensure that pathogens do not use the wound to enter the body. Protection from pathogens is also provided by conditions at or near the skin surface. These include relatively high acidity (pH of about 5.0), low amounts of water, the presence of antimicrobial substances produced by epidermal cells, and competition with non-pathogenic microorganisms that normally live on the epidermis.
Protection from UV Light
UV light that penetrates the epidermis can damage epidermal cells. In particular, it can cause mutations in DNA that lead to the development of skin cancer, in which epidermal cells grow out of control. UV light can also destroy vitamin B9 (in forms such as folate or folic acid), which is needed for good health and successful reproduction. In a person with light skin, just an hour of exposure to intense sunlight can reduce the body’s vitamin B9 level by 50 per cent.
Melanocytes in the stratum basale of the epidermis contain small organelles called melanosomes, which produce, store, and transport the dark brown pigment melanin. As melanosomes become full of melanin, they move into thin extensions of the melanocytes. From there, the melanosomes are transferred to keratinocytes in the epidermis, where they absorb UV light that strikes the skin. This prevents the light from penetrating deeper into the skin, where it can cause damage. The more melanin there is in the skin, the more UV light can be absorbed.
Water Retention
Skin's ability to hold water and not lose it to the surrounding environment is due mainly to the stratum corneum. Lipids arranged in an organized way among the cells of the stratum corneum form a barrier to water loss from the epidermis. This is critical for maintaining healthy skin and preserving proper water balance in the body.
Although the skin is impermeable to water, it is not impermeable to all substances. Instead, the skin is selectively permeable, allowing certain fat-soluble substances to pass through the epidermis. The selective permeability of the epidermis is both a benefit and a risk.
- Selective permeability allows certain medications to enter the bloodstream through the capillaries in the dermis. This is the basis of medications that are delivered using topical ointments, or patches (see Figure 10.3.4) that are applied to the skin. These include steroid hormones, such as estrogen (for hormone replacement therapy), scopolamine (for motion sickness), nitroglycerin (for heart problems), and nicotine (for people trying to quit smoking).
- Selective permeability of the epidermis also allows certain harmful substances to enter the body through the skin. Examples include the heavy metal lead, as well as many pesticides.
Vitamin D Synthesis
Vitamin D is a nutrient that is needed in the human body for the absorption of calcium from food. Molecules of a lipid compound named 7-dehydrocholesterol are precursors of vitamin D. These molecules are present in the stratum basale and stratum spinosum layers of the epidermis. When UV light strikes the molecules, it changes them to vitamin D3. In the kidneys, vitamin D3 is converted to calcitriol, which is the form of vitamin D that is active in the body.
What Gives Skin Its Colour?
Melanin in the epidermis is the main substance that determines the colour of human skin. It explains most of the variation in skin colour in people around the world. Two other substances also contribute to skin colour, however, especially in light-skinned people: carotene and hemoglobin.
- The pigment carotene is present in the epidermis and gives skin a yellowish tint, especially in skin with low levels of melanin.
- Hemoglobin is a red pigment found in red blood cells. It is visible through skin as a pinkish tint, mainly in skin with low levels of melanin. The pink colour is most visible when capillaries in the underlying dermis dilate, allowing greater blood flow near the surface.
Hear what Bill Nye has to say about the subject of skin colour in the video here.
Bacteria on Skin
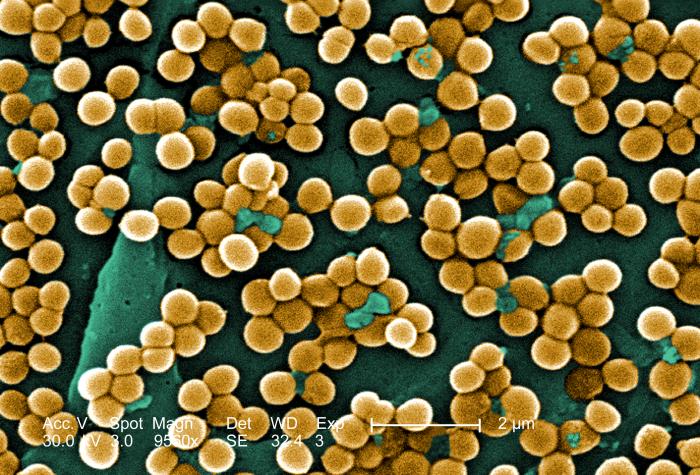
The surface of the human skin normally provides a home to countless numbers of bacteria. Just one square inch of skin normally has an average of about 50 million bacteria. These generally harmless bacteria represent roughly one thousand bacterial species (including the one in Figure 10.3.5) from 19 different bacterial phyla. Typical variations in the moistness and oiliness of the skin produce a variety of rich and diverse habitats for these microorganisms. For example, the skin in the armpits is warm and moist and often hairy, whereas the skin on the forearms is smooth and dry. These two areas of the human body are as diverse to microorganisms as rainforests and deserts are to larger organisms. The density of bacterial populations on the skin depends largely on the region of the skin and its ecological characteristics. For example, oily surfaces, such as the face, may contain over 500 million bacteria per square inch. Despite the huge number of individual microorganisms living on the skin, their total volume is only about the size of a pea.
In general, the normal microorganisms living on the skin keep one another in check, and thereby play an important role in keeping the skin healthy. If the balance of microorganisms is disturbed, however, there may be an overgrowth of certain species, and this may result in an infection. For example, when a patient is prescribed antibiotics, it may kill off normal bacteria and allow an overgrowth of single-celled yeast. Even if skin is disinfected, no amount of cleaning can remove all of the microorganisms it contains. Disinfected areas are also quickly recolonized by bacteria residing in deeper areas (such as hair follicles) and in adjacent areas of the skin.
Feature: Myth vs. Reality
Because of the negative health effects of excessive UV light exposure, it is important to know the facts about protecting the skin from UV light.
Myth |
Reality |
| "Sunblock and sunscreen are just different names for the same type of product. They both work the same way and are equally effective." | Sunscreens and sunblocks are different types of products that protect the skin from UV light in different ways. They are not equally effective. Sunblocks are opaque, so they do not let light pass through. They prevent most of the rays of UV light from penetrating to the skin surface. Sunblocks are generally stronger and more effective than sunscreens. Sunblocks also do not need to be reapplied as often as sunscreens. Sunscreens, in contrast, are transparent once they are applied the skin. Although they can prevent most UV light from penetrating the skin when first applied, the active ingredients in sunscreens tend to break down when exposed to UV light. Sunscreens, therefore, must be reapplied often to remain effective. |
| "The skin needs to be protected from UV light only on sunny days. When the sky is cloudy, UV light cannot penetrate to the ground and harm the skin." | Even on cloudy days, a significant amount of UV radiation penetrates the atmosphere to strike Earth’s surface. Therefore, using sunscreens or sunblocks to protect exposed skin is important even when there are clouds in the sky. |
| "People who have dark skin, such as African Americans, do not need to worry about skin damage from UV light." | No matter what colour skin you have, your skin can be damaged by too much exposure to UV light. Therefore, even dark-skinned people should use sunscreens or sunblocks to protect exposed skin from UV light. |
| "Sunscreens with an SPF (sun protection factor) of 15 are adequate to fully protect the skin from UV light." | Most dermatologists recommend using sunscreens with an SPF of at least 35 for adequate protection from UV light. They also recommend applying sunscreens at least 20 minutes before sun exposure and reapplying sunscreens often, especially if you are sweating or spending time in the water. |
| "Using tanning beds is safer than tanning outside in natural sunlight." | The light in tanning beds is UV light, and it can do the same damage to the skin as the natural UV light in sunlight. This is evidenced by the fact that people who regularly use tanning beds have significantly higher rates of skin cancer than people who do not. It is also the reason that the use of tanning beds is prohibited in many places in people who are under the age of 18, just as youth are prohibited from using harmful substances, such as tobacco and alcohol. |
10.3 Summary
- The epidermis is the outer of the two main layers of the skin. It is very thin, but has a complex structure.
- Cell types in the epidermis include keratinocytes that produce keratin and make up 90 per cent of epidermal cells, melanocytes that produce melanin, Langerhans cells that fight pathogens in the skin, and Merkel cells that respond to light touch.
- The epidermis in most parts of the body consists of four distinct layers. A fifth layer occurs only in the epidermis of the palms of the hands and soles of the feet.
- The innermost layer of the epidermis is the stratum basale, which contains stem cells that divide to form new keratinocytes. The next layer is the stratum spinosum, which is the thickest layer and contains Langerhans cells and spiny keratinocytes. This is followed by the stratum granulosum, in which keratinocytes are filling with keratin and starting to die. The stratum lucidum is next, but only on the palms and soles. It consists of translucent dead keratinocytes. The outermost layer is the stratum corneum, which consists of flat, dead, tightly packed keratinocytes that form a tough, waterproof barrier for the rest of the epidermis.
- Functions of the epidermis include protecting underlying tissues from physical damage and pathogens. Melanin in the epidermis absorbs and protects underlying tissues from UV light. The epidermis also prevents loss of water from the body and synthesizes vitamin D.
- Melanin is the main pigment that determines the colour of human skin. The pigments carotene and hemoglobin, however, also contribute to skin colour, especially in skin with low levels of melanin.
- The surface of healthy skin normally is covered by vast numbers of bacteria representing about one thousand species from 19 phyla. Different areas of the body provide diverse habitats for skin microorganisms. Usually, microorganisms on the skin keep each other in check unless their balance is disturbed.
10.3 Review Questions
- What is the epidermis?
- Identify the types of cells in the epidermis.
- Describe the layers of the epidermis.
-
- State one function of each of the four epidermal layers found all over the body.
- Explain three ways the epidermis protects the body.
- What makes the skin waterproof?
- Why is the selective permeability of the epidermis both a benefit and a risk?
- How is vitamin D synthesized in the epidermis?
- Identify three pigments that impart colour to skin.
- Describe bacteria that normally reside on the skin, and explain why they do not usually cause infections.
- Explain why the keratinocytes at the surface of the epidermis are dead, while keratinocytes located deeper in the epidermis are still alive.
- Which layer of the epidermis contains keratinocytes that have begun to die?
-
- Explain why our skin is not permanently damaged if we rub off some of the surface layer by using a rough washcloth.
10.3 Explore More
https://www.youtube.com/watch?v=27lMmdmy-b8
Jonathan Eisen: Meet your microbes, TED, 2015.
https://www.youtube.com/watch?v=9AcQXnOscQ8
Why Do We Blush?, SciShow, 2014.
https://www.youtube.com/watch?v=_r4c2NT4naQ
The science of skin colour - Angela Koine Flynn, TED-Ed, 2016.
Attributions
Figure 10.3.1
Sunburn by QuinnHK at English Wikipedia on Wikimedia Commons is released into the public domain (https://en.wikipedia.org/wiki/Public_domain).
Figure 10.3.2
Blausen_0353_Epidermis by BruceBlaus on Wikimedia Commons is used under a CC BY 3.0 (https://creativecommons.org/licenses/by/3.0) license.
Figure 10.3.3
Isaac's scraped knee close-up by Alpha on Flickr is used under a CC BY-NC-SA 2.0 (https://creativecommons.org/licenses/by-nc-sa/2.0/) license.
Figure 10.3.4
Nicoderm by RegBarc on Wikimedia Commons is used under a CC BY-SA 3.0 (http://creativecommons.org/licenses/by-sa/3.0/) license. (No machine-readable author provided for original.)
Figure 10.3.5
Staphylococcus aureus bacteria, MRSA by Microbe World on Flickr is used under a CC BY-NC-SA 2.0 (https://creativecommons.org/licenses/by-nc-sa/2.0/) license.
References
Blausen.com staff. (2014). Medical gallery of Blausen Medical 2014. WikiJournal of Medicine 1 (2). DOI:10.15347/wjm/2014.010. ISSN 2002-4436.
Jeff Bone 'n' Pookie. (2020, July 19). Bill Nye the science guy explains we have different skin color. Youtube. https://www.youtube.com/watch?v=zOkj5jgC4sM&feature=youtu.be
SciShow. (2014, July 15). Why do we blush? YouTube. https://www.youtube.com/watch?v=9AcQXnOscQ8
TED. (2015, July 17). Jonathan Eisen: Meet your microbes. YouTube. https://www.youtube.com/watch?v=27lMmdmy-b8
TED-Ed. (2016, February 16). The science of skin color - Angela Koine Flynn. YouTube. https://youtu.be/_r4c2NT4naQ
Created by CK-12 Foundation/Adapted by Christine Miller

We All Scream for Ice Cream
If you’re an ice cream lover, then just the sight of this yummy ice cream cone may make your mouth water. The “water” in your mouth is actually saliva, a fluid released by glands that are part of the digestive system. Saliva contains digestive enzymes, among other substances important for digestion. When your mouth waters at the sight of a tasty treat, it’s a sign that your digestive system is preparing to digest food.
What Is the Digestive System?
The digestive system consists of organs that break down food, absorb its nutrients, and expel any remaining waste. Organs of the digestive system are shown in Figure 15.2.2. Most of these organs make up the gastrointestinal (GI) tract, through which food actually passes. The rest of the organs of the digestive system are called accessory organs. These organs secrete enzymes and other substances into the GI tract, but food does not actually pass through them.
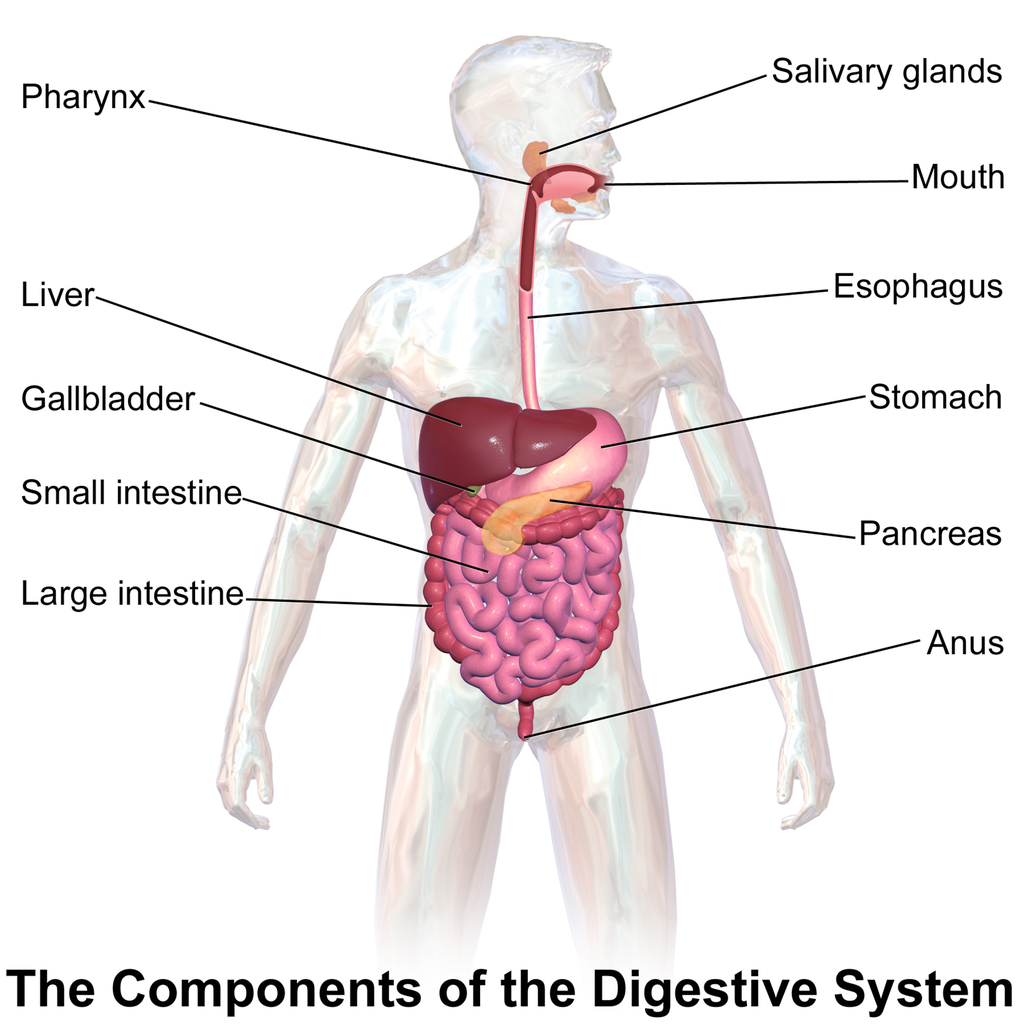
Functions of the Digestive System
The digestive system has three main functions relating to food: digestion of food, absorption of nutrients from food, and elimination of solid food waste. Digestion is the process of breaking down food into components the body can absorb. It consists of two types of processes: mechanical digestion and chemical digestion. Mechanical digestion is the physical breakdown of chunks of food into smaller pieces, and it takes place mainly in the mouth and stomach. Chemical digestion is the chemical breakdown of large, complex food molecules into smaller, simpler nutrient molecules that can be absorbed by body fluids (blood or lymph). This type of digestion begins in the mouth and continues in the stomach, but occurs mainly in the small intestine.
After food is digested, the resulting nutrients are absorbed. Absorption is the process in which substances pass into the bloodstream or lymph system to circulate throughout the body. Absorption of nutrients occurs mainly in the small intestine. Any remaining matter from food that is not digested and absorbed passes out of the body through the anus in the process of elimination.
Gastrointestinal Tract
The gastrointestinal (GI) tract is basically a long, continuous tube that connects the mouth with the anus. If it were fully extended, it would be about nine metres long in adults. It includes the mouth, pharynx, esophagus, stomach, and small and large intestines. Food enters the mouth, and then passes through the other organs of the GI tract, where it is digested and/or absorbed. Finally, any remaining food waste leaves the body through the anus at the end of the large intestine. It takes up to 50 hours for food or food waste to make the complete trip through the GI tract.
Tissues of the GI Tract
The walls of the organs of the GI tract consist of four different tissue layers, which are illustrated in Figure 15.2.3: mucosa, submucosa, muscularis externa, and serosa.
- The mucosa is the innermost layer surrounding the lumen (open space within the organs of the GI tract). This layer consists mainly of epithelium with the capacity to secrete and absorb substances. The epithelium can secret digestive enzymes and mucus, and it can absorb nutrients and water.
- The submucosa layer consists of connective tissue that contains blood and lymph vessels, as well as nerves. The vessels are needed to absorb and carry away nutrients after food is digested, and nerves help control the muscles of the GI tract organs.
- The muscularis externa layer contains two types of smooth muscle: longitudinal muscle and circular muscle. Longitudinal muscle runs the length of the GI tract organs, and circular muscle encircles the organs. Both types of muscles contract to keep food moving through the tract by the process of peristalsis, which is described below.
- The serosa layer is the outermost layer of the walls of GI tract organs. This is a thin layer that consists of connective tissue and separates the organs from surrounding cavities and tissues.
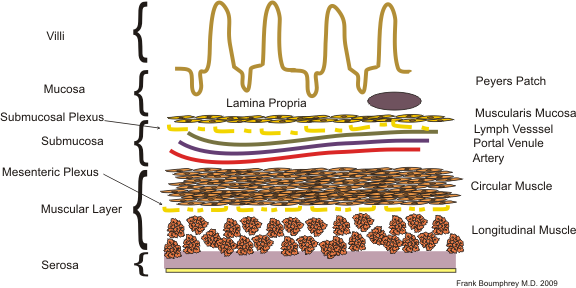 |
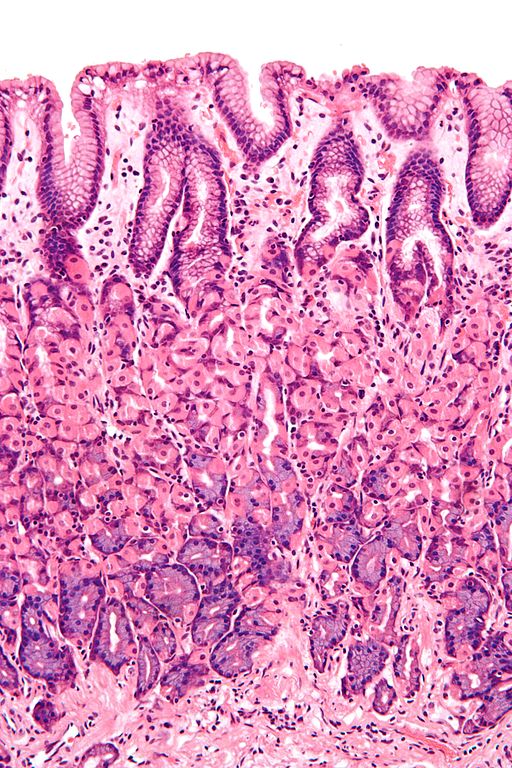 |
Peristalisis in the GI Tract
The muscles in the walls of GI tract organs enable peristalsis, which is illustrated in Figure 15.2.5. Peristalsis is a continuous sequence of involuntary muscle contraction and relaxation that moves rapidly along an organ like a wave, similar to the way a wave moves through a spring toy. Peristalsis in organs of the GI tract propels food through the tract.
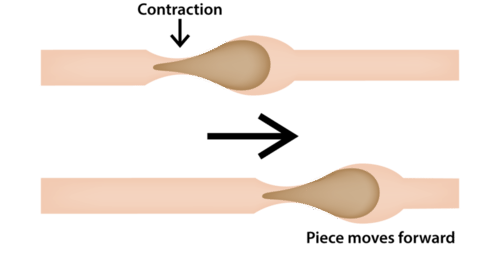
Watch the video "What is peristalsis?" by Mister Science to see peristalsis in action:
https://youtu.be/kVjeNZA5pi4
What is peristalsis?, Mister Science, 2018.
Immune Function of the GI Tract
The GI tract plays an important role in protecting the body from pathogens. The surface area of the GI tract is estimated to be about 32 square metres (105 square feet), or about half the area of a badminton court. This is more than three times the area of the exposed skin of the body, and it provides a lot of area for pathogens to invade the tissues of the body. The innermost mucosal layer of the walls of the GI tract provides a barrier to pathogens so they are less likely to enter the blood or lymph circulations. The mucus produced by the mucosal layer, for example, contains antibodies that mark many pathogenic microorganisms for destruction. Enzymes in some of the secretions of the GI tract also destroy pathogens. In addition, stomach acids have a very low pH that is fatal for many microorganisms that enter the stomach.
Divisions of the GI Tract
The GI tract is often divided into an upper GI tract and a lower GI tract. For medical purposes, the upper GI tract is typically considered to include all the organs from the mouth through the first part of the small intestine, called the duodenum. For our instructional purposes, it makes more sense to include the mouth through the stomach in the upper GI tract, and all of the small intestine — as well as the large intestine — in the lower GI tract.
Upper GI Tract
The mouth is the first digestive organ that food enters. The sight, smell, or taste of food stimulates the release of digestive enzymes and other secretions by salivary glands inside the mouth. The major salivary gland enzyme is amylase. It begins the chemical digestion of carbohydrates by breaking down starches into sugar. The mouth also begins the mechanical digestion of food. When you chew, your teeth break, crush, and grind food into increasingly smaller pieces. Your tongue helps mix the food with saliva and also helps you swallow.
A lump of swallowed food is called a bolus. The bolus passes from the mouth into the pharynx, and from the pharynx into the esophagus. The esophagus is a long, narrow tube that carries food from the pharynx to the stomach. It has no other digestive functions. Peristalsis starts at the top of the esophagus when food is swallowed and continues down the esophagus in a single wave, pushing the bolus of food ahead of it.
From the esophagus, food passes into the stomach, where both mechanical and chemical digestion continue. The muscular walls of the stomach churn and mix the food, thus completing mechanical digestion, as well as mixing the food with digestive fluids secreted by the stomach. One of these fluids is hydrochloric acid (HCl). In addition to killing pathogens in food, it gives the stomach the low pH needed by digestive enzymes that work in the stomach. One of these enzymes is pepsin, which chemically digests proteins. The stomach stores the partially digested food until the small intestine is ready to receive it. Food that enters the small intestine from the stomach is in the form of a thick slurry (semi-liquid) called chyme.
Lower GI Tract
The small intestine is a narrow, but very long tubular organ. It may be almost seven metres long in adults. It is the site of most chemical digestion and virtually all absorption of nutrients. Many digestive enzymes are active in the small intestine, some of which are produced by the small intestine itself, and some of which are produced by the pancreas, an accessory organ of the digestive system. Much of the inner lining of the small intestine is covered by tiny finger-like projections called villi, each of which is covered by even tinier projections called microvilli. These projections, shown in the drawing below (Figure 15.2.6), greatly increase the surface area through which nutrients can be absorbed from the small intestine.
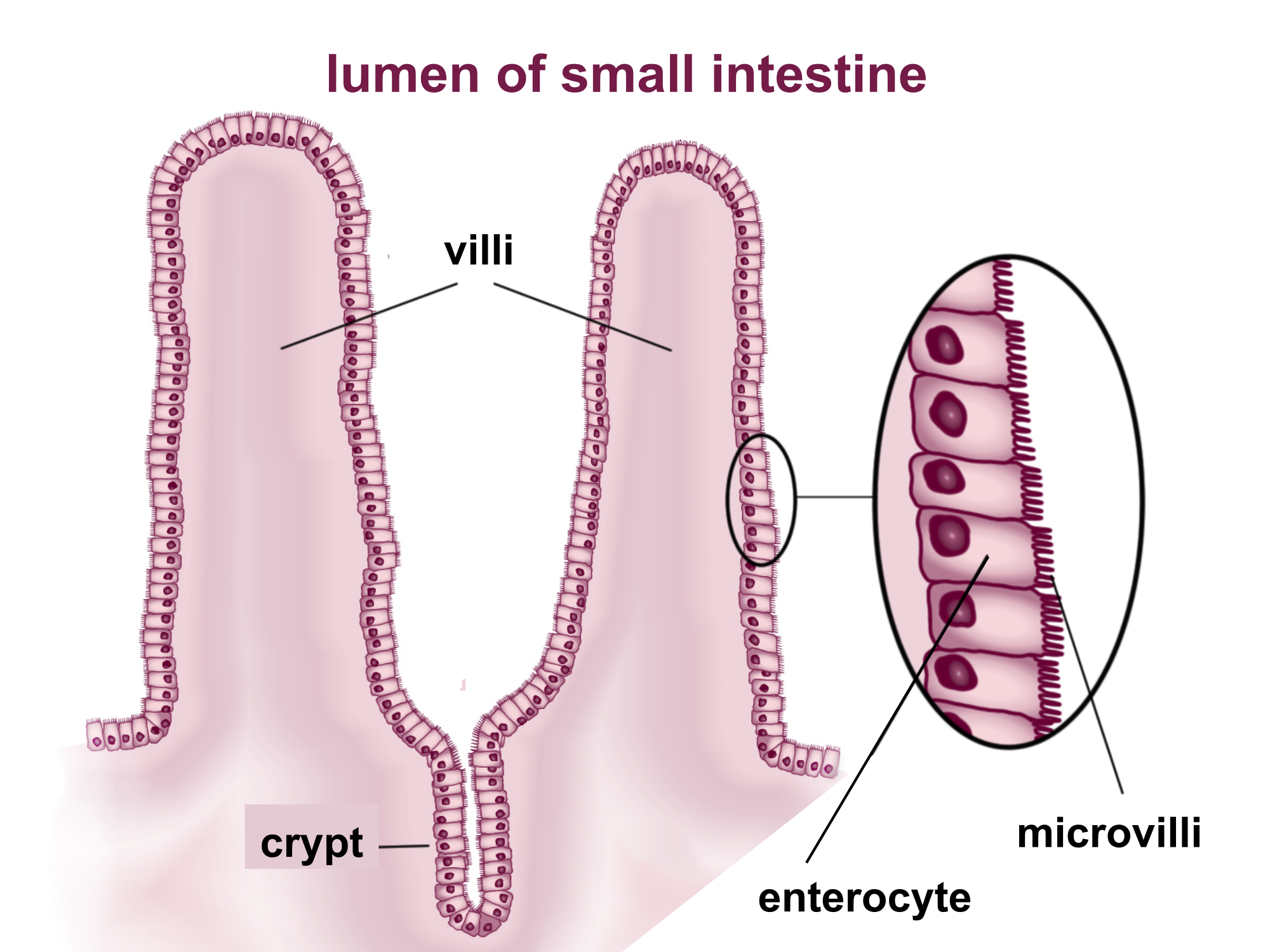
From the small intestine, any remaining nutrients and food waste pass into the large intestine. The large intestine is another tubular organ, but it is wider and shorter than the small intestine. It connects the small intestine and the anus. Waste that enters the large intestine is in a liquid state. As it passes through the large intestine, excess water is absorbed from it. The remaining solid waste — called feces — is eventually eliminated from the body through the anus.
Accessory Organs of the Digestive System
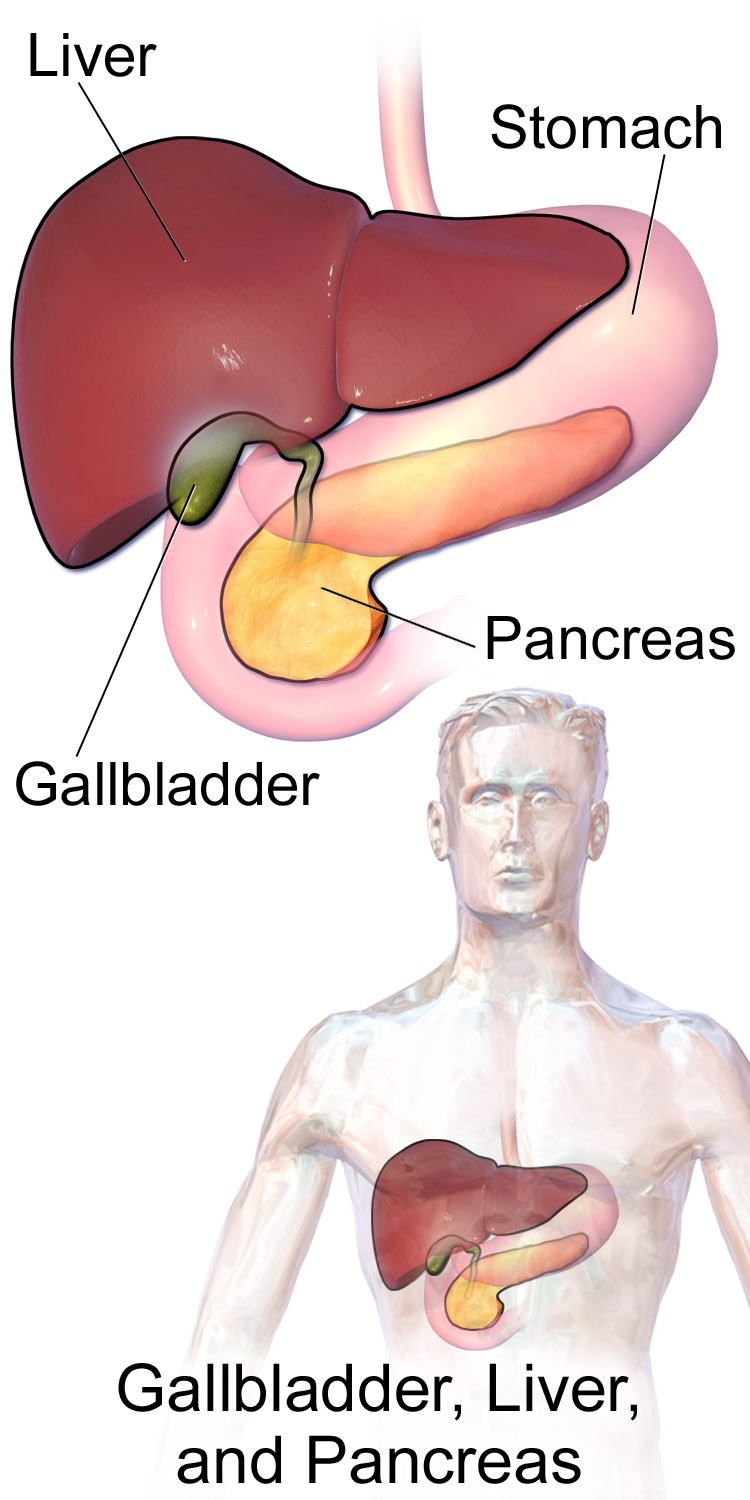
Accessory organs of the digestive system are not part of the GI tract, so they are not sites where digestion or absorption take place. Instead, these organs secrete or store substances needed for the chemical digestion of food. The accessory organs include the liver, gallbladder, and pancreas. They are shown in Figure 15.2.7 and described in the text that follows.
- The liver is an organ with multitude of functions. Its main digestive function is producing and secreting a fluid called bile, which reaches the small intestine through a duct. Bile breaks down large globules of lipids into smaller ones that are easier for enzymes to chemically digest. Bile is also needed to reduce the acidity of food entering the small intestine from the highly acidic stomach, because enzymes in the small intestine require a less acidic environment in order to work.
- The gallbladder is a small sac below the liver that stores some of the bile from the liver. The gallbladder also concentrates the bile by removing some of the water from it. It then secretes the concentrated bile into the small intestine as needed for fat digestion following a meal.
- The pancreas secretes many digestive enzymes, and releases them into the small intestine for the chemical digestion of carbohydrates, proteins, and lipids. The pancreas also helps lessen the acidity of the small intestine by secreting bicarbonate, a basic substance that neutralizes acid.
15.2 Summary
- The digestive system consists of organs that break down food, absorb its nutrients, and expel any remaining food waste.
- Digestion is the process of breaking down food into components that the body can absorb. It includes mechanical digestion and chemical digestion. Absorption is the process of taking up nutrients from food by body fluids for circulation to the rest of the body. Elimination is the process of excreting any remaining food waste after digestion and absorption are finished.
- Most digestive organs form a long, continuous tube called the gastrointestinal (GI) tract. It starts at the mouth, which is followed by the pharynx, esophagus, stomach, small intestine, and large intestine. The upper GI tract consists of the mouth through the stomach, while the lower GI tract consists of the small and large intestines.
- Digestion and/or absorption take place in most of the organs of the GI tract. Organs of the GI tract have walls that consist of several tissue layers that enable them to carry out these functions. The inner mucosa has cells that secrete digestive enzymes and other digestive substances, as well as cells that absorb nutrients. The muscle layer of the organs enables them to contract and relax in waves of peristalsis to move food through the GI tract.
- Three digestive organs — the liver, gallbladder, and pancreas — are accessory organs of digestion. They secrete substances needed for chemical digestion into the small intestine.
15.2 Review Questions
- What is the digestive system?
- What are the three main functions of the digestive system? Define each function.
-
- Relate the tissues in the walls of GI tract organs to the functions the organs perform.
15.2 Explore More
https://youtu.be/Og5xAdC8EUI
How your digestive system works - Emma Bryce, TED-Ed, 2017.
https://youtu.be/YVfyYrEmzgM
How does your body know you're full? - Hilary Coller, TED-Ed, 2017.
Attributions
Figure 15.2.1
Ice Cream [photo] by Mark Cruz on Unsplash is used under the Unsplash License (https://unsplash.com/license).
Figure 15.2.2
Blausen_0316_DigestiveSystem by BruceBlaus on Wikimedia Commons is used under a CC BY 3.0 (https://creativecommons.org/licenses/by/3.0) license.
Figure 15.2.3
Intestinal_layers by Boumphreyfr on Wikimedia Commons is used under a CC BY-SA 3.0 (https://creativecommons.org/licenses/by-sa/3.0) license.
Figure 15.2.4
512px-Normal_gastric_mucosa_intermed_mag by Nephron on Wikimedia Commons is used under a CC BY-SA 3.0 (https://creativecommons.org/licenses/by-sa/3.0) license.
Figure 15.2.5
Peristalsis pushes food through the GI tract by CK-12 Foundation is used under a CC BY NC 3.0 (https://creativecommons.org/licenses/by-nc/3.0/) license.
Figure 15.2.6
Villi_&_microvilli_of_small_intestine.svg by BallenaBlanca on Wikimedia Commons is used under a CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0) license.
Figure 15.2.7
Blausen_0428_Gallbladder-Liver-Pancreas_Location by BruceBlaus on Wikimedia Commons is used under a CC BY 3.0 (https://creativecommons.org/licenses/by/3.0) license.
References
Blausen.com Staff. (2014). Medical gallery of Blausen Medical 2014. WikiJournal of Medicine 1 (2). DOI:10.15347/wjm/2014.010. ISSN 2002-4436.
Brainard, J/ CK-12 Foundation. (2016). Figure 4 Peristalsis pushes food through the GI tract. [digital image]. In CK-12 College Human Biology (Section 17.2) [online Flexbook]. CK12.org. https://www.ck12.org/book/ck-12-college-human-biology/section/17.2/
Mister Science. (2018). What is peristalsis? YouTube. https://www.youtube.com/channel/UCxTlkZfjArUobBAeVwzJjYg/videos
TED-Ed. (2017, November 13). How does your body know you're full? - Hilary Coller. YouTube. https://www.youtube.com/watch?v=YVfyYrEmzgM&feature=youtu.be
TED-Ed. (2017, December 14). How your digestive system works - Emma Bryce. YouTube. https://www.youtube.com/watch?v=Og5xAdC8EUI&feature=youtu.be
Created by CK-12 Foundation/Adapted by Christine Miller

A Shot in the Arm
Giving yourself an injection can be difficult, but for someone with diabetes, it may be a matter of life or death. The person in the photo has diabetes and is injecting themselves with insulin, the hormone that helps control the level of glucose in the blood. Insulin is produced by the pancreas.
Introduction to the Pancreas
The pancreas is a large gland located in the upper left abdomen behind the stomach, as shown in Figure 9.7.2. The pancreas is about 15 cm (6 in) long, and it has a flat, oblong shape. Structurally, the pancreas is divided into a head, body, and tail. Functionally, the pancreas serves as both an endocrine gland and an exocrine gland.
- As an endocrine gland, the pancreas is part of the endocrine system. As such, it releases hormones (such as insulin) directly into the bloodstream for transport to cells throughout the body.
- As an exocrine gland, the pancreas is part of the digestive system. As such, it releases digestive enzymes into ducts that carry the enzymes to the gastrointestinal tract, where they assist with digestion. In this concept, the focus is on the pancreas as an endocrine gland. You can read about the pancreas as an exocrine gland in Chapter 15 Digestive System.
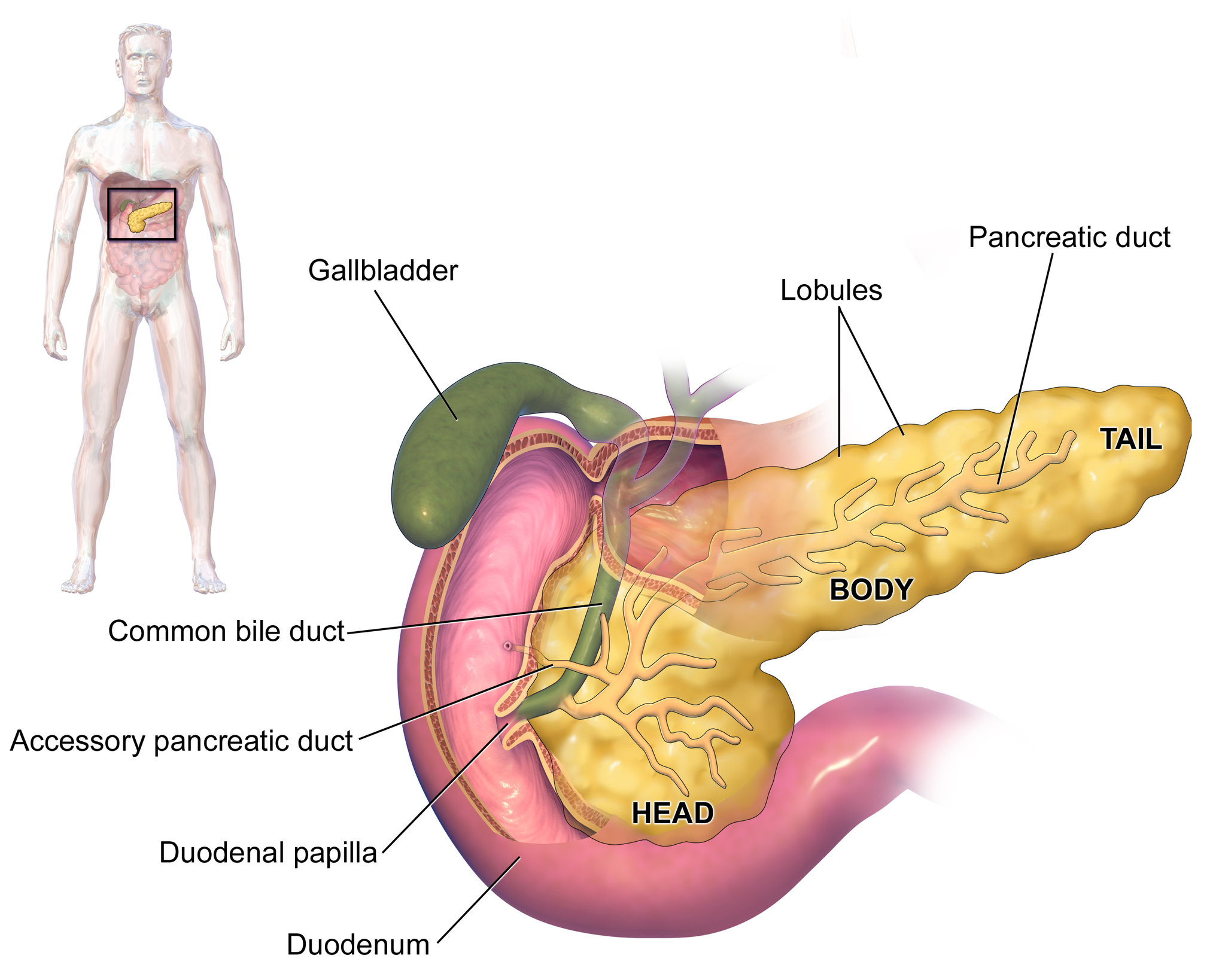
The Pancreas as an Endocrine Gland
The tissues within the pancreas that have an endocrine role exist as clusters of cells called pancreatic islets. They are also called the islets of Langerhans. You can see pancreatic tissue, including islets, in Figure 9.7.3. There are approximately three million pancreatic islets, and they are crisscrossed by a dense network of capillaries. The capillaries are lined by layers of islet cells that have direct contact with the blood vessels, into which they secrete their endocrine hormones.
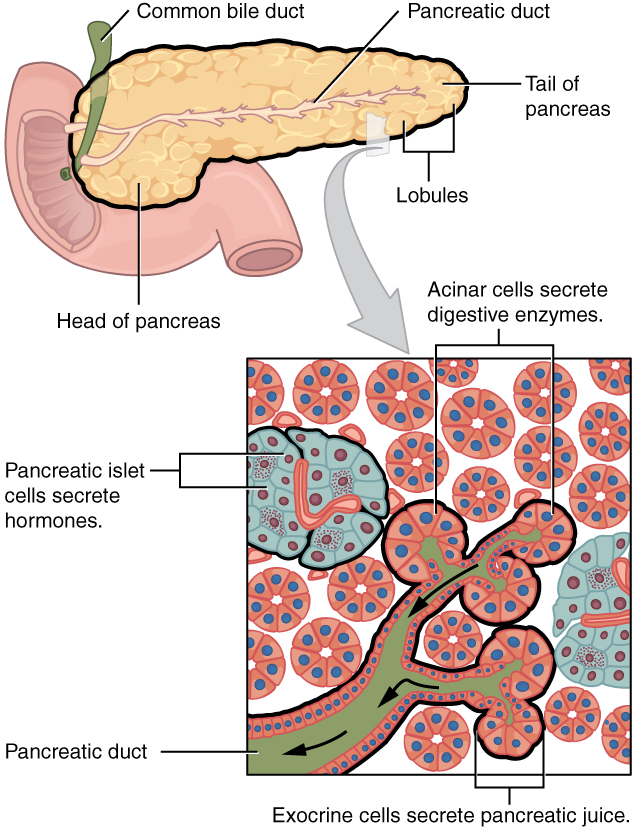
The pancreatic islets consist of four main types of cells, each of which secretes a different endocrine hormone. All of the hormones produced by the pancreatic islets, however, play crucial roles in glucose metabolism and the regulation of blood glucose levels, among other functions.
- Islet cells called alpha (α) cells secrete the hormone glucagon. The function of glucagon is to increase the level of glucose in the blood. It does this by stimulating the liver to convert stored glycogen into glucose, which is released into the bloodstream.
- Islets cells called beta (β) cells secrete the hormone insulin. The function of insulin is to decrease the level of glucose in the blood. It does this by promoting the absorption of glucose from the blood into fat, liver, and skeletal muscle cells. In these tissues, the absorbed glucose is converted into glycogen, fats (triglycerides), or both.
- Islet cells called delta (δ) cells secrete the hormone somatostatin. This hormone is also called growth hormone inhibiting hormone, because it inhibits the anterior lobe of the pituitary gland from producing growth hormone. Somatostatin also inhibits the secretion of pancreatic endocrine hormones and pancreatic exocrine enzymes.
- Islet cells called gamma (γ) cells secrete the hormone pancreatic polypeptide. The function of pancreatic polypeptide is to help regulate the secretion of both endocrine and exocrine substances by the pancreas.
Disorders of the Pancreas
There are a variety of disorders that affect the pancreas. They include pancreatitis, pancreatic cancer, and diabetes mellitus.
Pancreatitis

Pancreatitis is inflammation of the pancreas. It has a variety of possible causes, including gallstones, chronic alcohol use, infections (such as measles or mumps), and certain medications. Pancreatitis occurs when digestive enzymes produced by the pancreas damage the gland’s tissues, which causes problems with fat digestion. The disorder is usually associated with intense pain in the central abdomen, and the pain may radiate to the back. Yellowing of the skin and whites of the eyes (see Figure 9.7.4), which is called jaundice, is a common sign of pancreatitis. People with pancreatitis may also have pale stools and dark urine. Treatment of pancreatitis includes administering drugs to manage pain, and addressing the underlying cause of the disease, for example, by removing gallstones.
Pancreatic Cancer
There are several different types of pancreatic cancer that may affect either the endocrine or the exocrine tissues of the gland. Cancers affecting the endocrine tissues are all relatively rare. However, their incidence has been rising sharply. It is unclear to what extent this reflects increased detection, especially through medical imaging techniques. Unfortunately, pancreatic cancer is usually diagnosed at a relatively late stage when it is too late for surgery, which is the only way to cure the disorder. In 2020 it is estimated that 6,000 Canadians will be newly diagnosed with pancreatic cancer, and that during this same year, 5,300 will die of pancreatic cancer.
While it is rare before the age of 40, pancreatic cancer occurs most often after the age of 60. Factors that increase the risk of developing pancreatic cancer include smoking, obesity, diabetes, and a family history of the disease. About one in four cases of pancreatic cancer are attributable to smoking. Certain rare genetic conditions are also risk factors for pancreatic cancer.
Diabetes Mellitus
By far the most common type of pancreatic disorder is diabetes mellitus, more commonly called simply diabetes. There are many different types of diabetes, but diabetes mellitus is the most common. It occurs in two major types, type 1 diabetes and type 2 diabetes. The two types have different causes and may also have different treatments, but they generally produce the same initial symptoms, which include excessive urination and thirst. These symptoms occur because the kidneys excrete more urine in an attempt to rid the blood of excess glucose. Loss of water in urine stimulates greater thirst. Other signs and symptoms of diabetes are listed in Figure 9.7.5.
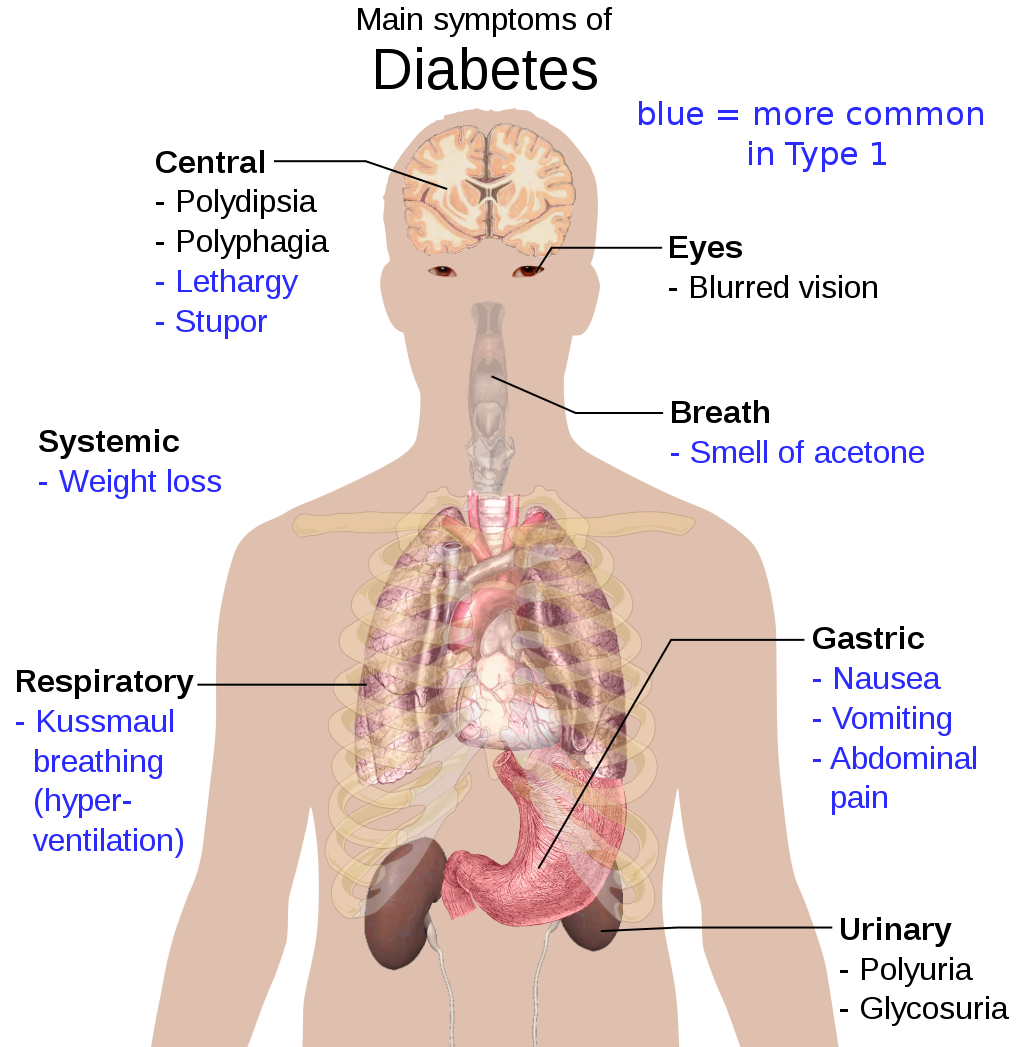
When diabetes is not well controlled, it is likely to have several serious long-term consequences. Most of these consequences are due to damage to small blood vessels caused by high glucose levels in the blood. Damage to blood vessels, in turn, may lead to increased risk of coronary artery disease and stroke. Damage to blood vessels in the retina of the eye can result in gradual vision loss and blindness. Damage to blood vessels in the kidneys can lead to chronic kidney disease, sometimes requiring dialysis or kidney transplant. Long-term consequences of diabetes may also include damage to the nerves of the body, known as diabetic neuropathy. In fact, this is the most common complication of diabetes. Symptoms of diabetic neuropathy may include numbness, tingling, and pain in the extremities.
Type 1 Diabetes
Type 1 diabetes is a chronic autoimmune disorder in which the immune system attacks the insulin-secreting beta cells of the pancreas. As a result, people with type 1 diabetes lack the insulin needed to keep blood glucose levels within the normal range. Type 1 diabetes may develop in people of any age, but is most often diagnosed before adulthood. For type 1 diabetics, insulin injections are critical for survival.
Type 2 Diabetes
Type 2 diabetes is the single most common form of diabetes. The cause of high blood glucose in this form of diabetes usually includes a combination of insulin resistance and impaired insulin secretion. Both genetic and environmental factors play roles in the development of type 2 diabetes. Type 2 diabetes can be managed with changes in diet and physical activity, which may increase insulin sensitivity and help reduce blood glucose levels to normal ranges. Medications may also be used as part of the treatment, as may insulin injections.
Feature: Human Biology in the News
Some patients with type 1 diabetes have been given pancreatic islet cells transplants from other human donors. If the transplanted cells are not rejected by the recipient’s immune system, they can cure the patient of diabetes. However, because of a shortage of appropriate human donors, only about one thousand such surgeries have been performed over the past ten years.
In June of 2016, a research team led by Dr. David K.C. Cooper at the Thomas E. Starzl Transplantation Institute in Pittsburgh, Pennsylvania, reported on their work developing pig islet cells for transplant into human diabetes patients. The researchers genetically engineered the pig islet cells to be protected from the human immune response. As a result, patients receiving the transplanted cells would require only minimal suppression of their immune system after the surgery. The pig islet cells would also be less likely to transmit pathogenic agents, because the animals could be raised in a controlled environment.
The researchers have successfully transplanted the pig islet cells into monkey models of type 1 diabetes. As of June 2016, the scientists were looking for funding to undertake clinical trials in humans with type 1 diabetes. Dr. Cooper predicted then that if the human trials go as well as expected, the pig islet cells could be available for curing patients in as little as two years.
9.7 Summary
- The pancreas is a gland located in the upper left abdomen behind the stomach that functions as both an endocrine gland and an exocrine gland. As an endocrine gland, the pancreas releases hormones (such as insulin) directly into the bloodstream. As an exocrine gland, the pancreas releases digestive enzymes into ducts that carry them to the gastrointestinal tract.
- Tissues in the pancreas that have an endocrine role exist as clusters of cells called pancreatic islets. The islets consist of four main types of cells, each of which secretes a different endocrine hormone. Alpha (α) cells secrete glucagon, beta (β) cells secrete insulin, delta (δ) cells secrete somatostatin, and gamma (γ) cells secrete pancreatic polypeptide.
- The endocrine hormones secreted by the pancreatic islets all play a role, either directly or indirectly, in glucose metabolism and homeostasis of blood glucose levels. For example, insulin stimulates the uptake of glucose by cells and decreases the level of glucose in the blood, whereas glucagon stimulates the conversion of glycogen to glucose and increases the level of glucose in the blood.
- Disorders of the pancreas include pancreatitis, pancreatic cancer, and diabetes mellitus. Pancreatitis is painful inflammation of the pancreas that has many possible causes. Pancreatic cancer of the endocrine tissues is rare, but increasing in frequency. It is generally discovered too late to cure surgically. Smoking is a major risk factor for pancreatic cancer.
- Diabetes mellitus is the most common type of pancreatic disorder. In diabetes, inadequate activity of insulin results in high blood levels of glucose. Type 1 diabetes is a chronic autoimmune disorder in which the immune system attacks the insulin-secreting beta cells of the pancreas. Type 2 diabetes is usually caused by a combination of insulin resistance and impaired insulin secretion due to a variety of environmental and genetic factors.
9.7 Review Questions
- Describe the structure and location of the pancreas.
- Distinguish between the endocrine and exocrine functions of the pancreas.
-
-
- What is pancreatitis? What are possible causes and effects of pancreatitis?
- Describe the incidence, prognosis, and risk factors of cancer of the endocrine tissues of the pancreas.
- Compare and contrast type 1 and type 2 diabetes.
- If the alpha islet cells of the pancreas were damaged to the point that they no longer functioned, how would this affect blood glucose levels? Assume that no outside regulation of this system is occurring and explain your answer. Further, would administration of insulin be more likely to help or hurt this condition? Explain your answer.
- Explain why diabetes causes excessive thirst.
9.7 Explore More
https://www.youtube.com/watch?v=8dgoeYPoE-0&t=2s
What does the pancreas do? - Emma Bryce, TED-Ed, 2015.
https://www.youtube.com/watch?v=qlzLSbAGMqA&feature=emb_logo
Type 2 diabetes in children, Children's Health, 2008.
https://www.youtube.com/watch?v=da1vvigy5tQ
Reversing Type 2 diabetes starts with ignoring the guidelines | Sarah Hallberg | TEDxPurdueU, TEDx Talks, 2015.
Attributions
Figure 9.7.1
Insulin_Application by Mr Hyde at Czech Wikipedia (Original text: moje foto) on Wikimedia Commons is released into the public domain (https://en.wikipedia.org/wiki/Public_domain).
Figure 9.7.2
Blausen_0699_PancreasAnatomy2 by BruceBlaus on Wikimedia Commons is used under a CC BY 3.0 (https://creativecommons.org/licenses/by/3.0) license.
Figure 9.7.3
Exocrine_and_Endocrine_Pancreas by OpenStax College is used under a CC BY 3.0 (https://creativecommons.org/licenses/by/3.0/deed.en) license.
Figure 9.7.4
Jaundice_eye_new by Info-farmer on Wikimedia Commons is in the public domain (https://en.wikipedia.org/wiki/Public_domain). (Original image, File:Jaundice eye.jpg, is from Centers for Disease Control and Prevention's Public Health Image Library (PHIL), with identification number #2860)
Figure 9.7.5
Main_symptoms_of_diabetes.svg by Mikael Häggström on Wikimedia Commons is released into the public domain (https://en.wikipedia.org/wiki/Public_domain).
Betts, J. G., Young, K.A., Wise, J.A., Johnson, E., Poe, B., Kruse, D.H., Korol, O., Johnson, J.E., Womble, M., DeSaix, P. (2013, July 19). Figure 23.26 Exocrine and endocrine pancreas [digital image]. In Anatomy and Physiology (Section 23.6). OpenStax. https://openstax.org/books/anatomy-and-physiology/pages/23-6-accessory-organs-in-digestion-the-liver-pancreas-and-gallbladder
Blausen.com Staff. (2014). Medical gallery of Blausen Medical 2014. WikiJournal of Medicine 1 (2). DOI:10.15347/wjm/2014.010. ISSN 2002-4436.
Children's Health. (2008, June 13). Type 2 diabetes in children. YouTube. https://www.youtube.com/watch?v=qlzLSbAGMqA&feature=youtu.be
, , , , , , . (2016, March 4). First update of the International Xenotransplantation Association consensus statement on conditions for undertaking clinical trials of porcine islet products in type 1 diabetes—Executive summary. Xenotransplantation 2016, 23: 3– 13. https://doi.org/10.1111/xen.12231
TED-Ed. (2015, February 19). What does the pancreas do? - Emma Bryce. YouTube. https://www.youtube.com/watch?v=8dgoeYPoE-0&feature=youtu.be
TEDx Talks. (2015, May 4). Reversing Type 2 diabetes starts with ignoring the guidelines | Sarah Hallberg | TEDxPurdueU. YouTube. https://www.youtube.com/watch?v=da1vvigy5tQ&feature=youtu.be
Created by CK-12 Foundation/Adapted by Christine Miller

Head Stand
Did you ever wonder what would happen if you tried to swallow food while standing on your head like this person in Figure 15.4.1? Many people think that food travels down the gullet from the mouth by the force of gravity. If that were the case, then food you swallowed would stay in your throat while you were standing on your head. In reality, your position doesn’t have much to do with your ability to swallow. Food will travel from your mouth to your stomach whether you are standing upright or upside down. That’s because the tube the food travels through — the esophagus — moves the food along via muscular contractions known as peristalsis. The esophagus is one of several organs that make up the upper gastrointestinal tract.
Organs of the Upper Gastrointestinal Tract
Besides the esophagus, organs of the upper gastrointestinal (GI) tract include the mouth, pharynx, and stomach. These hollow organs are all connected to form a tube through which food passes during digestion. The only role in digestion played by the pharynx and esophagus is to move food through the GI tract. The mouth and stomach, in contrast, are organs where digestion — or the breakdown of food — also occurs. In both of these organs, food is broken into smaller pieces (mechanical digestion), as well as broken down chemically (chemical digestion). It should be noted that the first part of the small intestine (duodenum) is considered in some contexts to be part of the upper GI tract, but that practice is not followed here.
Mouth
The mouth is the first organ of the GI tract. Most of the oral cavity is lined with mucous membrane. This tissue produces mucus, which helps moisten, soften, and lubricate food. Underlying the mucous membrane is a thin layer of smooth muscle to which the mucous membrane is only loosely connected. This gives the mucous membrane considerable ability to stretch as you eat food. The roof of the mouth, called the palate, separates the oral cavity from the nasal cavity. The front part is hard, consisting of mucous membrane covering a plate of bone. The back part of the palate is softer and more pliable, consisting of mucous membrane over muscle and connective tissue. The hard surface of the front of the palate allows for pressure needed in chewing and mixing food. The soft, pliable surface of the back of the palate can move to accommodate the passage of food while swallowing. Muscles at either side of the soft palate contract to create the swallowing action.
Several specific structures in the mouth are specialized for digestion. These include salivary glands, tongue, and teeth.
Salivary Glands
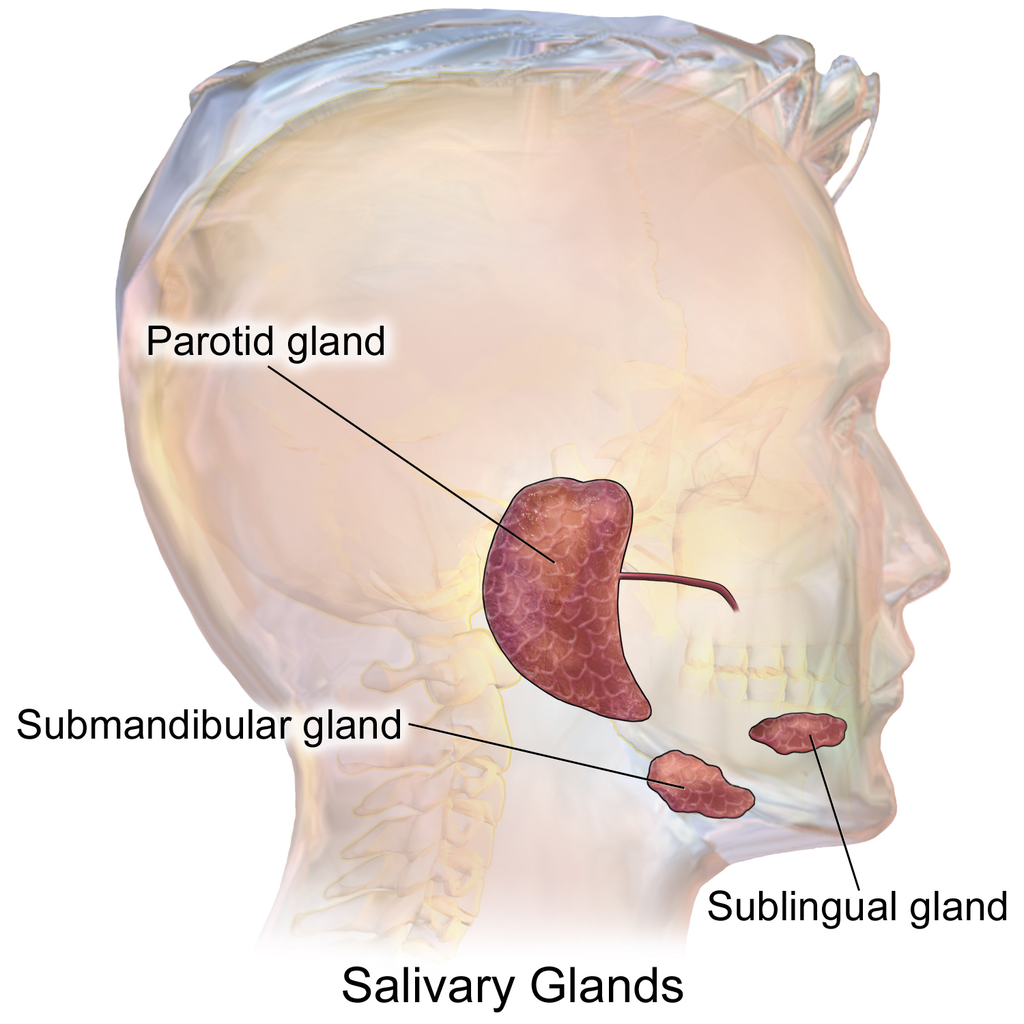
The mouth contains three pairs of major salivary glands, shown in Figure 15.4.2. These three pairs are all exocrine glands that secrete saliva into the mouth through ducts.
- The largest of the three major pairs of salivary glands are the parotid glands, which are located on either side of the mouth in front of the ears.
- The next largest pair is the submandibular glands, located beneath the lower jaw.
- The third pair is the sublingual glands, located underneath the tongue.
In addition to these three pairs of major salivary glands, there are also hundreds of minor salivary glands in the oral mucosa lining the mouth and on the tongue. Along with the major glands, most of the minor glands secrete the digestive enzyme amylase, which begins the chemical digestion of starch and glycogen (polysaccharides). However, the minor salivary glands on the tongue secrete the fat-digesting enzyme lipase, which in the mouth is called lingual lipase (to distinguish it from pancreatic lipase secreted by the pancreas).
Saliva secreted by the salivary glands mainly helps digestion, but it also plays other roles. It helps maintain dental health by cleaning the teeth, and it contains antibodies that help protect against infection. By keeping the mouth lubricated, saliva also allows the mouth movements needed for speech.
Tongue
The tongue is a fleshy, muscular organ that is attached to the floor of the mouth by a band of ligaments that gives it great mobility. This is necessary so the tongue can manipulate food for chewing and swallowing. Movements of the tongue are also necessary for speaking. The upper surface of the tongue is covered with tiny projections called papillae, which contain taste buds. The latter are collections of chemoreceptor cells (shown in Figure 15.4.3). These sensory cells sense chemicals in food and send the information to the brain via cranial nerves, thus enabling the sense of taste.
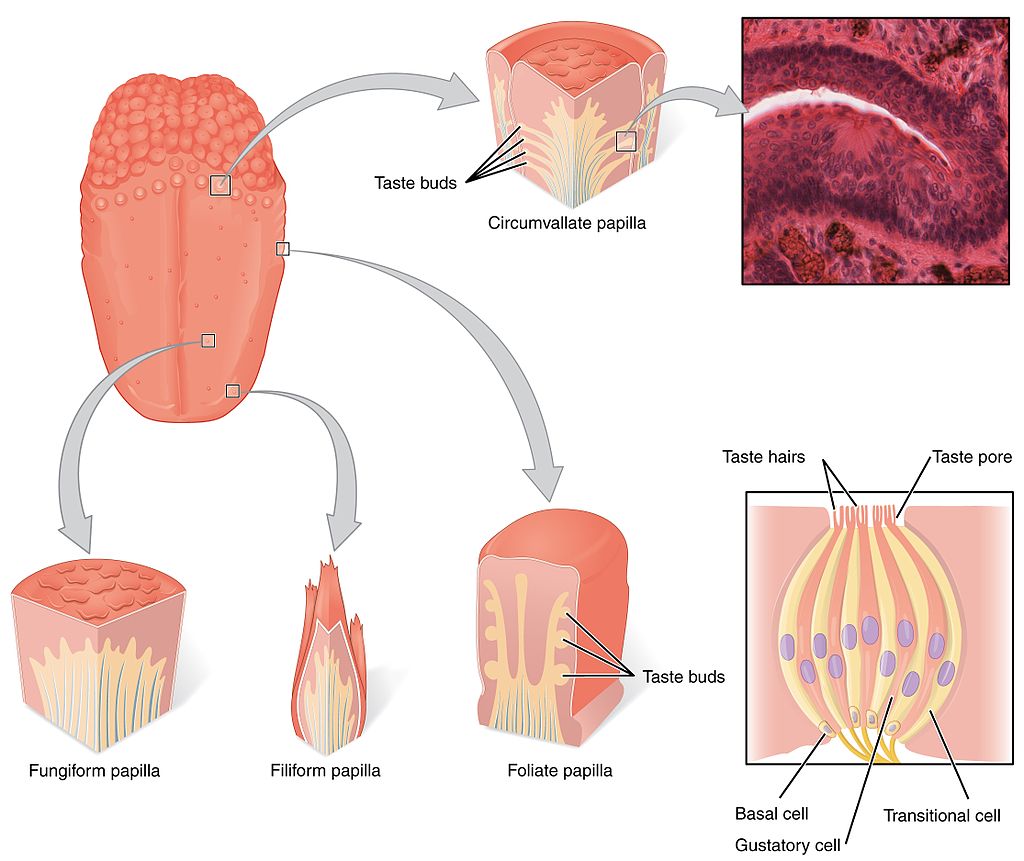
There are five basic tastes detected by the chemoreceptor cells in taste buds: saltiness, sourness, bitterness, sweetness, and umami (often described as a meaty taste). Contrary to popular belief, taste buds for the five basic tastes are not located on different parts of the tongue. Why does taste matter? The taste of food helps to stimulate the secretion of saliva from the salivary glands. It also helps us to eat foods that are good for us, instead of rotten or toxic foods. The detection of saltiness, for example, enables the control of salt intake and salt balance in the body. The detection of sourness may help us avoid spoiled foods, which often taste sour due to fermentation by bacteria. The detection of bitterness warns of poisons, because many plants defend themselves with toxins that taste bitter. The detection of sweetness guides us to foods that supply quick energy. The detection of umami may signal protein-rich foods.
Teeth
The teeth are complex structures made of a bone-like material called dentin and covered with enamel, which is the hardest tissue in the body. Adults normally have a total of 32 teeth, with 16 in each jaw. The right and left sides of each jaw are mirror images in terms of the numbers and types of teeth they contain. Teeth have different shapes to suit them for different aspects of mastication (chewing). The different types of teeth are illustrated in Figure 15.4.4.
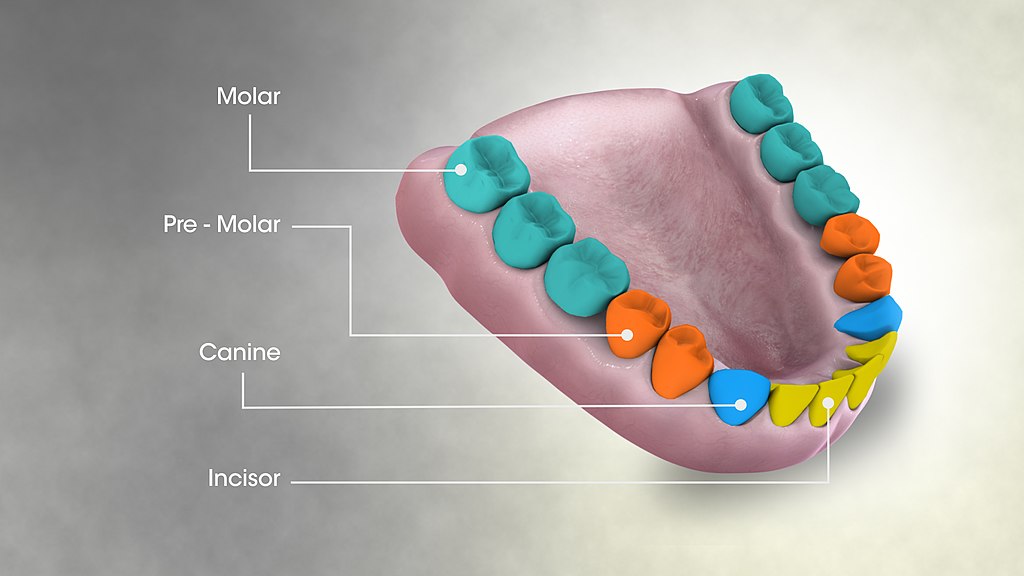
- Incisors are the sharp, blade-like teeth at the front of the mouth. They are used for cutting or biting off pieces of food. In adults, there are normally four incisors in each jaw, or eight in total.
- Canines are the pointed teeth on either side of the incisors. They are used for tearing foods that are tough or stringy. Adults normally have two canines in each jaw, or four altogether.
- Premolars and molars are cuboid teeth with cusps and grooves that are located on the sides and toward the back of the jaws. Premolars are closer to the front of the mouth. Molars are larger and have more cusps than premolars, but both are used for crushing and grinding food. Adults normally have two premolars and three molars on each side of each jaw, for a total of eight premolars and twelve molars.
Pharynx
The tube-like pharynx (see Figure 15.4.5 below) plays a dual role as an organ of both respiration and digestion. As part of the respiratory system, it conducts air between the nasal cavity and larynx. As part of the digestive system, it allows swallowed food to pass from the oral cavity to the esophagus. Anything swallowed has priority over inhaled air when passing through the pharynx. During swallowing, the backward motion of the tongue causes a flap of elastic cartilage — called the epiglottis — to close over the opening to the larynx. This prevents food or drink from entering the larynx.
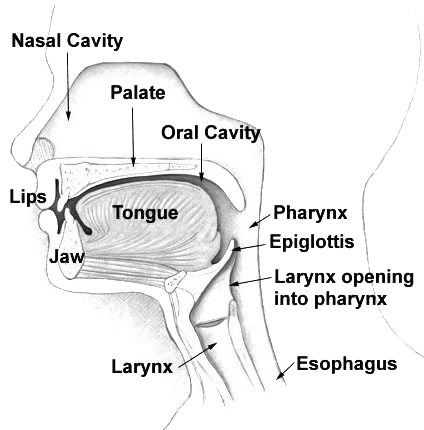
Esophagus
The esophagus (shown in Figure 15.4.6) is a muscular tube through which food is pushed from the pharynx to the stomach. The esophagus passes through an opening in the diaphragm (the large breathing muscle that separates the abdomen from the thorax) before reaching the stomach. In adults, the esophagus averages about 25 cm (about 9.8 inches) in length, depending on a person’s height. The inner lining of the esophagus consists of mucous membrane, which provides a smooth, slippery surface for the passage of food. The cells of this membrane are constantly being replaced as they are worn away from the frequent passage of food over them.
When food is not being swallowed, the esophagus is closed at both ends by upper and lower esophageal sphincters. Sphincters are rings of muscle that can contract to close off openings between structures. The upper esophageal sphincter is triggered to relax and open by the act of swallowing, allowing a bolus of food to enter the esophagus from the pharynx. Then, the esophageal sphincter closes again to prevent food from moving back into the pharynx from the esophagus.
Once in the esophagus, the food bolus travels down to the stomach, pushed along by the rhythmic contraction and relaxation of muscles (peristalsis). The lower esophageal sphincter is located at the junction between the esophagus and the stomach. This sphincter opens when the bolus reaches it, allowing the food to enter the stomach. The sphincter normally remains closed at other times to prevent the contents of the stomach from entering the esophagus. Failure of this sphincter to remain completely closed can lead to heartburn. If it happens chronically, it can lead to gastroesophageal reflux disease (GERD), in which the mucous membrane of the esophagus may become damaged by the highly acidic contents of the stomach.
See the video below to see how the parts of the upper GI tract work together to carry out swallowing:
https://youtu.be/pNcV6yAfq-g
Swallowing, uploaded by Alejandra Cork, 2012.
Stomach
The stomach is a J-shaped organ (shown in Figure 15.4.7) that is joined to the esophagus at its upper end, and to the first part of the small intestine (duodenum) at its lower end. When the stomach is empty of food, it normally has a volume of about 75 millilitres, but it can expand to hold up to about a litre of food. Waves of muscle contractions (peristalsis) passing through the muscular walls of the stomach cause the food inside to be mixed and churned. The wall of the stomach has an extra layer of muscle tissue not found in other organs of the GI tract that helps it squeeze and mix the food. These movements of the stomach wall contribute greatly to mechanical digestion by breaking the food into much smaller pieces. The churning also helps mix the food with stomach secretions that aid in its chemical digestion.
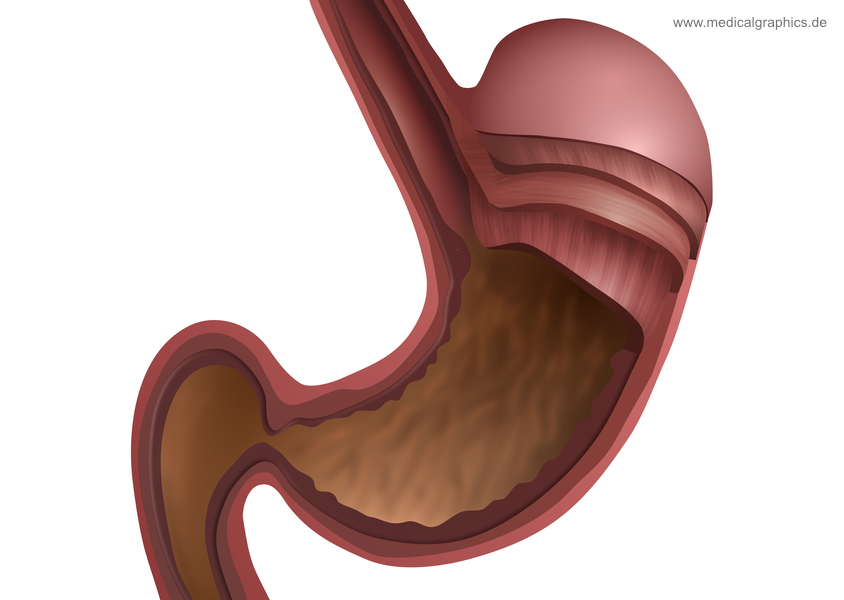
Secretions of the stomach include gastric acid, which consists mainly of hydrochloric acid (HCl). This makes the stomach contents highly acidic, which is necessary so that the enzyme pepsin — also secreted by the stomach — can begin the digestion of protein. Mucus is secreted by the lining of stomach to provide a slimy protective coating against the otherwise damaging effects of gastric acid. The fat-digesting enzyme lipase is secreted in small amounts in the stomach, but very little fat digestion occurs there.
By the time food has been in the stomach for about an hour, it has become the thick, semi-liquid chyme. When the small intestine is ready to receive chyme, a sphincter between the stomach and duodenum — called the pyloric sphincter — opens to allow the chyme to enter the small intestine for further digestion and absorption.
Feature: Reliable Sources
The ongoing epidemic of obesity in the wealthier nations of the world, including Canada, has led to the development of several different bariatric surgeries that modify the stomach to help obese patients reduce their food intake and lose weight. Go online to learn more about bariatric surgery. Find sources you judge to be reliable that answer the following questions:
- Who qualifies for bariatric surgery?
- Describe the bariatric surgeries commonly called stomach stapling, lap band, and gastric sleeve. How does each type of surgery modify the stomach? In terms of weight loss, how effective is each type?
- What are the major potential risks of bariatric surgery?
- Besides weight loss, what other benefits have been shown to result from bariatric surgery?
15.4 Summary
- Organs of the upper gastrointestinal (GI) tract include the mouth, pharynx, esophagus, and stomach.
- The mouth is the first organ of the GI tract. It has several structures that are specialized for digestion, including salivary glands, tongue, and teeth. Both mechanical digestion and chemical digestion of carbohydrates and fats begin in the mouth.
- The pharynx and esophagus move food from the mouth to the stomach, but are not involved in the process of digestion or absorption. Food moves through the esophagus by peristalsis.
- Mechanical and chemical digestion continue in the stomach. Acid and digestive enzymes secreted by the stomach start the chemical digestion of proteins. The stomach turns masticated food into a semi-fluid mixture called chyme.
15.4 Review Questions
-
- Identify structures in the mouth that are specialized for digestion.
- Describe digestion in the mouth.
- What general role do the pharynx and esophagus play in the digestion of food?
- How does food travel through the esophagus?
- Describe digestion in the stomach.
- Describe the differences between how air and food normally move past the pharynx.
- Name two structures in the mouth that contribute to mechanical digestion.
- What structure normally keeps stomach contents from backing up into the esophagus?
- Thirty minutes after you eat a meal, where is most of your food located? Explain your answer.
- What are two roles of mucus in the upper GI tract?
15.4 Explore More
https://youtu.be/zGoBFU1q4g0
What causes cavities? - Mel Rosenberg, TED-Ed, 2016.
https://youtu.be/gCrmFbgT37I
How does alcohol make you drunk? - Judy Grisel, TED-Ed, 2020.
https://youtu.be/twJBEypJDfU
Gastric Bypass Surgery: One Patient’s Journey - Mayo Clinic, 2014.
https://youtu.be/u_1sVri3b2w
Here's What Happens In Your Body When You Swallow Gum | The Human Body, Tech Insider, 2018.
Attributions
Figure 15.4.1
Handstand, Pender Island, B.C. [photo] by Jasper Garratt on Unsplash is used under the Unsplash License (https://unsplash.com/license).
Figure 15.4.2
Blausen_0780_SalivaryGlands by BruceBlaus on Wikimedia Commons is used under a CC BY 3.0 (https://creativecommons.org/licenses/by/3.0) license.
Figure 15.4.3
1402_The_Tongue by OpenStax on Wikimedia Commons is used under a CC BY 4.0 (https://creativecommons.org/licenses/by/4.0) license.
Figure 15.4.4
1024px-3D_Medical_Animation_Still_Showing_Types_of_Teeth by http://www.scientificanimations.com on Wikimedia Commons is used under a CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0) license.
Figure 15.4.5
Illu01_head_neck by Arcadian from NCI/ SEER Training Modules on Wikimedia Common is in the public domain (https://en.wikipedia.org/wiki/public_domain).
Figure 15.4.6
ZenkerSchraeg by Bernd Brägelmann Braegel on Wikimedia Commons is used under a CC BY 3.0 (https://creativecommons.org/licenses/by/3.0) license. (Courtesy of Dr. Martin Steinhoff. It is not known whether there is a possibly necessary approval from the patient.)
Figure 15.4.7
Anatomy stomach – white by www.medicalgraphics.de from MedicalGraphics is used under a CC BY-ND 4.0 (https://creativecommons.org/licenses/by-nd/4.0/) license.
References
Alejandra Cork. (2012). Swallowing. YouTube. https://www.youtube.com/watch?v=pNcV6yAfq-g&t=4s
Betts, J. G., Young, K.A., Wise, J.A., Johnson, E., Poe, B., Kruse, D.H., Korol, O., Johnson, J.E., Womble, M., DeSaix, P. (2016, May 27). Figure 14.3 The tongue [digital image]. In Anatomy and Physiology (Section 14.1). OpenStax. https://openstax.org/books/anatomy-and-physiology/pages/14-1-sensory-perception
Blausen.com Staff. (2014). Medical gallery of Blausen Medical 2014. WikiJournal of Medicine 1 (2). DOI:10.15347/wjm/2014.010. ISSN 2002-4436.
Mayo Clinic. (2014, August 26). Gastric bypass surgery: One patient’s journey - Mayo Clinic. https://www.youtube.com/watch?v=twJBEypJDfU&feature=youtu.be
Mayo Clinic Staff. (n.d.). Gastroesophageal reflux disease (GERD) [online article]. MayoClinic.org. https://www.mayoclinic.org/diseases-conditions/gerd/symptoms-causes/syc-20361940
Tech Insider. (2018, March 20). Here's what happens in your body when you swallow gum | The human body. YouTube. https://www.youtube.com/watch?v=u_1sVri3b2w&feature=youtu.be
TED-Ed. (2020, April 9). How does alcohol make you drunk? - Judy Grisel. YouTube. https://www.youtube.com/watch?v=gCrmFbgT37I&feature=youtu.be
TED-Ed. (2016, October 17). What causes cavities? - Mel Rosenberg. YouTube. https://www.youtube.com/watch?v=zGoBFU1q4g0&feature=youtu.be
A complex organic chemical that provides energy to drive many processes in living cells, e.g. muscle contraction, nerve impulse propagation, and chemical synthesis. Found in all forms of life, ATP is often referred to as the "molecular unit of currency" of intracellular energy transfer.
Created by CK-12 Foundation/Adapted by Christine Miller

Crohn’s Rash
If you had a skin rash like the one shown in Figure 15.7.1, you probably wouldn’t assume that it was caused by a digestive system disease. However, that’s exactly why the individual in the picture has a rash. He has a gastrointestinal (GI) tract disorder called Crohn’s disease. This disease is one of a group of GI tract disorders that are known collectively as inflammatory bowel disease. Unlike other inflammatory bowel diseases, signs and symptoms of Crohn’s disease may not be confined to the GI tract.
Inflammatory Bowel Disease
Inflammatory bowel disease (IBD) is a collection of inflammatory conditions primarily affecting the intestines. The two principal inflammatory bowel diseases are Crohn’s disease and ulcerative colitis. Unlike Crohn’s disease — which may affect any part of the GI tract and the joints, as well as the skin — ulcerative colitis mainly affects just the colon and rectum. Both diseases occur when the body’s own immune system attacks the digestive system. Both diseases typically first appear in the late teens or early twenties, and occur equally in males and females. Approximately 270,000 Canadians are currently living with IBD, 7,000 of which are children. The annual cost of caring for these Canadians is estimated at $1.28 billion. The number of cases of IBD has been steadily increasing and it is expected that by 2030 the number of Canadians suffering from IBD will grow to 400,000.
Crohn’s Disease
Crohn’s disease is a type of inflammatory bowel disease that may affect any part of the GI tract from the mouth to the anus, among other body tissues. The most commonly affected region is the ileum, which is the final part of the small intestine. Signs and symptoms of Crohn’s disease typically include abdominal pain, diarrhea (with or without blood), fever, and weight loss. Malnutrition because of faulty absorption of nutrients may also occur. Potential complications of Crohn’s disease include obstructions and abscesses of the bowel. People with Crohn’s disease are also at slightly greater risk than the general population of developing bowel cancer. Although there is a slight reduction in life expectancy in people with Crohn’s disease, if the disease is well-managed, affected people can live full and productive lives. Approximately 135,000 Canadians are living with Crohn's disease.
Crohn’s disease is caused by a combination of genetic and environmental factors that lead to impairment of the generalized immune response (called innate immunity). The chronic inflammation of Crohn’s disease is thought to be the result of the immune system “trying” to compensate for the impairment. Dozens of genes are likely to be involved, only a few of which have been identified. Because of the genetic component, close relatives such as siblings of people with Crohn’s disease are many times more likely to develop the disease than people in the general population. Environmental factors that appear to increase the risk of the disease include smoking tobacco and eating a diet high in animal proteins. Crohn’s disease is typically diagnosed on the basis of a colonoscopy, which provides a direct visual examination of the inside of the colon and the ileum of the small intestine.
People with Crohn’s disease typically experience recurring periods of flare-ups followed by remission. There are no medications or surgical procedures that can cure Crohn’s disease, although medications such as anti-inflammatory or immune-suppressing drugs may alleviate symptoms during flare-ups and help maintain remission. Lifestyle changes, such as dietary modifications and smoking cessation, may also help control symptoms and reduce the likelihood of flare-ups. Surgery may be needed to resolve bowel obstructions, abscesses, or other complications of the disease.
Ulcerative Colitis
Ulcerative colitis is an inflammatory bowel disease that causes inflammation and ulcers (sores) in the colon and rectum. Unlike Crohn’s disease, other parts of the GI tract are rarely affected in ulcerative colitis. The primary symptoms of the disease are lower abdominal pain and bloody diarrhea. Weight loss, fever, and anemia may also be present. Symptoms typically occur intermittently with periods of no symptoms between flare-ups. People with ulcerative colitis have a considerably increased risk of colon cancer and should be screened for colon cancer more frequently than the general population. Ulcerative colitis, however, seems to primarily reduce the quality of life, and not the lifespan.
The exact cause of ulcerative colitis is not known. Theories about its cause involve immune system dysfunction, genetics, changes in normal gut bacteria, and lifestyle factors, such as a diet high in animal protein and the consumption of alcoholic beverages. Genetic involvement is suspected in part because ulcerative colitis tens to “run” in families. It is likely that multiple genes are involved. Diagnosis is typically made on the basis of colonoscopy and tissue biopsies.
Lifestyle changes, such as reducing the consumption of animal protein and alcohol, may improve symptoms of ulcerative colitis. A number of medications are also available to treat symptoms and help prolong remission. These include anti-inflammatory drugs and drugs that suppress the immune system. In cases of severe disease, removal of the colon and rectum may be required and can cure the disease.
Diverticulitis
Diverticulitis is a digestive disease in which tiny pouches in the wall of the large intestine become infected and inflamed. Symptoms typically include lower abdominal pain of sudden onset. There may also be fever, nausea, diarrhea or constipation, and blood in the stool. Having large intestine pouches called diverticula (see Figure 15.7.2) that are not inflamed is called diverticulosis. Diverticulosis is thought to be caused by a combination of genetic and environmental factors, and is more common in people who are obese. Infection and inflammation of the pouches (diverticulitis) occurs in about 10–25% of people with diverticulosis, and is more common at older ages. The infection is generally caused by bacteria.
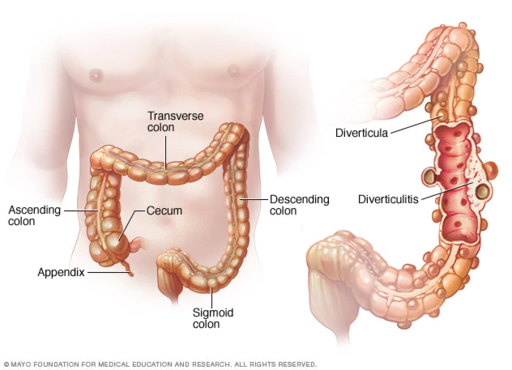
Diverticulitis can usually be diagnosed with a CT scan and can be monitored with a colonoscopy (as seen in Figure 15.7.3). Mild diverticulitis may be treated with oral antibiotics and a short-term liquid diet. For severe cases, intravenous antibiotics, hospitalization, and complete bowel rest (no nourishment via the mouth) may be recommended. Complications such as abscess formation or perforation of the colon require surgery.
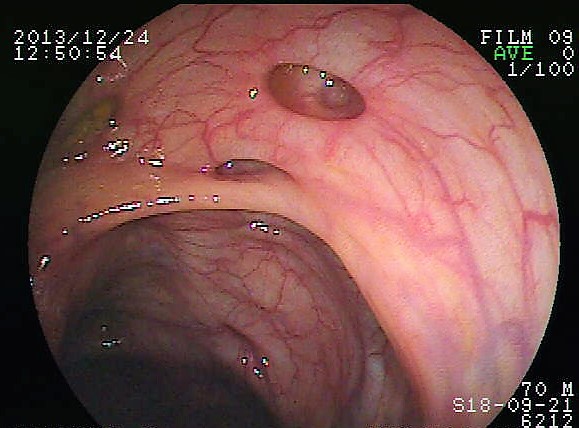
Peptic Ulcer
A peptic ulcer is a sore in the lining of the stomach or the duodenum (first part of the small intestine). If the ulcer occurs in the stomach, it is called a gastric ulcer. If it occurs in the duodenum, it is called a duodenal ulcer. The most common symptoms of peptic ulcers are upper abdominal pain that often occurs in the night and improves with eating. Other symptoms may include belching, vomiting, weight loss, and poor appetite. Many people with peptic ulcers, particularly older people, have no symptoms. Peptic ulcers are relatively common, with about ten per cent of people developing a peptic ulcer at some point in their life.
The most common cause of peptic ulcers is infection with the bacterium Helicobacter pylori, which may be transmitted by food, contaminated water, or human saliva (for example, by kissing or sharing eating utensils). Surprisingly, the bacterial cause of peptic ulcers was not discovered until the 1980s. The scientists who made the discovery are Australians Robin Warren and Barry J. Marshall. Although the two scientists eventually won a Nobel Prize for their discovery, their hypothesis was poorly received at first. To demonstrate the validity of their discovery, Marshall used himself in an experiment. He drank a culture of bacteria from a peptic ulcer patient and developed symptoms of peptic ulcer in a matter of days. His symptoms resolved on their own within a couple of weeks, but, at his wife's urging, he took antibiotics to kill any remaining bacteria. Marshall’s self-experiment was published in the Australian Medical Journal, and is among the most cited articles ever published in the journal. Figure 15.7.4 shows how H. pylori cause peptic ulcers.
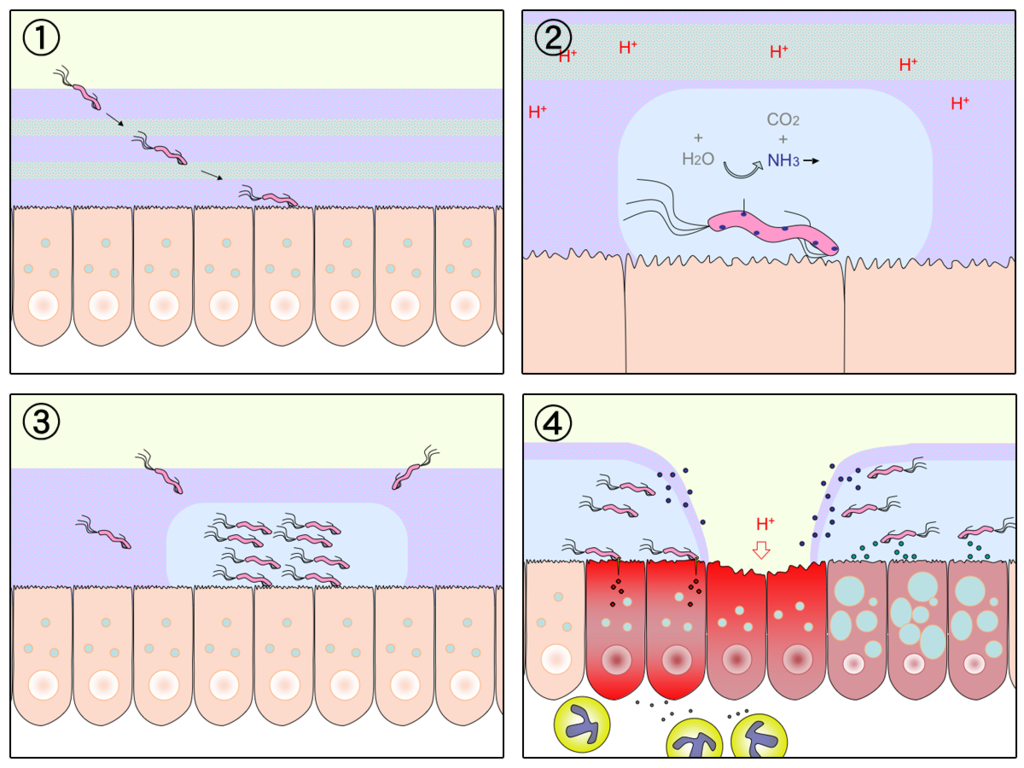
Another relatively common cause of peptic ulcers is chronic use of non-steroidal anti-inflammatory drugs (NSAIDs), such as aspirin or ibuprofen. Additional contributing factors may include tobacco smoking and stress, although these factors have not been demonstrated conclusively to cause peptic ulcers independent of H. pylori infection. Contrary to popular belief, diet does not appear to play a role in either causing or preventing peptic ulcers. Eating spicy foods and drinking coffee and alcohol were once thought to cause peptic ulcers. These lifestyle choices are no longer thought to have much (if any) of an effect on the development of peptic ulcers.
Peptic ulcers are typically diagnosed on the basis of symptoms or the presence of H. pylori in the GI tract. However, endoscopy (shown in Figure 15.7.5), which allows direct visualization of the stomach and duodenum with a camera, may be required for a definitive diagnosis. Peptic ulcers are usually treated with antibiotics to kill H. pylori, along with medications to temporarily decrease stomach acid and aid in healing. Unfortunately, H. pylori has developed resistance to commonly used antibiotics, so treatment is not always effective. If a peptic ulcer has penetrated so deep into the tissues that it causes a perforation of the wall of the stomach or duodenum, then emergency surgery is needed to repair the damage.

Gastroenteritis
Gastroenteritis, also known as infectious diarrhea or stomach flu, is an acute and usually self-limiting infection of the GI tract by pathogens. Symptoms typically include some combination of diarrhea, vomiting, and abdominal pain. Fever, lack of energy, and dehydration may also occur. The illness generally lasts less than two weeks, even without treatment, but in young children it is potentially deadly. Gastroenteritis is very common, especially in poorer nations. Worldwide, up to five billion cases occur each year, resulting in about 1.4 million deaths.
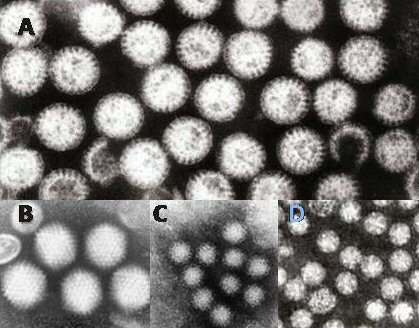
Commonly called “stomach flu,” gastroenteritis is unrelated to the influenza virus, although viruses are the most common cause of the disease (see Figure 15.7.6). In children, rotavirus is most often the cause which is why the British Columbia immunization schedule now includes a rotovirus vaccine. Norovirus is more likely to be the cause of gastroenteritis in adults. Besides viruses, other potential causes of gastroenteritis include fungi, bacteria (most often E. coli or Campylobacter jejuni), and protozoa(including Giardia lamblia, more commonly called Beaver Fever, described below). Transmission of pathogens may occur due to eating improperly prepared foods or foods left to stand at room temperature, drinking contaminated water, or having close contact with an infected individual.
Gastroenteritis is less common in adults than children, partly because adults have acquired immunity after repeated exposure to the most common infectious agents. Adults also tend to have better hygiene than children. If children have frequent repeated incidents of gastroenteritis, they may suffer from malnutrition, stunted growth, and developmental delays. Many cases of gastroenteritis in children can be avoided by giving them a rotavirus vaccine. Frequent and thorough handwashing can cut down on infections caused by other pathogens.
Treatment of gastroenteritis generally involves increasing fluid intake to replace fluids lost in vomiting or diarrhea. Oral rehydration solution, which is a combination of water, salts, and sugar, is often recommended. In severe cases, intravenous fluids may be needed. Antibiotics are not usually prescribed, because they are ineffective against viruses that cause most cases of gastroenteritis.
Giardiasis
Giardiasis, popularly known as beaver fever, is a type of gastroenteritis caused by a GI tract parasite, the single-celled protozoan Giardia lamblia (pictured in Figure 15.7.7). In addition to human beings, the parasite inhabits the digestive tract of a wide variety of domestic and wild animals, including cows, rodents, and sheep, as well as beavers (hence its popular name). Giardiasis is one of the most common parasitic infections in people the world over, with hundreds of millions of people infected worldwide each year.

Transmission of G. lamblia is via a fecal-oral route (as in, you got feces in your food). Those at greatest risk include travelers to countries where giardiasis is common, people who work in child-care settings, backpackers and campers who drink untreated water from lakes or rivers, and people who have close contact with infected people or animals in other settings. In Canada, Giardia is the most commonly identified intestinal parasite and approximately 3,000 Canadians will contract the parasite annually.
Symptoms of giardiasis can vary widely. About one-third third of people with the infection have no symptoms, whereas others have severe diarrhea with poor absorption of nutrients. Problems with absorption occur because the parasites inhibit intestinal digestive enzyme production, cause detrimental changes in microvilli lining the small intestine, and kill off small intestinal epithelial cells. The illness can result in weakness, loss of appetite, stomach cramps, vomiting, and excessive gas. Without treatment, symptoms may continue for several weeks. Treatment with anti-parasitic medications may be needed if symptoms persist longer or are particularly severe.
15.7 Summary
- Inflammatory bowel disease is a collection of inflammatory conditions primarily affecting the intestines. The diseases involve the immune system attacking the GI tract, and they have multiple genetic and environmental causes. Typical symptoms include abdominal pain and diarrhea, which show a pattern of repeated flare-ups interrupted by periods of remission. Lifestyle changes and medications may control flare-ups and extend remission. Surgery is sometimes required.
- The two principal inflammatory bowel diseases are Crohn’s disease and ulcerative colitis. Crohn’s disease may affect any part of the GI tract from the mouth to the anus, among other body tissues. Ulcerative colitis affects the colon and/or rectum.
- Some people have little pouches, called diverticula, in the lining of their large intestine, a condition called diverticulosis. People with diverticulosis may develop diverticulitis, in which one or more of the diverticula become infected and inflamed. Diverticulitis is generally treated with antibiotics and bowel rest. Sometimes, surgery is required.
- A peptic ulcer is a sore in the lining of the stomach (gastric ulcer) or duodenum (duodenal ulcer). The most common cause is infection with the bacterium Helicobacter pylori. NSAIDs (such as aspirin) can also cause peptic ulcers, and some lifestyle factors may play contributing roles. Antibiotics and acid reducers are typically prescribed, and surgery is not often needed.
- Gastroenteritis, or infectious diarrhea, is an acute and usually self-limiting infection of the GI tract by pathogens, most often viruses. Symptoms typically include diarrhea, vomiting, and/or abdominal pain. Treatment includes replacing lost fluids. Antibiotics are not usually effective.
- Giardiasis is a type of gastroenteritis caused by infection of the GI tract with the protozoa parasite Giardia lamblia. It may cause malnutrition. Generally self-limiting, severe or long-lasting cases may require antibiotics.
15.7 Review Questions
-
-
- Compare and contrast Crohn’s disease and ulcerative colitis.
- How are diverticulosis and diverticulitis related?
- Identify the cause of giardiasis. Why may it cause malabsorption?
- Name three disorders of the GI tract that can be caused by bacteria.
- Name one disorder of the GI tract that can be helped by anti-inflammatory medications, and one that can be caused by chronic use of anti-inflammatory medications.
- Describe one reason why it can be dangerous to drink untreated water.
15.7 Explore More
https://youtu.be/H5zin8jKeT0
Who's at risk for colon cancer? - Amit H. Sachdev and Frank G. Gress, TED-Ed, 2018.
https://youtu.be/V_U6czbDHLE
The surprising cause of stomach ulcers - Rusha Modi, TED-Ed, 2017.
Attributions
Figure 15.7.1
BADAS_Crohn by Dayavathi Ashok and Patrick Kiely/ Journal of medical case reports on Wikimedia Commons is used under a CC BY 2.0 (https://creativecommons.org/licenses/by/2.0) license.
Figure 15.7.2
512px-Ds00070_an01934_im00887_divert_s_gif.webp by Lfreeman04 on Wikimedia Commons is used under a CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0) license.
Figure 15.7.3
Colon_diverticulum by melvil on Wikimedia Commons is used under a CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0) license.
Figure 15.7.4
H_pylori_ulcer_diagram by Y_tambe on Wikimedia Commons is used under a CC BY-SA 3.0 (http://creativecommons.org/licenses/by-sa/3.0/) license.
Figure 15.7.5
1024px-Endoscopy_training by Yuya Tamai on Wikimedia Commons is used under a CC BY 2.0 (https://creativecommons.org/licenses/by/2.0) license.
Figure 15.7.6
Gastroenteritis_viruses by Dr. Graham Beards [en:User:Graham Beards] at en.wikipedia on Wikimedia Commons is used under a CC BY 3.0 (https://creativecommons.org/licenses/by/3.0) license.
Figure 15.7.7
Giardia_lamblia_SEM_8698_lores by Janice Haney Carr from CDC/ Public Health Image Library (PHIL) ID# 8698 on Wikimedia Commons is in the public domain (https://en.wikipedia.org/wiki/public_domain).
References
Ashok, D., & Kiely, P. (2007). Bowel associated dermatosis - arthritis syndrome: a case report. Journal of medical case reports, 1, 81. https://doi.org/10.1186/1752-1947-1-81
Marshall, B. J., Armstrong, J. A., McGechie, D. B., & Glancy, R. J. (1985). Attempt to fulfil Koch's postulates for pyloric Campylobacter. The Medical Journal of Australia, 142(8), 436–439.
Marshall, B. J., McGechie, D. B., Rogers, P. A., & Glancy, R. J. (1985). Pyloric campylobacter infection and gastroduodenal disease. The Medical Journal of Australia, 142(8), 439–444.
TED-Ed. (2017, September 28). The surprising cause of stomach ulcers - Rusha Modi. YouTube. https://www.youtube.com/watch?v=V_U6czbDHLE&feature=youtu.be
TED-Ed. (2018, January 4). Who's at risk for colon cancer? - Amit H. Sachdev and Frank G. Gress. YouTube. https://www.youtube.com/watch?v=H5zin8jKeT0&feature=youtu.be
Glucose (also called dextrose) is a simple sugar with the molecular formula C6H12O6. Glucose is the most abundant monosaccharide, a subcategory of carbohydrates. Glucose is mainly made by plants and most algae during photosynthesis from water and carbon dioxide, using energy from sunlight.
Created by: CK-12/Adapted by Christine Miller
Case Study: Cancer in the Family
People tend to carry similar traits to their biological parents, as illustrated by the family tree. Beyond just appearance, you can also inherit traits from your parents that you can’t see.
Rebecca becomes very aware of this fact when she visits her new doctor for a physical exam. Her doctor asks several questions about her family medical history, including whether Rebecca has or had relatives with cancer. Rebecca tells her that her grandmother, aunt, and uncle — who have all passed away — had cancer. They all had breast cancer, including her uncle, and her aunt also had ovarian cancer. Her doctor asks how old they were when they were diagnosed with cancer. Rebecca is not sure exactly, but she knows that her grandmother was fairly young at the time, probably in her forties.
Rebecca’s doctor explains that while the vast majority of cancers are not due to inherited factors, a cluster of cancers within a family may indicate that there are mutations in certain genes that increase the risk of getting certain types of cancer, particularly breast and ovarian cancer. Some signs that cancers may be due to these genetic factors are present in Rebecca’s family, such as cancer with an early age of onset (e.g., breast cancer before age 50), breast cancer in men, and breast cancer and ovarian cancer within the same person or family.
Based on her family medical history, Rebecca’s doctor recommends that she see a genetic counselor, because these professionals can help determine whether the high incidence of cancers in her family could be due to inherited mutations in their genes. If so, they can test Rebecca to find out whether she has the particular variations of these genes that would increase her risk of getting cancer.
When Rebecca sees the genetic counselor, he asks how her grandmother, aunt, and uncle with cancer are related to her. She says that these relatives are all on her mother’s side — they are her mother’s mother and siblings. The genetic counselor records this information in the form of a specific type of family tree, called a pedigree, indicating which relatives had which type of cancer, and how they are related to each other and to Rebecca.
He also asks her ethnicity. Rebecca says that her family on both sides are Ashkenazi Jews (Jews whose ancestors came from central and eastern Europe). “But what does that have to do with anything?” she asks. The counselor tells Rebecca that mutations in two tumor-suppressor genes called BRCA1 and BRCA2, located on chromosome 17 and 13, respectively, are particularly prevalent in people of Ashkenazi Jewish descent and greatly increase the risk of getting cancer. About one in 40 Ashkenazi Jewish people have one of these mutations, compared to about one in 800 in the general population. Her ethnicity, along with the types of cancer, age of onset, and the specific relationships between her family members who had cancer, indicate to the counselor that she is a good candidate for genetic testing for the presence of these mutations.

Rebecca says that her 72-year-old mother never had cancer, nor had many other relatives on that side of the family. How could the cancers be genetic? The genetic counselor explains that the mutations in the BRCA1 and BRCA2 genes, while dominant, are not inherited by everyone in a family. Also, even people with mutations in these genes do not necessarily get cancer — the mutations simply increase their risk of getting cancer. For instance, 55 to 65 per cent of women with a harmful mutation in the BRCA1 gene will get breast cancer before age 70, compared to 12 per cent of women in the general population who will get breast cancer sometime over the course of their lives.
Rebecca is not sure she wants to know whether she has a higher risk of cancer. The genetic counselor understands her apprehension, but explains that if she knows that she has harmful mutations in either of these genes, her doctor will screen her for cancer more often and at earlier ages. Therefore, any cancers she may develop are likely to be caught earlier when they are often much more treatable. Rebecca decides to go through with the testing, which involves taking a blood sample, and nervously waits for her results.
Chapter Overview: Genetics
At the end of this chapter, you will find out Rebecca’s test results. By then, you will have learned how traits are inherited from parents to offspring through genes, and how mutations in genes such as BRCA1 and BRCA2 can be passed down and cause disease. Specifically, you will learn about:
- The structure of DNA.
- How DNA replication occurs.
- How DNA was found to be the inherited genetic material.
- How genes and their different alleles are located on chromosomes.
- The 23 pairs of human chromosomes, which include autosomal and sex chromosomes.
- How genes code for proteins using codons made of the sequence of nitrogen bases within RNA and DNA.
- The central dogma of molecular biology, which describes how DNA is transcribed into RNA, and then translated into proteins.
- The structure, functions, and possible evolutionary history of RNA.
- How proteins are synthesized through the transcription of RNA from DNA and the translation of protein from RNA, including how RNA and proteins can be modified, and the roles of the different types of RNA.
- What mutations are, what causes them, different specific types of mutations, and the importance of mutations in evolution and to human health.
- How the expression of genes into proteins is regulated and why problems in this process can cause diseases, such as cancer.
- How Gregor Mendel discovered the laws of inheritance for certain types of traits.
- The science of heredity, known as genetics, and the relationship between genes and traits.
- How gametes, such as eggs and sperm, are produced through meiosis.
- How sexual reproduction works on the cellular level and how it increases genetic variation.
- Simple Mendelian and more complex non-Mendelian inheritance of some human traits.
- Human genetic disorders, such as Down syndrome, hemophilia A, and disorders involving sex chromosomes.
- How biotechnology — which is the use of technology to alter the genetic makeup of organisms — is used in medicine and agriculture, how it works, and some of the ethical issues it may raise.
- The human genome, how it was sequenced, and how it is contributing to discoveries in science and medicine.
As you read this chapter, keep Rebecca’s situation in mind and think about the following questions:
- BCRA1 and BCRA2 are also called Breast cancer type 1 and 2 susceptibility proteins. What do the BRCA1 and BRCA2 genes normally do? How can they cause cancer?
- Are BRCA1 and BRCA2 linked genes? Are they on autosomal or sex chromosomes?
- After learning more about pedigrees, draw the pedigree for cancer in Rebecca’s family. Use the pedigree to help you think about why it is possible that her mother does not have one of the BRCA gene mutations, even if her grandmother, aunt, and uncle did have it.
- Why do you think certain gene mutations are prevalent in certain ethnic groups?
Attributions
Figure 5.1.1
Family Tree [all individual face images] from Clker.com used and adapted by Christine Miller under a CC0 1.0 public domain dedication license (https://creativecommons.org/publicdomain/zero/1.0/).
Figure 5.1.2
Rebecca by Kyle Broad on Unsplash is used under the Unsplash License (https://unsplash.com/license).
References
Wikipedia contributors. (2020, June 27). Ashkenazi Jews. In Wikipedia. https://en.wikipedia.org/w/index.php?title=Ashkenazi_Jews&oldid=964691647
Wikipedia contributors. (2020, June 22). BRCA1. In Wikipedia. https://en.wikipedia.org/w/index.php?title=BRCA1&oldid=963868423
Wikipedia contributors. (2020, May 25). BRCA2. In Wikipedia. https://en.wikipedia.org/w/index.php?title=BRCA2&oldid=958722957
The process of producing cellular energy involving oxygen. Cells break down food in the mitochondria in a long, multi-step process that produces roughly 36 ATP. The first step in is glycolysis, the second is the Krebs cycle and the third is the electron transport system.
Respiration using electron acceptors other than molecular oxygen. Although oxygen is not the final electron acceptor, the process still uses a respiratory electron transport chain.
A double-membrane-bound organelle found in most eukaryotic organisms. Mitochondria convert oxygen and nutrients into adenosine triphosphate (ATP). ATP is the chemical energy "currency" of the cell that powers the cell's metabolic activities.
Created by CK-12 Foundation/Adapted by Christine Miller

Getting Rid of Wastes
The many chimneys on these houses are one way that the inhabitants of the home get rid of the wastes they produce. The chimneys expel waste gases that are created when they burn fuel in their furnace or fireplace. Think about the other wastes that people create in their homes and how we dispose of them. Solid trash and recyclables may go to the curb in a trash can, or in a recycling bin for pick up and transport to a landfill or recycling centre. Wastewater from sinks, showers, toilets, and the washing machine goes into a main sewer pipe and out of the house to join the community’s sanitary sewer system.
Like a busy home, your body also produces a lot of wastes that must be eliminated. Like a home, the way your body gets rid of wastes depends on the nature of the waste products. Some human body wastes are gases, some are solids, and some are in a liquid state. Getting rid of body wastes is called excretion, and there are a number of different organs of excretion in the human body.
Excretion
Excretion is the process of removing wastes and excess water from the body. It is an essential process in all living things, and it is one of the major ways the human body maintains homeostasis. It also helps prevent damage to the body. Wastes include by-products of metabolism — some of which are toxic — and other non-useful materials, such as used up and broken down components. Some of the specific waste products that must be excreted from the body include carbon dioxide from cellular respiration, ammonia and urea from protein catabolism, and uric acid from nucleic acid catabolism.
Excretory Organs
Organs of excretion include the skin, liver, large intestine, lungs, and kidneys (see Figure 16.2.2). Together, these organs make up the excretory system. They all excrete wastes, but they don’t work together in the same way that organs do in most other body systems. Each of the excretory organs “does its own thing” more-or-less independently of the others, but all are necessary to successfully excrete the full range of wastes from the human body.
Figure 16.2.2 Internal organs of excretion are identified in this illustration. They include the skin, liver, large intestine, lungs, and kidneys.
Skin

The skin is part of the integumentary system, but it also plays a role in excretion through the production of sweat by sweat glands in the dermis. Although the main role of sweat production is to cool the body and maintain temperature homeostasis, sweating also eliminates excess water and salts, as well as a small amount of urea. When sweating is copious, as in Figure 16.2.3, ingestion of salts and water may be helpful to maintain homeostasis in the body.
Liver
The liver (shown in Figure 16.2.4) has numerous major functions, including secreting bile for digestion of lipids, synthesizing many proteins and other compounds, storing glycogen and other substances, and secreting endocrine hormones. In addition to all of these functions, the liver is a very important organ of excretion. The liver breaks down many substances in the blood, including toxins. For example, the liver transforms ammonia — a poisonous by-product of protein catabolism — into urea, which is filtered from the blood by the kidneys and excreted in urine. The liver also excretes in its bile the protein bilirubin, a byproduct of hemoglobin catabolism that forms when red blood cells die. Bile travels to the small intestine and is then excreted in feces by the large intestine.
Large Intestine
The large intestine is an important part of the digestive system and the final organ in the gastrointestinal tract. As an organ of excretion, its main function is to eliminate solid wastes that remain after the digestion of food and the extraction of water from indigestible matter in food waste. The large intestine also collects wastes from throughout the body. Bile secreted into the gastrointestinal tract, for example, contains the waste product bilirubin from the liver. Bilirubin is a brown pigment that gives human feces its characteristic brown colour.
Lungs
The lungs are part of the respiratory system (shown in Figure 16.2.5), but they are also important organs of excretion. They are responsible for the excretion of gaseous wastes from the body. The main waste gas excreted by the lungs is carbon dioxide, which is a waste product of cellular respiration in cells throughout the body. Carbon dioxide is diffused from the blood into the air in the tiny air sacs called alveoli in the lungs (shown in the inset diagram). By expelling carbon dioxide from the blood, the lungs help maintain acid-base homeostasis. In fact, it is the pH of blood that controls the rate of breathing. Water vapor is also picked up from the lungs and other organs of the respiratory tract as the exhaled air passes over their moist linings, and the water vapor is excreted along with the carbon dioxide. Trace levels of some other waste gases are exhaled, as well.
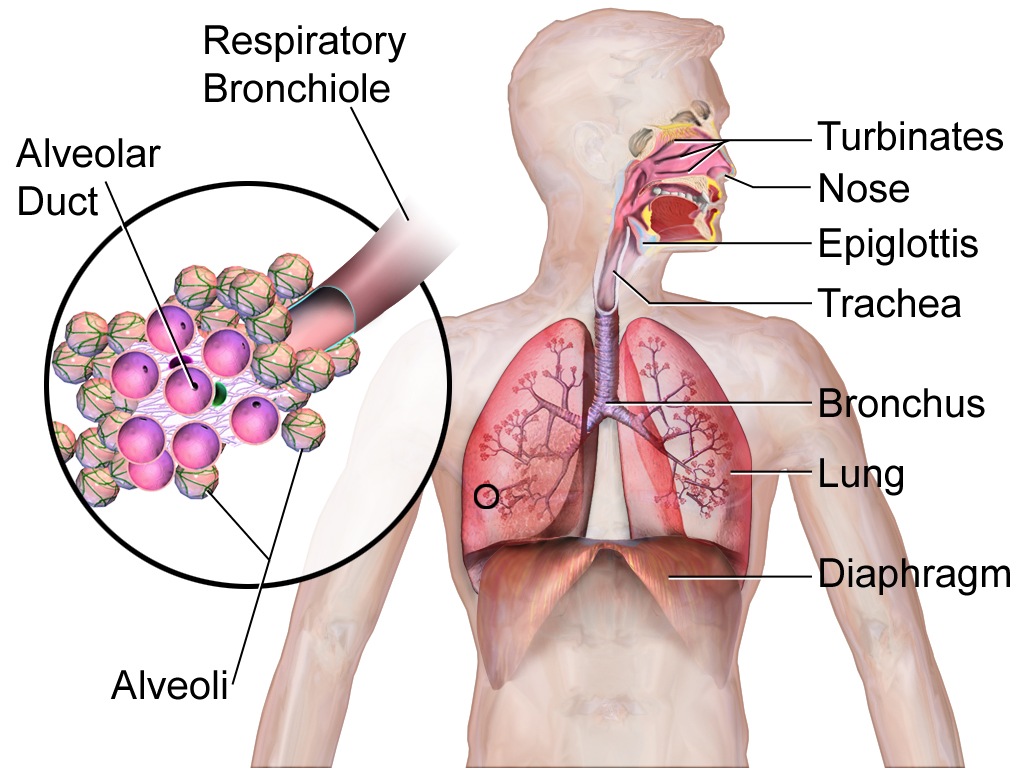
Kidneys
The paired kidneys are often considered the main organs of excretion. The primary function of the kidneys is the elimination of excess water and wastes from the bloodstream by the production of the liquid waste known as urine. The main structural and functional units of the kidneys are tiny structures called nephrons. Nephrons filter materials out of the blood, return to the blood what is needed, and excrete the rest as urine. As shown in Figure 16.2.6, the kidneys are organs of the urinary system, which also includes the ureters, bladder, and urethra — organs that transport, store, and eliminate urine, respectively.
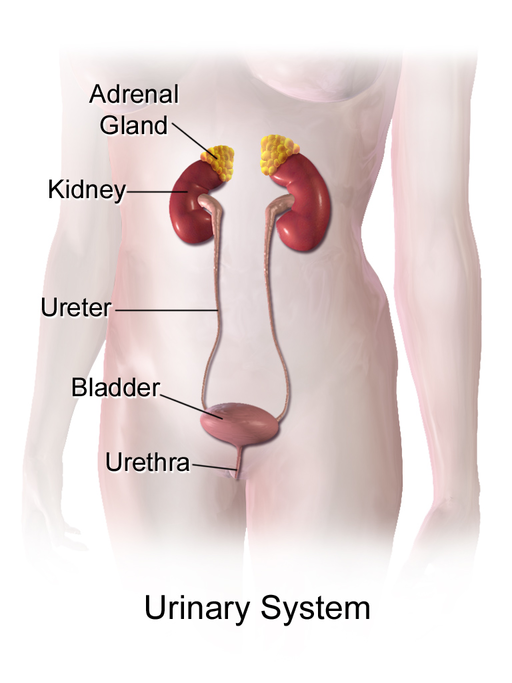
By producing and excreting urine, the kidneys play vital roles in body-wide homeostasis. They maintain the correct volume of extracellular fluid, which is all the fluid in the body outside of cells, including the blood and lymph. The kidneys also maintain the correct balance of salts and pH in extracellular fluid. In addition, the kidneys function as endocrine glands, secreting hormones into the blood that control other body processes. You can read much more about the kidneys in section 16.4 Kidneys.
16.2 Summary
- Excretion is the process of removing wastes and excess water from the body. It is an essential process in all living things and a major way the human body maintains homeostasis.
- Organs of excretion include the skin, liver, large intestine, lungs, and kidneys. All of them excrete wastes, and together they make up the excretory system.
- The skin plays a role in excretion through the production of sweat by sweat glands. Sweating eliminates excess water and salts, as well as a small amount of urea, a byproduct of protein catabolism.
- The liver is a very important organ of excretion. The liver breaks down many substances in the blood, including toxins. The liver also excretes bilirubin — a waste product of hemoglobin catabolism — in bile. Bile then travels to the small intestine, and is eventually excreted in feces by the large intestine.
- The main excretory function of the large intestine is to eliminate solid waste that remains after food is digested and water is extracted from the indigestible matter. The large intestine also collects and excretes wastes from throughout the body, including bilirubin in bile.
- The lungs are responsible for the excretion of gaseous wastes, primarily carbon dioxide from cellular respiration in cells throughout the body. Exhaled air also contains water vapor and trace levels of some other waste gases.
- The paired kidneys are often considered the main organs of excretion. Their primary function is the elimination of excess water and wastes from the bloodstream by the production of urine. The kidneys contain tiny structures called nephrons that filter materials out of the blood, return to the blood what is needed, and excrete the rest as urine. The kidneys are part of the urinary system, which also includes the ureters, urinary bladder, and urethra.
16.2 Review Questions
- What is excretion, and what is its significance?
-
- Describe the excretory functions of the liver.
- What are the main excretory functions of the large intestine?
- List organs of the urinary system.
- Describe the physical states in which the wastes from the human body are excreted.
- Give one example of why ridding the body of excess water is important.
- What gives feces its brown colour? Why is that substance produced?
16.2 Explore More
https://www.youtube.com/watch?v=erMCADOJcHk&feature=youtu.be
Why Can We Regrow A Liver (But Not A Limb)? MITK12Videos, 2015.
https://www.youtube.com/watch?v=SeK0zFB9yHg&feature=youtu.be
Are Sports Drinks Good For You? | Fit or Fiction, POPSUGAR Fitness, 2014.
https://www.youtube.com/watch?v=fctH_1NuqCQ&feature=youtu.be
Why do we sweat? - John Murnan, TED-Ed, 2018.
Attributions
Figure 16.2.1
Chimneys/ Kingston upon Hull, England [photo] by Angela Baker on Unsplash is used under the Unsplash License (https://unsplash.com/license).
Figure 16.2.2
- Sweat or rain? by Kullez on Flickr is used under a CC BY 2.0 (https://creativecommons.org/licenses/by/2.0/).
- Kidney front - white from www.medicalgraphics.de is used under a CC BY-ND 4.0 (https://creativecommons.org/licenses/by-nd/4.0/) license.
- File:Liver Cirrhosis.png by BruceBlaus on Wikimedia Commons is used under a CC BY SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0/deed.en) license.
- File:Human lungs.png by Sharanyaudupa on Wikimedia Commons is used under a CC BY SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0/deed.en) license.
- Tags: Offal Marking Medical Intestine Liver by Elionas2 on Pixabay is used under the Pixabay license (https://pixabay.com/service/license/).
Figure 16.2.3
gym_room_fitness_equipment_cardiovascular_exercise_elliptical_bike_cardio_training_sports_equipment_bodybuilding-825364 from Pxhere is used under a CC0 1.0 Universal public domain dedication license (https://creativecommons.org/publicdomain/zero/1.0/).
Figure 16.2.4
Tags: Liver Organ Anatomy by zachvanstone8 on Pixabay is used under the Pixabay License (https://pixabay.com/service/license/).
Figure 16.2.5
Lung_and_diaphragm by Terese Winslow/ National Cancer Institute on Wikimedia Commons is in the public domain (https://en.wikipedia.org/wiki/Public_domain).
Figure 16.2.6
512px-Urinary_System_(Female) by BruceBlaus on Wikimedia Commons is used under a CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0) license.
References
MITK12Videos. (2015, June 4). Why can we regrow a liver (but not a limb)? https://www.youtube.com/watch?v=erMCADOJcHk&feature=youtu.be
POPSUGAR Fitness. (2014, February 7). Are sports drinks good for you? | Fit or Fiction. YouTube. https://www.youtube.com/watch?v=SeK0zFB9yHg&feature=youtu.be
TED-Ed. (2018, May 15). Why do we sweat? - John Murnan. YouTube. https://www.youtube.com/watch?v=fctH_1NuqCQ&feature=youtu.be
Image shows a pictomicrograph of a protozoan parasite of the Giardia lamblia species. It is roughly cone-shaped, with several flagella trailing from the narrow end of it.
Image shows a pictomicrograph of the layers of the GI tract. Each of the mucosa, submucosa, muscularis and serosa are differentiated with respect to colouration and cell shape/size.


