17.2 Introduction to the Immune System

Worm Attack!
Does the organism in Figure 17.2.1 look like a space alien? A scary creature from a nightmare? In fact, it’s a 1-cm long worm in the genus Schistosoma. It may invade and take up residence in the human body, causing a very serious illness known as schistosomiasis. The worm gains access to the human body while it is in a microscopic life stage. It enters through a hair follicle when the skin comes into contact with contaminated water. The worm then grows and matures inside the human organism, causing disease.
Host vs. Pathogen
The Schistosoma worm has a parasitic relationship with humans. In this type of relationship, one organism, called the parasite, lives on or in another organism, called the host. The parasite always benefits from the relationship, and the host is always harmed. The human host of the Schistosoma worm is clearly harmed by the parasite when it invades the host’s tissues. The urinary tract or intestines may be infected, and signs and symptoms may include abdominal pain, diarrhea, bloody stool, or blood in the urine. Those who have been infected for a long time may experience liver damage, kidney failure, infertility, or bladder cancer. In children, Schistosoma infection may cause poor growth and difficulty learning.
Like the Schistosoma worm, many other organisms can make us sick if they manage to enter our body. Any such agent that can cause disease is called a pathogen. Most pathogens are microorganisms, although some — such as the Schistosoma worm — are much larger. In addition to worms, common types of pathogens of human hosts include bacteria, viruses, fungi, and single-celled organisms called protists. You can see examples of each of these types of pathogens in Table 17.1.1. Fortunately for us, our immune system is able to keep most potential pathogens out of the body, or quickly destroy them if they do manage to get in. When you read this chapter, you’ll learn how your immune system usually keeps you safe from harm — including from scary creatures like the Schistosoma worm!
| Type of Pathogen | Description | Disease Caused | |
|---|---|---|---|
| Bacteria:
Example shown: Escherichia coli |
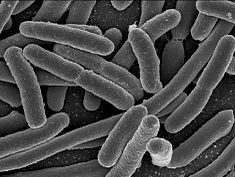 |
Single celled organisms without a nucleus | Strep throat, staph infections, tuberculosis, food poisoning, tetanus, pneumonia, syphillis |
| Viruses:
Example shown: Herpes simplex |
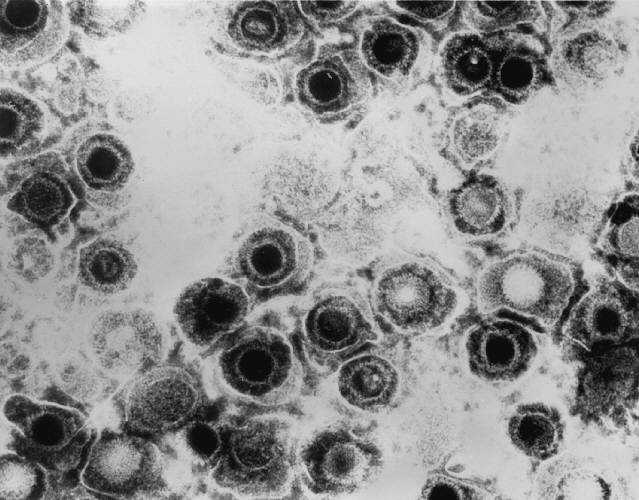 |
Non-living particles that reproduce by taking over living cells | Common cold, flu, genital herpes, cold sores, measles, AIDS, genital warts, chicken pox, small pox |
| Fungi:
Example shown: Death cap mushroom |
 |
Simple organisms, including mushrooms and yeast, that grow as single cells or thread-like filaments | Ringworm, athletes foot, tineas, candidias, histoplasmomis, mushroom poisoning |
| Protozoa:
Example shown: Giardia lamblia |
 |
Single celled organisms with a nucleus | Malaria, “traveller’s diarrhea”, giardiasis, typano somiasis (“sleeping sickness”) |
What is the Immune System?
The immune system is a host defense system. It comprises many biological structures —ranging from individual leukocytes to entire organs — as well as many complex biological processes. The function of the immune system is to protect the host from pathogens and other causes of disease, such as tumor (cancer) cells. To function properly, the immune system must be able to detect a wide variety of pathogens. It also must be able to distinguish the cells of pathogens from the host’s own cells, and also to distinguish cancerous or damaged host cells from healthy cells. In humans and most other vertebrates, the immune system consists of layered defenses that have increasing specificity for particular pathogens or tumor cells. The layered defenses of the human immune system are usually classified into two subsystems, called the innate immune system and the adaptive immune system.
Innate Immune System
The innate immune system (sometimes referred to as “non-specific defense”) provides very quick, but non-specific responses to pathogens. It responds the same way regardless of the type of pathogen that is attacking the host. It includes barriers — such as the skin and mucous membranes — that normally keep pathogens out of the body. It also includes general responses to pathogens that manage to breach these barriers, including chemicals and cells that attack the pathogens inside the human host. Certain leukocytes (white blood cells), for example, engulf and destroy pathogens they encounter in the process called phagocytosis, which is illustrated in Figure 17.2.2. Exposure to pathogens leads to an immediate maximal response from the innate immune system.
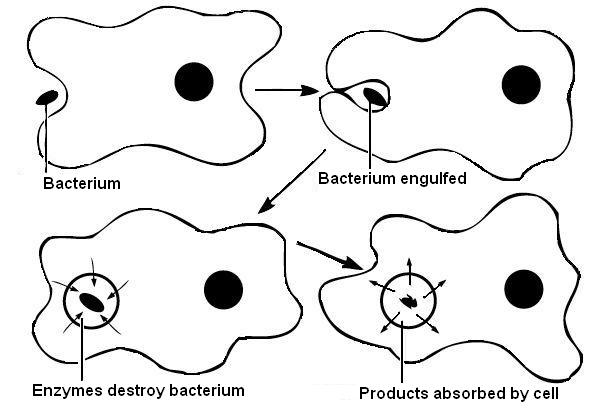
Watch the video below, “Neutrophil Phagocytosis – White Blood Cells Eats Staphylococcus Aureus Bacteria” by ImmiflexImmuneSystem, to see phagocytosis in action.
Neutrophil Phagocytosis – White Blood Cell Eats Staphylococcus Aureus Bacteria, ImmiflexImmuneSystem, 2013.
Adaptive Immune System
The adaptive immune system is activated if pathogens successfully enter the body and manage to evade the general defenses of the innate immune system. An adaptive response is specific to the particular type of pathogen that has invaded the body, or to cancerous cells. It takes longer to launch a specific attack, but once it is underway, its specificity makes it very effective. An adaptive response also usually leads to immunity. This is a state of resistance to a specific pathogen, due to the adaptive immune system’s ability to “remember” the pathogen and immediately mount a strong attack tailored to that particular pathogen if it invades again in the future.
Self vs. Non-Self
Both innate and adaptive immune responses depend on the immune system’s ability to distinguish between self- and non-self molecules. Self molecules are those components of an organism’s body that can be distinguished from foreign substances by the immune system. Virtually all body cells have surface proteins that are part of a complex called major histocompatibility complex (MHC). These proteins are one way the immune system recognizes body cells as self. Non-self proteins, in contrast, are recognized as foreign, because they are different from self proteins.
Antigens and Antibodies
Many non-self molecules comprise a class of compounds called antigens. Antigens, which are usually proteins, bind to specific receptors on immune system cells and elicit an adaptive immune response. Some adaptive immune system cells (B cells) respond to foreign antigens by producing antibodies. An antibody is a molecule that precisely matches and binds to a specific antigen. This may target the antigen (and the pathogen displaying it) for destruction by other immune cells.
Antigens on the surface of pathogens are how the adaptive immune system recognizes specific pathogens. Antigen specificity allows for the generation of responses tailored to the specific pathogen. It is also how the adaptive immune system ”remembers” the same pathogen in the future.
Immune Surveillance
Another important role of the immune system is to identify and eliminate tumor cells. This is called immune surveillance. The transformed cells of tumors express antigens that are not found on normal body cells. The main response of the immune system to tumor cells is to destroy them. This is carried out primarily by aptly-named killer T cells of the adaptive immune system.
Lymphatic System
The lymphatic system is a human organ system that is a vital part of the adaptive immune system. It is also part of the cardiovascular system and plays a major role in the digestive system (see section 17.3 Lymphatic System). The major structures of the lymphatic system are shown in Figure 17.2.3 .
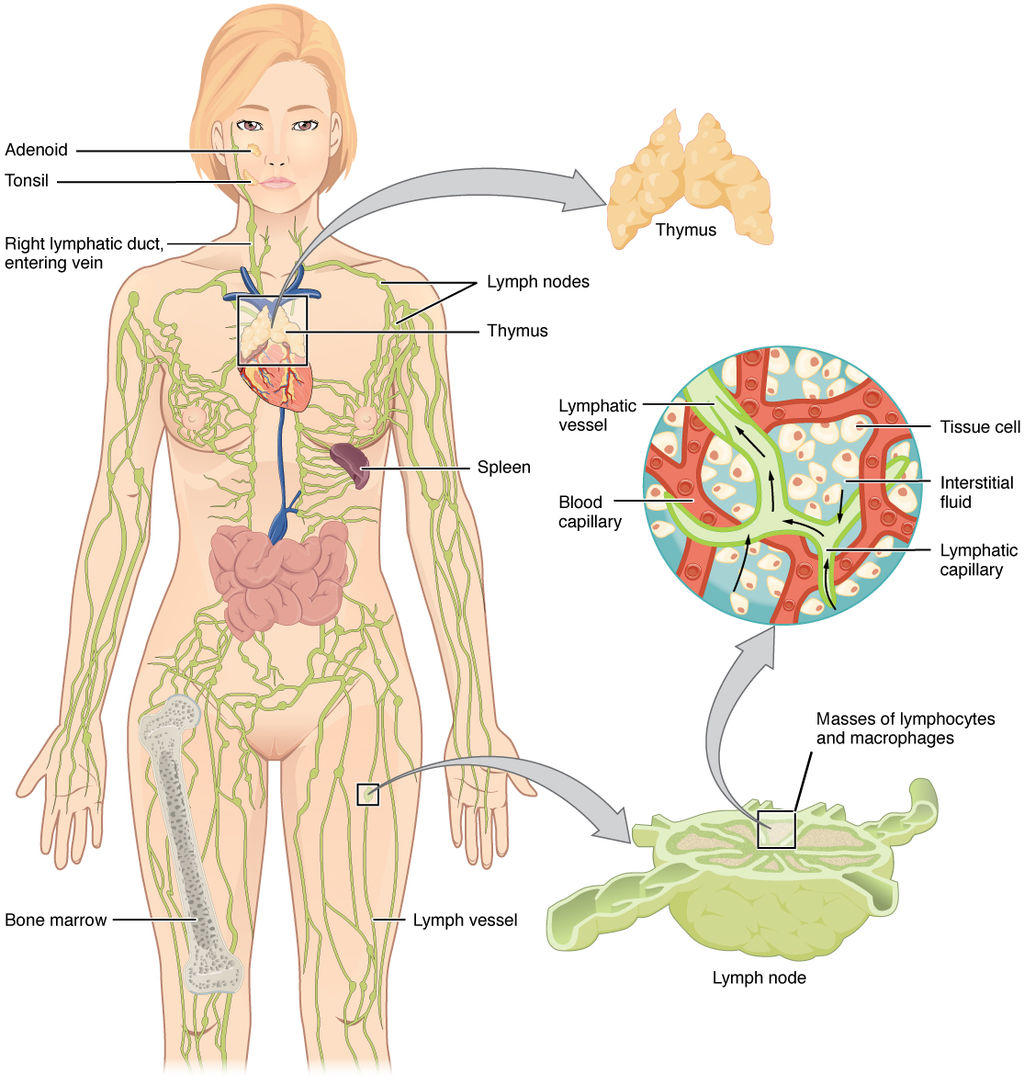
The lymphatic system consists of several lymphatic organs and a body-wide network of lymphatic vessels that transport the fluid called lymph. Lymph is essentially blood plasma that has leaked from capillaries into tissue spaces. It includes many leukocytes, especially lymphocytes, which are the major cells of the lymphatic system. Like other leukocytes, lymphocytes defend the body. There are several different types of lymphocytes that fight pathogens or cancer cells as part of the adaptive immune system.
Major lymphatic organs include the thymus and bone marrow. Their function is to form and/or mature lymphocytes. Other lymphatic organs include the spleen, tonsils, and lymph nodes, which are small clumps of lymphoid tissue clustered along lymphatic vessels. These other lymphatic organs harbor mature lymphocytes and filter lymph. They are sites where pathogens collect, and adaptive immune responses generally begin.
Neuroimmune System vs. Peripheral Immune System
The brain and spinal cord are normally protected from pathogens in the blood by the selectively permeable blood-brain and blood-spinal cord barriers. These barriers are part of the neuroimmune system. The neuroimmune system has traditionally been considered distinct from the rest of the immune system, which is called the peripheral immune system — although that view may be changing. Unlike the peripheral system, in which leukocytes are the main cells, the main cells of the neuroimmune system are thought to be nervous system cells called neuroglia. These cells can recognize and respond to pathogens, debris, and other potential dangers. Types of neuroglia involved in neuroimmune responses include microglial cells and astrocytes.
- Microglial cells are among the most prominent types of neuroglia in the brain. One of their main functions is to phagocytize cellular debris that remains when neurons die. Microglial cells also “prune” obsolete synapses between neurons.
- Astrocytes are neuroglia that have a different immune function. They allow certain immune cells from the peripheral immune system to cross into the brain via the blood-brain barrier to target both pathogens and damaged nervous tissue.
Feature: Human Biology in the News
“They’ll have to rewrite the textbooks!”
That sort of response to a scientific discovery is sure to attract media attention, and it did. It’s what Kevin Lee, a neuroscientist at the University of Virginia, said in 2016 when his colleagues told him they had discovered human anatomical structures that had never before been detected. The structures were tiny lymphatic vessels in the meningeal layers surrounding the brain.
How these lymphatic vessels could have gone unnoticed when all human body systems have been studied so completely is amazing in its own right. The suggested implications of the discovery are equally amazing:
- The presence of these lymphatic vessels means that the brain is directly connected to the peripheral immune system, presumably allowing a close association between the human brain and human pathogens. This suggests an entirely new avenue by which humans and their pathogens may have influenced each other’s evolution. The researchers speculate that our pathogens even may have influenced the evolution of our social behaviors.
- The researchers think there will also be many medical applications of their discovery. For example, the newly discovered lymphatic vessels may play a major role in neurological diseases that have an immune component, such as multiple sclerosis. The discovery might also affect how conditions such as autism spectrum disorders and schizophrenia are treated.
17.2 Summary
- Any agent that can cause disease is called a pathogen. Most human pathogens are microorganisms, such as bacteria and viruses. The immune system is the body system that defends the human host from pathogens and cancerous cells.
- The innate immune system is a subset of the immune system that provides very quick, but non-specific responses to pathogens. It includes multiple types of barriers to pathogens, leukocytes that phagocytize pathogens, and several other general responses.
- The adaptive immune system is a subset of the immune system that provides specific responses tailored to particular pathogens. It takes longer to put into effect, but it may lead to immunity to the pathogens.
- Both innate and adaptive immune responses depend on the immune system’s ability to distinguish between self and non-self molecules. Most body cells have major histocompatibility complex (MHC) proteins that identify them as self. Pathogens and tumor cells have non-self antigens that the immune system recognizes as foreign.
- Antigens are proteins that bind to specific receptors on immune system cells and elicit an adaptive immune response. Generally, they are non-self molecules on pathogens or infected cells. Some immune cells (B cells) respond to foreign antigens by producing antibodies that bind with antigens and target pathogens for destruction.
- Tumor surveillance is an important role of the immune system. Killer T cells of the adaptive immune system find and destroy tumor cells, which they can identify from their abnormal antigens.
- The lymphatic system is a human organ system vital to the adaptive immune system. It consists of several organs and a system of vessels that transport lymph. The main immune function of the lymphatic system is to produce, mature, and circulate lymphocytes, which are the main cells in the adaptive immune system.
- The neuroimmune system that protects the central nervous system is thought to be distinct from the peripheral immune system that protects the rest of the human body. The blood-brain and blood-spinal cord barriers are one type of protection for the neuroimmune system. Neuroglia also play role in this system, for example, by carrying out phagocytosis.
17.2 Review Questions
-
- What is a pathogen?
- State the purpose of the immune system.
- Compare and contrast the innate and adaptive immune systems.
- Explain how the immune system distinguishes self molecules from non-self molecules.
- What are antigens?
- Define tumor surveillance.
- Briefly describe the lymphatic system and its role in immune function.
- Identify the neuroimmune system.
- What does it mean that the immune system is not just composed of organs?
- Why is the immune system considered “layered?”
17.2 Explore More
The Antibiotic Apocalypse Explained, Kurzgesagt – In a Nutshell, 2016.
Overview of the Immune System, Handwritten Tutorials, 2011.
The surprising reason you feel awful when you’re sick – Marco A. Sotomayor, TED-Ed, 2016.
Attributions
Figure 17.1.1
Schistosome Parasite by Bruce Wetzel and Harry Schaefer (Photographers) from the National Cancer Institute, Visuals online is in the public domain (https://en.wikipedia.org/wiki/Public_domain).
Figure 17.1.2
Phagocytosis by Rlawson at en.wikibooks on Wikimedia Commons is used under a CC BY SA 3.0 (https://creativecommons.org/licenses/by-sa/3.0/deed.en) license. (Transferred from en.wikibooks to Commons by User:Adrignola.)
Figure 17.1.3
2201_Anatomy_of_the_Lymphatic_System by OpenStax College on Wikimedia Commons is used under a CC BY 3.0 (https://creativecommons.org/licenses/by/3.0) license.
Table 17.1.1
- EscherichiaColi NIAID [photo] by Rocky Mountain Laboratories, NIH National Institute of Allergy and Infectious Diseases (NIAID) on Wikimedia Commons is in the public domain (https://en.wikipedia.org/wiki/Public_domain).
- Herpes simplex virus TEM B82-0474 lores by Dr. Erskine Palmer/ CDC Public Health Image Library (PHIL) on Wikimedia Commons is in the public domain (https://en.wikipedia.org/wiki/Public_domain).
- Red death cap mushroom by Rosendahl on Wikimedia Commons is in the public domain (https://en.wikipedia.org/wiki/Public_domain). (Transferred from Pixnio by Fæ.)
- Scanning electron micrograph (SEM) of Giardia lamblia by Janice Haney Carr/ CDC, Public Health Image Library (PHIL) Photo ID# 8698 is in the public domain (https://en.wikipedia.org/wiki/Public_domain).
References
Barney, J. (2016, March 21). They’ll have to rewrite the textbooks [online article]. Illimitable – Discovery. UVA Today/ University of Virginia. https://news.virginia.edu/illimitable/discovery/theyll-have-rewrite-textbooks
Betts, J. G., Young, K.A., Wise, J.A., Johnson, E., Poe, B., Kruse, D.H., Korol, O., Johnson, J.E., Womble, M., DeSaix, P. (2013, June 19). Figure 21.2 Anatomy of the lymphatic system [digital image]. In Anatomy and Physiology (Section 21.1). OpenStax. https://openstax.org/books/anatomy-and-physiology/pages/21-1-anatomy-of-the-lymphatic-and-immune-systems
Handwritten Tutorials. (2011, October 25). Overview of the immune system. YouTube. https://www.youtube.com/watch?v=Nw27_jMWw10&feature=youtu.be
ImmiflexImmuneSystem. (2013). Neutrophil phagocytosis – White blood cell eats staphylococcus aureus bacteria. YouTube. https://www.youtube.com/watch?v=Z_mXDvZQ6dU
Kurzgesagt – In a Nutshell. (2016, March 16). The antibiotic apocalypse explained. YouTube. https://www.youtube.com/watch?v=xZbcwi7SfZE&feature=youtu.be
Louveau, A., Smirnov, I., Keyes, T. J., Eccles, J. D., Rouhani, S. J., Peske, J. D., Derecki, N. C., Castle, D., Mandell, J. W., Lee, K. S., Harris, T. H., & Kipnis, J. (2015). Structural and functional features of central nervous system lymphatic vessels. Nature, 523(7560), 337–341. https://doi.org/10.1038/nature14432
Mayo Clinic Staff. (n.d.). Autism spectrum disorder [online article]. MayoClinic.org. https://www.mayoclinic.org/diseases-conditions/autism-spectrum-disorder/symptoms-causes/syc-20352928
Mayo Clinic Staff. (n.d.). Multiple sclerosis [online article]. MayoClinic.org. https://www.mayoclinic.org/diseases-conditions/multiple-sclerosis/symptoms-causes/syc-20350269
Mayo Clinic Staff. (n.d.). Schizophrenia [online article]. MayoClinic.org. https://www.mayoclinic.org/diseases-conditions/schizophrenia/symptoms-causes/syc-20354443
TED-Ed. (2016, April 19). The surprising reason you feel awful when you’re sick – Marco A. Sotomayor. YouTube. https://www.youtube.com/watch?v=gVdY9KXF_Sg&feature=youtu.be
Created by CK-12 Foundation/Adapted by Christine Miller

Case Study: Hormonal Havoc
Eighteen-year-old Gabrielle checks her calendar. It has been 42 days since her last menstrual period, which is two weeks longer than the length of the average woman’s menstrual cycle. Although many women would suspect pregnancy if their period was late, Gabrielle has not been sexually active. She is not even sure she is “late,” because her period has never been regular. Ever since her first period when she was 13 years old, her cycle lengths have varied greatly, and there are months where she does not get a period at all. Her mother told her that a girl’s period is often irregular when it first starts, but five years later, Gabrielle’s still has not become regular. She decides to go to the student health center on her college campus to get it checked out.
The doctor asks her about the timing of her menstrual periods and performs a pelvic exam. She also notices that Gabrielle is overweight, has acne, and excess facial hair. As she explains to Gabrielle, while these physical characteristics can be perfectly normal, in combination with an irregular period, they can be signs of a disorder of the endocrine — or hormonal — system called polycystic ovary syndrome (PCOS).
In order to check for PCOS, the doctor refers Gabrielle for a pelvic ultrasound and sends her to the lab to get blood work done. When her lab results come back, Gabrielle learns that her levels of androgens (a group of hormones) are high, and so is her blood glucose (sugar). The ultrasound showed that she has multiple fluid-filled sacs (known as cysts) in her ovaries. Based on Gabrielle’s symptoms and test results, the doctor tells her that she does indeed have PCOS.
PCOS is common in young women. It is estimated that 6-10% women of childbearing age have PCOS — as many as 1.4 million women in in Canada. You may know someone with PCOS, or you may have it yourself.
Read the rest of this chapter to learn about the glands and hormones of the endocrine system, their functions, how they are regulated, and the disorders — such as PCOS — that can arise when hormones are not regulated properly. At the end of the chapter, you will learn more about PCOS, its possible long-term consequences (including fertility problems and diabetes), and how these negative outcomes can sometimes be prevented with lifestyle changes and medications.
Chapter Overview: Endocrine System
In this chapter, you will learn about the endocrine system, a system of glands that secrete hormones that regulate many of the body’s functions. Specifically, you will learn about:
- The glands that make up the endocrine system, and how hormones act as chemical messengers in the body.
- The general types of endocrine system disorders.
- The types of endocrine hormones — including steroid hormones (such as sex hormones) and non-steroid hormones (such as insulin) — and how they affect the functions of their target cells by binding to different types of receptor proteins.
- How the levels of hormones are regulated mostly through negative, but sometimes through positive, feedback loops.
- The master gland of the endocrine system, the pituitary gland, which controls other parts of the endocrine system through the hormones that it secretes, as well as how the pituitary itself is regulated by hormones secreted from the hypothalamus of the brain.
- The thyroid gland and its hormones — which regulate processes including metabolism and calcium homeostasis — how the thyroid is regulated, and the disorders that can occur when there are problems in thyroid hormone regulation (such as hyperthyroidism and hypothyroidism).
- The adrenal glands, which secrete hormones that regulate processes such as metabolism, electrolyte balance, responses to stress, and reproductive functions, and the disorders that can occur when there are problems in adrenal hormone regulation, such as Cushing’s syndrome and Addison’s disease.
- The pancreas, which secretes hormones that regulate blood glucose levels (such as insulin), and disorders of the pancreas and its hormones, including diabetes.
Later chapters in this book will discuss the glands and hormones involved in the reproductive and immune systems in more depth.
As you read this chapter, think about the following questions:
- Why can hormones have such broad range effects on the body, as we see in PCOS?
- Which hormones normally regulate blood glucose? How is this related to diabetes?
- What are androgens? How do you think their functions relate to some of the symptoms that Gabrielle is experiencing?
Attribution
Figure 9.1.1
Chapter 9 case study [photo] by niklas_hamann on Unsplash is used under the Unsplash License (https://unsplash.com/license).
Reference
Mayo Clinic Staff. (n.d.). Polycystic ovary syndrome [online article]. MayoClinic.com. https://www.mayoclinic.org/diseases-conditions/pcos/multimedia/polycystic-ovary-syndrome/img-20007768
Created by CK-12 Foundation/Adapted by Christine Miller

Doing the ‘Fly
The swimmer in the Figure 13.3.1 photo is doing the butterfly stroke, a swimming style that requires the swimmer to carefully control his breathing so it is coordinated with his swimming movements. Breathing is the process of moving air into and out of the lungs, which are the organs in which gas exchange takes place between the atmosphere and the body. Breathing is also called ventilation, and it is one of two parts of the life-sustaining process of respiration. The other part is gas exchange. Before you can understand how breathing is controlled, you need to know how breathing occurs.
How Breathing Occurs
Breathing is a two-step process that includes drawing air into the lungs, or inhaling, and letting air out of the lungs, or exhaling. Both processes are illustrated in Figure 13.3.2.
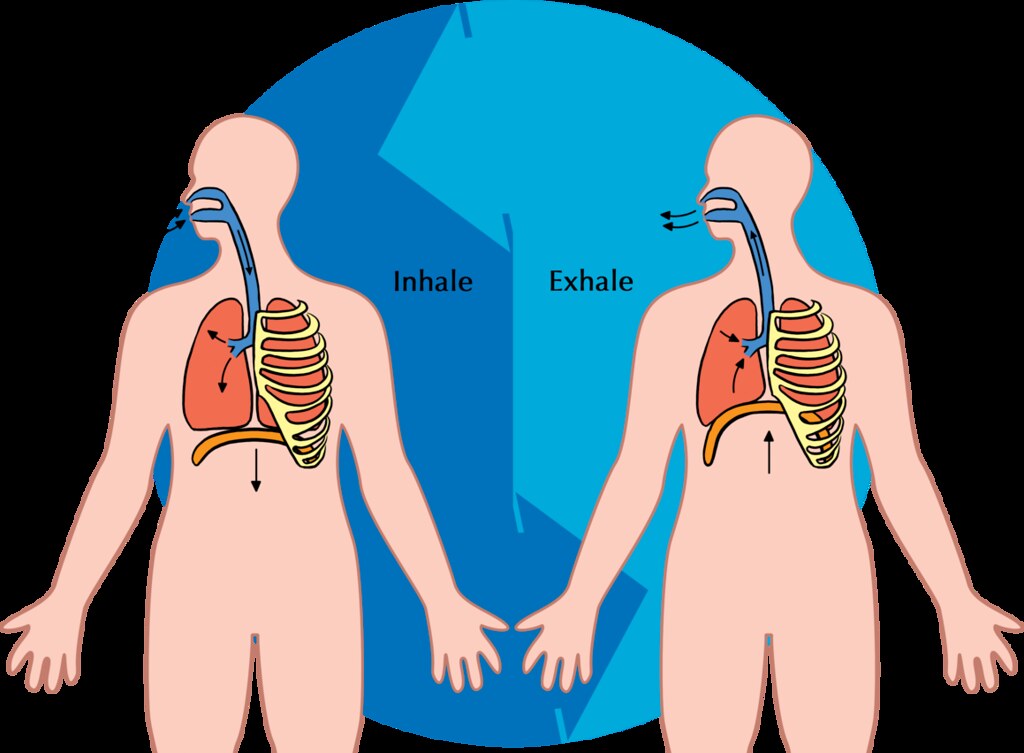
Inhaling
Inhaling is an active process that results mainly from contraction of a muscle called the diaphragm, shown in Figure 13.3.2. The diaphragm is a large, dome-shaped muscle below the lungs that separates the thoracic (chest) and abdominal cavities. When the diaphragm contracts it moves down causing the thoracic cavity to expand, and the contents of the abdomen to be pushed downward. Other muscles — such as intercostal muscles between the ribs — also contribute to the process of inhalation, especially when inhalation is forced, as when taking a deep breath. These muscles help increase thoracic volume by expanding the ribs outward. The increase in thoracic volume creates a decrease in thoracic air pressure. With the chest expanded, there is lower air pressure inside the lungs than outside the body, so outside air flows into the lungs via the respiratory tract according the the pressure gradient (high pressure flows to lower pressure).
Exhaling
Exhaling involves the opposite series of events. The diaphragm relaxes, so it moves upward and decreases the volume of the thorax. Air pressure inside the lungs increases, so it is higher than the air pressure outside the lungs. Exhalation, unlike inhalation, is typically a passive process that occurs mainly due to the elasticity of the lungs. With the change in air pressure, the lungs contract to their pre-inflated size, forcing out the air they contain in the process. Air flows out of the lungs, similar to the way air rushes out of a balloon when it is released. If exhalation is forced, internal intercostal and abdominal muscles may help move the air out of the lungs.
Control of Breathing
Breathing is one of the few vital bodily functions that can be controlled consciously, as well as unconsciously. Think about using your breath to blow up a balloon. You take a long, deep breath, and then you exhale the air as forcibly as you can into the balloon. Both the inhalation and exhalation are consciously controlled.
Conscious Control of Breathing
You can control your breathing by holding your breath, slowing your breathing, or hyperventilating, which is breathing more quickly and shallowly than necessary. You can also exhale or inhale more forcefully or deeply than usual. Conscious control of breathing is common in many activities besides blowing up balloons, including swimming, speech training, singing, playing many different musical instruments (Figure 13.3.3), and doing yoga, to name just a few.

There are limits on the conscious control of breathing. For example, it is not possible for a healthy person to voluntarily stop breathing indefinitely. Before long, there is an irrepressible urge to breathe. If you were able to stop breathing for a long enough time, you would lose consciousness. The same thing would happen if you were to hyperventilate for too long. Once you lose consciousness so you can no longer exert conscious control over your breathing, involuntary control of breathing takes over.
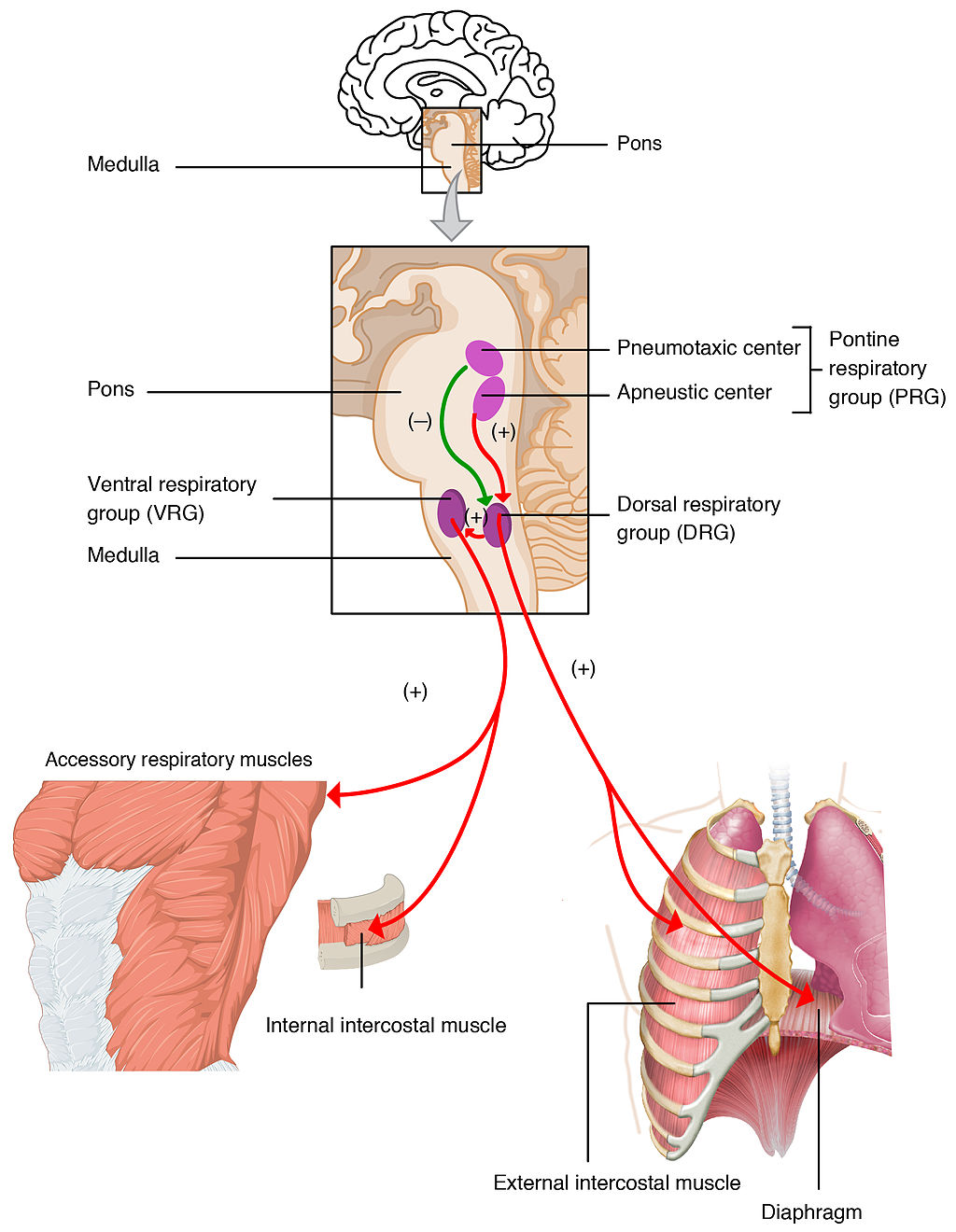
Unconscious Control of Breathing
Unconscious breathing is controlled by respiratory centers in the medulla and pons of the brainstem (see Figure 13.3.4). The respiratory centers automatically and continuously regulate the rate of breathing based on the body’s needs. These are determined mainly by blood acidity, or pH. When you exercise, for example, carbon dioxide levels increase in the blood, because of increased cellular respiration by muscle cells. The carbon dioxide reacts with water in the blood to produce carbonic acid, making the blood more acidic, so pH falls. The drop in pH is detected by chemoreceptors in the medulla. Blood levels of oxygen and carbon dioxide, in addition to pH, are also detected by chemoreceptors in major arteries, which send the “data” to the respiratory centers. The latter respond by sending nerve impulses to the diaphragm, “telling” it to contract more quickly so the rate of breathing speeds up. With faster breathing, more carbon dioxide is released into the air from the blood, and blood pH returns to the normal range.
The opposite events occur when the level of carbon dioxide in the blood becomes too low and blood pH rises. This may occur with involuntary hyperventilation, which can happen in panic attacks, episodes of severe pain, asthma attacks, and many other situations. When you hyperventilate, you blow off a lot of carbon dioxide, leading to a drop in blood levels of carbon dioxide. The blood becomes more basic (alkaline), causing its pH to rise.
Nasal vs. Mouth Breathing
Nasal breathing is breathing through the nose rather than the mouth, and it is generally considered to be superior to mouth breathing. The hair-lined nasal passages do a better job of filtering particles out of the air before it moves deeper into the respiratory tract. The nasal passages are also better at warming and moistening the air, so nasal breathing is especially advantageous in the winter when the air is cold and dry. In addition, the smaller diameter of the nasal passages creates greater pressure in the lungs during exhalation. This slows the emptying of the lungs, giving them more time to extract oxygen from the air.
Feature: Myth vs. Reality
Drowning is defined as respiratory impairment from being in or under a liquid. It is further classified according to its outcome into: death, ongoing health problems, or no ongoing health problems (full recovery). Four hundred Canadians die annually from drowning, and drowning is one of the leading causes of death in children under the age of five. There are some potentially dangerous myths about drowning, and knowing what they are might save your life or the life of a loved one, especially a child.
| Myth | Reality |
|---|---|
| "People drown when they aspirate water into their lungs." | Generally, in the early stages of drowning, very little water enters the lungs. A small amount of water entering the trachea causes a muscular spasm in the larynx that seals the airway and prevents the passage of water into the lungs. This spasm is likely to last until unconsciousness occurs. |
| "You can tell when someone is drowning because they will shout for help and wave their arms to attract attention." | The muscular spasm that seals the airway prevents the passage of air, as well as water, so a person who is drowning is unable to shout or call for help. In addition, instinctive reactions that occur in the final minute or so before a drowning person sinks under the water may look similar to calm, safe behavior. The head is likely to be low in the water, tilted back, with the mouth open. The person may have uncontrolled movements of the arms and legs, but they are unlikely to be visible above the water. |
| "It is too late to save a person who is unconscious in the water." | An unconscious person rescued with an airway still sealed from the muscular spasm of the larynx stands a good chance of full recovery if they start receiving CPR within minutes. Without water in the lungs, CPR is much more effective. Even if cardiac arrest has occurred so the heart is no longer beating, there is still a chance of recovery. The longer the brain goes without oxygen, however, the more likely brain cells are to die. Brain death is likely after about six minutes without oxygen, except in exceptional circumstances, such as young people drowning in very cold water. There are examples of children surviving, apparently without lasting ill effects, for as long as an hour in cold water. Rescuers retrieving a child from cold water should attempt resuscitation even after a protracted period of immersion. |
| "If someone is drowning, you should start administering CPR immediately, even before you try to get the person out of the water." | Removing a drowning person from the water is the first priority, because CPR is ineffective in the water. The goal should be to bring the person to stable ground as quickly as possible and then to start CPR. |
| "You are unlikely to drown unless you are in water over your head." | Depending on circumstances, people have drowned in as little as 30 mm (about 1 ½ in.) of water. Inebriated people or those under the influence of drugs, for example, have been known to have drowned in puddles. Hundreds of children have drowned in the water in toilets, bathtubs, basins, showers, pails, and buckets (see Figure 13.3.5). |

13.3 Summary
- Breathing, or ventilation, is the two-step process of drawing air into the lungs (inhaling) and letting air out of the lungs (exhaling). Inhalation is an active process that results mainly from contraction of a muscle called the diaphragm. Exhalation is typically a passive process that occurs mainly due to the elasticity of the lungs when the diaphragm relaxes.
- Breathing is one of the few vital bodily functions that can be controlled consciously, as well as unconsciously. Conscious control of breathing is common in many activities, including swimming and singing. There are limits on the conscious control of breathing, however. If you try to hold your breath, for example, you will soon have an irrepressible urge to breathe.
- Unconscious breathing is controlled by respiratory centers in the medulla and pons of the brainstem. They respond to variations in blood pH by either increasing or decreasing the rate of breathing as needed to return the pH level to the normal range.
- Nasal breathing is generally considered to be superior to mouth breathing because it does a better job of filtering, warming, and moistening incoming air. It also results in slower emptying of the lungs, which allows more oxygen to be extracted from the air.
- Drowning is a major cause of death in Canada, in particular in children under the age of five. It is important to supervise small children when they are playing in, around, or with water.
13.3 Review Questions
- Define breathing.
-
- Give examples of activities in which breathing is consciously controlled.
- Explain how unconscious breathing is controlled.
- Young children sometimes threaten to hold their breath until they get something they want. Why is this an idle threat?
- Why is nasal breathing generally considered superior to mouth breathing?
- Give one example of a situation that would cause blood pH to rise excessively. Explain why this occurs.
13.3 Explore More
https://www.youtube.com/watch?v=Kl4cU9sG_08
How breathing works - Nirvair Kaur, TED-Ed, 2012.
https://www.youtube.com/watch?v=yDtKBXOEsoM
How do ventilators work? - Alex Gendler, TED-Ed, 2020.
https://www.youtube.com/watch?v=XFnGhrC_3Gs&feature=emb_logo
How I held my breath for 17 minutes | David Blaine, TED, 2010.
https://www.youtube.com/watch?v=Vca6DyFqt4c&feature=emb_logo
The Ultimate Relaxation Technique: How To Practice Diaphragmatic Breathing For Beginners, Kai Simon, 2015.
Attributions
Figure 13.3.1
US_Marines_butterfly_stroke by Cpl. Jasper Schwartz from U.S. Marine Corps on Wikimedia Commons is in the public domain (https://en.wikipedia.org/wiki/Public_domain).
Figure 13.3.2
Inhale Exhale/Breathing cycle by Siyavula Education on Flickr is used under a CC BY 2.0 (https://creativecommons.org/licenses/by/2.0/) license.
Figure 13.3.3
Trumpet/ Frenchmen Street [photo] by Morgan Petroski on Unsplash is used under the Unsplash License (https://unsplash.com/license).
Figure 13.3.4
Respiratory_Centers_of_the_Brain by OpenStax College on Wikimedia Commons is used under a CC BY 3.0 (https://creativecommons.org/licenses/by/3.0) license.
Figure 13.3.5
Lily & Ava in the Kiddie Pool by mob mob on Flickr is used under a CC BY-NC 2.0 (https://creativecommons.org/licenses/by-nc/2.0/) license.
References
Betts, J. G., Young, K.A., Wise, J.A., Johnson, E., Poe, B., Kruse, D.H., Korol, O., Johnson, J.E., Womble, M., DeSaix, P. (2013, June 19). Figure 22.20 Respiratory centers of the brain [digital image]. In Anatomy and Physiology (Section 22.3). OpenStax. https://openstax.org/books/anatomy-and-physiology/pages/22-3-the-process-of-breathing
Kai Simon. (2015, January 11). The ultimate relaxation technique: How to practice diaphragmatic breathing for beginners. YouTube. https://www.youtube.com/watch?v=Vca6DyFqt4c&feature=youtu.be
TED. (2010, January 19). How I held my breath for 17 minutes | David Blaine. YouTube. https://www.youtube.com/watch?v=XFnGhrC_3Gs&feature=youtu.be
TED-Ed. (2012, October 4). How breathing works - Nirvair Kaur. YouTube. https://www.youtube.com/watch?v=Kl4cU9sG_08&feature=youtu.be
TED-Ed. (2020, May 21). How do ventilators work? - Alex Gendler. YouTube. https://www.youtube.com/watch?v=yDtKBXOEsoM&feature=youtu.be

One Piano, Four Hands
Did you ever see two people play the same piano? How do they coordinate all the movements of their own fingers — let alone synchronize them with those of their partner? The peripheral nervous system plays an important part in this challenge.
What Is the Peripheral Nervous System?
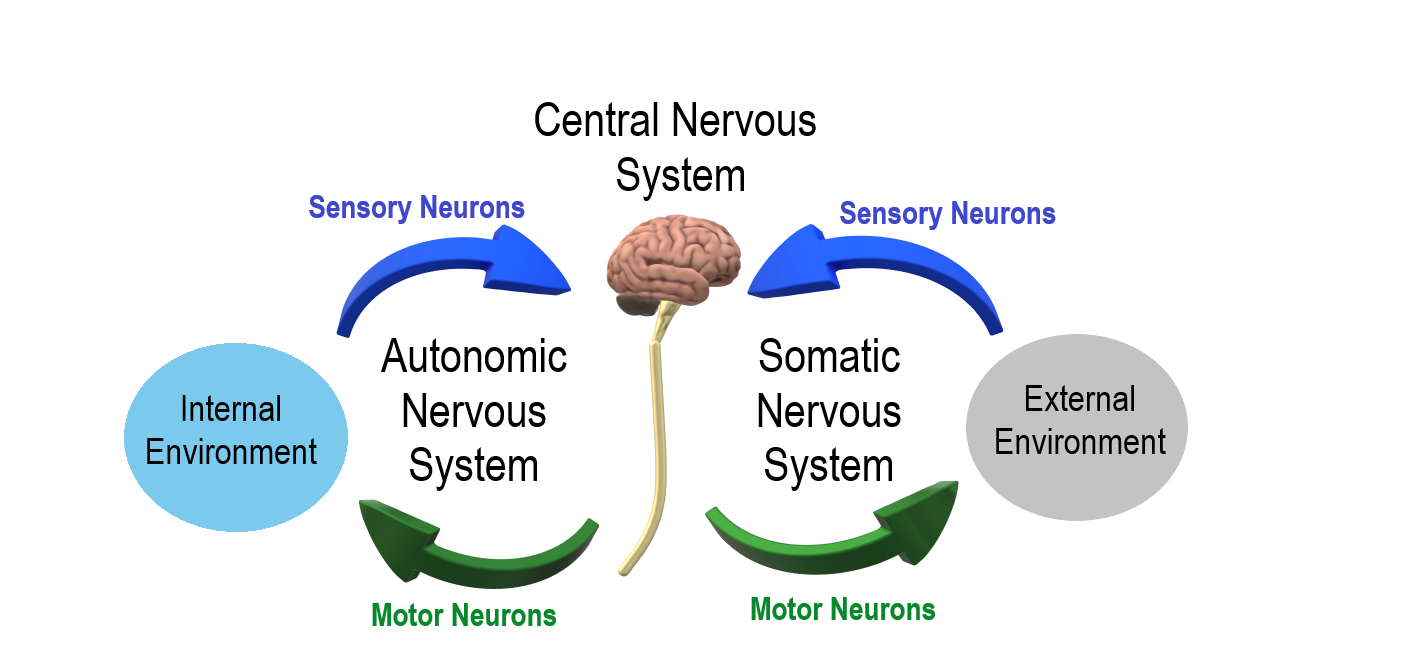
The peripheral nervous system (PNS) consists of all the nervous tissue that lies outside of the central nervous system (CNS). The main function of the PNS is to connect the CNS to the rest of the organism. It serves as a communication relay, going back and forth between the CNS and muscles, organs, and glands throughout the body.
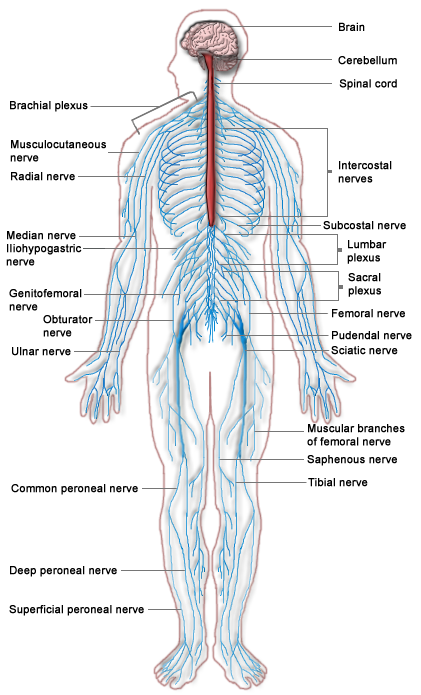
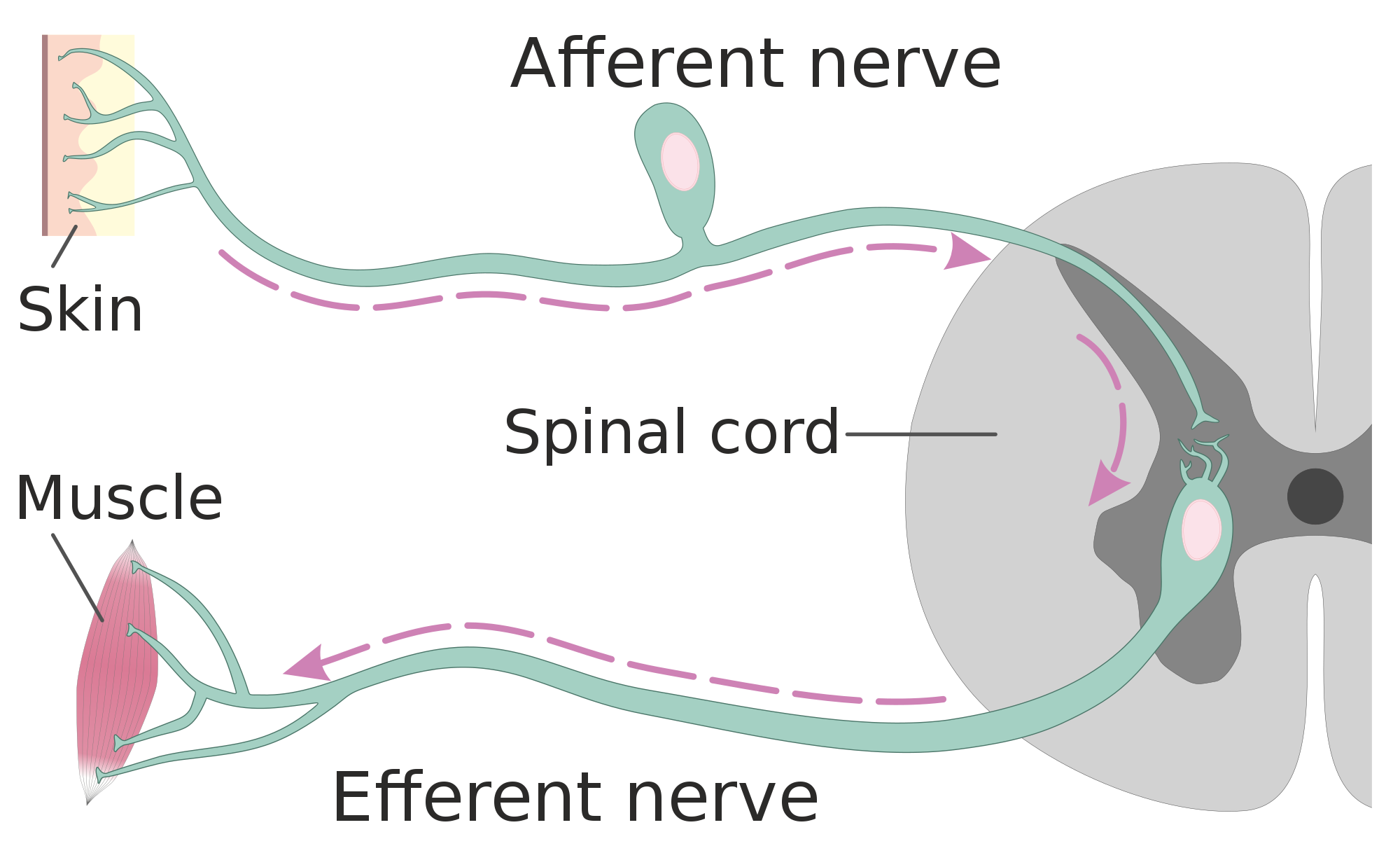
Tissues of the Peripheral Nervous System
The PNS is mostly made up of cable-like bundles of axons called nerves, as well as clusters of neuronal cell bodies called ganglia (singular, ganglion). Nerves are generally classified as sensory, motor, or mixed nerves based on the direction in which they carry nerve impulses.
- Sensory nerves transmit information from sensory receptors in the body to the CNS. Sensory nerves are also called afferent nerves. You can see an example in the figure below.
- Motor nerves transmit information from the CNS to muscles, organs, and glands. Motor nerves are also called efferent nerves. You can see one in the figure below.
- Mixed nerves contain both sensory and motor neurons, so they can transmit information in both directions. They have both afferent and efferent functions.
Divisions of the Peripheral Nervous System
The PNS is divided into two major systems, called the autonomic nervous system and the somatic nervous system. In the diagram below, the autonomic system is shown on the left, and the somatic system on the right. Both systems of the PNS interact with the CNS and include sensory and motor neurons, but they use different circuits of nerves and ganglia.
Somatic Nervous System
The somatic nervous system primarily senses the external environment and controls voluntary activities about which decisions and commands come from the cerebral cortex of the brain. When you feel too warm, for example, you decide to turn on the air conditioner. As you walk across the room to the thermostat, you are using your somatic nervous system. In general, the somatic nervous system is responsible for all of your conscious perceptions of the outside world, as well as all of the voluntary motor activities you perform in response. Whether it’s playing a piano, driving a car, or playing basketball, you can thank your somatic nervous system for making it possible.
Somatic sensory and motor information is transmitted through 12 pairs of cranial nerves and 31 pairs of spinal nerves. Cranial nerves are in the head and neck and connect directly to the brain. Sensory components of cranial nerves transmit information about smells, tastes, light, sounds, and body position. Motor components of cranial nerves control skeletal muscles of the face, tongue, eyeballs, throat, head, and shoulders. Motor components of cranial nerves also control the salivary glands and swallowing. Four of the 12 cranial nerves participate in both sensory and motor functions as mixed nerves, having both sensory and motor neurons.
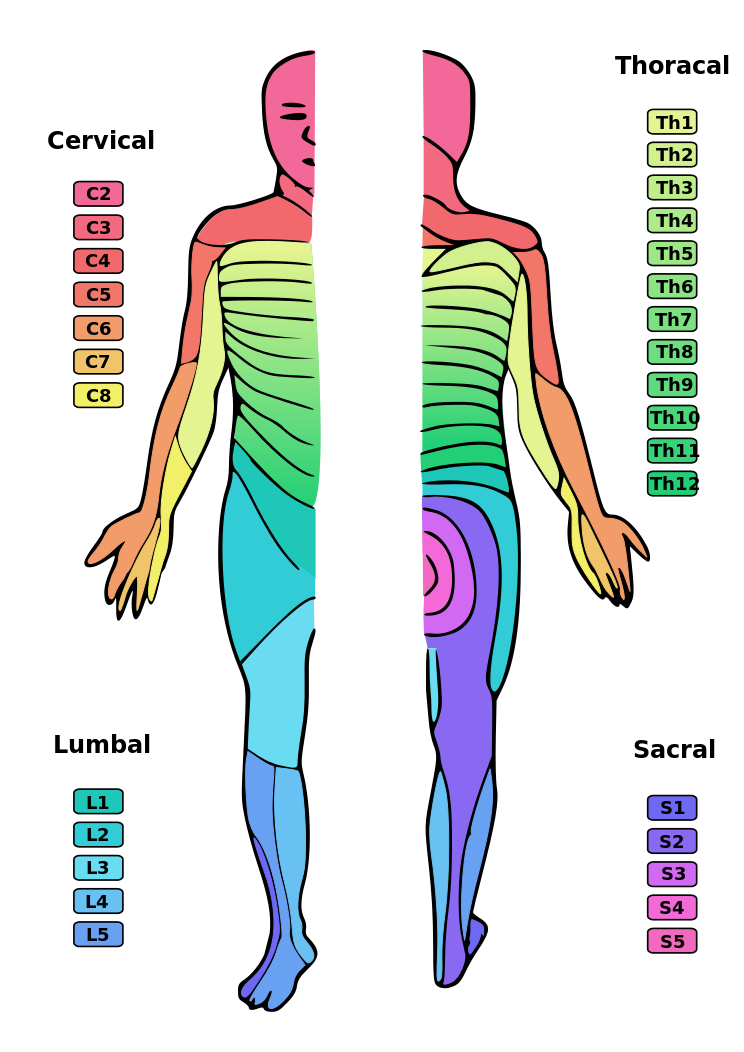
Spinal nerves emanate from the spinal column between vertebrae. All of the spinal nerves are mixed nerves, containing both sensory and motor neurons. The areas of skin innervated by the 31 pairs of spinal nerves are shown in the figure below. These include sensory nerves in the skin that sense pressure, temperature, vibrations, and pain. Other sensory nerves are in the muscles, and they sense stretching and tension. Spinal nerves also include motor nerves that stimulate skeletal muscles to contract, allowing for voluntary body movements.
Autonomic Nervous System
The autonomic nervous system primarily senses the internal environment and controls involuntary activities. It is responsible for monitoring conditions in the internal environment and bringing about appropriate changes in them. In general, the autonomic nervous system is responsible for all the activities that go on inside your body without your conscious awareness or voluntary participation.
Structurally, the autonomic nervous system consists of sensory and motor nerves that run between the CNS (especially the hypothalamus in the brain), internal organs (such as the heart, lungs, and digestive organs), and glands (such as the pancreas and sweat glands). Sensory neurons in the autonomic system detect internal body conditions and send messages to the brain. Motor nerves in the autonomic system affect appropriate responses by controlling contractions of smooth or cardiac muscle, or glandular tissue. For example, when sensory nerves of the autonomic system detect a rise in body temperature, motor nerves signal smooth muscles in blood vessels near the body surface to undergo vasodilation, and the sweat glands in the skin to secrete more sweat to cool the body.
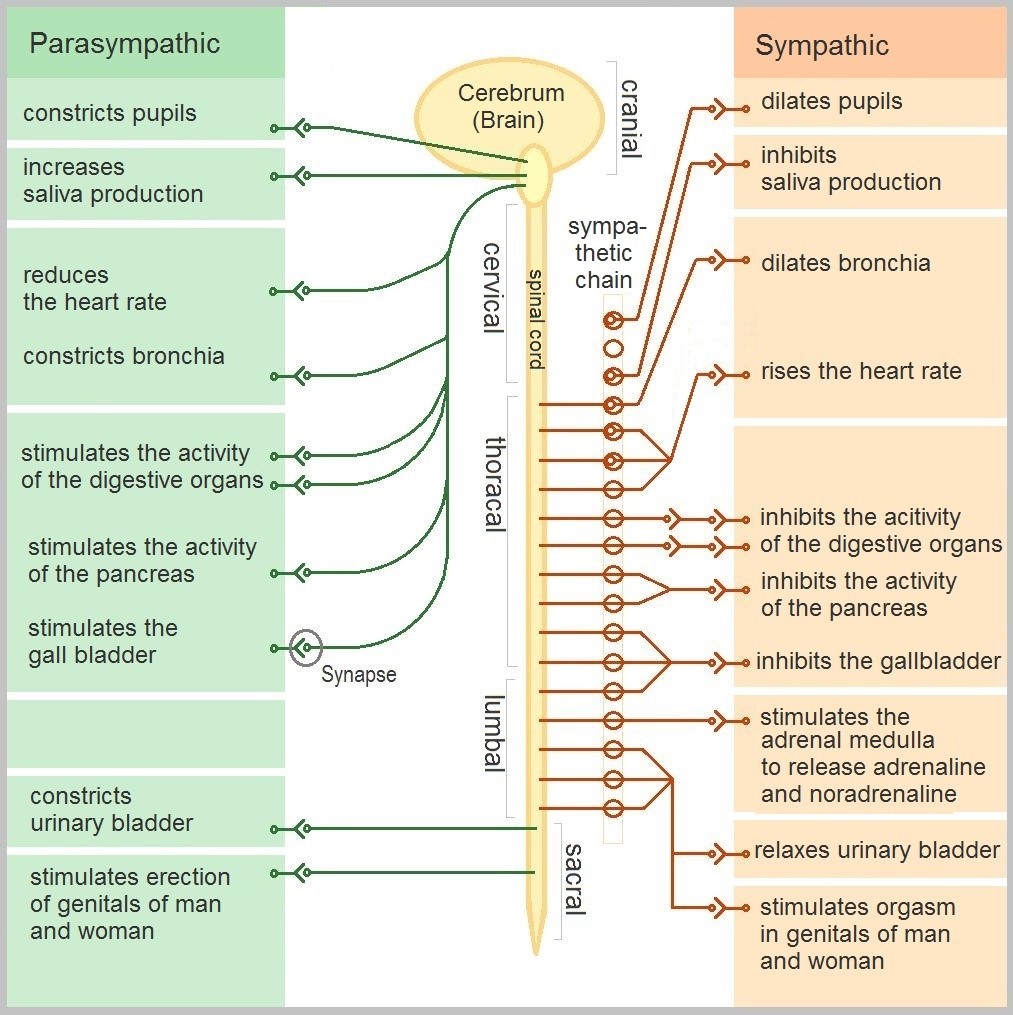
The autonomic nervous system, in turn, has three subdivisions: the sympathetic division, parasympathetic division, and enteric division. The first two subdivisions of the autonomic system are summarized in the figure below. Both affect the same organs and glands, but they generally do so in opposite ways.
- The sympathetic division controls the fight-or-flight response. Changes occur in organs and glands throughout the body that prepare the body to fight or flee in response to a perceived danger. For example, the heart rate speeds up, air passages in the lungs become wider, more blood flows to the skeletal muscles, and the digestive system temporarily shuts down.
- The parasympathetic division returns the body to normal after the fight-or-flight response has occurred. For example, it slows down the heart rate, narrows air passages in the lungs, reduces blood flow to the skeletal muscles, and stimulates the digestive system to start working again. The parasympathetic division also maintains internal homeostasis of the body at other times.
- The enteric division is made up of nerve fibres that supply the organs of the digestive system. This division allows for the local control of many digestive functions.
Disorders of the Peripheral Nervous System
Unlike the CNS — which is protected by bones, meninges, and cerebrospinal fluid — the PNS has no such protections. The PNS also has no blood-brain barrier to protect it from toxins and pathogens in the blood. Therefore, the PNS is more subject to injury and disease than is the CNS. Causes of nerve injury include diabetes, infectious diseases (such as shingles), and poisoning by toxins (such as heavy metals). PNS disorders often have symptoms like loss of feeling, tingling, burning sensations, or muscle weakness. If a traumatic injury results in a nerve being transected (cut all the way through), it may regenerate, but this is a very slow process and may take many months.
Two other diseases of the PNS are Guillain-Barre syndrome and Charcot-Marie-Tooth disease.
- Guillain-Barre syndrome is a rare disease in which the immune system attacks nerves of the PNS, leading to muscle weakness and even paralysis. The exact cause of Guillain-Barre syndrome is unknown, but it often occurs after a viral or bacterial infection. There is no known cure for the syndrome, but most people eventually make a full recovery. Recovery can be slow, however, lasting anywhere from several weeks to several years.
- Charcot-Marie-Tooth disease is a hereditary disorder of the nerves, and one of the most common inherited neurological disorders. It affects predominantly the nerves in the feet and legs, and often in the hands and arms, as well. The disease is characterized by loss of muscle tissue and sense of touch. It is presently incurable.
Feature: My Human Body
The autonomic nervous system is considered to be involuntary because it doesn't require conscious input. However, it is possible to exert some voluntary control over it. People who practice yoga or other so-called mind-body techniques, for example, can reduce their heart rate and certain other autonomic functions. Slowing down these otherwise involuntary responses is a good way to relieve stress and reduce the wear-and-tear that stress can place on the body. Such techniques may also be useful for controlling post-traumatic stress disorder and chronic pain. Three types of integrative practices for these purposes are breathing exercises, body-based tension modulation exercises, and mindfulness techniques.
Breathing exercises can help control the rapid, shallow breathing that often occurs when you are anxious or under stress. These exercises can be learned quickly, and they provide immediate feelings of relief. Specific breathing exercises include paced breath, diaphragmatic breathing, and Breathe2Relax or Chill Zone on MindShift™ CBT, which are downloadable breathing practice mobile applications, or "Apps". Try syncing your breathing with Eric Klassen's "Triangle breathing, 1 minute" video:
https://www.youtube.com/watch?v=u9Q8D6n-3qw
Triangle breathing, 1 minute, Erin Klassen, 2015.
Body-based tension modulation exercises include yoga postures (also known as “asanas”) and tension manipulation exercises. The latter include the Trauma/Tension Release Exercise (TRE) and the Trauma Resiliency Model (TRM). Watch this video for a brief — but informative — introduction to the TRE program:
https://www.youtube.com/watch?v=67R974D8swM&feature=youtu.be
TRE® : Tension and Trauma Releasing Exercises, an Introduction with Jessica Schaffer, Jessica Schaffer Nervous System RESET, 2015.
Mindfulness techniques have been shown to reduce symptoms of depression, as well as those of anxiety and stress. They have also been shown to be useful for pain management and performance enhancement. Specific mindfulness programs include Mindfulness Based Stress Reduction (MBSR) and Mindfulness Mind-Fitness Training (MMFT). You can learn more about MBSR by watching the video below.
https://www.youtube.com/watch?v=0TA7P-iCCcY&feature=youtu.be
Mindfulness-Based Stress Reduction (UMass Medical School, Center for Mindfulness), Palouse Mindfulness, 2017.
8.6 Summary
- The peripheral nervous system (PNS) consists of all the nervous tissue that lies outside the central nervous system (CNS). Its main function is to connect the CNS to the rest of the organism.
- The PNS is made up of nerves and ganglia. Nerves are bundles of axons, and ganglia are groups of cell bodies. Nerves are classified as sensory, motor, or a mix of the two.
- The PNS is divided into the somatic and autonomic nervous systems. The somatic system controls voluntary activities, whereas the autonomic system controls involuntary activities.
- The autonomic nervous system is further divided into sympathetic, parasympathetic, and enteric divisions. The sympathetic division controls fight-or-flight responses during emergencies, the parasympathetic system controls routine body functions the rest of the time, and the enteric division provides local control over the digestive system.
- The PNS is not as well protected physically or chemically as the CNS, so it is more prone to injury and disease. PNS problems include injury from diabetes, shingles, and heavy metal poisoning. Two disorders of the PNS are Guillain-Barre syndrome and Charcot-Marie-Tooth disease.
8.6 Review Questions
- Describe the general structure of the peripheral nervous system. State its primary function.
- What are ganglia?
- Identify three types of nerves based on the direction in which they carry nerve impulses.
- Outline all of the divisions of the peripheral nervous system.
- Compare and contrast the somatic and autonomic nervous systems.
- When and how does the sympathetic division of the autonomic nervous system affect the body?
- What is the function of the parasympathetic division of the autonomic nervous system? Specifically, how does it affect the body?
- Name and describe two peripheral nervous system disorders.
- Give one example of how the CNS interacts with the PNS to control a function in the body.
- For each of the following types of information, identify whether the neuron carrying it is sensory or motor, and whether it is most likely in the somatic or autonomic nervous system:
- Visual information
- Blood pressure information
- Information that causes muscle contraction in digestive organs after eating
- Information that causes muscle contraction in skeletal muscles based on the person’s decision to make a movement
-
8.6 Explore More
https://www.youtube.com/watch?v=ySIDMU2cy0Y&feature=emb_logo
Phantom Limbs Explained, Plethrons, 2015.
https://www.youtube.com/watch?time_continue=1&v=73yo5nJne6c&feature=emb_logo
Why Do Hot Peppers Cause Pain? Reactions, 2015.
Attributions
Figure 8.6.1
Kid’s piant duet by PJMixer on Flickr is used under a CC BY-NC-ND 2.0 (https://creativecommons.org/licenses/by-nc-nd/2.0/) license.
Figure 8.6.2
Nervous_system_diagram by ¤~Persian Poet Gal on Wikimedia Commons is released into the public domain (https://en.wikipedia.org/wiki/Public_domain).
Figure 8.6.3
Afferent_and_efferent_neurons_en.svg by Helixitta on Wikimedia Commons is used under a CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0) license.
Figure 8.6.4
Autonomic and Somatic Nervous System by Christinelmiller on Wikimedia Commons is used under a CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0) license.
Figure 8.6.5
Dermatoms.svg by Ralf Stephan (mailto:ralf@ark.in-berlin.de) on Wikimedia Commons is released into the public domain (https://en.wikipedia.org/wiki/Public_domain).
Figure 8.6.6
The_Autonomic_Nervous_System by Geo-Science-International on Wikimedia Commons is used and adapted by Christine Miller under a CC0 1.0 Universal
Public Domain Dedication license (https://creativecommons.org/publicdomain/zero/1.0/).
References
Erin Klassen. (2015, December 15). Triangle breathing, 1 minute. YouTube. https://www.youtube.com/watch?v=u9Q8D6n-3qw&feature=youtu.be
Jessica Schaffer Nervous System RESET. (2015, January 15). TRE® : Tension and trauma releasing exercises, an Introduction with Jessica Schaffer. YouTube. https://www.youtube.com/watch?v=67R974D8swM&feature=youtu.be
Mayo Clinic Staff. (n.d.). Charcot-Marie-Tooth disease [online article]. MayoClinic.org. https://www.mayoclinic.org/diseases-conditions/charcot-marie-tooth-disease/symptoms-causes/syc-20350517
Mayo Clinic Staff. (n.d.). Diabetes [online article]. MayoClinic.org. https://www.mayoclinic.org/diseases-conditions/diabetes/symptoms-causes/syc-20371444
Mayo Clinic Staff. (n.d.). Guillain-Barre syndrome [online article]. MayoClinic.org. https://www.mayoclinic.org/diseases-conditions/guillain-barre-syndrome/symptoms-causes/syc-20362793
Mayo Clinic Staff. (n.d.). Shingles [online article]. MayoClinic.org. https://www.mayoclinic.org/diseases-conditions/shingles/symptoms-causes/syc-20353054
Mayo Clinic Staff. (n.d.). Stroke [online article]. MayoClinic.org. https://www.mayoclinic.org/diseases-conditions/stroke/symptoms-causes/syc-20350113
Palouse Mindfulness. (2017, March 25). Mindfulness-based stress reduction (UMass Medical School, Center for Mindfulness), YouTube. https://www.youtube.com/watch?v=0TA7P-iCCcY&feature=youtu.be
Plethrons, (2015, March 23). Phantom limbs explained. YouTube. https://www.youtube.com/watch?v=ySIDMU2cy0Y&feature=youtu.be
Reactions. (2015, December 1). Why do hot peppers cause pain? YouTube. https://www.youtube.com/watch?v=73yo5nJne6c&feature=youtu.be
Image shows a diagram of all the components of the endocrine system. This includes the pineal and pituitary glands in the brain, the thyroid gland surrounding the larynx, the thymus gland sitting above the heart, the adrenal glands sitting above the kidneys, the pancreas, and in females, the uterus and ovaries and in males the testes.
A group of diseases involving abnormal cell growth with the potential to invade or spread to other parts of the body.
A microorganism which causes disease.
An organisms that is so small it is invisible to the human eye.
Created by CK-12 Foundation/Adapted by Christine Miller

Case Study: Flight Risk
Nineteen-year-old Malcolm is about to take his first plane flight. Shortly after he boards the plane and sits down, a man in his late sixties sits next to him in the aisle seat. About half an hour after the plane takes off, the pilot announces that she is turning the seat belt light off, and that it is safe to move around the cabin.
The man in the aisle seat — who has introduced himself to Malcolm as Willie — immediately unbuckles his seat belt and paces up and down the aisle a few times before returning to his seat. After about 45 minutes, Willie gets up again, walks some more, then sits back down and does some foot and leg exercises. After the third time Willie gets up and paces the aisles, Malcolm asks him whether he is walking so much to accumulate steps on a pedometer or fitness tracking device. Willie laughs and says no. He is actually trying to do something even more important for his health — prevent a blood clot from forming in his legs.
Willie explains that he has a chronic condition: heart failure. Although it sounds scary, his condition is currently well-managed, and he is able to lead a relatively normal lifestyle. However, it does put him at risk of developing other serious health conditions, such as deep vein thrombosis (DVT), which is when a blood clot occurs in the deep veins, usually in the legs. Air travel — and other situations where a person has to sit for a long period of time — increases the risk of DVT. Willie’s doctor said that he is healthy enough to fly, but that he should walk frequently and do leg exercises to help avoid a blood clot.
As you read this chapter, you will learn about the heart, blood vessels, and blood that make up the cardiovascular system, as well as disorders of the cardiovascular system, such as heart failure. At the end of the chapter you will learn more about why DVT occurs, why Willie has to take extra precautions when he flies, and what can be done to lower the risk of DVT and its potentially deadly consequences.
Chapter Overview: Cardiovascular System
In this chapter, you will learn about the cardiovascular system, which transports substances throughout the body. Specifically, you will learn about:
- The major components of the cardiovascular system: the heart, blood vessels, and blood.
- The functions of the cardiovascular system, including transporting needed substances (such as oxygen and nutrients) to the cells of the body, and picking up waste products.
- How blood is oxygenated through the pulmonary circulation, which transports blood between the heart and lungs.
- How blood is circulated throughout the body through the systemic circulation.
- The components of blood — including plasma, red blood cells, white blood cells, and platelets — and their specific functions.
- Types of blood vessels — including arteries, veins, and capillaries — and their functions, similarities, and differences.
- The structure of the heart, how it pumps blood, and how contractions of the heart are controlled.
- What blood pressure is and how it is regulated.
- Blood disorders, including anemia, HIV, and leukemia.
- Cardiovascular diseases (including heart attack, stroke, and angina), and the risk factors and precursors — such as high blood pressure and atherosclerosis — that contribute to them.
As you read the chapter, think about the following questions:
- What is heart failure?Why do you think it increases the risk of DVT?
- What is a blood clot? What are possible health consequences of blood clots?
- Why do you think sitting for long periods of time increases the risk of DVT? Why does walking and exercising the legs help reduce this risk?
Attribution
Figure 14.1.1
aircraft-1583871_1920 [photo] by olivier89 from Pixabay is used under the Pixabay License (https://pixabay.com/de/service/license/).
Image shows a diagram of the negative feedback loop governing thyroid gland function. In the absence of sufficient levels of thyroid hormones, the hypothalamus will secrete TRH, which stimulates the pituitary gland to secrete TSH, which stimulates the thyroid gland to make thyroid hormones. Sufficient blood levels of thyroid hormone inhibit the hypothalamus from secreting TRH, halting the pathway, until thyroid hormone level sdrop again
Image shows a diagram of how alzheimer's progresses. In preclinical AD, just a small portion of the brain is affected. More of the brain and more areas of the brain are affected in mild to moderate AD. In severe AD, most of the brain is affected.

Pills from Pee
The medication pictured in Figure 9.3.1 with the brand name Progynon was a drug used to control the effects of menopause in women. The pills first appeared in 1928 and contained the human sex hormone estrogen. Estrogen secretion declines in women around the time of menopause and may cause symptoms like mood swings and hot flashes. The pills were supposed to ease the symptoms by supplementing estrogen in the body. The manufacturer of Progynon obtained estrogen for the pills from the urine of pregnant women, because it was a cheap source of the hormone. Progynon is still used today to treat menopausal symptoms. Although the drug has been improved over the years, it still contains estrogen, which is an example of an endocrine hormone.
How Do Endocrine Hormones Work?
Endocrine hormones like estrogen are messenger molecules secreted by endocrine glands into the bloodstream. They travel throughout the body in the circulation. Although they reach virtually every cell in the body in this way, each hormone affects only certain cells, called target cells. A target cell is the type of cell on which a hormone has an effect. A target cell is affected by a particular hormone because it has receptor proteins — either on the cell surface or within the cell — that are specific to that hormone. An endocrine hormone travels through the bloodstream until it finds a target cell with a matching receptor to which it can bind. When the hormone binds to the receptor, it causes changes within the cell. The manner in which it changes the cell depends on whether the hormone is a steroid hormone or a non-steroid hormone.
Steroid Hormones
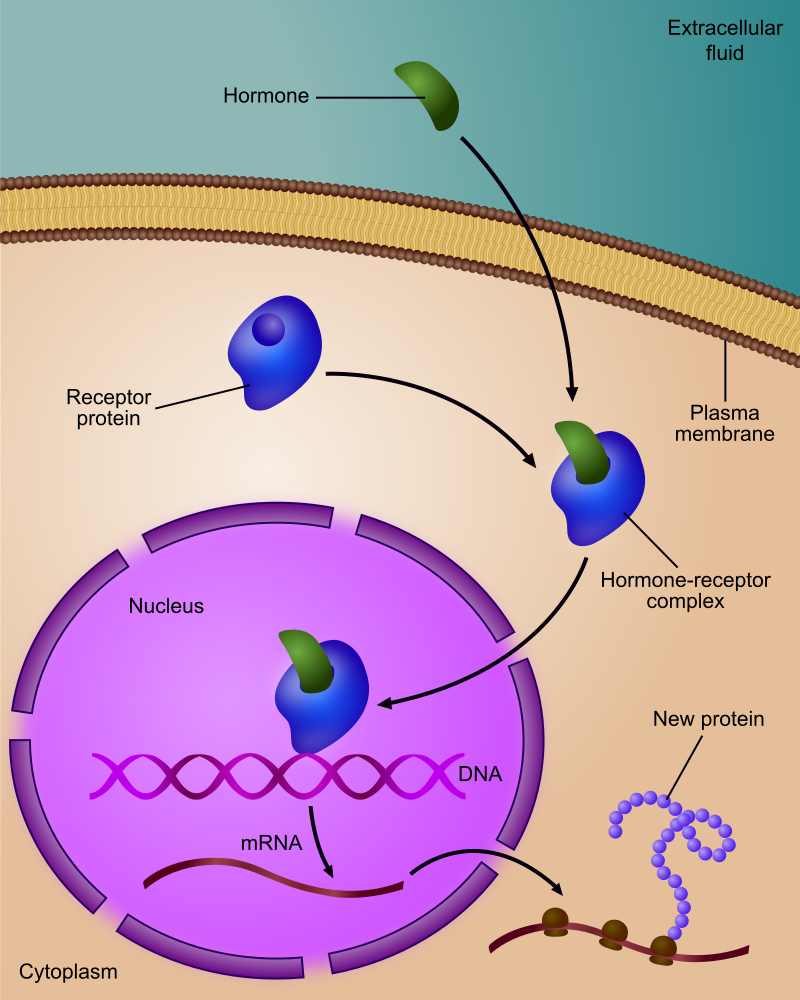
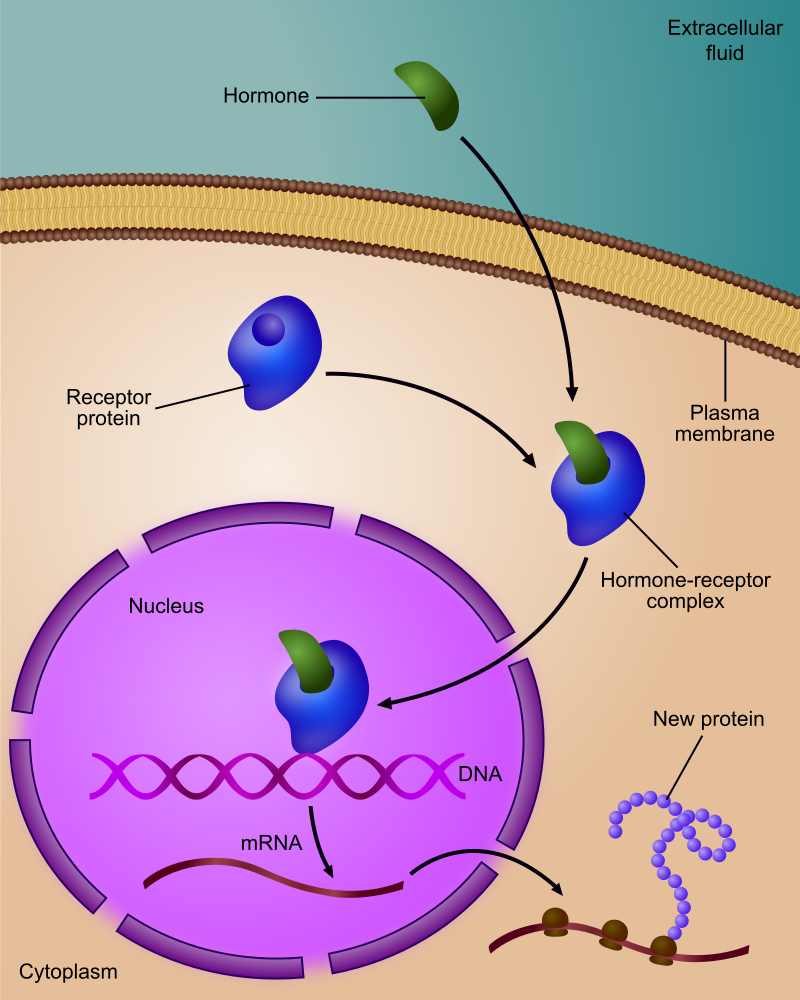
A steroid hormone (such as estrogen) is made of lipids. It is fat soluble, so it can diffuse across a target cell’s plasma membrane, which is also made of lipids. Once inside the cell, a steroid hormone binds with receptor proteins in the cytoplasm. As you can see in Figure 9.3.2, the steroid hormone and its receptor form a complex — called a steroid complex — which moves into the nucleus, where it influences the expression of genes. Examples of steroid hormones include cortisol, which is secreted by the adrenal glands, and sex hormones, which are secreted by the gonads.
Non-Steroid Hormones
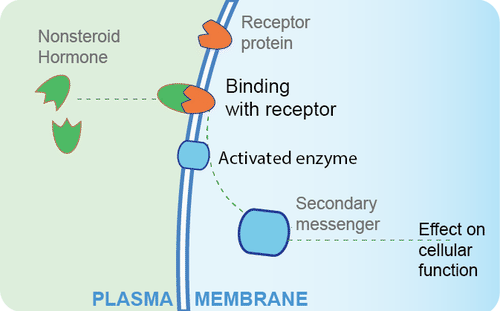
A non-steroid hormoneis made of amino acids. It is not fat soluble, so it cannot diffuse across the plasma membrane of a target cell. Instead, it binds to a receptor protein on the cell membrane. In the Figure 9.3.3 diagram, you can see that the binding of the hormone with the receptor activates an enzyme in the cell membrane. The enzyme then stimulates another molecule, called the second messenger, which influences processes inside the cell. Most endocrine hormones are non-steroid hormones. Examples include glucagon and insulin, both produced by the pancreas.
Regulation of Endocrine Hormones
Endocrine hormones regulate many body processes, but what regulates the secretion of endocrine hormones? Most endocrine hormones are controlled by feedback mechanisms. A feedback mechanism is a loop in which a product feeds back to control its own production. Feedback loops may be either negative or positive.
- Most endocrine hormones are regulated by negative feedback loops. Negative feedback keeps the concentration of a hormone within a relatively narrow range, and maintains homeostasis.
- Very few endocrine hormones are regulated by positive feedback loops. Positive feedback causes the concentration of a hormone to become increasingly higher.
Regulation by Negative Feedback
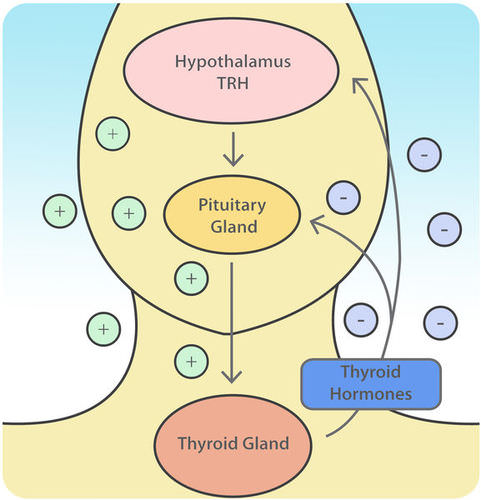
A negative feedback loop controls the synthesis and secretion of hormones by the thyroid gland. This loop includes the hypothalamus and pituitary gland, in addition to the thyroid, as shown in the diagram (Figure 9.3.4). When the levels of thyroid hormones circulating in the blood fall too low, the hypothalamus secretes thyrotropin releasing hormone (TRH). This hormone travels directly to the pituitary gland through the thin stalk connecting the two structures. In the pituitary gland, TRH stimulates the pituitary to secrete thyroid stimulating hormone (TSH). TSH, in turn, travels through the bloodstream to the thyroid gland, and stimulates it to secrete thyroid hormones. This continues until the blood levels of thyroid hormones are high enough. At that point, the thyroid hormones feed back to stop the hypothalamus from secreting TRH and the pituitary from secreting TSH. Without the stimulation of TSH, the thyroid gland stops secreting its hormones. Eventually, the levels of thyroid hormones in the blood start to fall too low again. When that happens, the hypothalamus releases TRH, and the loop repeats.
Regulation by Positive Feedback
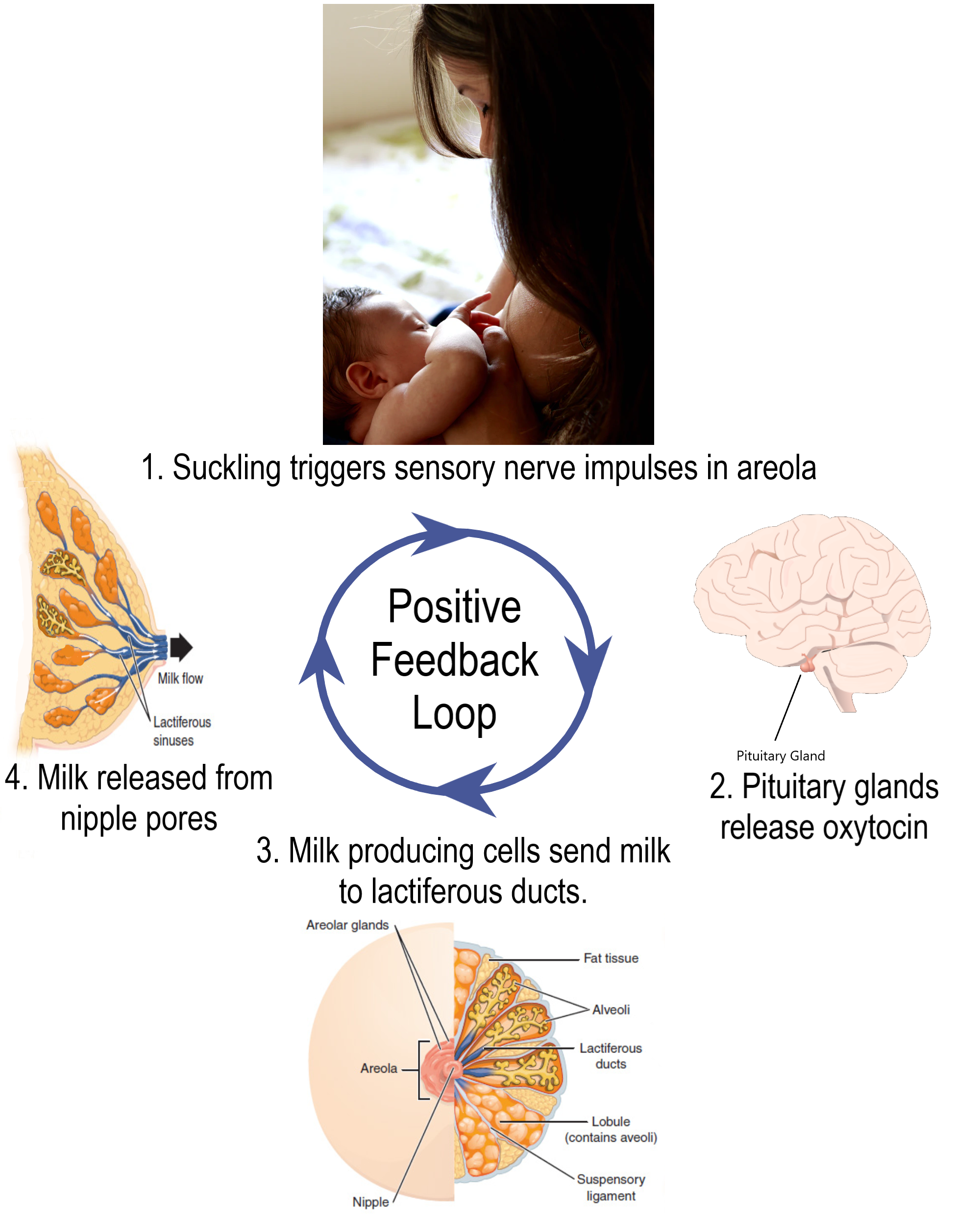
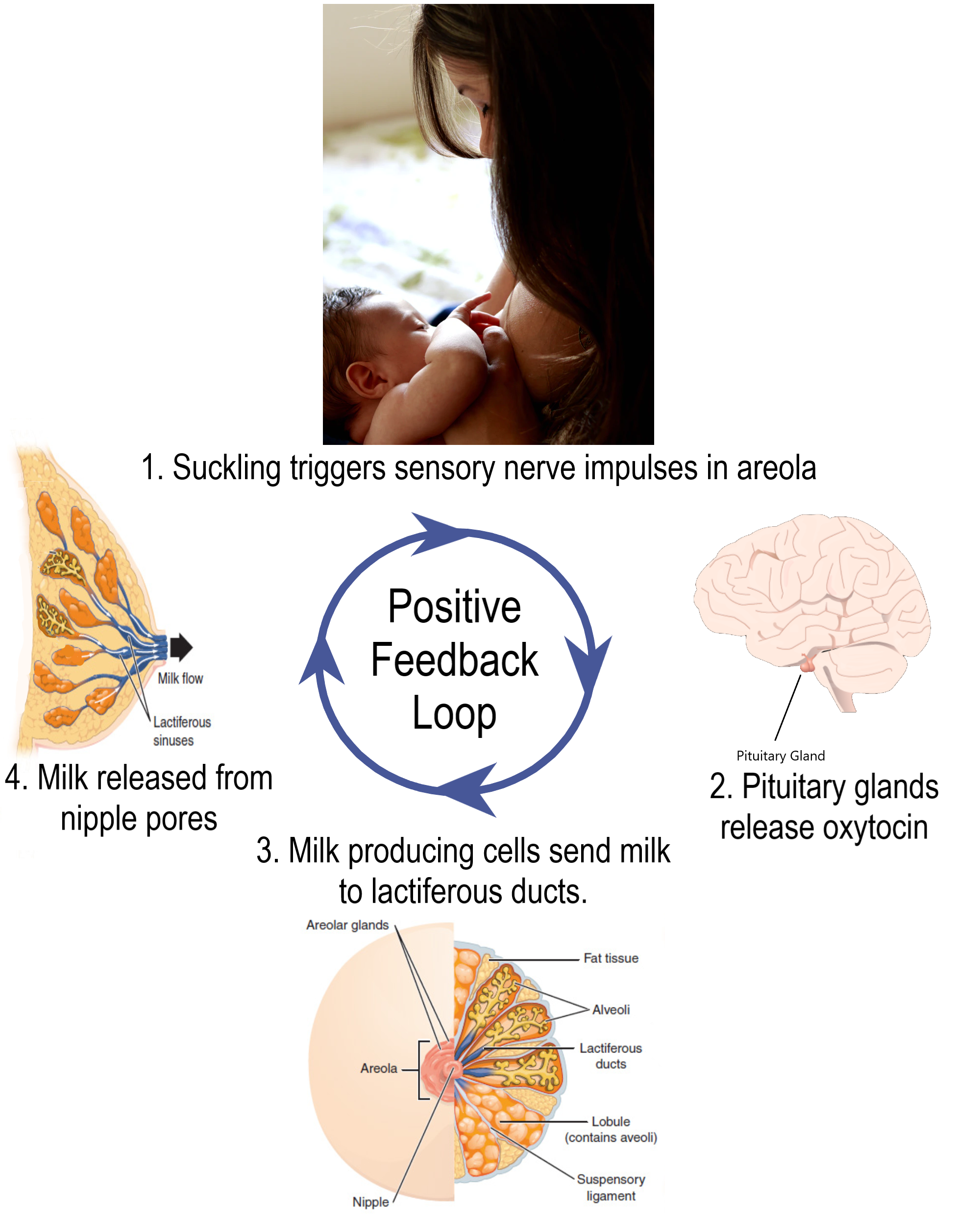
Prolactin is a non-steroid endocrine hormone secreted by the pituitary gland. One of the functions of prolactin is to stimulate a nursing mother’s mammary glands to produce milk. The regulation of prolactin in the mother is controlled by a positive feedback loop that involves the nipples, hypothalamus, pituitary gland, and mammary glands. Positive feedback begins when a baby suckles on the mother’s nipple. Nerve impulses from the nipple reach the hypothalamus, which stimulates the pituitary gland to secrete prolactin. Prolactin travels in the blood to the mammary glands and stimulates them to produce milk. The release of milk causes the baby to continue suckling, which causes more prolactin to be secreted and more milk to be produced. The positive feedback loop continues until the baby stops suckling at the breast.
Feature: Myth vs. Reality
Anabolic steroids are synthetic versions of the naturally occurring male sex hormone testosterone. Male hormones have androgenic (or masculinizing) effects, but they also have anabolic (or muscle-building) effects. The anabolic effects are the reason that synthetic steroids are used by athletes. In addition to building muscles, they also accelerate the development of bones and red blood cells, increase endurance so athletes can train harder and longer, and speed up muscle recovery. Unfortunately, these benefits of steroid use come with costs. If you ever consider taking anabolic steroids to build muscles and improve athletic performance, consider the following myths and corresponding realities.
Myth |
Reality |
| "Steroids are safe." | Steroid use may cause several serious side effects. Prolonged use may increase the risk of liver cancer, heart disease, and high blood pressure. |
| "Steroids will not stunt your growth." | Teens who take steroids before they have finished growing in height may have their growth stunted so they remain shorter throughout life than they would otherwise have been. Such stunting occurs because steroids increase the rate at which skeletal maturity is reached. Once skeletal maturity occurs, additional growth in height is impossible. |
| "Steroids do not cause drug dependency." | Steroid use may cause dependency, as evidenced by the negative effects of stopping steroid use. These negative effects may include insomnia, fatigue, and depressed mood, among others. |
| "There is no such thing as 'roid rage.'" | Steroid use has been shown to increase aggressiveness in some people. It has also been implicated in a number of violent acts committed by people who had not demonstrated violent tendencies until they started using steroids. |
| "Only males use steroids." | Although steroid use is more common in males than females, some females also use steroids. They use them to build muscle and improve physical performance, generally either for athletic competition or for self-defense. |
9.3 Summary
- Endocrine hormones are messenger molecules secreted by endocrine glands into the bloodstream. They travel throughout the body but affect only certain cells, called target cells, which have receptors specific to particular hormones.
- Steroid hormones such as estrogen are endocrine hormones made of lipids that cross plasma membranes and bind to receptors inside target cells. The hormone-receptor complexes then move into the nucleus, where they influence gene expression.
- Non-steroid hormones (such as insulin) are endocrine hormones made of amino acids that bind to receptors on the surface of target cells. This activates an enzyme in the plasma membrane, and the enzyme controls a second messenger molecule, which influences cell processes.
- Most endocrine hormones are controlled by negative feedback loops in which rising levels of a hormone feed back to stop its own production — and vice-versa. For example, a negative feedback loop controls production of thyroid hormones. The loop includes the hypothalamus, pituitary gland, and thyroid gland.
- Only a few endocrine hormones are controlled by positive feedback loops, in which rising levels of a hormone feed back to stimulate continued production of the hormone. Prolactin, the pituitary hormone that stimulates milk production by mammary glands, is controlled by a positive feedback loop. The loop includes the nipples, hypothalamus, pituitary gland, and mammary glands.
9.3 Review Questions
-
-
- Explain how steroid hormones influence target cells.
- How do non-steroid hormones affect target cells?
- Compare and contrast negative and positive feedback loops.
- Outline the way feedback controls the production of thyroid hormones.
- Describe the feedback mechanism that controls milk production by the mammary glands.
- People with a condition called hyperthyroidism produce too much thyroid hormone. What do you think this does to the level of TSH? Explain your answer.
- Which is more likely to maintain homeostasis— negative feedback or positive feedback? Explain your answer.
- Does testosterone bind to receptors on the plasma membrane of target cells or in the cytoplasm of target cells? Explain your answer.
9.3 Explore More
https://www.youtube.com/watch?v=WVrlHH14q3o&feature=emb_logo
Great Glands - Your Endocrine System: CrashCourse Biology #33, CrashCourse, 2012.
https://www.youtube.com/watch?v=qXaDDa3FB5Q&feature=emb_logo
National Geographic | Benefits and Side Effects of Steroids Use 2015, 24 Physic.
Attributions
Figure 9.3.1
L0058274 Glass bottle for ‘Progynon’ pills, United Kingdom, 1928-1948 by Wellcome Collection gallery (2018-03-29)/ Science Museum, London on Wikimedia Commons is used under a CC-BY-4.0 (https://creativecommons.org/licenses/by/4.0/) license.
Figure 9.3.2
Regulation_of_gene_expression_by_steroid_hormone_receptor.svg by Ali Zifan on Wikimedia Commons is used under a CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0/deed.en) license.
Figure 9.3.3
Non-steroid hormone pathway by CK-12 Foundation, Biology for High School is used under a CC BY-NC 3.0 (https://creativecommons.org/licenses/by-nc/3.0/) license.
Figure 9.3.4
Thyroid Negative Feedback Loop by CK-12 Foundation, College Human Biology is used under a CC BY-NC 3.0 (https://creativecommons.org/licenses/by-nc/3.0/) license.
 ©CK-12 Foundation Licensed under
©CK-12 Foundation Licensed under ![]() • Terms of Use • Attribution
• Terms of Use • Attribution
Figure 9.3.5
Lactation Positive Feedback Loop by Christinelmiller on Wikimedia Commons is used under a CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0/deed.en) license.
References
24 Physic. (2015,July 19). National Geographic | Benefits and side effects of steroids use 2015. YouTube. https://www.youtube.com/watch?v=qXaDDa3FB5Q&feature=youtu.be
Brainard, J/ CK-12 Foundation. (2016, August 15). Figure 4 Thyroid negative feedback loop [digital image]. In CK-12 College Human Biology (Section 11.3 Endocrine hormones). CK12.org. https://www.ck12.org/book/ck-12-human-biology/section/11.3/
CK-12 Foundation. (2019, March 5). Figure 3 A non-steroid hormone binds with a receptor on the plasma membrane of a target cell [digital image]. In Flexbook 2.0: CK-12 Biology For High School (Section 13.21 Hormone). CK12. https://flexbooks.ck12.org/cbook/ck-12-biology-flexbook-2.0/section/13.21/primary/lesson/hormones-bio
CrashCourse. (2012, September 10). Great glands - Your endocrine system: CrashCourse Biology #33. YouTube. https://www.youtube.com/watch?v=WVrlHH14q3o&feature=youtu.be
TED-Ed. (2018, June 21). How do your hormones work? - Emma Bryce. YouTube. https://www.youtube.com/watch?v=-SPRPkLoKp8&feature=youtu.be
Created by CK-12 Foundation/Adapted by Christine Miller

Pills from Pee
The medication pictured in Figure 9.3.1 with the brand name Progynon was a drug used to control the effects of menopause in women. The pills first appeared in 1928 and contained the human sex hormone estrogen. Estrogen secretion declines in women around the time of menopause and may cause symptoms like mood swings and hot flashes. The pills were supposed to ease the symptoms by supplementing estrogen in the body. The manufacturer of Progynon obtained estrogen for the pills from the urine of pregnant women, because it was a cheap source of the hormone. Progynon is still used today to treat menopausal symptoms. Although the drug has been improved over the years, it still contains estrogen, which is an example of an endocrine hormone.
How Do Endocrine Hormones Work?
Endocrine hormones like estrogen are messenger molecules secreted by endocrine glands into the bloodstream. They travel throughout the body in the circulation. Although they reach virtually every cell in the body in this way, each hormone affects only certain cells, called target cells. A target cell is the type of cell on which a hormone has an effect. A target cell is affected by a particular hormone because it has receptor proteins — either on the cell surface or within the cell — that are specific to that hormone. An endocrine hormone travels through the bloodstream until it finds a target cell with a matching receptor to which it can bind. When the hormone binds to the receptor, it causes changes within the cell. The manner in which it changes the cell depends on whether the hormone is a steroid hormone or a non-steroid hormone.
Steroid Hormones
A steroid hormone (such as estrogen) is made of lipids. It is fat soluble, so it can diffuse across a target cell’s plasma membrane, which is also made of lipids. Once inside the cell, a steroid hormone binds with receptor proteins in the cytoplasm. As you can see in Figure 9.3.2, the steroid hormone and its receptor form a complex — called a steroid complex — which moves into the nucleus, where it influences the expression of genes. Examples of steroid hormones include cortisol, which is secreted by the adrenal glands, and sex hormones, which are secreted by the gonads.
Non-Steroid Hormones
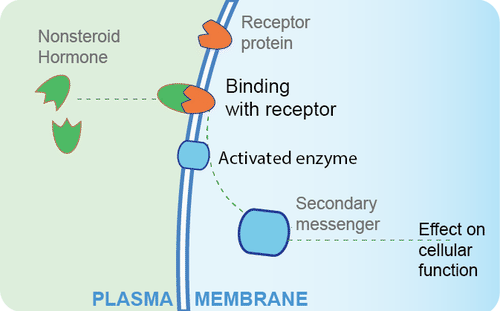
A non-steroid hormoneis made of amino acids. It is not fat soluble, so it cannot diffuse across the plasma membrane of a target cell. Instead, it binds to a receptor protein on the cell membrane. In the Figure 9.3.3 diagram, you can see that the binding of the hormone with the receptor activates an enzyme in the cell membrane. The enzyme then stimulates another molecule, called the second messenger, which influences processes inside the cell. Most endocrine hormones are non-steroid hormones. Examples include glucagon and insulin, both produced by the pancreas.
Regulation of Endocrine Hormones
Endocrine hormones regulate many body processes, but what regulates the secretion of endocrine hormones? Most endocrine hormones are controlled by feedback mechanisms. A feedback mechanism is a loop in which a product feeds back to control its own production. Feedback loops may be either negative or positive.
- Most endocrine hormones are regulated by negative feedback loops. Negative feedback keeps the concentration of a hormone within a relatively narrow range, and maintains homeostasis.
- Very few endocrine hormones are regulated by positive feedback loops. Positive feedback causes the concentration of a hormone to become increasingly higher.
Regulation by Negative Feedback
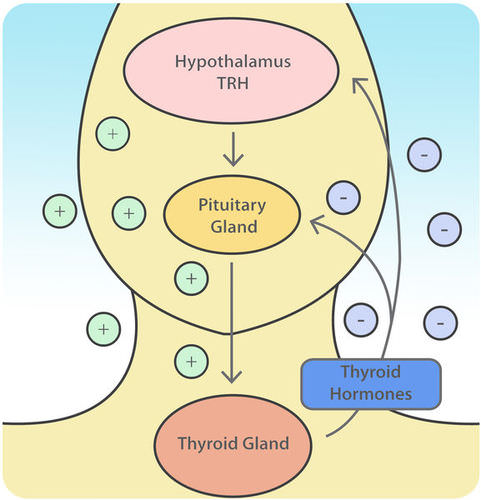
A negative feedback loop controls the synthesis and secretion of hormones by the thyroid gland. This loop includes the hypothalamus and pituitary gland, in addition to the thyroid, as shown in the diagram (Figure 9.3.4). When the levels of thyroid hormones circulating in the blood fall too low, the hypothalamus secretes thyrotropin releasing hormone (TRH). This hormone travels directly to the pituitary gland through the thin stalk connecting the two structures. In the pituitary gland, TRH stimulates the pituitary to secrete thyroid stimulating hormone (TSH). TSH, in turn, travels through the bloodstream to the thyroid gland, and stimulates it to secrete thyroid hormones. This continues until the blood levels of thyroid hormones are high enough. At that point, the thyroid hormones feed back to stop the hypothalamus from secreting TRH and the pituitary from secreting TSH. Without the stimulation of TSH, the thyroid gland stops secreting its hormones. Eventually, the levels of thyroid hormones in the blood start to fall too low again. When that happens, the hypothalamus releases TRH, and the loop repeats.
Regulation by Positive Feedback
Prolactin is a non-steroid endocrine hormone secreted by the pituitary gland. One of the functions of prolactin is to stimulate a nursing mother’s mammary glands to produce milk. The regulation of prolactin in the mother is controlled by a positive feedback loop that involves the nipples, hypothalamus, pituitary gland, and mammary glands. Positive feedback begins when a baby suckles on the mother’s nipple. Nerve impulses from the nipple reach the hypothalamus, which stimulates the pituitary gland to secrete prolactin. Prolactin travels in the blood to the mammary glands and stimulates them to produce milk. The release of milk causes the baby to continue suckling, which causes more prolactin to be secreted and more milk to be produced. The positive feedback loop continues until the baby stops suckling at the breast.
Feature: Myth vs. Reality
Anabolic steroids are synthetic versions of the naturally occurring male sex hormone testosterone. Male hormones have androgenic (or masculinizing) effects, but they also have anabolic (or muscle-building) effects. The anabolic effects are the reason that synthetic steroids are used by athletes. In addition to building muscles, they also accelerate the development of bones and red blood cells, increase endurance so athletes can train harder and longer, and speed up muscle recovery. Unfortunately, these benefits of steroid use come with costs. If you ever consider taking anabolic steroids to build muscles and improve athletic performance, consider the following myths and corresponding realities.
Myth |
Reality |
| "Steroids are safe." | Steroid use may cause several serious side effects. Prolonged use may increase the risk of liver cancer, heart disease, and high blood pressure. |
| "Steroids will not stunt your growth." | Teens who take steroids before they have finished growing in height may have their growth stunted so they remain shorter throughout life than they would otherwise have been. Such stunting occurs because steroids increase the rate at which skeletal maturity is reached. Once skeletal maturity occurs, additional growth in height is impossible. |
| "Steroids do not cause drug dependency." | Steroid use may cause dependency, as evidenced by the negative effects of stopping steroid use. These negative effects may include insomnia, fatigue, and depressed mood, among others. |
| "There is no such thing as 'roid rage.'" | Steroid use has been shown to increase aggressiveness in some people. It has also been implicated in a number of violent acts committed by people who had not demonstrated violent tendencies until they started using steroids. |
| "Only males use steroids." | Although steroid use is more common in males than females, some females also use steroids. They use them to build muscle and improve physical performance, generally either for athletic competition or for self-defense. |
9.3 Summary
- Endocrine hormones are messenger molecules secreted by endocrine glands into the bloodstream. They travel throughout the body but affect only certain cells, called target cells, which have receptors specific to particular hormones.
- Steroid hormones such as estrogen are endocrine hormones made of lipids that cross plasma membranes and bind to receptors inside target cells. The hormone-receptor complexes then move into the nucleus, where they influence gene expression.
- Non-steroid hormones (such as insulin) are endocrine hormones made of amino acids that bind to receptors on the surface of target cells. This activates an enzyme in the plasma membrane, and the enzyme controls a second messenger molecule, which influences cell processes.
- Most endocrine hormones are controlled by negative feedback loops in which rising levels of a hormone feed back to stop its own production — and vice-versa. For example, a negative feedback loop controls production of thyroid hormones. The loop includes the hypothalamus, pituitary gland, and thyroid gland.
- Only a few endocrine hormones are controlled by positive feedback loops, in which rising levels of a hormone feed back to stimulate continued production of the hormone. Prolactin, the pituitary hormone that stimulates milk production by mammary glands, is controlled by a positive feedback loop. The loop includes the nipples, hypothalamus, pituitary gland, and mammary glands.
9.3 Review Questions
-
-
- Explain how steroid hormones influence target cells.
- How do non-steroid hormones affect target cells?
- Compare and contrast negative and positive feedback loops.
- Outline the way feedback controls the production of thyroid hormones.
- Describe the feedback mechanism that controls milk production by the mammary glands.
- People with a condition called hyperthyroidism produce too much thyroid hormone. What do you think this does to the level of TSH? Explain your answer.
- Which is more likely to maintain homeostasis— negative feedback or positive feedback? Explain your answer.
- Does testosterone bind to receptors on the plasma membrane of target cells or in the cytoplasm of target cells? Explain your answer.
9.3 Explore More
https://www.youtube.com/watch?v=WVrlHH14q3o&feature=emb_logo
Great Glands - Your Endocrine System: CrashCourse Biology #33, CrashCourse, 2012.
https://www.youtube.com/watch?v=qXaDDa3FB5Q&feature=emb_logo
National Geographic | Benefits and Side Effects of Steroids Use 2015, 24 Physic.
Attributions
Figure 9.3.1
L0058274 Glass bottle for ‘Progynon’ pills, United Kingdom, 1928-1948 by Wellcome Collection gallery (2018-03-29)/ Science Museum, London on Wikimedia Commons is used under a CC-BY-4.0 (https://creativecommons.org/licenses/by/4.0/) license.
Figure 9.3.2
Regulation_of_gene_expression_by_steroid_hormone_receptor.svg by Ali Zifan on Wikimedia Commons is used under a CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0/deed.en) license.
Figure 9.3.3
Non-steroid hormone pathway by CK-12 Foundation, Biology for High School is used under a CC BY-NC 3.0 (https://creativecommons.org/licenses/by-nc/3.0/) license.
Figure 9.3.4
Thyroid Negative Feedback Loop by CK-12 Foundation, College Human Biology is used under a CC BY-NC 3.0 (https://creativecommons.org/licenses/by-nc/3.0/) license.
 ©CK-12 Foundation Licensed under
©CK-12 Foundation Licensed under ![]() • Terms of Use • Attribution
• Terms of Use • Attribution
Figure 9.3.5
Lactation Positive Feedback Loop by Christinelmiller on Wikimedia Commons is used under a CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0/deed.en) license.
References
24 Physic. (2015,July 19). National Geographic | Benefits and side effects of steroids use 2015. YouTube. https://www.youtube.com/watch?v=qXaDDa3FB5Q&feature=youtu.be
Brainard, J/ CK-12 Foundation. (2016, August 15). Figure 4 Thyroid negative feedback loop [digital image]. In CK-12 College Human Biology (Section 11.3 Endocrine hormones). CK12.org. https://www.ck12.org/book/ck-12-human-biology/section/11.3/
CK-12 Foundation. (2019, March 5). Figure 3 A non-steroid hormone binds with a receptor on the plasma membrane of a target cell [digital image]. In Flexbook 2.0: CK-12 Biology For High School (Section 13.21 Hormone). CK12. https://flexbooks.ck12.org/cbook/ck-12-biology-flexbook-2.0/section/13.21/primary/lesson/hormones-bio
CrashCourse. (2012, September 10). Great glands - Your endocrine system: CrashCourse Biology #33. YouTube. https://www.youtube.com/watch?v=WVrlHH14q3o&feature=youtu.be
TED-Ed. (2018, June 21). How do your hormones work? - Emma Bryce. YouTube. https://www.youtube.com/watch?v=-SPRPkLoKp8&feature=youtu.be
Image shows a diagram of the brain highlighting the region containing the hypothalamus and pituitary gland.
Foreign proteins on the surface of a cell that triggers an immune response.
The process by which information from a gene is used in the synthesis of a functional protein.
An antibody, also known as an immunoglobulin, is a large, Y-shaped protein produced mainly by plasma cells that is used by the immune system to neutralize pathogens such as pathogenic bacteria and viruses.
Created by CK-12 Foundation/Adapted by Christine Miller

Milk on Demand
This adorable nursing infant (Figure 9.4.1) is part of a positive feedback loop. When he suckles on the nipple, it sends nerve impulses to his mother’s hypothalamus. Those nerve impulses “tell” her pituitary gland to release the hormone prolactin into her bloodstream. Prolactin travels to the mammary glands in the breasts and stimulates milk production, which motivates the infant to keep suckling.
What Is the Pituitary Gland?
The pituitary gland is the master gland of the endocrine system, which is the system of glands that secrete hormones into the bloodstream. Endocrine hormones control virtually all physiological processes. They control growth, sexual maturation, reproduction, body temperature, blood pressure, and metabolism. The pituitary gland is considered the master gland of the endocrine system, because it controls the rest of the endocrine system. Many pituitary hormones either promote or inhibit hormone secretion by other endocrine glands.
Structure and Function of the Pituitary Gland
The pituitary gland is about the size of a pea. It protrudes from the bottom of the hypothalamus at the base of the inner brain (see Figure 9.4.2). The pituitary is connected to the hypothalamus by a thin stalk (called the infundibulum). Blood vessels and nerves in the stalk allow direct connections between the hypothalamus and pituitary gland.
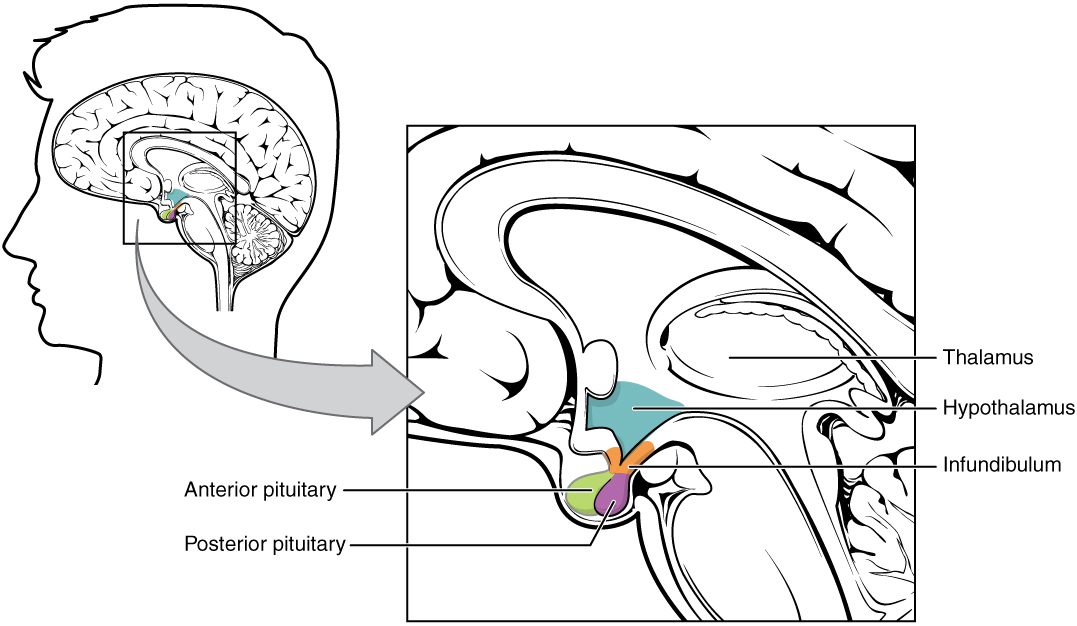
Anterior Lobe
The anterior pituitary is the lobe is at the front of the pituitary gland. It synthesizes and releases hormones into the blood. Table 9.4.1 shows some of the endocrine hormones released by the anterior pituitary, including their targets and effects.
Table 9.4.1
Endocrine Hormones Released by the Anterior Pituitary, and Their Targets and Effects.
| Anterior Pituitary Hormone | Target | Effect |
| Adrenocorticotropic hormone (ACTH) | Adrenal glands | Stimulates the cortex of each adrenal gland to secrete its hormones. |
| Thyroid-stimulating hormone (TSH) | Thyroid gland | Stimulates the thyroid gland to secrete thyroid hormone. |
| Growth hormone (GH) | Body cells | Stimulates body cells to synthesize proteins and grow. |
| Follicle-stimulating hormone (FSH) | Ovaries, testes | Stimulates the ovaries to develop mature eggs. stimulates the testes to produce sperm. |
| Luteinizing hormone (LH) | Ovaries, testes | Stimulates the ovaries and testes to secrete sex hormones; stimulates the ovaries to release eggs. |
| Prolactin (PRL) | Mammary glands | Stimulates the mammary glands to produce milk. |
The anterior pituitary gland is regulated mainly by hormones from the hypothalamus. The hypothalamus secretes hormones (called releasing hormones and inhibiting hormones) that travel through capillaries directly to the anterior lobe of the pituitary gland. The hormones stimulate the anterior pituitary to either release or stop releasing particular pituitary hormones. Several of these hypothalamic hormones and their effects on the anterior pituitary are shown in the table below.
Table 9.4.2
Hypothalamic Hormones and Their Effects on the Anterior Pituitary
| Hypothalamic Hormone | Effect on Anterior Pituitary |
| Thyrotropin releasing hormone (TRH) | Release of thyroid stimulating hormone (TSH) |
| Corticotropin releasing hormone (CRH) | Release of adrenocorticotropic hormone (ACTH) |
| Gonadotropin releasing hormone (GnRH) | Release of follicle-stimulating hormone (FSH) and luteinizing hormone (LH) |
| Growth hormone releasing hormone (GHRH) | Release of growth hormone (GH) |
| Growth hormone inhibiting hormone (GHIH) (Somatostatin) | Stopping of growth hormone release |
| Prolactin releasing hormone (PRH) | Release of prolactin |
| Prolactin inhibiting hormone (PIH) (Dopamine) | Stopping of prolactin release |
Posterior Lobe
The posterior pituitary is the lobe is at the back of the pituitary gland. This lobe does not synthesize any hormones. Instead, the posterior lobe stores hormones that come from the hypothalamus along the axons of nerves connecting the two structures (also shown in Figure 9.4.2). The posterior pituitary then secretes the hormones into the bloodstream as needed. Hypothalamic hormones secreted by the posterior pituitary include vasopressin and oxytocin.
- Vasopressin (also called antidiuretic hormone, or ADH) helps maintain homeostasis in body water. It stimulates the kidneys to conserve water by producing more concentrated urine. Specifically, vasopressin targets ducts in the kidneys and makes them more permeable to water. This allows more water to be resorbed by the body, rather than excreted in urine.
- Oxytocin (OXY) targets cells in the uterus to stimulate uterine contractions, as in childbirth. It also targets cells in the breasts of a nursing mother to stimulate the letdown of milk.
9.4 Summary
- The pituitary gland is the master gland of the endocrine system, because most of its hormones control other endocrine glands.
- The pituitary gland is at the base of the brain, where it is connected to the hypothalamus by nerves and capillaries. It has an anterior (front) lobe that synthesizes and secretes pituitary hormones and a posterior (back) lobe that stores and secretes hormones from the hypothalamus.
- Hormones synthesized and secreted by the anterior pituitary include growth hormone, which stimulates cell growth throughout the body, and thyroid stimulating hormone (TSH), which stimulates the thyroid gland to secrete its hormones.
- Hypothalamic hormones stored and secreted by the posterior pituitary gland include vasopressin, which helps maintain homeostasis in body water, and oxytocin, which stimulates uterine contractions during birth, as well as the letdown of milk during lactation.
9.4 Review Questions
-
-
- Explain why the pituitary gland is called the master gland of the endocrine system.
- Compare and contrast the two lobes of the pituitary gland and their general functions.
- Identify two hormones released by the anterior pituitary, their targets, and their effects.
- Explain how the hypothalamus influences the output of hormones by the anterior lobe of the pituitary gland.
- Name and give the function of two hypothalamic hormones released by the posterior pituitary gland.
- Answer the following questions about prolactin releasing hormone (PRH) and prolactin inhibiting hormone (PIH).
- Where are these hormones produced?
- Where are their target cells located?
- What are their effects on their target cells?
- What are their ultimate effects on milk production? Explain your answer.
- When a baby nurses, which of these hormones is most likely released in the mother? Explain your answer.
- For each of the following hormones, state whether it is synthesized in the pituitary or the hypothalamus.
- gonadotropin releasing hormone (GnRH)
- growth hormone (GH)
- oxytocin
- adrenocorticotropic hormone (ACTH)
9.4 Explore More
https://www.youtube.com/watch?v=jUKQFkmBuww&feature=emb_logo
Common Pituitary Diseases, Swedish, 2012.
https://www.youtube.com/watch?v=v41AJGP-XmI&feature=emb_logo
Diagnosing and Treating Pituitary Tumors - California Center for Pituitary Disorders at UCSF, UCSF Neurosurgery, 2015.
Attributions
Figure 9.4.1
Breastfeeding by Petr Kratochvil on Wikimedia Commons is used under a CC0 1.0 Universal
Public Domain Dedication (https://creativecommons.org/publicdomain/zero/1.0/deed.en) license.
Figure 9.4.2
The_Hypothalamus-Pituitary_Complex by OpenStax College on Wikimedia Commons is used under a CC BY 3.0 (https://creativecommons.org/licenses/by/3.0) license.
References
Betts, J. G., Young, K.A., Wise, J.A., Johnson, E., Poe, B., Kruse, D.H., Korol, O., Johnson, J.E., Womble, M., DeSaix, P. (2013, June 19). Figure 17.7 Hypothalamus–pituitary complex [digital image]. In Anatomy and Physiology (Section 17.3). OpenStax. https://openstax.org/books/anatomy-and-physiology/pages/17-3-the-pituitary-gland-and-hypothalamus
Swedish. (2012, April 19). Common pituitary diseases. YouTube. https://www.youtube.com/watch?v=jUKQFkmBuww&feature=youtu.be
UCSF Neurosurgery. (2015, May 13). Diagnosing and treating pituitary tumors - California Center for Pituitary Disorders at UCSF. YouTube. https://www.youtube.com/watch?v=v41AJGP-XmI&feature=youtu.be
Created by: CK-12/Adapted by Christine Miller

Like Pushing a Humvee Uphill
You can tell by their faces that these airmen (Figure 4.8.1) are expending a lot of energy trying to push this Humvee up a slope. The men are participating in a competition that tests their brute strength against that of other teams. The Humvee weighs about 13 thousand pounds (about 5,897 kilograms), so it takes every ounce of energy they can muster to move it uphill against the force of gravity. Transport of some substances across a plasma membrane is a little like pushing a Humvee uphill — it can't be done without adding energy.
What Is Active Transport?
Some substances can pass into or out of a cell across the plasma membrane without any energy required because they are moving from an area of higher concentration to an area of lower concentration. This type of transport is called passive transport. Other substances require energy to cross a plasma membrane, often because they are moving from an area of lower concentration to an area of higher concentration, against the concentration gradient. This type of transport is called active transport. The energy for active transport comes from the energy-carrying molecule called ATP (adenosine triphosphate). Active transport may also require proteins called pumps, which are embedded in the plasma membrane. Two types of active transport are membrane pumps (such as the sodium-potassium pump) and vesicle transport.
The Sodium-Potassium Pump
The sodium-potassium pump is a mechanism of active transport that moves sodium ions out of the cell and potassium ions into the cells — in all the trillions of cells in the body! Both ions are moved from areas of lower to higher concentration, so energy is needed for this "uphill" process. The energy is provided by ATP. The sodium-potassium pump also requires carrier proteins. Carrier proteins bind with specific ions or molecules, and in doing so, they change shape. As carrier proteins change shape, they carry the ions or molecules across the membrane. Figure 4.8.2 shows in greater detail how the sodium-potassium pump works, as well as the specific roles played by carrier proteins in this process.
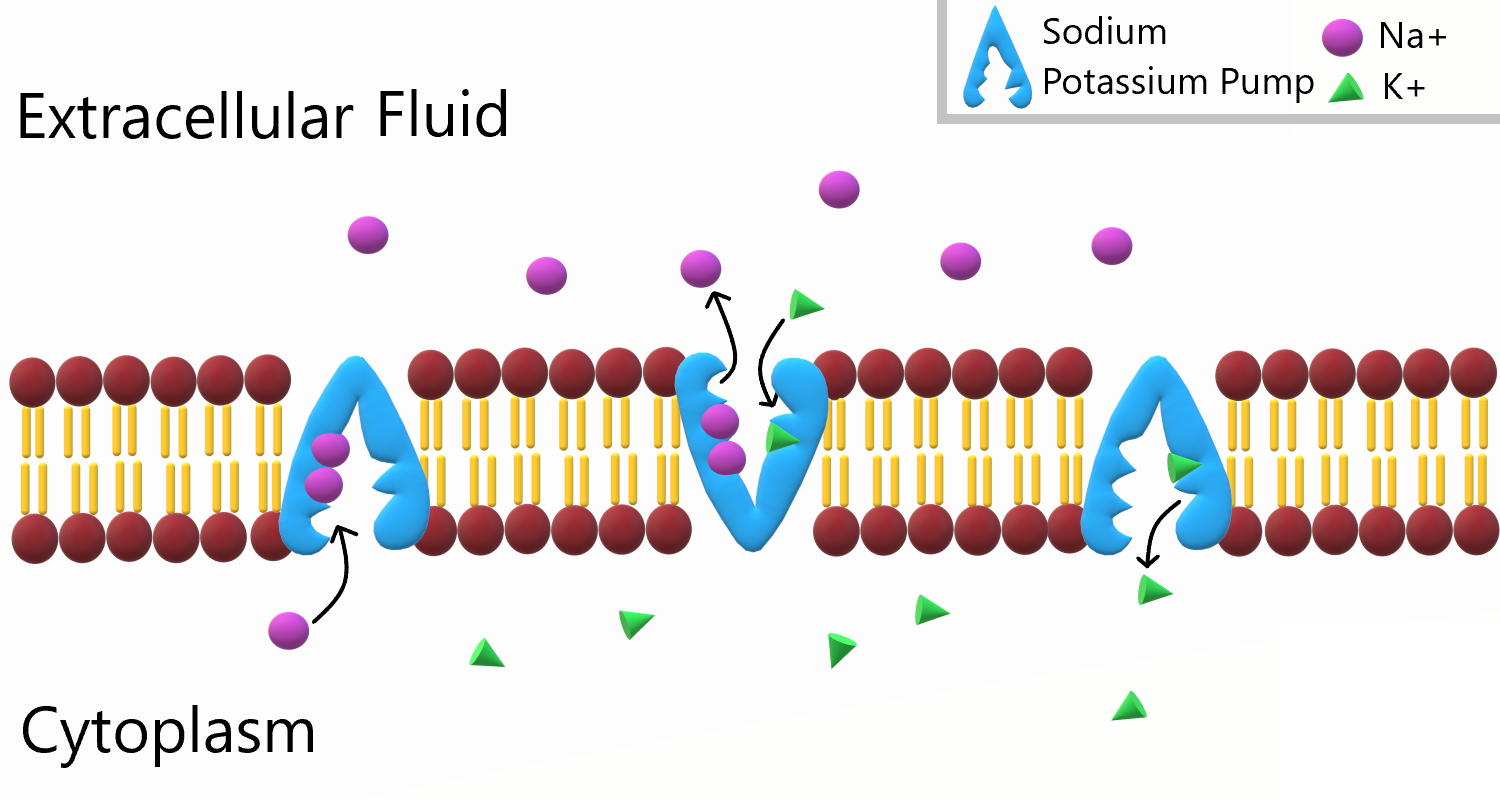
To appreciate the importance of the sodium-potassium pump, you need to know more about the roles of sodium and potassium in the body. Both are essential dietary minerals. You need to get them from the foods you eat. Both sodium and potassium are also electrolytes, which means they dissociate into ions (charged particles) in solution, allowing them to conduct electricity. Normal body functions require a very narrow range of concentrations of sodium and potassium ions in body fluids, both inside and outside of cells.
- Sodium is the principal ion in the fluid outside of cells. Normal sodium concentrations are about ten times higher outside of cells than inside of cells. To move sodium out of the cell is moving it against the concentration gradient
- Potassium is the principal ion in the fluid inside of cells. Normal potassium concentrations are about 30 times higher inside of cells than outside of cells. To move potassium into the cell is moving it against the concentration gradient.
These differences in concentration create an electrical and chemical gradient across the cell membrane, called the membrane potential. Tightly controlling the membrane potential is critical for vital body functions, including the transmission of nerve impulses and contraction of muscles. A large percentage of the body's energy goes to maintaining this potential across the membranes of its trillions of cells with the sodium-potassium pump.
Vesicle Transport
Some molecules, such as proteins, are too large to pass through the plasma membrane, regardless of their concentration inside and outside the cell. Very large molecules cross the plasma membrane with a different sort of help, called vesicle transport. Vesicle transport requires energy input from the cell, so it is also a form of active transport. There are two types of vesicle transport: endocytosis and exocytosis. Both types are shown in Figure 4.8.3.
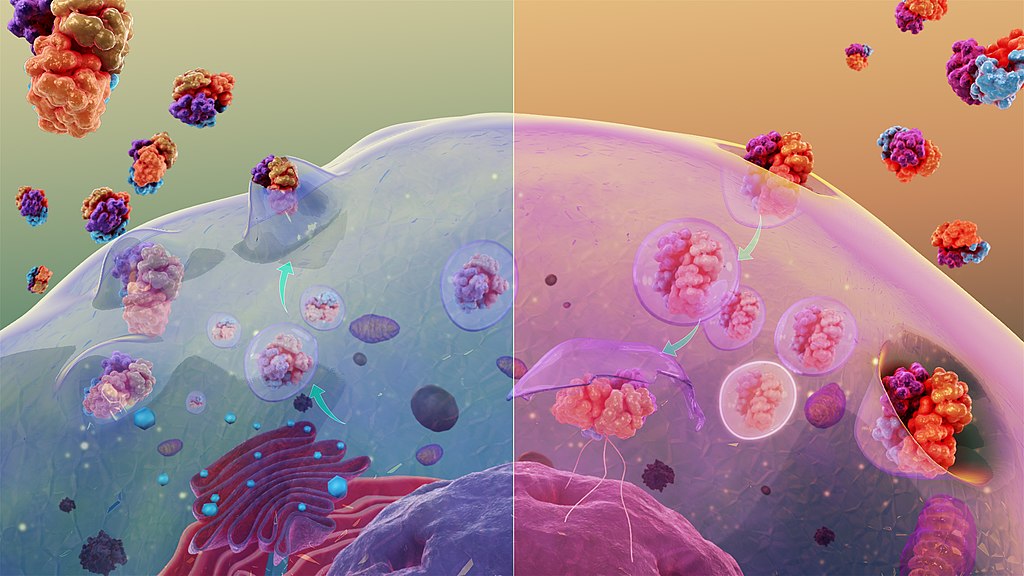
Endocytosis
Endocytosis is a type of vesicle transport that moves a substance into the cell. The plasma membrane completely engulfs the substance, a vesicle pinches off from the membrane, and the vesicle carries the substance into the cell. When an entire cell or other solid particle is engulfed, the process is called phagocytosis. When fluid is engulfed, the process is called pinocytosis.
Exocytosis
Exocytosis is a type of vesicle transport that moves a substance out of the cell (exo-, like "exit"). A vesicle containing the substance moves through the cytoplasm to the cell membrane. Because the vesicle membrane is a phospholipid bilayer like the plasma membrane, the vesicle membrane fuses with the cell membrane, and the substance is released outside the cell.
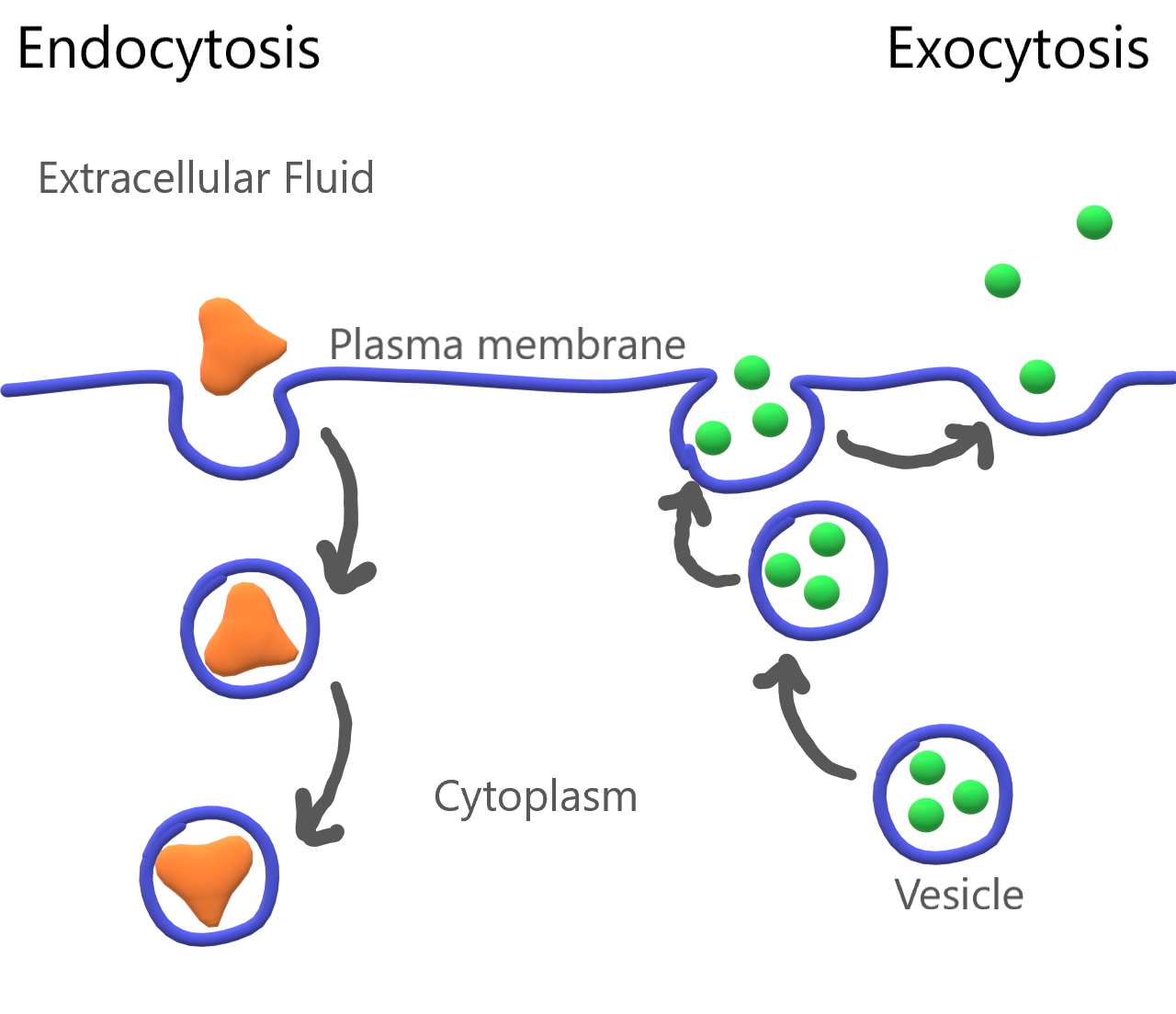
Feature: My Human Body
Maintaining the proper balance of sodium and potassium in body fluids by active transport is necessary for life itself, so it's no surprise that getting the right balance of sodium and potassium in the diet is important for good health. Imbalances may increase the risk of high blood pressure, heart disease, diabetes, and other disorders.
If you are like the majority of North Americans, sodium and potassium are out of balance in your diet. You are likely to consume too much sodium and too little potassium. Follow these guidelines to help ensure that these minerals are balanced in the foods you eat:
- Total sodium intake should be less than 2,300 mg/day. Most salt in the diet is found in processed foods, or added with a salt shaker. Stop adding salt and start checking food labels for sodium content. Foods considered low in sodium have less than 140 mg/serving (or 5 per cent daily value).
- Total potassium intake should be 4,700 mg/day. It's easy to add potassium to the diet by choosing the right foods — and there are plenty of choices! Most fruits and vegetables are high in potassium. Potatoes, bananas, oranges, apricots, plums, leafy greens, tomatoes, lima beans, and avocado are especially good sources. Other foods with substantial amounts of potassium are fish, meat, poultry, and whole grains. The collage below shows some of these potassium-rich foods.
Figure 4.8.5 Potassium power!
4.8 Summary
- Active transport requires energy to move substances across a plasma membrane, often because the substances are moving from an area of lower concentration to an area of higher concentration, or because of their large size. Two types of active transport are membrane pumps (such as the sodium-potassium pump) and vesicle transport.
- The sodium-potassium pump is a mechanism of active transport that moves sodium ions out of the cell and potassium ions into the cell against a concentration gradient, in order to maintain the proper concentrations of ions, both inside and outside the cell, and to thereby control membrane potential.
- Vesicle transport is a type of active transport that uses vesicles to move large molecules into or out of cells.
4.8 Review Questions
- Define active transport.
-
- What is the sodium-potassium pump? Why is it so important?
- The drawing below shows the fluid inside and outside of a cell. The dots represent molecules of a substance needed by the cell. Explain which type of transport — active or passive — is needed to move the molecules into the cell.
Figure 4.8.6 Use this image to answer question #4 - What are the similarities and differences between phagocytosis and pinocytosis?
- What is the functional significance of the shape change of the carrier protein in the sodium-potassium pump after the sodium ions bind?
- A potentially deadly poison derived from plants called ouabain blocks the sodium-potassium pump and prevents it from working. What do you think this does to the sodium and potassium balance in cells? Explain your answer.
4.8 Explore More
https://www.youtube.com/watch?v=Z_mXDvZQ6dU&feature=emb_logo
Neutrophil Phagocytosis - White Blood Cell Eats Staphylococcus Aureus Bacteria,
ImmiflexImmuneSystem, 2013.
https://www.youtube.com/watch?v=Ptmlvtei8hw
Cell Transport, The Amoeba Sisters, 2016.
Attributions
Figure 4.8.1
Humvee challenge by Airman 1st Class Collin Schmidt on Wikimedia Commons is released into the public domain (https://en.wikipedia.org/wiki/Public_domain).
Figure 4.8.2
Sodium Potassium Pump by Christine Miller is used under a CC BY 4.0 (https://creativecommons.org/licenses/by/4.0/) license.
Figure 4.8.3
Cytosis by Manu5 on Wikimedia Commons is used under a CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0) license.
Figure 4.8.4
Endocytosis and Exocytosis by Christine Miller is used under a CC BY 4.0 (https://creativecommons.org/licenses/by/4.0/) license.
Figure 4.8.5
- Canteloupes. Image Number K7355-11 by Scott Bauer/ USDA on Wikimedia Commons is in the public domain (https://en.wikipedia.org/wiki/Public_domain).
- Spinach by chiara conti on Unsplash is used under the Unsplash license (https://unsplash.com/license).
- Eleven long purple eggplants by JVRKPRASAD on Wikimedia commons is used under a CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0/deed.en) license.
- Bananas by Marco Antonio Victorino on Pexels is used under the Pexels license (https://www.pexels.com/license/).
- Potato picking by Nic D on Unsplash is used under the Unsplash license (https://unsplash.com/license).
- Maldives by Sebastian Pena Lambarri on Unsplash is used under the Unsplash license (https://unsplash.com/license).
Figure 4.8.6
Active Transport by Christine Miller is released into the public domain (https://en.wikipedia.org/wiki/Public_domain).
References
Amoeba Sisters. (2016, June 24). Cell transport [digital image]. YouTube. https://www.youtube.com/watch?v=Ptmlvtei8hw&feature=youtu.be
ImmiflexImmuneSystem. (2013). Neutrophil phagocytosis - White blood cell eats staphylococcus aureus bacteria. YouTube. https://www.youtube.com/watch?v=Z_mXDvZQ6dU
Mayo Clinic Staff. (n.d.). Diabetes [online]. MayoClinic.org. https://www.mayoclinic.org/diseases-conditions/diabetes/symptoms-causes/syc-20371444
Mayo Clinic Staff. (n.d.). High blood pressure (hypertension) [online]. MayoClinic.org. https://www.mayoclinic.org/diseases-conditions/high-blood-pressure/symptoms-causes/syc-20373410
Mayo Clinic Staff. (n.d.). Heart disease [online]. MayoClinic.org. https://www.mayoclinic.org/diseases-conditions/heart-disease/symptoms-causes/syc-20353118
Wikipedia contributors. (2020, June 19). Ouabain. In Wikipedia. https://en.wikipedia.org/w/index.php?title=Ouabain&oldid=963440756
Refers to the body system consisting of the heart, blood vessels and the blood. Blood contains oxygen and other nutrients which your body needs to survive. The body takes these essential nutrients from the blood.
A body system including a series of hollow organs joined in a long, twisting tube from the mouth to the anus. The hollow organs that make up the GI tract are the mouth, esophagus, stomach, small intestine, large intestine, and anus. The liver, pancreas, and gallbladder are the solid organs of the digestive system.
The smallest type of blood vessel that connects arterioles and venules and that transfers substances between blood and tissues.
Image shows a diagram of the hormones secreted by the thyroid gland, and how it is both controlled by and acting upon in a negative feedback the hypothalamus and the anterior pituitary gland.
Image shows a photograph of a women with a goiter. The centre bottom of her throat has a visible enlargement.
Created by CK-12 Foundation/Adapted by Christine Miller

Steady as She Goes
This device (Figure 7.8.1) looks simple, but it controls a complex system that keeps a home at a steady temperature — it's a thermostat. The device shows the current temperature in the room, and also allows the occupant to set the thermostat to the desired temperature. A thermostat is a commonly cited model of how living systems — including the human body— maintain a steady state called homeostasis.
What Is Homeostasis?
Homeostasis is the condition in which a system (such as the human body) is maintained in a more or less steady state. It is the job of cells, tissues, organs, and organ systems throughout the body to maintain many different variables within narrow ranges compatible with life. Keeping a stable internal environment requires continually monitoring the internal environment and constantly making adjustments to keep things in balance.
Set Point and Normal Range
For any given variable, such as body temperature or blood glucose level, there is a particular set point that is the physiological optimum value. The set point for human body temperature, for example, is about 37 degrees C (98.6 degrees F). As the body works to maintain homeostasis for temperature or any other internal variable, the value typically fluctuates around the set point. Such fluctuations are normal, as long as they do not become too extreme. The spread of values within which such fluctuations are considered insignificant is called the normal range. In the case of body temperature, for example, the normal range for an adult is about 36.5 to 37.5 degrees C (97.7 to 99.5 degrees F).
A good analogy for set point, normal range, and maintenance of homeostasis is driving. When you are driving a vehicle on the road, you are supposed to drive in the centre of your lane — this is analogous to the set point. Sometimes, you are not driving in the exact centre of the lane, but you are still within your lines, so you are in the equivalent of the normal range. However, if you were to get too close to the centre line or the shoulder of the road, you would take action to correct your position. You'd move left if you were too close to the shoulder, or right if too close to the centre line — which is analogous to our next concept, negative feedback to maintain homeostasis.
Maintaining Homeostasis
Homeostasis is normally maintained in the human body by an extremely complex balancing act. Regardless of the variable being kept within its normal range, maintaining homeostasis requires at least four interacting components: stimulus, sensor, control centre, and effector.
- The stimulus is provided by the variable being regulated. Generally, the stimulus indicates that the value of the variable has moved away from the set point or has left the normal range.
- The sensor monitors the values of the variable and sends data on it to the control centre.
- The control centre matches the data with normal values. If the value is not at the set point or is outside the normal range, the control centre sends a signal to the effector.
- The effector is an organ, gland, muscle, or other structure that acts on the signal from the control centre to move the variable back toward the set point.
Each of these components is illustrated in Figure 7.8.2. The diagram on the left is a general model showing how the components interact to maintain homeostasis. The diagram on the right shows the example of body temperature. From the diagrams, you can see that maintaining homeostasis involves feedback, which is data that feeds back to control a response. Feedback may be negative (as in the example below) or positive. All the feedback mechanisms that maintain homeostasis use negative feedback. Biological examples of positive feedback are much less common.
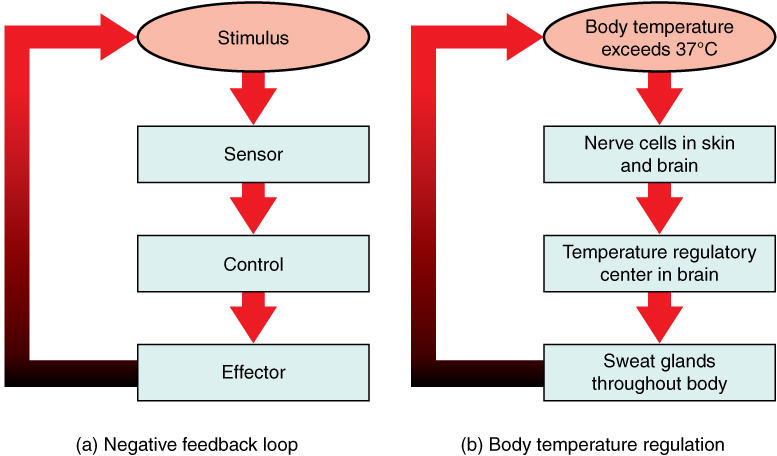
Negative Feedback
In a negative feedback loop, feedback serves to reduce an excessive response and keep a variable within the normal range. Two processes controlled by negative feedback are body temperature regulation and control of blood glucose.
Body Temperature
Body temperature regulation involves negative feedback, whether it lowers the temperature or raises it, as shown in Figure 7.8.3 and explained in the text that follows.
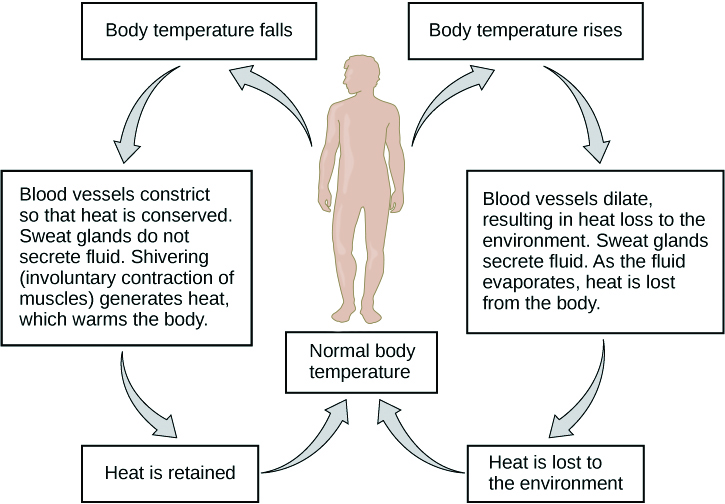
Cooling Down
The human body’s temperature regulatory centre is the hypothalamus in the brain. When the hypothalamus receives data from sensors in the skin and brain that body temperature is higher than the set point, it sets into motion the following responses:
- Blood vessels in the skin dilate (vasodilation) to allow more blood from the warm body core to flow close to the surface of the body, so heat can be radiated into the environment.
- As blood flow to the skin increases, sweat glands in the skin are activated to increase their output of sweat (diaphoresis). When the sweat evaporates from the skin surface into the surrounding air, it takes heat with it.
- Breathing becomes deeper, and the person may breathe through the mouth instead of the nasal passages. This increases heat loss from the lungs.
Heating Up
When the brain’s temperature regulatory centre receives data that body temperature is lower than the set point, it sets into motion the following responses:
- Blood vessels in the skin contract (vasoconstriction) to prevent blood from flowing close to the surface of the body, which reduces heat loss from the surface.
- As temperature falls lower, random signals to skeletal muscles are triggered, causing them to contract. This causes shivering, which generates a small amount of heat.
- The thyroid gland may be stimulated by the brain (via the pituitary gland) to secrete more thyroid hormone. This hormone increases metabolic activity and heat production in cells throughout the body.
- The adrenal glands may also be stimulated to secrete the hormone adrenaline. This hormone causes the breakdown of glycogen (the carbohydrate used for energy storage in animals) to glucose, which can be used as an energy source. This catabolic chemical process is exothermic, or heat producing.
Blood Glucose
In controlling the blood glucose level, certain endocrine cells in the pancreas (called alpha and beta cells) detect the level of glucose in the blood. They then respond appropriately to keep the level of blood glucose within the normal range.
- If the blood glucose level rises above the normal range, pancreatic beta cells release the hormone insulin into the bloodstream. Insulin signals cells to take up the excess glucose from the blood until the level of blood glucose decreases to the normal range.
- If the blood glucose level falls below the normal range, pancreatic alpha cells release the hormone glucagon into the bloodstream. Glucagon signals cells to break down stored glycogen to glucose and release the glucose into the blood until the level of blood glucose increases to the normal range.
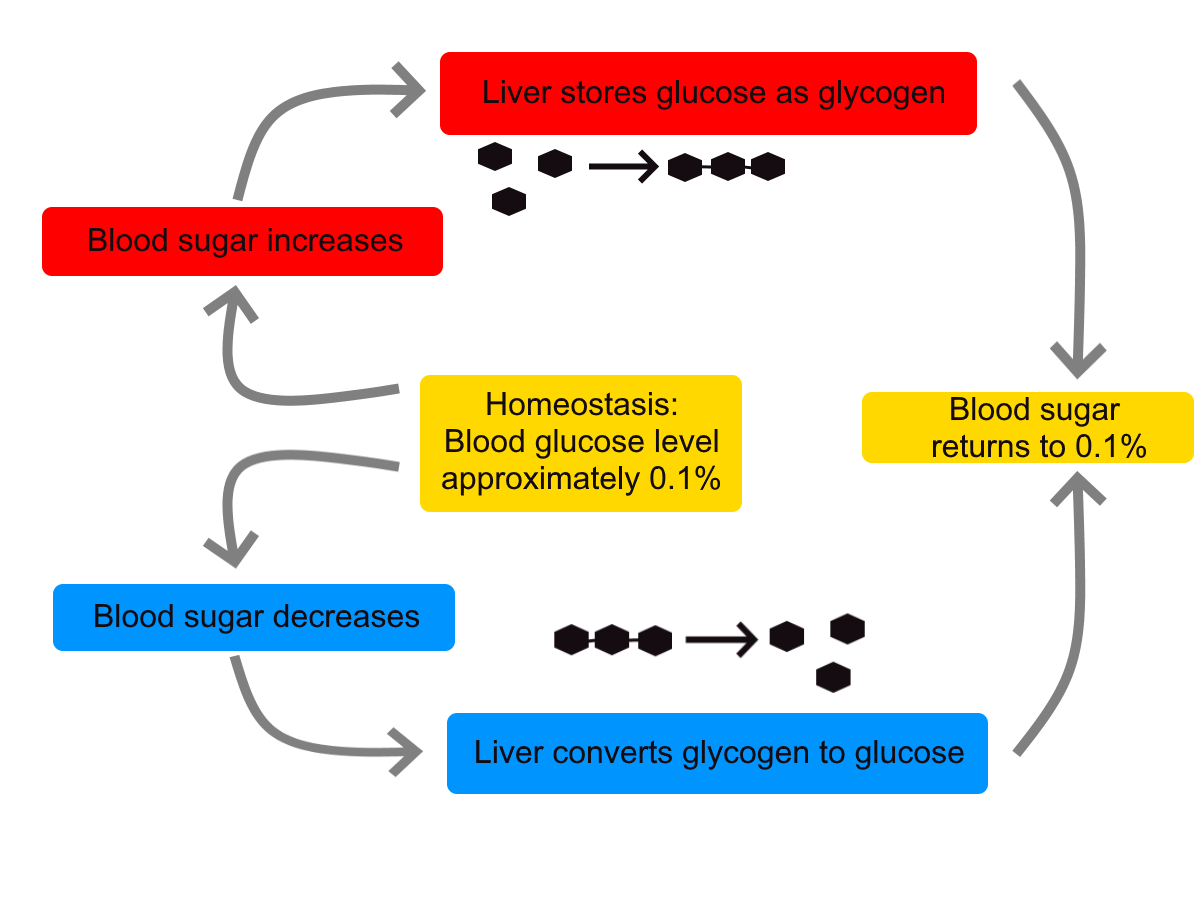
https://www.youtube.com/watch?v=Iz0Q9nTZCw4
Homeostasis and Negative/Positive Feedback, Amoeba Sisters, 2017.
Positive Feedback
In a positive feedback loop, feedback serves to intensify a response until an end point is reached. Examples of processes controlled by positive feedback in the human body include blood clotting and childbirth.
Blood Clotting
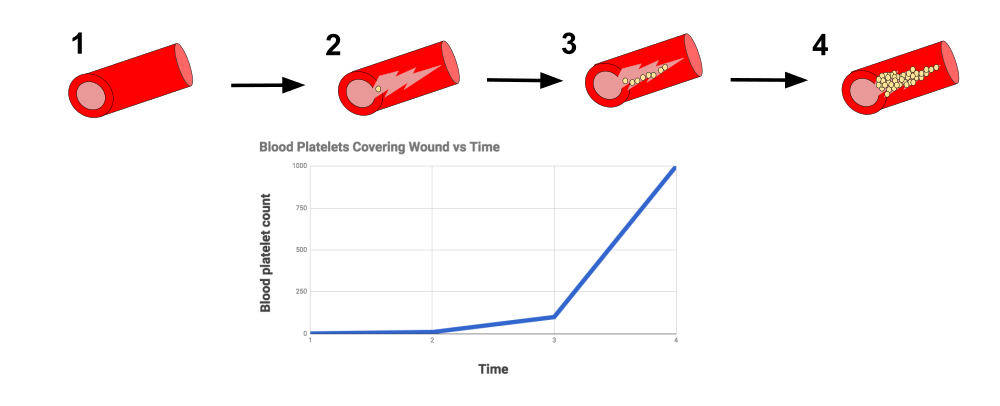
When a wound causes bleeding, the body responds with a positive feedback loop to clot the blood and stop blood loss. Substances released by the injured blood vessel wall begin the process of blood clotting. Platelets in the blood start to cling to the injured site and release chemicals that attract additional platelets. As the platelets continue to amass, more of the chemicals are released and more platelets are attracted to the site of the clot. The positive feedback accelerates the process of clotting until the clot is large enough to stop the bleeding.
Childbirth
Figure 7.8.6 shows the positive feedback loop that controls childbirth. The process normally begins when the head of the infant pushes against the cervix. This stimulates nerve impulses, which travel from the cervix to the hypothalamus in the brain. In response, the hypothalamus sends the hormone oxytocin to the pituitary gland, which secretes it into the bloodstream so it can be carried to the uterus. Oxytocin stimulates uterine contractions, which push the baby harder against the cervix. In response, the cervix starts to dilate in preparation for the passage of the baby. This cycle of positive feedback continues, with increasing levels of oxytocin, stronger uterine contractions, and wider dilation of the cervix until the baby is pushed through the birth canal and out of the body. At that point, the cervix is no longer stimulated to send nerve impulses to the brain, and the entire process stops.
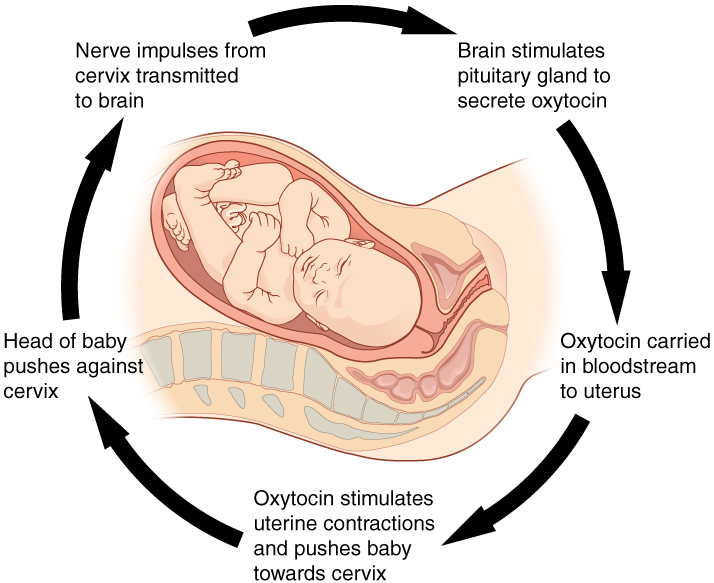
Normal childbirth is driven by a positive feedback loop. Positive feedback causes an increasing deviation from the normal state to a fixed end point, rather than a return to a normal set point as in homeostasis.
When Homeostasis Fails
Homeostatic mechanisms work continuously to maintain stable conditions in the human body. Sometimes, however, the mechanisms fail. When they do, homeostatic imbalance may result, in which cells may not get everything they need or toxic wastes may accumulate in the body. If homeostasis is not restored, the imbalance may lead to disease — or even death. Diabetes is an example of a disease caused by homeostatic imbalance. In the case of diabetes, blood glucose levels are no longer regulated and may be dangerously high. Medical intervention can help restore homeostasis and possibly prevent permanent damage to the organism.
Normal aging may bring about a reduction in the efficiency of the body’s control systems, which makes the body more susceptible to disease. Older people, for example, may have a harder time regulating their body temperature. This is one reason they are more likely than younger people to develop serious heat-induced illnesses, such as heat stroke.
Feature: My Human Body
Diabetes is diagnosed in people who have abnormally high levels of blood glucose after fasting for at least 12 hours. A fasting level of blood glucose below 100 is normal. A level between 100 and 125 places you in the pre-diabetes category, and a level higher than 125 results in a diagnosis of diabetes.
Of the two types of diabetes, type 2 diabetes is the most common, accounting for about 90 per cent of all cases of diabetes in the United States. Type 2 diabetes typically starts after the age of 40. However, because of the dramatic increase in recent decades in obesity in younger people, the age at which type 2 diabetes is diagnosed has fallen. Even children are now being diagnosed with type 2 diabetes. Today, about 3 million Canadians (8.1% of total population) are living with diabetes.
You may at some point have your blood glucose level tested during a routine medical exam. If your blood glucose level indicates that you have diabetes, it may come as a shock to you because you may not have any symptoms of the disease. You are not alone, because as many as one in four diabetics do not know they have the disease. Once the diagnosis of diabetes sinks in, you may be devastated by the news. Diabetes can lead to heart attacks, strokes, blindness, kidney failure, nerve damage, and loss of toes or feet. The risk of death in adults with diabetes is 50 per cent greater than it is in adults without diabetes, and diabetes is the seventh leading cause of death of adults. In addition, controlling diabetes usually requires frequent blood glucose testing, watching what and when you eat, and taking medications or even insulin injections. All of this may seem overwhelming.
The good news is that changing your lifestyle may stop the progression of type 2 diabetes or even reverse it. By adopting healthier habits, you may be able to keep your blood glucose level within the normal range without medications or insulin. Here’s how:
- Lose weight. Any weight loss is beneficial. Losing as little as seven per cent of your weight may be all that is needed to stop diabetes in its tracks. It is especially important to eliminate excess weight around your waist.
- Exercise regularly. You should try to exercise for at least 30 minutes, five days a week. This will not only lower your blood sugar and help your insulin work better, but it will also lower your blood pressure and improve your heart health. Another bonus of exercise is that it will help you lose weight by increasing your basal metabolic rate.
- Adopt a healthy diet. Decrease your consumption of refined carbohydrates, such as sweets and sugary drinks. Increase your intake of fibre-rich foods, such as fruits, vegetables, and whole grains. About one-quarter of each meal should consist of high-protein foods, such as fish, chicken, dairy products, legumes, or nuts.
- Control stress. Stress can increase your blood glucose and also raise your blood pressure and risk of heart disease. When you feel stressed out, do breathing exercises or take a brisk walk or jog. Try to replace stressful thoughts with more calming ones.
- Establish a support system. Enlist the help and support of loved ones, as well as medical professionals, such as a nutritionist and diabetes educator. Having a support system will help ensure that you are on the path to wellness, and that you can stick to your plan.
7.8 Summary
- Homeostasis is the condition in which a system (such as the human body) is maintained in a more or less steady state. It is the job of cells, tissues, organs, and organ systems throughout the body to maintain homeostasis.
- For any given variable, such as body temperature, there is a particular set point that is the physiological optimum value. The spread of values around the set point that is considered insignificant is called the normal range.
- Homeostasis is generally maintained by a negative feedback loop that includes a stimulus, sensor, control centre, and effector. Negative feedback serves to reduce an excessive response and to keep a variable within the normal range. Negative feedback loops control body temperature and the blood glucose level.
- Positive feedback loops are not common in biological systems. Positive feedback serves to intensify a response until an end point is reached. Positive feedback loops control blood clotting and childbirth.
- Sometimes homeostatic mechanisms fail, resulting in homeostatic imbalance. Diabetes is an example of a disease caused by homeostatic imbalance. Aging can bring about a reduction in the efficiency of the body’s control system, which makes the elderly more susceptible to disease.
7.8 Review Questions
-
-
- Compare and contrast negative and positive feedback loops.
- Explain how negative feedback controls body temperature.
- Give two examples of physiological processes controlled by positive feedback loops.
- During breastfeeding, the stimulus of the baby sucking on the nipple increases the amount of milk produced by the mother. The more sucking, the more milk is usually produced. Is this an example of negative or positive feedback? Explain your answer. What do you think might be the evolutionary benefit of the milk production regulation mechanism you described?
- Explain why homeostasis is regulated by negative feedback loops, rather than positive feedback loops.
- The level of a sex hormone, testosterone (T), is controlled by negative feedback. Another hormone, gonadotropin-releasing hormone (GnRH), is released by the hypothalamus of the brain, which triggers the pituitary gland to release luteinizing hormone (LH). LH stimulates the gonads to produce T. When there is too much T in the bloodstream, it feeds back on the hypothalamus, causing it to produce less GnRH. While this does not describe all the feedback loops involved in regulating T, answer the following questions about this particular feedback loop.
- What is the stimulus in this system? Explain your answer.
- What is the control centre in this system? Explain your answer.
- In this system, is the pituitary considered the stimulus, sensor, control centre, or effector? Explain your answer.
7.8 Explore More
https://www.youtube.com/watch?v=LSgEJSlk6W4
Homeostasis - What Is Homeostasis - What Is Set Point For Homeostasis - Homeostasis In The Human Body, Whats Up Dude, 2017.
https://www.youtube.com/watch?v=XMsJ-3qRVJM
Attributions
Figure 7.8.1
Nest_Thermostat by Amanitamano on Wikimedia Commons is used under a CC BY-SA 3.0 (https://creativecommons.org/licenses/by-sa/3.0/deed.en) license.
Figure 7.8.2
Negative_Feedback_Loops by OpenStax on Wikimedia Commons is used under a CC BY 4.0 (https://creativecommons.org/licenses/by/4.0/deed.en) license.
Figure 7.8.3
Body Temperature Homeostasis by OpenStax College, Biology is used under a CC BY 4.0 license.
Figure 7.8.4
Homeostasis_of_blood_sugar by Christinelmiller on Wikimedia Commons is used under a CC0 1.0 Universal Public Domain Dedication (https://creativecommons.org/publicdomain/zero/1.0/deed.en) license.
Figure 7.8.5
Positive_Feedback_Diagram_Blood_Clotting by Elliottuttle on Wikimedia Commons is used under a CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0) license.
Figure 7.8.6
Pregnancy-Positive_Feedback by OpenStax on Wikimedia Commons is used under a CC BY 4.0 (https://creativecommons.org/licenses/by/4.0/deed.en) license.
References
Amoeba Sisters. (2017, September 7). Homeostasis and negative/positive feedback. YouTube. https://www.youtube.com/watch?v=Iz0Q9nTZCw4&feature=youtu.be
Betts, J. G., Young, K.A., Wise, J.A., Johnson, E., Poe, B., Kruse, D.H., Korol, O., Johnson, J.E., Womble, M., DeSaix, P. (2013, April 25). Figure 1.10 Negative feedback loop [digital image/ diagram]. In Anatomy and Physiology (Section 1.5). OpenStax. https://openstax.org/books/anatomy-and-physiology/pages/1-5-homeostasis
Betts, J. G., Young, K.A., Wise, J.A., Johnson, E., Poe, B., Kruse, D.H., Korol, O., Johnson, J.E., Womble, M., DeSaix, P. (2013, April 25). Figure 1.11 Positive feedback loop normal childbirth is driven by a positive feedback loop [digital image/ diagram]. In Anatomy and Physiology (Section 1.5). OpenStax. https://openstax.org/books/anatomy-and-physiology/pages/1-5-homeostasis
Cognito. (2018, December 18). GCSE Biology - Homeostasis #38. YouTube. https://www.youtube.com/watch?v=XMsJ-3qRVJM&feature=youtu.be
Mayo Clinic Staff. (n.d.). Type 2 diabetes [online article]. MayoClinic.org. https://www.mayoclinic.org/diseases-conditions/type-2-diabetes/symptoms-causes/syc-20351193
OpenStax CNX. (2016, March 23). Figure 4 The body is able to regulate temperature in response to signals from the nervous system [digital image]. In OpenStax, Biology (Section 33.3). https://cnx.org/contents/GFy_h8cu@10.8:BP24ZReh@7/Homeostasis
Whats Up Dude. (2017, September 20). Homeostasis - What is homeostasis - What is set point for homeostasis - Homeostasis in the human body. YouTube. https://www.youtube.com/watch?v=LSgEJSlk6W4&feature=youtu.be
Image shows an illustration of the thyroid gland. It is located in front of where an Adam's apple would be. It is roughly butterfly shaped. The "wings" are the right and left lobes, and the connecting part is the isthmus.
As per caption.
The central nervous system organ inside the skull that is the control center of the nervous system.
Created by CK-12 Foundation/Adapted by Christine Miller

Kidneys on the Menu
Pictured in Figure 16.4.1 is a steak and kidney pie; this savory dish is a British favorite. When kidneys are on a menu, they typically come from sheep, pigs, or cows. In these animals (as in the human animal), kidneys are the main organs of excretion.
Location of the Kidneys
The two bean-shaped kidneys are located high in the back of the abdominal cavity, one on each side of the spine. Both kidneys sit just below the diaphragm, the large breathing muscle that separates the abdominal and thoracic cavities. As you can see in the following figure, the right kidney is slightly smaller and lower than the left kidney. The right kidney is behind the liver, and the left kidney is behind the spleen. The location of the liver explains why the right kidney is smaller and lower than the left.
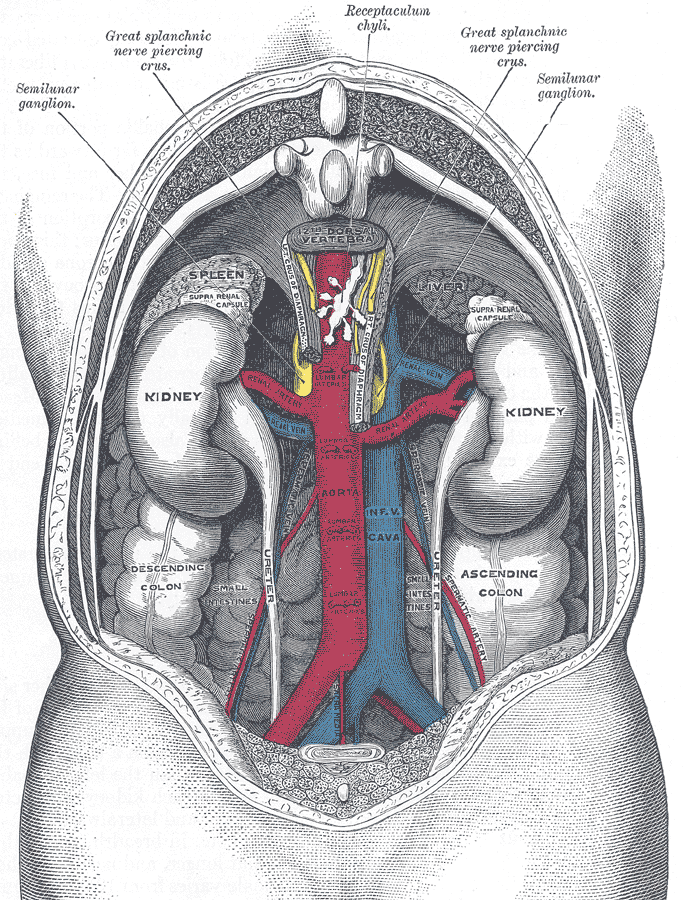
Kidney Anatomy
The shape of each kidney gives it a convex side (curving outward) and a concave side (curving inward). You can see this clearly in the detailed diagram of kidney anatomy shown in Figure 16.4.3. The concave side is where the renal artery enters the kidney, as well as where the renal vein and ureter leave the kidney. This area of the kidney is called the hilum. The entire kidney is surrounded by tough fibrous tissue — called the renal capsule — which, in turn, is surrounded by two layers of protective, cushioning fat.
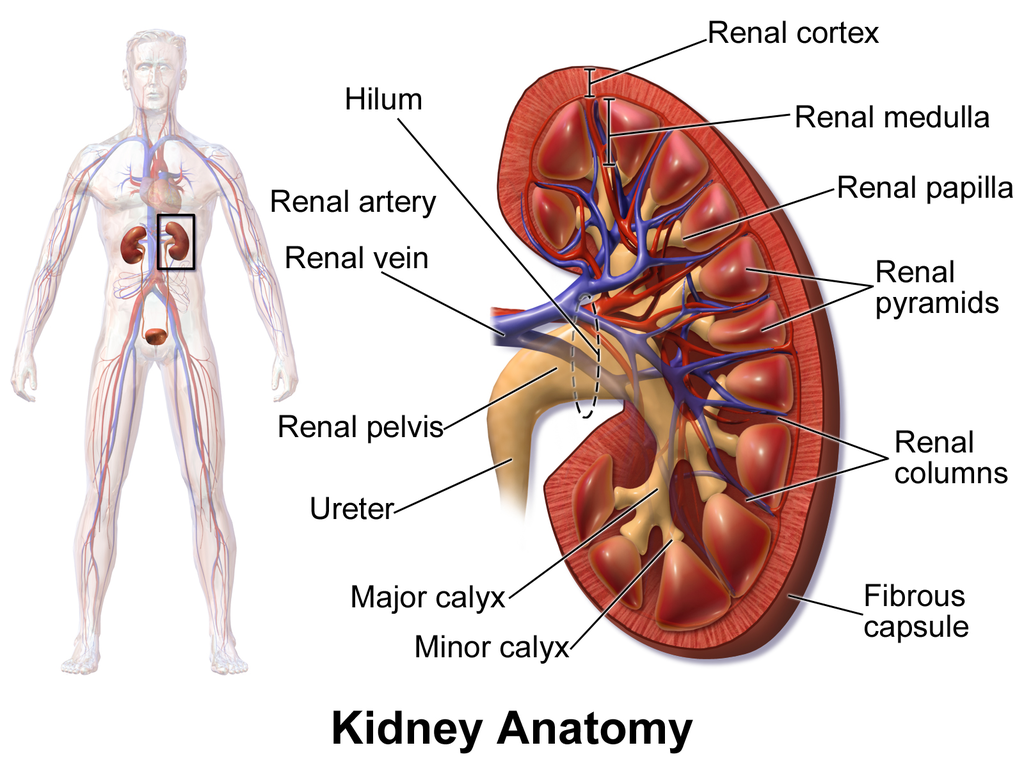
Internally, each kidney is divided into two major layers: the outer renal cortex and the inner renal medulla (see Figure 16.4.3 above). These layers take the shape of many cone-shaped renal lobules, each containing renal cortex surrounding a portion of medulla called a renal pyramid. Within the renal pyramids are the structural and functional units of the kidneys, the tiny nephrons. Between the renal pyramids are projections of cortex called renal columns. The tip, or papilla, of each pyramid empties urine into a minor calyx (chamber). Several minor calyces empty into a major calyx, and the latter empty into the funnel-shaped cavity called the renal pelvis, which becomes the ureter as it leaves the kidney.
Renal Circulation
The renal circulation is an important part of the kidney’s primary function of filtering waste products from the blood. Blood is supplied to the kidneys via the renal arteries. The right renal artery supplies the right kidney, and the left renal artery supplies the left kidney. These two arteries branch directly from the aorta, which is the largest artery in the body. Each kidney is only about 11 cm (4.4 in) long, and has a mass of just 150 grams (5.3 oz), yet it receives about ten per cent of the total output of blood from the heart. Blood is filtered through the kidneys every 3 minutes, 24 hours a day, every day of your life.
As indicated in Figure 16.4.4, each renal artery carries blood with waste products into the kidney. Within the kidney, the renal artery branches into increasingly smaller arteries that extend through the renal columns between the renal pyramids. These arteries, in turn, branch into arterioles that penetrate the renal pyramids. Blood in the arterioles passes through nephrons, the structures that actually filter the blood. After blood passes through the nephrons and is filtered, the clean blood moves through a network of venules that converge into small veins. Small veins merge into increasingly larger ones, and ultimately into the renal vein, which carries clean blood away from the kidney to the inferior vena cava.
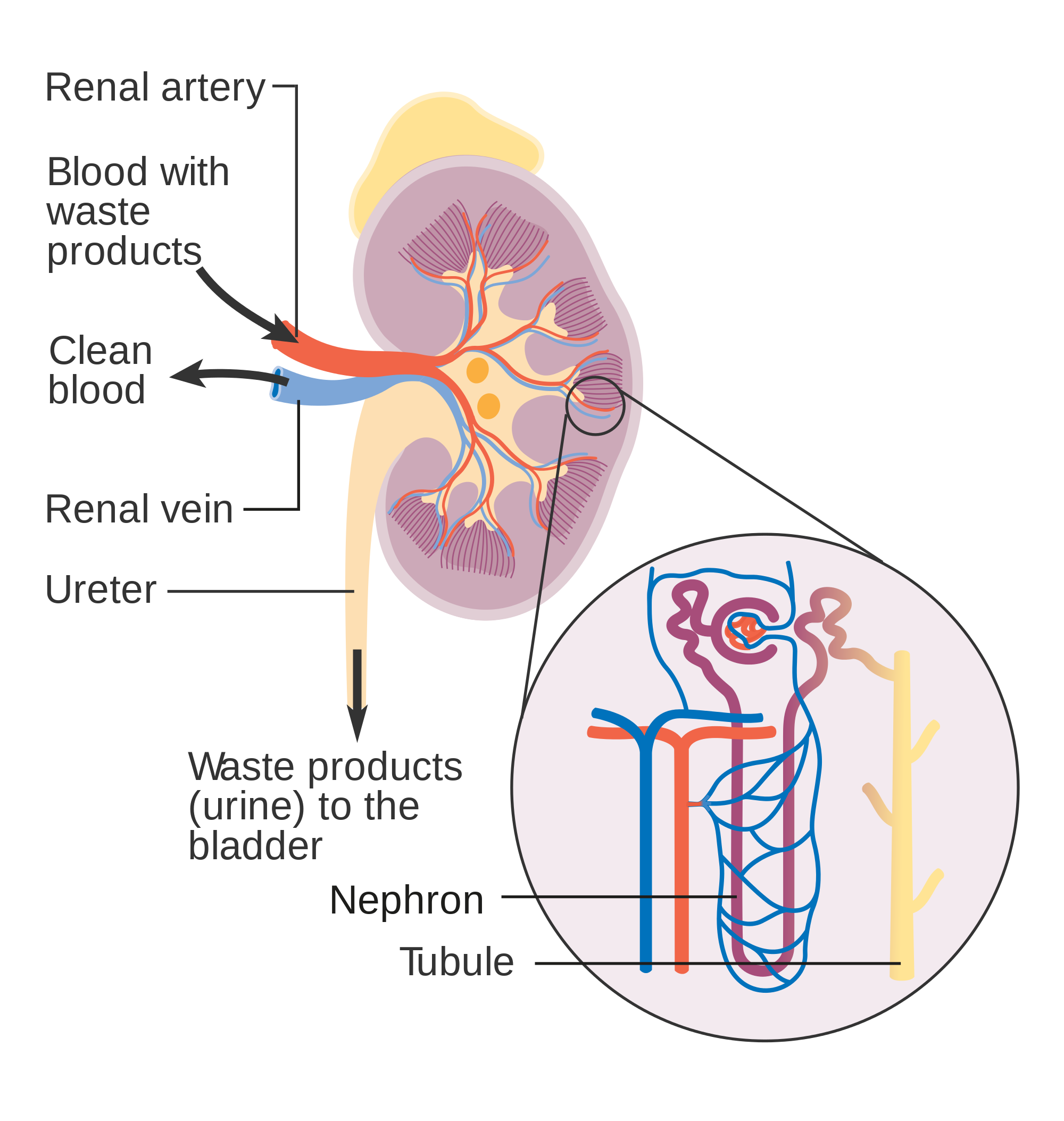
Nephron Structure and Function
Figure 16.4.4 gives an indication of the complex structure of a nephron. The nephron is the basic structural and functional unit of the kidney, and each kidney typically contains at least a million of them. As blood flows through a nephron, many materials are filtered out of the blood, needed materials are returned to the blood, and the remaining materials form urine. Most of the waste products removed from the blood and excreted in urine are byproducts of metabolism. At least half of the waste is urea, a waste product produced by protein catabolism. Another important waste is uric acid, produced in nucleic acid catabolism.
Components of a Nephron
Figure 16.4.5 shows in greater detail the components of a nephron. Each nephron is composed of an initial filtering component that consists of a network of capillaries called the glomerulus (plural, glomeruli), which is surrounded by a space within a structure called glomerular capsule (also known as the Bowman's capsule). Extending from glomerular capsule is the renal tubule. The proximal end (nearest glomerular capsule) of the renal tubule is called the proximal convoluted (coiled) tubule. From here, the renal tubule continues as a loop (known as the loop of Henle) (also known as the loop of the nephron), which in turn becomes the distal convoluted tubule. The latter finally joins with a collecting duct. As you can see in the diagram, arterioles surround the total length of the renal tubule in a mesh called the peritubular capillary network.
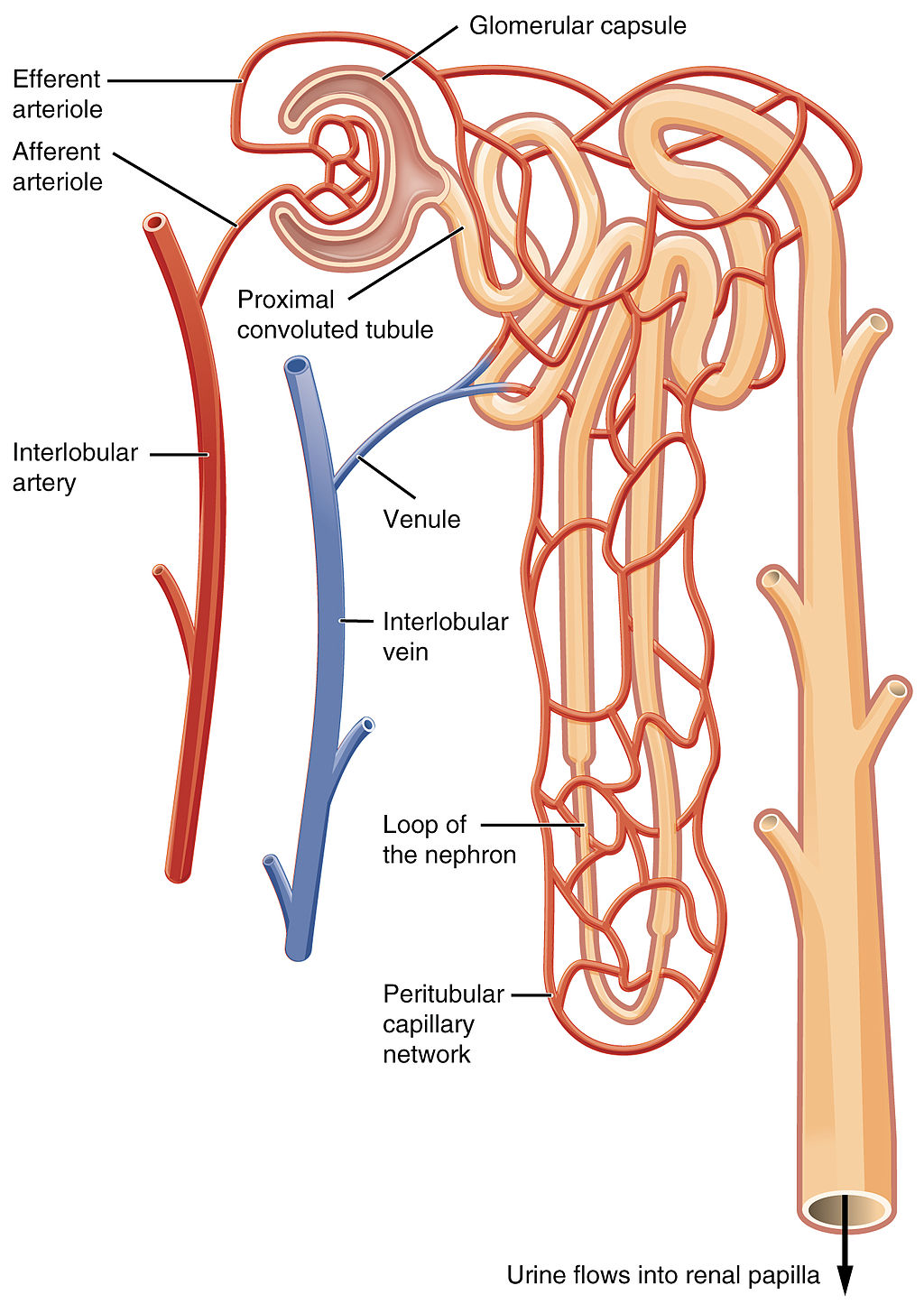
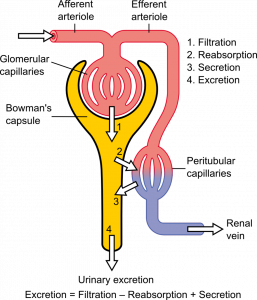
Function of a Nephron
The simplified diagram of a nephron in Figure 16.4.6 shows an overview of how the nephron functions. Blood enters the nephron through an arteriole called the afferent arteriole. Next, some of the blood passes through the capillaries of the glomerulus. Any blood that doesn’t pass through the glomerulus — as well as blood after it passes through the glomerular capillaries — continues on through an arteriole called the efferent arteriole. The efferent arteriole follows the renal tubule of the nephron, where it continues playing a role in nephron functioning.
Filtration
As blood from the afferent arteriole flows through the glomerular capillaries, it is under pressure. Because of the pressure, water and solutes are filtered out of the blood and into the space made by glomerular capsule, almost like the water you cook pasta is is filtered out through a strainer. This is the filtration stage of nephron function. The filtered substances — called filtrate — pass into glomerular capsule, and from there into the proximal end of the renal tubule. Anything too large to move through the pores in the glomerulus, such as blood cells, large proteins, etc., stay in the cardiovascular system. At this stage, filtrate (fluid in the nephron) includes water, salts, organic solids (such as nutrients), and waste products of metabolism (such as urea).
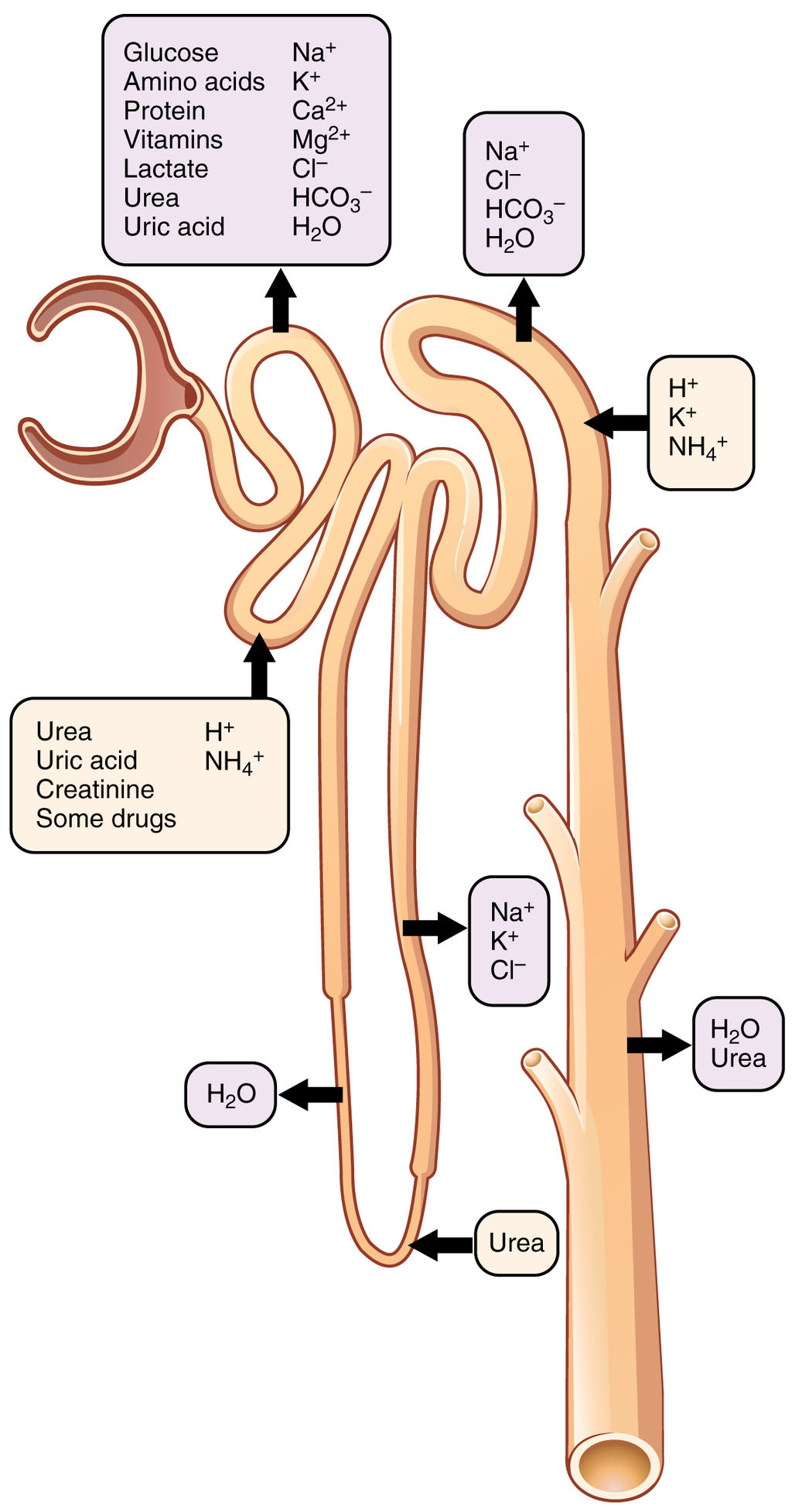
Reabsorption and Secretion
As filtrate moves through the renal tubule, some of the substances it contains are reabsorbed from the filtrate back into the blood in the efferent arteriole (via peritubular capillary network). This is the reabsorption stage of nephron function and it is about returning "the good stuff" back to the blood so that it doesn't exit the body in urine. About two-thirds of the filtered salts and water, and all of the filtered organic solutes (mainly glucose and amino acids) are reabsorbed from the filtrate by the blood in the peritubular capillary network. Reabsorption occurs mainly in the proximal convoluted tubule and the loop of Henle, as seen in Figure 16.4.7.
At the distal end of the renal tubule, some additional reabsorption generally occurs. This is also the region of the tubule where other substances from the blood are added to the filtrate in the tubule. The addition of other substances to the filtrate from the blood is called secretion. Both reabsorption and secretion (shown in Figure 16.4.7) in the distal convoluted tubule are largely under the control of endocrine hormones that maintain homeostasis of water and mineral salts in the blood. These hormones work by controlling what is reabsorbed into the blood from the filtrate and what is secreted from the blood into the filtrate to become urine. For example, parathyroid hormone causes more calcium to be reabsorbed into the blood and more phosphorus to be secreted into the filtrate.
Collection of Urine and Excretion

By the time the filtrate has passed through the entire renal tubule, it has become the liquid waste known as urine. Urine empties from the distal end of the renal tubule into a collecting duct. From there, the urine flows into increasingly larger collecting ducts. As urine flows through the system of collecting ducts, more water may be reabsorbed from it. This will occur in the presence of antidiuretic hormone from the posterior pituitary gland. This hormone makes the collecting ducts permeable to water, allowing water molecules to pass through them into capillaries by osmosis, while preventing the passage of ions or other solutes. As much as 75% of the water may be reabsorbed from urine in the collecting ducts, making the urine more concentrated.
Urine finally exits the largest collecting ducts through the renal papillae. It empties into the renal calyces, and finally into the renal pelvis. From there, it travels through the ureter to the urinary bladder for eventual excretion from the body. An average of roughly 1.5 litres (a little over 6 cups) of urine is excreted each day. Normally, urine is yellow or amber in colour (see Figure 16.4.8). The darker the colour, generally speaking, the more concentrated the urine is.
Besides filtering blood and forming urine for excretion of soluble wastes, the kidneys have several vital functions in maintaining body-wide homeostasis. Most of these functions are related to the composition or volume of urine formed by the kidneys. The kidneys must maintain the proper balance of water and salts in the body, normal blood pressure, and the correct range of blood pH. Through the processes of absorption and secretion by nephrons, more or less water, salt ions, acids, or bases are returned to the blood or excreted in urine, as needed, to maintain homeostasis.
Blood Pressure Regulation
The kidneys do not control homeostasis all alone. As indicated above, endocrine hormones are also involved. Consider the regulation of blood pressure by the kidneys. Blood pressure is the pressure exerted by blood on the walls of the arteries. The regulation of blood pressure is part of a complex system, called the renin-angiotensin-aldosterone system. This system regulates the concentration of sodium in the blood to control blood pressure.
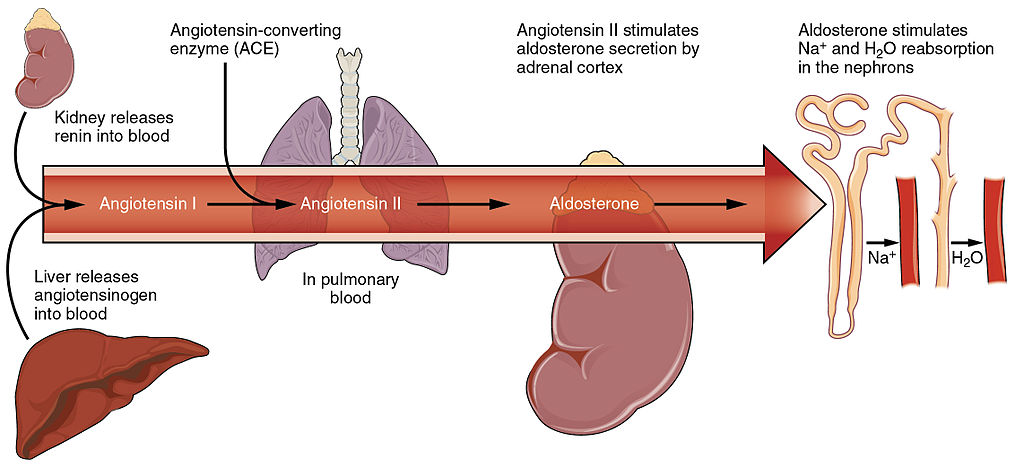
The renin-angiotensin-aldosterone system is put into play when the concentration of sodium ions in the blood falls lower than normal. This causes the kidneys to secrete an enzyme called renin into the blood. It also causes the liver to secrete a protein called angiotensinogen. Renin changes angiotensinogen into a proto-hormone called angiotensin I. This is converted to angiotensin II by an enzyme (angiotensin-converting enzyme) in lung capillaries.
Angiotensin II is a potent hormone that causes arterioles to constrict. This, in turn, increases blood pressure. Angiotensin II also stimulates the secretion of the hormone aldosterone from the adrenal cortex. Aldosterone causes the kidneys to increase the reabsorption of sodium ions and water from the filtrate into the blood. This returns the concentration of sodium ions in the blood to normal. The increased water in the blood also increases blood volume and blood pressure.
Other Kidney Hormones
Hormones other than renin are also produced and secreted by the kidneys. These include calcitriol and erythropoietin.
- Calcitriol is secreted by the kidneys in response to low levels of calcium in the blood. This hormone stimulates uptake of calcium by the intestine, thus raising blood levels of calcium.
- Erythropoietin is secreted by the kidneys in response to low levels of oxygen in the blood. This hormone stimulates erythropoiesis, which is the production of erythrocytes in bone marrow. Extra red blood cells increase the level of oxygen carried in the blood.
Feature: Human Biology in the News
Kidney failure is a complication of common disorders including diabetes mellitus and hypertension. It is estimated that approximately 12.5% of Canadians have some form of kidney disease. If the disease is serious, the patient must either receive a donated kidney or have frequent hemodialysis, a medical procedure in which the blood is artificially filtered through a machine. Transplant generally results in better outcomes than hemodialysis, but demand for organs far outstrips the supply. The average time on the organ donation waitlist for a kidney is four years. There are over 3,000 Canadians on the wait list for a kidney transplant and some will die waiting for a kidney to become available.
For the past decade, Dr. William Fissell, a kidney specialist at Vanderbilt University, has been working to create an implantable part-biological and part-artificial kidney. Using microchips like those used in computers, he has produced an artificial kidney small enough to implant in the patient’s body in place of the failed kidney. According to Dr. Fissell, the artificial kidney is “... a bio-hybrid device that can mimic a kidney to remove enough waste products, salt, and water to keep a patient off [hemo]dialysis.”
The filtration system in the artificial kidney consists of a stack of 15 microchips. Tiny pores in the microchips act as a scaffold for the growth of living kidney cells that can mimic the natural functions of the kidney. The living cells form a membrane to filter the patient’s blood as a biological kidney would, but with less risk of rejection by the patient’s immune system, because they are embedded within the device. The new kidney doesn’t need a power source, because it uses the natural pressure of blood flowing through arteries to push the blood through the filtration system. A major part of the design of the artificial organ was devoted to fine tuning the fluid dynamics so blood flows through the device without clotting.
Because of the potential life-saving benefits of the device, the implantable kidney was given fast-track approval for testing in people by the U.S. Food and Drug Administration. The artificial kidney is expected to be tested in pilot trials by 2018. Dr. Fissell says he has a long list of patients eager to volunteer for the trials.
16.4 Summary
- The two bean-shaped kidneys are located high in the back of the abdominal cavity on either side of the spine. A renal artery connects each kidney with the aorta, and transports unfiltered blood to the kidney. A renal vein connects each kidney with the inferior vena cava and transports filtered blood back to the circulation.
- The kidney has two main layers involved in the filtration of blood and formation of urine: the outer cortex and inner medulla. At least a million nephrons — which are the tiny functional units of the kidney — span the cortex and medulla. The entire kidney is surrounded by a fibrous capsule and protective fat layers.
- As blood flows through a nephron, many materials are filtered out of the blood, needed materials are returned to the blood, and the remaining materials are used to form urine.
- In each nephron, the glomerulus and surrounding Bowman’s capsule form the unit that filters blood. From Bowman’s capsule, the material filtered from blood (called filtrate) passes through the long renal tubule. As it does, some substances are reabsorbed into the blood, and other substances are secreted from the blood into the filtrate, finally forming urine. The urine empties into collecting ducts, where more water may be reabsorbed.
- The kidneys control homeostasis with the help of endocrine hormones. The kidneys, for example, are part of the renin-angiotensin-aldosterone system that regulates the concentration of sodium in the blood to control blood pressure. In this system, the enzyme renin secreted by the kidneys works with hormones from the liver and adrenal gland to stimulate nephrons to reabsorb more sodium and water from urine.
- The kidneys also secrete endocrine hormones, including calcitriol — which helps control the level of calcium in the blood — and erythropoietin, which stimulates bone marrow to produce red blood cells.
16.4 Review Questions
-
- Contrast the renal artery and renal vein.
- Identify the functions of a nephron. Describe in detail what happens to fluids (blood, filtrate, and urine) as they pass through the parts of a nephron.
- Identify two endocrine hormones secreted by the kidneys, along with the functions they control.
- Name two regions in the kidney where water is reabsorbed.
- Is the blood in the glomerular capillaries more or less filtered than the blood in the peritubular capillaries? Explain your answer.
- What do you think would happen if blood flow to the kidneys is blocked?
16.4 Explore More
https://youtu.be/FN3MFhYPWWo
How do your kidneys work? - Emma Bryce, TED-Ed, 2015.
https://youtu.be/es-t8lO1KpA
Urine Formation, Hamada Abass, 2013.
https://youtu.be/bX3C201O4MA
Printing a human kidney - Anthony Atala, TED-Ed, 2013.
Attributions
Figure 16.4.1
Steak and Kidney Pie by Charles Haynes on Flickr is used under a CC BY-SA 2.0 (https://creativecommons.org/licenses/by-sa/2.0/) license.
Figure 16.4.2
Gray Kidneys by Henry Vandyke Carter (1831-1897) on Wikimedia Commons is in the public domain (https://en.wikipedia.org/wiki/public_domain). (Bartleby.com: Gray’s Anatomy, Plate 1120).
Figure 16.4.3
Blausen_0592_KidneyAnatomy_01 by BruceBlaus on Wikimedia Commons is used under a CC BY 3.0 (https://creativecommons.org/licenses/by/3.0) license.
Figure 16.4.4
Diagram_showing_how_the_kidneys_work_CRUK_138.svg by Cancer Research UK on Wikimedia Commons is used under a CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0) license.
Figure 16.4.5
Blood_Flow_in_the_Nephron by OpenStax College on Wikimedia Commons is used under a CC BY 3.0 (https://creativecommons.org/licenses/by/3.0) license.
Figure 16.4.6
1024px-Physiology_of_Nephron by Madhero88 on Wikimedia Commons is used under a CC BY 3.0 (https://creativecommons.org/licenses/by/3.0) license.
Figure 16.4.7
Nephron_Secretion_Reabsorption by OpenStax College on Wikimedia Commons is used under a CC BY 3.0 (https://creativecommons.org/licenses/by/3.0) license.
Figure 16.4.8
Urine by User:Markhamilton at English Wikipedia on Wikimedia Commons is in the public domain (https://en.wikipedia.org/wiki/Public_domain).
Figure 16.4.9
Renin_Angiotensin_System-01 by OpenStax College on Wikimedia Commons is used under a CC BY 3.0 (https://creativecommons.org/licenses/by/3.0) license.
References
Betts, J. G., Young, K.A., Wise, J.A., Johnson, E., Poe, B., Kruse, D.H., Korol, O., Johnson, J.E., Womble, M., DeSaix, P. (2013, June 19). Figure 25.10 Blood flow in the nephron [digital image]. In Anatomy and Physiology (Section 25.3). OpenStax. https://openstax.org/books/anatomy-and-physiology/pages/25-3-gross-anatomy-of-the-kidney
Betts, J. G., Young, K.A., Wise, J.A., Johnson, E., Poe, B., Kruse, D.H., Korol, O., Johnson, J.E., Womble, M., DeSaix, P. (2013, June 19). Figure 25.17 Locations of secretion and reabsorption in the nephron [digital image]. In Anatomy and Physiology (Section 25.6). OpenStax. https://openstax.org/books/anatomy-and-physiology/pages/25-6-tubular-reabsorption
Betts, J. G., Young, K.A., Wise, J.A., Johnson, E., Poe, B., Kruse, D.H., Korol, O., Johnson, J.E., Womble, M., DeSaix, P. (2013, June 19). Figure 26.14 The renin-angiotensin system [digital image]. In Anatomy and Physiology (Section 26.3). OpenStax. https://openstax.org/books/anatomy-and-physiology/pages/26-3-electrolyte-balance
Blausen.com Staff. (2014). Medical gallery of Blausen Medical 2014. WikiJournal of Medicine 1 (2). DOI:10.15347/wjm/2014.010. ISSN 2002-4436
Hamada Abass. (2013). Urine formation. YouTube. https://www.youtube.com/watch?v=es-t8lO1KpA&feature=youtu.be
TED-Ed. (2015, February 9). How do your kidneys work? - Emma Bryce. YouTube. https://www.youtube.com/watch?v=FN3MFhYPWWo&feature=youtu.be
TED-Ed. (2013, March 15). Printing a human kidney - Anthony Atala. YouTube. https://www.youtube.com/watch?v=bX3C201O4MA&feature=youtu.be
Image shows an old photograph of a lady suffering from Grave's Disease, her eyes are protruding, giving her a permanent look of surprise.
Image shows a diagram of the human body with labels pointing to all areas affected by hypothyroidism. Some examples include: General effects - fatigue, feeling cold, weight gain, poor appetite; Lungs - shortness of breath, pleural effusion; Skin - presthesia, myxedema; Muscular - delayed reflex action; Heart - slow pulse rate.
Image shows a diagram of locations in the body where the effects of anemia are experienced. Some of these include: Central nervous system: fatigue, dizziness and possibly fainting. Low blood pressure. In the heart: heart palpitations, rapid heart rate, chest palpitations, in extreme cases chest pain, angina and heart attack. Enlargement of the spleen. Changed stool (poo) colour. Muscular weakness. Shortness of breath. Pale, cold and/or yellowing skin. Yellowing eyes.
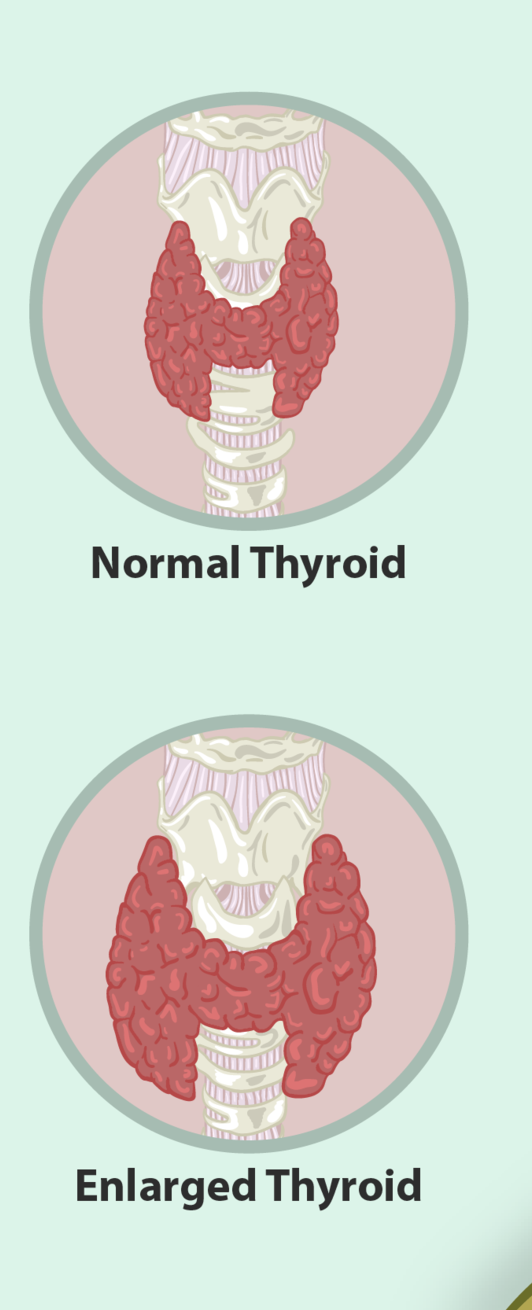

Too Much of a Good Thing
The woman in this photo has a goiter, an abnormal enlargement of the thyroid gland, located in the neck. A goiter may form as a result of a number of different thyroid disorders. You’ll learn why in this section.
Thyroid Structure
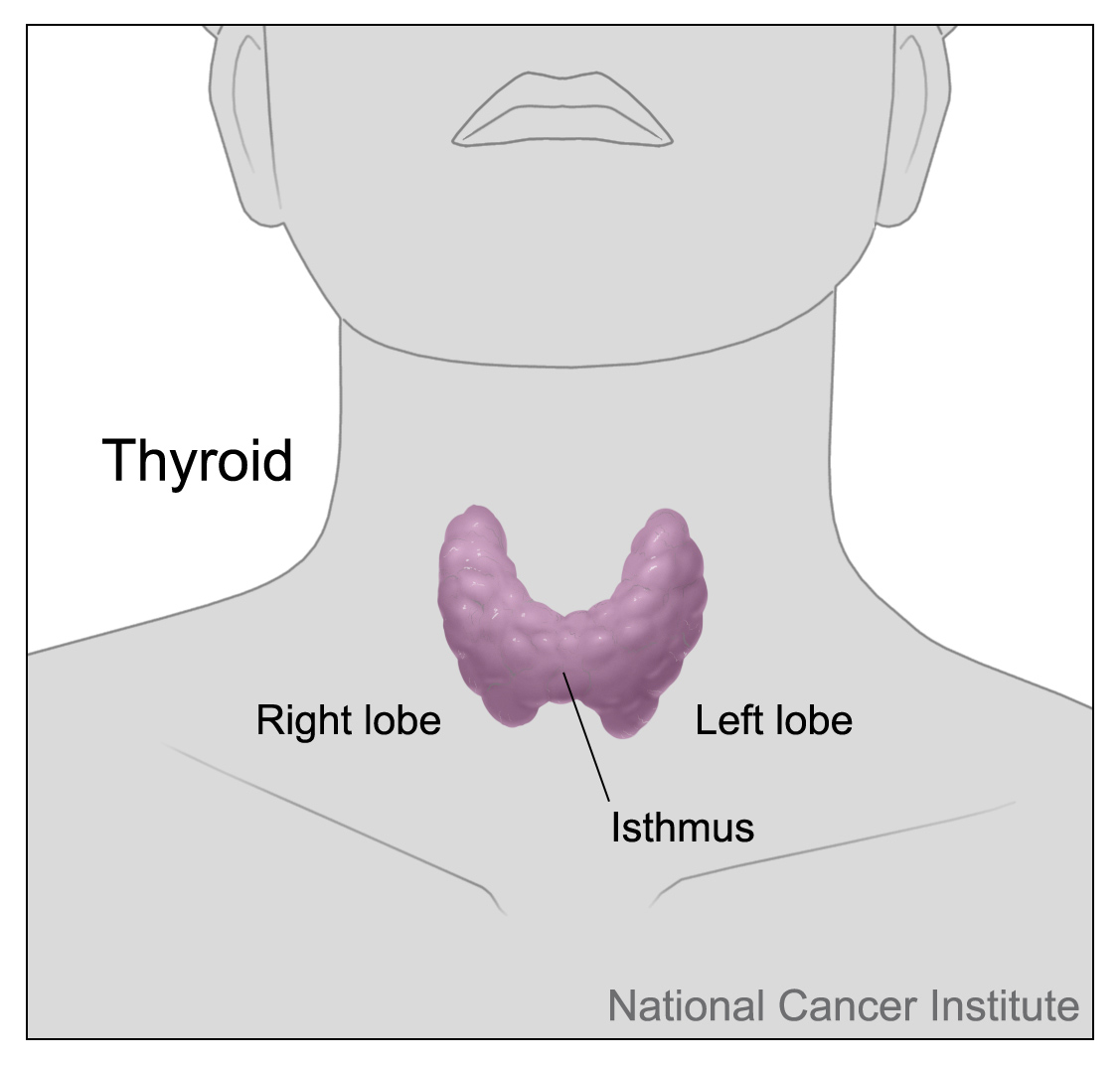
The thyroid gland is one of the largest endocrine glands in the body. It is located in the front of the neck below the Adam’s apple (see Figure 9.5.2). The gland is butterfly shaped and composed of two lobes. The lobes are connected by a narrow band of thyroid tissue called an isthmus.
Internally, the thyroid gland is composed mainly of follicles. A follicle is a small cluster of cells surrounding a central cavity, which stores hormones and other molecules made by the follicular cells. Thyroid follicular cells are unique in being highly specialized to absorb and use iodine. They absorb iodine as iodide ions (I-) from the blood and use the iodide to produce thyroid hormones. The cells also use some of the iodide they absorb to form a protein called thyroglobulin, which serves to store iodide for later hormone synthesis. The outer layer of cells of each follicle secretes thyroid hormones as needed. Scattered among the follicles are another type of thyroid cells, called parafollicular cells (or C cells). These cells synthesize and secrete the hormone calcitonin.
Function of the Thyroid
Like all endocrine glands, the function of the thyroid is to synthesize hormones and secrete them into the bloodstream. Once in the blood, they can travel to cells throughout the body and influence their functions.
Thyroid Hormones: T4 and T3
There are two main thyroid hormones produced by the follicles: thyroxine (T4), which contains four iodide ions and is represented by the structural diagram below (Figure 9.5.3), and triiodothyronine (T3), which contains three iodide ions. T3 is much more powerful than T4, but T4 makes up about 90 per cent of circulating thyroid hormone, and T3 makes up only about ten per cent. However, most of the T4 is converted to T3 by target tissues.
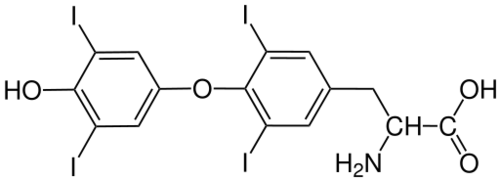
Like steroid hormones, T3 and T4 cross cell membranes everywhere in the body and bind to intracellular receptors to regulate gene expression. Unlike steroid hormones, however, thyroid hormones can cross cell membranes only with the help of special transporter proteins. Once inside the nucleus of cells, T3 and T4 turn on genes that control protein synthesis. Thyroid hormones increase the rate of metabolism in cells, allowing them to absorb more carbohydrates, use more energy, and produce more heat. Thyroid hormones also increase the rate and force of the heartbeat. In addition, they increase the sensitivity of cells to fight-or-flight hormones (that is, catecholamine hormones, such as adrenaline).
The production of both T4 and T3 is regulated primarily by thyroid stimulating hormone (TSH), which is secreted by the anterior pituitary gland (see Figure 9.5.4). TSH production, in turn, is regulated by thyrotropin releasing hormone (TRH), which is produced by the hypothalamus. The thyroid gland, pituitary gland, and hypothalamus form a negative feedback loop to keep thyroid hormone secretion within a normal range. TRH and TSH production is suppressed when T4 levels start to become too high. The opposite occurs when T4 levels start to become too low.
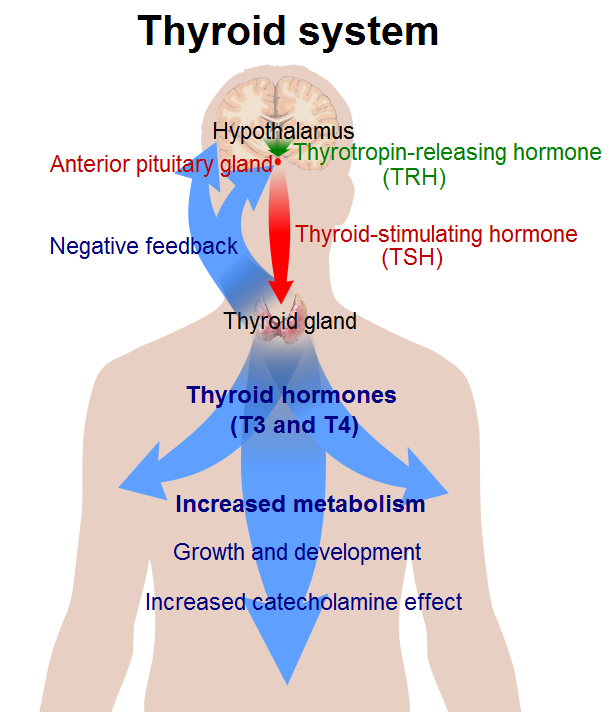
Calcitonin
The calcitonin produced by the parafollicular cells of the thyroid gland has the role of helping to regulate blood calcium levels by stimulating the movement of calcium into bone. Calcitonin is secreted in response to rising blood calcium levels. It decreases blood calcium levels by enhancing calcium absorption and deposition in bone. Calcitonin works hand-in-hand with parathyroid hormone, which is secreted by the parathyroid glands and has the opposite effects as calcitonin. Together, these two hormones maintain calcium homeostasis.
Thyroid Disorders
As with other endocrine disorders, thyroid disorders are generally associated with either over- or under-secretion of hormones. Abnormal secretion of thyroid hormones may occur for a variety of reasons.
Hyperthyroidism
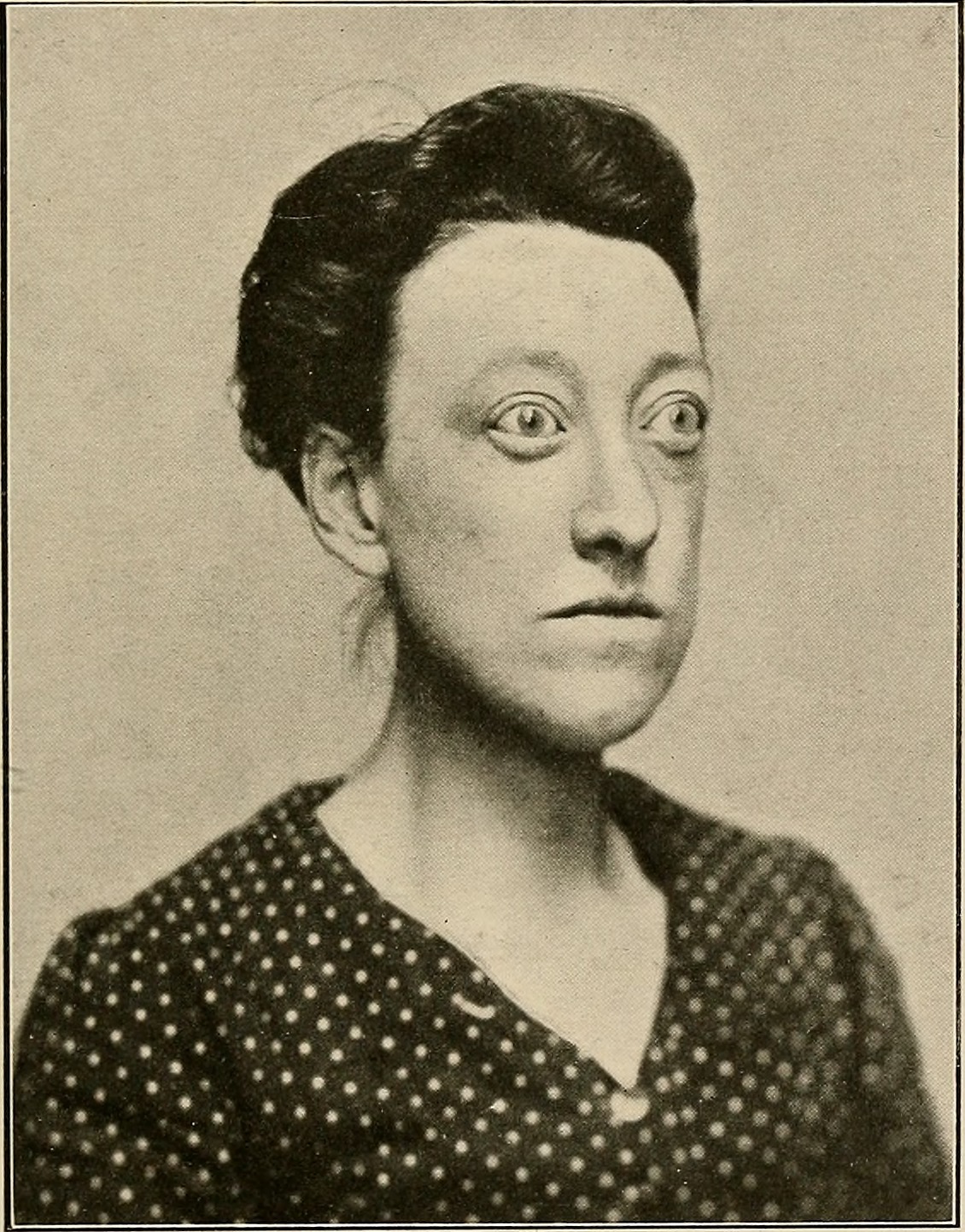
Hyperthyroidism occurs when the thyroid gland produces excessive amounts of thyroid hormones. The most common cause of hyperthyroidism is Graves’ disease. Graves’ disease is an autoimmune disorder in which abnormal antibodies produced by the immune system stimulate the thyroid to secrete excessive quantities of its hormones. This stimulation overrides the usual negative feedback mechanism that normally controls thyroid hormone output. Graves’ disease often results in the formation of an enlarged thyroid (goiter) because of the continued stimulation to produce more hormones.
Besides a goiter, other signs and symptoms of hyperthyroidism may include protruding eyes (see Figure 9.5.5), heart palpitations, excessive sweating, diarrhea, weight loss despite increased appetite, muscle weakness, and unusual sensitivity to heat. Medications can be prescribed to mitigate the symptoms of the disease. Anti-thyroid drugs can also be given to decrease the production of thyroid hormones. If the drugs are ineffective, the gland can be partially or entirely removed. This can be done surgically or with the administration of radioactive iodine. Removal of the thyroid produces hypothyroidism.
Hypothyroidism
Hypothyroidism occurs when the thyroid gland produces insufficient amounts of thyroid hormones. It can result from surgical removal of the thyroid. However, worldwide, the most common cause of hypothyroidism is dietary iodine deficiency. In cases of iodine deficiency, the negative feedback loop controlling the release of thyroid hormone causes repeated stimulation of the thyroid, resulting in the thyroid gland growing in size and producing a goiter. Although the gland gets larger, it cannot increase hormone output because of the lack of iodine in the diet.
Iodine deficiency is uncommon in the Western world because iodine is added to salt. In places like this where iodine deficiency isn't a problem, the most common cause of hypothyroidism is Hashimoto’s thyroiditis. This is another autoimmune disease, but in this case, the immune system destroys the thyroid gland, producing hypothyroidism. Hashimoto’s thyroiditis tends to run in families, so it is likely to have a genetic component. It usually appears after the age of 30, and is more common in females than males.
Hypothyroidism produces many signs and symptoms, as shown in Figure 9.5.6. These may include abnormal weight gain, tiredness, baldness, cold intolerance, and slow heart rate. Hypothyroidism is generally treated with thyroid hormone replacement therapy. This may be needed for the rest of a person’s life.
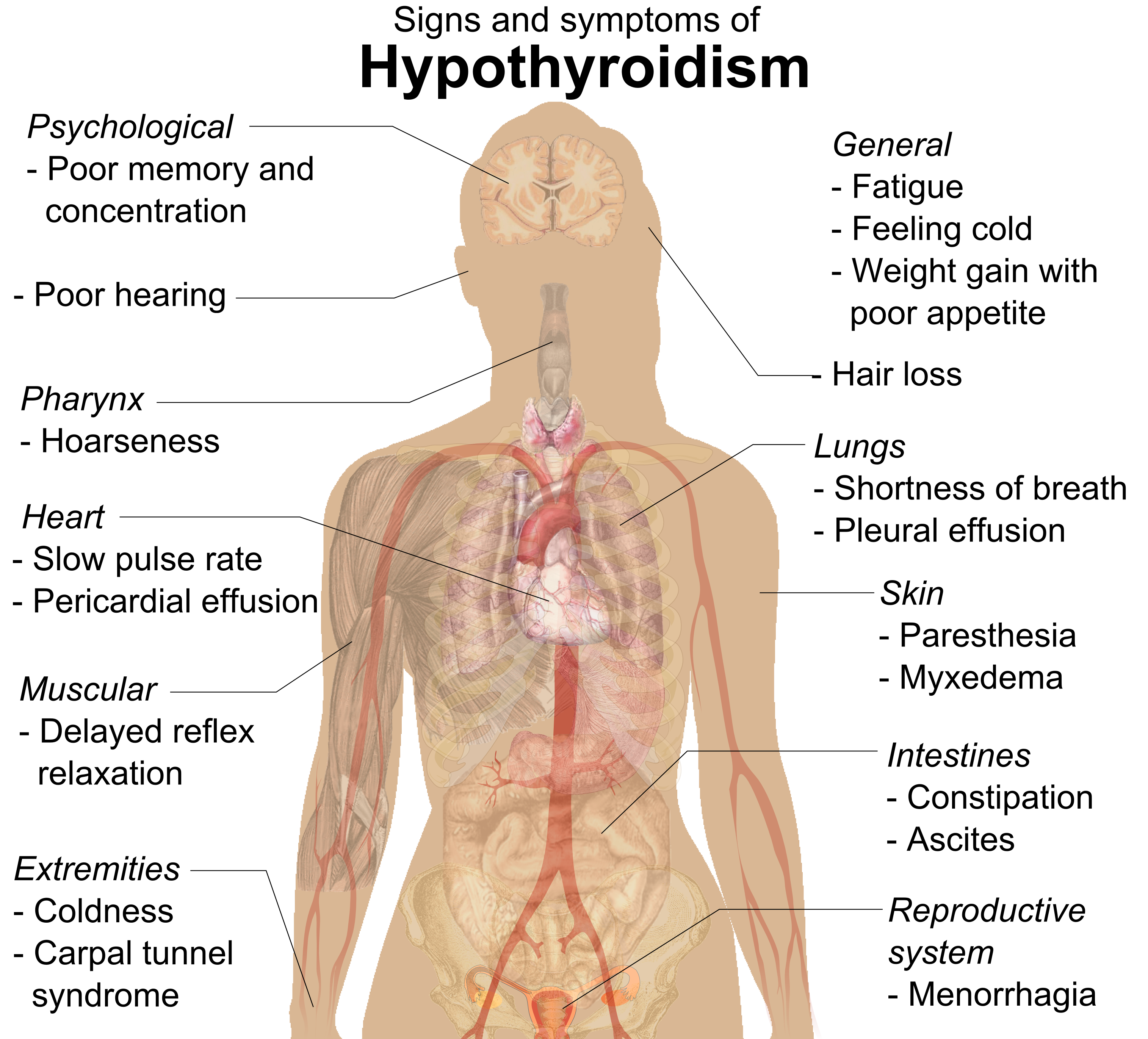
Hypothyroidism in a pregnant woman can have serious adverse consequences for the fetus. During the fetal period, cells of the developing brain are a major target for thyroid hormones, which play a crucial role in brain maturation. When levels of thyroid hormones are too low, the fetus may suffer permanent deficits in cognitive abilities. Deafness is also a potential outcome of hypothyroidism in utero.
Feature: Myth vs. Reality
Thyroid disorders are relatively common, affecting as many as 20 million people in the United States. According to recent studies, one in ten Canadians have some type of thyroid condition and up to 50 per cent may be undiagnosed! Because thyroid disorders are common, there are also many common myths about them.
Myth |
Reality |
| "If you have a thyroid problem, you will know something is wrong because you will have obvious symptoms." | The majority of people with a thyroid disorder are not aware they have it, because the symptoms are often mild, nonspecific, and easy to ignore. Generally, blood tests of thyroid hormone levels are needed to make a conclusive diagnosis. |
| "If you are diagnosed with a thyroid disorder, you will have to take medication for the rest of your life." | Whether you need to continue thyroid medication for life depends on the cause of the disorder. For example, some women develop hypothyroidism during pregnancy but no longer need medication after the pregnancy is over and hormone levels return to normal. |
| "As soon as you start taking thyroid medication, your symptoms will resolve." | It often takes weeks — or even months — for thyroid hormone levels to return to normal and for symptoms to disappear. |
| "You can take an over-the-counter iodine supplement to correct hypothyroidism." | In the United States, where dietary iodine is almost always adequate, iodine deficiency is unlikely to be the cause of hypothyroidism. Therefore, taking supplemental iodine is not likely to correct the problem. |
| "If thyroid symptoms are mild, you don’t need to take medication." | Because thyroid hormones are responsible for so many vital body functions, failing to treat even a mild thyroid disorder may lead to a range of other problems, such as osteoporosis or infertility. |
| "Goiter may be caused by eating “goitrogenic” vegetables, such as broccoli, Brussels sprouts, and spinach." | Although these foods can interfere with the thyroid’s ability to process iodide, you would have to eat huge amounts of them to cause a goiter. |
| "Thyroid disorders occur only after middle age and only in women." | Thyroid disorders may occur at any age and in any sex. Hypothyroidism occurs more commonly in older adults, but hyperthyroidism occurs more commonly in younger adults. Although women are more likely to develop thyroid disorders, about 20 per cent of cases occur in men. |
9.5 Summary
- The thyroid gland is a large endocrine gland in the front of the neck. It is composed mainly of clusters of cells called follicles, which are specialized to absorb iodine and use it to make thyroid hormones. Parafollicular cells among the follicles synthesize the hormone calcitonin.
- Thyroxine (T4) and triiodothyronine (T3) cross cell membranes and regulate gene expression to control the rate of metabolism in cells body-wide, among other functions. The production of T4 and T3 is regulated by thyroid stimulating hormone (TSH) from the pituitary, which is regulated, in turn, by thyrotropin releasing hormone (TRH) from the hypothalamus.
- Calcitonin helps regulate blood calcium levels by stimulating the movement of calcium into bone. It works in conjunction with parathyroid hormone to maintain calcium homeostasis.
- Abnormal secretion of thyroid hormones may occur for a variety of reasons, and it may lead to the development of a goiter. The most common cause of hyperthyroidism is Graves’ disease, an autoimmune disorder. Iodine deficiency is a common cause of hypothyroidism worldwide. In the United States, the most common cause of hypothyroidism is Hashimoto’s thyroiditis, another autoimmune disorder. Hypothyroidism in pregnant women may cause permanent cognitive deficits in children.
9.5 Review Questions
- Describe the structure and location of the thyroid gland.
- Identify the types of cells within the thyroid gland that produce hormones.
-
- Compare and contrast T4 and T3.
- How do T4 and T3 affect body cells?
- Explain how T4 and T3 production is regulated.
- What is calcitonin's function?
- Identify the chief cause and effects of hyperthyroidism.
- What are two possible causes of hypothyroidism?
- List signs and symptoms of hypothyroidism.
- Why is it that both hyperthyroidism and hypothyroidism cause goiters?
- Choose one symptom each for hyperthyroidism and hypothyroidism. Based on the functions of thyroid hormones, explain why each symptom occurs.
- In cases of hypothyroidism caused by Hashimoto’s thyroiditis or removal of the thyroid gland to treat hyperthyroidism, patients are often given medication to replace the missing thyroid hormone. Explain why the level of replacement thyroid hormone must be carefully monitored and adjusted if needed.
9.5 Explore More
https://www.youtube.com/watch?v=iNrUpBwU3q0
How does the thyroid manage your metabolism? - Emma Bryce, TED-Ed, 2015.
https://www.youtube.com/watch?v=oINxr8_nR_Y&feature=emb_logo
Graves' Disease and Hashimoto's Thyroiditis, hardgrindcoffeeyo, 2014.
https://www.youtube.com/watch?v=-5W7eEX-u3U&feature=emb_logo
The Fukushima Nuclear Accident documentary, World Disasters, 2014.
Attribution
Figure 9.5.1
- Goiter by Drahreg01 on Wikimedia Commons is used under a CC BY-SA 3.0 (https://creativecommons.org/licenses/by-sa/3.0) license.
- [adapted] A_woman_suffering_from_Goiter by MyUpchar.com on Wikimedia Commons is used under a CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0) license.
Figure 9.5.2
Thyroid gland by National Cancer Institute is in the public domain (https://en.wikipedia.org/wiki/Public_domain).
Figure 9.5.3
Structural model representing a single molecule of thyroxine (T4) from CK-12 Foundation is an image of a chemical structure model and is non-copyrightable.
Figure 9.5.4
Thyroid_system by Mikael Häggström on Wikimedia Commons is in the public domain (https://en.wikipedia.org/wiki/Public_domain).
Figure 9.5.5
Case of Graves disease without goitre by Internet Archive Book Images on Flickr is believed to have No known copyright restrictions. [Image from page 226 of "The thyroid gland in health and disease" (1917)]
Figure 9.5.6
Signs_and_symptoms_of_hypothyroidism by Mikael Häggström. on Wikimedia Commons is used under a CC0 1.0 Universal Public Domain Dedication license (https://creativecommons.org/publicdomain/zero/1.0/deed.en).
About thyroid disease. (n.d.). Thyroid Foundation of Canada. https://thyroid.ca/thyroid-disease/
Häggström, M. (2014). Medical gallery of Mikael Häggström 2014. WikiJournal of Medicine 1 (2). DOI:10.15347/wjm/2014.008. ISSN 2002-4436.
hardgrindcoffeeyo. (2014, July 19). Graves' disease and Hashimoto's thyroiditis. YouTube. https://www.youtube.com/watch?v=oINxr8_nR_Y&feature=youtu.be
TED-Ed. (2015, March 2). How does the thyroid manage your metabolism? - Emma Bryce. YouTube. https://www.youtube.com/watch?v=iNrUpBwU3q0&feature=youtu.be
World Disasters. (2014, April 5). The Fukushima nuclear accident documentary. YouTube. https://www.youtube.com/watch?v=-5W7eEX-u3U&feature=youtu.be
Created by CK-12 Foundation/Adapted by Christine Miller
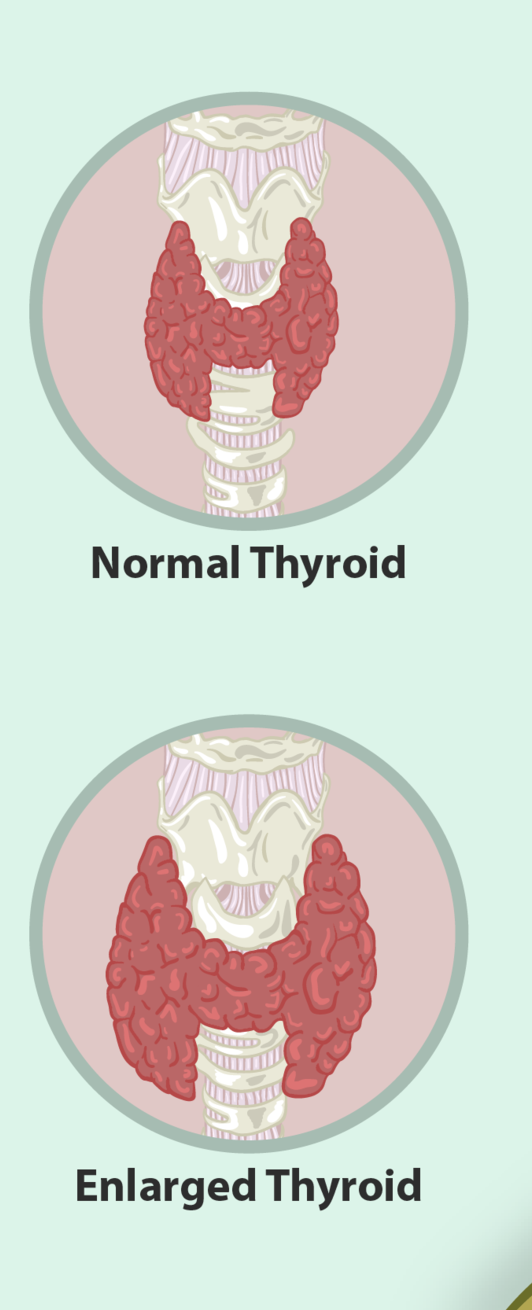

Too Much of a Good Thing
The woman in this photo has a goiter, an abnormal enlargement of the thyroid gland, located in the neck. A goiter may form as a result of a number of different thyroid disorders. You’ll learn why in this section.
Thyroid Structure
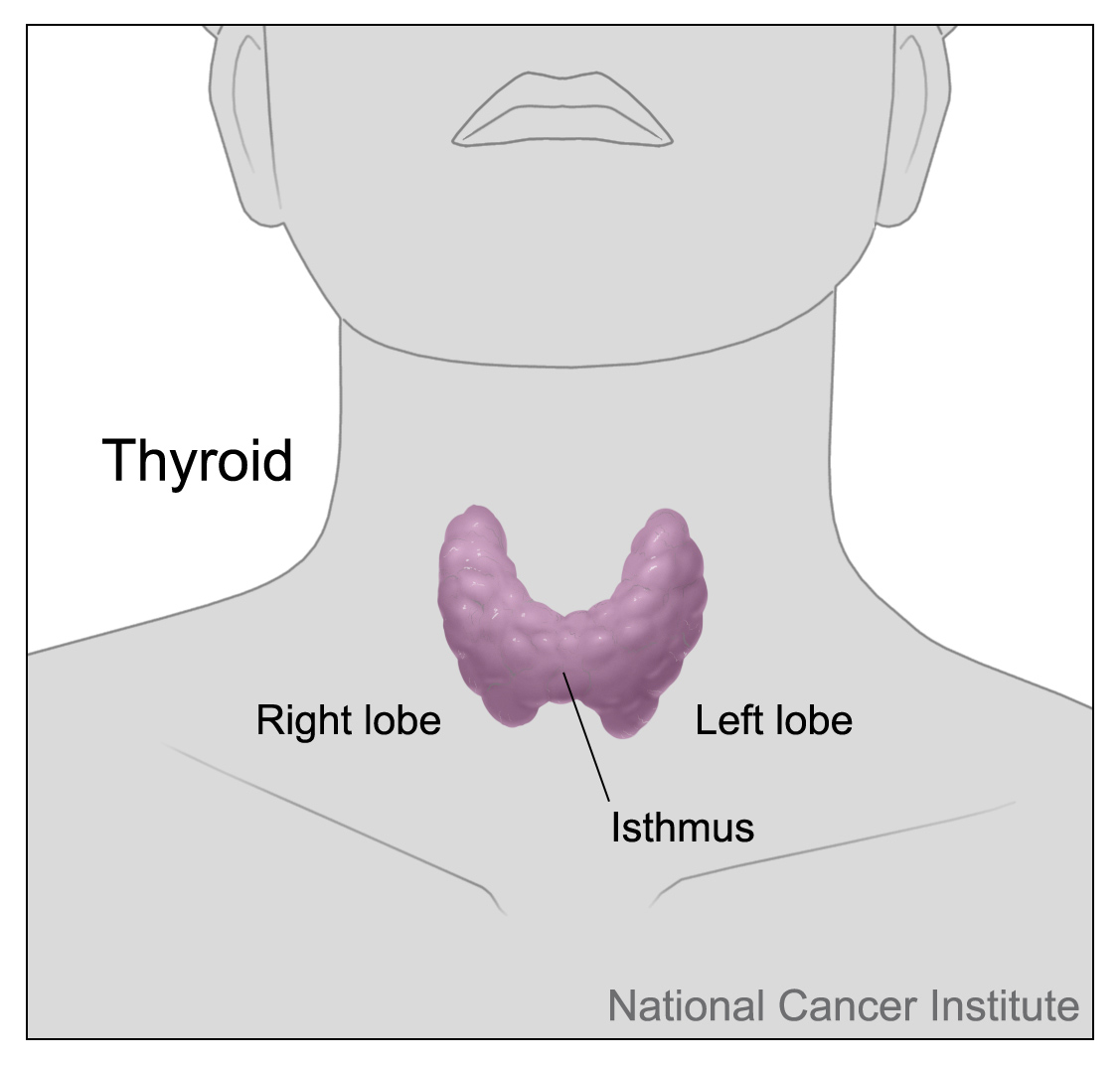
The thyroid gland is one of the largest endocrine glands in the body. It is located in the front of the neck below the Adam’s apple (see Figure 9.5.2). The gland is butterfly shaped and composed of two lobes. The lobes are connected by a narrow band of thyroid tissue called an isthmus.
Internally, the thyroid gland is composed mainly of follicles. A follicle is a small cluster of cells surrounding a central cavity, which stores hormones and other molecules made by the follicular cells. Thyroid follicular cells are unique in being highly specialized to absorb and use iodine. They absorb iodine as iodide ions (I-) from the blood and use the iodide to produce thyroid hormones. The cells also use some of the iodide they absorb to form a protein called thyroglobulin, which serves to store iodide for later hormone synthesis. The outer layer of cells of each follicle secretes thyroid hormones as needed. Scattered among the follicles are another type of thyroid cells, called parafollicular cells (or C cells). These cells synthesize and secrete the hormone calcitonin.
Function of the Thyroid
Like all endocrine glands, the function of the thyroid is to synthesize hormones and secrete them into the bloodstream. Once in the blood, they can travel to cells throughout the body and influence their functions.
Thyroid Hormones: T4 and T3
There are two main thyroid hormones produced by the follicles: thyroxine (T4), which contains four iodide ions and is represented by the structural diagram below (Figure 9.5.3), and triiodothyronine (T3), which contains three iodide ions. T3 is much more powerful than T4, but T4 makes up about 90 per cent of circulating thyroid hormone, and T3 makes up only about ten per cent. However, most of the T4 is converted to T3 by target tissues.
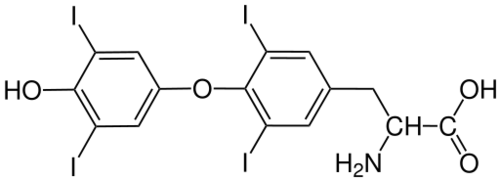
Like steroid hormones, T3 and T4 cross cell membranes everywhere in the body and bind to intracellular receptors to regulate gene expression. Unlike steroid hormones, however, thyroid hormones can cross cell membranes only with the help of special transporter proteins. Once inside the nucleus of cells, T3 and T4 turn on genes that control protein synthesis. Thyroid hormones increase the rate of metabolism in cells, allowing them to absorb more carbohydrates, use more energy, and produce more heat. Thyroid hormones also increase the rate and force of the heartbeat. In addition, they increase the sensitivity of cells to fight-or-flight hormones (that is, catecholamine hormones, such as adrenaline).
The production of both T4 and T3 is regulated primarily by thyroid stimulating hormone (TSH), which is secreted by the anterior pituitary gland (see Figure 9.5.4). TSH production, in turn, is regulated by thyrotropin releasing hormone (TRH), which is produced by the hypothalamus. The thyroid gland, pituitary gland, and hypothalamus form a negative feedback loop to keep thyroid hormone secretion within a normal range. TRH and TSH production is suppressed when T4 levels start to become too high. The opposite occurs when T4 levels start to become too low.
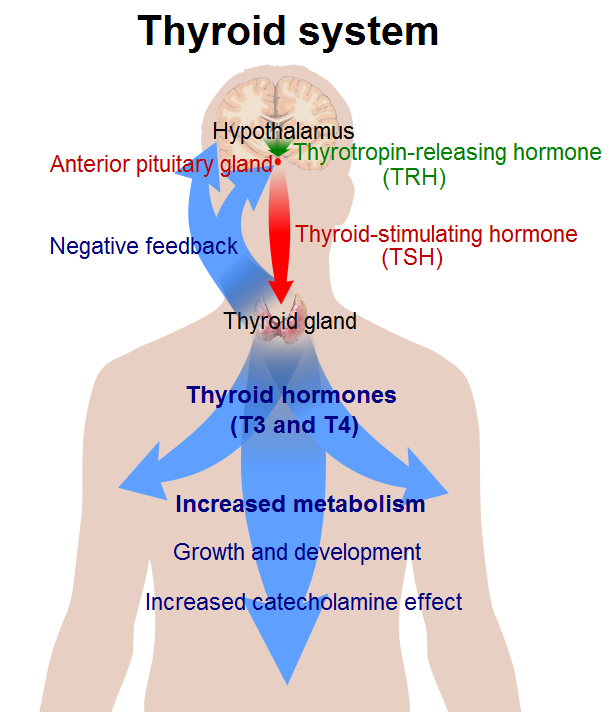
Calcitonin
The calcitonin produced by the parafollicular cells of the thyroid gland has the role of helping to regulate blood calcium levels by stimulating the movement of calcium into bone. Calcitonin is secreted in response to rising blood calcium levels. It decreases blood calcium levels by enhancing calcium absorption and deposition in bone. Calcitonin works hand-in-hand with parathyroid hormone, which is secreted by the parathyroid glands and has the opposite effects as calcitonin. Together, these two hormones maintain calcium homeostasis.
Thyroid Disorders
As with other endocrine disorders, thyroid disorders are generally associated with either over- or under-secretion of hormones. Abnormal secretion of thyroid hormones may occur for a variety of reasons.
Hyperthyroidism
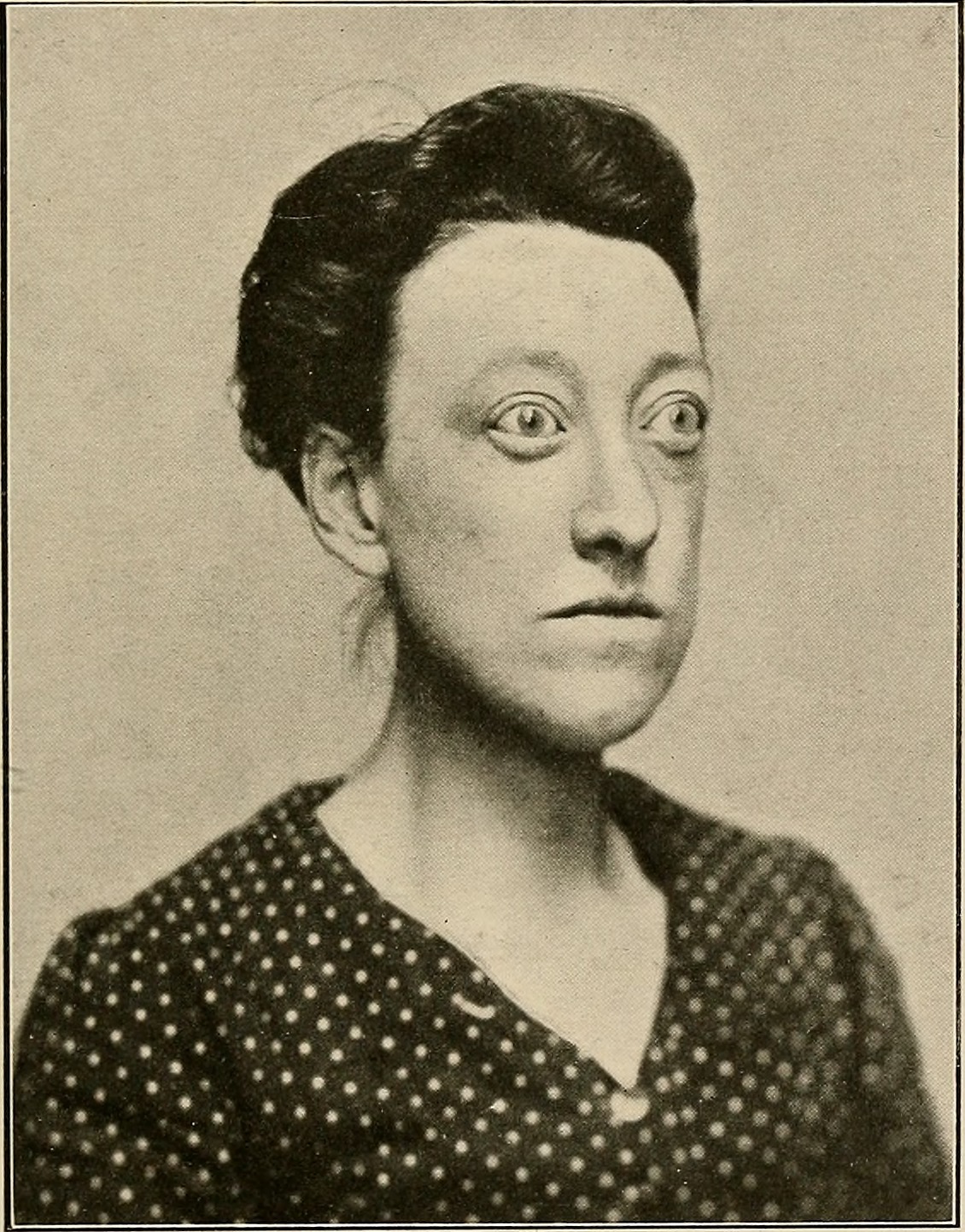
Hyperthyroidism occurs when the thyroid gland produces excessive amounts of thyroid hormones. The most common cause of hyperthyroidism is Graves’ disease. Graves’ disease is an autoimmune disorder in which abnormal antibodies produced by the immune system stimulate the thyroid to secrete excessive quantities of its hormones. This stimulation overrides the usual negative feedback mechanism that normally controls thyroid hormone output. Graves’ disease often results in the formation of an enlarged thyroid (goiter) because of the continued stimulation to produce more hormones.
Besides a goiter, other signs and symptoms of hyperthyroidism may include protruding eyes (see Figure 9.5.5), heart palpitations, excessive sweating, diarrhea, weight loss despite increased appetite, muscle weakness, and unusual sensitivity to heat. Medications can be prescribed to mitigate the symptoms of the disease. Anti-thyroid drugs can also be given to decrease the production of thyroid hormones. If the drugs are ineffective, the gland can be partially or entirely removed. This can be done surgically or with the administration of radioactive iodine. Removal of the thyroid produces hypothyroidism.
Hypothyroidism
Hypothyroidism occurs when the thyroid gland produces insufficient amounts of thyroid hormones. It can result from surgical removal of the thyroid. However, worldwide, the most common cause of hypothyroidism is dietary iodine deficiency. In cases of iodine deficiency, the negative feedback loop controlling the release of thyroid hormone causes repeated stimulation of the thyroid, resulting in the thyroid gland growing in size and producing a goiter. Although the gland gets larger, it cannot increase hormone output because of the lack of iodine in the diet.
Iodine deficiency is uncommon in the Western world because iodine is added to salt. In places like this where iodine deficiency isn't a problem, the most common cause of hypothyroidism is Hashimoto’s thyroiditis. This is another autoimmune disease, but in this case, the immune system destroys the thyroid gland, producing hypothyroidism. Hashimoto’s thyroiditis tends to run in families, so it is likely to have a genetic component. It usually appears after the age of 30, and is more common in females than males.
Hypothyroidism produces many signs and symptoms, as shown in Figure 9.5.6. These may include abnormal weight gain, tiredness, baldness, cold intolerance, and slow heart rate. Hypothyroidism is generally treated with thyroid hormone replacement therapy. This may be needed for the rest of a person’s life.
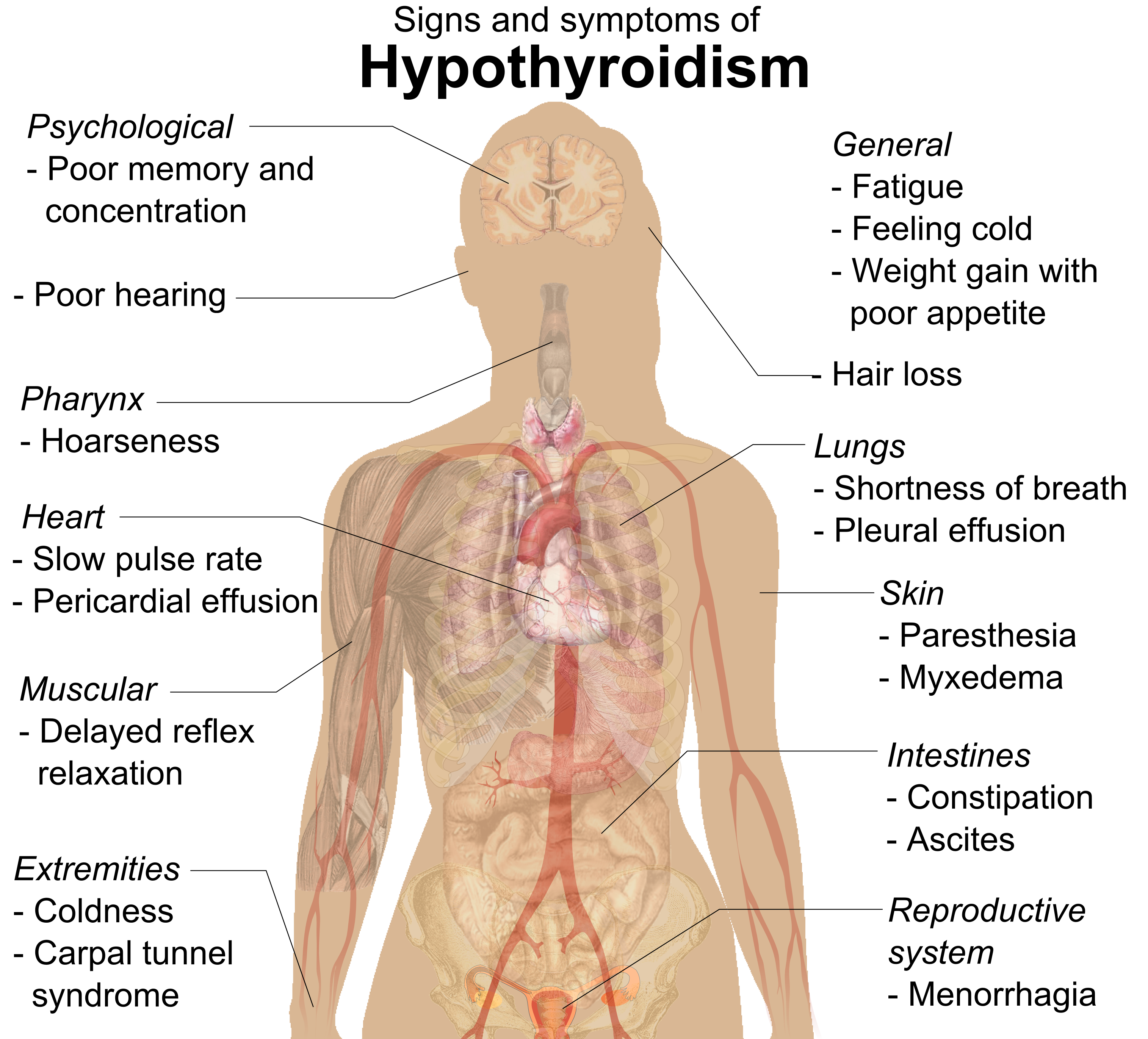
Hypothyroidism in a pregnant woman can have serious adverse consequences for the fetus. During the fetal period, cells of the developing brain are a major target for thyroid hormones, which play a crucial role in brain maturation. When levels of thyroid hormones are too low, the fetus may suffer permanent deficits in cognitive abilities. Deafness is also a potential outcome of hypothyroidism in utero.
Feature: Myth vs. Reality
Thyroid disorders are relatively common, affecting as many as 20 million people in the United States. According to recent studies, one in ten Canadians have some type of thyroid condition and up to 50 per cent may be undiagnosed! Because thyroid disorders are common, there are also many common myths about them.
Myth |
Reality |
| "If you have a thyroid problem, you will know something is wrong because you will have obvious symptoms." | The majority of people with a thyroid disorder are not aware they have it, because the symptoms are often mild, nonspecific, and easy to ignore. Generally, blood tests of thyroid hormone levels are needed to make a conclusive diagnosis. |
| "If you are diagnosed with a thyroid disorder, you will have to take medication for the rest of your life." | Whether you need to continue thyroid medication for life depends on the cause of the disorder. For example, some women develop hypothyroidism during pregnancy but no longer need medication after the pregnancy is over and hormone levels return to normal. |
| "As soon as you start taking thyroid medication, your symptoms will resolve." | It often takes weeks — or even months — for thyroid hormone levels to return to normal and for symptoms to disappear. |
| "You can take an over-the-counter iodine supplement to correct hypothyroidism." | In the United States, where dietary iodine is almost always adequate, iodine deficiency is unlikely to be the cause of hypothyroidism. Therefore, taking supplemental iodine is not likely to correct the problem. |
| "If thyroid symptoms are mild, you don’t need to take medication." | Because thyroid hormones are responsible for so many vital body functions, failing to treat even a mild thyroid disorder may lead to a range of other problems, such as osteoporosis or infertility. |
| "Goiter may be caused by eating “goitrogenic” vegetables, such as broccoli, Brussels sprouts, and spinach." | Although these foods can interfere with the thyroid’s ability to process iodide, you would have to eat huge amounts of them to cause a goiter. |
| "Thyroid disorders occur only after middle age and only in women." | Thyroid disorders may occur at any age and in any sex. Hypothyroidism occurs more commonly in older adults, but hyperthyroidism occurs more commonly in younger adults. Although women are more likely to develop thyroid disorders, about 20 per cent of cases occur in men. |
9.5 Summary
- The thyroid gland is a large endocrine gland in the front of the neck. It is composed mainly of clusters of cells called follicles, which are specialized to absorb iodine and use it to make thyroid hormones. Parafollicular cells among the follicles synthesize the hormone calcitonin.
- Thyroxine (T4) and triiodothyronine (T3) cross cell membranes and regulate gene expression to control the rate of metabolism in cells body-wide, among other functions. The production of T4 and T3 is regulated by thyroid stimulating hormone (TSH) from the pituitary, which is regulated, in turn, by thyrotropin releasing hormone (TRH) from the hypothalamus.
- Calcitonin helps regulate blood calcium levels by stimulating the movement of calcium into bone. It works in conjunction with parathyroid hormone to maintain calcium homeostasis.
- Abnormal secretion of thyroid hormones may occur for a variety of reasons, and it may lead to the development of a goiter. The most common cause of hyperthyroidism is Graves’ disease, an autoimmune disorder. Iodine deficiency is a common cause of hypothyroidism worldwide. In the United States, the most common cause of hypothyroidism is Hashimoto’s thyroiditis, another autoimmune disorder. Hypothyroidism in pregnant women may cause permanent cognitive deficits in children.
9.5 Review Questions
- Describe the structure and location of the thyroid gland.
- Identify the types of cells within the thyroid gland that produce hormones.
-
- Compare and contrast T4 and T3.
- How do T4 and T3 affect body cells?
- Explain how T4 and T3 production is regulated.
- What is calcitonin's function?
- Identify the chief cause and effects of hyperthyroidism.
- What are two possible causes of hypothyroidism?
- List signs and symptoms of hypothyroidism.
- Why is it that both hyperthyroidism and hypothyroidism cause goiters?
- Choose one symptom each for hyperthyroidism and hypothyroidism. Based on the functions of thyroid hormones, explain why each symptom occurs.
- In cases of hypothyroidism caused by Hashimoto’s thyroiditis or removal of the thyroid gland to treat hyperthyroidism, patients are often given medication to replace the missing thyroid hormone. Explain why the level of replacement thyroid hormone must be carefully monitored and adjusted if needed.
9.5 Explore More
https://www.youtube.com/watch?v=iNrUpBwU3q0
How does the thyroid manage your metabolism? - Emma Bryce, TED-Ed, 2015.
https://www.youtube.com/watch?v=oINxr8_nR_Y&feature=emb_logo
Graves' Disease and Hashimoto's Thyroiditis, hardgrindcoffeeyo, 2014.
https://www.youtube.com/watch?v=-5W7eEX-u3U&feature=emb_logo
The Fukushima Nuclear Accident documentary, World Disasters, 2014.
Attribution
Figure 9.5.1
- Goiter by Drahreg01 on Wikimedia Commons is used under a CC BY-SA 3.0 (https://creativecommons.org/licenses/by-sa/3.0) license.
- [adapted] A_woman_suffering_from_Goiter by MyUpchar.com on Wikimedia Commons is used under a CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0) license.
Figure 9.5.2
Thyroid gland by National Cancer Institute is in the public domain (https://en.wikipedia.org/wiki/Public_domain).
Figure 9.5.3
Structural model representing a single molecule of thyroxine (T4) from CK-12 Foundation is an image of a chemical structure model and is non-copyrightable.
Figure 9.5.4
Thyroid_system by Mikael Häggström on Wikimedia Commons is in the public domain (https://en.wikipedia.org/wiki/Public_domain).
Figure 9.5.5
Case of Graves disease without goitre by Internet Archive Book Images on Flickr is believed to have No known copyright restrictions. [Image from page 226 of "The thyroid gland in health and disease" (1917)]
Figure 9.5.6
Signs_and_symptoms_of_hypothyroidism by Mikael Häggström. on Wikimedia Commons is used under a CC0 1.0 Universal Public Domain Dedication license (https://creativecommons.org/publicdomain/zero/1.0/deed.en).
About thyroid disease. (n.d.). Thyroid Foundation of Canada. https://thyroid.ca/thyroid-disease/
Häggström, M. (2014). Medical gallery of Mikael Häggström 2014. WikiJournal of Medicine 1 (2). DOI:10.15347/wjm/2014.008. ISSN 2002-4436.
hardgrindcoffeeyo. (2014, July 19). Graves' disease and Hashimoto's thyroiditis. YouTube. https://www.youtube.com/watch?v=oINxr8_nR_Y&feature=youtu.be
TED-Ed. (2015, March 2). How does the thyroid manage your metabolism? - Emma Bryce. YouTube. https://www.youtube.com/watch?v=iNrUpBwU3q0&feature=youtu.be
World Disasters. (2014, April 5). The Fukushima nuclear accident documentary. YouTube. https://www.youtube.com/watch?v=-5W7eEX-u3U&feature=youtu.be

