18.4 Functions of the Male Reproductive System
Colourful Sperm
This false-colour image (Figure 18.4.1) shows real human sperm. The tiny gametes are obviously greatly magnified in the picture, because they are actually the smallest of all human cells. In fact, human sperm cells are small, even when compared with sperm cells of other animals. Mice sperm are about twice the length of human sperm! Human sperm may be small in size, but in a normal, healthy man, huge numbers of them are usually released during each ejaculation. There may be hundreds of millions of sperm cells in a single teaspoon of semen. Producing sperm is one of the major functions of the male reproductive system.
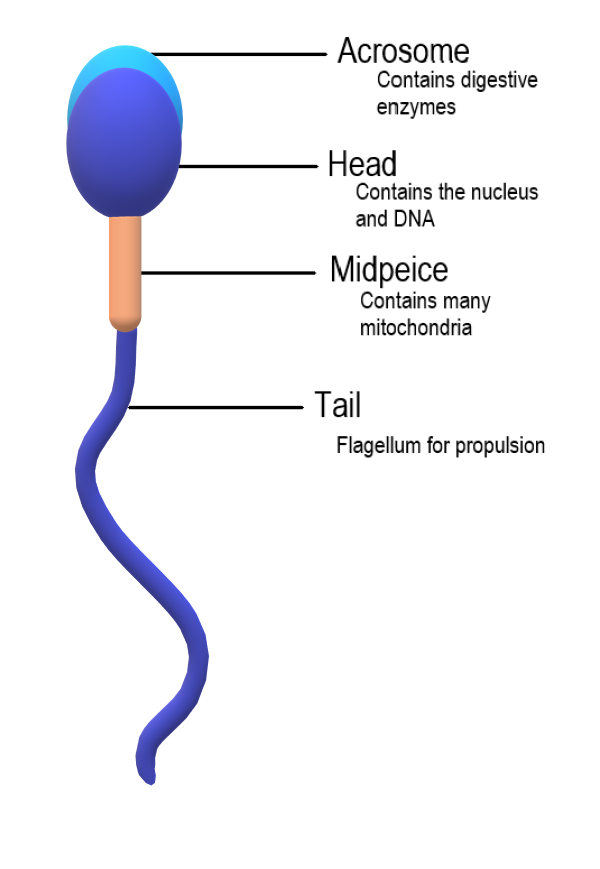
Sperm Anatomy
A mature sperm cell has several structures that help it reach and penetrate an egg. These are labeled in the drawing of a sperm shown in Figure 18.4.2.
- The head is the part of the sperm that contains the nucleus — and not much else. The nucleus, in turn, contains tightly coiled DNA that is the male parent’s contribution to the genetic makeup of a zygote (if one forms). Each sperm is a haploid cell, containing half the chromosomal complement of a normal, diploid body cell.
- The front of the head is an area called the acrosome. The acrosome contains enzymes that help the sperm penetrate an ovum (if it reaches one).
- The midpiece is the part of the sperm between the head and the flagellum. The midpiece is packed with mitochondria that produce the energy needed to move the flagellum.
- The flagellum (also called the tail) can rotate like a propeller, allowing the sperm to “swim” through the female reproductive tract to reach an ovum if one is present.
Spermatogenesis
The process of producing sperm is known as spermatogenesis. Spermatogenesis normally starts when a male reaches puberty, and it usually continues uninterrupted until death, although a decrease in sperm production generally occurs at older ages. A young, healthy male may produce hundreds of millions of sperm a day! Only about half of these, however, are likely to become viable, mature sperm.
Where Sperm Are Produced
Spermatogenesis occurs in the seminiferous tubules in the testes. Spermatogenesis requires high concentrations of testosterone. Testosterone is secreted by Leydig cells, which are adjacent to the seminiferous tubules in the testes.
Sperm production in the seminiferous tubules is very sensitive to temperature. This may be the most important reason the testes are located outside the body in the scrotum. The temperature inside the scrotum is generally about 2 degrees Celsius cooler than core body temperature. This lower temperature is optimal for spermatogenesis. The scrotum regulates its internal temperature as needed by contractions of the smooth muscles lining the scrotum. When the temperature inside the scrotum becomes too low, the scrotal muscles contract. The contraction of the muscles pulls the scrotum higher against the body, where the temperature is warmer. The opposite occurs when the temperature inside the scrotum becomes too high.
Events of Spermatogenesis
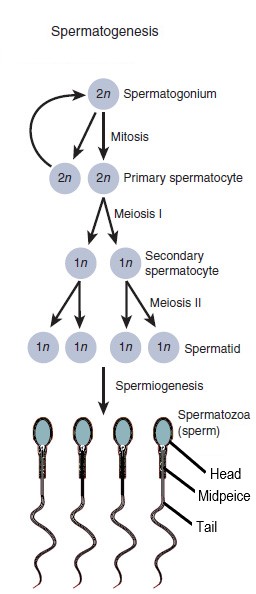
Figure 18.4.3 summarizes the main cellular events that occur in the process of spermatogenesis. The process begins with a diploid stem cell called a spermatogonium (plural, spermatogonia), and involves several cell divisions. The entire process takes at least ten weeks to complete, including maturation in the epididymis.
- A spermatogonium undergoes mitosis to produce two diploid cells called primary spermatocytes. One of the primary spermatocytes goes on to produce sperm. The other replenishes the reserve of spermatogonia.
- The primary spermatocyte undergoes meiosis I to produce two haploid daughter cells called secondary spermatocytes.
- The secondary spermatocytes rapidly undergo meiosis II to produce a total of four haploid daughter cells called spermatids.
- The spermatids begin to form a tail, and their DNA becomes highly condensed. Unnecessary cytoplasm and organelles are removed from the cells, and they form a head, midpiece, and flagellum. The resulting cells are sperm (spermatozoa).
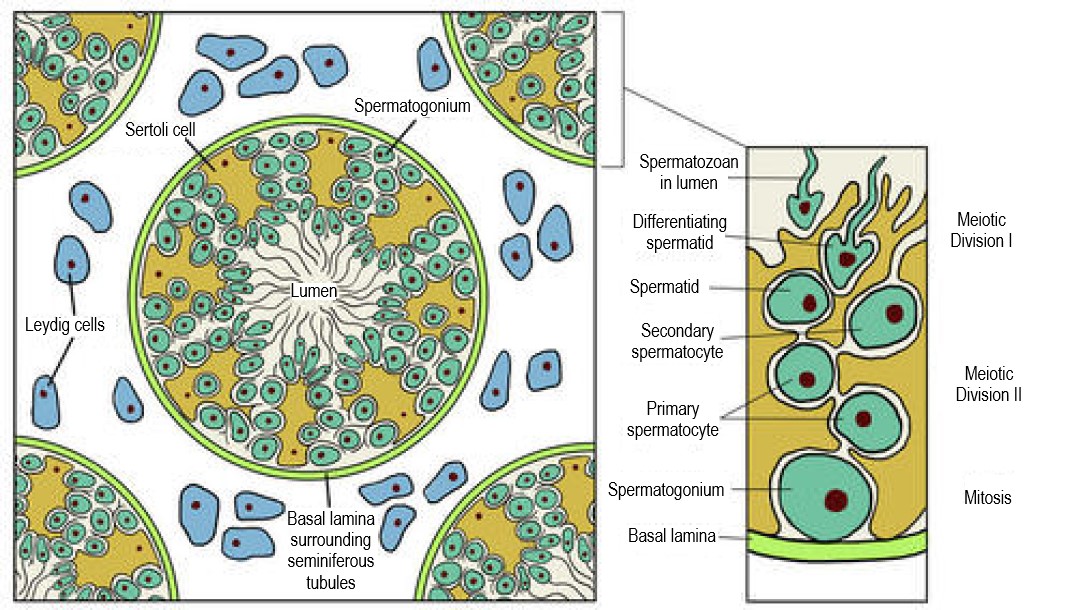
As shown in Figure 18.4.4, the events of spermatogenesis begin near the wall of the seminiferous tubule — where spermatogonia are located — and continue inward toward the lumen of the tubule. Sertoli cells extend from the wall of the seminiferous tubule inward toward the lumen, so they are in contact with developing sperm at all stages of spermatogenesis. Sertoli cells play several roles in spermatogenesis:
- They secrete endocrine hormones that help regulate spermatogenesis.
- They secrete substances that initiate meiosis.
- They concentrate testosterone (from Leydig cells), which is needed at high levels to maintain spermatogenesis.
- They phagocytize the extra cytoplasm that is shed from developing sperm cells.
- They secrete testicular fluid that helps carry sperm into the epididymis.
- They maintain a blood-testis barrier, so immune system cells cannot reach and attack the sperm.
Maturation in the Epididymis
Although the sperm produced in the testes have tails, they are not yet motile (able to “swim”). The non-motile sperm are transported to the epididymis in testicular fluid that is secreted by Sertoli cells with the help of peristaltic contractions. In the epididymis, the sperm gain motility, so they are capable of swimming up the female genital tract and reaching an ovum. The mature sperm are stored in the epididymis until ejaculation occurs.
Ejaculation
Sperm are released from the body during ejaculation, which typically occurs during orgasm. Hundreds of millions of mature sperm — contained within a small amount of thick, whitish fluid called semen — are propelled from the penis during a normal ejaculation.
How Ejaculation Occurs
Ejaculation occurs when peristalsis of the muscle layers of the vas deferens and other accessory structures propel sperm from the epididymes, where mature sperm are stored. The muscle contractions force the sperm through the vas deferens and the ejaculatory ducts, and then out of the penis through the urethra. Due to the peristaltic action of the muscles, the ejaculation occurs in a series of spurts.
The Role of Semen
As sperm travel through the ejaculatory ducts during ejaculation, they mix with secretions from the seminal vesicles, prostate gland, and bulbourethral glands to form semen (see Figure 18.4.5 ). The average amount of semen per ejaculate is about 3.7 mL, which is a little less than a teaspoonful. Most of this volume of semen consists of glandular secretions, with the hundreds of millions of sperm cells actually contributing relatively little to the total volume.

The secretions in semen are important for the survival and motility of sperm. They provide a medium through which sperm can swim. They also include sperm-sustaining substances, such as high concentrations of the sugar fructose, which is the main source of energy for sperm. In addition, semen contains many alkaline substances that help neutralize the acidic environment in the female vagina. This protects the DNA in sperm from being denatured by acid, and prolongs the life of sperm in the female reproductive tract.
Erection
Besides providing a way for sperm to leave the body, the main role of the penis in reproduction is intromission, or depositing sperm in the vagina of the female reproductive tract. Intromission depends on the ability of the penis to become stiff and erect, a state referred to as an erection. The human penis, unlike that of most other mammals, contains no erectile bone. Instead, in order to reach its erect state, it relies entirely on engorgement with blood of its columns of spongy tissue. During sexual arousal, the arteries that supply blood to the penis dilate, allowing more blood to fill the spongy tissue. The now-engorged spongy tissue presses against and constricts the veins that carry blood away from the penis. As a result, more blood enters than leaves the penis, until a constant erectile size is achieved.
In addition to sperm, the penis also transports urine out of the body. These two functions cannot occur simultaneously. During an erection, the sphincters that prevent urine from leaving the bladder are controlled by centres in the brain so they cannot relax and allow urine to enter the urethra.
Testosterone Production
The final major function of the male reproductive system is the production of the male sex hormone testosterone. In mature males, this occurs mainly in the testes. Testosterone production is under the control of luteinizing hormone (LH) from the pituitary gland. LH stimulates Leydig cells in the testes to secrete testosterone.
Testosterone is important for male sexual development at puberty. It stimulates maturation of the male reproductive organs, as well as the development of secondary male sex characteristics (such as facial hair). Testosterone is also needed in mature males for normal spermatogenesis to be maintained in the testes. Follicle stimulating hormone (FSH) from the pituitary gland is also needed for spermatogenesis to occur, in part because it helps Sertoli cells in the testes concentrate testosterone to high enough levels to maintain sperm production. Testosterone is also needed for proper functioning of the prostate gland. In addition, testosterone plays a role in erection, allowing sperm to be deposited within the female reproductive tract.
Feature: My Human Body

If you’re a man and you use a laptop computer on your lap for long periods of time, you may be decreasing your fertility. The reason? A laptop computer generates considerable heat, and its proximity to the scrotum during typical use results in a significant rise in temperature inside the scrotum. Spermatogenesis is very sensitive to high temperatures, so it may be adversely affected by laptop computer use. If you want to avoid the potentially fertility-depressing effect of laptop computer use, you might want to consider using your laptop computer on a table or other surface rather than on your lap — at least when you log on for long computer sessions. Other activities that raise scrotal temperature and have the potential to reduce spermatogenesis including soaking in hot tubs, wearing tight clothing, and biking. Although the effects of short-term scrotal heating on fertility seem to be temporary, years of such heat exposure may cause irreversible effects on sperm production.
18.4 Summary
- Parts of a mature sperm include the head, acrosome, midpiece, and flagellum. The process of producing sperm is called spermatogenesis. This normally starts during puberty, and continues uninterrupted until death.
- Spermatogenesis occurs in the seminiferous tubules in the testes, and requires high concentrations of testosterone. Sertoli cells in the testes play many roles in spermatogenesis, including concentrating testosterone under the influence of follicle stimulating hormone from the pituitary gland.
- Spermatogenesis begins with a diploid stem cell called a spermatogonium, which undergoes mitosis to produce a primary spermatocyte. The primary spermatocyte undergoes meiosis I to produce haploid secondary spermatocytes, and these cells in turn undergo meiosis II to produce spermatids. After the spermatids grow a tail and undergo other changes, they become sperm.
- Before sperm are able to “swim,” they must mature in the epididymis. The mature sperm are then stored in the epididymis until ejaculation occurs.
- Ejaculation is the process in which semen is propelled by peristalsis in the vas deferens and ejaculatory ducts from the urethra in the penis. Semen is a whitish fluid that contains sperm and secretions from the seminal vesicles, prostate gland, and bulbourethral glands. These alkaline secretions are important for sperm survival and motility.
- Besides ejaculating sperm, another reproductive role of the penis is intromission, which is depositing sperm in the female vagina. This requires the penis to become stiff and erect, a state referred to as an erection. Erection usually occurs with sexual arousal as the columns of spongy tissue inside the penis become engorged with blood.
- Leydig cells in the testes secrete testosterone under the control of luteinizing hormone (LH) from the pituitary gland. Testosterone is needed for male sexual development at puberty, and to maintain normal spermatogenesis after puberty. It also plays a role in prostate function and penis’s ability to become erect.
18.4 Review Questions
-
- Compare and contrast the terms: erection, ejaculation, and intromission.
- Describe semen and its components.
- Explain how erection occurs.
18.4 Explore More
How You’re Destroying Your Sperm! Seeker, 2014.
Human Physiology – Reproduction: Spermatogenesis, Janux, 2015.
Attributions
Figure 18.4.1
Sperm-20051108 by Gilberto Santa Rosa from Rio de Janeiro, Brazil on Wikimedia Commons is used under a CC BY 2.0 (https://creativecommons.org/licenses/by/2.0) license.
Figure 18.4.2
Sperm Anatomy by Christinelmiller on Wikimedia Commons is used under a CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0) license.
Figure 18.4.3
Spermatogenesis by OpenStax College is used and adapted by Christine Miller under a CC BY 3.0 (https://creativecommons.org/licenses/by/3.0) license.
Figure 18.4.4
Testis-cross-section by CK-12 Foundation is used under a CC BY-NC 3.0 (https://creativecommons.org/licenses/by-nc/3.0/) license.
Figure 18.4.5
Human_semen_in_a_petri_dish by Digitalkil on Wikimedia Commons is in the public domain (https://en.wikipedia.org/wiki/en:public_domain).
Figure 18.4.6
Laptop by logan-weaver-b76PEyeIptQ-unsplash [photo] by LOGAN WEAVER on Unsplash is used under the Unsplash License (https://unsplash.com/license).
References
Betts, J. G., Young, K.A., Wise, J.A., Johnson, E., Poe, B., Kruse, D.H., Korol, O., Johnson, J.E., Womble, M., DeSaix, P. (2013, June 19). Figure 27.5 Spermatogenesis [digital image]. In Anatomy and Physiology (Section 27.1). OpenStax. https://openstax.org/books/anatomy-and-physiology/pages/27-1-anatomy-and-physiology-of-the-male-reproductive-system
Brainard, J/ CK-12 Foundation. (2016). Figure 4 Cross-section of a testis and seminiferous tubules [digital image]. In CK-12 College Human Biology (Section 20.4) [online Flexbook]. CK12.org. https://www.ck12.org/book/ck-12-college-human-biology/section/20.4/
Janux. (2015, January 10). Human physiology – Reproduction: spermatogenesis. YouTube. https://www.youtube.com/watch?v=krSMZDsjLuU&feature=youtu.be
Seeker. (2014, June 16). How you’re destroying your sperm! YouTube. https://www.youtube.com/watch?v=gNHSTa0Yct4&feature=youtu.be

Crohn’s Rash
If you had a skin rash like the one shown in Figure 15.7.1, you probably wouldn’t assume that it was caused by a digestive system disease. However, that’s exactly why the individual in the picture has a rash. He has a gastrointestinal (GI) tract disorder called Crohn’s disease. This disease is one of a group of GI tract disorders that are known collectively as inflammatory bowel disease. Unlike other inflammatory bowel diseases, signs and symptoms of Crohn’s disease may not be confined to the GI tract.
Inflammatory Bowel Disease
Inflammatory bowel disease (IBD) is a collection of inflammatory conditions primarily affecting the intestines. The two principal inflammatory bowel diseases are Crohn’s disease and ulcerative colitis. Unlike Crohn’s disease — which may affect any part of the GI tract and the joints, as well as the skin — ulcerative colitis mainly affects just the colon and rectum. Both diseases occur when the body’s own immune system attacks the digestive system. Both diseases typically first appear in the late teens or early twenties, and occur equally in males and females. Approximately 270,000 Canadians are currently living with IBD, 7,000 of which are children. The annual cost of caring for these Canadians is estimated at $1.28 billion. The number of cases of IBD has been steadily increasing and it is expected that by 2030 the number of Canadians suffering from IBD will grow to 400,000.
Crohn’s Disease
Crohn’s disease is a type of inflammatory bowel disease that may affect any part of the GI tract from the mouth to the anus, among other body tissues. The most commonly affected region is the ileum, which is the final part of the small intestine. Signs and symptoms of Crohn’s disease typically include abdominal pain, diarrhea (with or without blood), fever, and weight loss. Malnutrition because of faulty absorption of nutrients may also occur. Potential complications of Crohn’s disease include obstructions and abscesses of the bowel. People with Crohn’s disease are also at slightly greater risk than the general population of developing bowel cancer. Although there is a slight reduction in life expectancy in people with Crohn’s disease, if the disease is well-managed, affected people can live full and productive lives. Approximately 135,000 Canadians are living with Crohn's disease.
Crohn’s disease is caused by a combination of genetic and environmental factors that lead to impairment of the generalized immune response (called innate immunity). The chronic inflammation of Crohn’s disease is thought to be the result of the immune system “trying” to compensate for the impairment. Dozens of genes are likely to be involved, only a few of which have been identified. Because of the genetic component, close relatives such as siblings of people with Crohn’s disease are many times more likely to develop the disease than people in the general population. Environmental factors that appear to increase the risk of the disease include smoking tobacco and eating a diet high in animal proteins. Crohn’s disease is typically diagnosed on the basis of a colonoscopy, which provides a direct visual examination of the inside of the colon and the ileum of the small intestine.
People with Crohn’s disease typically experience recurring periods of flare-ups followed by remission. There are no medications or surgical procedures that can cure Crohn’s disease, although medications such as anti-inflammatory or immune-suppressing drugs may alleviate symptoms during flare-ups and help maintain remission. Lifestyle changes, such as dietary modifications and smoking cessation, may also help control symptoms and reduce the likelihood of flare-ups. Surgery may be needed to resolve bowel obstructions, abscesses, or other complications of the disease.
Ulcerative Colitis
Ulcerative colitis is an inflammatory bowel disease that causes inflammation and ulcers (sores) in the colon and rectum. Unlike Crohn’s disease, other parts of the GI tract are rarely affected in ulcerative colitis. The primary symptoms of the disease are lower abdominal pain and bloody diarrhea. Weight loss, fever, and anemia may also be present. Symptoms typically occur intermittently with periods of no symptoms between flare-ups. People with ulcerative colitis have a considerably increased risk of colon cancer and should be screened for colon cancer more frequently than the general population. Ulcerative colitis, however, seems to primarily reduce the quality of life, and not the lifespan.
The exact cause of ulcerative colitis is not known. Theories about its cause involve immune system dysfunction, genetics, changes in normal gut bacteria, and lifestyle factors, such as a diet high in animal protein and the consumption of alcoholic beverages. Genetic involvement is suspected in part because ulcerative colitis tens to “run” in families. It is likely that multiple genes are involved. Diagnosis is typically made on the basis of colonoscopy and tissue biopsies.
Lifestyle changes, such as reducing the consumption of animal protein and alcohol, may improve symptoms of ulcerative colitis. A number of medications are also available to treat symptoms and help prolong remission. These include anti-inflammatory drugs and drugs that suppress the immune system. In cases of severe disease, removal of the colon and rectum may be required and can cure the disease.
Diverticulitis
Diverticulitis is a digestive disease in which tiny pouches in the wall of the large intestine become infected and inflamed. Symptoms typically include lower abdominal pain of sudden onset. There may also be fever, nausea, diarrhea or constipation, and blood in the stool. Having large intestine pouches called diverticula (see Figure 15.7.2) that are not inflamed is called diverticulosis. Diverticulosis is thought to be caused by a combination of genetic and environmental factors, and is more common in people who are obese. Infection and inflammation of the pouches (diverticulitis) occurs in about 10–25% of people with diverticulosis, and is more common at older ages. The infection is generally caused by bacteria.
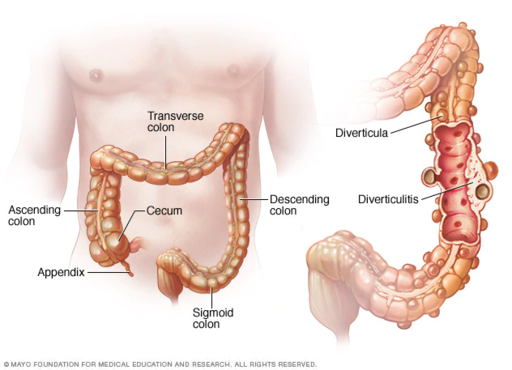
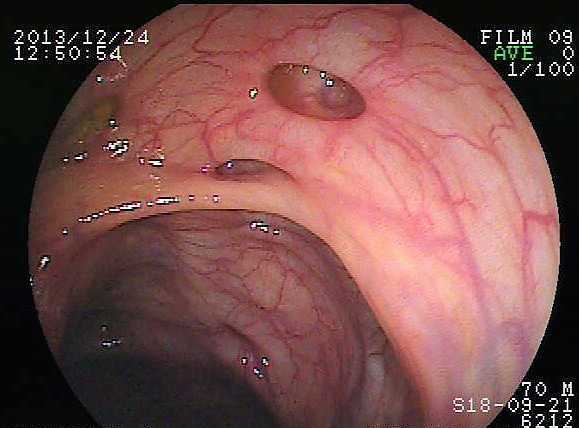
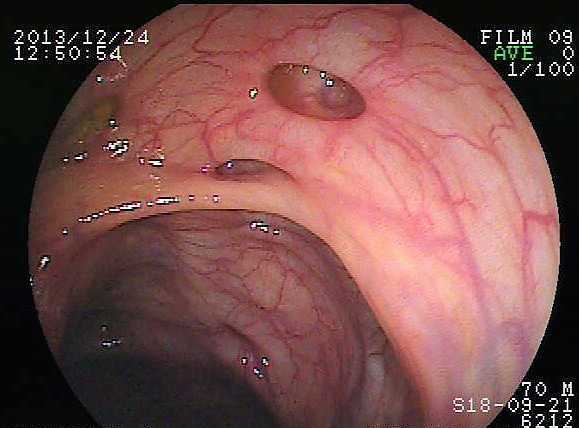
Diverticulitis can usually be diagnosed with a CT scan and can be monitored with a colonoscopy (as seen in Figure 15.7.3). Mild diverticulitis may be treated with oral antibiotics and a short-term liquid diet. For severe cases, intravenous antibiotics, hospitalization, and complete bowel rest (no nourishment via the mouth) may be recommended. Complications such as abscess formation or perforation of the colon require surgery.
Peptic Ulcer
A peptic ulcer is a sore in the lining of the stomach or the duodenum (first part of the small intestine). If the ulcer occurs in the stomach, it is called a gastric ulcer. If it occurs in the duodenum, it is called a duodenal ulcer. The most common symptoms of peptic ulcers are upper abdominal pain that often occurs in the night and improves with eating. Other symptoms may include belching, vomiting, weight loss, and poor appetite. Many people with peptic ulcers, particularly older people, have no symptoms. Peptic ulcers are relatively common, with about ten per cent of people developing a peptic ulcer at some point in their life.
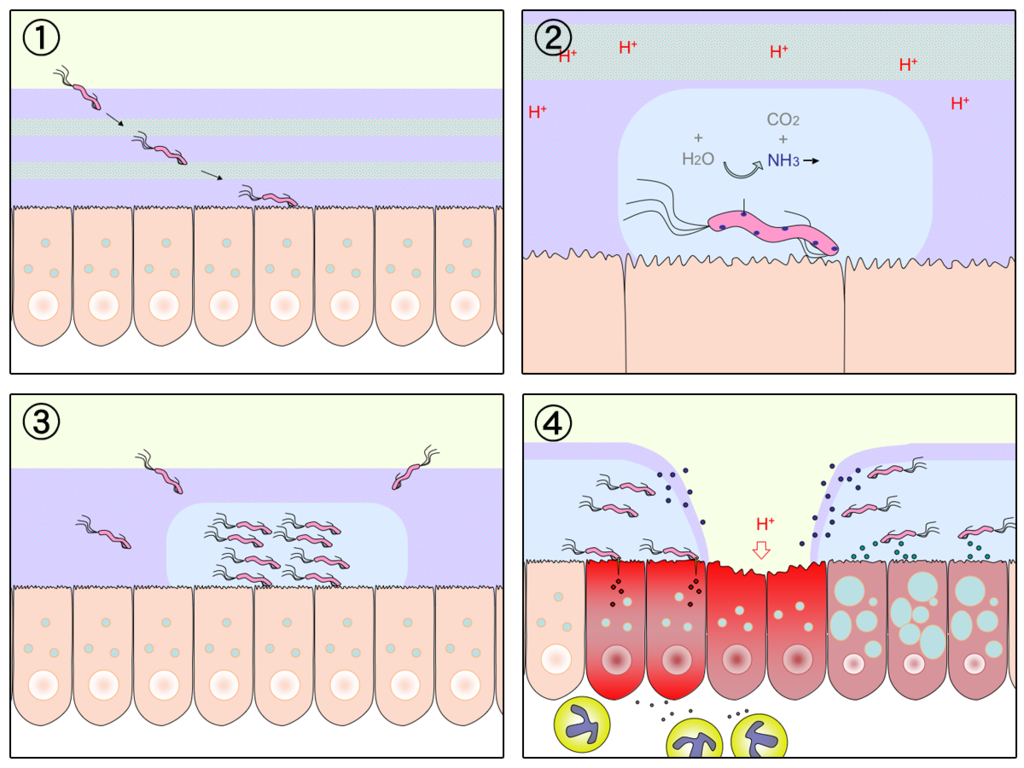
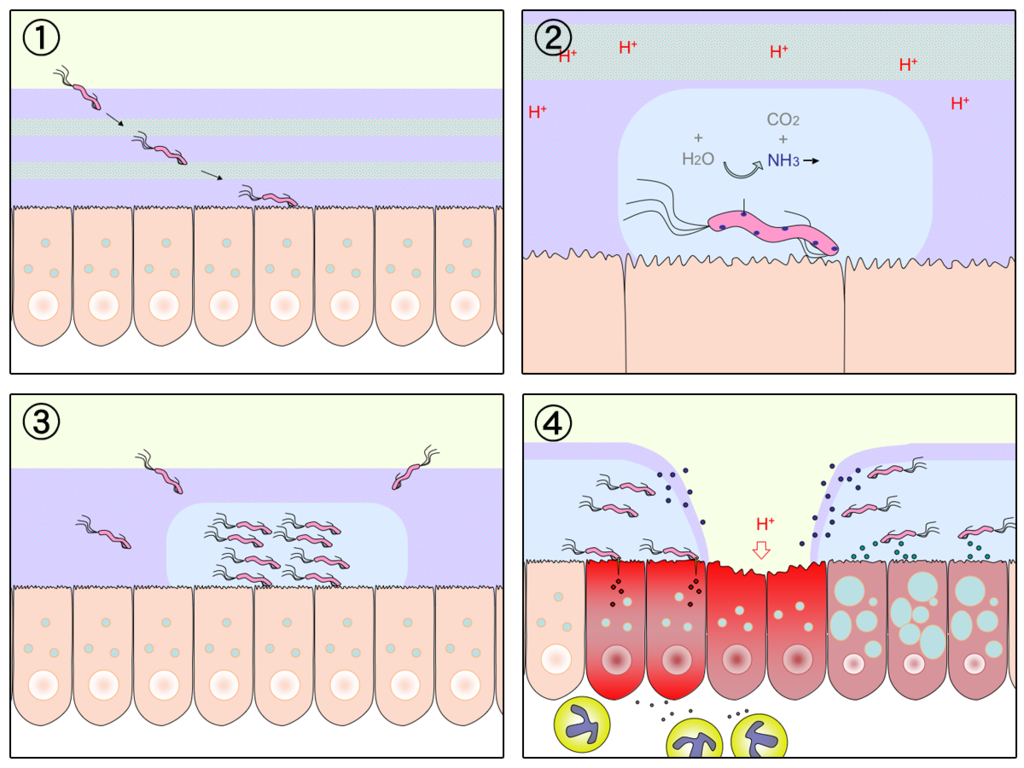
The most common cause of peptic ulcers is infection with the bacterium Helicobacter pylori, which may be transmitted by food, contaminated water, or human saliva (for example, by kissing or sharing eating utensils). Surprisingly, the bacterial cause of peptic ulcers was not discovered until the 1980s. The scientists who made the discovery are Australians Robin Warren and Barry J. Marshall. Although the two scientists eventually won a Nobel Prize for their discovery, their hypothesis was poorly received at first. To demonstrate the validity of their discovery, Marshall used himself in an experiment. He drank a culture of bacteria from a peptic ulcer patient and developed symptoms of peptic ulcer in a matter of days. His symptoms resolved on their own within a couple of weeks, but, at his wife's urging, he took antibiotics to kill any remaining bacteria. Marshall’s self-experiment was published in the Australian Medical Journal, and is among the most cited articles ever published in the journal. Figure 15.7.4 shows how H. pylori cause peptic ulcers.
Another relatively common cause of peptic ulcers is chronic use of non-steroidal anti-inflammatory drugs (NSAIDs), such as aspirin or ibuprofen. Additional contributing factors may include tobacco smoking and stress, although these factors have not been demonstrated conclusively to cause peptic ulcers independent of H. pylori infection. Contrary to popular belief, diet does not appear to play a role in either causing or preventing peptic ulcers. Eating spicy foods and drinking coffee and alcohol were once thought to cause peptic ulcers. These lifestyle choices are no longer thought to have much (if any) of an effect on the development of peptic ulcers.
Peptic ulcers are typically diagnosed on the basis of symptoms or the presence of H. pylori in the GI tract. However, endoscopy (shown in Figure 15.7.5), which allows direct visualization of the stomach and duodenum with a camera, may be required for a definitive diagnosis. Peptic ulcers are usually treated with antibiotics to kill H. pylori, along with medications to temporarily decrease stomach acid and aid in healing. Unfortunately, H. pylori has developed resistance to commonly used antibiotics, so treatment is not always effective. If a peptic ulcer has penetrated so deep into the tissues that it causes a perforation of the wall of the stomach or duodenum, then emergency surgery is needed to repair the damage.

Gastroenteritis
Gastroenteritis, also known as infectious diarrhea or stomach flu, is an acute and usually self-limiting infection of the GI tract by pathogens. Symptoms typically include some combination of diarrhea, vomiting, and abdominal pain. Fever, lack of energy, and dehydration may also occur. The illness generally lasts less than two weeks, even without treatment, but in young children it is potentially deadly. Gastroenteritis is very common, especially in poorer nations. Worldwide, up to five billion cases occur each year, resulting in about 1.4 million deaths.
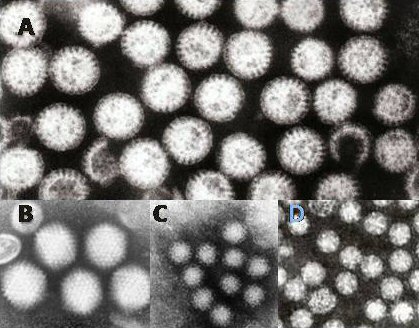
Commonly called “stomach flu,” gastroenteritis is unrelated to the influenza virus, although viruses are the most common cause of the disease (see Figure 15.7.6). In children, rotavirus is most often the cause which is why the British Columbia immunization schedule now includes a rotovirus vaccine. Norovirus is more likely to be the cause of gastroenteritis in adults. Besides viruses, other potential causes of gastroenteritis include fungi, bacteria (most often E. coli or Campylobacter jejuni), and protozoa(including Giardia lamblia, more commonly called Beaver Fever, described below). Transmission of pathogens may occur due to eating improperly prepared foods or foods left to stand at room temperature, drinking contaminated water, or having close contact with an infected individual.
Gastroenteritis is less common in adults than children, partly because adults have acquired immunity after repeated exposure to the most common infectious agents. Adults also tend to have better hygiene than children. If children have frequent repeated incidents of gastroenteritis, they may suffer from malnutrition, stunted growth, and developmental delays. Many cases of gastroenteritis in children can be avoided by giving them a rotavirus vaccine. Frequent and thorough handwashing can cut down on infections caused by other pathogens.
Treatment of gastroenteritis generally involves increasing fluid intake to replace fluids lost in vomiting or diarrhea. Oral rehydration solution, which is a combination of water, salts, and sugar, is often recommended. In severe cases, intravenous fluids may be needed. Antibiotics are not usually prescribed, because they are ineffective against viruses that cause most cases of gastroenteritis.
Giardiasis
Giardiasis, popularly known as beaver fever, is a type of gastroenteritis caused by a GI tract parasite, the single-celled protozoan Giardia lamblia (pictured in Figure 15.7.7). In addition to human beings, the parasite inhabits the digestive tract of a wide variety of domestic and wild animals, including cows, rodents, and sheep, as well as beavers (hence its popular name). Giardiasis is one of the most common parasitic infections in people the world over, with hundreds of millions of people infected worldwide each year.

Transmission of G. lamblia is via a fecal-oral route (as in, you got feces in your food). Those at greatest risk include travelers to countries where giardiasis is common, people who work in child-care settings, backpackers and campers who drink untreated water from lakes or rivers, and people who have close contact with infected people or animals in other settings. In Canada, Giardia is the most commonly identified intestinal parasite and approximately 3,000 Canadians will contract the parasite annually.
Symptoms of giardiasis can vary widely. About one-third third of people with the infection have no symptoms, whereas others have severe diarrhea with poor absorption of nutrients. Problems with absorption occur because the parasites inhibit intestinal digestive enzyme production, cause detrimental changes in microvilli lining the small intestine, and kill off small intestinal epithelial cells. The illness can result in weakness, loss of appetite, stomach cramps, vomiting, and excessive gas. Without treatment, symptoms may continue for several weeks. Treatment with anti-parasitic medications may be needed if symptoms persist longer or are particularly severe.
15.7 Summary
- Inflammatory bowel disease is a collection of inflammatory conditions primarily affecting the intestines. The diseases involve the immune system attacking the GI tract, and they have multiple genetic and environmental causes. Typical symptoms include abdominal pain and diarrhea, which show a pattern of repeated flare-ups interrupted by periods of remission. Lifestyle changes and medications may control flare-ups and extend remission. Surgery is sometimes required.
- The two principal inflammatory bowel diseases are Crohn’s disease and ulcerative colitis. Crohn’s disease may affect any part of the GI tract from the mouth to the anus, among other body tissues. Ulcerative colitis affects the colon and/or rectum.
- Some people have little pouches, called diverticula, in the lining of their large intestine, a condition called diverticulosis. People with diverticulosis may develop diverticulitis, in which one or more of the diverticula become infected and inflamed. Diverticulitis is generally treated with antibiotics and bowel rest. Sometimes, surgery is required.
- A peptic ulcer is a sore in the lining of the stomach (gastric ulcer) or duodenum (duodenal ulcer). The most common cause is infection with the bacterium Helicobacter pylori. NSAIDs (such as aspirin) can also cause peptic ulcers, and some lifestyle factors may play contributing roles. Antibiotics and acid reducers are typically prescribed, and surgery is not often needed.
- Gastroenteritis, or infectious diarrhea, is an acute and usually self-limiting infection of the GI tract by pathogens, most often viruses. Symptoms typically include diarrhea, vomiting, and/or abdominal pain. Treatment includes replacing lost fluids. Antibiotics are not usually effective.
- Giardiasis is a type of gastroenteritis caused by infection of the GI tract with the protozoa parasite Giardia lamblia. It may cause malnutrition. Generally self-limiting, severe or long-lasting cases may require antibiotics.
15.7 Review Questions
-
-
- Compare and contrast Crohn’s disease and ulcerative colitis.
- How are diverticulosis and diverticulitis related?
- Identify the cause of giardiasis. Why may it cause malabsorption?
- Name three disorders of the GI tract that can be caused by bacteria.
- Name one disorder of the GI tract that can be helped by anti-inflammatory medications, and one that can be caused by chronic use of anti-inflammatory medications.
- Describe one reason why it can be dangerous to drink untreated water.
15.7 Explore More
https://youtu.be/H5zin8jKeT0
Who's at risk for colon cancer? - Amit H. Sachdev and Frank G. Gress, TED-Ed, 2018.
https://youtu.be/V_U6czbDHLE
The surprising cause of stomach ulcers - Rusha Modi, TED-Ed, 2017.
Attributions
Figure 15.7.1
BADAS_Crohn by Dayavathi Ashok and Patrick Kiely/ Journal of medical case reports on Wikimedia Commons is used under a CC BY 2.0 (https://creativecommons.org/licenses/by/2.0) license.
Figure 15.7.2
512px-Ds00070_an01934_im00887_divert_s_gif.webp by Lfreeman04 on Wikimedia Commons is used under a CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0) license.
Figure 15.7.3
Colon_diverticulum by melvil on Wikimedia Commons is used under a CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0) license.
Figure 15.7.4
H_pylori_ulcer_diagram by Y_tambe on Wikimedia Commons is used under a CC BY-SA 3.0 (http://creativecommons.org/licenses/by-sa/3.0/) license.
Figure 15.7.5
1024px-Endoscopy_training by Yuya Tamai on Wikimedia Commons is used under a CC BY 2.0 (https://creativecommons.org/licenses/by/2.0) license.
Figure 15.7.6
Gastroenteritis_viruses by Dr. Graham Beards [en:User:Graham Beards] at en.wikipedia on Wikimedia Commons is used under a CC BY 3.0 (https://creativecommons.org/licenses/by/3.0) license.
Figure 15.7.7
Giardia_lamblia_SEM_8698_lores by Janice Haney Carr from CDC/ Public Health Image Library (PHIL) ID# 8698 on Wikimedia Commons is in the public domain (https://en.wikipedia.org/wiki/public_domain).
References
Ashok, D., & Kiely, P. (2007). Bowel associated dermatosis - arthritis syndrome: a case report. Journal of medical case reports, 1, 81. https://doi.org/10.1186/1752-1947-1-81
Marshall, B. J., Armstrong, J. A., McGechie, D. B., & Glancy, R. J. (1985). Attempt to fulfil Koch's postulates for pyloric Campylobacter. The Medical Journal of Australia, 142(8), 436–439.
Marshall, B. J., McGechie, D. B., Rogers, P. A., & Glancy, R. J. (1985). Pyloric campylobacter infection and gastroduodenal disease. The Medical Journal of Australia, 142(8), 439–444.
TED-Ed. (2017, September 28). The surprising cause of stomach ulcers - Rusha Modi. YouTube. https://www.youtube.com/watch?v=V_U6czbDHLE&feature=youtu.be
TED-Ed. (2018, January 4). Who's at risk for colon cancer? - Amit H. Sachdev and Frank G. Gress. YouTube. https://www.youtube.com/watch?v=H5zin8jKeT0&feature=youtu.be
Created by CK-12 Foundation/Adapted by Christine Miller

Crohn’s Rash
If you had a skin rash like the one shown in Figure 15.7.1, you probably wouldn’t assume that it was caused by a digestive system disease. However, that’s exactly why the individual in the picture has a rash. He has a gastrointestinal (GI) tract disorder called Crohn’s disease. This disease is one of a group of GI tract disorders that are known collectively as inflammatory bowel disease. Unlike other inflammatory bowel diseases, signs and symptoms of Crohn’s disease may not be confined to the GI tract.
Inflammatory Bowel Disease
Inflammatory bowel disease (IBD) is a collection of inflammatory conditions primarily affecting the intestines. The two principal inflammatory bowel diseases are Crohn’s disease and ulcerative colitis. Unlike Crohn’s disease — which may affect any part of the GI tract and the joints, as well as the skin — ulcerative colitis mainly affects just the colon and rectum. Both diseases occur when the body’s own immune system attacks the digestive system. Both diseases typically first appear in the late teens or early twenties, and occur equally in males and females. Approximately 270,000 Canadians are currently living with IBD, 7,000 of which are children. The annual cost of caring for these Canadians is estimated at $1.28 billion. The number of cases of IBD has been steadily increasing and it is expected that by 2030 the number of Canadians suffering from IBD will grow to 400,000.
Crohn’s Disease
Crohn’s disease is a type of inflammatory bowel disease that may affect any part of the GI tract from the mouth to the anus, among other body tissues. The most commonly affected region is the ileum, which is the final part of the small intestine. Signs and symptoms of Crohn’s disease typically include abdominal pain, diarrhea (with or without blood), fever, and weight loss. Malnutrition because of faulty absorption of nutrients may also occur. Potential complications of Crohn’s disease include obstructions and abscesses of the bowel. People with Crohn’s disease are also at slightly greater risk than the general population of developing bowel cancer. Although there is a slight reduction in life expectancy in people with Crohn’s disease, if the disease is well-managed, affected people can live full and productive lives. Approximately 135,000 Canadians are living with Crohn's disease.
Crohn’s disease is caused by a combination of genetic and environmental factors that lead to impairment of the generalized immune response (called innate immunity). The chronic inflammation of Crohn’s disease is thought to be the result of the immune system “trying” to compensate for the impairment. Dozens of genes are likely to be involved, only a few of which have been identified. Because of the genetic component, close relatives such as siblings of people with Crohn’s disease are many times more likely to develop the disease than people in the general population. Environmental factors that appear to increase the risk of the disease include smoking tobacco and eating a diet high in animal proteins. Crohn’s disease is typically diagnosed on the basis of a colonoscopy, which provides a direct visual examination of the inside of the colon and the ileum of the small intestine.
People with Crohn’s disease typically experience recurring periods of flare-ups followed by remission. There are no medications or surgical procedures that can cure Crohn’s disease, although medications such as anti-inflammatory or immune-suppressing drugs may alleviate symptoms during flare-ups and help maintain remission. Lifestyle changes, such as dietary modifications and smoking cessation, may also help control symptoms and reduce the likelihood of flare-ups. Surgery may be needed to resolve bowel obstructions, abscesses, or other complications of the disease.
Ulcerative Colitis
Ulcerative colitis is an inflammatory bowel disease that causes inflammation and ulcers (sores) in the colon and rectum. Unlike Crohn’s disease, other parts of the GI tract are rarely affected in ulcerative colitis. The primary symptoms of the disease are lower abdominal pain and bloody diarrhea. Weight loss, fever, and anemia may also be present. Symptoms typically occur intermittently with periods of no symptoms between flare-ups. People with ulcerative colitis have a considerably increased risk of colon cancer and should be screened for colon cancer more frequently than the general population. Ulcerative colitis, however, seems to primarily reduce the quality of life, and not the lifespan.
The exact cause of ulcerative colitis is not known. Theories about its cause involve immune system dysfunction, genetics, changes in normal gut bacteria, and lifestyle factors, such as a diet high in animal protein and the consumption of alcoholic beverages. Genetic involvement is suspected in part because ulcerative colitis tens to “run” in families. It is likely that multiple genes are involved. Diagnosis is typically made on the basis of colonoscopy and tissue biopsies.
Lifestyle changes, such as reducing the consumption of animal protein and alcohol, may improve symptoms of ulcerative colitis. A number of medications are also available to treat symptoms and help prolong remission. These include anti-inflammatory drugs and drugs that suppress the immune system. In cases of severe disease, removal of the colon and rectum may be required and can cure the disease.
Diverticulitis
Diverticulitis is a digestive disease in which tiny pouches in the wall of the large intestine become infected and inflamed. Symptoms typically include lower abdominal pain of sudden onset. There may also be fever, nausea, diarrhea or constipation, and blood in the stool. Having large intestine pouches called diverticula (see Figure 15.7.2) that are not inflamed is called diverticulosis. Diverticulosis is thought to be caused by a combination of genetic and environmental factors, and is more common in people who are obese. Infection and inflammation of the pouches (diverticulitis) occurs in about 10–25% of people with diverticulosis, and is more common at older ages. The infection is generally caused by bacteria.
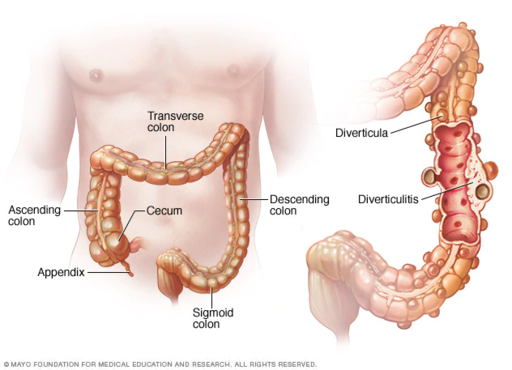
Diverticulitis can usually be diagnosed with a CT scan and can be monitored with a colonoscopy (as seen in Figure 15.7.3). Mild diverticulitis may be treated with oral antibiotics and a short-term liquid diet. For severe cases, intravenous antibiotics, hospitalization, and complete bowel rest (no nourishment via the mouth) may be recommended. Complications such as abscess formation or perforation of the colon require surgery.
Peptic Ulcer
A peptic ulcer is a sore in the lining of the stomach or the duodenum (first part of the small intestine). If the ulcer occurs in the stomach, it is called a gastric ulcer. If it occurs in the duodenum, it is called a duodenal ulcer. The most common symptoms of peptic ulcers are upper abdominal pain that often occurs in the night and improves with eating. Other symptoms may include belching, vomiting, weight loss, and poor appetite. Many people with peptic ulcers, particularly older people, have no symptoms. Peptic ulcers are relatively common, with about ten per cent of people developing a peptic ulcer at some point in their life.
The most common cause of peptic ulcers is infection with the bacterium Helicobacter pylori, which may be transmitted by food, contaminated water, or human saliva (for example, by kissing or sharing eating utensils). Surprisingly, the bacterial cause of peptic ulcers was not discovered until the 1980s. The scientists who made the discovery are Australians Robin Warren and Barry J. Marshall. Although the two scientists eventually won a Nobel Prize for their discovery, their hypothesis was poorly received at first. To demonstrate the validity of their discovery, Marshall used himself in an experiment. He drank a culture of bacteria from a peptic ulcer patient and developed symptoms of peptic ulcer in a matter of days. His symptoms resolved on their own within a couple of weeks, but, at his wife's urging, he took antibiotics to kill any remaining bacteria. Marshall’s self-experiment was published in the Australian Medical Journal, and is among the most cited articles ever published in the journal. Figure 15.7.4 shows how H. pylori cause peptic ulcers.
Another relatively common cause of peptic ulcers is chronic use of non-steroidal anti-inflammatory drugs (NSAIDs), such as aspirin or ibuprofen. Additional contributing factors may include tobacco smoking and stress, although these factors have not been demonstrated conclusively to cause peptic ulcers independent of H. pylori infection. Contrary to popular belief, diet does not appear to play a role in either causing or preventing peptic ulcers. Eating spicy foods and drinking coffee and alcohol were once thought to cause peptic ulcers. These lifestyle choices are no longer thought to have much (if any) of an effect on the development of peptic ulcers.
Peptic ulcers are typically diagnosed on the basis of symptoms or the presence of H. pylori in the GI tract. However, endoscopy (shown in Figure 15.7.5), which allows direct visualization of the stomach and duodenum with a camera, may be required for a definitive diagnosis. Peptic ulcers are usually treated with antibiotics to kill H. pylori, along with medications to temporarily decrease stomach acid and aid in healing. Unfortunately, H. pylori has developed resistance to commonly used antibiotics, so treatment is not always effective. If a peptic ulcer has penetrated so deep into the tissues that it causes a perforation of the wall of the stomach or duodenum, then emergency surgery is needed to repair the damage.

Gastroenteritis
Gastroenteritis, also known as infectious diarrhea or stomach flu, is an acute and usually self-limiting infection of the GI tract by pathogens. Symptoms typically include some combination of diarrhea, vomiting, and abdominal pain. Fever, lack of energy, and dehydration may also occur. The illness generally lasts less than two weeks, even without treatment, but in young children it is potentially deadly. Gastroenteritis is very common, especially in poorer nations. Worldwide, up to five billion cases occur each year, resulting in about 1.4 million deaths.
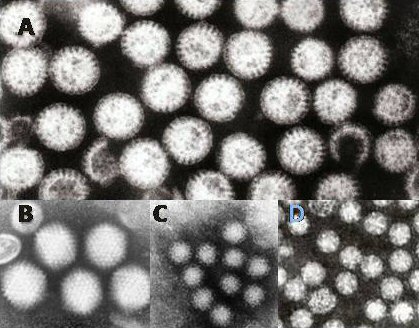
Commonly called “stomach flu,” gastroenteritis is unrelated to the influenza virus, although viruses are the most common cause of the disease (see Figure 15.7.6). In children, rotavirus is most often the cause which is why the British Columbia immunization schedule now includes a rotovirus vaccine. Norovirus is more likely to be the cause of gastroenteritis in adults. Besides viruses, other potential causes of gastroenteritis include fungi, bacteria (most often E. coli or Campylobacter jejuni), and protozoa(including Giardia lamblia, more commonly called Beaver Fever, described below). Transmission of pathogens may occur due to eating improperly prepared foods or foods left to stand at room temperature, drinking contaminated water, or having close contact with an infected individual.
Gastroenteritis is less common in adults than children, partly because adults have acquired immunity after repeated exposure to the most common infectious agents. Adults also tend to have better hygiene than children. If children have frequent repeated incidents of gastroenteritis, they may suffer from malnutrition, stunted growth, and developmental delays. Many cases of gastroenteritis in children can be avoided by giving them a rotavirus vaccine. Frequent and thorough handwashing can cut down on infections caused by other pathogens.
Treatment of gastroenteritis generally involves increasing fluid intake to replace fluids lost in vomiting or diarrhea. Oral rehydration solution, which is a combination of water, salts, and sugar, is often recommended. In severe cases, intravenous fluids may be needed. Antibiotics are not usually prescribed, because they are ineffective against viruses that cause most cases of gastroenteritis.
Giardiasis
Giardiasis, popularly known as beaver fever, is a type of gastroenteritis caused by a GI tract parasite, the single-celled protozoan Giardia lamblia (pictured in Figure 15.7.7). In addition to human beings, the parasite inhabits the digestive tract of a wide variety of domestic and wild animals, including cows, rodents, and sheep, as well as beavers (hence its popular name). Giardiasis is one of the most common parasitic infections in people the world over, with hundreds of millions of people infected worldwide each year.

Transmission of G. lamblia is via a fecal-oral route (as in, you got feces in your food). Those at greatest risk include travelers to countries where giardiasis is common, people who work in child-care settings, backpackers and campers who drink untreated water from lakes or rivers, and people who have close contact with infected people or animals in other settings. In Canada, Giardia is the most commonly identified intestinal parasite and approximately 3,000 Canadians will contract the parasite annually.
Symptoms of giardiasis can vary widely. About one-third third of people with the infection have no symptoms, whereas others have severe diarrhea with poor absorption of nutrients. Problems with absorption occur because the parasites inhibit intestinal digestive enzyme production, cause detrimental changes in microvilli lining the small intestine, and kill off small intestinal epithelial cells. The illness can result in weakness, loss of appetite, stomach cramps, vomiting, and excessive gas. Without treatment, symptoms may continue for several weeks. Treatment with anti-parasitic medications may be needed if symptoms persist longer or are particularly severe.
15.7 Summary
- Inflammatory bowel disease is a collection of inflammatory conditions primarily affecting the intestines. The diseases involve the immune system attacking the GI tract, and they have multiple genetic and environmental causes. Typical symptoms include abdominal pain and diarrhea, which show a pattern of repeated flare-ups interrupted by periods of remission. Lifestyle changes and medications may control flare-ups and extend remission. Surgery is sometimes required.
- The two principal inflammatory bowel diseases are Crohn’s disease and ulcerative colitis. Crohn’s disease may affect any part of the GI tract from the mouth to the anus, among other body tissues. Ulcerative colitis affects the colon and/or rectum.
- Some people have little pouches, called diverticula, in the lining of their large intestine, a condition called diverticulosis. People with diverticulosis may develop diverticulitis, in which one or more of the diverticula become infected and inflamed. Diverticulitis is generally treated with antibiotics and bowel rest. Sometimes, surgery is required.
- A peptic ulcer is a sore in the lining of the stomach (gastric ulcer) or duodenum (duodenal ulcer). The most common cause is infection with the bacterium Helicobacter pylori. NSAIDs (such as aspirin) can also cause peptic ulcers, and some lifestyle factors may play contributing roles. Antibiotics and acid reducers are typically prescribed, and surgery is not often needed.
- Gastroenteritis, or infectious diarrhea, is an acute and usually self-limiting infection of the GI tract by pathogens, most often viruses. Symptoms typically include diarrhea, vomiting, and/or abdominal pain. Treatment includes replacing lost fluids. Antibiotics are not usually effective.
- Giardiasis is a type of gastroenteritis caused by infection of the GI tract with the protozoa parasite Giardia lamblia. It may cause malnutrition. Generally self-limiting, severe or long-lasting cases may require antibiotics.
15.7 Review Questions
-
-
- Compare and contrast Crohn’s disease and ulcerative colitis.
- How are diverticulosis and diverticulitis related?
- Identify the cause of giardiasis. Why may it cause malabsorption?
- Name three disorders of the GI tract that can be caused by bacteria.
- Name one disorder of the GI tract that can be helped by anti-inflammatory medications, and one that can be caused by chronic use of anti-inflammatory medications.
- Describe one reason why it can be dangerous to drink untreated water.
15.7 Explore More
https://youtu.be/H5zin8jKeT0
Who's at risk for colon cancer? - Amit H. Sachdev and Frank G. Gress, TED-Ed, 2018.
https://youtu.be/V_U6czbDHLE
The surprising cause of stomach ulcers - Rusha Modi, TED-Ed, 2017.
Attributions
Figure 15.7.1
BADAS_Crohn by Dayavathi Ashok and Patrick Kiely/ Journal of medical case reports on Wikimedia Commons is used under a CC BY 2.0 (https://creativecommons.org/licenses/by/2.0) license.
Figure 15.7.2
512px-Ds00070_an01934_im00887_divert_s_gif.webp by Lfreeman04 on Wikimedia Commons is used under a CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0) license.
Figure 15.7.3
Colon_diverticulum by melvil on Wikimedia Commons is used under a CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0) license.
Figure 15.7.4
H_pylori_ulcer_diagram by Y_tambe on Wikimedia Commons is used under a CC BY-SA 3.0 (http://creativecommons.org/licenses/by-sa/3.0/) license.
Figure 15.7.5
1024px-Endoscopy_training by Yuya Tamai on Wikimedia Commons is used under a CC BY 2.0 (https://creativecommons.org/licenses/by/2.0) license.
Figure 15.7.6
Gastroenteritis_viruses by Dr. Graham Beards [en:User:Graham Beards] at en.wikipedia on Wikimedia Commons is used under a CC BY 3.0 (https://creativecommons.org/licenses/by/3.0) license.
Figure 15.7.7
Giardia_lamblia_SEM_8698_lores by Janice Haney Carr from CDC/ Public Health Image Library (PHIL) ID# 8698 on Wikimedia Commons is in the public domain (https://en.wikipedia.org/wiki/public_domain).
References
Ashok, D., & Kiely, P. (2007). Bowel associated dermatosis - arthritis syndrome: a case report. Journal of medical case reports, 1, 81. https://doi.org/10.1186/1752-1947-1-81
Marshall, B. J., Armstrong, J. A., McGechie, D. B., & Glancy, R. J. (1985). Attempt to fulfil Koch's postulates for pyloric Campylobacter. The Medical Journal of Australia, 142(8), 436–439.
Marshall, B. J., McGechie, D. B., Rogers, P. A., & Glancy, R. J. (1985). Pyloric campylobacter infection and gastroduodenal disease. The Medical Journal of Australia, 142(8), 439–444.
TED-Ed. (2017, September 28). The surprising cause of stomach ulcers - Rusha Modi. YouTube. https://www.youtube.com/watch?v=V_U6czbDHLE&feature=youtu.be
TED-Ed. (2018, January 4). Who's at risk for colon cancer? - Amit H. Sachdev and Frank G. Gress. YouTube. https://www.youtube.com/watch?v=H5zin8jKeT0&feature=youtu.be
Image shows a photograph of a basket full of sliced bread.
A whip-like structure that allows a cell to move.
A biological process which converts sugars such as glucose, fructose, and sucrose into cellular energy, producing ethanol and carbon dioxide as by-products.
Image shows a diagram of all the locations that chemical and mechanical digestion take place along the GI tract. In the mouth and pharynx, mechanical digestion includes chewing and swallowing and chemical digestion of carbohydrates and fats occurs. In the stomach, mechanical digestion includes peristaltic mixing and propulsion, and the chemical digestion of proteins and fats occurs. In the small intestine, mechanical digestion includes mixing and propulsion, and chemical digestion of carbohydrates, fats, polypeptides and nucleic acids takes place.
Image shows a scanning electroflourescent pictomicrograph. It shows the villi of the small intestine, with a layer of mucus, and then a multitude of smaller bacterial cells above the mucous.
A substance that takes part in and undergoes change during a chemical reaction.

Head Stand
Did you ever wonder what would happen if you tried to swallow food while standing on your head like this person in Figure 15.4.1? Many people think that food travels down the gullet from the mouth by the force of gravity. If that were the case, then food you swallowed would stay in your throat while you were standing on your head. In reality, your position doesn’t have much to do with your ability to swallow. Food will travel from your mouth to your stomach whether you are standing upright or upside down. That’s because the tube the food travels through — the esophagus — moves the food along via muscular contractions known as peristalsis. The esophagus is one of several organs that make up the upper gastrointestinal tract.
Organs of the Upper Gastrointestinal Tract
Besides the esophagus, organs of the upper gastrointestinal (GI) tract include the mouth, pharynx, and stomach. These hollow organs are all connected to form a tube through which food passes during digestion. The only role in digestion played by the pharynx and esophagus is to move food through the GI tract. The mouth and stomach, in contrast, are organs where digestion — or the breakdown of food — also occurs. In both of these organs, food is broken into smaller pieces (mechanical digestion), as well as broken down chemically (chemical digestion). It should be noted that the first part of the small intestine (duodenum) is considered in some contexts to be part of the upper GI tract, but that practice is not followed here.
Mouth
The mouth is the first organ of the GI tract. Most of the oral cavity is lined with mucous membrane. This tissue produces mucus, which helps moisten, soften, and lubricate food. Underlying the mucous membrane is a thin layer of smooth muscle to which the mucous membrane is only loosely connected. This gives the mucous membrane considerable ability to stretch as you eat food. The roof of the mouth, called the palate, separates the oral cavity from the nasal cavity. The front part is hard, consisting of mucous membrane covering a plate of bone. The back part of the palate is softer and more pliable, consisting of mucous membrane over muscle and connective tissue. The hard surface of the front of the palate allows for pressure needed in chewing and mixing food. The soft, pliable surface of the back of the palate can move to accommodate the passage of food while swallowing. Muscles at either side of the soft palate contract to create the swallowing action.
Several specific structures in the mouth are specialized for digestion. These include salivary glands, tongue, and teeth.
Salivary Glands
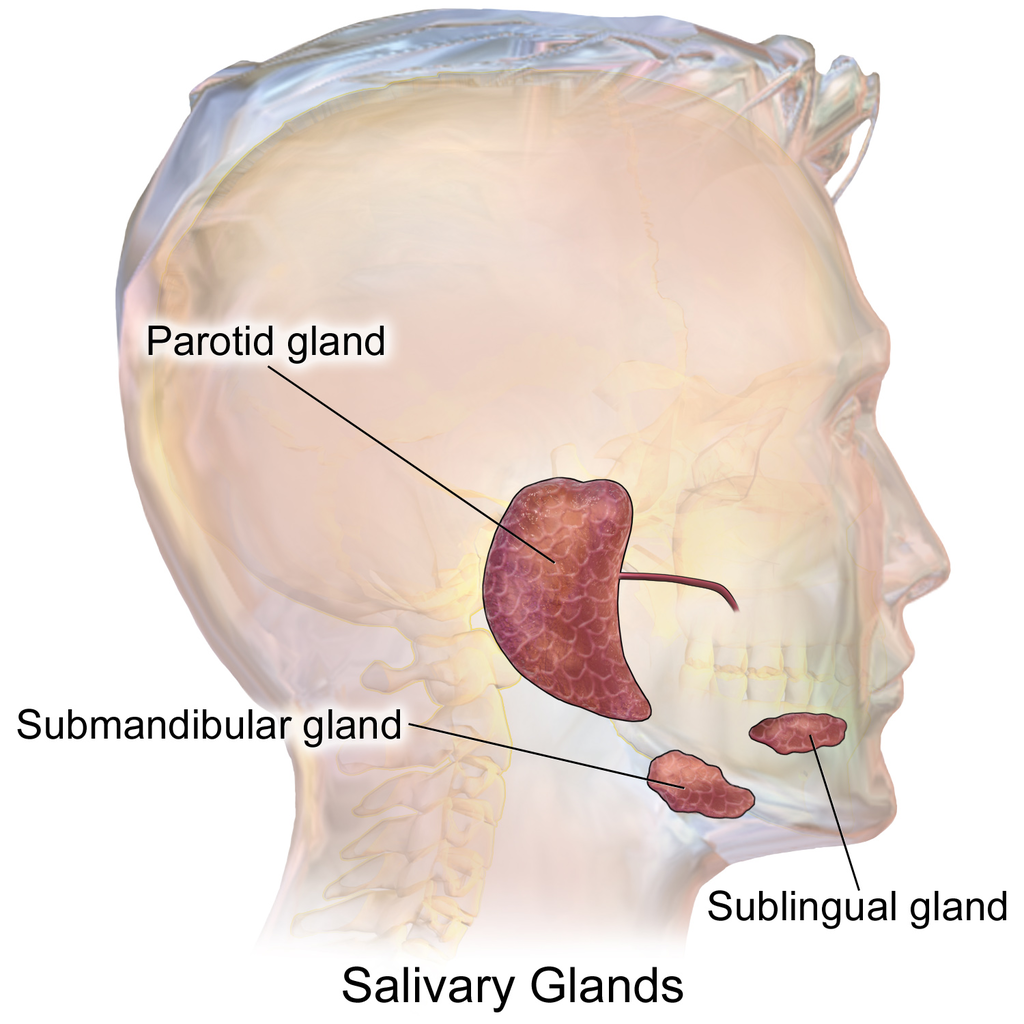
The mouth contains three pairs of major salivary glands, shown in Figure 15.4.2. These three pairs are all exocrine glands that secrete saliva into the mouth through ducts.
- The largest of the three major pairs of salivary glands are the parotid glands, which are located on either side of the mouth in front of the ears.
- The next largest pair is the submandibular glands, located beneath the lower jaw.
- The third pair is the sublingual glands, located underneath the tongue.
In addition to these three pairs of major salivary glands, there are also hundreds of minor salivary glands in the oral mucosa lining the mouth and on the tongue. Along with the major glands, most of the minor glands secrete the digestive enzyme amylase, which begins the chemical digestion of starch and glycogen (polysaccharides). However, the minor salivary glands on the tongue secrete the fat-digesting enzyme lipase, which in the mouth is called lingual lipase (to distinguish it from pancreatic lipase secreted by the pancreas).
Saliva secreted by the salivary glands mainly helps digestion, but it also plays other roles. It helps maintain dental health by cleaning the teeth, and it contains antibodies that help protect against infection. By keeping the mouth lubricated, saliva also allows the mouth movements needed for speech.
Tongue
The tongue is a fleshy, muscular organ that is attached to the floor of the mouth by a band of ligaments that gives it great mobility. This is necessary so the tongue can manipulate food for chewing and swallowing. Movements of the tongue are also necessary for speaking. The upper surface of the tongue is covered with tiny projections called papillae, which contain taste buds. The latter are collections of chemoreceptor cells (shown in Figure 15.4.3). These sensory cells sense chemicals in food and send the information to the brain via cranial nerves, thus enabling the sense of taste.
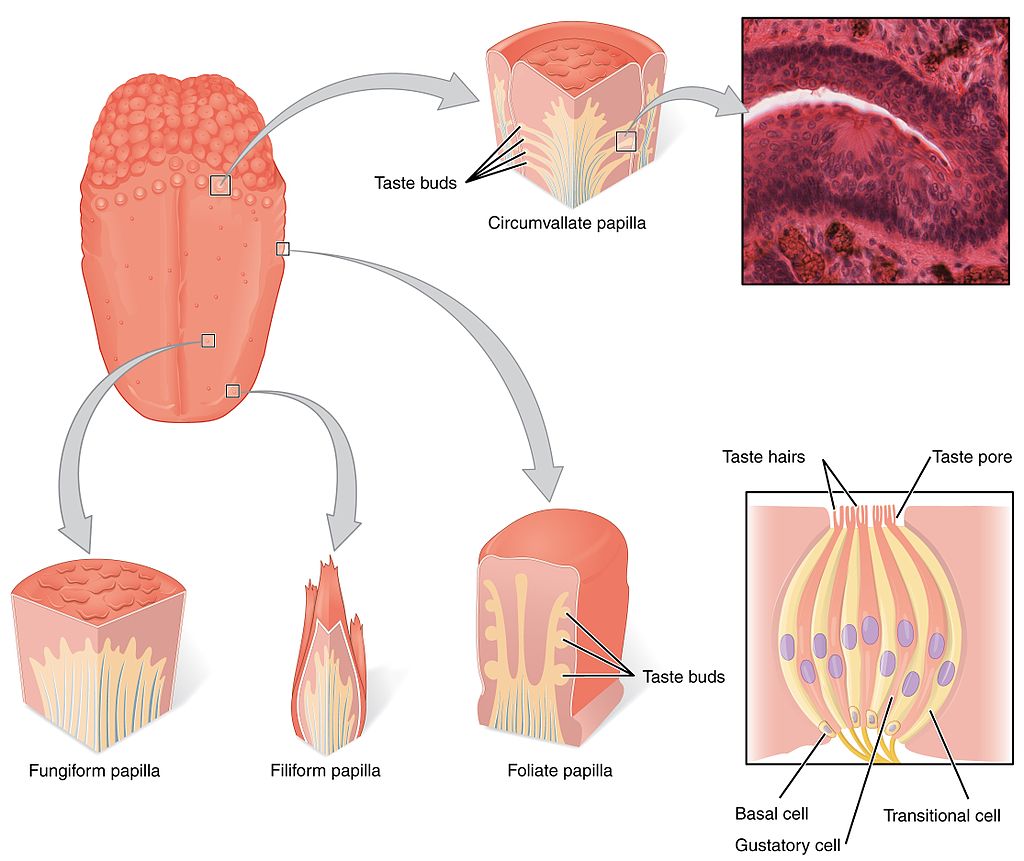
There are five basic tastes detected by the chemoreceptor cells in taste buds: saltiness, sourness, bitterness, sweetness, and umami (often described as a meaty taste). Contrary to popular belief, taste buds for the five basic tastes are not located on different parts of the tongue. Why does taste matter? The taste of food helps to stimulate the secretion of saliva from the salivary glands. It also helps us to eat foods that are good for us, instead of rotten or toxic foods. The detection of saltiness, for example, enables the control of salt intake and salt balance in the body. The detection of sourness may help us avoid spoiled foods, which often taste sour due to fermentation by bacteria. The detection of bitterness warns of poisons, because many plants defend themselves with toxins that taste bitter. The detection of sweetness guides us to foods that supply quick energy. The detection of umami may signal protein-rich foods.
Teeth
The teeth are complex structures made of a bone-like material called dentin and covered with enamel, which is the hardest tissue in the body. Adults normally have a total of 32 teeth, with 16 in each jaw. The right and left sides of each jaw are mirror images in terms of the numbers and types of teeth they contain. Teeth have different shapes to suit them for different aspects of mastication (chewing). The different types of teeth are illustrated in Figure 15.4.4.
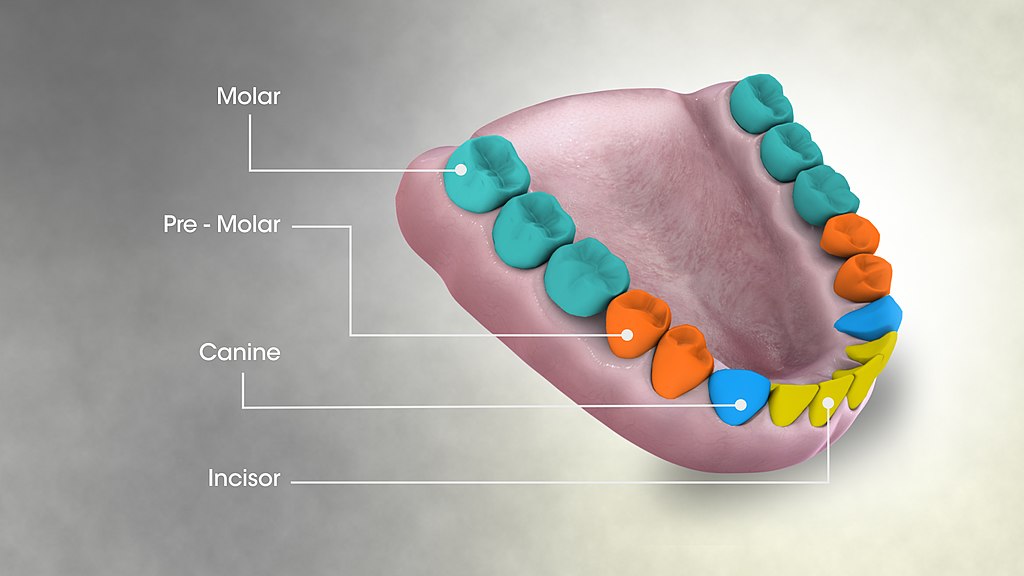
- Incisors are the sharp, blade-like teeth at the front of the mouth. They are used for cutting or biting off pieces of food. In adults, there are normally four incisors in each jaw, or eight in total.
- Canines are the pointed teeth on either side of the incisors. They are used for tearing foods that are tough or stringy. Adults normally have two canines in each jaw, or four altogether.
- Premolars and molars are cuboid teeth with cusps and grooves that are located on the sides and toward the back of the jaws. Premolars are closer to the front of the mouth. Molars are larger and have more cusps than premolars, but both are used for crushing and grinding food. Adults normally have two premolars and three molars on each side of each jaw, for a total of eight premolars and twelve molars.
Pharynx
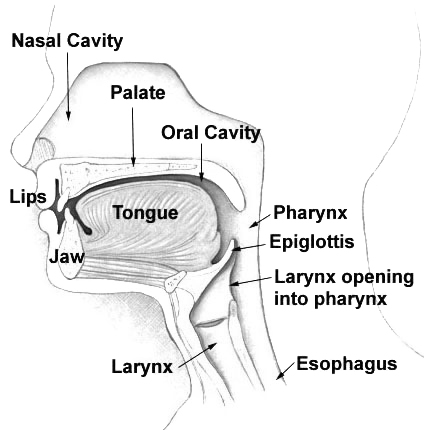
The tube-like pharynx (see Figure 15.4.5 below) plays a dual role as an organ of both respiration and digestion. As part of the respiratory system, it conducts air between the nasal cavity and larynx. As part of the digestive system, it allows swallowed food to pass from the oral cavity to the esophagus. Anything swallowed has priority over inhaled air when passing through the pharynx. During swallowing, the backward motion of the tongue causes a flap of elastic cartilage — called the epiglottis — to close over the opening to the larynx. This prevents food or drink from entering the larynx.
Esophagus
The esophagus (shown in Figure 15.4.6) is a muscular tube through which food is pushed from the pharynx to the stomach. The esophagus passes through an opening in the diaphragm (the large breathing muscle that separates the abdomen from the thorax) before reaching the stomach. In adults, the esophagus averages about 25 cm (about 9.8 inches) in length, depending on a person’s height. The inner lining of the esophagus consists of mucous membrane, which provides a smooth, slippery surface for the passage of food. The cells of this membrane are constantly being replaced as they are worn away from the frequent passage of food over them.
When food is not being swallowed, the esophagus is closed at both ends by upper and lower esophageal sphincters. Sphincters are rings of muscle that can contract to close off openings between structures. The upper esophageal sphincter is triggered to relax and open by the act of swallowing, allowing a bolus of food to enter the esophagus from the pharynx. Then, the esophageal sphincter closes again to prevent food from moving back into the pharynx from the esophagus.
Once in the esophagus, the food bolus travels down to the stomach, pushed along by the rhythmic contraction and relaxation of muscles (peristalsis). The lower esophageal sphincter is located at the junction between the esophagus and the stomach. This sphincter opens when the bolus reaches it, allowing the food to enter the stomach. The sphincter normally remains closed at other times to prevent the contents of the stomach from entering the esophagus. Failure of this sphincter to remain completely closed can lead to heartburn. If it happens chronically, it can lead to gastroesophageal reflux disease (GERD), in which the mucous membrane of the esophagus may become damaged by the highly acidic contents of the stomach.
See the video below to see how the parts of the upper GI tract work together to carry out swallowing:
https://youtu.be/pNcV6yAfq-g
Swallowing, uploaded by Alejandra Cork, 2012.
Stomach
The stomach is a J-shaped organ (shown in Figure 15.4.7) that is joined to the esophagus at its upper end, and to the first part of the small intestine (duodenum) at its lower end. When the stomach is empty of food, it normally has a volume of about 75 millilitres, but it can expand to hold up to about a litre of food. Waves of muscle contractions (peristalsis) passing through the muscular walls of the stomach cause the food inside to be mixed and churned. The wall of the stomach has an extra layer of muscle tissue not found in other organs of the GI tract that helps it squeeze and mix the food. These movements of the stomach wall contribute greatly to mechanical digestion by breaking the food into much smaller pieces. The churning also helps mix the food with stomach secretions that aid in its chemical digestion.
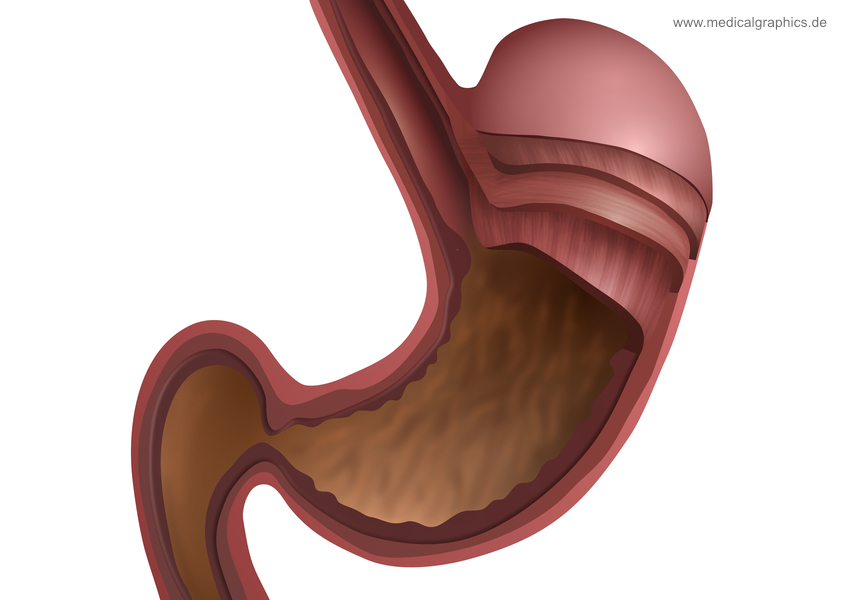
Secretions of the stomach include gastric acid, which consists mainly of hydrochloric acid (HCl). This makes the stomach contents highly acidic, which is necessary so that the enzyme pepsin — also secreted by the stomach — can begin the digestion of protein. Mucus is secreted by the lining of stomach to provide a slimy protective coating against the otherwise damaging effects of gastric acid. The fat-digesting enzyme lipase is secreted in small amounts in the stomach, but very little fat digestion occurs there.
By the time food has been in the stomach for about an hour, it has become the thick, semi-liquid chyme. When the small intestine is ready to receive chyme, a sphincter between the stomach and duodenum — called the pyloric sphincter — opens to allow the chyme to enter the small intestine for further digestion and absorption.
Feature: Reliable Sources
The ongoing epidemic of obesity in the wealthier nations of the world, including Canada, has led to the development of several different bariatric surgeries that modify the stomach to help obese patients reduce their food intake and lose weight. Go online to learn more about bariatric surgery. Find sources you judge to be reliable that answer the following questions:
- Who qualifies for bariatric surgery?
- Describe the bariatric surgeries commonly called stomach stapling, lap band, and gastric sleeve. How does each type of surgery modify the stomach? In terms of weight loss, how effective is each type?
- What are the major potential risks of bariatric surgery?
- Besides weight loss, what other benefits have been shown to result from bariatric surgery?
15.4 Summary
- Organs of the upper gastrointestinal (GI) tract include the mouth, pharynx, esophagus, and stomach.
- The mouth is the first organ of the GI tract. It has several structures that are specialized for digestion, including salivary glands, tongue, and teeth. Both mechanical digestion and chemical digestion of carbohydrates and fats begin in the mouth.
- The pharynx and esophagus move food from the mouth to the stomach, but are not involved in the process of digestion or absorption. Food moves through the esophagus by peristalsis.
- Mechanical and chemical digestion continue in the stomach. Acid and digestive enzymes secreted by the stomach start the chemical digestion of proteins. The stomach turns masticated food into a semi-fluid mixture called chyme.
15.4 Review Questions
-
- Identify structures in the mouth that are specialized for digestion.
- Describe digestion in the mouth.
- What general role do the pharynx and esophagus play in the digestion of food?
- How does food travel through the esophagus?
- Describe digestion in the stomach.
- Describe the differences between how air and food normally move past the pharynx.
- Name two structures in the mouth that contribute to mechanical digestion.
- What structure normally keeps stomach contents from backing up into the esophagus?
- Thirty minutes after you eat a meal, where is most of your food located? Explain your answer.
- What are two roles of mucus in the upper GI tract?
15.4 Explore More
https://youtu.be/zGoBFU1q4g0
What causes cavities? - Mel Rosenberg, TED-Ed, 2016.
https://youtu.be/gCrmFbgT37I
How does alcohol make you drunk? - Judy Grisel, TED-Ed, 2020.
https://youtu.be/twJBEypJDfU
Gastric Bypass Surgery: One Patient’s Journey - Mayo Clinic, 2014.
https://youtu.be/u_1sVri3b2w
Here's What Happens In Your Body When You Swallow Gum | The Human Body, Tech Insider, 2018.
Attributions
Figure 15.4.1
Handstand, Pender Island, B.C. [photo] by Jasper Garratt on Unsplash is used under the Unsplash License (https://unsplash.com/license).
Figure 15.4.2
Blausen_0780_SalivaryGlands by BruceBlaus on Wikimedia Commons is used under a CC BY 3.0 (https://creativecommons.org/licenses/by/3.0) license.
Figure 15.4.3
1402_The_Tongue by OpenStax on Wikimedia Commons is used under a CC BY 4.0 (https://creativecommons.org/licenses/by/4.0) license.
Figure 15.4.4
1024px-3D_Medical_Animation_Still_Showing_Types_of_Teeth by http://www.scientificanimations.com on Wikimedia Commons is used under a CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0) license.
Figure 15.4.5
Illu01_head_neck by Arcadian from NCI/ SEER Training Modules on Wikimedia Common is in the public domain (https://en.wikipedia.org/wiki/public_domain).
Figure 15.4.6
ZenkerSchraeg by Bernd Brägelmann Braegel on Wikimedia Commons is used under a CC BY 3.0 (https://creativecommons.org/licenses/by/3.0) license. (Courtesy of Dr. Martin Steinhoff. It is not known whether there is a possibly necessary approval from the patient.)
Figure 15.4.7
Anatomy stomach – white by www.medicalgraphics.de from MedicalGraphics is used under a CC BY-ND 4.0 (https://creativecommons.org/licenses/by-nd/4.0/) license.
References
Alejandra Cork. (2012). Swallowing. YouTube. https://www.youtube.com/watch?v=pNcV6yAfq-g&t=4s
Betts, J. G., Young, K.A., Wise, J.A., Johnson, E., Poe, B., Kruse, D.H., Korol, O., Johnson, J.E., Womble, M., DeSaix, P. (2016, May 27). Figure 14.3 The tongue [digital image]. In Anatomy and Physiology (Section 14.1). OpenStax. https://openstax.org/books/anatomy-and-physiology/pages/14-1-sensory-perception
Blausen.com Staff. (2014). Medical gallery of Blausen Medical 2014. WikiJournal of Medicine 1 (2). DOI:10.15347/wjm/2014.010. ISSN 2002-4436.
Mayo Clinic. (2014, August 26). Gastric bypass surgery: One patient’s journey - Mayo Clinic. https://www.youtube.com/watch?v=twJBEypJDfU&feature=youtu.be
Mayo Clinic Staff. (n.d.). Gastroesophageal reflux disease (GERD) [online article]. MayoClinic.org. https://www.mayoclinic.org/diseases-conditions/gerd/symptoms-causes/syc-20361940
Tech Insider. (2018, March 20). Here's what happens in your body when you swallow gum | The human body. YouTube. https://www.youtube.com/watch?v=u_1sVri3b2w&feature=youtu.be
TED-Ed. (2020, April 9). How does alcohol make you drunk? - Judy Grisel. YouTube. https://www.youtube.com/watch?v=gCrmFbgT37I&feature=youtu.be
TED-Ed. (2016, October 17). What causes cavities? - Mel Rosenberg. YouTube. https://www.youtube.com/watch?v=zGoBFU1q4g0&feature=youtu.be

Case Study Conclusion: Please Don’t Pass the Bread
The bread above may or may not look appetizing to you, but for people with celiac disease, it is certainly off limits. Bread and pasta are traditionally made with wheat, which contains proteins called gluten. As you learned in the beginning of the chapter, even trace amounts of gluten can damage the digestive system of people with celiac disease. When Angela and Saloni met for lunch, Angela chose a restaurant that she knew could provide her with gluten-free food because she has this disease.
When people with celiac disease eat gluten, it causes an autoimmune reaction that results in inflammation and flattening of the villi of the small intestine. What do you think happens if the villi are inflamed and flattened? Think about what you have learned about the functions of the villi and small intestine. The small intestine is where most chemical digestion and absorption of nutrients occurs in the body. The villi increase the surface area in the small intestine to maximize the digestion of food and absorption of nutrients into the blood and lymph. If the villi are inflamed and flattened, there is less surface area where digestion and absorption can occur. Therefore, damage from celiac disease can result in an inadequate absorption of nutrients called malabsorption.
Malabsorption explains why there can be so many different types of symptoms of celiac disease, ranging from diarrhea and other forms of digestive distress, to anemia, nutritional deficiencies, skin rashes, osteoporosis and bone pain, depression and anxiety, and rarer — but potentially serious — complications, such as cancer. Our bodies need to digest and absorb adequate amounts of nutrients in order to function properly and stay healthy. Lack of nutrients can affect and damage cells, tissues, and organs throughout the body, sometimes seriously and irreversibly. A person with celiac disease can limit and often heal intestinal damage just by not eating gluten. In fact, eliminating all gluten from the diet is the main treatment for celiac disease. In some people with celiac disease, a gluten-free diet may not be enough, and steroids and other medications may be used to reduce the inflammation in the small intestine.
Celiac disease is an autoimmune disorder in which the body’s immune system attacks its own tissues. It is thought to be caused by the presence of particular genes in combination with exposure to gluten. What are some other autoimmune disorders that you read about in this chapter that affect the digestive system? The two main inflammatory bowel diseases, Crohn’s disease and ulcerative colitis, are both due to the body’s immune system attacking the digestive system, resulting in inflammation. Crohn’s disease can affect any part of the GI tract, most commonly the ileum of the small intestine, while ulcerative colitis mainly affects the colon and rectum. Similar to celiac disease, treatments for these diseases also focus on reducing GI tract damage through lifestyle changes and medications.
Gluten is clearly dangerous for people with celiac disease, but should people who do not have celiac disease or other diagnosed medical problem with gluten also eliminate gluten from their diet? Many medical experts say no, because gluten-free diets are so restrictive, they may cause nutritional deficiencies without providing any proven health benefits. They can also be expensive and, as Saloni’s cousin found out, difficult to maintain, given that gluten is present in so many foods. It is estimated that only one per cent of the population has celiac disease. Most people should enjoy a varied diet and consult with their doctor if they are concerned about celiac disease, other types of gluten intolerance, or food allergies.
Watch this TED-Ed video "What's the big deal with gluten? - William D. Chey" to learn more:
https://youtu.be/uEM2iDT-VAk
What’s the big deal with gluten? - William D. Chey, TED-Ed, 2015.
Chapter 15 Summary
In this chapter, you learned about the digestive system, which allows the body to obtain needed nutrients from food. Specifically, you learned that:
- The digestive system consists of organs that break down food, absorb its nutrients, and expel any remaining food waste.
- Most digestive organs form a long, continuous tube through which food passes, called the gastrointestinal (GI) tract. It starts at the mouth, which is followed by the pharynx, esophagus, stomach, small intestine, and large intestine.
- Organs of the GI tract have walls that consist of several tissue layers that enable them to carry out digestion and/or absorption. For example, the inner mucosa has cells that secrete digestive enzymes and other digestive substances and also cells that absorb nutrients. The muscle layer of the organs enables them to contract and relax in waves of peristalsis to move food through the GI tract.
- Digestion is a form of catabolism, in which food is broken down into small molecules that the body can absorb and use for energy, growth, and repair. Digestion occurs when food moves through the GI tract. The digestive process is controlled by both hormones and nerves.
-
- Mechanical digestion is a physical process in which food is broken into smaller pieces without becoming chemically changed. It occurs mainly in the mouth and stomach.
- Chemical digestion is a chemical process in which macromolecules — including carbohydrates, proteins, lipids, and nucleic acids — in food are changed into simple nutrient molecules that can be absorbed into body fluids. Carbohydrates are chemically digested to sugars, proteins to amino acids, lipids to fatty acids, and nucleic acids to individual nucleotides. Chemical digestion requires digestive enzymes. Gut flora carry out additional chemical digestion.
- Absorption occurs when the simple nutrient molecules that result from digestion are absorbed into blood or lymph. They are then circulated through the body.
- Organs of the upper gastrointestinal (GI) tract include the mouth, pharynx, esophagus, and stomach.
-
- The mouth is the first organ of the GI tract. It has several structures that are specialized for digestion, including salivary glands, tongue, and teeth. Both mechanical digestion and chemical digestion of carbohydrates and fats begin in the mouth.
- The pharynx and esophagus move food from the mouth to the stomach but are not directly involved in the process of digestion or absorption. Food moves through the esophagus by peristalsis.
- Mechanical and chemical digestion continue in the stomach. Acid and digestive enzymes secreted by the stomach start the chemical digestion of proteins. The stomach turns masticated food into a semi-fluid mixture called chyme.
- The lower GI tract includes the small intestine and large intestine. The small intestine is where most chemical digestion and virtually all absorption of nutrients occur. The large intestine contains huge numbers of beneficial bacteria, and removes water and salts from food waste before it is eliminated.
-
- The small intestine consists of three parts: the duodenum, jejunum, and ileum. All three parts of the small intestine are lined with mucosa that is very wrinkled and covered with villi and microvilli, giving the small intestine a huge surface area for digestion and absorption.
-
-
- The duodenum secretes digestive enzymes and also receives bile from the liver or gallbladder and digestive enzymes and bicarbonate from the pancreas. These digestive substances neutralize acidic chyme and allow for the chemical digestion of carbohydrates, proteins, lipids, and nucleic acids in the duodenum.
- The jejunum carries out most of the absorption of nutrients in the small intestine, including the absorption of simple sugars, amino acids, fatty acids, and many vitamins.
- The ileum carries out any remaining digestion and absorption of nutrients, but its main function is to absorb vitamin B12 and bile salts.
- The large intestine consists of the colon (which in turn includes the cecum, ascending colon, transverse colon, descending colon, and sigmoid colon), rectum, and anus. The appendix is attached to the cecum of the colon.
-
-
-
- The main function of the large intestine is to remove water and salts from chyme for recycling within the body and eliminating the remaining solid feces from the body through the anus. The large intestine is also the site where trillions of bacteria help digest certain compounds, produce vitamins, stimulate the immune system, and break down toxins, among other important functions.
-
- Accessory organs of digestion are organs that secrete substances needed for the chemical digestion of food, but through which food does not actually pass as it is digested. The accessory organs include the liver, gallbladder, and pancreas. These organs secrete or store substances that are carried to the duodenum of the small intestine as needed for digestion.
-
- The liver is a large organ in the abdomen that is divided into lobes and smaller lobules, which consist of metabolic cells called hepatic cells, or hepatocytes. The liver receives oxygen in blood from the aorta through the hepatic artery. It receives nutrients in blood from the GI tract and wastes in blood from the spleen through the portal vein.
-
-
- The main digestive function of the liver is the production of the alkaline liquid called bile. Bile is carried directly to the duodenum by the common bile duct or to the gallbladder first for storage. Bile neutralizes acidic chyme that enters the duodenum from the stomach and also emulsifies fat globules into smaller particles (micelles) that are easier to digest chemically.
- Other vital functions of the liver include regulating blood sugar levels by storing excess sugar as glycogen; storing many vitamins and minerals; synthesizing numerous proteins and lipids; and breaking down waste products and toxic substances.
- The gallbladder is a small pouch-like organ near the liver. It stores and concentrates bile from the liver until it is needed in the duodenum to neutralize chyme and help digest lipids.
- The pancreas is a glandular organ that secretes both endocrine hormones and digestive enzymes. As an endocrine gland, the pancreas secretes insulin and glucagon to regulate blood sugar. As a digestive organ, the pancreas secretes digestive enzymes into the duodenum through ducts. Pancreatic digestive enzymes include amylase (starches); trypsin and chymotrypsin (proteins); lipase (lipids); and ribonucleases and deoxyribonucleases (RNA and DNA).
-
- Inflammatory bowel disease is a collection of inflammatory conditions primarily affecting the intestines. The diseases involve the immune system attacking the GI tract, and they have multiple genetic and environmental causes. Typical symptoms include abdominal pain and diarrhea, which show a pattern of repeated flare-ups interrupted by periods of remission. Lifestyle changes and medications may control flare-ups and extend remission. Surgery is sometimes required.
-
- The two principal inflammatory bowel diseases are Crohn’s disease and ulcerative colitis. Crohn’s disease may affect any part of the GI tract from the mouth to the anus, among other body tissues. Ulcerative colitis affects the colon and/or rectum.
- Some people have little pouches, called diverticula, in the lining of their large intestine, a condition called diverticulosis. People with diverticulosis may develop diverticulitis, in which one or more of the diverticula become infected and inflamed. Diverticulitis is generally treated with antibiotics and bowel rest. Sometimes, surgery is required.
- A peptic ulcer is a sore in the lining of the stomach (gastric ulcer) or duodenum (duodenal ulcer). The most common cause is infection with the bacterium Helicobacter pylori. NSAIDs such as aspirin can also cause peptic ulcers, and some lifestyle factors may play contributing roles. Antibiotics and acid reducers are typically prescribed. Surgery is not often needed.
- Gastroenteritis, or infectious diarrhea, is an acute and usually self-limiting infection of the GI tract by pathogens, most often viruses. Symptoms typically include diarrhea, vomiting, and/or abdominal pain. Treatment includes replacing lost fluids. Antibiotics are not usually effective.
- Giardiasis is a type of gastroenteritis caused by infection of the GI tract with the protozoa parasite Giardia lamblia. It may cause malnutrition. Generally self-limiting, severe or long-lasting cases may require antibiotics.
As you have learned, the process of digestion, in which food is broken down and nutrients are absorbed by the body, also involves the elimination of solid wastes. Elimination of waste is also called excretion. Some of the organs of the digestive system, such as the liver and large intestine, are also considered part of the excretory system. Read the next chapter to learn more about the excretory system and how wastes are eliminated from our bodies.
Chapter 15 Review
-
- Explain how the accessory organs of digestion interact with the GI tract.
- If the pH in the duodenum was too low (acidic), what effect do you think this would have on the processes of the digestive system?
- Discuss whether digestion occurs in the large intestine.
- Lipids are digested at different points in the digestive system. Describe how lipids are digested at two of these points.
- Describe two different functions of stomach acid.
- Name and describe the location and function of three of the valves of the GI tract.
- What is the name of the rhythmic muscle contractions that move food through the GI tract?
- What are the major roles of the upper GI tract?
- What is the physiological cause of heartburn?
- What are two ways in which the tongue participates in digestion?
- Where is the epiglottis located? If the epiglottis were to not close properly, what might happen?
Attribution
Figure 15.8.1
Sliced Bread/ Bread Basket by Daria Nepriakhina on Unsplash is used under the Unsplash License (https://unsplash.com/license).
Reference
TED-Ed. (2015, June 2). What’s the big deal with gluten? - William D. Chey. YouTube. https://www.youtube.com/watch?v=uEM2iDT-VAk&feature=youtu.be
Image shows a diagram of the cross sectional layering of heart tissues. As described in the preceding paragraph, the endocardium is a thin layer on the inside of the heart chambers, and myocardium is an extremely thick layer of cardiac muscle, and the pericardium consists of two membranes separated by fluid. The visceral pericardium envelopes the myocardium and the parietal pericardium envelopes the entire heart structure.
An evolutionary theory of the origin of eukaryotic cells from prokaryotic organisms.
A type of immune cell that has granules (small particles) with enzymes that are released during allergic reactions and asthma. A basophil is a type of white blood cell and a type of granulocyte.
A biological process which converts sugars such as glucose, fructose, and sucrose into cellular energy, producing ethanol and carbon dioxide as by-products.
Image shows a man at an oxygen bar. There are several erlenmeyer flasks of differently scented oxygen with tubes coming out of the top of each. The man is wearing a nasal cannula (tube that blows air into your nostrils).
Image is a GIF of an xray of someone swallowing. You can see the bones of the head and neck from a side view. The liquid is swallowed and flows in through the mouth, down the pharynx and down the esophagus.
A hormone is a signaling molecule produced by glands in multicellular organisms that target distant organs to regulate physiology and behavior.
A genetically-based trait that has evolved because it helps living things survive and reproduce in a given environment.
Image shows a diagram of how alzheimer's progresses. In preclinical AD, just a small portion of the brain is affected. More of the brain and more areas of the brain are affected in mild to moderate AD. In severe AD, most of the brain is affected.
Created by CK-12/Adapted by Christine Miller
As you read in the beginning of this chapter, new parents Samantha and Aki left their pediatrician’s office still unsure whether or not to vaccinate baby James. Dr. Rodriguez gave them a list of reputable sources where they could look up information about the safety of vaccines, including the Centers for Disease Control and Prevention (CDC). Samantha and Aki read that the consensus within the scientific community is that there is no link between vaccines and autism. They find a long list of studies published in peer-reviewed scientific journals that disprove any link. Additionally, some of the studies are “meta-analyses” that analyzed the findings from many individual studies. The new parents are reassured by the fact that many different researchers, using a large number of subjects in numerous well-controlled and well-reviewed studies, all came to the same conclusion.

Samantha also went back to the web page that originally scared her about the safety of vaccines. She found that the author was not a medical doctor or scientific researcher, but rather a self-proclaimed “child wellness expert.” He sold books and advertising on his site, some of which were related to claims of vaccine injury. She realized that he was both an unqualified and potentially biased source of information.
Samantha also realized that some of his arguments were based on correlations between autism and vaccines, but, as the saying goes, “correlation does not imply causation.” For instance, the recent rise in autism rates may have occurred during the same time period as an increase in the number of vaccines given in childhood, but Samantha could think of many other environmental and social factors that have also changed during this time period. There are just too many variables to come to the conclusion that vaccines, or anything else, are the cause of the rise in autism rates based on that type of argument alone. Also, she learned that the age of onset of autism symptoms happens to typically be around the time that the MMR vaccine is first given, so the apparent association in the timing may just be a coincidence.
Finally, Samantha came across news about a measles outbreak in Vancouver, British Columbia in the winter of 2019. Measles wasn’t just a disease of the past! She learned that measles and whooping cough, which had previously been rare thanks to widespread vaccinations, are now on the rise, and that people choosing not to vaccinate their children seems to be one of the contributing factors. She realized that it is important to vaccinate her baby against these diseases, not only to protect him from their potentially deadly effects, but also to protect others in the population.
In their reading, Samantha and Aki learn that scientists do not yet know the causes of autism, but they feels reassured by the abundance of data that disproves any link with vaccines. Both parents think that the potential benefits of protecting their baby’s health against deadly diseases outweighs any unsubstantiated claims about vaccines. They will be making an appointment to get baby James his shots soon.
Chapter 1 Summary
In this chapter, you learned about some of the same concepts that helped Samantha and Aki make an informed decision. Specifically:
- Science is a distinctive way of gaining knowledge about the natural world that is based on the use of evidence to logically test ideas. As such, science is a process, as well as a body of knowledge.
- A scientific theory, such as the germ theory of disease, is the highest level of explanation in science. A theory is a broad explanation for many phenomena that is widely accepted because it is supported by a great deal of evidence.
- The scientific investigation is the cornerstone of science as a process. A scientific investigation is a systematic approach to answering questions about the physical and natural world. An investigation may be observational or experimental.
- A scientific experiment is a type of scientific investigation in which the researcher manipulates variables under controlled conditions to test expected outcomes. Experiments are the gold standard for scientific investigations and can establish causation between variables.
- Nonexperimental scientific investigations such as observational studies and modeling may be undertaken when experiments are impractical, unethical, or impossible. Observational studies generally can establish correlation — but not causation — between variables.
- A pseudoscience, such as astrology, is a field that is presented as scientific but that does not adhere to scientific standards and methods. Other misuses of science include deliberate hoaxes, frauds, and fallacies made by researchers.
- Strict guidelines must be followed when using human subjects in scientific research. Among the most important protections is the requirement for informed consent.
Now that you know about the nature and process of science, you can apply these concepts in the next chapter to the study of human biology.
Chapter 1 Review
-
- Why does a good hypothesis have to be falsifiable?
- Name one scientific law.
- Name one scientific theory.
- Give an example of a scientific idea that was later discredited.
- A statistical measurement called a P-value is often used in science to determine whether or not a difference between two groups is actually significant or simply due to chance. A P-value of 0.03 means that there is a 3% chance that the difference is due to chance alone. Do you think a P-value of 0.03 would indicate that the difference is likely to be significant? Why or why not?
- Why is it important that scientists communicate their findings to others? How do they usually do this?
- What is a “control group” in science?
- In a scientific experiment, why is it important to only change one variable at a time?
- Which is the dependent variable – the variable that is manipulated or the variable that is being affected by the change?
- You see an ad for a “miracle supplement” called NQP3 that claims the supplement will reduce belly fat. They say it works by reducing the hormone cortisol and by providing your body with missing unspecified “nutrients”, but they do not cite any peer-reviewed clinical studies. They show photographs of three people who appear slimmer after taking the product. A board-certified plastic surgeon endorses the product on television. Answer the following questions about this product.
a. Do you think that because a doctor endorsed the product, it really works? Explain your answer.
b. What are two signs that these claims could actually be pseudoscience instead of true science?
c. Do you think the photographs are good evidence that the product works? Why or why not?
d. If you wanted to do a strong scientific study of whether this supplement does what it claims, what would you do? Be specific about the subjects, data collected, how you would control variables, and how you would analyze the data.
e. What are some ways that you would ensure that the subjects in your experiment in part d are treated ethically and according to human subjects protections regulations?
Attribution
Figure 1.8.1
[Photo of person sitting in front of personal computer] by Avel Chuklanov on Unsplash is used under the Unsplash License (https://unsplash.com/license).
As per caption
Image shows a photograph of an Amish man. His hairstyle and beard with no mustache is evidence that he is married.
Image shows a flowchart of the path of blood through the heart. Beginning at the lungs, oxygenated blood enters the pulmonary veins, then enters the left atrium. Blood then passes through the bicuspid AV valve to enter the left ventricle, which contracts to send blood through the aortic semilunar valve into the aorta. The aorta connects to arteries of the systemic circuit and ultimately deliver oxygen to body tissues. From here, blood is deoxygenated and returns to the heart via veins which merge to form the two vena cava. The vena cava delivers blood to the right atrium, which contracts to send blood through the tricuspid AV valve into the right ventricle, which contracts to send blood through the pulmonary semilunar valve into the pulmonary arteries and to the lungs for re-oxygenation.
image shows the signs for mens and women's washroom.
As per caption.
Image shows a diagram of the heart with all chambers and major vessels labelled. Arrows indicate blood flow. Deoxygenated blood is brought the the right atrium by the superior and inferior vena cava. The right atrium moves blood into the right ventricle, which then sends blood to the lungs via the pulmonary arteries. Oxygenated blood returns to the heart from the lungs via the pulmonary veins and enters the left atrium. From there, blood is pumped into the left ventricle and then into the aorta for distribution to the body.

Case Study: Drink and Flush
“Wow, this line for the restroom is long!” Shae says to Talia, anxiously bobbing from side to side to ease the pressure in her bladder. Talia nods and says, “It’s always like this at parties. It’s the alcohol.”
Shae and Talia are 21-year-old college students at a party. They — along with the other party guests — have been drinking alcoholic beverages over the course of the evening. As the night goes on, the line for the restroom has gotten longer and longer. You may have noticed this phenomenon if you have been to places where large numbers of people are drinking alcohol, like at the ballpark in Figure 16.1.2.

Shae says, “I wonder why alcohol makes you have to pee?” Talia says she learned about this in her Human Biology class. She tells Shae that alcohol inhibits a hormone that helps you retain water. Instead of your body retaining water, you urinate more out. This could lead to dehydration, so she suggests that after their trip to the restroom, they start drinking water, instead of alcohol.
For people who drink occasionally or moderately, this effect of alcohol on the excretory system — the system that removes wastes such as urine — is usually temporary. However, in people who drink excessively, alcohol can have serious, long-term effects on the excretory system. Heavy drinking on a regular basis can cause liver and kidney disease.
As you will learn in this chapter, the liver and kidneys are important organs of the excretory system, and impairment of the functioning of these organs can cause serious health consequences. At the end of the chapter, you will learn which hormone Talia was referring to. You will also learn some of the ways alcohol can affect the excretory system — both after the occasional drink, and in cases of excessive alcohol use and abuse.
Chapter Overview: Excretory System
In this chapter, you will learn about the excretory system, which rids the body of toxic waste products and helps maintain homeostasis. Specifically, you will learn about:
- The organs of the excretory system —including the skin, liver, large intestine, lungs, and kidneys — that eliminate waste and excess water from the body.
- How wastes are eliminated through sweat, feces, urine, and exhaled gases.
- How toxic substances in the blood are broken down by the liver.
- The urinary system, which includes the kidneys, ureters, bladder, and urethra.
- The main function of the urinary system, which is to filter the blood and eliminate wastes, mineral ions, and excess water from the body in the form of urine.
- How the kidneys filter the blood, retain necessary substances, produce urine, and help maintain homeostasis (such as proper ion and water balance).
- How urine is stored, transported, and released from the body.
- Disorders of the urinary system, including bladder infections, kidney stones, polycystic kidney disease, urinary incontinence, and kidney damage caused by factors such as uncontrolled diabetes and high blood pressure.
As you read the chapter, think about the following questions:
- Which hormone do you think Talia was referring to? Remember that this hormone causes the urinary system to retain water and excrete less water out in urine.
- How and where does this hormone work?
- Long-term, excessive use of alcohol can affect the liver and kidneys. How do these two organs of excretion interact and work together?
Attributions
Figure 16.1.1
Gotta Pee [photo] by Jon-Eric Melsæter on Flickr is used under a CC BY 2.0 (https://creativecommons.org/licenses/by/2.0/) license.
Figure 16.1.2
Bathroom line up [photo] by Dorothy on Flickr is used under a CC BY 2.0 (https://creativecommons.org/licenses/by/2.0/) license.
Created by: CK-12/Adapted by Christine Miller
Giving the Gift of Life
Did you ever donate blood? If you did, then you probably know that your blood type is an important factor in blood transfusions. People vary in the type of blood they inherit, and this determines which type(s) of blood they can safely receive in a transfusion. Do you know your blood type?
What Are Blood Types?
Blood is composed of cells suspended in a liquid called plasma. There are three types of cells in blood: red blood cells, which carry oxygen; white blood cells, which fight infections and other threats; and platelets, which are cell fragments that help blood clot. Blood type (or blood group) is a genetic characteristic associated with the presence or absence of certain molecules, called antigens, on the surface of red blood cells. These molecules may help maintain the integrity of the cell membrane, act as receptors, or have other biological functions. A blood group system refers to all of the gene(s), alleles, and possible genotypes and phenotypes that exist for a particular set of blood type antigens. Human blood group systems include the well-known ABO and Rhesus (Rh) systems, as well as at least 33 others that are less well known.
Antigens and Antibodies
Antigens — such as those on the red blood cells — are molecules that the immune system identifies as either self (produced by your own body) or non-self (not produced by your own body). Blood group antigens may be proteins, carbohydrates, glycoproteins (proteins attached to chains of sugars), or glycolipids (lipids attached to chains of sugars), depending on the particular blood group system. If antigens are identified as non-self, the immune system responds by forming antibodies that are specific to the non-self antigens. Antibodies are large, Y-shaped proteins produced by the immune system that recognize and bind to non-self antigens. The analogy of a lock and key is often used to represent how an antibody and antigen fit together, as shown in the illustration below (Figure 6.5.2). When antibodies bind to antigens, it marks them for destruction by other immune system cells. Non-self antigens may enter your body on pathogens (such as bacteria or viruses), on foods, or on red blood cells in a blood transfusion from someone with a different blood type than your own. The last way is virtually impossible nowadays because of effective blood typing and screening protocols.
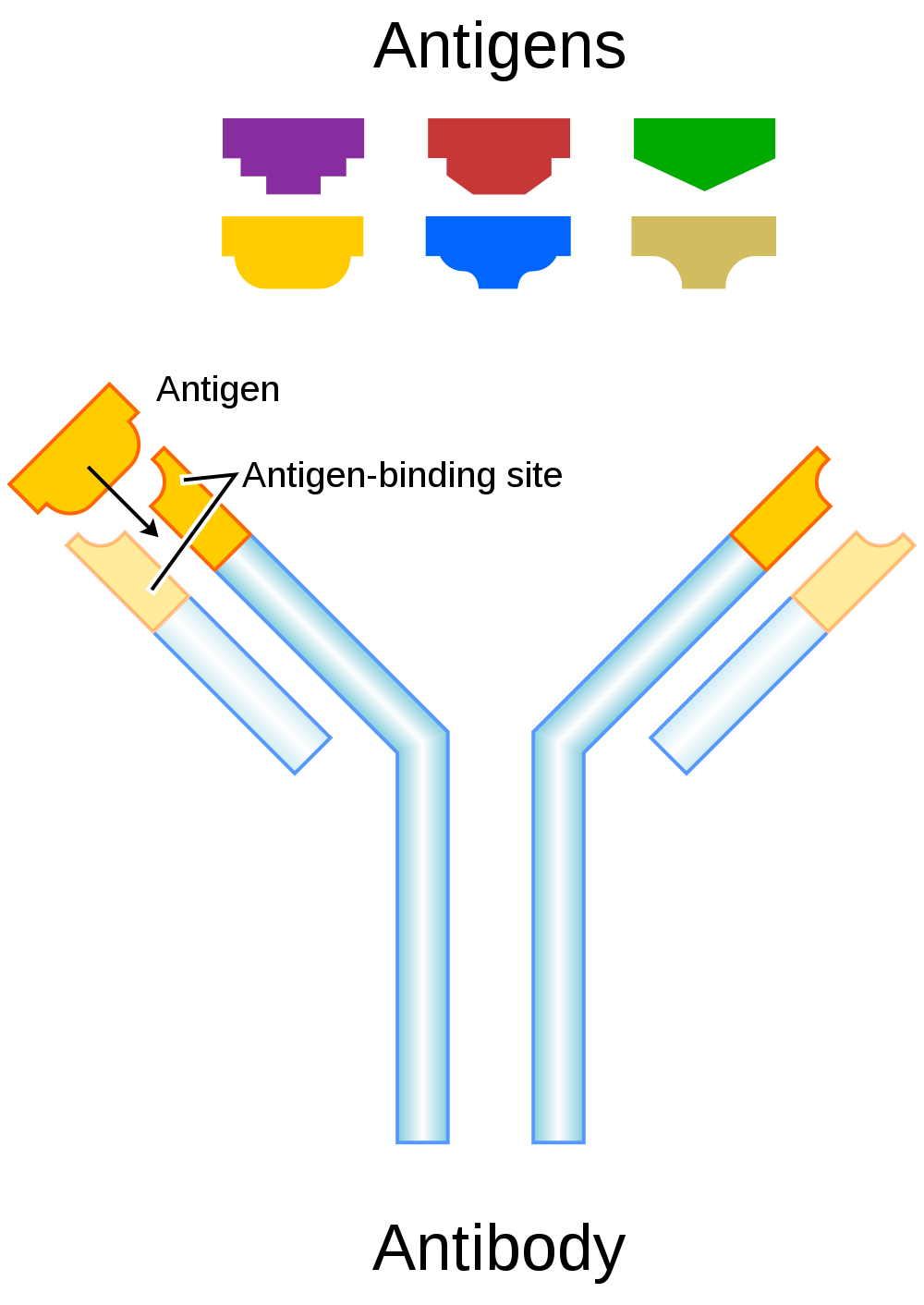
Genetics of Blood Type
An individual’s blood type depends on which alleles for a blood group system were inherited from their parents. Generally, blood type is controlled by alleles for a single gene, or for two or more very closely linked genes. Closely linked genes are almost always inherited together, because there is little or no recombination between them. Like other genetic traits, a person’s blood type is generally fixed for life, but there are rare instances in which blood type can change. This could happen, for example, if an individual receives a bone marrow transplant to treat a disease, such as leukemia. If the bone marrow comes from a donor who has a different blood type, the patient’s blood type may eventually convert to the donor’s blood type, because red blood cells are produced in bone marrow.
ABO Blood Group System
The ABO blood group system is the best known human blood group system. Antigens in this system are glycoproteins. These antigens are shown in the list below. There are four common blood types for the ABO system:
- Type A, in which only the A antigen is present.
- Type B, in which only the B antigen is present.
- Type AB, in which both the A and B antigens are present.
- Type O, in which neither the A nor the B antigen is present.
Genetics of the ABO System
The ABO blood group system is controlled by a single gene on chromosome 9. There are three common alleles for the gene, often represented by the letters A , B , and O. With three alleles, there are six possible genotypes for ABO blood group. Alleles A and B, however, are both dominant to allele O and codominant to each other. This results in just four possible phenotypes (blood types) for the ABO system. These genotypes and phenotypes are shown in Table 6.5.1.
Table 6.5.1
ABO Blood Group System: Genotypes and Phenotypes
| ABO Blood Group System | |
| Genotype | Phenotype (Blood Type, or Group) |
| AA | A |
| AO | A |
| BB | B |
| BO | B |
| OO | O |
| AB | AB |
The diagram below (Figure 6.5.3) shows an example of how ABO blood type is inherited. In this particular example, the father has blood type A (genotype AO) and the mother has blood type B (genotype BO). This mating type can produce children with each of the four possible ABO phenotypes, although in any given family, not all phenotypes may be present in the children.
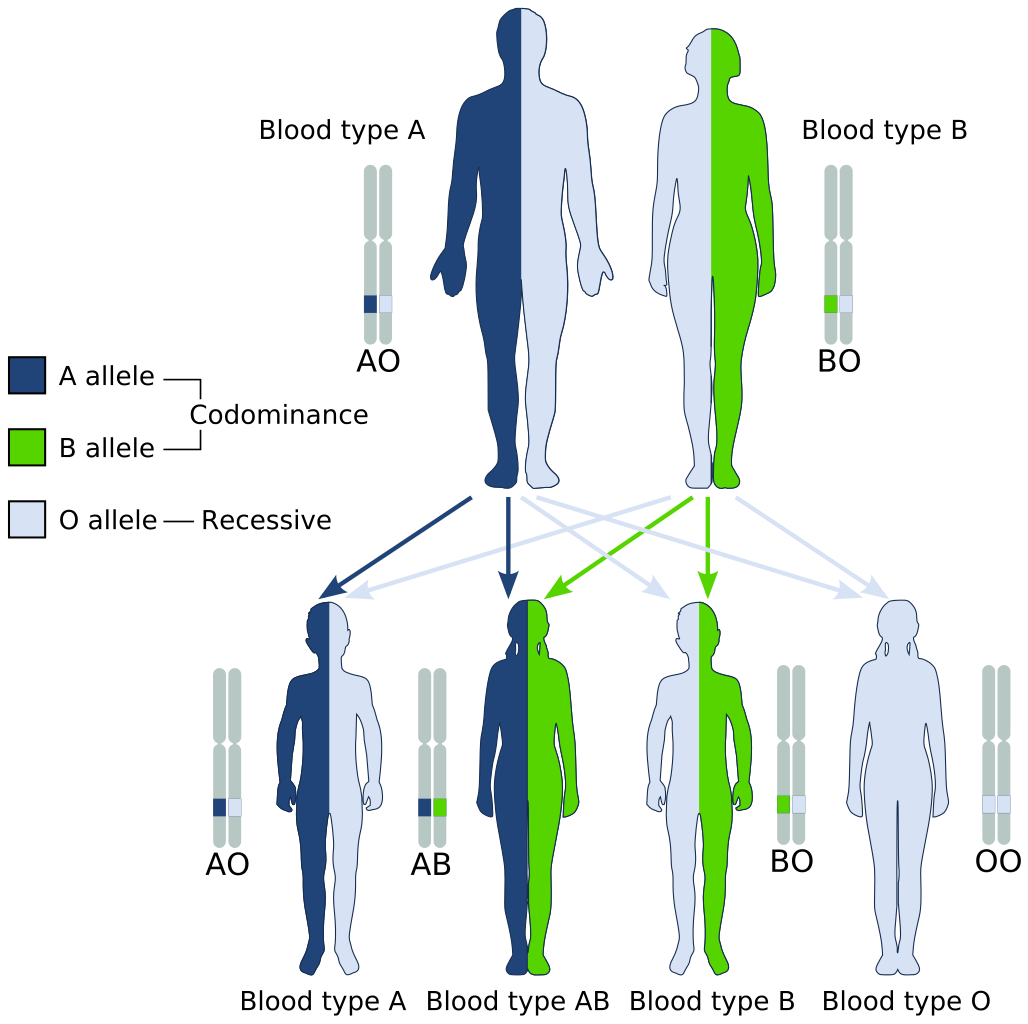
Medical Significance of ABO Blood Type
The ABO system is the most important blood group system in blood transfusions. If red blood cells containing a particular ABO antigen are transfused into a person who lacks that antigen, the person’s immune system will recognize the antigen on the red blood cells as non-self. Antibodies specific to that antigen will attack the red blood cells, causing them to agglutinate (or clump) and break apart. If a unit of incompatible blood were to be accidentally transfused into a patient, a severe reaction (called acute hemolytic transfusion reaction) is likely to occur, in which many red blood cells are destroyed. This may result in kidney failure, shock, and even death. Fortunately, such medical accidents virtually never occur today.
These antibodies are often spontaneously produced in the first years of life, after exposure to common microorganisms in the environment that have antigens similar to blood antigens. Specifically, a person with type A blood will produce anti-B antibodies, while a person with type B blood will produce anti-A antibodies. A person with type AB blood does not produce either antibody, while a person with type O blood produces both anti-A and anti-B antibodies. Once the antibodies have been produced, they circulate in the plasma. The relationship between ABO red blood cell antigens and plasma antibodies is shown in Figure 6.5.4.
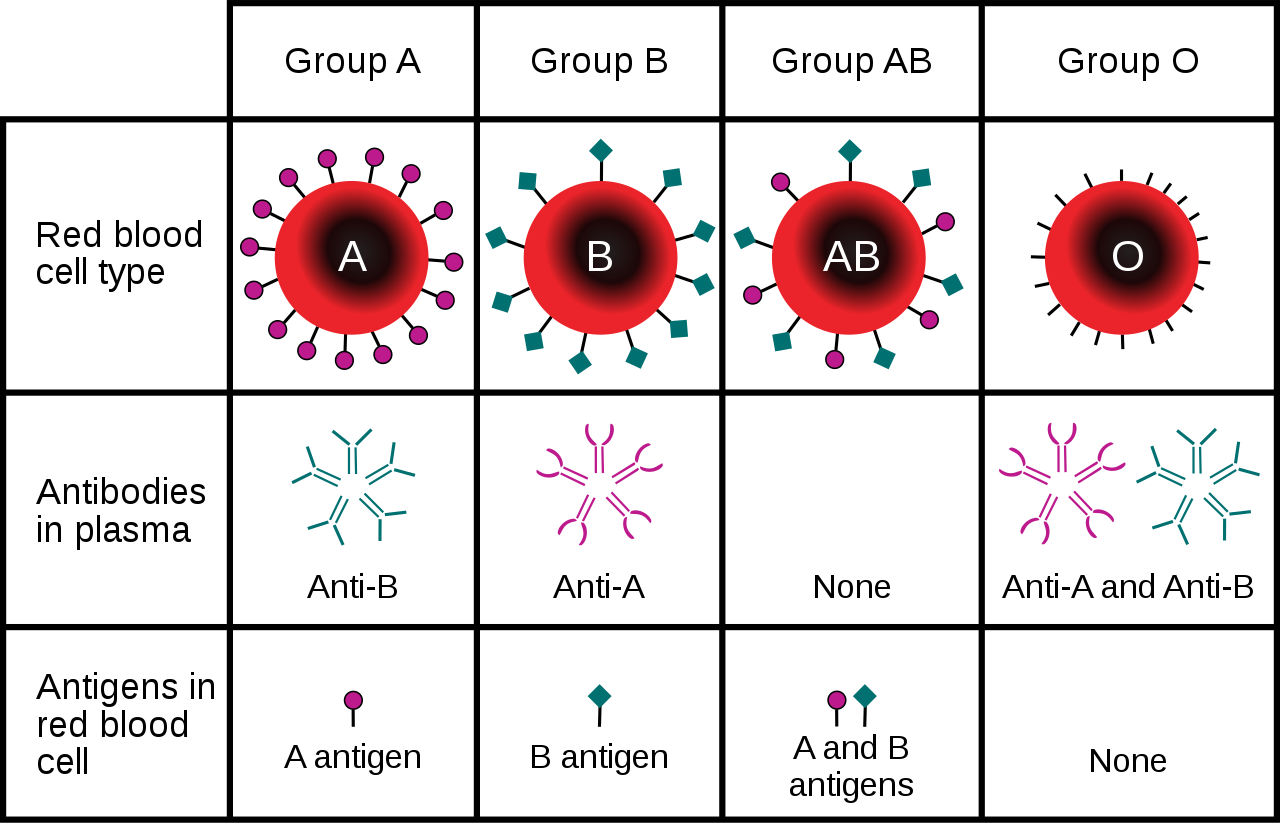
The antibodies that circulate in the plasma are for different antigens than those on red blood cells, which are recognized as self antigens.
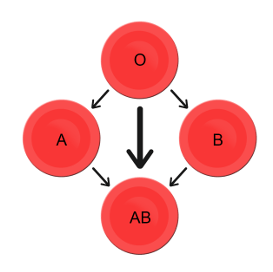
Which blood types are compatible and which are not? Type O blood contains both anti-A and anti-B antibodies, so people with type O blood can only receive type O blood. However, they can donate blood to people of any ABO blood type, which is why individuals with type O blood are called universal donors. Type AB blood contains neither anti-A nor anti-B antibodies, so people with type AB blood can receive blood from people of any ABO blood type. That’s why individuals with type AB blood are called universal recipients. They can donate blood, however, only to people who also have type AB blood. These and other relationships between blood types of donors and recipients are summarized in the simple diagram to the right.
Geographic Distribution of ABO Blood Groups
The frequencies of blood groups for the ABO system vary around the world. You can see how the A and B alleles and the blood group O are distributed geographically on the maps in Figure 6.5.6.
- Worldwide, B is the rarest ABO allele, so type B blood is the least common ABO blood type. Only about 16 per cent of all people have the B allele. Its highest frequency is in Asia. Its lowest frequency is among the indigenous people of Australia and the Americas.
- The A allele is somewhat more common around the world than the B allele, so type A blood is also more common than type B blood. The highest frequencies of the A allele are in Australian Aborigines, the Lapps (Sami) of Northern Scandinavia, and Blackfoot Native Americans in North America. The allele is nearly absent among Native Americans in Central and South America.
- The O allele is the most common ABO allele around the world, and type O blood is the most common ABO blood type. Almost two-thirds of people have at least one copy of the O allele. It is especially common in Native Americans in Central and South America, where it reaches frequencies close to 100 per cent. It also has relatively high frequencies in Australian Aborigines and Western Europeans. Its frequencies are lowest in Eastern Europe and Central Asia.
Figure 6.5.6 Maps of populations that have the A, B and O alleles.
Evolution of the ABO Blood Group System
The geographic distribution of ABO blood type alleles provides indirect evidence for the evolutionary history of these alleles. Evolutionary biologists hypothesize that the allele for blood type A evolved first, followed by the allele for blood type O, and then by the allele for blood type B. This chronology accounts for the percentages of people worldwide with each blood group, and is also consistent with known patterns of early population movements.
The evolutionary forces of founder effect and genetic drift have no doubt played a significant role in the current distribution of ABO blood types worldwide. Geographic variation in ABO blood groups is also likely to be influenced by natural selection, because different blood types are thought to vary in their susceptibility to certain diseases. For example:
- People with type O blood may be more susceptible to cholera and plague. They are also more likely to develop gastrointestinal ulcers.
- People with type A blood may be more susceptible to smallpox and more likely to develop certain cancers.
- People with types A, B, and AB blood appear to be less likely to form blood clots that can cause strokes. However, early in our history, the ability of blood to form clots — which appears greater in people with type O blood — may have been a survival advantage.
- Perhaps the greatest natural selective force associated with ABO blood types is malaria. There is considerable evidence to suggest that people with type O blood are somewhat resistant to malaria, giving them a selective advantage where malaria is endemic.
Rhesus Blood Group System
Another well-known blood group system is the Rhesus (Rh) blood group system. The Rhesus system has dozens of different antigens, but only five main antigens (called D, C, c, E, and e). The major Rhesus antigen is the D antigen. People with the D antigen are called Rh positive (Rh+), and people who lack the D antigen are called Rh negative (Rh-). Rhesus antigens are thought to play a role in transporting ions across cell membranes by acting as channel proteins.
The Rhesus blood group system is controlled by two linked genes on chromosome 1. One gene, called RHD, produces a single antigen, antigen D. The other gene, called RHCE, produces the other four relatively common Rhesus antigens (C, c, E, and e), depending on which alleles for this gene are inherited.
Rhesus Blood Group and Transfusions
After the ABO system, the Rhesus system is the second most important blood group system in blood transfusions. The D antigen is the one most likely to provoke an immune response in people who lack the antigen. People who have the D antigen (Rh+) can be safely transfused with either Rh+ or Rh- blood, whereas people who lack the D antigen (Rh-) can be safely transfused only with Rh- blood.
Unlike anti-A and anti-B antibodies to ABO antigens, anti-D antibodies for the Rhesus system are not usually produced by sensitization to environmental substances. People who lack the D antigen (Rh-), however, may produce anti-D antibodies if exposed to Rh+ blood. This may happen accidentally in a blood transfusion, although this is extremely unlikely today. It may also happen during pregnancy with an Rh+ fetus if some of the fetal blood cells pass into the mother’s blood circulation.
Hemolytic Disease of the Newborn
If a woman who is Rh- is carrying an Rh+ fetus, the fetus may be at risk. This is especially likely if the mother has formed anti-D antibodies during a prior pregnancy because of a mixing of maternal and fetal blood during childbirth. Unlike antibodies against ABO antigens, antibodies against the Rhesus D antigen can cross the placenta and enter the blood of the fetus. This may cause hemolytic disease of the newborn (HDN), also called erythroblastosis fetalis, an illness in which fetal red blood cells are destroyed by maternal antibodies, causing anemia. This illness may range from mild to severe. If it is severe, it may cause brain damage and is sometimes fatal for the fetus or newborn. Fortunately, HDN can be prevented by preventing the formation of anti-D antibodies in the Rh- mother. This is achieved by injecting the mother with a medication called Rho(D) immune globulin.
Geographic Distribution of Rhesus Blood Types
The majority of people worldwide are Rh+, but there is regional variation in this blood group system, as there is with the ABO system. The aboriginal inhabitants of the Americas and Australia originally had very close to 100 per cent Rh+ blood. The frequency of the Rh+ blood type is also very high in African populations, at about 97 to 99 per cent. In East Asia, the frequency of Rh+ is slightly lower, at about 93 to 99 per cent. Europeans have the lowest frequency of the Rh+ blood type at about 83 to 85 per cent.
What explains the population variation in Rhesus blood types? Prior to the advent of modern medicine, Rh+ positive children conceived by Rh- women were at risk of fetal or newborn death or impairment from HDN. This was an enigma, because presumably, natural selection would work to remove the rarer phenotype (Rh-) from populations. However, the frequency of this phenotype is relatively high in many populations.
Recent studies have found evidence that natural selection may actually favor heterozygotes for the Rhesus D antigen. The selective agent in this case is thought to be toxoplasmosis, a parasitic disease caused by the protozoan Toxoplasma gondii, which is very common worldwide. You can see a life cycle diagram of the parasite in Figure 6.5.7. Infection by this parasite often causes no symptoms at all, or it may cause flu-like symptoms for a few days or weeks. Exposure to the parasite has been linked, however, to increased risk of mental disorders (such as schizophrenia), neurological disorders (such as Alzheimer’s), and other neurological problems, including delayed reaction times. One study found that people who tested positive for antibodies to the parasite were more than twice as likely to be involved in traffic accidents.
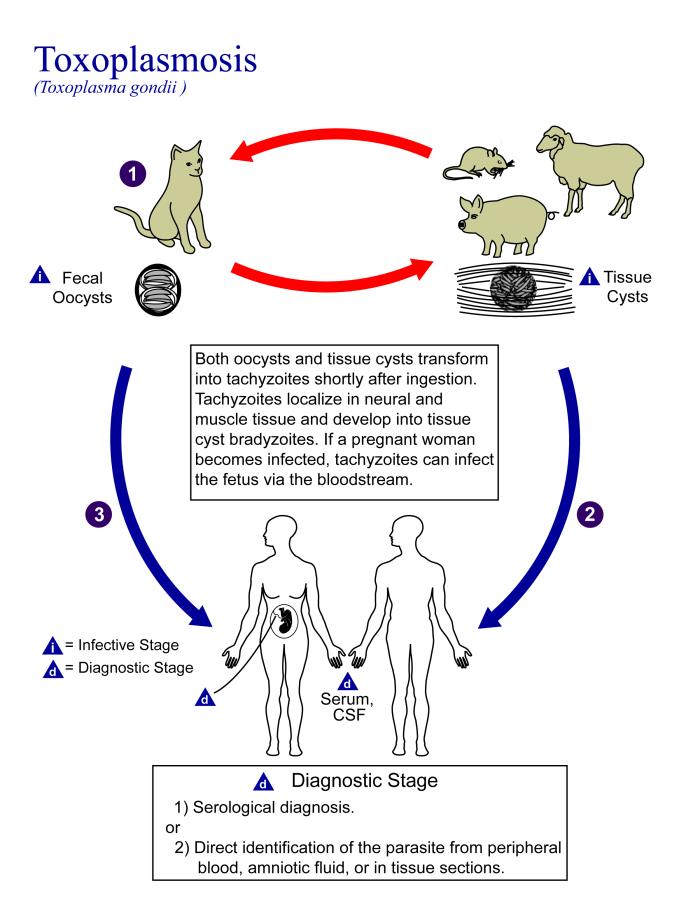
People who are heterozygous for the D antigen appear less likely to develop the negative neurological and mental effects of Toxoplasma gondii infection. This could help explain why both phenotypes (Rh+ and Rh-) are maintained in most populations. There are also striking geographic differences in the prevalence of toxoplasmosis worldwide, ranging from zero to 95 per cent in different regions. This could explain geographic variation in the D antigen worldwide, because its strength as a selective agent would vary with its prevalence.
Feature: Myth vs. Reality
Myth |
Reality |
| "Your nutritional needs can be determined by your ABO blood type. Knowing your blood type allows you to choose the appropriate foods that will help you lose weight, increase your energy, and live a longer, healthier life." | This idea was proposed in 1996 in a New York Times bestseller Eat Right for Your Type, by Peter D’Adamo, a naturopath. Naturopathy is a method of treating disorders that involves the use of herbs, sunlight, fresh air, and other natural substances. Some medical doctors consider naturopathy a pseudoscience. A major scientific review of the blood type diet could find no evidence to support it. In one study, adults eating the diet designed for blood type A showed improved health — but this occurred in everyone, regardless of their blood type. Because the blood type diet is based solely on blood type, it fails to account for other factors that might require dietary adjustments or restrictions. For example, people with diabetes — but different blood types — would follow different diets, and one or both of the diets might conflict with standard diabetes dietary recommendations and be dangerous. |
| "ABO blood type is associated with certain personality traits. People with blood type A, for example, are patient and responsible, but may also be stubborn and tense, whereas people with blood type B are energetic and creative, but may also be irresponsible and unforgiving. In selecting a spouse, both your own and your potential mate’s blood type should be taken into account to ensure compatibility of your personalities." | The belief that blood type is correlated with personality is widely held in Japan and other East Asian countries. The idea was originally introduced in the 1920s in a study commissioned by the Japanese government, but it was later shown to have no scientific support. The idea was revived in the 1970s by a Japanese broadcaster, who wrote popular books about it. There is no scientific basis for the idea, and it is generally dismissed as pseudoscience by the scientific community. Nonetheless, it remains popular in East Asian countries, just as astrology is popular in many other countries. |
6.5 Summary
- Blood type (or blood group) is a genetic characteristic associated with the presence or absence of antigens on the surface of red blood cells. A blood group system refers to all of the gene(s), alleles, and possible genotypes and phenotypes that exist for a particular set of blood type antigens.
- Antigens are molecules that the immune system identifies as either self or non-self. If antigens are identified as non-self, the immune system responds by forming antibodies that are specific to the non-self antigens, leading to the destruction of cells bearing the antigens.
- The ABO blood group system is a system of red blood cell antigens controlled by a single gene with three common alleles on chromosome 9. There are four possible ABO blood types: A, B, AB, and O. The ABO system is the most important blood group system in blood transfusions. People with type O blood are universal donors, and people with type AB blood are universal recipients.
- The frequencies of ABO blood type alleles and blood groups vary around the world. The allele for the B antigen is least common, and blood type O is the most common. The evolutionary forces of founder effect, genetic drift, and natural selection are responsible for the geographic distribution of ABO alleles and blood types. People with type O blood, for example, may be somewhat resistant to malaria, possibly giving them a selective advantage where malaria is endemic.
- The Rhesus blood group system is a system of red blood cell antigens controlled by two genes with many alleles on chromosome 1. There are five common Rhesus antigens, of which antigen D is most significant. Individuals who have antigen D are called Rh+, and individuals who lack antigen D are called Rh-. Rh- mothers of Rh+ fetuses may produce antibodies against the D antigen in the fetal blood, causing hemolytic disease of the newborn (HDN).
- The majority of people worldwide are Rh+, but there is regional variation in this blood group system. This variation may be explained by natural selection that favors heterozygotes for the D antigen, because this genotype seems to be protected against some of the neurological consequences of the common parasitic infection toxoplasmosis.
6.5 Review Questions
- Define blood type and blood group system.
- Explain the relationship between antigens and antibodies.
- Identify the alleles, genotypes, and phenotypes in the ABO blood group system.
- Discuss the medical significance of the ABO blood group system.
- Compare the relative worldwide frequencies of the three ABO alleles.
- Give examples of how different ABO blood types vary in their susceptibility to diseases.
- Describe the Rhesus blood group system.
- Relate Rhesus blood groups to blood transfusions.
- What causes hemolytic disease of the newborn?
- Describe how toxoplasmosis may explain the persistence of the Rh- blood type in human populations.
- A woman is blood type O and Rh-, and her husband is blood type AB and Rh+. Answer the following questions about this couple and their offspring.
- What are the possible genotypes of their offspring in terms of ABO blood group?
- What are the possible phenotypes of their offspring in terms of ABO blood group?
- Can the woman donate blood to her husband? Explain your answer.
- Can the man donate blood to his wife? Explain your answer.
- Type O blood is characterized by the presence of O antigens — explain why this statement is false.
- Explain why newborn hemolytic disease may be more likely to occur in a second pregnancy than in a first.
6.5 Explore More
https://www.youtube.com/watch?v=xfZhb6lmxjk
Why do blood types matter? - Natalie S. Hodge, TED-Ed, 2015.
https://www.youtube.com/watch?v=qcZKbjYyOfE
How do blood transfusions work? - Bill Schutt, TED-Ed, 2020.
Attributes
Figure 6.5.1
Following the Blood Donation Trail by EJ Hersom/ USA Department of Defense is in the public domain. [Disclaimer: The appearance of U.S. Department of Defense (DoD) visual information does not imply or constitute DoD endorsement.]
Figure 6.5.2
Antibody by Fvasconcellos on Wikimedia Commons is released into the public domain (https://en.wikipedia.org/wiki/Public_domain).
Figure 6.5.3
ABO system codominance.svg, adapted by YassineMrabet (original "Codominant" image from US National Library of Medicine) on Wikimedia Commons is in the public domain (https://en.wikipedia.org/wiki/Public_domain).
Figure 6.5.4
ABO_blood_type.svg by InvictaHOG on Wikimedia Commons is released into the public domain (https://en.wikipedia.org/wiki/Public_domain).
Figure 6.5.5
Blood Donor and recipient ABO by CK-12 Foundation is used under a CC BY-NC 3.0 (https://creativecommons.org/licenses/by-nc/3.0/) license.
Figure 6.5.6
- Map of Blood Group A by Muntuwandi at en.wikipedia on Wikimedia Commons is used under a CC BY-SA 3.0 (https://creativecommons.org/licenses/by-sa/3.0/) license.
- Map of Blood Group B by Muntuwandi at en.wikipedia on Wikimedia Commons is used under a CC BY-SA 3.0 (https://creativecommons.org/licenses/by-sa/3.0/) license.
- Map of Blood Group O by anthro palomar at en.wikipedia on Wikimedia Commons is used under a CC BY-SA 3.0 (https://creativecommons.org/licenses/by-sa/3.0/) license.
Figure 6.5.7
Toxoplasma_gondii_Life_cycle_PHIL_3421_lores by Alexander J. da Silva, PhD/Melanie Moser, Centers for Disease Control and Prevention's Public Health Image Library (PHIL#3421) on Wikimedia Commons is in the public domain (https://en.wikipedia.org/wiki/Public_domain).
Table 6.5.1
ABO Blood Group System: Genotypes and Phenotypes was created by Christine Miller.
References
Dean, L. (2005). Chapter 4 Hemolytic disease of the newborn. In Blood Groups and Red Cell Antigens [Internet]. National Center for Biotechnology Information (US). https://www.ncbi.nlm.nih.gov/books/NBK2266/
Mayo Clinic Staff. (n.d.). Toxoplasmosis [online article]. MayoClinic.org. https://www.mayoclinic.org/diseases-conditions/toxoplasmosis/symptoms-causes/syc-20356249
MedlinePlus. (2019, January 29). Hemolytic transfusion reaction [online article]. U.S. National Library of Medicine. https://en.wikipedia.org/w/index.php?title=Chromosome_9&oldid=946440619
TED-Ed. (2015, June 29). Why do blood types matter? - Natalie S. Hodge. YouTube. https://www.youtube.com/watch?v=xfZhb6lmxjk&feature=youtu.be
TED-Ed. (2020, February 18). How do blood transfusions work? - Bill Schutt. YouTube. https://www.youtube.com/watch?v=qcZKbjYyOfE&feature=youtu.be
Wikipedia contributors. (2020, May 10). Chromosome 1. In Wikipedia. https://en.wikipedia.org/w/index.php?title=Chromosome_1&oldid=955942444
Wikipedia contributors. (2020, March 20). Chromosome 9. In Wikipedia. https://en.wikipedia.org/w/index.php?title=Chromosome_9&oldid=946440619
a hormonal disorder common among women of reproductive age. Women with PCOS may have infrequent or prolonged menstrual periods or excess male hormone (androgen) levels. The ovaries may develop numerous small collections of fluid (follicles) and fail to regularly release eggs.
Created by CK-12 Foundation/Adapted by Christine Miller

Case Study: Drink and Flush
“Wow, this line for the restroom is long!” Shae says to Talia, anxiously bobbing from side to side to ease the pressure in her bladder. Talia nods and says, “It’s always like this at parties. It’s the alcohol.”
Shae and Talia are 21-year-old college students at a party. They — along with the other party guests — have been drinking alcoholic beverages over the course of the evening. As the night goes on, the line for the restroom has gotten longer and longer. You may have noticed this phenomenon if you have been to places where large numbers of people are drinking alcohol, like at the ballpark in Figure 16.1.2.

Shae says, “I wonder why alcohol makes you have to pee?” Talia says she learned about this in her Human Biology class. She tells Shae that alcohol inhibits a hormone that helps you retain water. Instead of your body retaining water, you urinate more out. This could lead to dehydration, so she suggests that after their trip to the restroom, they start drinking water, instead of alcohol.
For people who drink occasionally or moderately, this effect of alcohol on the excretory system — the system that removes wastes such as urine — is usually temporary. However, in people who drink excessively, alcohol can have serious, long-term effects on the excretory system. Heavy drinking on a regular basis can cause liver and kidney disease.
As you will learn in this chapter, the liver and kidneys are important organs of the excretory system, and impairment of the functioning of these organs can cause serious health consequences. At the end of the chapter, you will learn which hormone Talia was referring to. You will also learn some of the ways alcohol can affect the excretory system — both after the occasional drink, and in cases of excessive alcohol use and abuse.
Chapter Overview: Excretory System
In this chapter, you will learn about the excretory system, which rids the body of toxic waste products and helps maintain homeostasis. Specifically, you will learn about:
- The organs of the excretory system —including the skin, liver, large intestine, lungs, and kidneys — that eliminate waste and excess water from the body.
- How wastes are eliminated through sweat, feces, urine, and exhaled gases.
- How toxic substances in the blood are broken down by the liver.
- The urinary system, which includes the kidneys, ureters, bladder, and urethra.
- The main function of the urinary system, which is to filter the blood and eliminate wastes, mineral ions, and excess water from the body in the form of urine.
- How the kidneys filter the blood, retain necessary substances, produce urine, and help maintain homeostasis (such as proper ion and water balance).
- How urine is stored, transported, and released from the body.
- Disorders of the urinary system, including bladder infections, kidney stones, polycystic kidney disease, urinary incontinence, and kidney damage caused by factors such as uncontrolled diabetes and high blood pressure.
As you read the chapter, think about the following questions:
- Which hormone do you think Talia was referring to? Remember that this hormone causes the urinary system to retain water and excrete less water out in urine.
- How and where does this hormone work?
- Long-term, excessive use of alcohol can affect the liver and kidneys. How do these two organs of excretion interact and work together?
Attributions
Figure 16.1.1
Gotta Pee [photo] by Jon-Eric Melsæter on Flickr is used under a CC BY 2.0 (https://creativecommons.org/licenses/by/2.0/) license.
Figure 16.1.2
Bathroom line up [photo] by Dorothy on Flickr is used under a CC BY 2.0 (https://creativecommons.org/licenses/by/2.0/) license.
Image shows systole and diastole of the heart. In diastole, the ventricles of the heart are relaxed and are able to receive blood from the atria. In systole, both ventricles contract, squeezing the blood out and into the pulmonary trunk and aorta.
Image shows a diagram highlighting the different sections of the small intestine. The duodenum is the shortest portion and is the part of the small intestine that receives chyme directly from the stomch. Next, chyme would pass through the jejenum and then finally the ileum. The jejenum and ileum are a similar length (2.5-3 meters).
As described in the caption.
Image shows a diagram of the location of the sinoatrial and atrioventricular nodes. The SA node is located at the top right corner of the right atrium, and the AV node is in left wall of the right atrium, very close to the tricuspid AV valve.
Image shows a diagram of the vessels going into and out of the liver. The hepatic artery bring blood from the heart to the liver and the hepatic vein returns this blood to the heart. The portal vein brings blood from the lower GI tract to the liver.

Case Study: Please Don’t Pass the Bread
Angela and Saloni are college students who met in physics class. They decide to study together for their upcoming midterm, but first, they want to grab some lunch. Angela says there is a particular restaurant she would like to go to, because they are able to accommodate her dietary restrictions. Saloni agrees and they head to the restaurant.
At lunch, Saloni asks Angela what is special about her diet. Angela tells her that she can’t eat gluten. Saloni says, “My cousin did that for a while because she heard that gluten is bad for you. But it was too hard for her to not eat bread and pasta, so she gave it up.” Angela tells Saloni that avoiding gluten isn’t optional for her — she has celiac disease. Eating even very small amounts of gluten could damage her digestive system. It can be difficult for people living with celiac disease to find foods when eating out.
You have probably heard of gluten, but what is it, and why is it harmful to people with celiac disease? Gluten is a protein present in wheat and some other grains (such as barley, rye, and oats), so it is commonly found in foods like bread, pasta, baked goods, and many packaged foods, like the ones pictured in Figure 15.1.2.
Figure 15.1.2 Gluten is a protein present in foods like bread, pasta, and baked goods.
For people with celiac disease, eating gluten causes an autoimmune reaction that results in damage to the small, finger-like villi lining the small intestine, causing them to become inflamed and flattened (see Figure 15.1.3). This damage interferes with the digestive process, which can result in a wide variety of symptoms including diarrhea, anemia, skin rash, bone pain, depression, and anxiety, among others. The degree of damage to the villi can vary from mild to severe, with more severe damage generally resulting in more significant symptoms and complications. Celiac disease can have serious long-term consequences, such as osteoporosis, problems in the nervous and reproductive systems, and the development of certain types of cancers.
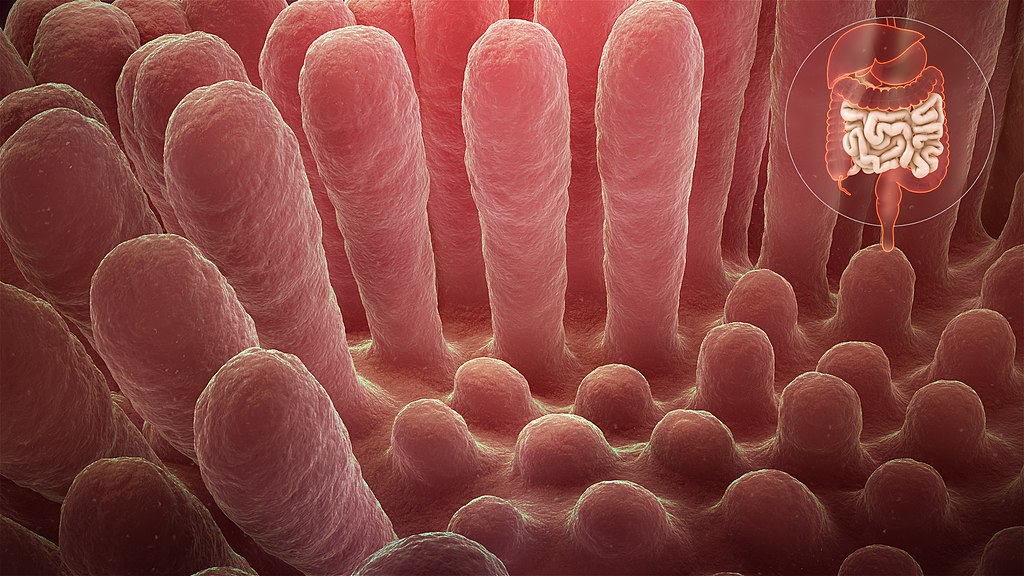
Why does celiac disease cause so many different types of symptoms and have such significant negative health consequences? As you read this chapter and learn about how the digestive system works, you will see just how important the villi of the small intestine are to the body as a whole. At the end of the chapter, you will learn more about celiac disease, why it can be so serious, and whether it is worth avoiding gluten for people who do not have a diagnosed medical issue with it.
Chapter Overview: Digestive System
In this chapter, you will learn about the digestive system, which processes food so that our bodies can obtain nutrients. Specifically, you will learn about:
- The structures and organs of the gastrointestinal (GI) tract through which food directly passes. This includes the mouth, pharynx, esophagus, stomach, small intestine, and large intestine.
- The functions of the GI tract, including mechanical and chemical digestion, absorption of nutrients, and the elimination of solid waste.
- The accessory organs of digestion — the liver, gallbladder, and pancreas — which secrete substances needed for digestion into the GI tract, in addition to performing other important functions.
- Specializations of the tissues of the digestive system that allow it to carry out its functions.
- How different types of nutrients (such as carbohydrates, proteins, and fats) are digested and absorbed by the body.
- Beneficial bacteria that live in the GI tract and help us digest food, produce vitamins, and protect us from harmful pathogens and toxic substances.
- Disorders of the digestive system, including inflammatory bowel diseases, ulcers, diverticulitis, and gastroenteritis (commonly known as “stomach flu”).
As you read this chapter, think about the following questions related to celiac disease:
- What are the general functions of the small intestine? What do the villi in the small intestine do?
- Why do you think celiac disease causes so many different types of symptoms and potentially serious complications?
- What are some other autoimmune diseases that involve the body attacking its own digestive system?
Attributions
Figure 15.1.1
Bread [photo] by Sergio Arze on Unsplash is used under the Unsplash License (https://unsplash.com/license).
Figure 15.1.2
- Paste cu sos de roșii by Sestrjevitovschii Ina on Unsplash is used under the Unsplash License (https://unsplash.com/license).
- Cookies and More by Sarah Shaffer on Unsplash is used under the Unsplash License (https://unsplash.com/license).
- Raspberry waffles by Izabelle Acheson on Unsplash is used under the Unsplash License (https://unsplash.com/license).
- Homemade croissant & pain au chocolat by Cristiano Pinto on Unsplash is used under the Unsplash License (https://unsplash.com/license).
Figure 15.1.3
Inflammed_mucous_layer_of_the_intestinal_villi_depicting_Celiac_disease by www.scientificanimations.com (image 140/191) on Wikimedia Commons is used under a CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0) license.


