17.5 Adaptive Immune System
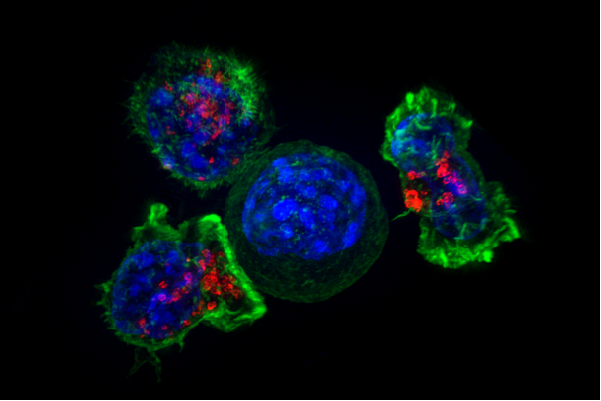
The Kiss of Death
The photomicrograph in Figure 17.5.1 shows a group of killer T cells (green and red) surrounding a cancer cell (blue, centre). When a killer T cell makes contact with the cancer cell, it attaches to and spreads over the dangerous target. The killer T cell then uses special chemicals stored in vesicles (red) to deliver the killing blow. This event has thus been nicknamed “the kiss of death.” After the target cell is killed, the killer T cells move on to find the next victim. Killer T cells like these are important players in the adaptive immune system.
What Is the Adaptive Immune System?
The adaptive immune system is a subsystem of the overall immune system. It is composed of highly specialized cells and processes that eliminate specific pathogens and tumor cells. An adaptive immune response is set in motion by antigens that the immune system recognizes as foreign. Unlike an innate immune response, an adaptive immune response is highly specific to a particular pathogen (or its antigen). An important function of the adaptive immune system that is not shared by the innate immune system is the creation of immunological memory — or immunity — which occurs after the initial response to a specific pathogen. It allows for a faster, stronger response on subsequent encounters with the same pathogen, usually before the pathogen can even cause symptoms of illness.
Lymphocytes are the main cells of the adaptive immune system. They are leukocytes that arise and mature in organs of the lymphatic system, including the bone marrow and thymus. The human body normally has about 2 trillion lymphocytes, which constitute about 1/3 of all leukocytes. Most of the lymphocytes are normally sequestered within tissue fluid or organs of the lymphatic system, including the tonsils, spleen, and lymph nodes. Only about 2% of the lymphocytes are normally circulating in the blood. There are two main types of lymphocytes involved in adaptive immune responses, called T cells and B cells. T cells destroy infected cells or release chemicals that regulate immune responses. B cells secrete antibodies that bind with antigens[/pb_glossary] of [pb_glossary id="271"]pathogens so they can be removed by other immune cells or processes.
Pathways of the Adaptive Immune Response
There are some general similarities in the way in which the separate adaptive immune responses occur in T cell and B cell responses. In both pathways, a foreign antigen is recognized by the B or T cell. From there, cytokines produced by helper T-cells promote clonal expansion of lymphocytes. From this clonal expansion, two types of B or T cells are produced- cells that directly fight the pathogen invasion and cells that remain behind to provide long-term immunity. Finally, once the pathogen invasion has been eradicated, the plasma cells and killer T cells go through apoptosis (programmed cell death).
T Cells
There are multiple types of T cells, or T lymphocytes. Major types are killer (or cytotoxic) T cells and helper T cells. Both types develop from immature T cells that become activated by exposure to an antigen.
T Cell Activation (or Cell-Mediated Immunity)
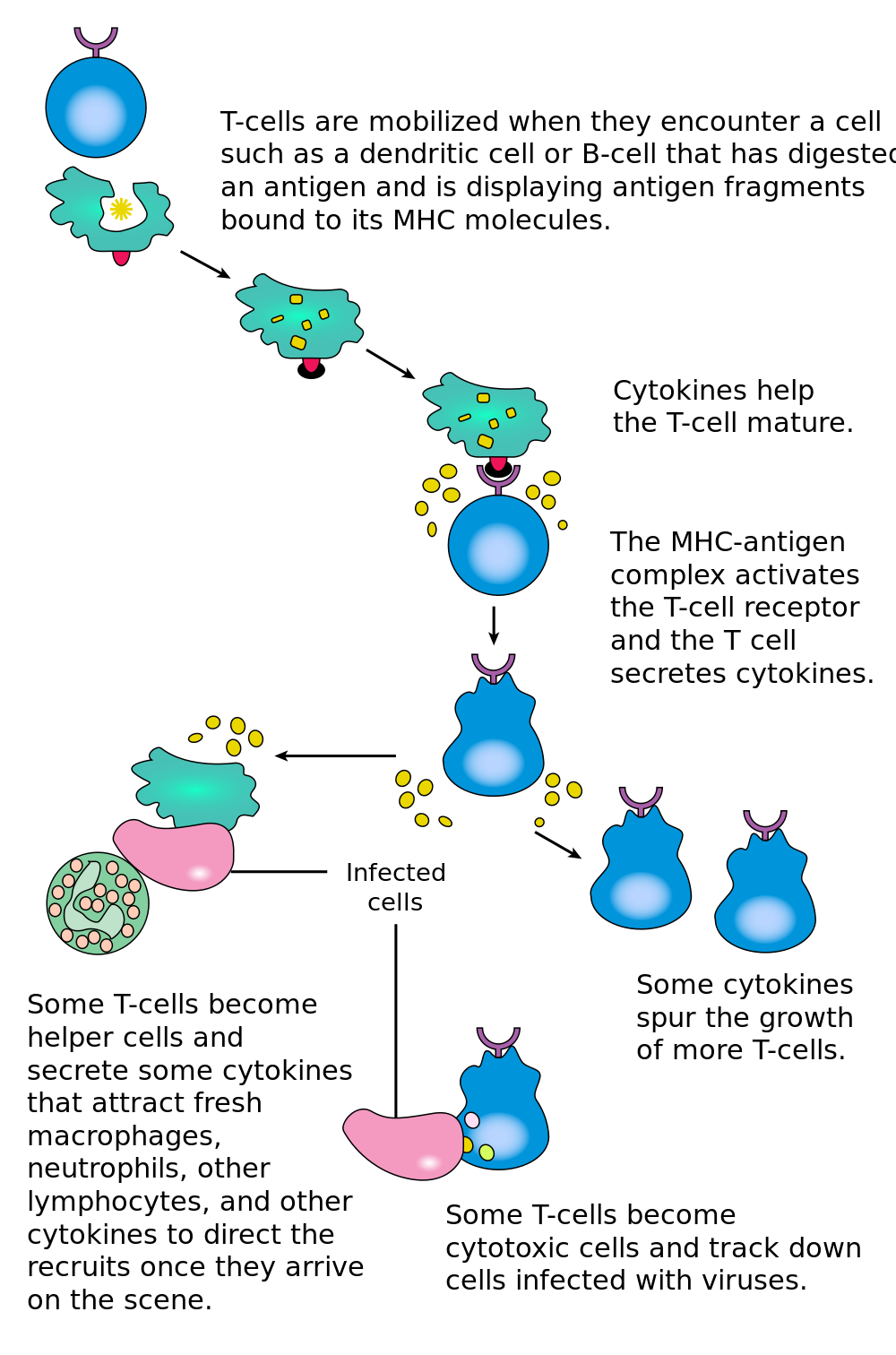
T cells must be activated to become either killer T cells or helper T cells. This requires presentation of a foreign antigen by antigen-presenting cells, as shown in Figure 17.5.2. Antigen-presenting cells may be dendritic cells, macrophages, or B cells. Activation occurs when T cells are presented with a foreign antigen coupled with an MHC self antigen. Helper T cells are more easily activated than killer T cells. Activation of killer T cells is strongly regulated and may require additional stimulation from helper T cells.
Killer T Cells
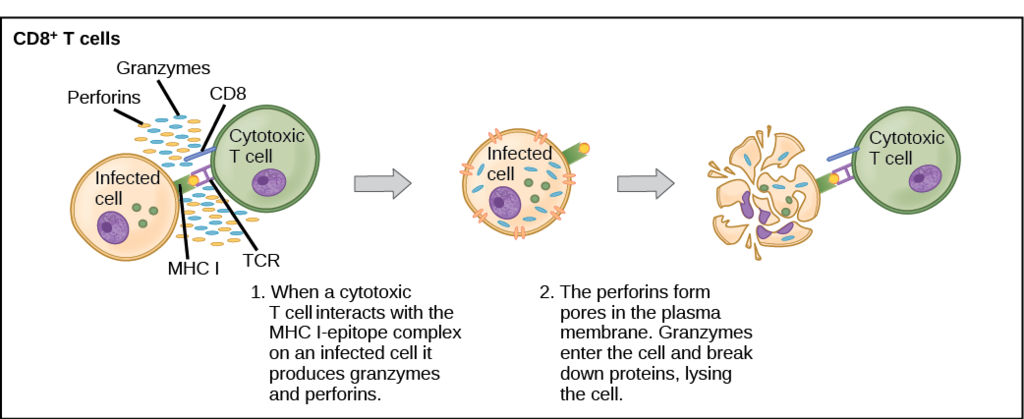
Activated killer T cells induce the death of cells that bear a specific non-self antigen because they are infected with pathogens or are cancerous. The antigen targets the cell for destruction by killer T cells, which travel through the bloodstream searching for target cells to kill. Killer T cells may use various mechanisms to kill target cells. One way is by releasing toxins in granules that enter and kill infected or cancerous cells (see Figure 17.5.3).
Helper T Cells
Activated helper T cells do not kill infected or cancerous cells. Instead, their role is to “manage” both innate and adaptive immune responses by directing other cells to perform these tasks. They control other cells by releasing cytokines, which are proteins that can influence the activity of many cell types, including killer T cells, B cells, and macrophages. Some cytokines released by helper T cells assist with the activation of killer T cells.
B Cells
B cells, or B lymphocytes, are the major cells involved in the creation of antibodies that circulate in blood plasma and lymph. Antibodies are large, Y-shaped proteins used by the immune system to identify and neutralize foreign invaders. Besides producing antibodies, B cells may also function as antigen-presenting cells, or secrete cytokines that help control other immune cells and responses.
B Cell Activation (or Antibody-Mediated Immunity)
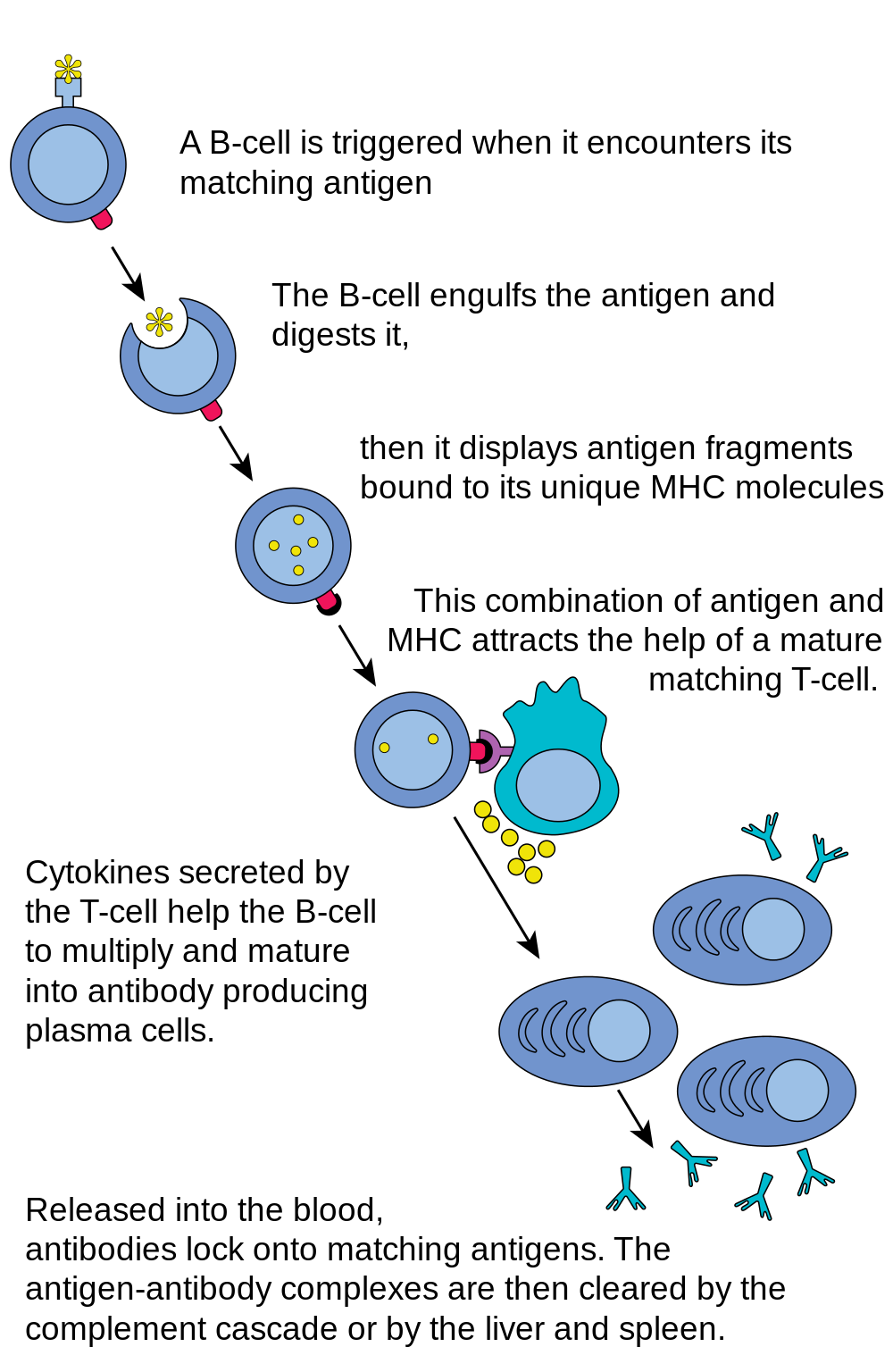
Before B cells can actively function to defend the host, they must be activated. As shown in Figure 17.5.4, B cell activation begins when a B cell engulfs and digests an antigen. The antigen may be either free floating in the lymph, or it may be presented by an antigen-presenting cell, such as a dendritic cell or macrophage. In either case, the B cell then displays antigen fragments bound to its own MHC antigens. The MHC-antigen complex on the B cell attracts helper T cells. The helper T cells, in turn, secrete cytokines that help the B cell to multiply, and the daughter cells to mature into plasma cells.
Plasma Cells
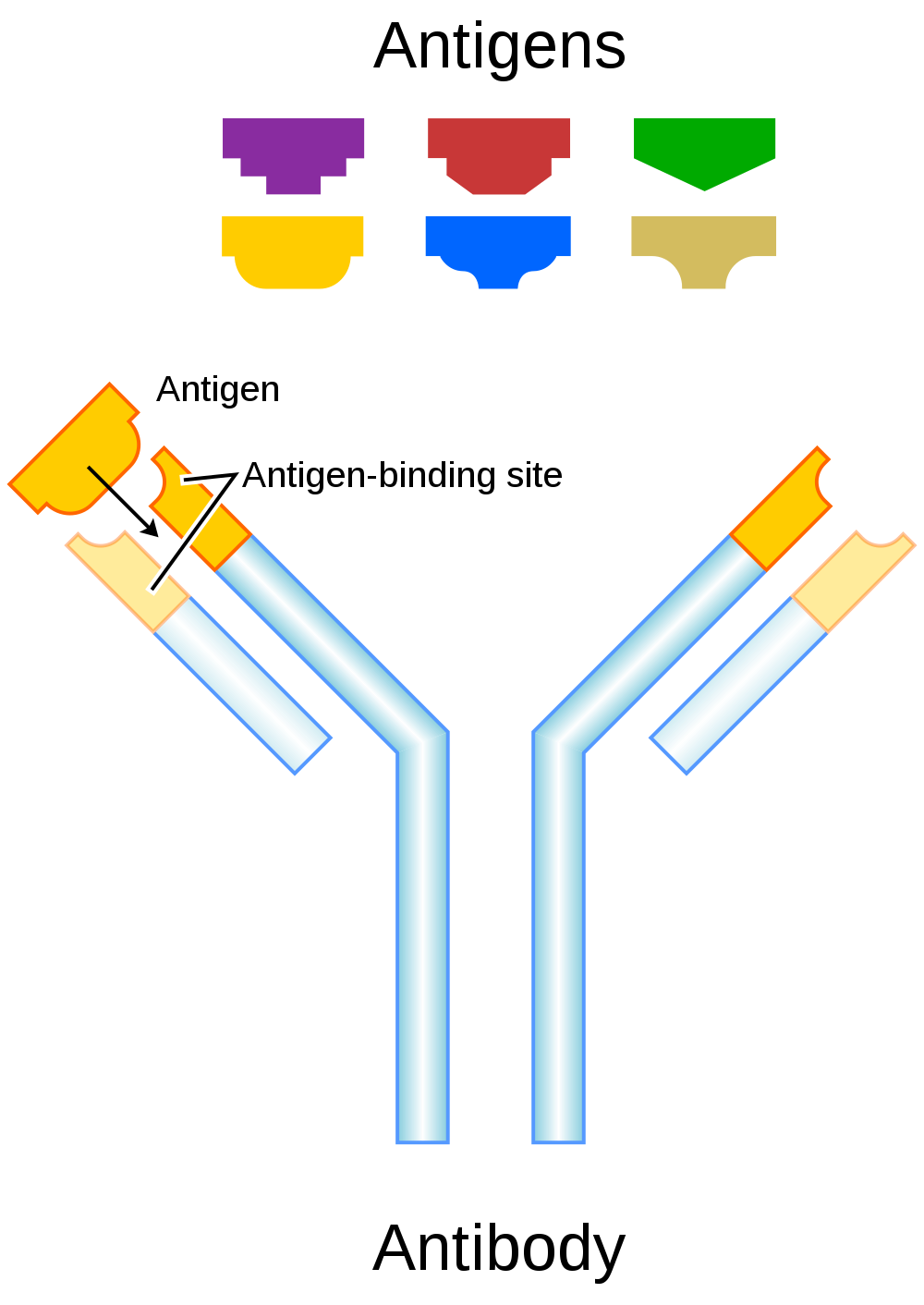
Plasma cells are antibody-secreting cells that form from activated B cells. Each plasma cell is like a tiny antibody factory. It may secrete millions of copies of an antibody, each of which can bind to the specific antigen that activated the original B cell. The specificity of an antibody to a specific antigen is illustrated in Figure 17.5.5. When antibodies bind with antigens, it makes the cells bearing them easier targets for phagocytes to find and destroy. Antibody-antigen complexes may also trigger the complement system of the innate immune system, which destroys the cells in a cascade of protein enzymes. In addition, the complexes are likely to clump together (agglutinate). If this occurs, they are filtered out of the blood in the spleen or liver.
Immunity
Once a pathogen has been cleared from the body, most activated T cells and B cells die within a few days. A few of the cells, however, survive and remain in the body as memory T cells or memory B cells. These memory cells are ready to activate an immediate response if they are exposed to the same antigen again in the future. This is the basis of immunity.
The earliest known reference to the concept of immunity relates to the bubonic plaque (see Figure 17.5.6). In 430 B.C., a Greek historian and general named Thucydides noted that people who had recovered from a previous bout of the plague could nurse people who were sick with the plague without contracting the illness a second time. We now know that this is true of many diseases, and that it occurs because of active immunity.

Active Immunity
Active immunity is the ability of the adaptive immune system to resist a specific pathogen because it has formed an immunological memory of the pathogen. Active immunity is adaptive, because it occurs during the lifetime of an individual as an adaptation to infection with a specific pathogen, and prepares the immune system for future challenges from that pathogen. Active immunity can come about naturally or artificially.
Naturally Acquired Active Immunity
Active immunity is acquired naturally when a pathogen invades the body and activates the adaptive immune system. When the initial infection is over, memory B cells and memory T cells remain, providing immunological memory of the pathogen. As long as the memory cells are alive, the immune system is ready to mount an immediate response if the same pathogen tries to infect the body again.
Artificially Acquired Active Immunity
Active immunity can also be acquired artificially through immunization. Immunization is the deliberate exposure of a person to a pathogen in order to provoke an adaptive immune response and the formation of memory cells specific to that pathogen. The pathogen is introduced in a vaccine — usually by injection, sometimes by nose or mouth (see Figure 17.5.7) — so immunization is also called vaccination.

Typically, only part of a pathogen, a weakened form of the pathogen, or a dead pathogen is used in a vaccine, which causes an adaptive immune response without making the immunized person sick. This is how you most likely became immune to diseases such as measles, mumps, and chicken pox. Immunizations may last for a lifetime, or they may require periodic booster shots to maintain immunity. While immunization generally has long-lasting effects, it usually takes several weeks to develop full immunity.
Immunization is the most effective method ever discovered of preventing infectious diseases. As many as 3 million deaths are prevented each year because of vaccinations. Widespread immunity from vaccinations is largely responsible for the worldwide eradication of smallpox, and the near elimination of several other infectious diseases from many populations, including polio and measles. Immunization is so successful because it exploits the natural specificity and inducibility of the adaptive immune system.
Passive Immunity
Passive immunity results when pathogen-specific antibodies or activated T cells are transferred to a person who has never been exposed to the pathogen. Passive immunity provides immediate protection from a pathogen, but the adaptive immune system does not develop immunological memory to protect the host from the same pathogen in the future. Unlike active immunity, passive immunity lasts only as long as the transferred antibodies or T cells survive in the blood — usually between a few days and a few months. However, like active immunity, passive immunity can be acquired both naturally and artificially.
Naturally Acquired Passive Immunity
Passive immunity is acquired naturally by a fetus through its mother’s blood. Antibodies are transported from mother to fetus across the placenta, so babies have high levels of antibodies at birth. Their antibodies have the same range of antigen specificities as their mother’s. Passive immunity may also be acquired by an infant through the mother’s breast milk. This gives young infants protection from common pathogens in their environment while their own immune system matures.
Artificially Acquired Passive Immunity
Older children and adults can acquire passive immunity artificially through the injection of antibodies or activated T cells, which may be done when there is a high risk of infection and insufficient time for the body to develop active immunity through vaccination. It may also be done to reduce symptoms of ongoing disease, or to compensate for immunodeficiency diseases.
Adaptive Immune Evasion
Many pathogens have been around for a long time, living with human populations for generations. To persist, some have evolved mechanisms to evade the adaptive immune system of human hosts. One way they have done this is by rapidly changing their non-essential antigens. This is called antigenic variation. An example of a pathogen that takes this approach is human immunodeficiency virus (HIV). It mutates rapidly so the proteins on its viral envelope are constantly changing. By the time the adaptive immune system responds, the virus’s antigens have changed. Antigenic variation is the main reason that efforts to develop a vaccine against HIV have not yet been successful.
Another evasion approach that some pathogens may take is to mask pathogen antigens with host molecules so the host’s immune system cannot detect the antigens. HIV takes this approach, as well. The envelope that covers the virus is formed from the outermost membrane of the host cell.
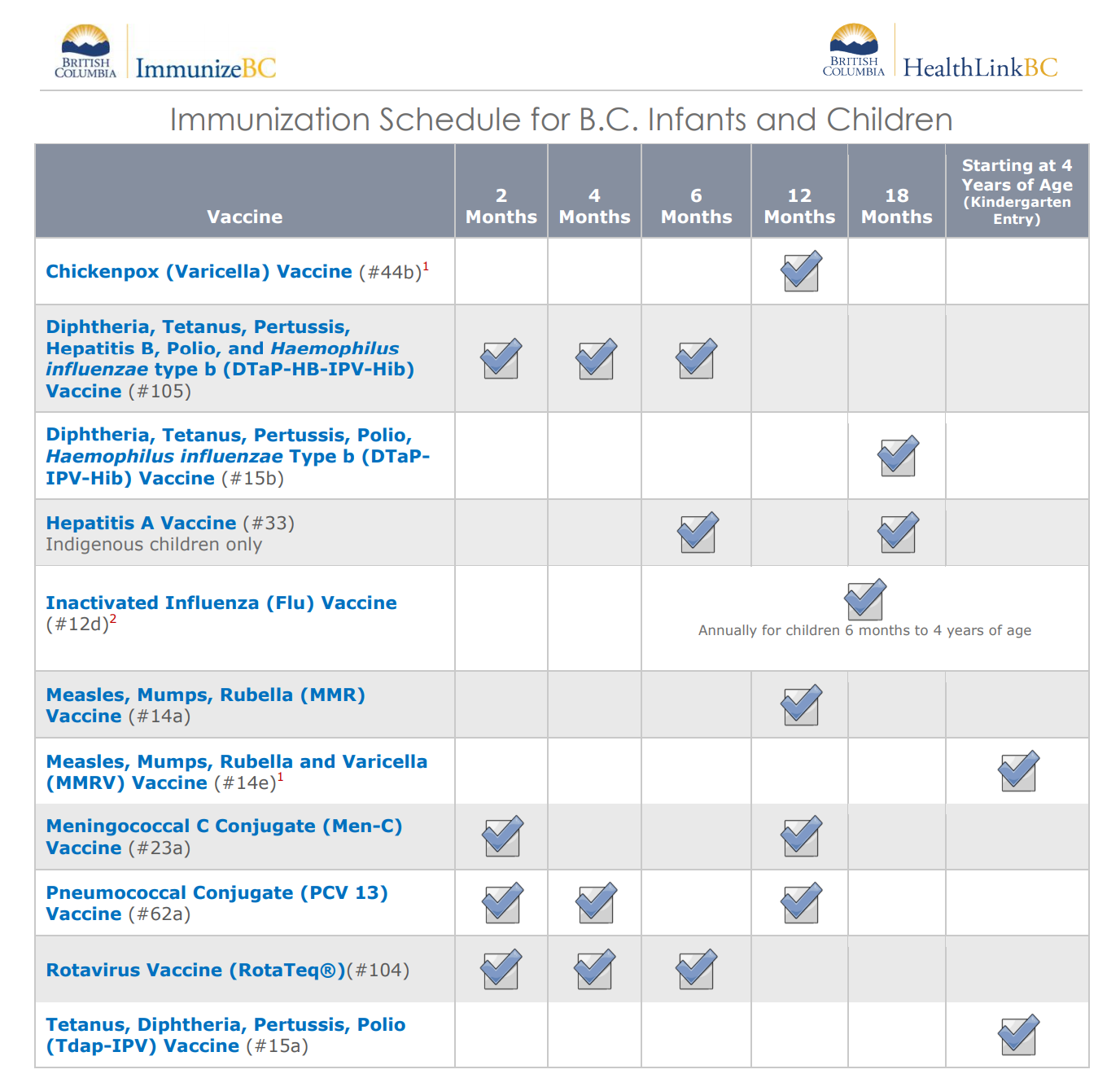
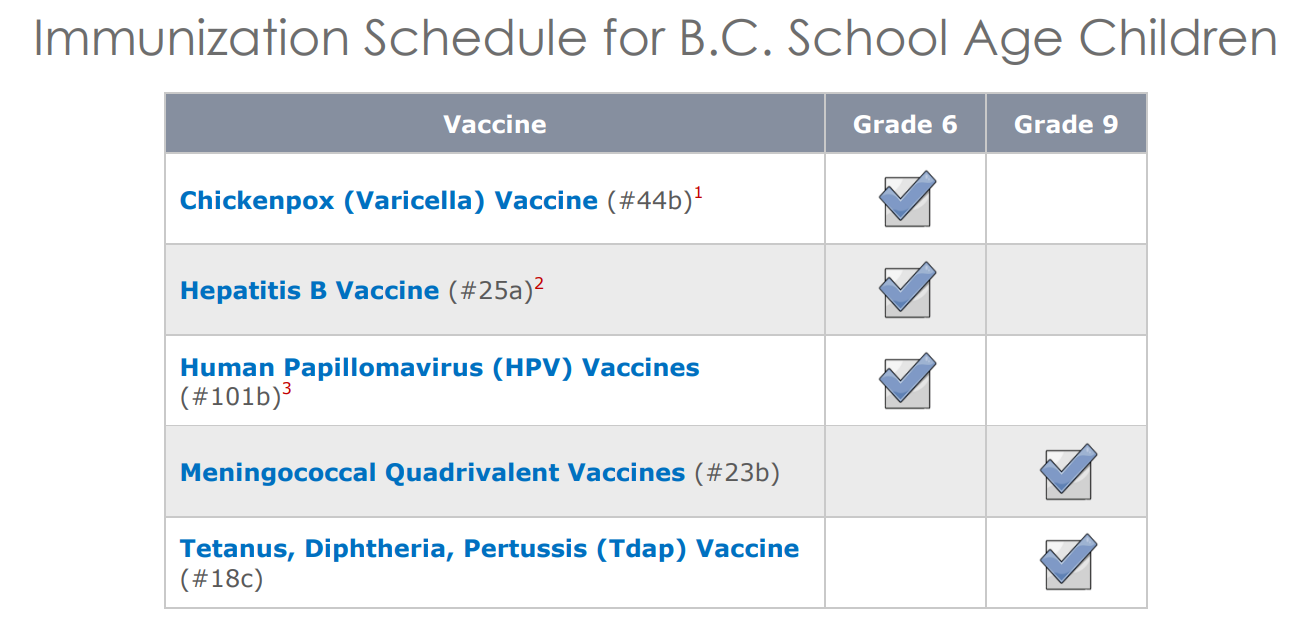
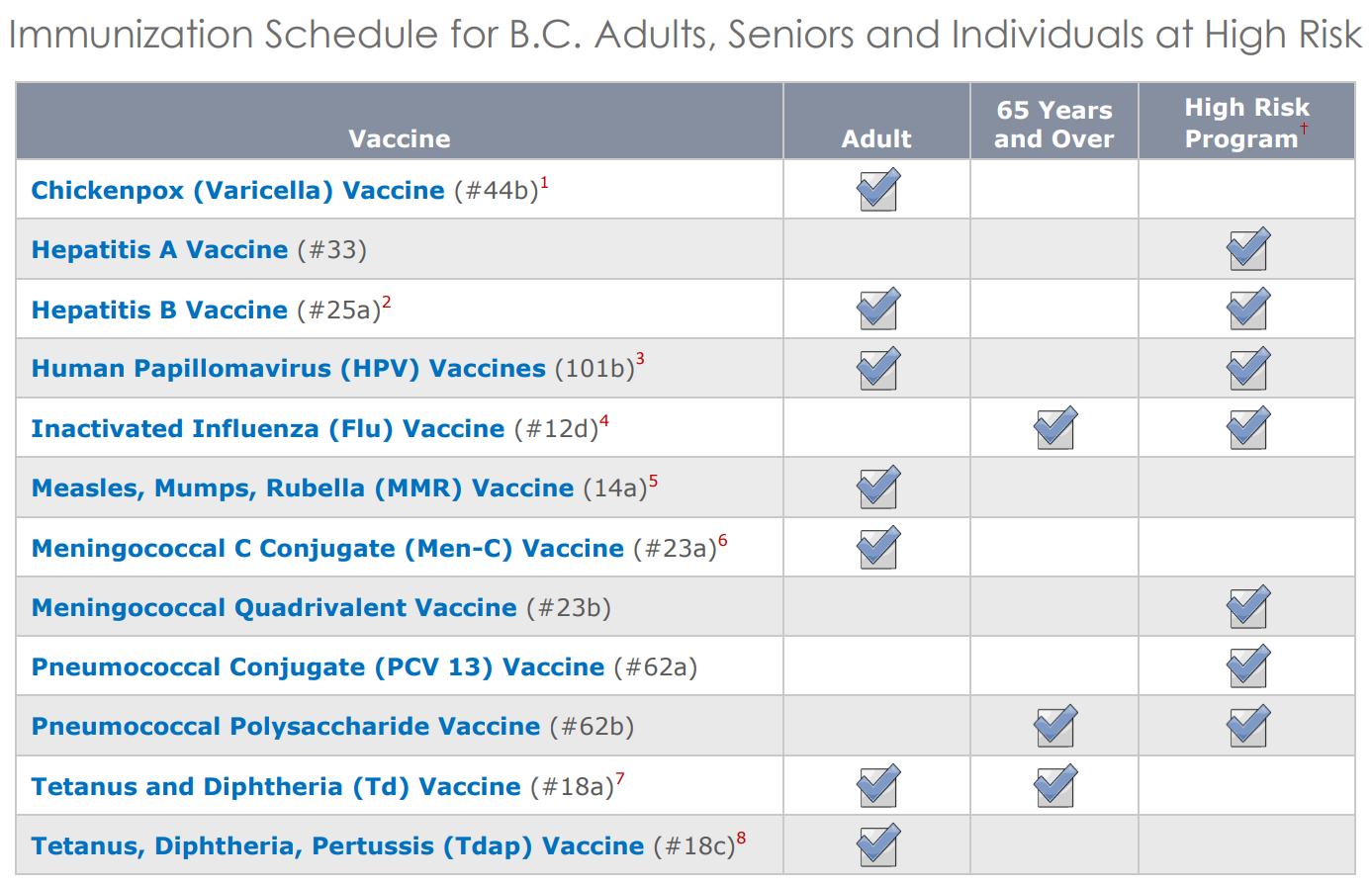
Feature: My Human Body
If you think that immunizations are just for kids, think again. There are several vaccines recommended by HealthLinkBC for people over the age of 18. The tables below from HealthLinkBC show the vaccine schedules recommended for infants and children, school-aged children, and adults and senior. Additional vaccines may be recommended for certain adults based on specific travel plans, medical conditions or other indications. Are you up to date with your vaccines? You can check with your doctor to be sure.
17.5 Summary
- The adaptive immune system is a subsystem of the overall immune system that recognizes and makes a tailored attack against specific pathogens or tumor cells. It is a slower, but more effective response than the innate immune response, and also leads to immunity to particular pathogens.
- Lymphocytes produced by the lymphatic system are the main cells of the adaptive immune system. There are two major types of lymphocytes: T cells and B cells. Both types must be activated by foreign antigens to become functioning immune cells.
- Most activated T cells become either killer T cells or helper T cells. Killer T cells destroy cells that are infected with pathogens or are cancerous. Helper T cells manage immune responses by releasing cytokines that control other types of leukocytes.
- Activated B cells form plasma cells that secrete antibodies, which bind to specific antigens on pathogens or infected cells. The antibody-antigen complexes generally lead to the destruction of the cells, for example, by attracting phagocytes or triggering the complement system.
- After an adaptive immune response occurs, long-lasting memory B cells and memory T cells may remain to confer immunity to the specific pathogen that caused the adaptive immune response. These memory cells are ready to activate an immediate response if they are exposed to the same antigen again in the future.
- Immunity may be active or passive. Active immunity occurs when the immune system has been presented with antigens that elicit an adaptive immune response. This may occur naturally as the result of an infection, or artificially as the result of immunization. Active immunity may last for years or even for life.
- Passive immunity occurs without an adaptive immune response by the transfer of antibodies or activated T cells. This may occur naturally between a mother and her fetus or her nursing infant, or it may occur artificially by injection. Passive immunity lasts only as long as the antibodies or activated T cells remain alive in the body, generally just weeks or months.
- Many pathogens have evolved mechanisms to evade the adaptive immune system. For example, human immunodeficiency virus (HIV) evades the adaptive immune system by frequently changing its antigens and by forming its outer envelope from the host’s cell membrane.
17.5 Review Questions
- What is the adaptive immune system?
- Define immunity.
-
- How are lymphocytes activated?
- Identify two common types of T cells and their functions.
- How do activated B cells help defend against pathogens?
- How does passive immunity differ from active immunity? How may passive immunity occur?
- What are two ways that active immunity may come about?
- What ways of evading the human adaptive immune system evolved in human immunodeficiency virus (HIV)?
- Why do vaccinations expose a person to a version of a pathogen?
17.5 Explore More
How do vaccines work? - Kelwalin Dhanasarnsombut, TED-Ed, 2015.
How we conquered the deadly smallpox virus - Simona Zompi, TED-Ed, 2013.
Why Do We Need A New Flu Shot Every Year? Seeker, 2015.
An HIV Vaccine: Mapping Uncharted Territory, NIAID, 2016.
Attributions
Figure 17.5.1
Killer_T_cells_surround_a_cancer_cell by Alex Ritter, Jennifer Lippincott Schwartz and Gillian Griffiths at the National Institutes of Health/ Visuals Online on Wikimedia Commons is in the public domain (https://en.wikipedia.org/wiki/Public_domain).
Figure 17.5.2
T_cell_activation.svg by Rehua (derivative work) on Wikimedia Commons is in the public domain (https://en.wikipedia.org/wiki/Public_domain). (Original image: T_cell_activation.png: from The Immune System - NIH Publication No. 03–5423)
Figure 17.5.3
Cytotoxic T Cell function by CNX OpenStax on Wikimedia Commons is used under a CC BY 4.0 (https://creativecommons.org/licenses/by/4.0) license.
Figure 17.5.4
B_cell_activation.svg by Fred the Oyster on Wikimedia Commons is in the public domain (https://en.wikipedia.org/wiki/Public_domain). (Original from The Immune System - NIH Publication No. 03–5423)
Figure 17.5.5
Antibody.svg by Fvasconcellos on Wikimedia Commons is in the public domain (https://en.wikipedia.org/wiki/Public_domain). (Original black and white image from the National Human Genome Research Institute's Talking Genetics Glossary)
Figure 17.5.7
immunizations by U.S. Air Force photo by Airman 1st Class Destinee Dougherty from Military Health System website, Health.mil, is in the public domain (https://en.wikipedia.org/wiki/Public_domain).
References
HealthLinkBC. (2018). B.C. immunization schedules. Gov.BC.CA. https://www.healthlinkbc.ca/tools-videos/bc-immunization-schedules
Mayo Clinic Staff. (n.d.). Measles [online article]. MayoClinic.org. https://www.mayoclinic.org/diseases-conditions/measles/symptoms-causes/syc-20374857
Mayo Clinic Staff. (n.d.). Mumps [online article]. MayoClinic.org. https://www.mayoclinic.org/diseases-conditions/mumps/symptoms-causes/syc-20375361
Mayo Clinic Staff. (n.d.). Polio [online article]. MayoClinic.org. https://www.mayoclinic.org/diseases-conditions/polio/symptoms-causes/syc-20376512
Mayo Clinic Staff. (n.d.). Smallpox [online article]. MayoClinic.org. https://www.mayoclinic.org/diseases-conditions/smallpox/symptoms-causes/syc-20353027
NIAID. (2016, August 11). An HIV vaccine: Mapping uncharted territory. YouTube. https://www.youtube.com/watch?v=X-rC78MKZvw&feature=youtu.be
OpenStax. (2016, March 23). Figure 4 Naïve CD4+ T cells engage MHC II molecules on antigen-presenting cells (APCs) and become activated. Clones of the activated helper T cell, in turn, activate B cells and CD8+ T cells, which become cytotoxic T cells. Cytotoxic T cells kill infected cells [digital image]. In OpenStax, Biology (Section 42.2). OpenStax CNX. https://cnx.org/contents/GFy_h8cu@10.53:etZobsU-@6/Adaptive-Immune-Response
Seeker. (2015, September 2). Why do we need a new flu shot every year? YouTube. https://www.youtube.com/watch?v=5THf6gTNqO8
TED-Ed. (2015, January 12). How do vaccines work? - Kelwalin Dhanasarnsombut. YouTube. https://www.youtube.com/watch?v=rb7TVW77ZCs&feature=youtu.be
TED-Ed. (2013, October 28). How we conquered the deadly smallpox virus - Simona Zompi. YouTube. https://www.youtube.com/watch?v=yqUFy-t4MlQ&feature=youtu.be
A group of diseases involving abnormal cell growth with the potential to invade or spread to other parts of the body.
A structure within a cell, consisting of lipid bilayer. Vesicles form naturally during the processes of secretion, uptake and transport of materials within the plasma membrane.

Pills from Pee
The medication pictured in Figure 9.3.1 with the brand name Progynon was a drug used to control the effects of menopause in women. The pills first appeared in 1928 and contained the human sex hormone estrogen. Estrogen secretion declines in women around the time of menopause and may cause symptoms like mood swings and hot flashes. The pills were supposed to ease the symptoms by supplementing estrogen in the body. The manufacturer of Progynon obtained estrogen for the pills from the urine of pregnant women, because it was a cheap source of the hormone. Progynon is still used today to treat menopausal symptoms. Although the drug has been improved over the years, it still contains estrogen, which is an example of an endocrine hormone.
How Do Endocrine Hormones Work?
Endocrine hormones like estrogen are messenger molecules secreted by endocrine glands into the bloodstream. They travel throughout the body in the circulation. Although they reach virtually every cell in the body in this way, each hormone affects only certain cells, called target cells. A target cell is the type of cell on which a hormone has an effect. A target cell is affected by a particular hormone because it has receptor proteins — either on the cell surface or within the cell — that are specific to that hormone. An endocrine hormone travels through the bloodstream until it finds a target cell with a matching receptor to which it can bind. When the hormone binds to the receptor, it causes changes within the cell. The manner in which it changes the cell depends on whether the hormone is a steroid hormone or a non-steroid hormone.
Steroid Hormones
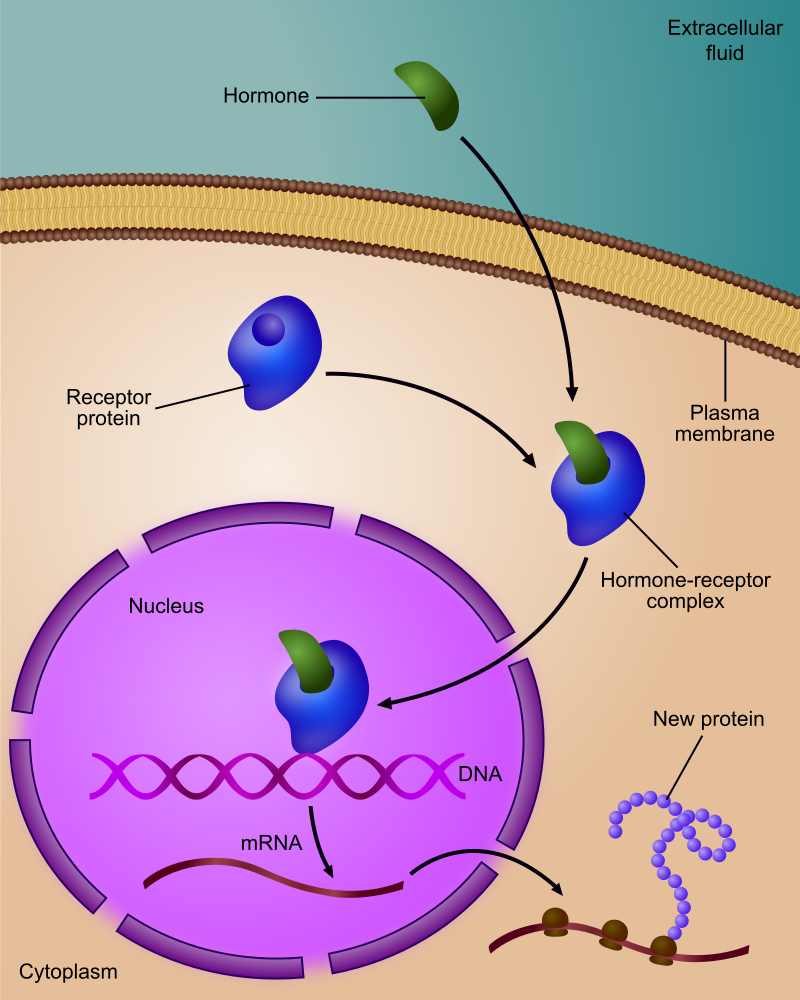
A steroid hormone (such as estrogen) is made of lipids. It is fat soluble, so it can diffuse across a target cell’s plasma membrane, which is also made of lipids. Once inside the cell, a steroid hormone binds with receptor proteins in the cytoplasm. As you can see in Figure 9.3.2, the steroid hormone and its receptor form a complex — called a steroid complex — which moves into the nucleus, where it influences the expression of genes. Examples of steroid hormones include cortisol, which is secreted by the adrenal glands, and sex hormones, which are secreted by the gonads.
Non-Steroid Hormones
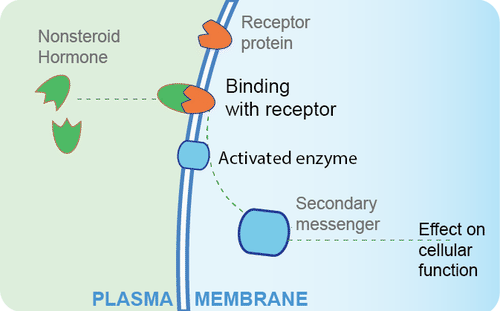
A non-steroid hormoneis made of amino acids. It is not fat soluble, so it cannot diffuse across the plasma membrane of a target cell. Instead, it binds to a receptor protein on the cell membrane. In the Figure 9.3.3 diagram, you can see that the binding of the hormone with the receptor activates an enzyme in the cell membrane. The enzyme then stimulates another molecule, called the second messenger, which influences processes inside the cell. Most endocrine hormones are non-steroid hormones. Examples include glucagon and insulin, both produced by the pancreas.
Regulation of Endocrine Hormones
Endocrine hormones regulate many body processes, but what regulates the secretion of endocrine hormones? Most endocrine hormones are controlled by feedback mechanisms. A feedback mechanism is a loop in which a product feeds back to control its own production. Feedback loops may be either negative or positive.
- Most endocrine hormones are regulated by negative feedback loops. Negative feedback keeps the concentration of a hormone within a relatively narrow range, and maintains homeostasis.
- Very few endocrine hormones are regulated by positive feedback loops. Positive feedback causes the concentration of a hormone to become increasingly higher.
Regulation by Negative Feedback
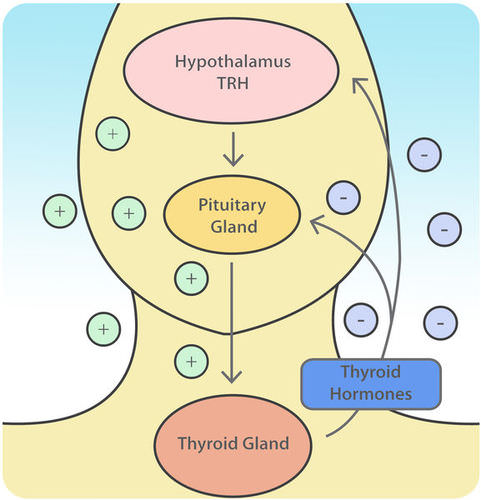
A negative feedback loop controls the synthesis and secretion of hormones by the thyroid gland. This loop includes the hypothalamus and pituitary gland, in addition to the thyroid, as shown in the diagram (Figure 9.3.4). When the levels of thyroid hormones circulating in the blood fall too low, the hypothalamus secretes thyrotropin releasing hormone (TRH). This hormone travels directly to the pituitary gland through the thin stalk connecting the two structures. In the pituitary gland, TRH stimulates the pituitary to secrete thyroid stimulating hormone (TSH). TSH, in turn, travels through the bloodstream to the thyroid gland, and stimulates it to secrete thyroid hormones. This continues until the blood levels of thyroid hormones are high enough. At that point, the thyroid hormones feed back to stop the hypothalamus from secreting TRH and the pituitary from secreting TSH. Without the stimulation of TSH, the thyroid gland stops secreting its hormones. Eventually, the levels of thyroid hormones in the blood start to fall too low again. When that happens, the hypothalamus releases TRH, and the loop repeats.
Regulation by Positive Feedback
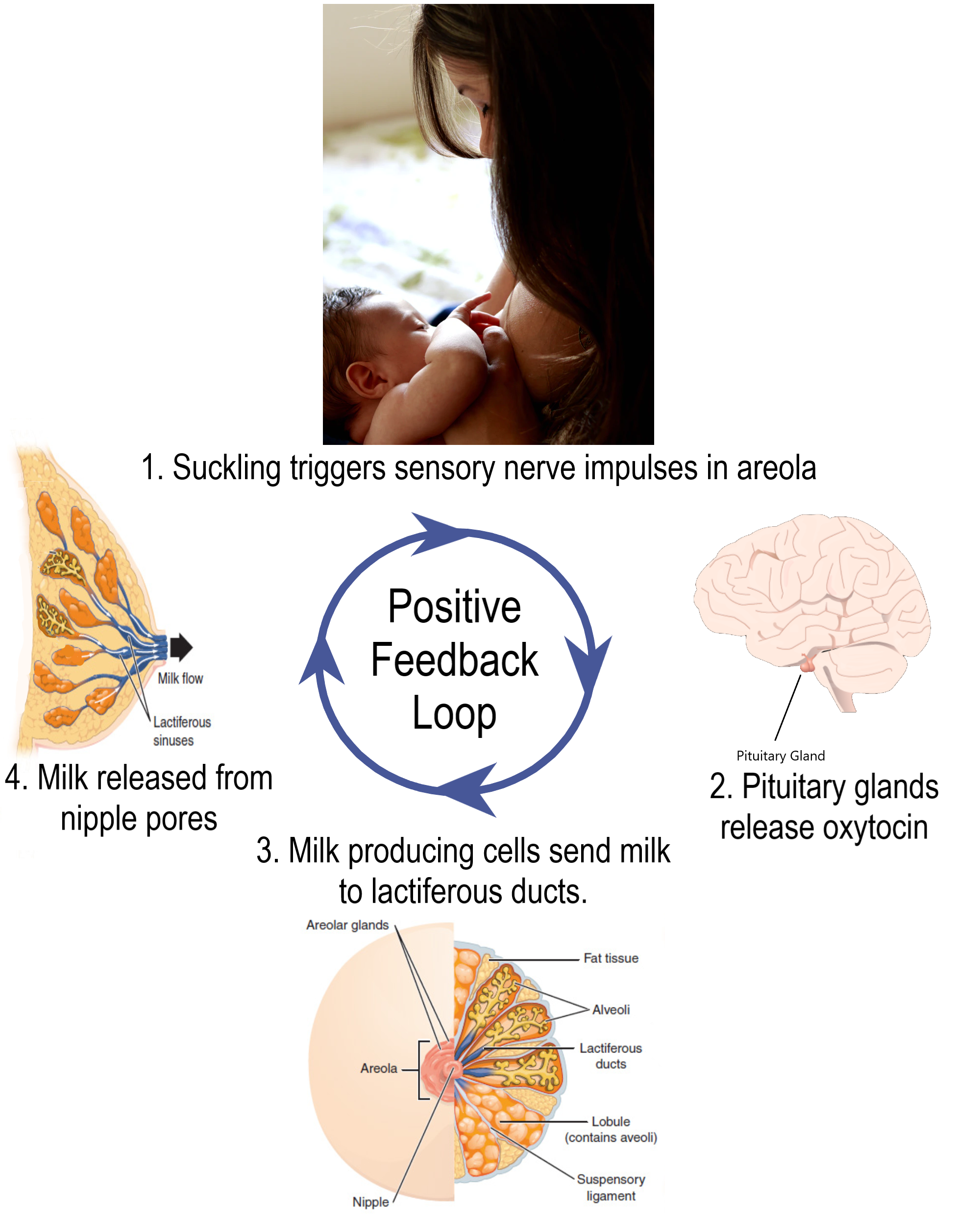
Prolactin is a non-steroid endocrine hormone secreted by the pituitary gland. One of the functions of prolactin is to stimulate a nursing mother’s mammary glands to produce milk. The regulation of prolactin in the mother is controlled by a positive feedback loop that involves the nipples, hypothalamus, pituitary gland, and mammary glands. Positive feedback begins when a baby suckles on the mother’s nipple. Nerve impulses from the nipple reach the hypothalamus, which stimulates the pituitary gland to secrete prolactin. Prolactin travels in the blood to the mammary glands and stimulates them to produce milk. The release of milk causes the baby to continue suckling, which causes more prolactin to be secreted and more milk to be produced. The positive feedback loop continues until the baby stops suckling at the breast.
Feature: Myth vs. Reality
Anabolic steroids are synthetic versions of the naturally occurring male sex hormone testosterone. Male hormones have androgenic (or masculinizing) effects, but they also have anabolic (or muscle-building) effects. The anabolic effects are the reason that synthetic steroids are used by athletes. In addition to building muscles, they also accelerate the development of bones and red blood cells, increase endurance so athletes can train harder and longer, and speed up muscle recovery. Unfortunately, these benefits of steroid use come with costs. If you ever consider taking anabolic steroids to build muscles and improve athletic performance, consider the following myths and corresponding realities.
Myth |
Reality |
| "Steroids are safe." | Steroid use may cause several serious side effects. Prolonged use may increase the risk of liver cancer, heart disease, and high blood pressure. |
| "Steroids will not stunt your growth." | Teens who take steroids before they have finished growing in height may have their growth stunted so they remain shorter throughout life than they would otherwise have been. Such stunting occurs because steroids increase the rate at which skeletal maturity is reached. Once skeletal maturity occurs, additional growth in height is impossible. |
| "Steroids do not cause drug dependency." | Steroid use may cause dependency, as evidenced by the negative effects of stopping steroid use. These negative effects may include insomnia, fatigue, and depressed mood, among others. |
| "There is no such thing as 'roid rage.'" | Steroid use has been shown to increase aggressiveness in some people. It has also been implicated in a number of violent acts committed by people who had not demonstrated violent tendencies until they started using steroids. |
| "Only males use steroids." | Although steroid use is more common in males than females, some females also use steroids. They use them to build muscle and improve physical performance, generally either for athletic competition or for self-defense. |
9.3 Summary
- Endocrine hormones are messenger molecules secreted by endocrine glands into the bloodstream. They travel throughout the body but affect only certain cells, called target cells, which have receptors specific to particular hormones.
- Steroid hormones such as estrogen are endocrine hormones made of lipids that cross plasma membranes and bind to receptors inside target cells. The hormone-receptor complexes then move into the nucleus, where they influence gene expression.
- Non-steroid hormones (such as insulin) are endocrine hormones made of amino acids that bind to receptors on the surface of target cells. This activates an enzyme in the plasma membrane, and the enzyme controls a second messenger molecule, which influences cell processes.
- Most endocrine hormones are controlled by negative feedback loops in which rising levels of a hormone feed back to stop its own production — and vice-versa. For example, a negative feedback loop controls production of thyroid hormones. The loop includes the hypothalamus, pituitary gland, and thyroid gland.
- Only a few endocrine hormones are controlled by positive feedback loops, in which rising levels of a hormone feed back to stimulate continued production of the hormone. Prolactin, the pituitary hormone that stimulates milk production by mammary glands, is controlled by a positive feedback loop. The loop includes the nipples, hypothalamus, pituitary gland, and mammary glands.
9.3 Review Questions
-
-
- Explain how steroid hormones influence target cells.
- How do non-steroid hormones affect target cells?
- Compare and contrast negative and positive feedback loops.
- Outline the way feedback controls the production of thyroid hormones.
- Describe the feedback mechanism that controls milk production by the mammary glands.
- People with a condition called hyperthyroidism produce too much thyroid hormone. What do you think this does to the level of TSH? Explain your answer.
- Which is more likely to maintain homeostasis— negative feedback or positive feedback? Explain your answer.
- Does testosterone bind to receptors on the plasma membrane of target cells or in the cytoplasm of target cells? Explain your answer.
9.3 Explore More
https://www.youtube.com/watch?v=WVrlHH14q3o&feature=emb_logo
Great Glands - Your Endocrine System: CrashCourse Biology #33, CrashCourse, 2012.
https://www.youtube.com/watch?v=qXaDDa3FB5Q&feature=emb_logo
National Geographic | Benefits and Side Effects of Steroids Use 2015, 24 Physic.
Attributions
Figure 9.3.1
L0058274 Glass bottle for ‘Progynon’ pills, United Kingdom, 1928-1948 by Wellcome Collection gallery (2018-03-29)/ Science Museum, London on Wikimedia Commons is used under a CC-BY-4.0 (https://creativecommons.org/licenses/by/4.0/) license.
Figure 9.3.2
Regulation_of_gene_expression_by_steroid_hormone_receptor.svg by Ali Zifan on Wikimedia Commons is used under a CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0/deed.en) license.
Figure 9.3.3
Non-steroid hormone pathway by CK-12 Foundation, Biology for High School is used under a CC BY-NC 3.0 (https://creativecommons.org/licenses/by-nc/3.0/) license.
Figure 9.3.4
Thyroid Negative Feedback Loop by CK-12 Foundation, College Human Biology is used under a CC BY-NC 3.0 (https://creativecommons.org/licenses/by-nc/3.0/) license.
 ©CK-12 Foundation Licensed under
©CK-12 Foundation Licensed under ![]() • Terms of Use • Attribution
• Terms of Use • Attribution
Figure 9.3.5
Lactation Positive Feedback Loop by Christinelmiller on Wikimedia Commons is used under a CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0/deed.en) license.
References
24 Physic. (2015,July 19). National Geographic | Benefits and side effects of steroids use 2015. YouTube. https://www.youtube.com/watch?v=qXaDDa3FB5Q&feature=youtu.be
Brainard, J/ CK-12 Foundation. (2016, August 15). Figure 4 Thyroid negative feedback loop [digital image]. In CK-12 College Human Biology (Section 11.3 Endocrine hormones). CK12.org. https://www.ck12.org/book/ck-12-human-biology/section/11.3/
CK-12 Foundation. (2019, March 5). Figure 3 A non-steroid hormone binds with a receptor on the plasma membrane of a target cell [digital image]. In Flexbook 2.0: CK-12 Biology For High School (Section 13.21 Hormone). CK12. https://flexbooks.ck12.org/cbook/ck-12-biology-flexbook-2.0/section/13.21/primary/lesson/hormones-bio
CrashCourse. (2012, September 10). Great glands - Your endocrine system: CrashCourse Biology #33. YouTube. https://www.youtube.com/watch?v=WVrlHH14q3o&feature=youtu.be
TED-Ed. (2018, June 21). How do your hormones work? - Emma Bryce. YouTube. https://www.youtube.com/watch?v=-SPRPkLoKp8&feature=youtu.be
A microorganism which causes disease.
The process by which information from a gene is used in the synthesis of a functional protein.
Image shows a photograph of a cotton-top tamarin monkey, which displays the straight hair characteristic of non-human primates.
Image shows a diagram of the hormones secreted by the thyroid gland, and how it is both controlled by and acting upon in a negative feedback the hypothalamus and the anterior pituitary gland.
a colorless cell that circulates in the blood and body fluids and is involved in counteracting foreign substances and disease; a white (blood) cell. There are several types, all amoeboid cells with a nucleus, including lymphocytes, granulocytes, monocytes, and macrophages.
Created by CK-12 Foundation/Adapted by Christine Miller

Steady as She Goes
This device (Figure 7.8.1) looks simple, but it controls a complex system that keeps a home at a steady temperature — it's a thermostat. The device shows the current temperature in the room, and also allows the occupant to set the thermostat to the desired temperature. A thermostat is a commonly cited model of how living systems — including the human body— maintain a steady state called homeostasis.
What Is Homeostasis?
Homeostasis is the condition in which a system (such as the human body) is maintained in a more or less steady state. It is the job of cells, tissues, organs, and organ systems throughout the body to maintain many different variables within narrow ranges compatible with life. Keeping a stable internal environment requires continually monitoring the internal environment and constantly making adjustments to keep things in balance.
Set Point and Normal Range
For any given variable, such as body temperature or blood glucose level, there is a particular set point that is the physiological optimum value. The set point for human body temperature, for example, is about 37 degrees C (98.6 degrees F). As the body works to maintain homeostasis for temperature or any other internal variable, the value typically fluctuates around the set point. Such fluctuations are normal, as long as they do not become too extreme. The spread of values within which such fluctuations are considered insignificant is called the normal range. In the case of body temperature, for example, the normal range for an adult is about 36.5 to 37.5 degrees C (97.7 to 99.5 degrees F).
A good analogy for set point, normal range, and maintenance of homeostasis is driving. When you are driving a vehicle on the road, you are supposed to drive in the centre of your lane — this is analogous to the set point. Sometimes, you are not driving in the exact centre of the lane, but you are still within your lines, so you are in the equivalent of the normal range. However, if you were to get too close to the centre line or the shoulder of the road, you would take action to correct your position. You'd move left if you were too close to the shoulder, or right if too close to the centre line — which is analogous to our next concept, negative feedback to maintain homeostasis.
Maintaining Homeostasis
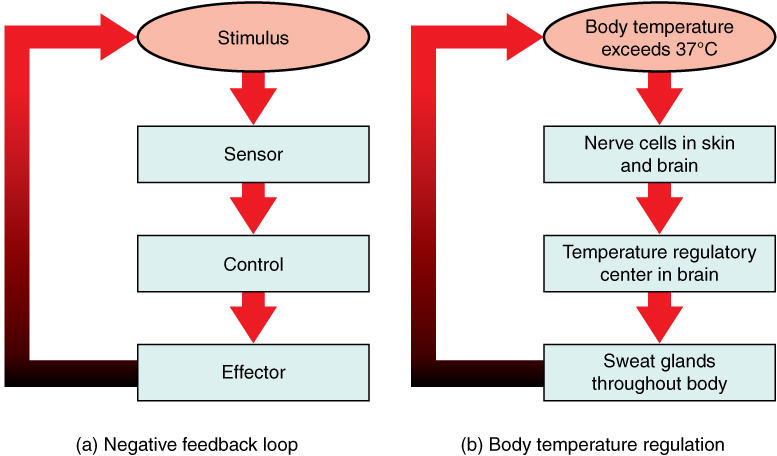
Homeostasis is normally maintained in the human body by an extremely complex balancing act. Regardless of the variable being kept within its normal range, maintaining homeostasis requires at least four interacting components: stimulus, sensor, control centre, and effector.
- The stimulus is provided by the variable being regulated. Generally, the stimulus indicates that the value of the variable has moved away from the set point or has left the normal range.
- The sensor monitors the values of the variable and sends data on it to the control centre.
- The control centre matches the data with normal values. If the value is not at the set point or is outside the normal range, the control centre sends a signal to the effector.
- The effector is an organ, gland, muscle, or other structure that acts on the signal from the control centre to move the variable back toward the set point.
Each of these components is illustrated in Figure 7.8.2. The diagram on the left is a general model showing how the components interact to maintain homeostasis. The diagram on the right shows the example of body temperature. From the diagrams, you can see that maintaining homeostasis involves feedback, which is data that feeds back to control a response. Feedback may be negative (as in the example below) or positive. All the feedback mechanisms that maintain homeostasis use negative feedback. Biological examples of positive feedback are much less common.
Negative Feedback
In a negative feedback loop, feedback serves to reduce an excessive response and keep a variable within the normal range. Two processes controlled by negative feedback are body temperature regulation and control of blood glucose.
Body Temperature
Body temperature regulation involves negative feedback, whether it lowers the temperature or raises it, as shown in Figure 7.8.3 and explained in the text that follows.
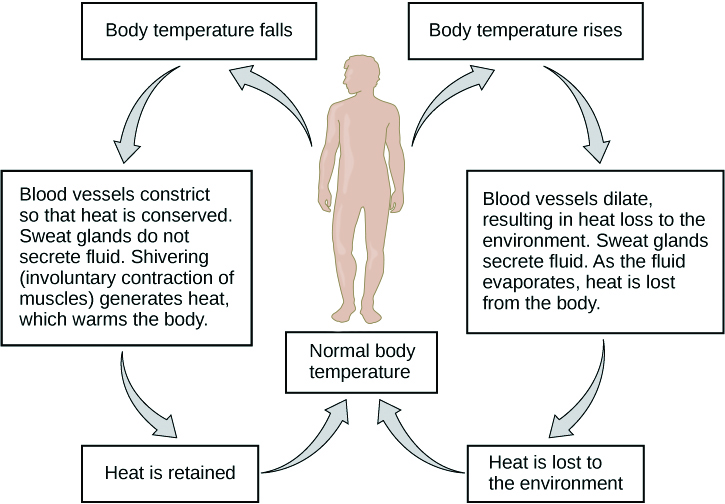
Cooling Down
The human body’s temperature regulatory centre is the hypothalamus in the brain. When the hypothalamus receives data from sensors in the skin and brain that body temperature is higher than the set point, it sets into motion the following responses:
- Blood vessels in the skin dilate (vasodilation) to allow more blood from the warm body core to flow close to the surface of the body, so heat can be radiated into the environment.
- As blood flow to the skin increases, sweat glands in the skin are activated to increase their output of sweat (diaphoresis). When the sweat evaporates from the skin surface into the surrounding air, it takes heat with it.
- Breathing becomes deeper, and the person may breathe through the mouth instead of the nasal passages. This increases heat loss from the lungs.
Heating Up
When the brain’s temperature regulatory centre receives data that body temperature is lower than the set point, it sets into motion the following responses:
- Blood vessels in the skin contract (vasoconstriction) to prevent blood from flowing close to the surface of the body, which reduces heat loss from the surface.
- As temperature falls lower, random signals to skeletal muscles are triggered, causing them to contract. This causes shivering, which generates a small amount of heat.
- The thyroid gland may be stimulated by the brain (via the pituitary gland) to secrete more thyroid hormone. This hormone increases metabolic activity and heat production in cells throughout the body.
- The adrenal glands may also be stimulated to secrete the hormone adrenaline. This hormone causes the breakdown of glycogen (the carbohydrate used for energy storage in animals) to glucose, which can be used as an energy source. This catabolic chemical process is exothermic, or heat producing.
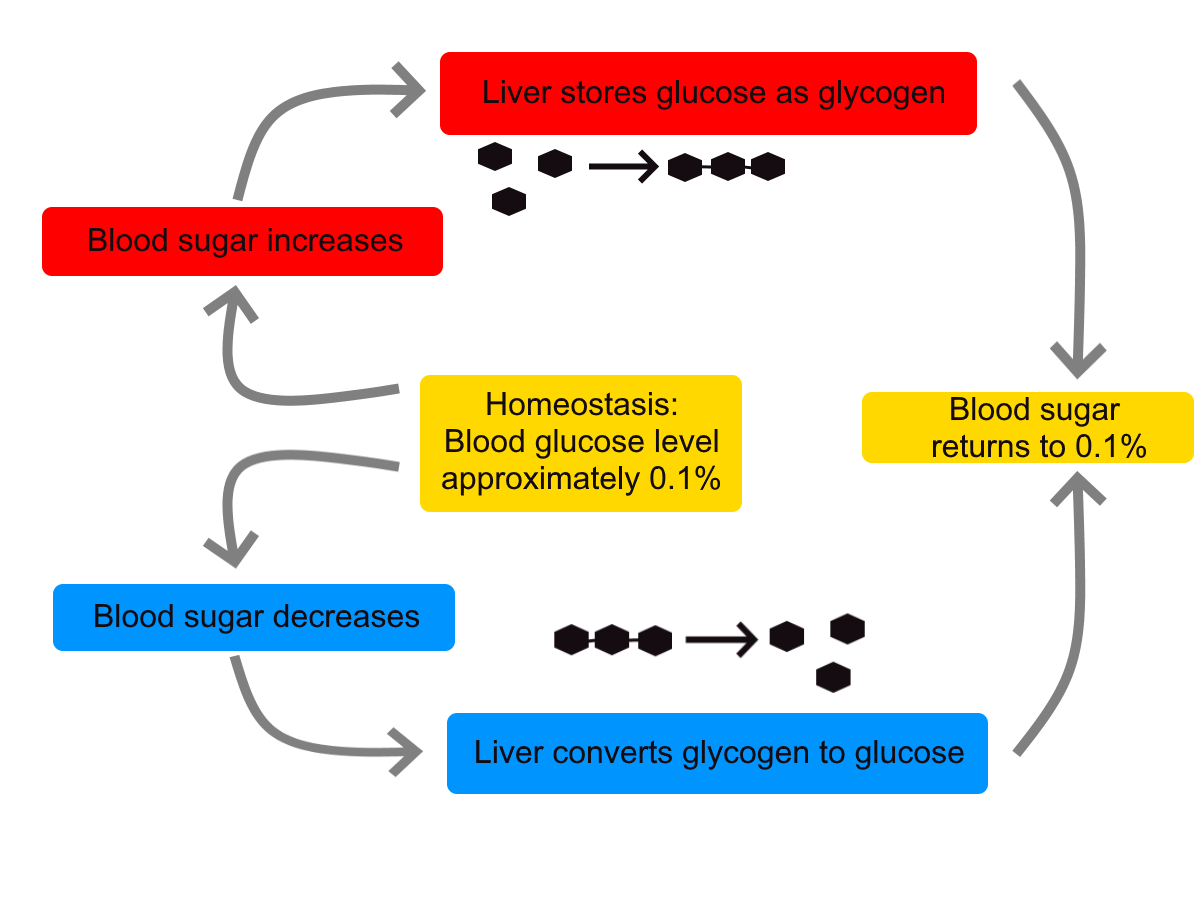
Blood Glucose
In controlling the blood glucose level, certain endocrine cells in the pancreas (called alpha and beta cells) detect the level of glucose in the blood. They then respond appropriately to keep the level of blood glucose within the normal range.
- If the blood glucose level rises above the normal range, pancreatic beta cells release the hormone insulin into the bloodstream. Insulin signals cells to take up the excess glucose from the blood until the level of blood glucose decreases to the normal range.
- If the blood glucose level falls below the normal range, pancreatic alpha cells release the hormone glucagon into the bloodstream. Glucagon signals cells to break down stored glycogen to glucose and release the glucose into the blood until the level of blood glucose increases to the normal range.
https://www.youtube.com/watch?v=Iz0Q9nTZCw4
Homeostasis and Negative/Positive Feedback, Amoeba Sisters, 2017.
Positive Feedback
In a positive feedback loop, feedback serves to intensify a response until an end point is reached. Examples of processes controlled by positive feedback in the human body include blood clotting and childbirth.
Blood Clotting
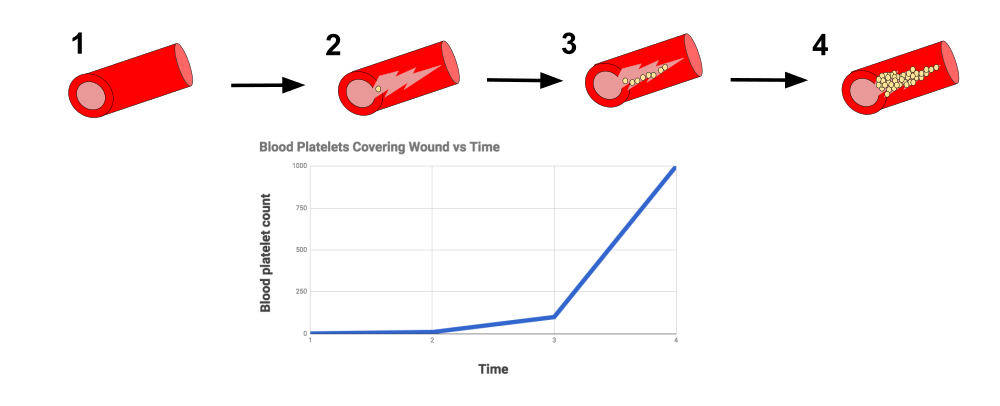
When a wound causes bleeding, the body responds with a positive feedback loop to clot the blood and stop blood loss. Substances released by the injured blood vessel wall begin the process of blood clotting. Platelets in the blood start to cling to the injured site and release chemicals that attract additional platelets. As the platelets continue to amass, more of the chemicals are released and more platelets are attracted to the site of the clot. The positive feedback accelerates the process of clotting until the clot is large enough to stop the bleeding.
Childbirth
Figure 7.8.6 shows the positive feedback loop that controls childbirth. The process normally begins when the head of the infant pushes against the cervix. This stimulates nerve impulses, which travel from the cervix to the hypothalamus in the brain. In response, the hypothalamus sends the hormone oxytocin to the pituitary gland, which secretes it into the bloodstream so it can be carried to the uterus. Oxytocin stimulates uterine contractions, which push the baby harder against the cervix. In response, the cervix starts to dilate in preparation for the passage of the baby. This cycle of positive feedback continues, with increasing levels of oxytocin, stronger uterine contractions, and wider dilation of the cervix until the baby is pushed through the birth canal and out of the body. At that point, the cervix is no longer stimulated to send nerve impulses to the brain, and the entire process stops.
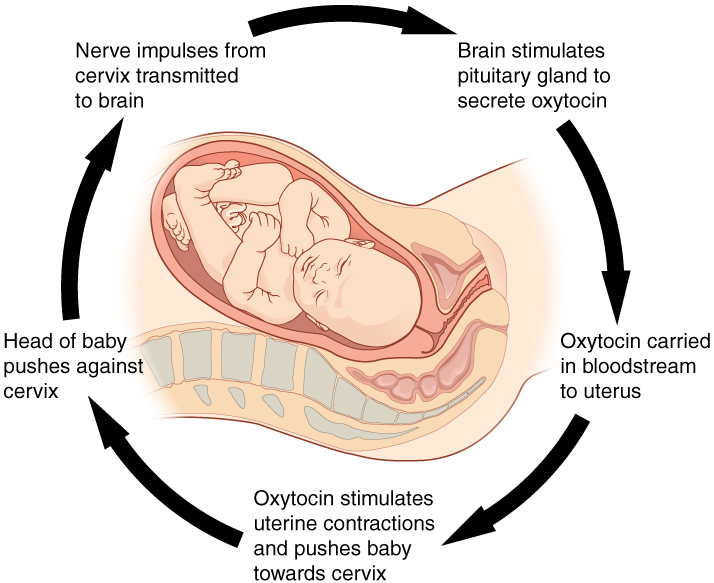
Normal childbirth is driven by a positive feedback loop. Positive feedback causes an increasing deviation from the normal state to a fixed end point, rather than a return to a normal set point as in homeostasis.
When Homeostasis Fails
Homeostatic mechanisms work continuously to maintain stable conditions in the human body. Sometimes, however, the mechanisms fail. When they do, homeostatic imbalance may result, in which cells may not get everything they need or toxic wastes may accumulate in the body. If homeostasis is not restored, the imbalance may lead to disease — or even death. Diabetes is an example of a disease caused by homeostatic imbalance. In the case of diabetes, blood glucose levels are no longer regulated and may be dangerously high. Medical intervention can help restore homeostasis and possibly prevent permanent damage to the organism.
Normal aging may bring about a reduction in the efficiency of the body’s control systems, which makes the body more susceptible to disease. Older people, for example, may have a harder time regulating their body temperature. This is one reason they are more likely than younger people to develop serious heat-induced illnesses, such as heat stroke.
Feature: My Human Body
Diabetes is diagnosed in people who have abnormally high levels of blood glucose after fasting for at least 12 hours. A fasting level of blood glucose below 100 is normal. A level between 100 and 125 places you in the pre-diabetes category, and a level higher than 125 results in a diagnosis of diabetes.
Of the two types of diabetes, type 2 diabetes is the most common, accounting for about 90 per cent of all cases of diabetes in the United States. Type 2 diabetes typically starts after the age of 40. However, because of the dramatic increase in recent decades in obesity in younger people, the age at which type 2 diabetes is diagnosed has fallen. Even children are now being diagnosed with type 2 diabetes. Today, about 3 million Canadians (8.1% of total population) are living with diabetes.
You may at some point have your blood glucose level tested during a routine medical exam. If your blood glucose level indicates that you have diabetes, it may come as a shock to you because you may not have any symptoms of the disease. You are not alone, because as many as one in four diabetics do not know they have the disease. Once the diagnosis of diabetes sinks in, you may be devastated by the news. Diabetes can lead to heart attacks, strokes, blindness, kidney failure, nerve damage, and loss of toes or feet. The risk of death in adults with diabetes is 50 per cent greater than it is in adults without diabetes, and diabetes is the seventh leading cause of death of adults. In addition, controlling diabetes usually requires frequent blood glucose testing, watching what and when you eat, and taking medications or even insulin injections. All of this may seem overwhelming.
The good news is that changing your lifestyle may stop the progression of type 2 diabetes or even reverse it. By adopting healthier habits, you may be able to keep your blood glucose level within the normal range without medications or insulin. Here’s how:
- Lose weight. Any weight loss is beneficial. Losing as little as seven per cent of your weight may be all that is needed to stop diabetes in its tracks. It is especially important to eliminate excess weight around your waist.
- Exercise regularly. You should try to exercise for at least 30 minutes, five days a week. This will not only lower your blood sugar and help your insulin work better, but it will also lower your blood pressure and improve your heart health. Another bonus of exercise is that it will help you lose weight by increasing your basal metabolic rate.
- Adopt a healthy diet. Decrease your consumption of refined carbohydrates, such as sweets and sugary drinks. Increase your intake of fibre-rich foods, such as fruits, vegetables, and whole grains. About one-quarter of each meal should consist of high-protein foods, such as fish, chicken, dairy products, legumes, or nuts.
- Control stress. Stress can increase your blood glucose and also raise your blood pressure and risk of heart disease. When you feel stressed out, do breathing exercises or take a brisk walk or jog. Try to replace stressful thoughts with more calming ones.
- Establish a support system. Enlist the help and support of loved ones, as well as medical professionals, such as a nutritionist and diabetes educator. Having a support system will help ensure that you are on the path to wellness, and that you can stick to your plan.
7.8 Summary
- Homeostasis is the condition in which a system (such as the human body) is maintained in a more or less steady state. It is the job of cells, tissues, organs, and organ systems throughout the body to maintain homeostasis.
- For any given variable, such as body temperature, there is a particular set point that is the physiological optimum value. The spread of values around the set point that is considered insignificant is called the normal range.
- Homeostasis is generally maintained by a negative feedback loop that includes a stimulus, sensor, control centre, and effector. Negative feedback serves to reduce an excessive response and to keep a variable within the normal range. Negative feedback loops control body temperature and the blood glucose level.
- Positive feedback loops are not common in biological systems. Positive feedback serves to intensify a response until an end point is reached. Positive feedback loops control blood clotting and childbirth.
- Sometimes homeostatic mechanisms fail, resulting in homeostatic imbalance. Diabetes is an example of a disease caused by homeostatic imbalance. Aging can bring about a reduction in the efficiency of the body’s control system, which makes the elderly more susceptible to disease.
7.8 Review Questions
-
-
- Compare and contrast negative and positive feedback loops.
- Explain how negative feedback controls body temperature.
- Give two examples of physiological processes controlled by positive feedback loops.
- During breastfeeding, the stimulus of the baby sucking on the nipple increases the amount of milk produced by the mother. The more sucking, the more milk is usually produced. Is this an example of negative or positive feedback? Explain your answer. What do you think might be the evolutionary benefit of the milk production regulation mechanism you described?
- Explain why homeostasis is regulated by negative feedback loops, rather than positive feedback loops.
- The level of a sex hormone, testosterone (T), is controlled by negative feedback. Another hormone, gonadotropin-releasing hormone (GnRH), is released by the hypothalamus of the brain, which triggers the pituitary gland to release luteinizing hormone (LH). LH stimulates the gonads to produce T. When there is too much T in the bloodstream, it feeds back on the hypothalamus, causing it to produce less GnRH. While this does not describe all the feedback loops involved in regulating T, answer the following questions about this particular feedback loop.
- What is the stimulus in this system? Explain your answer.
- What is the control centre in this system? Explain your answer.
- In this system, is the pituitary considered the stimulus, sensor, control centre, or effector? Explain your answer.
7.8 Explore More
https://www.youtube.com/watch?v=LSgEJSlk6W4
Homeostasis - What Is Homeostasis - What Is Set Point For Homeostasis - Homeostasis In The Human Body, Whats Up Dude, 2017.
https://www.youtube.com/watch?v=XMsJ-3qRVJM
Attributions
Figure 7.8.1
Nest_Thermostat by Amanitamano on Wikimedia Commons is used under a CC BY-SA 3.0 (https://creativecommons.org/licenses/by-sa/3.0/deed.en) license.
Figure 7.8.2
Negative_Feedback_Loops by OpenStax on Wikimedia Commons is used under a CC BY 4.0 (https://creativecommons.org/licenses/by/4.0/deed.en) license.
Figure 7.8.3
Body Temperature Homeostasis by OpenStax College, Biology is used under a CC BY 4.0 license.
Figure 7.8.4
Homeostasis_of_blood_sugar by Christinelmiller on Wikimedia Commons is used under a CC0 1.0 Universal Public Domain Dedication (https://creativecommons.org/publicdomain/zero/1.0/deed.en) license.
Figure 7.8.5
Positive_Feedback_Diagram_Blood_Clotting by Elliottuttle on Wikimedia Commons is used under a CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0) license.
Figure 7.8.6
Pregnancy-Positive_Feedback by OpenStax on Wikimedia Commons is used under a CC BY 4.0 (https://creativecommons.org/licenses/by/4.0/deed.en) license.
References
Amoeba Sisters. (2017, September 7). Homeostasis and negative/positive feedback. YouTube. https://www.youtube.com/watch?v=Iz0Q9nTZCw4&feature=youtu.be
Betts, J. G., Young, K.A., Wise, J.A., Johnson, E., Poe, B., Kruse, D.H., Korol, O., Johnson, J.E., Womble, M., DeSaix, P. (2013, April 25). Figure 1.10 Negative feedback loop [digital image/ diagram]. In Anatomy and Physiology (Section 1.5). OpenStax. https://openstax.org/books/anatomy-and-physiology/pages/1-5-homeostasis
Betts, J. G., Young, K.A., Wise, J.A., Johnson, E., Poe, B., Kruse, D.H., Korol, O., Johnson, J.E., Womble, M., DeSaix, P. (2013, April 25). Figure 1.11 Positive feedback loop normal childbirth is driven by a positive feedback loop [digital image/ diagram]. In Anatomy and Physiology (Section 1.5). OpenStax. https://openstax.org/books/anatomy-and-physiology/pages/1-5-homeostasis
Cognito. (2018, December 18). GCSE Biology - Homeostasis #38. YouTube. https://www.youtube.com/watch?v=XMsJ-3qRVJM&feature=youtu.be
Mayo Clinic Staff. (n.d.). Type 2 diabetes [online article]. MayoClinic.org. https://www.mayoclinic.org/diseases-conditions/type-2-diabetes/symptoms-causes/syc-20351193
OpenStax CNX. (2016, March 23). Figure 4 The body is able to regulate temperature in response to signals from the nervous system [digital image]. In OpenStax, Biology (Section 33.3). https://cnx.org/contents/GFy_h8cu@10.8:BP24ZReh@7/Homeostasis
Whats Up Dude. (2017, September 20). Homeostasis - What is homeostasis - What is set point for homeostasis - Homeostasis in the human body. YouTube. https://www.youtube.com/watch?v=LSgEJSlk6W4&feature=youtu.be
Image shows a photograph of a women with a goiter. The centre bottom of her throat has a visible enlargement.
Image shows an illustration of the thyroid gland. It is located in front of where an Adam's apple would be. It is roughly butterfly shaped. The "wings" are the right and left lobes, and the connecting part is the isthmus.
As per caption.
An antibody, also known as an immunoglobulin, is a large, Y-shaped protein produced mainly by plasma cells that is used by the immune system to neutralize pathogens such as pathogenic bacteria and viruses.
Image shows a photograph of a person getting a pedicure at a salon.

Nail Art
Painting nails with coloured polish for aesthetic reasons is nothing new. In fact, there is evidence of this practice dating back to at least 3000 BCE. Today, painting and otherwise decorating the nails is big business, with annual revenues in the billions of dollars in North America alone! With all the attention (and money) given to nails as decorative objects, it’s easy to forget that they also have important biological functions.
What Are Nails?
Nails are accessory organs of the skin. They are made of sheets of dead keratinocytes and are found on the far (or distal) ends of the fingers and toes. The keratin in nails makes them hard, but flexible. Nails serve a number of purposes, including protecting the digits, enhancing sensations, and acting as tools.
Nail Anatomy
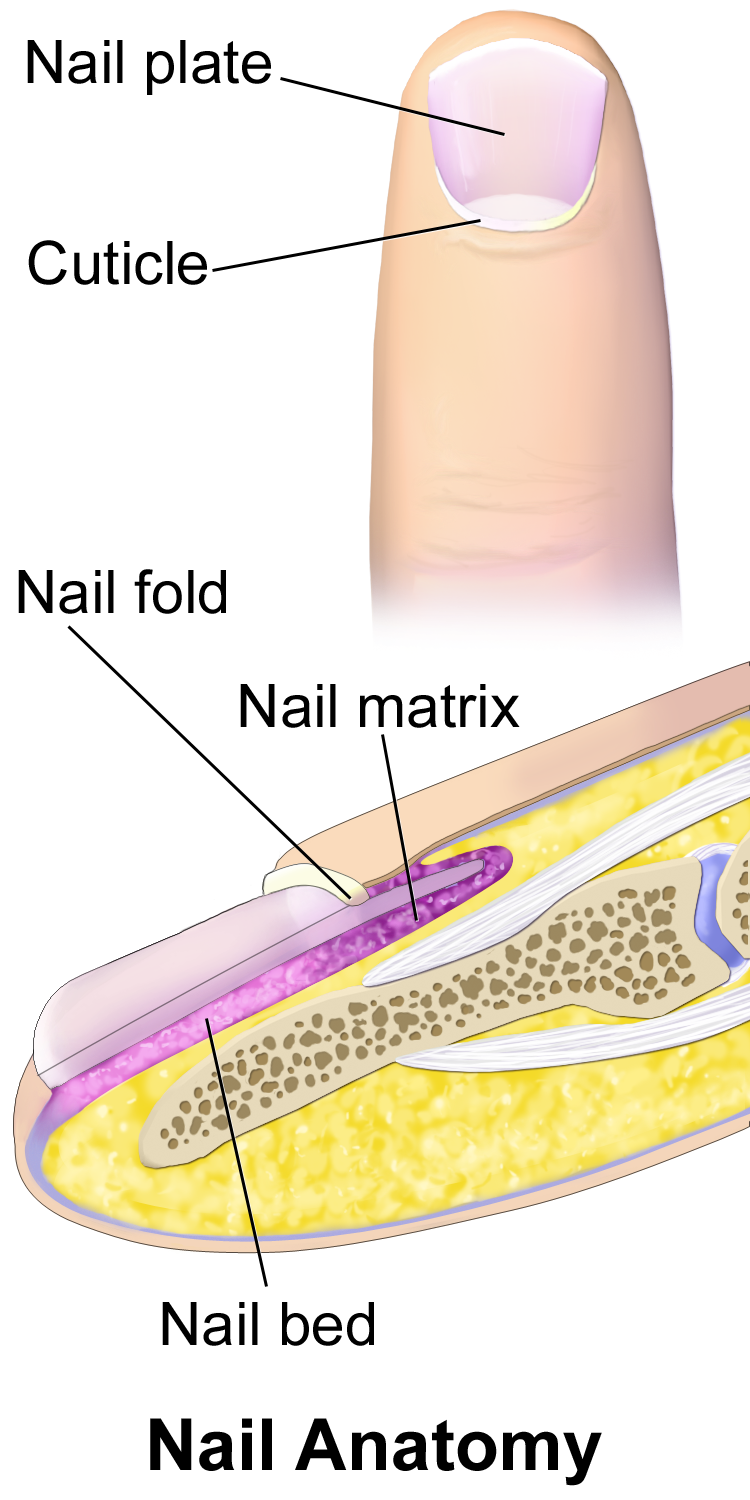
A nail has three main parts: the root, plate, and free margin. Other structures around or under the nail include the nail bed, cuticle, and nail fold. These structures are shown in Figure 10.6.2.
- The nail root is the portion of the nail found under the surface of the skin at the near (or proximal) end of the nail. It is where the nail begins.
- The nail plate (or body) is the portion of the nail that is external to the skin. It is the visible part of the nail.
- The free margin is the portion of the nail that protrudes beyond the distal end of the finger or toe. This is the part that is cut or filed to keep the nail trimmed.
- The nail bed is the area of skin under the nail plate. It is pink in colour, due to the presence of capillaries in the dermis.
- The cuticle is a layer of dead epithelial cells that overlaps and covers the edge of the nail plate. It helps to seal the edges of the nail to prevent infection of the underlying tissues.
- The nail fold is a groove in the skin in which the side edges of the nail plate are embedded.
Nail Growth
Nails grow from a deep layer of living epidermal tissue, known as the nail matrix, at the proximal end of the nail (see the bottom of the diagram in Figure 10.6.2). The nail matrix surrounds the nail root. It contains stem cells that divide to form keratinocytes, which are cells that produce keratin and make up the nail.
Formation of the Nail Root and Nail Plate
The keratinocytes produced by the nail matrix accumulate to form tough, hard, translucent sheets of dead cells filled with keratin. The sheets make up the nail root, which slowly grows out of the skin and becomes the nail plate when it reaches the skin surface. As the nail grows longer, the cells of the nail root and nail plate are pushed toward the distal end of the finger or toe by new cells being formed in the nail matrix. The upper epidermal cells of the nail bed also move along with the nail plate as it grows toward the tip of the digit.
The proximal end of the nail plate near the root has a whitish crescent shape called the lunula. This is where a small amount of the nail matrix is visible through the nail plate. The lunula is most pronounced in the nails of the thumbs, and may not be visible in the nails of the little fingers.
Rate of Nail Growth
Nails grow at an average rate of 3 mm a month. Fingernails, however, grow up to four times as fast as toenails. If a fingernail is lost, it takes between three and six months to regrow completely, whereas a toenail takes between 12 and 18 months to regrow. The actual rate of growth of an individual’s nails depends on many factors, including age, sex, season, diet, exercise level, and genes. If protected from breaking, nails can sometimes grow to be very long. The Chinese doctor in the photo below (Figure 10.6.3) has very long nails on two fingers of his left hand. This picture was taken in 1920 in China, where having long nails was a sign of aristocracy since it implied that one was wealthy enough to not have to do physical labour.

Functions of Nails
Both fingernails and toenails protect the soft tissues of the fingers and toes from injury. Fingernails also serve to enhance sensation and precise movements of the fingertips through the counter-pressure exerted on the pulp of the fingers by the nails. In addition, fingernails can function as several different types of tools. For example, they enable a fine precision grip like tweezers, and can also be used for cutting and scraping.
Nails and Health
Healthcare providers, particularly EMTs, often examine the fingernail beds as a quick and easy indicator of oxygen saturation of the blood, or the amount of blood reaching the extremities. If the nail beds are bluish or purple, it is generally a sign of low oxygen saturation. To see if blood flow to the extremities is adequate, a blanch test may be done. In this test, a fingernail is briefly depressed to turn the nail bed white by forcing the blood out of its capillaries. When the pressure is released, the pink colour of the nail bed should return within a second or two if there is normal blood flow. If the return to a pink colour is delayed, then it can be an indicator of low blood volume, due to dehydration or shock.

How the visible portion of the nails appears can be used as an indicator of recent health status. In fact, nails have been used as diagnostic tools for hundreds — if not thousands — of years. Nail abnormalities, such as deep grooves, brittleness, discolouration, or unusually thin or thick nails, may indicate various illnesses, nutrient deficiencies, drug reactions, or other health problems.
Nails — especially toenails — are common sites of fungal infections (shown in Figure 10.6.4), causing nails to become thickened and yellowish in colour. Toenails are more often infected than fingernails because they are often confined in shoes, which creates a dark, warm, moist environment where fungi can thrive. Toes also tend to have less blood flow than fingers, making it harder for the immune system to detect and stop infections in toenails.
Although nails are harder and tougher than skin, they are also more permeable. Harmful substances may be absorbed through the nails and cause health problems. Some of the substances that can pass through the nails include the herbicide Paraquat, fungicidal agents such as miconazole (e.g., Monistat), and sodium hypochlorite, which is an ingredient in common household bleach. Care should be taken to protect the nails from such substances when handling or immersing the hands in them by wearing latex or rubber gloves.
Feature: Reliable Sources

Do you get regular manicures or pedicures from a nail technician? If so, there is a chance that you are putting your health at risk. Nail tools that are not properly disinfected between clients may transmit infections from one person to another. Cutting the cuticles with scissors may create breaks in the skin that let infective agents enter the body. Products such as acrylics, adhesives, and UV gels that are applied to the nails may be harmful, especially if they penetrate the nails and enter the skin.
Use the Internet to find several reliable sources that address the health risks of professional manicures or pedicures. Try to find answers to the following questions:
- What training and certification are required for professional nail technicians?
- What licenses and inspections are required for nail salons?
- What hygienic practices should be followed in nail salons to reduce the risk of infections being transmitted to clients?
- Which professional nail products are potentially harmful to the human body and which are safer?
- How likely is it to have an adverse health consequence when you get a professional manicure or pedicure?
- What steps can you take to ensure that a professional manicure or pedicure is safe?
10.6 Summary
- Nails are accessory organs of the skin, consisting of sheets of dead, keratin-filled keratinocytes. The keratin in nails makes them hard, but flexible.
- A nail has three main parts: the nail root (which is under the epidermis), the nail plate (which is the visible part of the nail), and the free margin (which is the distal edge of the nail). Other structures under or around a nail include the nail bed, cuticle, and nail fold.
- A nail grows from a deep layer of living epidermal tissues — called the nail matrix — at the proximal end of the nail. Stem cells in the nail matrix keep dividing to allow nail growth, forming first the nail root and then the nail plate as the nail continues to grow longer and emerges from the epidermis.
- Fingernails grow faster than toenails. Actual rates of growth depend on many factors, such as age, sex, and season.
- Functions of nails include protecting the digits, enhancing sensations and precise movements of the fingertips, and acting as tools.
- The colour of the nail bed can be used to quickly assess oxygen and blood flow in a patient. How the nail plate grows out can reflect recent health problems, such as illness or nutrient deficiency.
- Nails — and especially toenails — are prone to fungus infections. Nails are more permeable than skin and can absorb several harmful substances, such as herbicides.
10.6 Review Questions
- What are nails?
-
- Explain why most of the nail plate looks pink.
- Describe a lunula.
- Explain how a nail grows.
- Identify three functions of nails.
- Give several examples of how nails are related to health.
- What is the cuticle of the nail composed of? What is the function of the cuticle? Why is it a bad idea to cut the cuticle during a manicure?
- Is the nail plate composed of living or dead cells?
10.6 Explore More
https://www.youtube.com/watch?v=G35kPhbUZdg
Longest Fingernails - Guinness World Records 60th Anniversary,
Guinness World Records, 2014.
https://www.youtube.com/watch?v=aTSVHwzkYI4&feature=emb_logo
5 Things Your Nails Can Say About Your Health, SciShow, 2015.
https://www.youtube.com/watch?v=7w2gCBL1MCg
Claws vs. Nails - Matthew Borths, TED-Ed, 2019.
Attributions
Figure 10.6.1
Nails by allison-christine-vPrqHSLdF28 [photo] by allison christine on Unsplash is used under the Unsplash License (https://unsplash.com/license).
Figure 10.6.2
Blausen_0406_FingerNailAnatomy by BruceBlaus on Wikimedia Commons is used under a CC BY 3.0 (https://creativecommons.org/licenses/by/3.0) license.
Figure 10.6.3
Chinese_doctor_with_long_finger_nails_(an_aristocrat),_ca.1920_(CHS-249) by Pierce, C.C. (Charles C.), 1861-1946 from the USC Digital Library on Wikimedia Commons is in the public domain (https://en.wikipedia.org/wiki/public_domain).
Figure 10.6.4
Toenail fungus Nagelpilz-3 by Pepsyrock on Wikimedia Commons is released into the public domain (https://en.wikipedia.org/wiki/public_domain).
Figure 10.6.5
OLYMPUS DIGITAL CAMERA by Stoive at the English language Wikipedia, on Wikimedia Commons is used under a CC BY-SA 3.0 (http://creativecommons.org/licenses/by-sa/3.0/) license.
References
Blausen.com staff. (2014). Medical gallery of Blausen Medical 2014. WikiJournal of Medicine 1 (2). DOI:10.15347/wjm/2014.010. ISSN 2002-4436.
Guiness World Records. (2014, December 8). Longest fingernails - Guinness World Records 60th Anniversary. YouTube. https://www.youtube.com/watch?v=G35kPhbUZdg
SciShow. (2015, September 14). 5 things your nails can say about your health. YouTube. https://www.youtube.com/watch?v=aTSVHwzkYI4
TED-Ed. (2019, October 29). Claws vs. nails - Matthew Borths. YouTube. https://www.youtube.com/watch?v=7w2gCBL1MCg
A type of immune cell that stimulates killer T cells, macrophages, and B cells to make immune responses. A helper T cell is a type of white blood cell and a type of lymphocyte.
Image shows a photograph of two adults laying on the grass in the sun in their swimsuits.
Image shows a diagram of the types and locations of sensory receptors in the dermis.
There are free nerve endings towards the exterior of the dermis, Merkle cells and Meissners corpuscles are embedded just below the free nerve endings. Ruffini corpuscles and lamellated corpuscles are present deeper in the dermal tissue.
A type of white blood cell and, specifically, a type of lymphocyte.
Many B cells mature into what are called plasma cells that produce antibodies (proteins) necessary to fight off infections while other B cells mature into memory B cells.
Foreign proteins on the surface of a cell that triggers an immune response.
Image shows a diagram of the negative feedback loop governing thyroid gland function. In the absence of sufficient levels of thyroid hormones, the hypothalamus will secrete TRH, which stimulates the pituitary gland to secrete TSH, which stimulates the thyroid gland to make thyroid hormones. Sufficient blood levels of thyroid hormone inhibit the hypothalamus from secreting TRH, halting the pathway, until thyroid hormone level sdrop again
Image shows a diagram of the layers of the epidermis. The outermost layer is the stratum corneum, below that is the stratum lucidum, below that the stratum granulosum, below that the stratum spinosum, below that the stratum basale, and then a basement membrane which connects the dermis to the epidermis.
Image shows a photograph of a person applying henna to a persons hand.
Created by CK-12 Foundation/Adapted by Christine Miller

Case Study Conclusion: Wearing His Heart on His Sleeve
Are you still wondering whether Ayko, who you read about in the beginning of this chapter, actually got a tattoo of his new girlfriend’s name on his arm? Figure 10.8.1 is your answer! Let’s hope his love for Larissa — and for the artwork — lasts as long as his tattoo. According to a poll conducted for Global TV by Ipsos Reid in 2012, 10% of Canadian and 11% of American adults regret getting a tattoo. Although laser tattoo removal is available, it does not always work fully, can cause pain and scarring, and is expensive and time-consuming. Some people who regret a tattoo opt instead (or additionally) to cover it with another tattoo, see Figure 10.8.2 below.

Why are tattoos essentially permanent? Tattoos are created by inserting a needle containing pigment through the epidermis and into the dermis of the skin. The pigment is injected into the dermal layer, creating the design. The pigment can remain in the dermal layer for a person’s lifetime for a few reasons. One, unlike the thinner outer epidermal layer, the dermis is not continually shed and replaced, so the pigment generally stays put. Two, the pigments used in tattooing mainly consist of large particles. When you get a tattoo, the penetration of the skin and insertion of foreign particles causes an immune response in which white blood cells attempt to engulf and remove the pigment. Because most of the pigment particles are so large, however, they cannot be removed from the dermis by the immune cells, and the design remains.
In laser tattoo removal, pulses from a high-intensity laser are applied to the tattoo and absorbed by the pigments. This breaks up the large pigment particles into particles that are small enough to be removed by the immune system. The pigments may then be excreted out of the body, or moved to other areas of the body, such as the lymph nodes. Different wavelengths of laser energy are often required to remove different colours of pigments, because they absorb different wavelengths of light. Generally, blue and black are the easiest colours to remove. Green, red, and yellow tend to be the hardest to remove. It may take as many as six to ten laser treatments — with a few weeks of recovery time in between — to remove a tattoo. Some tattoos can never be completely removed.
Why are mehndi designs (like Ayko’s trial “henna tattoo”) not permanent? Unlike real tattoos, henna paste is applied on the surface of the skin (shown below in Figure 10.8.3), and not injected into the skin with a needle. The dye molecules simply migrate from the paste into the top layer of the epidermis, the stratum corneum.

As you have learned, the stratum corneum consists of dead, keratin-filled keratinocytes, which are continually shed and replaced with new cells from the layers below. As a result, mehndi is not permanent. The design is lost as the cells that contain the dye are shed and replaced.
As you read in the beginning of this chapter, mehndi is often applied to the palms of the hands and soles of the feet, which generally results in a darker stain than other areas of the body. This is because the stratum corneum is thicker in these regions, so the dye penetrates through more layers of cells, making the design appear darker. What else is different about the epidermis of the palms and soles? You may recall that these regions are the only place where there is a fifth layer of epidermis — the stratum lucidum — making the skin in these areas even thicker and tougher.
Hopefully, Ayko thought carefully about the potential emotional and social implications of getting a tattoo — and learned how difficult they are to remove — before getting a real one. Health and safety should also be of utmost concern to anyone considering getting a tattoo. As you have learned in this chapter, the skin acts as a barrier against dangerous pathogens and substances. When you penetrate the skin using a needle, it can introduce harmful viruses and bacteria directly into the dermis, where the blood vessels are. Tattoo artists and shops need to take precautions to protect their clients against diseases that can be transmitted through blood (such as HIV and hepatitis), as well as bacterial infections. The tattoo artist should wear disposable gloves and a mask, use new and unopened needles and ink tubes, and properly sterilize other equipment. Even if the artist takes all the proper precautions, there is still a chance that the unopened ink could have been contaminated with pathogens during the production process. The shop should be aware of any ink recalls. Anyone getting a tattoo should make sure their artist and shop strictly adhere to all local health and safety regulations.
The risk of disease is not the only risk from tattoos. The pigments in tattoos may contain heavy metals and other potentially toxic substances. Tattoo parlours are regulated by provincial guidelines in Canada, and these guidelines vary from province to province — but these guidelines are mainly concerned with sterilization of equipment and don't address anything about pigments. A recent study published in the scientific journal Nature (Scientific Reports) showed that pigments from tattoos may migrate from a person's tattoos into their lymph nodes. Among the substances that make up the tattoo ink that migrated were aluminum, chromium, iron, nickel and copper - all considered "toxic".
Additionally, people can sometimes have an allergic reaction to the pigments, or develop scarring or granulomas (small bumps of tissue due to an immune response) around the tattoo. Rarely, people can experience temporary swelling or burning of their tattoos when they get scanned in an MRI machine for a medical procedure. Clearly, people should think carefully about the potential health implications before getting a tattoo.
Fortunately, Ayko found a reputable and safe tattoo artist, and is not experiencing any ill effects from his tattoo. He is happy with his tattoo, at least for now. Tattoos — and other kinds of decoration of the integumentary system — are forms of artistic, personal, and cultural expression that have been used by many cultures over the course of human history. The system that protects us from the elements, helps us maintain homeostasis, and mediates our interactions with the outside world also happens to be easily modifiable! Whether it is a haircut, makeup, beard style, nail polish, piercing or a tattoo, humans have a variety of ways of altering our integumentary system, which changes our outward appearance and what we communicate to others.
Chapter 10 Summary
In this chapter, you learned about the structures and functions of the organs of the integumentary system. Specifically, you learned that:
- The integumentary system consists of the skin, hair, and nails. Functions of the integumentary system include providing a protective covering for the body, sensing the environment, and helping the body maintain homeostasis.
- The skin’s main functions include preventing water loss from the body, serving as a barrier to the entry of microorganisms, synthesizing vitamin D, blocking UV light, and helping to regulate body temperature.
- The skin consists of two distinct layers: a thinner outer layer called the epidermis, and a thicker inner layer called the dermis.
-
- The epidermis consists mainly of epithelial cells called keratinocytes, which produce keratin. New keratinocytes form at the bottom of the epidermis. They become filled with keratin and die as they move upward toward the surface of the skin, where they form a protective, waterproof layer.
- The dermis consists mainly of tough connective tissues that provide strength and stretch, as well as almost all skin structures, including blood vessels, sensory receptors, hair follicles, and oil and sweat glands.
- Cell types in the epidermis include keratinocytes (which make up 90 per cent of epidermal cells), melanocytes that produce melanin, Langerhans cells that fight pathogens in the skin, and Merkel cells that respond to light touch.
- In most parts of the body, the epidermis consists of four distinct layers. A fifth layer occurs only in the epidermis of the palms of the hands and soles of the feet.
-
- The innermost layer of the epidermis is the stratum basale, which contains stem cells that divide to form new keratinocytes.
- The next layer is the stratum spinosum, which is the thickest layer, and contains Langerhans cells and spiny keratinocytes.
- This is followed by the stratum granulosum, in which keratinocytes are filling with keratin and beginning to die.
- The stratum lucidum is next, but only on the palms and soles. It consists of translucent dead keratinocytes.
- The outermost layer is the stratum corneum, which consists of flat, dead, tightly packed keratinocytes that form a tough, waterproof barrier for the rest of the epidermis.
- The epidermis protects underlying tissues from physical damage and pathogens. Melanin in the epidermis absorbs and protects underlying tissues from UV light. The epidermis also prevents loss of water from the body and synthesizes vitamin D.
-
- Melanin is the main pigment that determines the colour of human skin. However, the pigments carotene and hemoglobin also contribute to skin colour, especially in skin with low levels of melanin.
- The surface of healthy skin normally is covered by vast numbers of bacteria representing about one thousand species from 19 phyla. Different areas of the body provide diverse habitats for skin microorganisms. Usually, microorganisms on the skin keep each other in check unless their balance is disturbed.
- The thicker inner layer of the skin — the dermis — has two layers. The upper papillary layer has papillae extending upward into the epidermis and loose connective tissues. The lower reticular layer has denser connective tissues and structures, such as glands and hair follicles. Glands in the dermis include eccrine and apocrine sweat glands, as well as sebaceous glands. Hair follicles are structures where hairs originate.
- Functions of the dermis include cushioning subcutaneous tissues, regulating body temperature, sensing the environment, and excreting wastes. The dense connective tissues of the dermis provide cushioning. The dermis regulates body temperature mainly by sweating and by vasodilation or vasoconstriction. The many tactile sensory receptors in the dermis make it the main organ for the sense of touch. Wastes excreted in sweat include excess water, electrolytes, and certain metabolic wastes.
- Hair is a filament that grows from a hair follicle in the dermis of the skin. It consists mainly of tightly packed, dead keratinocytes that are filled with keratin. The human body is almost completely covered with hair follicles.
- Hair helps prevent heat loss from the head and protects its skin from UV light. Hair in the nose filters incoming air, and the eyelashes and eyebrows keep harmful substances out of the eyes. Hair all over the body provides tactile sensory input. The eyebrows also play a role in nonverbal communication.
- The part of a hair that is within the follicle is the hair root. This is the only living part of a hair. The part of a hair that is visible above the skin surface is the hair shaft. It consists of dead cells.
-
- Hair growth begins inside a follicle when stem cells within the follicle divide to produce new keratinocytes.
- A hair shaft has three zones: the outermost zone called the cuticle, the middle zone called the cortex, and the innermost zone called the medulla.
- Genetically controlled, visible characteristics of hair include hair colour, hair texture, and the extent of balding in adult males. Melanin (eumelanin and/or pheomelanin) is the pigment that gives hair its colour. Aspects of hair texture include curl pattern, thickness, and consistency.
- Among mammals, humans are nearly unique in having undergone significant loss of body hair during their evolution, probably because sweat evaporates more quickly from less hairy skin. Curly hair also is thought to have evolved at some point during human evolution, perhaps because it provided better protection from UV light.
- Hair has social significance for human beings, being an indicator of biological sex, age, and ethnic ancestry. Human hair also has cultural significance. For example, hairstyle may be an indicator of social group membership.
- Nails consist of sheets of dead, keratin-filled keratinocytes. The keratin in nails makes them hard but flexible. They help protect the ends of the fingers and toes, enhance the sense of touch in the fingertips, and may be used as tools.
- A nail has three main parts: the nail root, which is under the epidermis; the nail plate, which is the visible part of the nail; and the free margin, which is the distal edge of the nail. Other structures under or around a nail include the nail bed, cuticle, and nail fold.
- A nail grows from a deep layer of living epidermal tissues, called the nail matrix, at the proximal end of the nail. Stem cells in the nail matrix keep dividing to allow nail growth, forming first the nail root and then the nail plate as the nail continues to grow longer and emerges from the epidermis.
- Fingernails grow faster than toenails. Actual rates of growth depend on many factors, such as age, sex, and season.
- The colour of the nail bed can be used to quickly assess oxygen and blood flow in a patient. How the nail plate grows out can reflect recent health problems, such as illness or nutrient deficiency. Nails — and especially toenails — are prone to fungus infections. Nails are more permeable than skin and can absorb several harmful substances, such as herbicides.
- Skin cancer is a disease in which skin cells grow out of control. It is caused mainly by excessive exposure to UV light, which damages DNA.
- There are three common types of skin cancer: basal cell carcinoma, squamous cell carcinoma, and melanoma. Carcinomas are more common and unlikely to metastasize. Melanoma is rare and likely to metastasize. It causes most skin cancer deaths.
- Besides exposure to UV light, risk factors for skin cancer include having light coloured skin, having many moles, and a family history of skin cancer, among several others.
Now that you have learned about the organs on surface of the body, read the next chapter to travel inside and learn about the skeletal system, which protects and supports us internally, among other functions.
Chapter 10 Review
- Describe one way in which the integumentary system works with another organ system to carry out a particular function.
-
- Describe two types of waterproofing used in the integumentary system. Include the types of molecules and where they are located.
- Explain why nails enhance touch sensations.
- Why do you think light coloured skin is a risk factor for skin cancer?
- Describe the similarities between how the epidermis, hair, and nails all grow.
- What does the whitish crescent-shaped area at the base of your nails (toward your hands) represent? What is its function?
- What is one difference between human hair and the hair of non-human primates?
- Describe the relationship between skin and hair.
- What kind of skin cancer is a cancer of a type of stem cell?
- For the skin and hair, describe one way in which they each protect the body against pathogens.
- If sweat glands are in the dermis, how is sweat released to the surface of the body?
- Explain why you think that physicians usually insist that patients remove any nail polish before having surgery.
- Describe generally how the brain gets touch information from the skin.
Attributions
Figure 10.8.1
Larissa Tattoo4039922685_46bf0bcfe5_c by Micael Faccio on Flickr is used under a CC BY 2.0 (https://creativecommons.org/licenses/by/2.0/) license.
Figure 10.8.2
Tattoo laser and cover-631211_1280 [photo] by Herco Roelofs on Pixabay is used under the Pixabay License (https://pixabay.com/ja/service/license/).
Figure 10.8.3
henna-tattoo-abu-dhabi by MarieFrance on Pixabay is used under the Pixabay License (https://pixabay.com/ja/service/license/).
References
Global News Staff. (2017, September 15). Health: ‘Toxic’ tattoo ink particles can travel to your lymph nodes: study. Globalnews.ca. https://globalnews.ca/news/3746925/tattoo-ink-safety-lymph-nodes/
Ipsos Reid. (2012). "Two in ten Canadians (22%), Americans (21%)
have a tattoo; One in ten tattooed Canadians (10%), Americans (11%) regret it" [News release]. Ipsos.com. https://www.ipsos.com/sites/default/files/publication/2012-01/5490.pdf
Rideout, K. (2010, July). Comparison of guidelines and regulatory frameworks for personal services establishments. National Collaborating Centre for Environmental Health. https://www.ncceh.ca/sites/default/files/PSE_Guidelines_Comparison_Table_July%202010.pdf
Schreiver, I., Hesse, B., Seim, C. et al. Synchrotron-based ν-XRF mapping and μ-FTIR microscopy enable to look into the fate and effects of tattoo pigments in human skin. Scientific Reports 7,11395. https://doi.org/10.1038/s41598-017-11721-z

Case Study: A Pain in the Foot
Sophia loves wearing high heels when she goes out at night, like the stiletto heels shown in Figure 11.1.1. She knows they are not the most practical shoes, but she likes how they look.
Lately, she has been experiencing pain in the balls of her feet — the area just behind the toes. Even when she trades her heels for comfortable sneakers, it still hurts when she stands or walks.
What could be going on? She searches online to try to find some answers. She finds a reputable source for foot pain information — a website from a professional organization of physicians that peer reviews the content by experts in the field. There, she reads about a condition called metatarsalgia, which produces pain in the ball of the foot that sounds very similar to what she is experiencing.
She learns that a common cause of metatarsalgia is the wearing of high heels. Shoes like this push the foot into an abnormal position, resulting in excessive pressure being placed on the ball of the foot. Looking at the photograph above (Figure 11.1.1), you can imagine how much of the woman’s body weight is focused on the ball of her foot, because of the shape of her high heels. If she were not wearing high heels, her weight would be more evenly distributed across her foot.
As she reads more about the hazards of high heels, Sophia learns that they can also cause foot deformities, such as hammertoes, bunions, and small cracks in bone called stress fractures. High heels may even contribute to the development of osteoarthritis of the knees at an early age.
These conditions caused by high heels are all problems of the skeletal system, which includes bones and connective tissues that hold bones together and cushion them at joints (such as the knee). The skeletal system supports the body’s weight and protects internal organs, but as you will learn as you read this chapter, it also carries out a variety of other important physiological functions.
At the end of the chapter, you will find out why high heels can cause these skeletal system problems, as well as the steps Sophia takes to recover from her foot pain and prevent long-term injury.
Chapter 11 Overview: Skeletal System
In this chapter, you will learn about the structure, functions, growth, repair, and disorders of the skeletal system. Specifically you will learn about:
- The components of the skeletal system, which includes bones, ligaments, and cartilage.
- The functions of the skeletal system, including supporting and giving shape to the body; protecting internal organs; facilitating movement; producing blood cells; helping maintain homeostasis; and producing endocrine hormones.
- The organization and functions of the two main divisions of the skeletal system: the axial skeletal system (which includes the skull, spine, and rib cage), and the appendicular skeletal system (which includes the limbs and girdles that attach the limbs to the axial skeleton).
- The tissues and cells that make up bones, along with their specific functions, which include making new bone, breaking down bone, producing blood cells, and regulating mineral homeostasis.
- The different types of bones in the skeletal system, based on shape and location.
- How bones grow, remodel, and repair themselves.
- The different types of joints between bones, where they are located, and the ways in which they allow different types of movement, depending on their structure.
- The causes, risk factors, and treatments for the two most common disorders of the skeletal system — osteoporosis and osteoarthritis.
As you read this chapter, think about the following questions:
- Sophia suspects she has a condition called metatarsalgia. This term is related to the term “metatarsals.” What are metatarsals, where are they located, and how do you think they are related to metatarsalgia?
- High heels can cause stress fractures, which are small cracks in bone that usually appear after repeated mechanical stress, instead of after a significant acute injury. What other condition described in this chapter involves a similar process?
- What are bunions and osteoarthritis of the knee? Why do you think they can be caused by wearing high heels?
Attribution
Figure 11.1.1
Heels by apostolos-vamvouras-_pdbqMcNWus [photo] by Apostolos Vamvouras on Unsplash is used under the Unsplash License (https://unsplash.com/license).
Reference
Mayo Clinic Staff. (n.p.). Metatarsalgia [online article]. MayoClinic.org. https://www.mayoclinic.org/diseases-conditions/metatarsalgia/symptoms-causes/syc-20354790
Created by: CK-12/Adapted by Christine Miller

Like Pushing a Humvee Uphill
You can tell by their faces that these airmen (Figure 4.8.1) are expending a lot of energy trying to push this Humvee up a slope. The men are participating in a competition that tests their brute strength against that of other teams. The Humvee weighs about 13 thousand pounds (about 5,897 kilograms), so it takes every ounce of energy they can muster to move it uphill against the force of gravity. Transport of some substances across a plasma membrane is a little like pushing a Humvee uphill — it can't be done without adding energy.
What Is Active Transport?
Some substances can pass into or out of a cell across the plasma membrane without any energy required because they are moving from an area of higher concentration to an area of lower concentration. This type of transport is called passive transport. Other substances require energy to cross a plasma membrane, often because they are moving from an area of lower concentration to an area of higher concentration, against the concentration gradient. This type of transport is called active transport. The energy for active transport comes from the energy-carrying molecule called ATP (adenosine triphosphate). Active transport may also require proteins called pumps, which are embedded in the plasma membrane. Two types of active transport are membrane pumps (such as the sodium-potassium pump) and vesicle transport.
The Sodium-Potassium Pump
The sodium-potassium pump is a mechanism of active transport that moves sodium ions out of the cell and potassium ions into the cells — in all the trillions of cells in the body! Both ions are moved from areas of lower to higher concentration, so energy is needed for this "uphill" process. The energy is provided by ATP. The sodium-potassium pump also requires carrier proteins. Carrier proteins bind with specific ions or molecules, and in doing so, they change shape. As carrier proteins change shape, they carry the ions or molecules across the membrane. Figure 4.8.2 shows in greater detail how the sodium-potassium pump works, as well as the specific roles played by carrier proteins in this process.
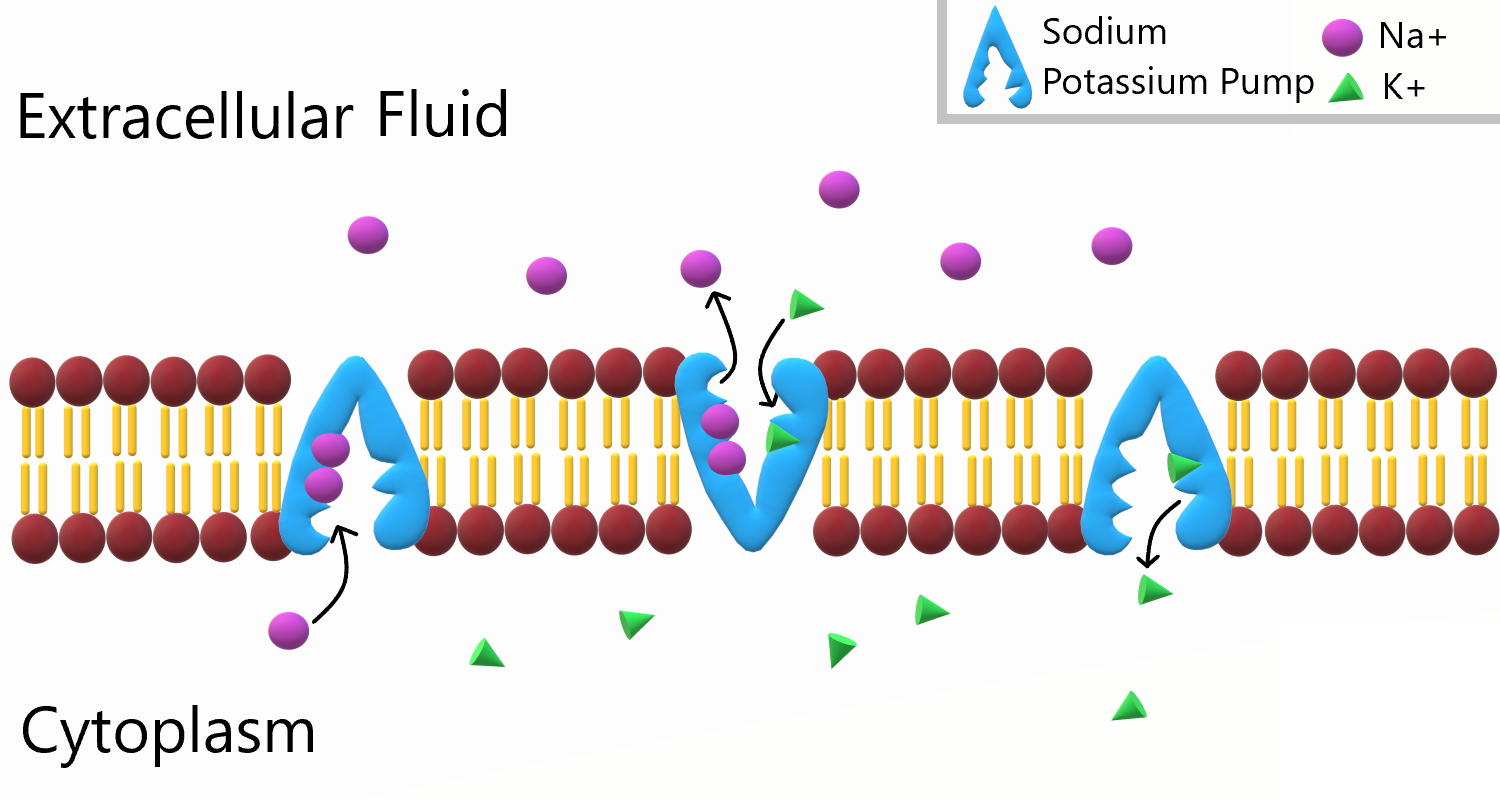
To appreciate the importance of the sodium-potassium pump, you need to know more about the roles of sodium and potassium in the body. Both are essential dietary minerals. You need to get them from the foods you eat. Both sodium and potassium are also electrolytes, which means they dissociate into ions (charged particles) in solution, allowing them to conduct electricity. Normal body functions require a very narrow range of concentrations of sodium and potassium ions in body fluids, both inside and outside of cells.
- Sodium is the principal ion in the fluid outside of cells. Normal sodium concentrations are about ten times higher outside of cells than inside of cells. To move sodium out of the cell is moving it against the concentration gradient
- Potassium is the principal ion in the fluid inside of cells. Normal potassium concentrations are about 30 times higher inside of cells than outside of cells. To move potassium into the cell is moving it against the concentration gradient.
These differences in concentration create an electrical and chemical gradient across the cell membrane, called the membrane potential. Tightly controlling the membrane potential is critical for vital body functions, including the transmission of nerve impulses and contraction of muscles. A large percentage of the body's energy goes to maintaining this potential across the membranes of its trillions of cells with the sodium-potassium pump.
Vesicle Transport
Some molecules, such as proteins, are too large to pass through the plasma membrane, regardless of their concentration inside and outside the cell. Very large molecules cross the plasma membrane with a different sort of help, called vesicle transport. Vesicle transport requires energy input from the cell, so it is also a form of active transport. There are two types of vesicle transport: endocytosis and exocytosis. Both types are shown in Figure 4.8.3.
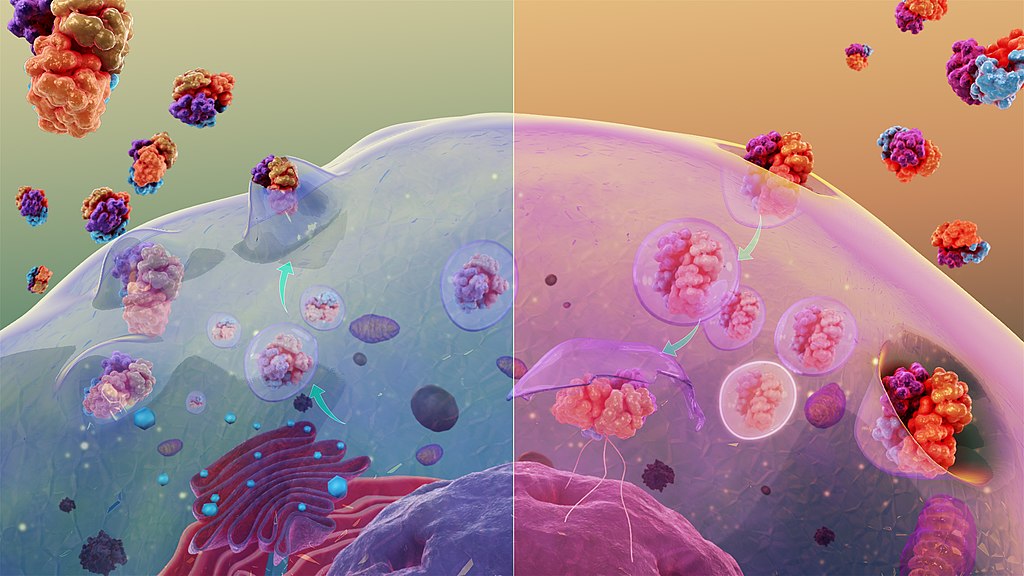
Endocytosis
Endocytosis is a type of vesicle transport that moves a substance into the cell. The plasma membrane completely engulfs the substance, a vesicle pinches off from the membrane, and the vesicle carries the substance into the cell. When an entire cell or other solid particle is engulfed, the process is called phagocytosis. When fluid is engulfed, the process is called pinocytosis.
Exocytosis
Exocytosis is a type of vesicle transport that moves a substance out of the cell (exo-, like "exit"). A vesicle containing the substance moves through the cytoplasm to the cell membrane. Because the vesicle membrane is a phospholipid bilayer like the plasma membrane, the vesicle membrane fuses with the cell membrane, and the substance is released outside the cell.
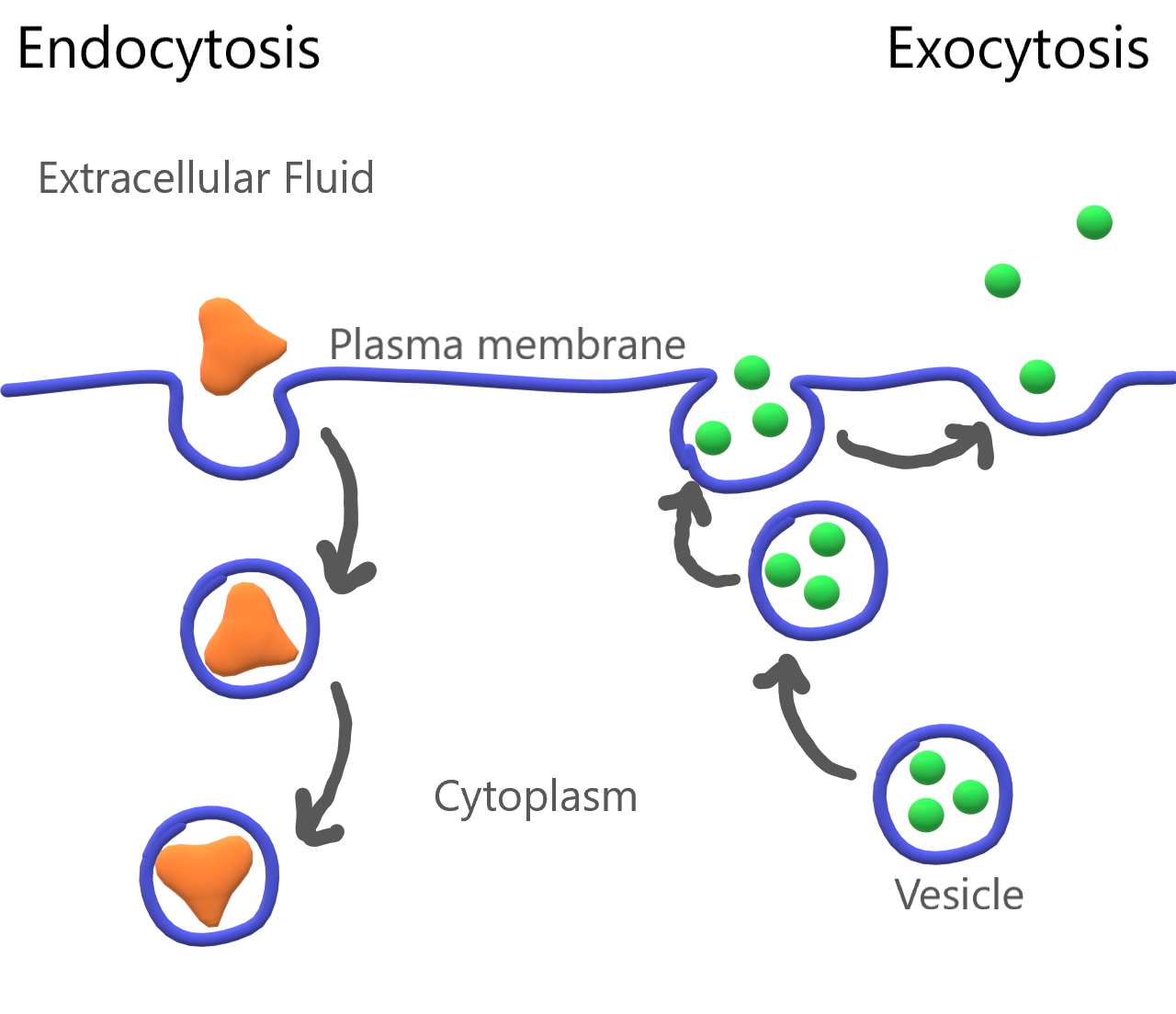
Feature: My Human Body
Maintaining the proper balance of sodium and potassium in body fluids by active transport is necessary for life itself, so it's no surprise that getting the right balance of sodium and potassium in the diet is important for good health. Imbalances may increase the risk of high blood pressure, heart disease, diabetes, and other disorders.
If you are like the majority of North Americans, sodium and potassium are out of balance in your diet. You are likely to consume too much sodium and too little potassium. Follow these guidelines to help ensure that these minerals are balanced in the foods you eat:
- Total sodium intake should be less than 2,300 mg/day. Most salt in the diet is found in processed foods, or added with a salt shaker. Stop adding salt and start checking food labels for sodium content. Foods considered low in sodium have less than 140 mg/serving (or 5 per cent daily value).
- Total potassium intake should be 4,700 mg/day. It's easy to add potassium to the diet by choosing the right foods — and there are plenty of choices! Most fruits and vegetables are high in potassium. Potatoes, bananas, oranges, apricots, plums, leafy greens, tomatoes, lima beans, and avocado are especially good sources. Other foods with substantial amounts of potassium are fish, meat, poultry, and whole grains. The collage below shows some of these potassium-rich foods.
Figure 4.8.5 Potassium power!
4.8 Summary
- Active transport requires energy to move substances across a plasma membrane, often because the substances are moving from an area of lower concentration to an area of higher concentration, or because of their large size. Two types of active transport are membrane pumps (such as the sodium-potassium pump) and vesicle transport.
- The sodium-potassium pump is a mechanism of active transport that moves sodium ions out of the cell and potassium ions into the cell against a concentration gradient, in order to maintain the proper concentrations of ions, both inside and outside the cell, and to thereby control membrane potential.
- Vesicle transport is a type of active transport that uses vesicles to move large molecules into or out of cells.
4.8 Review Questions
- Define active transport.
-
- What is the sodium-potassium pump? Why is it so important?
- The drawing below shows the fluid inside and outside of a cell. The dots represent molecules of a substance needed by the cell. Explain which type of transport — active or passive — is needed to move the molecules into the cell.
Figure 4.8.6 Use this image to answer question #4 - What are the similarities and differences between phagocytosis and pinocytosis?
- What is the functional significance of the shape change of the carrier protein in the sodium-potassium pump after the sodium ions bind?
- A potentially deadly poison derived from plants called ouabain blocks the sodium-potassium pump and prevents it from working. What do you think this does to the sodium and potassium balance in cells? Explain your answer.
4.8 Explore More
https://www.youtube.com/watch?v=Z_mXDvZQ6dU&feature=emb_logo
Neutrophil Phagocytosis - White Blood Cell Eats Staphylococcus Aureus Bacteria,
ImmiflexImmuneSystem, 2013.
https://www.youtube.com/watch?v=Ptmlvtei8hw
Cell Transport, The Amoeba Sisters, 2016.
Attributions
Figure 4.8.1
Humvee challenge by Airman 1st Class Collin Schmidt on Wikimedia Commons is released into the public domain (https://en.wikipedia.org/wiki/Public_domain).
Figure 4.8.2
Sodium Potassium Pump by Christine Miller is used under a CC BY 4.0 (https://creativecommons.org/licenses/by/4.0/) license.
Figure 4.8.3
Cytosis by Manu5 on Wikimedia Commons is used under a CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0) license.
Figure 4.8.4
Endocytosis and Exocytosis by Christine Miller is used under a CC BY 4.0 (https://creativecommons.org/licenses/by/4.0/) license.
Figure 4.8.5
- Canteloupes. Image Number K7355-11 by Scott Bauer/ USDA on Wikimedia Commons is in the public domain (https://en.wikipedia.org/wiki/Public_domain).
- Spinach by chiara conti on Unsplash is used under the Unsplash license (https://unsplash.com/license).
- Eleven long purple eggplants by JVRKPRASAD on Wikimedia commons is used under a CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0/deed.en) license.
- Bananas by Marco Antonio Victorino on Pexels is used under the Pexels license (https://www.pexels.com/license/).
- Potato picking by Nic D on Unsplash is used under the Unsplash license (https://unsplash.com/license).
- Maldives by Sebastian Pena Lambarri on Unsplash is used under the Unsplash license (https://unsplash.com/license).
Figure 4.8.6
Active Transport by Christine Miller is released into the public domain (https://en.wikipedia.org/wiki/Public_domain).
References
Amoeba Sisters. (2016, June 24). Cell transport [digital image]. YouTube. https://www.youtube.com/watch?v=Ptmlvtei8hw&feature=youtu.be
ImmiflexImmuneSystem. (2013). Neutrophil phagocytosis - White blood cell eats staphylococcus aureus bacteria. YouTube. https://www.youtube.com/watch?v=Z_mXDvZQ6dU
Mayo Clinic Staff. (n.d.). Diabetes [online]. MayoClinic.org. https://www.mayoclinic.org/diseases-conditions/diabetes/symptoms-causes/syc-20371444
Mayo Clinic Staff. (n.d.). High blood pressure (hypertension) [online]. MayoClinic.org. https://www.mayoclinic.org/diseases-conditions/high-blood-pressure/symptoms-causes/syc-20373410
Mayo Clinic Staff. (n.d.). Heart disease [online]. MayoClinic.org. https://www.mayoclinic.org/diseases-conditions/heart-disease/symptoms-causes/syc-20353118
Wikipedia contributors. (2020, June 19). Ouabain. In Wikipedia. https://en.wikipedia.org/w/index.php?title=Ouabain&oldid=963440756
Image shows a pictomicrograph of staphylococcus.
Divide and Split
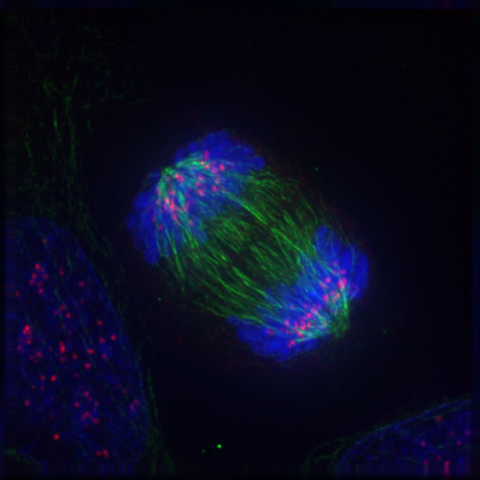
Can you guess what the colourful image in Figure 4.13.1 represents? It shows a eukaryotic cell during the process of cell division. In particular, the image shows the cell in a part of cell division called anaphase, where the DNA is being pulled to opposite ends of the cell. Normally, DNA is located in the nucleus of most human cells. The nucleus divides before the cell itself splits in two, and before the nucleus divides, the cell’s DNA is replicated (or copied). There must be two copies of the DNA so that each daughter cell will have a complete copy of the genetic material from the parent cell. How is the replicated DNA sorted and separated so that each daughter cell gets a complete set of the genetic material? To answer that question, you first need to know more about DNA and the forms it takes.
The Forms of DNA
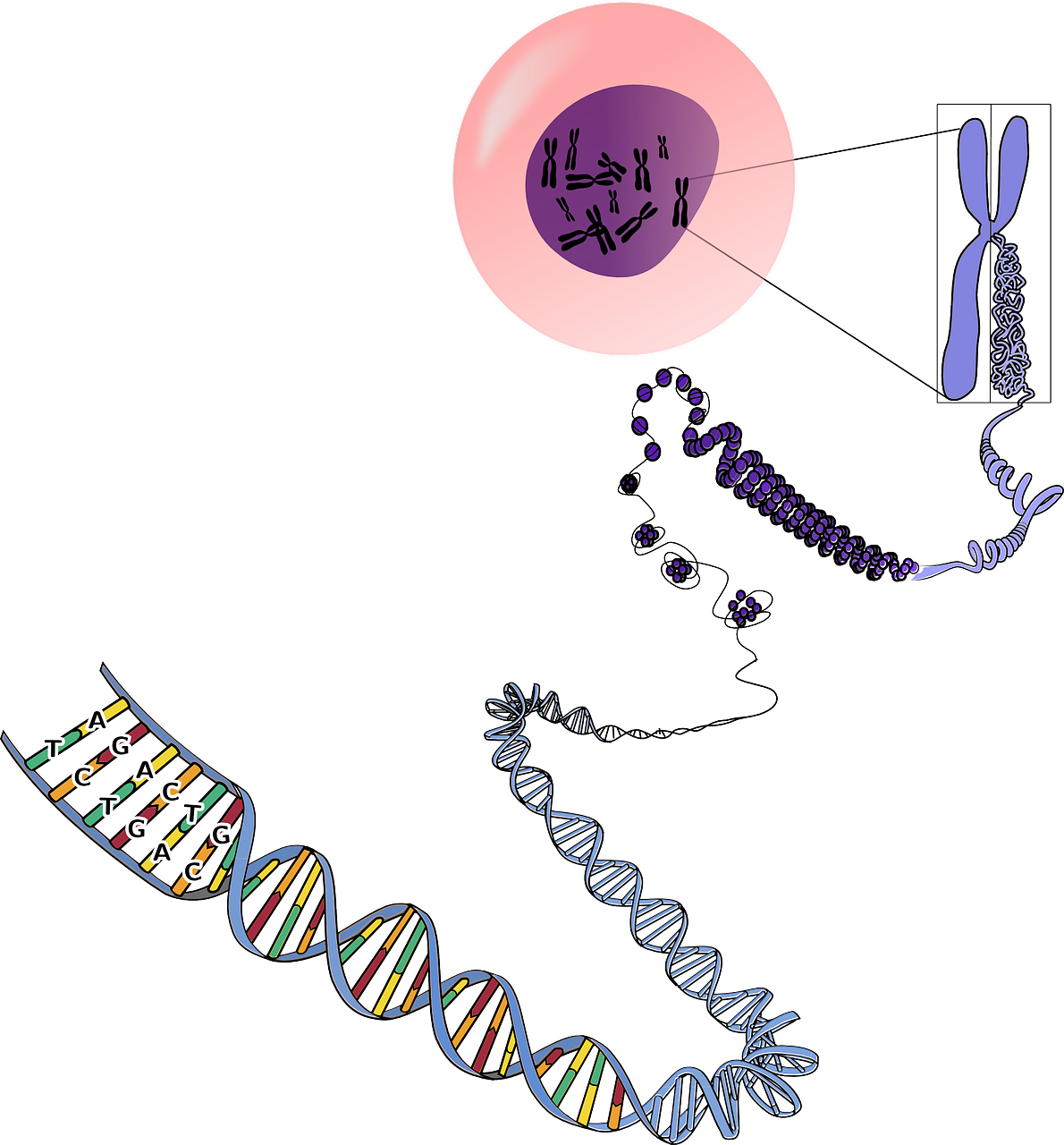
Except when a eukaryotic cell divides, its nuclear DNA exists as a grainy material called chromatin. Only once a cell is about to divide and its DNA has replicated does DNA condense and coil into the familiar X-shaped form of a chromosome, like the one shown below.
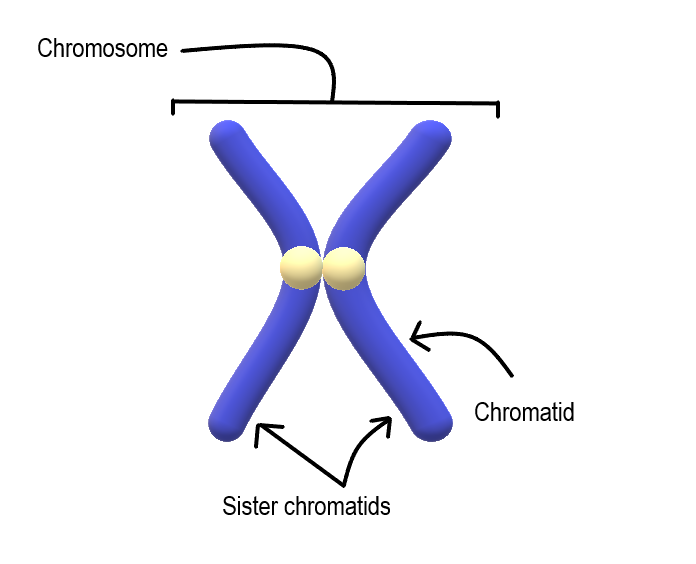
Most cells in the human body have two pairs of 23 different chromosomes, for a total of 46 chromosomes. Cells that have two pairs of chromosomes are called diploid. Because DNA has already replicated when it coils into a chromosome, each chromosome actually consists of two identical structures called sister chromatids. Sister chromatids are joined together at a region called a centromere.
Mitosis
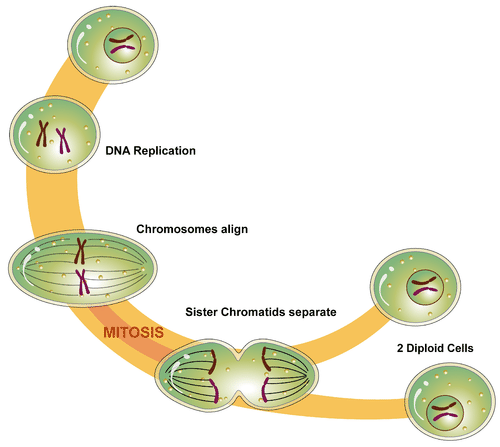
The process in which the nucleus of a eukaryotic cell divides is called mitosis. During mitosis, the two sister chromatids that make up each chromosome separate from each other and move to opposite poles of the cell. This is shown in the figure below.
Mitosis actually occurs in four phases. The phases are called prophase, metaphase, anaphase, and telophase.
Prophase
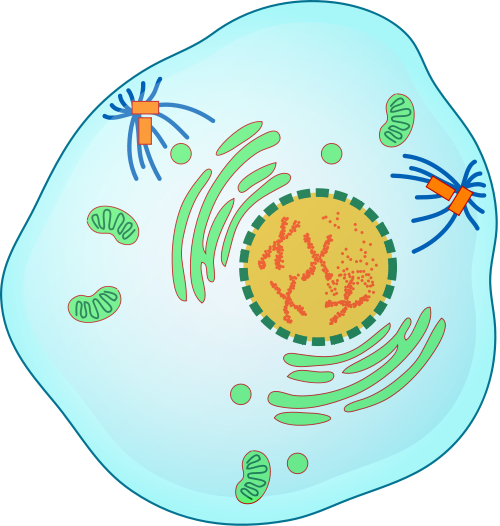
The first and longest phase of mitosis is prophase. During prophase, chromatin condenses into chromosomes, and the nuclear envelope (the membrane surrounding the nucleus) breaks down. In animal cells, the centrioles near the nucleus begin to separate and move to opposite poles of the cell. Centrioles are small organelles found only in eukaryotic cells. They help ensure that the new cells that form after cell division each contain a complete set of chromosomes. As the centrioles move apart, a spindle starts to form between them. The spindle consists of fibres made of microtubules.
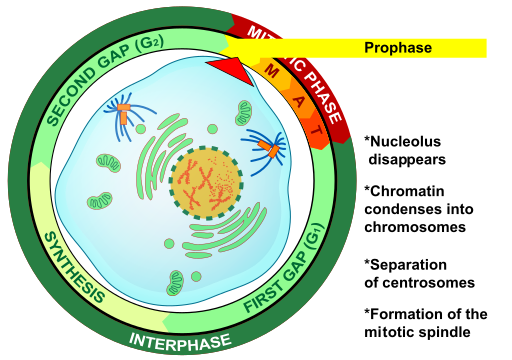
Metaphase
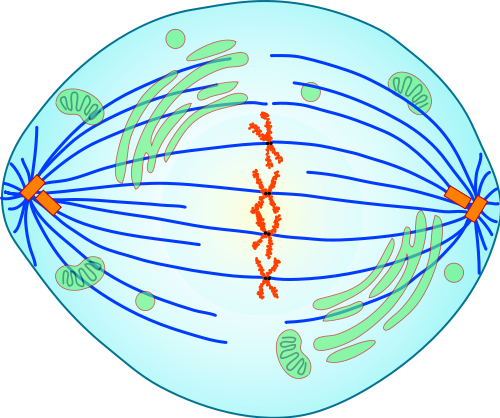
During metaphase, spindle fibres attach to the centromere of each pair of sister chromatids. As you can see in Figure 4.13.7, the sister chromatids line up at the equator (or center) of the cell. The spindle fibres ensure that sister chromatids will separate and go to different daughter cells when the cell divides.
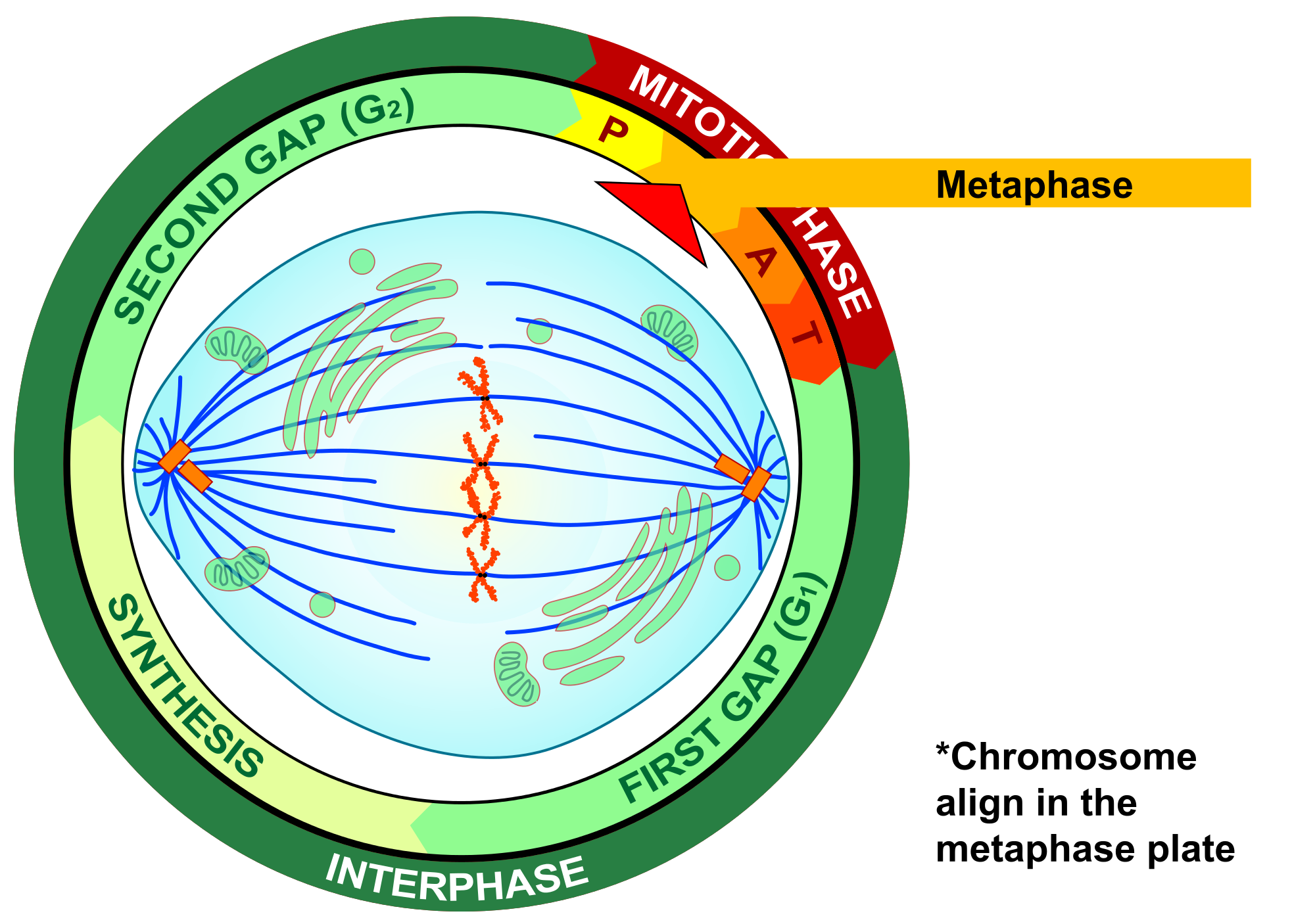
Anaphase
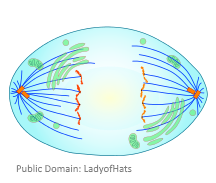
During anaphase, sister chromatids separate and the centromeres divide. The sister chromatids are pulled apart by the shortening of the spindle fibres. This is a little like reeling in a fish by shortening the fishing line. One sister chromatid moves to one pole of the cell, and the other sister chromatid moves to the opposite pole. At the end of anaphase, each pole of the cell has a complete set of chromosomes.
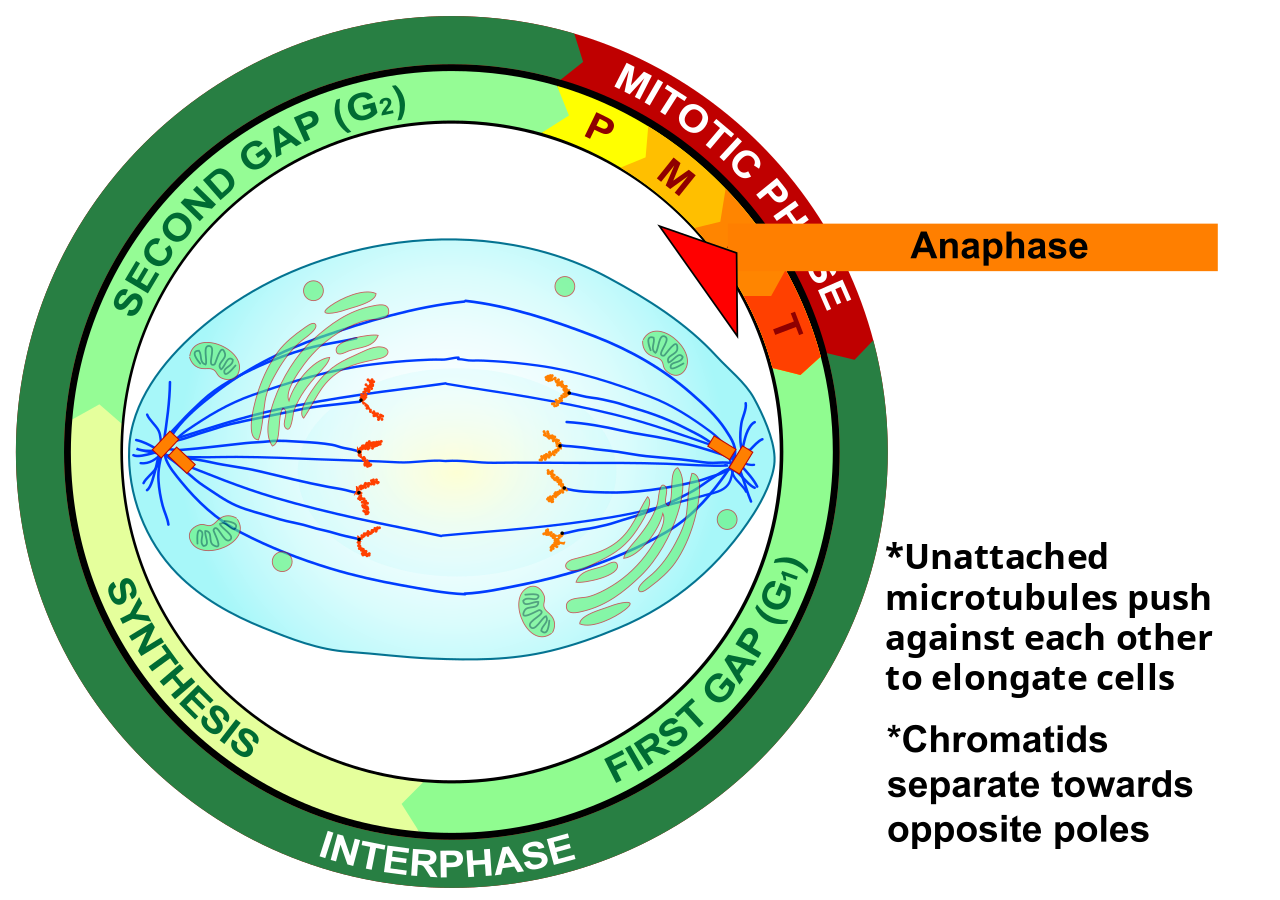
Telophase
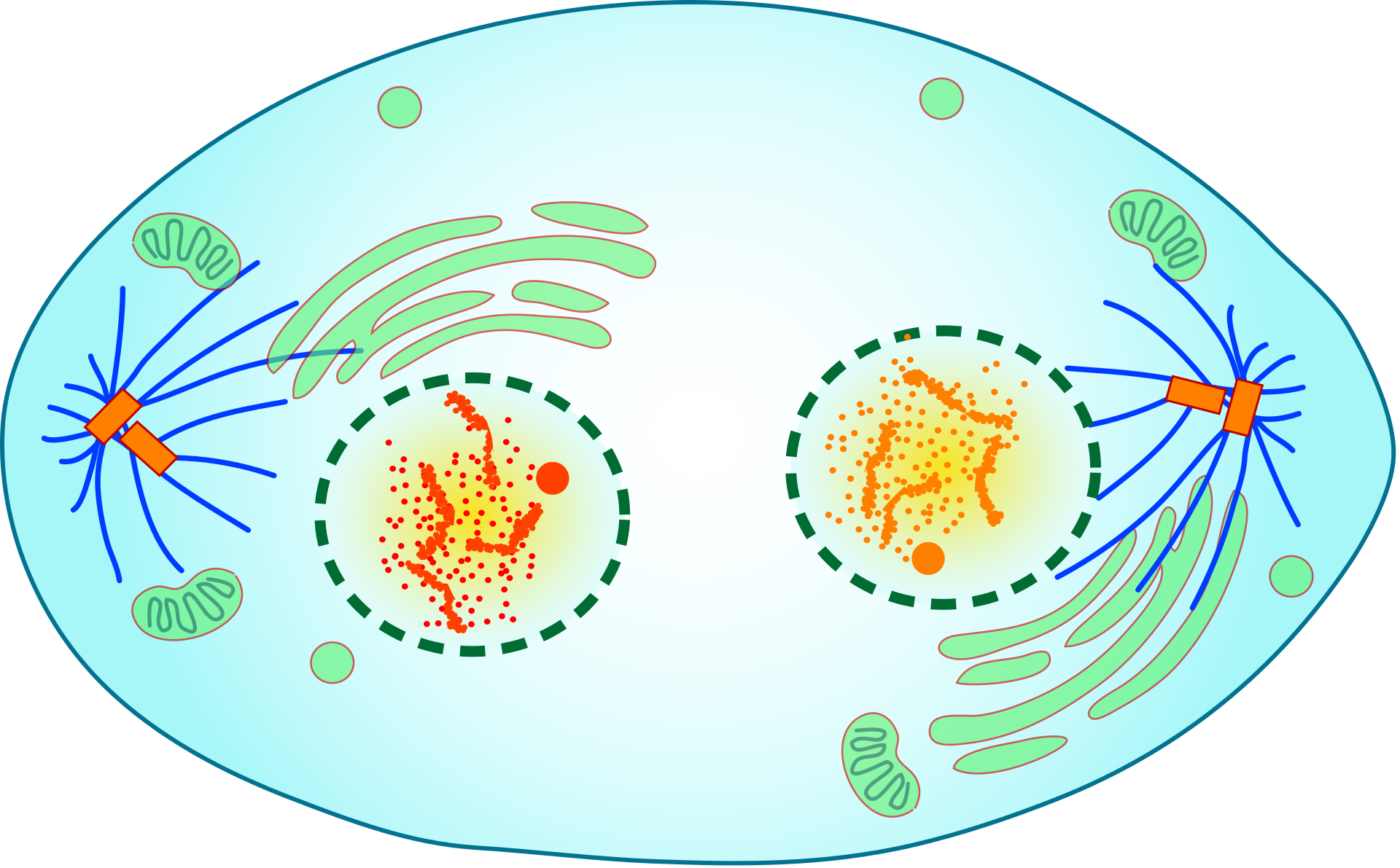
During telophase, the chromosomes begin to uncoil and form chromatin. This prepares the genetic material for directing the metabolic activities of the new cells. The spindle also breaks down, and new nuclear envelopes form.
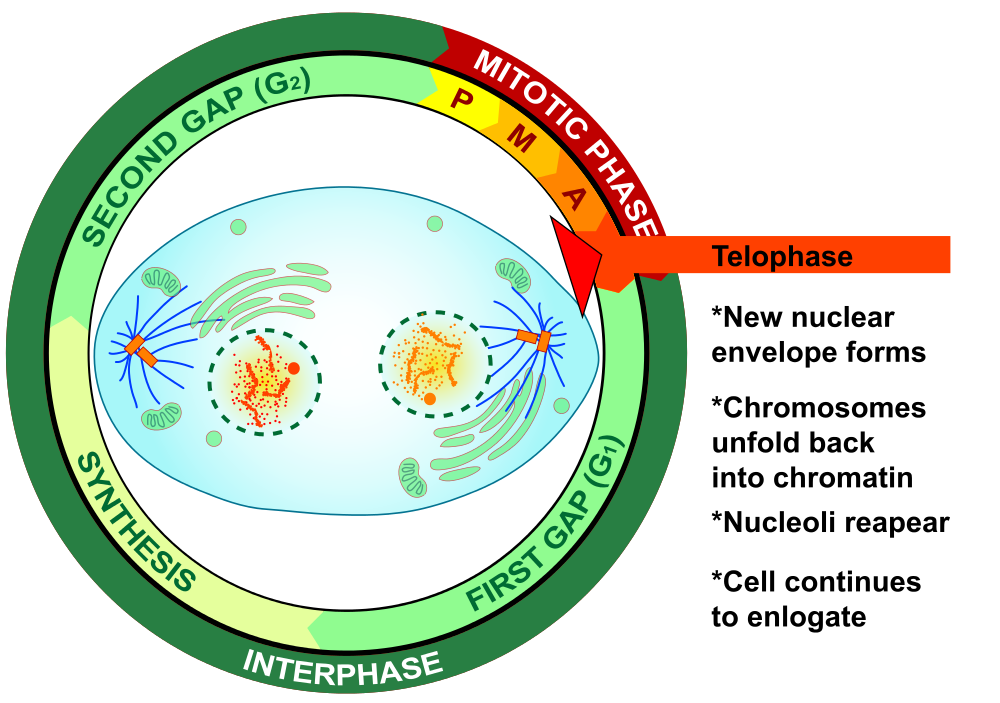
Cytokinesis
Cytokinesis is the final stage of cell division. During cytokinesis, the cytoplasm splits in two and the cell divides, as shown below. In animal cells, the plasma membrane of the parent cell pinches inward along the cell’s equator until two daughter cells form. Thus, the goal of mitosis and cytokinesis is now complete, because one parent cell has given rise to two daughter cells. The daughter cells have the same chromosomes as the parent cell.
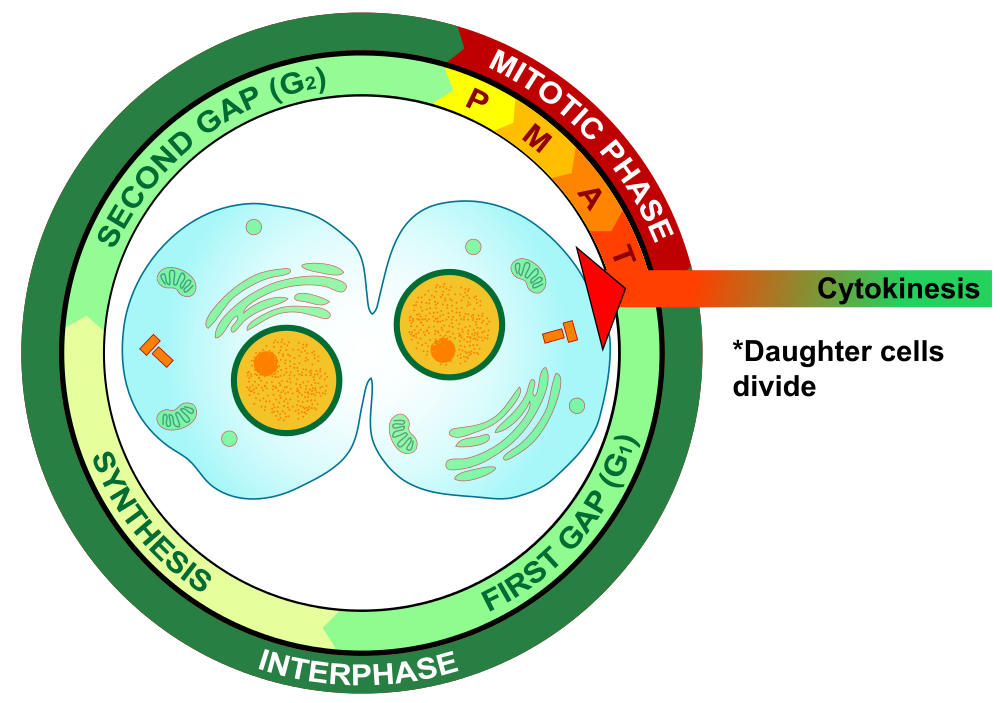
4.13 Summary
- Until a eukaryotic cell divides, its nuclear DNA exists as a grainy material called chromatin. After DNA replicates and the cell is about to divide, the DNA condenses and coils into the X-shaped form of a chromosome. Each chromosome actually consists of two sister chromatids, which are joined together at a centromere.
- Mitosis is the process during which the nucleus of a eukaryotic cell divides. During this process, sister chromatids separate from each other and move to opposite poles of the cell. This happens in four phases: prophase, metaphase, anaphase, and telophase.
- Cytokinesis is the final stage of cell division, during which the cytoplasm splits in two and two daughter cells form.
4.13 Review Questions
- Describe the different forms that DNA takes before and during cell division in a eukaryotic cell.
-
- Identify the four phases of mitosis in an animal cell, and summarize what happens during each phase.
- Order the diagrams of the stages of mitosis:
- Explain what happens during cytokinesis in an animal cell.
- What do you think would happen if the sister chromatids of one of the chromosomes did not separate during mitosis?
- True or False:
4.13 Explore More
https://www.youtube.com/watch?time_continue=3&v=C6hn3sA0ip0&feature=emb_logo
Mitosis, NDSU Virtual Cell Animations project (ndsuvirtualcell), 2012.
https://www.youtube.com/watch?time_continue=19&v=EA0qxhR2oOk&feature=emb_logo
Nondisjunction (Trisomy 21) - An Animated Tutorial, Kristen Koprowski, 2012.
Attributions
Figure 4.13.1
Anaphase_IF by Roy van Heesbeen on Wikimedia Commons is released into the public domain (https://en.wikipedia.org/wiki/Public_domain).
Figure 4.13.2
Chromosomes by OpenClipArt-Vectors on Pixabay is used under the Pixabay License (https://pixabay.com/service/license/).
Figure 4.13.3
Chromosome/ Chromatid/ Sister Chromatid by Christine Miller is released into the public domain (https://en.wikipedia.org/wiki/Public_domain).
Figure 4.13.4
Simple Mitosis by Mariana Ruiz Villarreal [LadyofHats] via CK-12 Foundation is used under a CC BY-NC 3.0 (https://creativecommons.org/licenses/by-nc/3.0/) license.
 ©CK-12 Foundation Licensed under
©CK-12 Foundation Licensed under ![]() • Terms of Use • Attribution
• Terms of Use • Attribution
Figure 4.13.5
Mitotic Prophase [tiny] by Mariana Ruiz Villarreal [LadyofHats] on Wikimedia Commons is released into the public domain (https://en.wikipedia.org/wiki/Public_domain).
Figure 4.13.6
Prophase Eukaryotic Mitosis by Mariana Ruiz Villarreal [LadyofHats] on Wikimedia Commons is released into the public domain (https://en.wikipedia.org/wiki/Public_domain).
Figure 4.13.7
Mitotic_Metaphase by Mariana Ruiz Villarreal [LadyofHats] on Wikimedia Commons is released into the public domain (https://en.wikipedia.org/wiki/Public_domain).
Figure 4.13.8
Metaphase Eukaryotic Mitosis by Mariana Ruiz Villarreal [LadyofHats] on Wikimedia Commons is released into the public domain (https://en.wikipedia.org/wiki/Public_domain).
Figure 4.13.9
Anaphase [adapted] by Mariana Ruiz Villarreal [LadyofHats] on Wikimedia Commons is released into the public domain (https://en.wikipedia.org/wiki/Public_domain).
Figure 4.13.10
Anaphase_eukaryotic_mitosis.svg by Mariana Ruiz Villarreal [LadyofHats] on Wikimedia Commons is released into the public domain (https://en.wikipedia.org/wiki/Public_domain).
Figure 4.13.11
Mitotic Telophase by Mariana Ruiz Villarreal [LadyofHats] on Wikimedia Commons is released into the public domain (https://en.wikipedia.org/wiki/Public_domain).
Figure 4.13.12
Telophase Eukaryotic Mitosis by Mariana Ruiz Villarreal [LadyofHats] on Wikimedia Commons is released into the public domain (https://en.wikipedia.org/wiki/Public_domain).
Figure 4.13.13
Mitotic Cytokinesis by Mariana Ruiz Villarreal [LadyofHats] on Wikimedia Commons is released into the public domain (https://en.wikipedia.org/wiki/Public_domain).
Figure 4.13.14
Cytokinesis Eukaryotic Mitosis by Mariana Ruiz Villarreal [LadyofHats] on Wikimedia Commons is released into the public domain (https://en.wikipedia.org/wiki/Public_domain).
References
Koprowski, K., Cabey, R. [Kristen Koprowski]. (2012). Nondisjunction (Trisomy 21) - An Animated Tutorial. YouTube. https://www.youtube.com/watch?v=EA0qxhR2oOk&feature=youtu.be
NDSU Virtual Cell Animations project [ndsuvirtualcell]. (2012). Mitosis. YouTube. https://www.youtube.com/watch?v=C6hn3sA0ip0&t=21s

