18.11 Contraception

Family Planning Pioneer
Her name was Marie Stopes, and she was a British author and paleobotanist who lived from 1880 to 1958. She is pictured in Figure 18.11.1 in her lab next to her microscope. Stopes made significant contributions to science and was the first woman on the faculty of the University of Manchester in England. Her primary claim to fame was her work as a family planning pioneer.
Along with her husband, Stopes founded the first birth control clinic in Britain. She also edited a newsletter called Birth Control News, which gave explicit practical advice on how to avoid unwanted pregnancies. In 1918, she published a sex manual titled Married Love. The book was controversial and influential, bringing the subject of contraception into wide public discourse for the first time.
What Is Contraception?
About a century after Married Love, more than half of all fertile married couples worldwide use some form of contraception. Contraception, also known as birth control, is any method or device used to prevent pregnancy. Birth control methods have been used for centuries, but safe and effective methods only became available in the 20th century, in part because of the work of people like Marie Stopes.
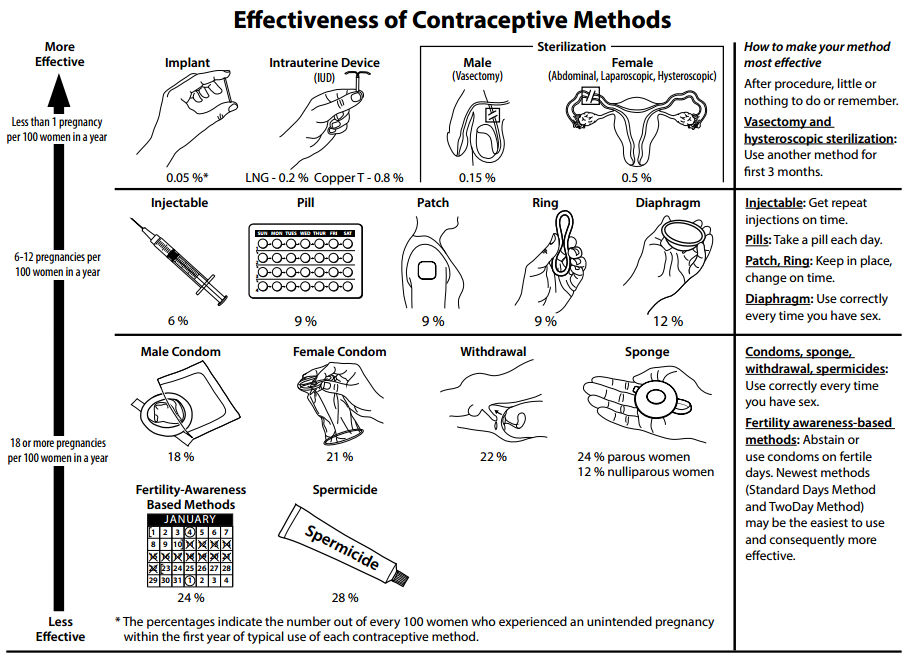
Many different birth control methods are currently available, but they differ considerably in their effectiveness at preventing pregnancy. The effectiveness of contraception is generally expressed as the failure rate, which is the percentage of women who become pregnant using a given method during the first year of use. Virtually no one uses any method of birth control perfectly, so the failure rate with typical use is almost always higher — and often much higher — than the failure rate with perfect use. For example, with perfect use, a birth control method might have a failure rate of just 1%, whereas with typical use, the failure rate might be 25%. For comparison, there is an average one-year pregnancy rate of 85% if no contraception is used.
All methods of birth control have potential adverse effects, but their health risks are less than the health risks associated with pregnancy. Using contraception to space the children in a family is also good for the children’s health and development, as well as for the health of the mother.
Types of Contraception and Their Effectiveness
Types of birth control methods include barrier methods, hormonal methods, intrauterine devices, behavioural methods, and sterilization. With the exception of sterilization, all of these methods are reversible. Examples of each type of birth control method and their failure rates with typical use are described below. Much of the information is also summarized in Figure 18.11.2.
Barrier Methods
Barrier methods are devices that are used to physically block sperm from entering the uterus. They include condoms and diaphragms.

Condoms
Condoms are the most commonly used method of birth control globally. There are condoms for females and males, but male condoms are more widely used, less expensive, and more readily available. Both types of condoms are pictured in Figures 18.11.3 and 18.11.4. A male condom is placed on a man’s erect penis, and a female condom is placed inside a woman’s vagina. Whichever type of condom is used, it must be put in place before sexual intercourse occurs. Condoms work by physically blocking ejaculated sperm from entering the vagina of the sexual partner. With typical use, male condoms have an 18% failure rate, and female condoms have a 21% failure rate. Unlike virtually all other birth control methods, condoms also help prevent the spread of sexually transmitted infections (STIs), in addition to helping to prevent pregnancy.


Diaphragms
Diaphragms, like the one pictured in Figure 18.11.5, ideally prevent sperm from passing through the cervical canal and into the uterus. A diaphragm is inserted vaginally before sexual intercourse occurs and must be placed over the cervix to be effective. It is usually recommended that a diaphragm be covered with spermicide before insertion for extra protection. It is also recommended that the diaphragm be left in place for at least six hours after intercourse. The failure rate of diaphragms with typical use is about 12%, which is about half that of condoms. However, diaphragms do not help prevent the spread of STIs, and their use is also associated with an increased frequency of urinary tract infections in females.
Hormonal Methods
Hormonal contraception is the administration of hormones to prevent ovulation. Hormones can be taken orally in birth control pills, implanted under the skin, injected into a muscle, or received transdermally from a skin patch. Hormonal methods are currently available only for women, although hormonal contraceptives for men are being tested in clinical trials.
Birth control pills are the most common form of hormonal contraception. There are two types of pills: the combined pill (which contains both estrogen and progesterone) and the progesterone-only pill. Both types of pills inhibit ovulation and thicken cervical mucus. The failure rate of birth control pills is only about 1% or less, if used perfectly. However, the failure rate rises to about 10% with typical use, because women do not always remember to take the pill at the same time every day. The combined pill is associated with a slightly increased risk of blood clots, but a reduced risk of ovarian and endometrial cancers. The progesterone-only pill does not increase the risk of blood clots, but it may cause irregular menstrual periods. It may take a few weeks or even months for fertility to return to normal after long-term use of birth control pills.
Intrauterine Devices
An intrauterine device (IUD) is a T-shaped or coiled plastic structure that is inserted into the uterus via the vagina and cervix that contains either copper or a hormone. You can see an IUD in the uterus in the drawing of the female reproductive system in Figure 18.11.6. An IUD is inserted by a physician and may be left in place for months or even years. A physician also must remove an IUD, using the strings attached to the device. The copper in copper IUDs prevents pregnancy by interfering with the movement of sperm so they cannot reach and fertilize an egg. The copper may also prevent implantation in the unlikely circumstance of a sperm managing to reach and fertilize an ovum, in which case the blastocyst/zygote would be shed during menstruation. The hormones in hormonal IUDs prevent pregnancy by thickening cervical mucus and trapping sperm. The hormones may also interfere with ovulation, so there is no egg to fertilize.
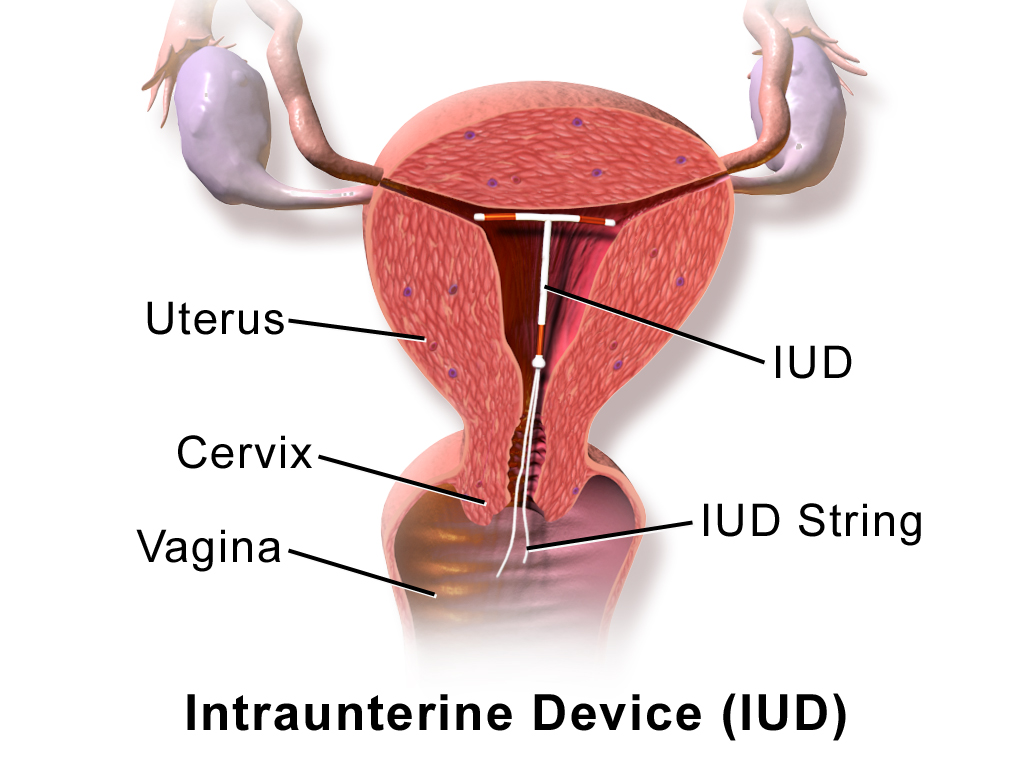
For both types of IUDs, the failure rates are <1%, and failure rates with typical use are virtually the same as failure rates with perfect use. Their effectiveness is one reason that IUDs are among the most widely used forms of reversible contraception. Once removed, even after long-term use, fertility returns to normal immediately. On the other hand, IUDs do have a risk of complications, including increased menstrual bleeding and more painful menstrual cramps. IUDs are also occasionally expelled from the uterus, and there is a slight risk of perforation of the uterus by the IUD.
Behavioural Methods
The least effective methods of contraception are behavioural methods. They involve regulating the timing or method of intercourse to prevent introduction of sperm into the female reproductive tract, either altogether or when an egg may be present. Behavioural methods include fertility awareness methods and withdrawal. Abstinence from sexual activity, or at least from vaginal intercourse, is sometimes considered a behavioural method, as well — but it is unlikely to be practiced consistently enough by most people to prevent pregnancy. Even teens who receive abstinence-only sex education do not have reduced rates of pregnancy. Abstinence is also ineffective in cases of non-consensual sex.
Fertility Awareness Methods
Fertility awareness methods involve estimating the most fertile days of the menstrual cycle and then avoiding unprotected vaginal intercourse on those days. The most fertile days are generally a few days before ovulation occurs, the day of ovulation, and another day or two after that. Unless unprotected sex occurs on those days, pregnancy is unlikely. Techniques for estimating the most fertile days include monitoring and detecting minor changes in basal body temperature or cervical secretions. This requires daily motivation and diligence, so it is not surprising that typical-use failure rates of these methods are at least 20–25%, and for some individuals may be as high as using no contraception at all (85%).
Basal body temperature is the lowest body temperature when the body is at rest (usually during sleep). It is most often estimated by a temperature measurement taken immediately upon awakening in the morning and before any physical activity has occurred. Basal body temperature normally rises after ovulation occurs, as shown in the graph below (Figure 18.11.7). The increase in temperature is small but consistent and may be used to determine when ovulation occurs, around which time unprotected intercourse should be avoided to prevent pregnancy. However, basal body temperature only shows when ovulation has already occurred, and it cannot predict in advance when ovulation will occur. Sperm can live for up to a week in the female reproductive tract, so determining the occurrence of ovulation only after ovulation has already happened is a major drawback of this method.
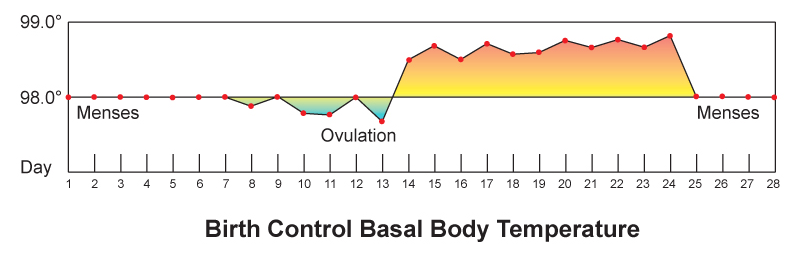
Monitoring cervical mucus has the potential for being more effective than monitoring basal body temperature, because it can predict ovulation ahead of time. As ovulation approaches, cervical secretions usually increase in amount and become thinner (which helps sperm swim through the cervical canal). By recognizing the changing characteristics of cervical mucus, a woman may be able to predict when she will ovulate. From this information, she can determine when she should avoid unprotected sex to prevent pregnancy.
Withdrawal
Withdrawal (also called coitus interruptus) is the practice of withdrawing the penis from the vagina before ejaculation ensues. The main risk of the withdrawal method is that the man may not perform the maneuver correctly or in a timely manner. Fluid typically released from the penis before ejaculation occurs may also contain some sperm. In addition, if sperm are ejaculated just outside of the vagina, there is a chance they will be able to enter the vagina and travel through the female reproductive tract to fertilize an egg. For all these reasons, the withdrawal method has a relatively high failure rate of about 22% with typical use.
Sterilization
The most effective contraceptive method is sterilization. In both sexes, sterilization generally involves surgical procedures that are considered irreversible. Additional surgery may be able to reverse a sterilization procedure, but there are no guarantees. Male sterilization is generally less invasive and less risky than female sterilization.
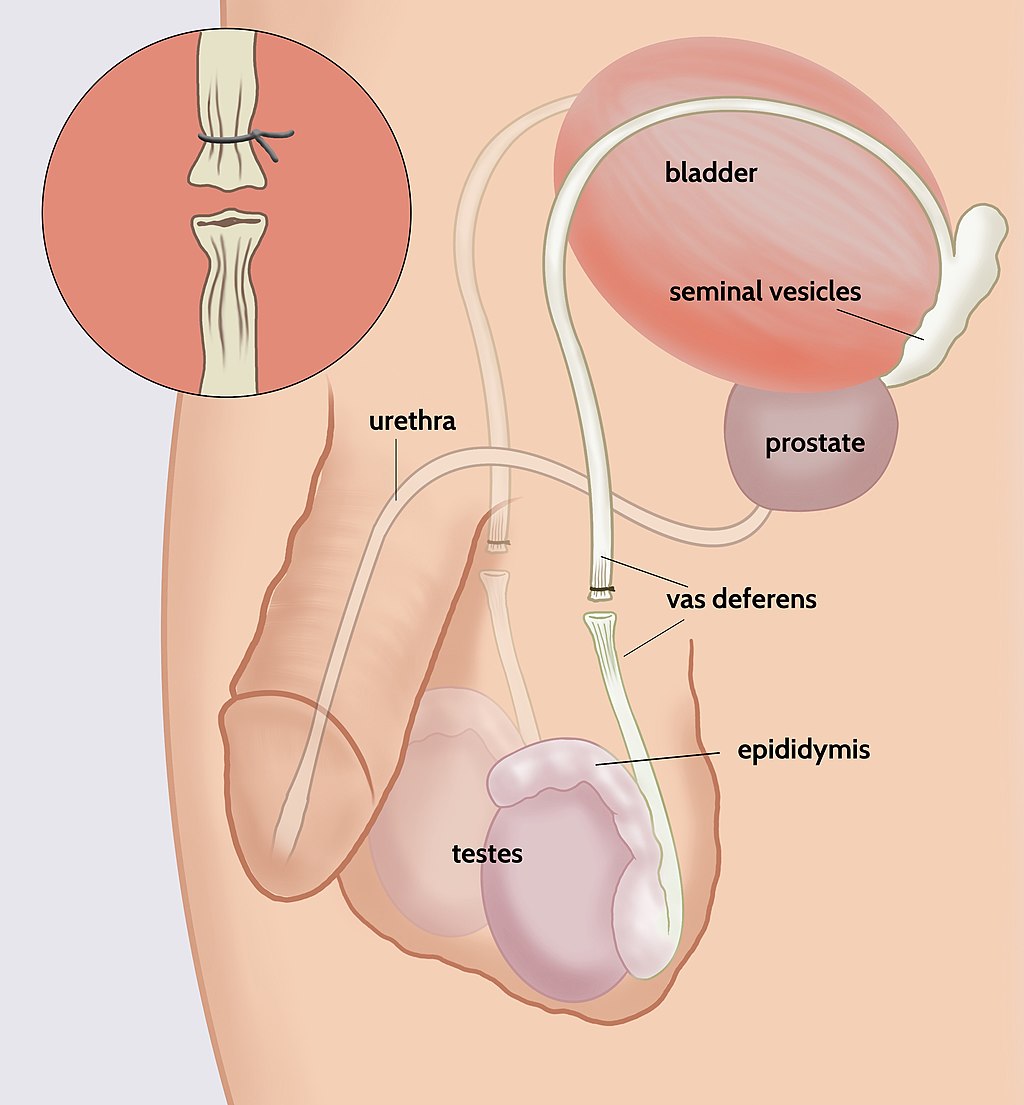
Male Sterilization
Male sterilization is usually achieved with a vasectomy. In this surgery, the vas deferens from each testis is clamped, cut, or otherwise sealed (see Figure 18.11.8). This prevents sperm from traveling from the epididymis to the ejaculatory ducts and being ejaculated from the penis. The same amount of semen will still be ejaculated, but it will not contain any sperm, making fertilization impossible. After a vasectomy, the testes continue to produce sperm, but the sperm are reabsorbed. It usually takes several months after a vasectomy for all remaining sperm to be ejaculated or reabsorbed. In the meantime, another method of birth control should be used.
Female Sterilization
The procedure undertaken for female sterilization is usually tubal ligation. The oviducts may be tied or cut in a surgical procedure, which permanently blocks the tubes. Alternatively, tiny metal implants may be inserted into the oviducts in a nonsurgical procedure. Over time, scar tissue grows around the implants and permanently blocks the tubes. Either method stops eggs from traveling from the ovaries through the oviducts, where fertilization usually takes place.
Emergency Contraception
Emergency contraception is any form of contraception that is used after unprotected vaginal intercourse. One method is the so-called “morning-after” pill. This is essentially a high-dose birth control pill that helps prevent pregnancy by temporarily preventing ovulation. It works only if ovulation has not already occurred, and when taken within five days after unprotected sex. The sooner the pill is taken, the more likely it is to work. Another method of emergency contraception is the IUD. An IUD that is inserted up to five days after unprotected sex can prevent nearly 100% of pregnancies. It keeps sperm from reaching and fertilizing an egg, or inhibits implantation if an ovum has already been fertilized. The IUD can then be left in place to prevent future pregnancies.
18.11 Summary
- More than half of all fertile couples worldwide use contraception (birth control), which is any method or device used to prevent pregnancy. Different methods of contraception vary in their effectiveness, typically expressed as the failure rate, or the percentage of women who become pregnant using a given method during the first year of use. For most methods, the failure rate with typical use is much higher than the failure rate with perfect use.
- Types of birth control methods include barrier methods, hormonal methods, intrauterine devices, behavioural methods, and sterilization. Except for sterilization, all of the methods are reversible. All of the methods have health risks, but they are less than the risks of pregnancy.
- Barrier methods are devices that block sperm from entering the uterus. They include condoms and diaphragms. Of all birth control methods, only condoms can prevent the spread of sexually transmitted infections in addition to pregnancy.
- Hormonal methods involve the administration of hormones to prevent ovulation. Hormones can be administered in various ways, such as in an injection, through a skin patch, or — most commonly — in birth control pills. There are two types of birth control pills: those that contain estrogen and progesterone, and those that contain only progesterone. Both types are equally effective, but they have different potential side effects.
- An intrauterine device (IUD) is a small T-shaped plastic structure containing copper or a hormone that is inserted into the uterus by a physician and left in place for months or even years. It is highly effective even with typical use, but it does have some risks, such as increased menstrual bleeding and, rarely, perforation of the uterus.
- Behavioural methods involve regulating the timing or method of intercourse to prevent introduction of sperm into the female reproductive tract, either altogether or when an egg may be present. In fertility awareness methods, unprotected intercourse is avoided during the most fertile days of the cycle, as estimated by basal body temperature or the characteristics of cervical mucus. In withdrawal (coitus interruptus), the penis is withdrawn from the vagina before ejaculation occurs. Behavioural methods are the least effective methods of contraception.
- Sterilization is the most effective contraceptive method, but it requires a surgical procedure and may be irreversible. Male sterility is usually achieved with a vasectomy, in which the vas deferens are clamped or cut to prevent sperm from being ejaculated in semen. Female sterility is usually achieved with a tubal ligation, in which the oviducts are clamped or cut to prevent sperm from reaching and fertilizing eggs.
- Emergency contraception is any form of contraception used after unprotected vaginal intercourse. One method is the “morning after” pill, which is a high-dose birth control pill that can be taken up to five days after unprotected sex. Another method is an IUD, which can be inserted up to five days after unprotected sex.
18.11 Review Questions
-
- How is the effectiveness of contraceptive methods typically measured?
- What is an IUD?
- Discuss sterilization as a birth control method. Compare sterilization in males and females.
- What is emergency contraception? When is it used? What are two forms of emergency contraception?
- How does the thickness of cervical mucus relate to fertility? How do two methods of contraception take advantage of this relationship?
- If a newly developed method of contraception had a 35% failure rate, would you consider this to be an effective method? Explain your answer.
18.11 Explore More
How do contraceptives work? – NWHunter, TED-Ed, 2016.
The History Of Birth Control | TIME, 2015.
Finally, A Male Pill? SciShow, 2012.
Attributions
Figure 18.11.1
512px-Marie_Stopes [cropped] by AdamBMorgan on Wikimedia Commons is in the public domain (https://en.wikipedia.org/wiki/public_domain). (Original by Unknown author: File:Marie Stopes in her laboratory, 1904.jpg).
Figure 18.11.2
Effectivenessofcontraceptives by Center for Disease Control and Prevention on Wikimedia Commons is in the public domain (https://en.wikipedia.org/wiki/public_domain).
Figure 18.11.3
Condom by Reproductive Health Supplies Coalition on Unsplash is used under the Unsplash License (https://unsplash.com/license).
Figure 18.11.4
Female condom by Ceridwen on Wikimedia Commons is used under a CC BY-SA 2.0 FR (https://creativecommons.org/licenses/by-sa/2.0/fr/deed.en) license.
Figure 18.11.5
Contraceptive_diaphragm by Axefan2 on Wikimedia Commons is in the public domain (https://en.wikipedia.org/wiki/public_domain).
Figure 18.11.6
1024px-Blausen_0585_IUD by BruceBlaus on Wikimedia Commons is used under a CC BY 3.0 (https://creativecommons.org/licenses/by/3.0) license.
Figure 18.11.7
Basal_Body_Temperature by BruceBlaus on Wikimedia Commons is used under a CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0) license.
Figure 18.11.8
1024px-Open_Vasectomy_ by Timdwilliamson on Wikimedia Commons is used under a CC BY SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0) license.
References
Blausen.com Staff. (2014). Medical gallery of Blausen Medical 2014. WikiJournal of Medicine 1 (2). DOI:10.15347/wjm/2014.010. ISSN 2002-4436
SciShow. (2012, August 16). Finally, a male pill? YouTube. https://www.youtube.com/watch?v=vIaL5QiKbWI&feature=youtu.be
Stopes, M. (1918). Married love. Wikisource. https://en.wikisource.org/w/index.php?title=Married_Love&oldid=6230157 (Originally published with Preface and Notes by William J. Robinson, by The Critic and Guide Company. This book was banned in the United States until 1933.)
TED-Ed. (2016, September). How do contraceptives work? – NWHunter. YouTube. https://www.youtube.com/watch?v=Zx8zbTMTncs&feature=youtu.be
Time. (2015, January 30). The history of birth control | TIME. YouTube. https://www.youtube.com/watch?v=jdr1yDO7MoY&feature=youtu.be
Wikipedia contributors. (2020, August 9). Marie Stopes. In Wikipedia. https://en.wikipedia.org/w/index.php?title=Marie_Stopes&oldid=972063381
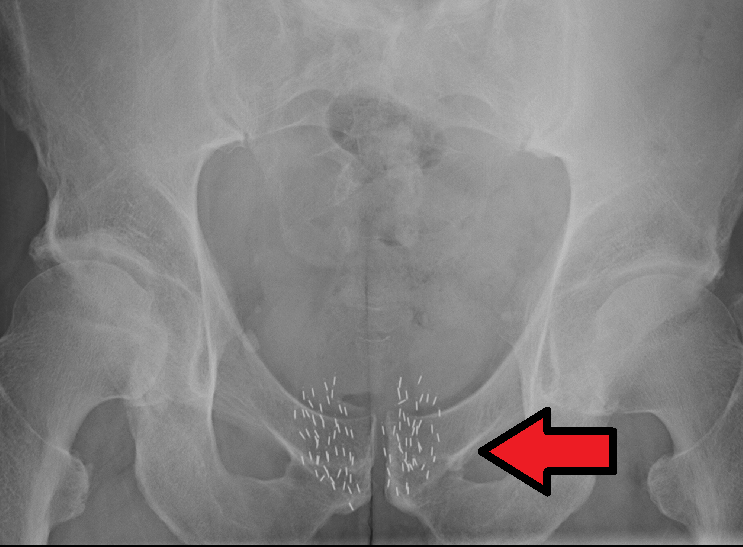
Image shows an Xray of the pelvic region of a male undergoing Brachytherapy. You cannot see the actual prostate gland in the xray, but you can see the tiny radioactvie beads that have been implanted in the prostate to kill the cancer cells.
Created by CK-12 Foundation/Adapted by Christine Miller

Offering to the Gods
The marble penis and scrotum depicted in Figure 18.5.1 comes from ancient Rome, during the period from about 200 BCE to 400 CE. During that time, offerings like this were commonly given to the gods by people with health problems, either in the hopes of a cure, or as thanks for receiving one. The offerings were generally made in the shape of the afflicted body part. Scholars think this marble penis and scrotum may have been an offering given in hopes of — or thanks for — a cure for impotence, known medically today as erectile dysfunction.
Erectile Dysfunction
Erectile dysfunction (ED) is sexual dysfunction characterized by the regular and repeated inability of a sexually mature male to obtain or maintain an erection. It is a common disorder that affects about 40% of males, at least occasionally.
Causes of Erectile Dysfunction
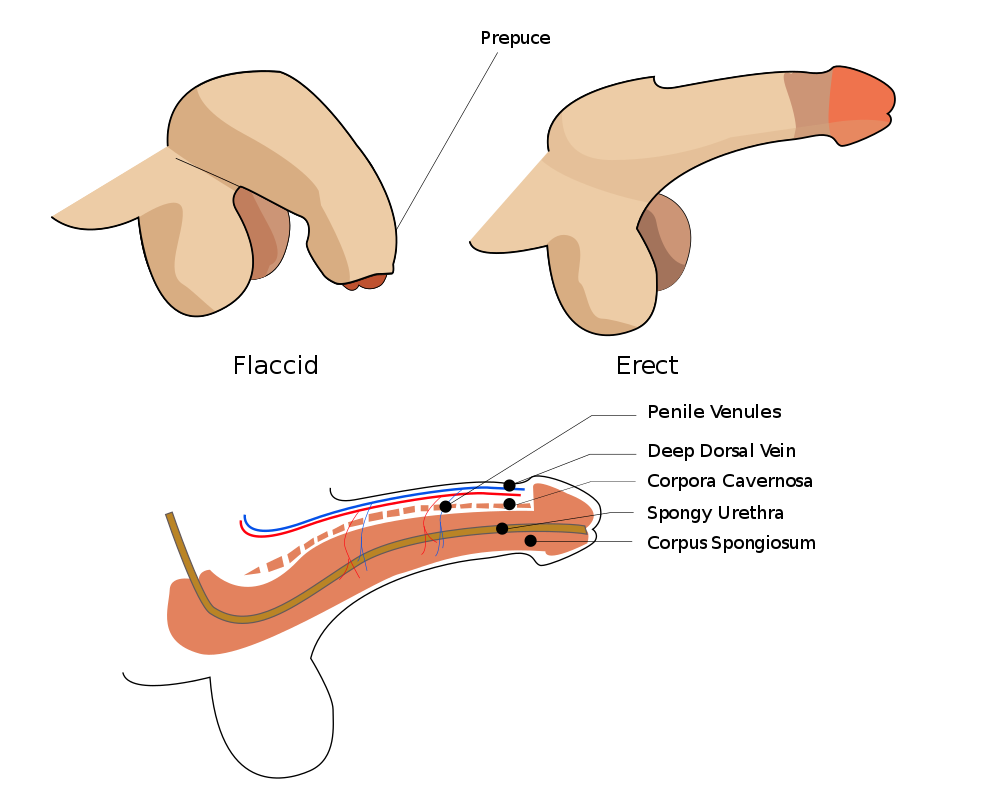
The penis normally stiffens and becomes erect when the columns of spongy tissue within the shaft of the penis (the corpus cavernosa and corpus spongiosum in Figure 18.5.2) become engorged with blood. Anything that hampers normal blood flow to the penis may therefore interfere with its potential to fill with blood and become erect. The normal nervous control of sexual arousal or penile engorgement may also fail and lead to problems obtaining or maintaining an erection.
Specific causes of ED include both physiological and psychological causes. Physiological causes include the use of therapeutic drugs (such as antidepressants), aging, kidney failure, diseases (such as diabetes or multiple sclerosis), tobacco smoking, and treatments for other disorders (such as prostate cancer). Psychological causes are less common, but may include stress, performance anxiety, or mental disorders. The risk of ED may also be greater in men with obesity, cardiovascular disease, poor dietary habits, and overall poor physical health. Having an untreated hernia in the groin may also lead to ED.
Treatments for Erectile Dysfunction
Treatment of ED depends on its cause or contributing factors. For example, for tobacco smokers, smoking cessation may bring significant improvement in ED. Improving overall physical health by losing weight and exercising regularly may also be beneficial. The most common first-line treatment for ED, however, is the use of oral prescription drugs, known by brand names such as Viagra® and Cialis®. These drugs help ED by increasing blood flow to the penis. Other potential treatments include topical creams applied to the penis, injection of drugs into the penis, or the use of a vacuum pump that helps draw blood into the penis by applying negative pressure. More invasive approaches may be used as a last resort if other treatments fail. These usually involve surgery to implant inflatable tubes or rigid rods into the penis.
Ironically, the world’s most venomous spider —the Brazilian wandering spider (see Figure 18.5.3) — may offer a new treatment for ED. The venom of this spider is known to cause priapism in human males. Priapism is a prolonged erection that may damage the reproductive organs and lead to infertility if it continues too long. Researchers are investigating one of the components of the spider’s venom as a possible treatment for ED, if taken in minute quantities.

Epididymitis
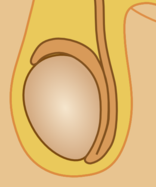
Epididymitis is inflammation of the epididymis. The epididymis is one of the paired organs within the scrotum where sperm mature and are stored. You can see its location in Figure 18.5.4. Discomfort or pain and swelling in the scrotum are typical symptoms of epididymitis, which is a relatively common condition, especially in young men.
Acute vs. Chronic Epididymitis
Epididymitis may be acute or chronic. Acute diseases are generally short-term conditions, whereas chronic diseases may last years — or even lifelong.
Acute Epididymitis
Acute epididymitis generally has a fairly rapid onset, and is most often caused by a bacterial infection. Bacteria in the urethra can back-flow through the urinary and reproductive structures to the epididymis. In sexually active males, approximately 65% of cases of acute epididymitis are caused by sexually transmitted bacteria. Besides pain and swelling, common symptoms of acute epididymitis include redness and warmth in the scrotum, and a fever. There may also be a urethral discharge.
Chronic Epididymitis
Chronic epididymitis is epididymitis that lasts for more than three months. In some men, the condition may last for years. It may occur with or without a bacterial infection being diagnosed. Sometimes, it is associated with lower back pain that occurs after an activity that stresses the lower back, such as heavy lifting or a long period spent driving a vehicle.
Treatment of Epididymitis
If a bacterial infection is suspected, both acute and chronic epididymitis are generally treated with antibiotics. For chronic epididymitis, antibiotic treatment may be prescribed for as long as four to six weeks to ensure the complete eradication of any possible bacteria. Additional treatments often include anti-inflammatory drugs to reduce inflammation of the tissues, and painkillers to control the pain, which may be severe. Physically supporting the scrotum and applying cold compresses may also be recommended to help relieve swelling and pain.
Regardless of symptoms, treatment is important for both acute and chronic epididymitis, because major complications may occur otherwise. Untreated acute epididymitis may lead to an abscess — which is a buildup of pus — or to the infection spreading to other organs. Untreated chronic epididymitis may lead to permanent damage to the epididymis and testis, and it may even cause infertility.
Male Reproductive Cancers

Why does the airplane in Figure 18.5.5 have a huge mustache on its “face”? The mustache is a symbol of “Movember.” This is an international campaign to raise awareness of prostate cancer, as well as money to fund prostate cancer research.
Prostate Cancer
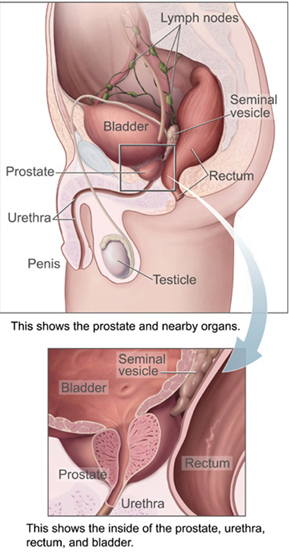
The prostate gland is an organ located in the male pelvis (see Figure 18.5.6). The urethra passes through the prostate gland after it leaves the bladder and before it reaches the penis. The function of the prostate is to secrete zinc and other substances into semen during an ejaculation. In Canada, prostate cancer is the most common type of cancer in men, and the second leading cause of male cancer death. About 1 in 9 Canadian men will be diagnosed with prostate cancer. Prostate cancer occurs at higher rates in rich nations like Canada and the United States, but the rates are increasing everywhere.
How Prostate Cancer Occurs
Prostate cancer occurs when glandular cells of the prostate mutate into tumor cells. Eventually, the tumor, if undetected, may invade nearby structures, such as the seminal vesicles. Tumor cells may also metastasize and travel in the bloodstream or lymphatic system to organs elsewhere in the body. Prostate cancer most commonly metastasizes to the bones, lymph nodes, rectum, or lower urinary tract organs.
Symptoms of Prostate Cancer
Early in the course of prostate cancer, there may be no symptoms. When symptoms do occur, they mainly involve urination, because the urethra passes through the prostate gland. The symptoms typically include frequent urination, difficulty starting and maintaining a steady stream of urine, blood in the urine, and painful urination. Prostate cancer may also cause problems with sexual function, such as difficulty achieving erection or painful ejaculation.
Risk Factors for Prostate Cancer
Some factors that increase the risk of prostate cancer can be changed, and others cannot.
- Risk factors that can be changed include a diet high in meat, a sedentary lifestyle, obesity, and high blood pressure.
- Risk factors that cannot be changed include older age, a family history of prostate cancer, and African ancestry. Family history is an important risk factor, so genes are clearly involved. Many different genes have been implicated.
Diagnosing Prostate Cancer
The only definitive test to confirm a diagnosis of prostate cancer is a biopsy. In this procedure, a small piece of the prostate gland is surgically removed and then examined microscopically. A biopsy is done only after less invasive tests have found evidence that a patient may have prostate cancer.
A routine exam by a doctor may find a lump on the prostate, which might be followed by a blood test that detects an elevated level of prostate-specific antigen (PSA). PSA is a protein secreted by the prostate that normally circulates in the blood. Higher-than-normal levels of PSA can be caused by prostate cancer, but they may also have other causes. Ultrasound or magnetic resonance imaging (MRI) might also be undertaken to provide images of the prostate gland and additional information about the cancer.
Treatment of Prostate Cancer
The average age at which men are diagnosed with prostate cancer is 70 years. Prostate cancer typically is such a slow-growing cancer that elderly patients may not require treatment. Instead, the patients are watched carefully over the subsequent years to make sure the cancer isn’t growing and posing an immediate threat — an approach that is called active surveillance. It is used for at least 50% of patients who are expected to die from other causes before their prostate cancer causes symptoms.
Treatment of younger patients — or those with more aggressively growing tumors — may include surgery to remove the prostate, chemotherapy, and/or radiation therapy (such as brachytherapy, see Figure 18.5.7). All of these treatment options can have significant side effects, such as erectile dysfunction or urinary incontinence. Patients should learn the risks and benefits of the different treatments, and discuss them with their healthcare provider to decide on the best treatment options for their particular case.
Testicular Cancer
The reproductive cancer that most commonly affects young men is testicular cancer. The testes are the paired reproductive organs in the scrotum that produce sperm and secrete testosterone. Although testicular cancer is rare, it is one of the few cancers that is more common in younger than older people. In fact, cancer of the testis is the most common cancer in males between the ages of 20 and 39 years. The risk of testicular cancer is about four to five times greater in men of European than African ancestry. The cause of this difference is unknown.
Signs and Symptoms of Testicular Cancer
One of the first signs of testicular cancer is often a lump or swelling in one of the two testes. The lump may or may not be painful. If pain is present, it may occur as a sharp pain or a dull ache in the lower abdomen or scrotum. Some men with testicular cancer report a feeling of heaviness in the scrotum. Testicular cancer does not commonly spread beyond the testis, but if it does, it most often spreads to the lungs, where it may cause shortness of breath or a cough.
Diagnosis of Testicular Cancer
The main way that testicular cancer is diagnosed is by detection of a lump in the testis. This is likely followed by further diagnostic tests. An ultrasound may be done to determine the exact location, size, and characteristics of the lump. Blood tests may be done to identify and measure tumor-marker proteins in the blood that are specific to testicular cancer. CT scans may also be done to determine whether the disease has spread beyond the testis. However, unlike the case with prostate cancer, a biopsy is not recommended, because it increases the risk of cancer cells spreading into the scrotum.
Treatment of Testicular Cancer
Testicular cancer has one of the highest cure rates of all cancers; it is estimated that 1 in every 250 men will develop this cancer in their lifetime. Three basic types of treatment for testicular cancer are surgery, radiation therapy, and/or chemotherapy. Generally, the initial treatment is surgery to remove the affected testis. If the cancer is caught at an early stage, the surgery is likely to cure the cancer, and has nearly a 100% five-year survival rate. When just one testis is removed, the remaining testis (if healthy) is adequate to maintain fertility, hormone production, and other normal male functions. Radiation therapy and/or chemotherapy may follow surgery to kill any tumor cells that might exist outside the affected testis, even when there is no indication that the cancer has spread. In many cases, however, surgery is followed by surveillance instead of additional treatments.
Feature: My Human Body
Testicular self-exams may catch testicular cancer at a relatively early stage, when a cure is most likely. The Testicular Cancer Foundation of Canada recommends monthly testicular self-exams for all male adolescents and young men. There is no medical consensus on testicular self-exams, however, and some medical organizations even recommend against them. The latter argue that the potential harms of self exams — which include false positive results, anxiety, and risks from diagnostic procedures — outweigh the potential benefits, given the very low incidence and high cure rate of even advanced testicular cancer. If you are a young male, you should discuss with your physician whether you should perform routine testicular self-exams. The self-exam is quick, easy, and painless to do. You can see how to perform a testicular self-exam by visiting the Testicular Canada Website. or watching the video "How to perform a testicular self exam from #TheRCT" below:
https://youtu.be/NvDglB_HXyE
How to perform a testicular self exam from #TheRCT, The Robin Cancer Trust, 2013.
Regardless of whether you perform regular testicular self-exams, if you notice any of the following signs or symptoms, you should be examined by a doctor:
- A lump in one testis.
- A change in size of one testis.
- Pain or tenderness in the testis.
- Blood in the semen during ejaculation.
- Blood in the urine.
- Build-up of fluid in the scrotum.
18.5 Summary
- Erectile dysfunction (ED) is a disorder characterized by the regular and repeated inability of a sexually mature male to obtain and maintain an erection. ED is a common disorder that occurs when normal blood flow to the penis is disturbed, or when there are problems with the nervous control of penile engorgement or arousal.
- Possible physiological causes of ED include aging, illness, drug use, tobacco smoking, and obesity, among others. Possible psychological causes of ED include stress, performance anxiety, and mental disorders.
- Treatments for ED may include lifestyle changes, such as stopping smoking, adopting a healthier diet, and regular exercise. The first-line treatment, however, is prescription drugs such as Viagra® or Cialis® that increase blood flow to the penis. Vacuum pumps or penile implants may be used to treat ED if other types of treatment fail.
- Epididymitis is inflammation of the epididymis. It is a common disorder, especially in young men. It may be acute or chronic, and is often caused by a bacterial infection. Treatments may include antibiotics, anti-inflammatory drugs, and painkillers. Treatment is important to prevent the possible spread of infection, permanent damage to the epididymis or testes, and even infertility.
- Prostate cancer is the most common type of cancer in men, and the second leading cause of cancer death in men. If there are symptoms, they typically involve urination, such as frequent or painful urination. Risk factors for prostate cancer include older age, family history, high-meat diet, and sedentary lifestyle, among others.
- Prostate cancer may be detected by a physical exam or a high level of prostate-specific antigen (PSA) in the blood, but a biopsy is required for a definitive diagnosis. Prostate cancer is typically diagnosed relatively late in life and is usually slow growing, so treatment may not be necessary. In younger patients or those with faster-growing tumors, treatment is likely to include surgery to remove the prostate, followed by chemotherapy and/or radiation therapy.
- Testicular cancer, or cancer of the testes, is the most common cancer in males between the ages of 20 and 39 years. It is more common in males of European than African ancestry. A lump or swelling in one testis, fluid in the scrotum, and testicular pain or tenderness are possible signs and symptoms of testicular cancer.
- Testicular cancer can be diagnosed by a physical exam and diagnostic tests, such as ultrasound or blood tests. Testicular cancer has one of the highest cure rates of all cancers. It is typically treated with surgery to remove the affected testis, and this may be followed by radiation therapy and/or chemotherapy. If the remaining testis is healthy, normal male reproductive functions are still possible after one testis is removed.
18.5 Review Questions
-
- Identify some of the underlying causes of erectile dysfunction. Discuss types of treatment for erectile dysfunction.
- Identify possible treatments for epididymitis. Why is treatment important, even when there are no symptoms?
- What are some of the symptoms of prostate cancer? List risk factors for prostate cancer. How is prostate cancer detected?
- In many cases, treatment for prostate cancer is unnecessary. Why? When is treatment necessary, and what are treatment options?
- Testicular cancer is generally rare, but it is the most common cancer in one age group. What age group is it?
- Identify possible signs and symptoms of testicular cancer. How can testicular cancer be diagnosed? Describe how testicular cancer is typically treated.
18.5 Explore More
https://youtu.be/6D4Mmr2E7hM
Healthier men, one moustache at a time - Adam Garone, TED-Ed, 2013.
https://youtu.be/5i9X8h17VNM
Can Spider Venom Cure Erectile Dysfunction? Gross Science, 2015.
https://youtu.be/DuGXcEjDblI
Undescended Testes: Ask The Expert featuring Dr. Earl Cheng, Lurie Children's, Ann & Robert H. Lurie Children's Hospital of Chicago, 2012.
https://youtu.be/PEIVtXY39NM
What Can Herpes Do To Your Brain? Gross Science, 2015.
https://youtu.be/ECx8YHo2f5c
Dangers of Herbal Viagra Exposed After Lamar Odom Reportedly Took Pills, Inside Edition, 2017.
Attributions
Figure 18.5.1
Votive_male_genitalia,_Roman,_200_BCE-400_CE_Wellcome_L0058590 by Wellcome Images on Wikimedia Commons is used under a CC BY 4.0 (https://creativecommons.org/licenses/by/4.0) license.
Figure 18.5.2
Erection.svg by Hariadhi on Wikimedia Commons is used under a CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0) license.
Figure 18.5.3
Wandering spider by Andreas Kay on Flickr is used under a CC BY-NC-SA 2.0 (https://creativecommons.org/licenses/by-nc-sa/2.0/) license.
Figure 18.5.4
Male_reproductive_system unlabeled by Tsaitgaist (derivative work) on Wikimedia Commons is used under a CC BY-SA 3.0 (http://creativecommons.org/licenses/by-sa/3.0/) license. (Original: Male anatomy.png)
Figure 18.5.5
Movember_(8140167077) by Eva Rinaldi on Wikimedia Commons is used under a CC BY-SA 2.0 (https://creativecommons.org/licenses/by-sa/2.0) license.
Figure 18.5.6
Prostatelead by National Cancer Institute on Wikimedia Commons is in the public domain (https://en.wikipedia.org/wiki/en:Public_domain).
Figure 18.5.7
Brachytherapybeads by James Heilman, MD on Wikimedia Commons CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0) license.
References
Ann & Robert H. Lurie Children's Hospital of Chicago. (2012, December 21). Undescended testes: Ask the expert featuring Dr. Earl Cheng, Lurie Children's. YouTube. https://www.youtube.com/watch?v=DuGXcEjDblI&feature=youtu.be
Gross Science. (2015, August 17). Can spider venom cure erectile dysfunction? YouTube. https://www.youtube.com/watch?v=5i9X8h17VNM&feature=youtu.be
Gross Science. (2015, May 27). What can herpes do to your brain? YouTube. https://www.youtube.com/watch?v=PEIVtXY39NM&feature=youtu.be
Inside Edition. (2017, ). Dangers of herbal viagra exposed after Lamar Odom reportedly took pills. YouTube. https://www.youtube.com/watch?v=ECx8YHo2f5c&feature=youtu.be
Self-examination guide. (n.d.). Testicular Cancer Canada. https://www.testicularcancer.ngo/selfexamination-guide
TED-Ed. (2013, April 7). Healthier men, one moustache at a time - Adam Garone. YouTube. https://www.youtube.com/watch?v=6D4Mmr2E7hM&feature=youtu.be
The Robin Cancer Trust. (2013, November 11). How to perform a testicular self exam from #TheRCT. YouTube. https://www.youtube.com/watch?v=NvDglB_HXyE&feature=youtu.be
A biological process which converts sugars such as glucose, fructose, and sucrose into cellular energy, producing ethanol and carbon dioxide as by-products.
Image shows a diagram labeling the major arteries of the body. Some of these include the carotid artery which provides blood to the neck and head, the brachiocephalic artery which supplies blood to the arms and head, the renal artery supplying blood to the kidneys, the mesenteric arteries supplying blood to the intestines, the femoral arteries supplying blood to the legs.
Image shows a photograph of A Cat Tien fertility stone. The stone is square, with grooves on the top that represent the vagina which leads to a cavity representing the uterus.
As per caption.
Image shows a diagram illustrating how peristalsis pushes food through the digestive tract by squeezing just behind the food, pushing it forward.
Image shows a side view diagram of the male and female pelvis. The male urethra is much longer because it extends through the penis, and in women it exits through the pelvic floor.
As per caption.
Image shows a labelled diagram of the internal structures of the breast. Overlaying the chest muscles are adipose tissue alternating with milk producing structures. These include lobules and ducts, which bring their products to the nipple.
Created by CK-12 Foundation/Adapted by Christine Miller

Fertility Symbol
The geometric design on the ancient stone carving in Figure 18.6.1 represents a powerful symbol of female fertility: the vagina. The symbol is called yoni in Hindu, and it reflects the value placed by Hindu culture on the ability of females to give birth. The vagina is one of several organs in the female reproductive system.
Female Reproductive Organs
The female reproductive system is made up of internal and external organs that function to produce haploid female gametes called ova (or oocytes), secrete female sex hormones (such as estrogen), and carry and give birth to a fetus. The internal female reproductive organs include the vagina, uterus, oviducts, and ovaries. The external organs — collectively called the vulva — include the clitoris and labia.
The vagina is an elastic, muscular canal leading from its opening in the vulva to the neck of the uterus, called the cervix. It is about 7.5 cm (about 3 in) long at the front, and about 9 cm (3.5 in) long at the back. The vagina accommodates the penis and is the site where sperm are usually ejaculated during sexual intercourse. In the context of pregnancy and natural (vaginal) childbirth, the vagina is referred to as the birth canal. In addition, it channels the flow of menstrual blood from the uterus.
Structure of the Vagina
Muscles and ligaments support the vagina within the pelvic cavity. The vagina itself is made up of several layers of fibrous and muscular tissues and lined with mucous membranes. Folds in the mucosa provide the vagina with extra surface area so it can stretch in both length and width during intercourse or childbirth. The elasticity of the vagina and the extra mucosa allow it to stretch to many times its normal diameter in order to deliver a baby.
Bacteria and pH in the Vagina
A healthy vagina is home to many symbiotic bacteria that help prevent pathogens (such as yeast) from colonizing the vagina. The pH in the vagina is normally between 3.8 and 4.5, and this acidity also helps keep pathogenic microorganisms from colonizing it. The vagina constantly sheds its epithelium, so it is considered self-cleaning. As a consequence, there is no need for douching to clean it. Physicians actually discourage the practice, as it may upset the normal bacterial and pH balance in the vagina, although washing the vulva with a mild soap is good practice.
Uterus
The uterus (commonly called the womb) is a pear-shaped, muscular organ that is about 7.6 cm (about 3 in) long. It is located above the vagina and behind the bladder in the centre of the pelvis. The position of the uterus in the pelvis is stabilized by several ligaments and bands of supportive tissue. The uterus is where a fetus develops during gestation, and the organ provides mechanical protection and support for the developing offspring. Contractions of the muscular wall of the uterus are responsible for pushing the fetus out of the uterus during childbirth.
Parts of the Uterus
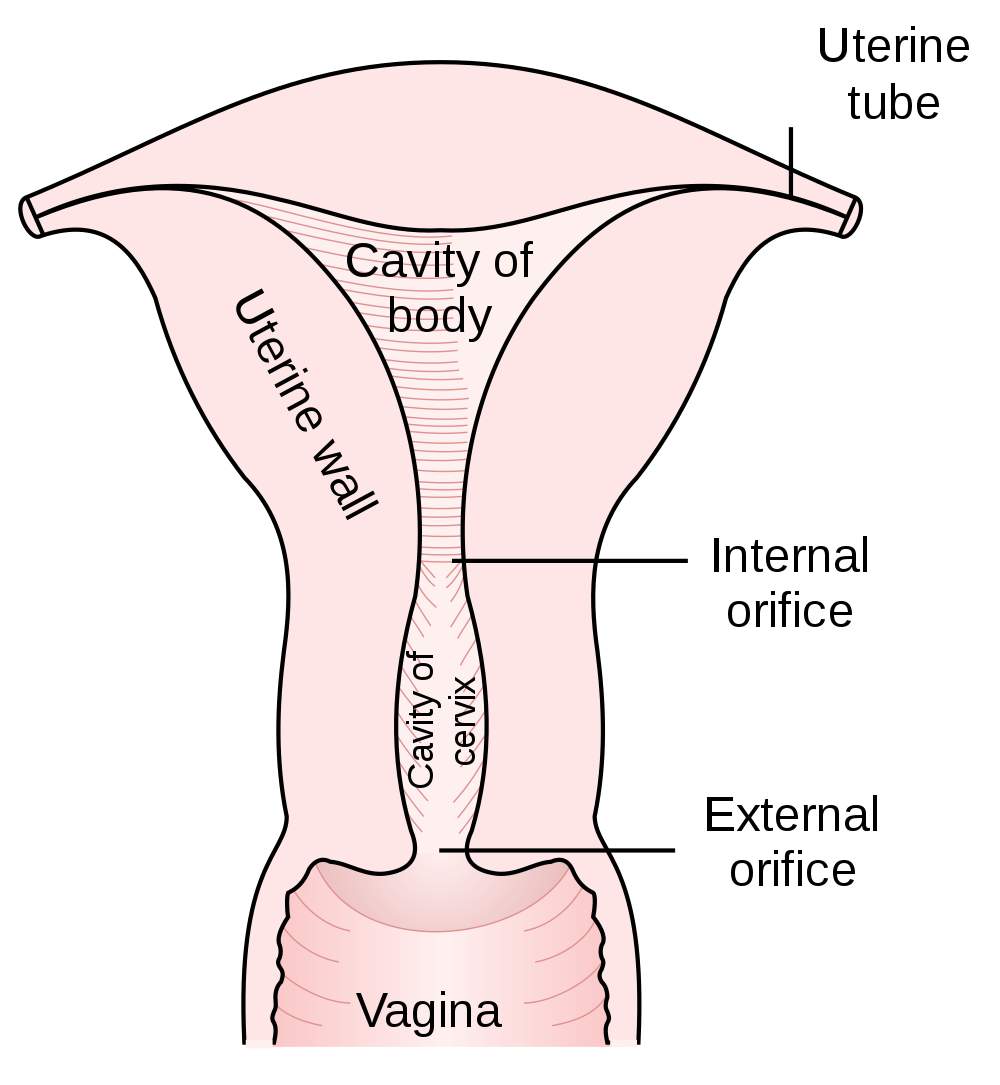
As shown in Figure 18.6.2, the lower end of the uterus forms the cervix, which is also called the neck of the uterus. The cervix is about 2.5 cm (almost 1 in) long and protrudes downward into the vagina. A small canal runs the length of the cervix, connecting the uterine cavity with the lumen of the vagina. This allows semen deposited in the vagina to enter the uterus, and a baby to pass from the uterus into the vagina during birth. Glands in the cervix secrete mucus that varies in water content and thickness, so it can function either as a barrier to keep microorganisms out of the uterus during pregnancy, or as a transport medium to help sperm enter the uterus around the time of ovulation. The rest of the uterus above the cervix is called the body of the uterus. The upper end of the uterus is connected with the two oviducts.
Tissues of the Uterus
As indicated in Figure 18.6.3, the uterus consists of three tissue layers, called the endometrium, myometrium, and perimetrium.
- The endometrium is the innermost tissue layer of the uterus. It consists of epithelial tissue, including mucous membranes. This layer thickens during each menstrual cycle and, unless an egg is fertilized, sloughs off during the following menstrual period. If an ovum is fertilized, the thickened endometrium is maintained by hormones and provides nourishment to the embryo. As gestation progresses, the endometrium develops into the maternal portion of the placenta.
- The placenta is a temporary organ that consists of a mass of maternal and fetal blood vessels through which the mother’s and fetus’s blood exchange substances.
- The myometrium is the middle layer of the uterus. It consists mostly of a thick layer of smooth muscle tissue. Powerful contractions of the smooth muscle allow the uterus to contract and expel an infant during childbirth.
- The perimetrium is the outermost layer of the uterus. It covers the outer surface of the uterus. This layer actually consists of two layers of epithelium that secrete fluid into the space between them. The fluid allows for small movements of the uterus within the pelvis, without causing it to rub against other organs.
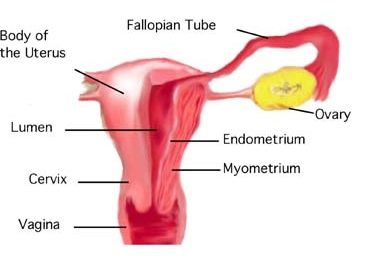
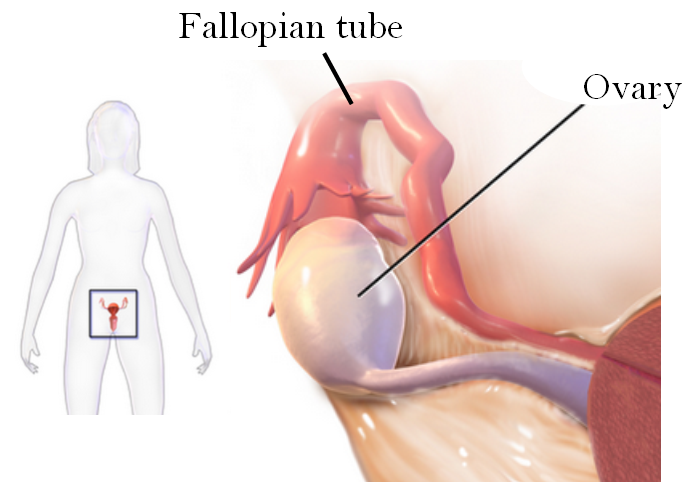
Oviducts
The oviducts (often referred to as Fallopian tubes) are two thin tubes that lie between the ovaries and the uterus. The oviducts are not attached to the ovaries, but their broad upper ends — called infundibula — lie very close to the ovaries. The infundibula also have fringe-like extensions called fimbriae that move in a waving motion to help guide eggs from the ovaries into the oviducts. The lower ends of the oviducts are attached to the upper part of the body of the uterus on either side of the body. They open into the uterus.
The oviducts are made up of multiple tissue layers. The innermost layer consists of mucosal epithelium. The epithelium is covered with cilia, which can move in a sweeping motion to help ova move through the tube from the ovary to the uterus. In between the ciliated cells of the epithelium are cells that secrete a fluid called tubular fluid. This fluid contains nutrients for sperm, ova, and zygotes. The secretions in tubular fluid also remove certain molecules from the plasma membrane of sperm so they are better able to penetrate an egg. Other layers of the oviducts consist of connective tissue and smooth muscle. Contractions of the smooth muscle allow peristalsis to help move eggs through the tubes.
Ovaries
Like the testes in males, the ovaries in females are gonads that produce gametes and secrete sex hormones. The gametes produced by the ovaries are called ova, or oocytes. The main sex hormone secreted by the ovaries is estrogen. The position of the paired ovaries relative to the other reproductive system organs is shown in Figure 18.6.4. Each ovary lies along one side of the uterus and is about 4 cm (a little more than 1.5 in) long. Fibrous ligaments attach one end of each ovary to its nearby oviduct and the other and to its side of the uterus. These ligaments keep the ovaries in place within the pelvis.
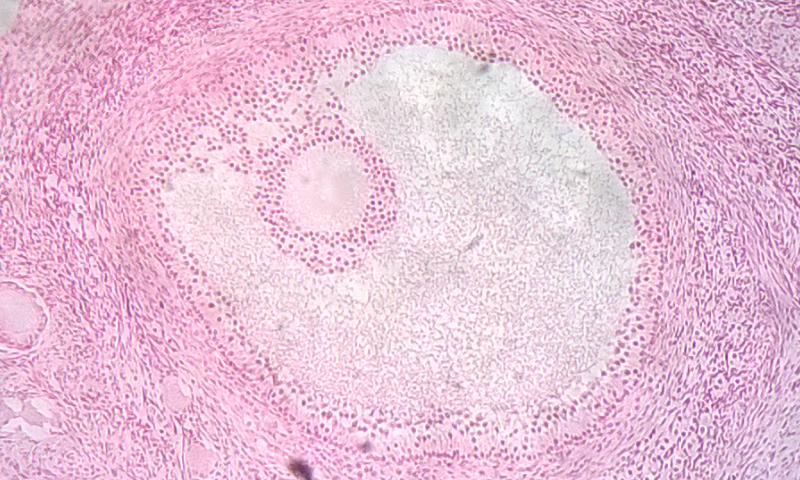
Ovarian Follicles
The ovary consists of two main layers, called the ovarian medulla (the inner layer) and the ovarian cortex (the outer layer). The ovary also contains blood and lymphatic vessels. The ovarian cortex consists primarily of the functional units of the ovaries, which are called ovarian follicles. The follicles are nests of epithelial cells, within each of which is an ovum. The photomicrograph in Figure 18.6.5 shows an ovarian follicle and the developing ovum inside it. If an ovum and follicle complete maturation, the follicle ruptures and the ovum is released from the ovary. This event is called ovulation.
Ova in the Ovaries
Whereas the male testes produce sperm continuously after puberty, the female ovary already contains all the ova it will ever produce by the time a female is born. At birth, a baby girl’s ovaries contain at least a million eggs, each of which is contained within a follicle. Only about 500 of these eggs will eventually mature and be ovulated. This process starts at puberty and typically continues at monthly intervals until menopause occurs around age 52. The remaining eggs never mature, and their number declines as the woman ages. By menopause, a woman’s reserve of eggs is nearly depleted, and ovulation no longer occurs.
Vulva
The vulva is a general term for all of the external female reproductive organs. The vulva includes the clitoris, labia, and external openings for the urethra and vagina.
Labia
The labia (singular, labium) refer to the “lips” of the vulva, which are folds of tissue that contain and protect the other, more delicate structures of the vulva (as shown in Figure 18.6.6). There are two pairs of labia: the outer and larger labia majora, and the inner and smaller labia minora. The labia minora contain numerous sebaceous glands. These glands release secretions that help lubricate the labia and vulvar area.
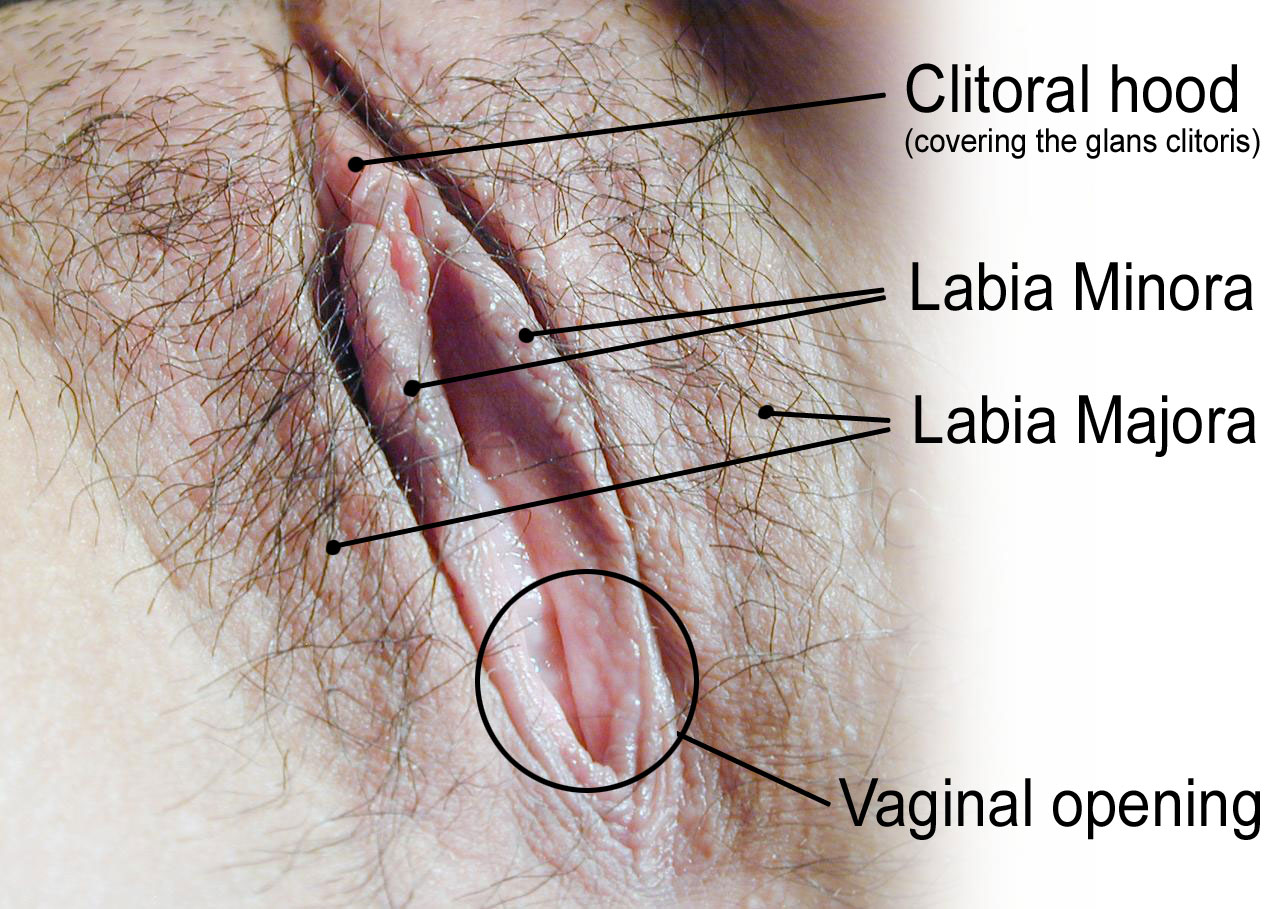
Clitoris
The clitoris, is located at the front of the vulva where the labia minora meet. The visible portion of the clitoris is called the glans clitoris. It is roughly the size and shape of a pea. It is highly sensitive, because it contains many nerve endings. A hood of tissue called the clitoral hood (shown in Figure 18.6.5 above), or prepuce, normally covers and protects the clitoris. The clitoris is the homologue to the male penis, and they both contain spongy tissue. Stimulation of the glans clitoris during sexual activity generally results in sexual arousal in females, and may lead to orgasm. The glans clitoris is the only part of the overall clitoris visible externally, but this spongy tissue extends down either side of the openings to the urethra and vagina, as seen in Figure 18.6.7.
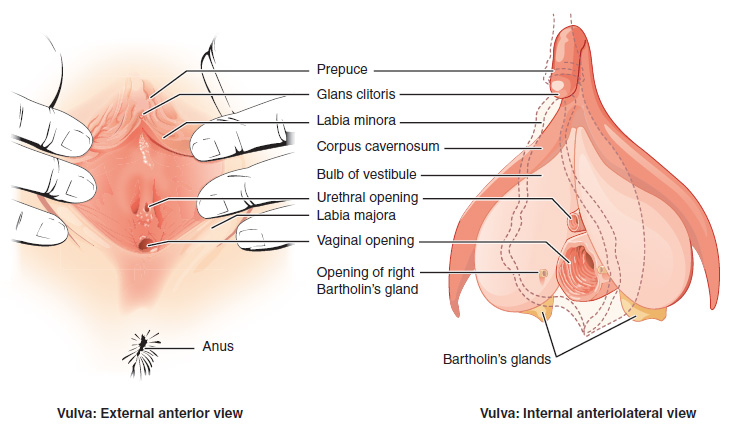
Other Vulvar Structures
The area between the two labia minora is called the vestibule of the vulva. Both the urethra and vagina have openings to the outside of the body in the vestibule. As you can see in Figure 18.6.7 above, the urethral opening (or meatus) is located just in front of, and is much smaller than, the vaginal opening. Both openings are protected by the labia. Two glands — called Bartholin’s glands — open on either side of the vaginal opening. These glands secrete mucus and a vaginal and vulvar lubricant.
Breasts
The breasts are not directly involved in reproduction, but because they contain mammary glands, they can provide nourishment to an infant after birth. The breasts overlay major muscles in the chest from which they project outward in a conical shape. The two main types of tissues in the breast are adipose (fat) tissue and glandular tissue that produces milk. As shown in Figure 18.6.8, each mature breast contains many lobules, where milk is produced and stored during pregnancy. During breastfeeding (or lactation), the milk drains into ducts and sacs, which in turn converge at the nipple. Milk exits the breast through the nipple in response to the suckling action of an infant and is regulated by a positive feedback loop. The nipple is surrounded by a more darkly pigmented area called the areola. The areola contains glands that secrete an oily fluid, which lubricates and protects the nipple during breastfeeding.
18.6 Summary
- The female reproductive system is made up of internal and external organs that function to produce haploid female gametes called ova, secrete female sex hormones (such as estrogen), and carry and give birth to a fetus.
- The vagina is an elastic, muscular canal that can accommodate the penis. It is also where sperm are usually ejaculated during sexual intercourse. The vagina is the birth canal, and it channels the flow of menstrual blood from the uterus. A healthy vagina has a balance of symbiotic bacteria and an acidic pH.
- The uterus is a muscular organ above the vagina where a fetus develops. Its muscular walls contract to push out the fetus during childbirth. The cervix is the neck of the uterus that extends down into the vagina. It contains a canal connecting the vagina and uterus for sperm, or for an infant to pass through. The innermost layer of the uterus — the endometrium — thickens each month in preparation for an embryo, but is shed in the following menstrual period if fertilization does not occur.
- The oviducts extend from the uterus to the ovaries. Waving fimbriae at the ovary ends of the oviducts guide ovulated eggs into the tubes where fertilization may occur as the ova travel to the uterus. Cilia and peristalsis help ova move through the tubes. Tubular fluid helps nourish sperm as they swim up the tubes toward ova.
- The ovaries are gonads that produce ova and secrete sex hormones, including estrogen. Nests of cells called follicles in the ovarian cortex are the functional units of ovaries. Each follicle surrounds an immature ovum. At birth, a baby girl’s ovaries contain at least a million ova, and they will not produce any more during her lifetime. During a woman’s reproductive years, one ova typically matures and is ovulated each month.
- The vulva is a general term for external female reproductive organs. The vulva includes the clitoris, two pairs of labia, and openings for the urethra and vagina. Secretions from mucosal glands near the vaginal opening lubricate the vulva.
- The breasts are not technically reproductive organs, but their mammary glands produce milk to feed an infant after birth. Milk drains through ducts and sacs, and out through the nipple when a baby sucks during breastfeeding.
18.6 Review Questions
-
- State the general functions of the female reproductive system.
- Describe the vagina and its reproductive functions.
- Outline the structure and basic functions of the uterus.
- What is the endometrium? How does it change during the monthly cycle?
- Why are breasts included in discussions of reproduction, if they are not organs of the female reproductive system?
- What is the function of the folds in the mucous membrane lining of the vagina?
- What are two ways in which the female reproductive system protects itself from pathogens?
18.6 Explore More
https://youtu.be/SkB4gG8ke7Q
The uncomplicated truth about women's sexuality | Sarah Barmak, TED, 2019.
https://youtu.be/9rs2gNchQig
Human Physiology - Functional Anatomy of the Female Reproductive System, Janux, 2015.
Attributes
Figure 18.6.1
1024px-Cattien_stone_yoni by Binh Giang on Wikimedia Commons is in the public domain (https://en.wikipedia.org/wiki/en:public_domain).
Figure 18.6.2
1000px-Gray1167.svg by Henry Vandyke Carter (1831-1897) on Wikimedia Commons is in the public domain (https://en.wikipedia.org/wiki/public_domain). (Bartleby.com: Gray’s Anatomy, Plate 1167).
Figure 18.6.3
Uterine_anatomy. from Uterine Stem cells by The Stem Cell Research Community, StemBook on Wikimedia Commons is used under a CC BY 3.0 (https://creativecommons.org/licenses/by/3.0) license.
Figure 18.6.4
Sites_of_tubo_ovarian_abscess by Bfpage on Wikimedia Commons is used under a CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0) license.
Figure 18.6.5
Ovarian_follicle by TiagoLubiana on Wikimedia Commons is used under a CC BY 4.0 (https://creativecommons.org/licenses/by-sa/4.0) license.
Figure 18.6.6
HumanVulva-NewText-PhiloViv by Amphis (edited) on Wikimedia Commons is used under a CC BY-SA 3.0 (https://creativecommons.org/licenses/by-sa/3.0/deed.en) license. (Original en:Image:HumanVulva-NoText-PhiloVivero.jpg by en:user:PhiloVivero)
Figure 18.6.7
Vulva by OpenStax College on Wikimedia Commons is used under a CC BY 3.0 (https://creativecommons.org/licenses/by/3.0) license.
Figure 18.6.8
Breast-Diagram by Women's Health (NCI/ NIH) on Wikimedia Commons is in the public domain (https://en.wikipedia.org/wiki/en:Public_domain).
References
Betts, J. G., Young, K.A., Wise, J.A., Johnson, E., Poe, B., Kruse, D.H., Korol, O., Johnson, J.E., Womble, M., DeSaix, P. (2013, June 19). Figure 27.10 The vulva [digital image]. In Anatomy and Physiology (Section 27.2). OpenStax. https://openstax.org/books/anatomy-and-physiology/pages/27-2-anatomy-and-physiology-of-the-female-reproductive-system
Janux. (2015, January 10). Human physiology - Functional anatomy of the female reproductive system. YouTube. https://www.youtube.com/watch?v=9rs2gNchQig&feature=youtu.be
TED. (2019, March 22). The uncomplicated truth about women's sexuality | Sarah Barmak. YouTube. https://www.youtube.com/watch?v=SkB4gG8ke7Q&feature=youtu.be
Teixeira, J., Rueda, B.R., and Pru, J.K. (September 30, 2008). Figure 1 Uterine anatomy. In Uterine Stem Cells (StemBook, ed.). The Stem Cell Research Community, StemBook, doi/10.3824/stembook.1.16.1, http://www.stembook.org
As per caption
As per caption and preceding paragraph.
Image shows a diagram of the path sperm must take through the female reproductive structures in order to fertilize an ovum. Sperm enters the vagina, swims through the cervis, into the uterus, and then into one of the oviducts, which is where fertilization typically takes place.
Image shows a flowchart of the path of blood through the heart. Beginning at the lungs, oxygenated blood enters the pulmonary veins, then enters the left atrium. Blood then passes through the bicuspid AV valve to enter the left ventricle, which contracts to send blood through the aortic semilunar valve into the aorta. The aorta connects to arteries of the systemic circuit and ultimately deliver oxygen to body tissues. From here, blood is deoxygenated and returns to the heart via veins which merge to form the two vena cava. The vena cava delivers blood to the right atrium, which contracts to send blood through the tricuspid AV valve into the right ventricle, which contracts to send blood through the pulmonary semilunar valve into the pulmonary arteries and to the lungs for re-oxygenation.
a hormonal disorder common among women of reproductive age. Women with PCOS may have infrequent or prolonged menstrual periods or excess male hormone (androgen) levels. The ovaries may develop numerous small collections of fluid (follicles) and fail to regularly release eggs.
Image shows a diagram of the cross sectional layering of heart tissues. As described in the preceding paragraph, the endocardium is a thin layer on the inside of the heart chambers, and myocardium is an extremely thick layer of cardiac muscle, and the pericardium consists of two membranes separated by fluid. The visceral pericardium envelopes the myocardium and the parietal pericardium envelopes the entire heart structure.
Image shows a diagram highlighting the different sections of the small intestine. The duodenum is the shortest portion and is the part of the small intestine that receives chyme directly from the stomch. Next, chyme would pass through the jejenum and then finally the ileum. The jejenum and ileum are a similar length (2.5-3 meters).
Image shows a photograph of an Amish man. His hairstyle and beard with no mustache is evidence that he is married.
As per caption, the photo shows a woman in her second trimester, and then the same woman in her third trimester. Her belly is considerably larger in the third trimester
Image shows a diagram of the stages of labor: Stage 1) Dilation: the cervix begins undilated, and then at full dilation is 10 cm in diameter. 2) Birth: The presentation of the head, then rotation and delivery of anterior shoulder, then delivery of the posterior shoulder, then delivery of the lower body and umbilical cord. 3) Afterbirth delivery: placenta detaches and exits through vagina.
Image shows a diagram comparing a healthy nephron and its blood supply and one with diabetic nephropathy. The diseased one has blood vessels that look deformed and fragile.
A hormone is a signaling molecule produced by glands in multicellular organisms that target distant organs to regulate physiology and behavior.

