15.7 Disorders of the Gastrointestinal Tract

Crohn’s Rash
If you had a skin rash like the one shown in Figure 15.7.1, you probably wouldn’t assume that it was caused by a digestive system disease. However, that’s exactly why the individual in the picture has a rash. He has a gastrointestinal (GI) tract disorder called Crohn’s disease. This disease is one of a group of GI tract disorders that are known collectively as inflammatory bowel disease. Unlike other inflammatory bowel diseases, signs and symptoms of Crohn’s disease may not be confined to the GI tract.
Inflammatory Bowel Disease
Inflammatory bowel disease (IBD) is a collection of inflammatory conditions primarily affecting the intestines. The two principal inflammatory bowel diseases are Crohn’s disease and ulcerative colitis. Unlike Crohn’s disease — which may affect any part of the GI tract and the joints, as well as the skin — ulcerative colitis mainly affects just the colon and rectum. Both diseases occur when the body’s own immune system attacks the digestive system. Both diseases typically first appear in the late teens or early twenties, and occur equally in males and females. Approximately 270,000 Canadians are currently living with IBD, 7,000 of which are children. The annual cost of caring for these Canadians is estimated at $1.28 billion. The number of cases of IBD has been steadily increasing and it is expected that by 2030 the number of Canadians suffering from IBD will grow to 400,000.
Crohn’s Disease
Crohn’s disease is a type of inflammatory bowel disease that may affect any part of the GI tract from the mouth to the anus, among other body tissues. The most commonly affected region is the ileum, which is the final part of the small intestine. Signs and symptoms of Crohn’s disease typically include abdominal pain, diarrhea (with or without blood), fever, and weight loss. Malnutrition because of faulty absorption of nutrients may also occur. Potential complications of Crohn’s disease include obstructions and abscesses of the bowel. People with Crohn’s disease are also at slightly greater risk than the general population of developing bowel cancer. Although there is a slight reduction in life expectancy in people with Crohn’s disease, if the disease is well-managed, affected people can live full and productive lives. Approximately 135,000 Canadians are living with Crohn’s disease.
Crohn’s disease is caused by a combination of genetic and environmental factors that lead to impairment of the generalized immune response (called innate immunity). The chronic inflammation of Crohn’s disease is thought to be the result of the immune system “trying” to compensate for the impairment. Dozens of genes are likely to be involved, only a few of which have been identified. Because of the genetic component, close relatives such as siblings of people with Crohn’s disease are many times more likely to develop the disease than people in the general population. Environmental factors that appear to increase the risk of the disease include smoking tobacco and eating a diet high in animal proteins. Crohn’s disease is typically diagnosed on the basis of a colonoscopy, which provides a direct visual examination of the inside of the colon and the ileum of the small intestine.
People with Crohn’s disease typically experience recurring periods of flare-ups followed by remission. There are no medications or surgical procedures that can cure Crohn’s disease, although medications such as anti-inflammatory or immune-suppressing drugs may alleviate symptoms during flare-ups and help maintain remission. Lifestyle changes, such as dietary modifications and smoking cessation, may also help control symptoms and reduce the likelihood of flare-ups. Surgery may be needed to resolve bowel obstructions, abscesses, or other complications of the disease.
Ulcerative Colitis
Ulcerative colitis is an inflammatory bowel disease that causes inflammation and ulcers (sores) in the colon and rectum. Unlike Crohn’s disease, other parts of the GI tract are rarely affected in ulcerative colitis. The primary symptoms of the disease are lower abdominal pain and bloody diarrhea. Weight loss, fever, and anemia may also be present. Symptoms typically occur intermittently with periods of no symptoms between flare-ups. People with ulcerative colitis have a considerably increased risk of colon cancer and should be screened for colon cancer more frequently than the general population. Ulcerative colitis, however, seems to primarily reduce the quality of life, and not the lifespan.
The exact cause of ulcerative colitis is not known. Theories about its cause involve immune system dysfunction, genetics, changes in normal gut bacteria, and lifestyle factors, such as a diet high in animal protein and the consumption of alcoholic beverages. Genetic involvement is suspected in part because ulcerative colitis tens to “run” in families. It is likely that multiple genes are involved. Diagnosis is typically made on the basis of colonoscopy and tissue biopsies.
Lifestyle changes, such as reducing the consumption of animal protein and alcohol, may improve symptoms of ulcerative colitis. A number of medications are also available to treat symptoms and help prolong remission. These include anti-inflammatory drugs and drugs that suppress the immune system. In cases of severe disease, removal of the colon and rectum may be required and can cure the disease.
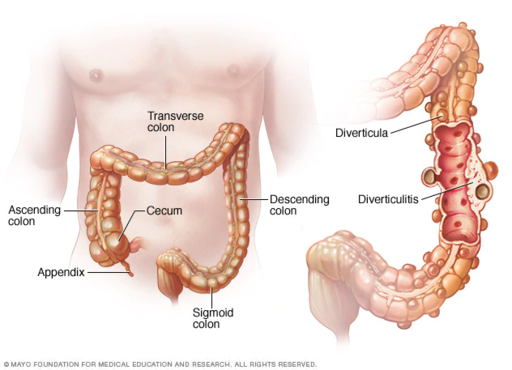
Diverticulitis
Diverticulitis is a digestive disease in which tiny pouches in the wall of the large intestine become infected and inflamed. Symptoms typically include lower abdominal pain of sudden onset. There may also be fever, nausea, diarrhea or constipation, and blood in the stool. Having large intestine pouches called diverticula (see Figure 15.7.2) that are not inflamed is called diverticulosis. Diverticulosis is thought to be caused by a combination of genetic and environmental factors, and is more common in people who are obese. Infection and inflammation of the pouches (diverticulitis) occurs in about 10–25% of people with diverticulosis, and is more common at older ages. The infection is generally caused by bacteria.
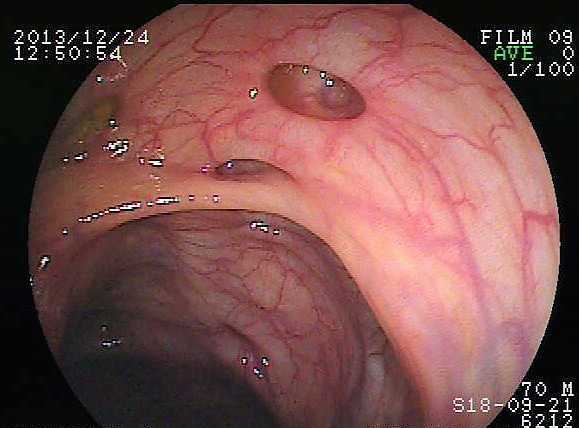
Diverticulitis can usually be diagnosed with a CT scan and can be monitored with a colonoscopy (as seen in Figure 15.7.3). Mild diverticulitis may be treated with oral antibiotics and a short-term liquid diet. For severe cases, intravenous antibiotics, hospitalization, and complete bowel rest (no nourishment via the mouth) may be recommended. Complications such as abscess formation or perforation of the colon require surgery.
Peptic Ulcer
A peptic ulcer is a sore in the lining of the stomach or the duodenum (first part of the small intestine). If the ulcer occurs in the stomach, it is called a gastric ulcer. If it occurs in the duodenum, it is called a duodenal ulcer. The most common symptoms of peptic ulcers are upper abdominal pain that often occurs in the night and improves with eating. Other symptoms may include belching, vomiting, weight loss, and poor appetite. Many people with peptic ulcers, particularly older people, have no symptoms. Peptic ulcers are relatively common, with about ten per cent of people developing a peptic ulcer at some point in their life.
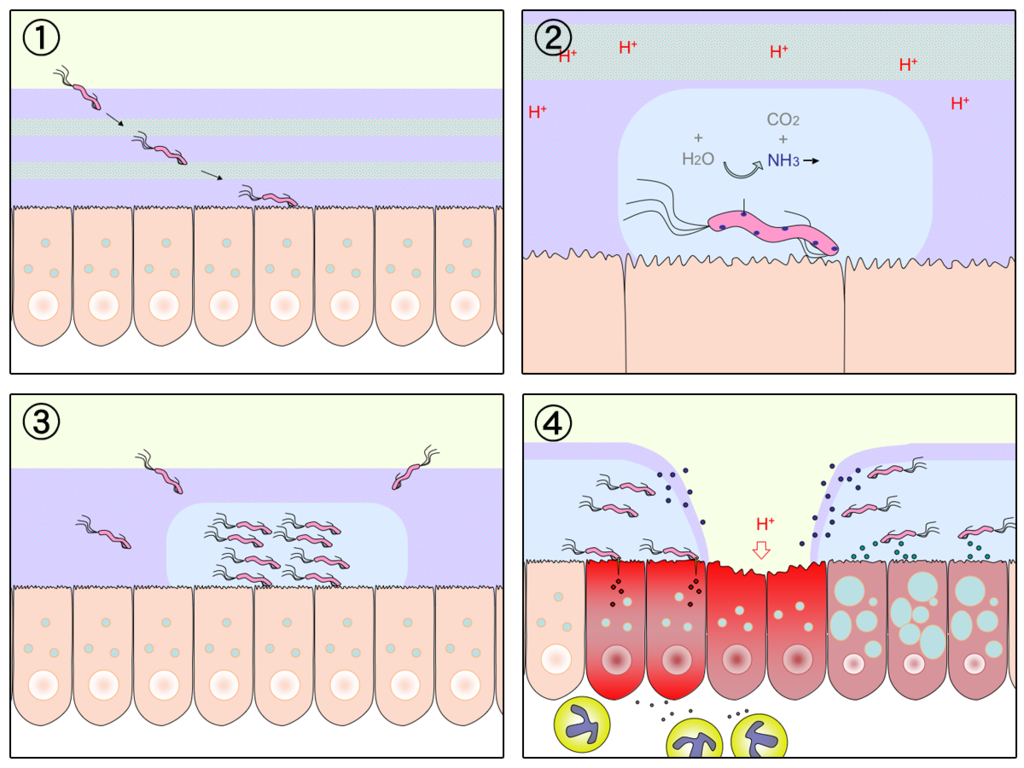
The most common cause of peptic ulcers is infection with the bacterium Helicobacter pylori, which may be transmitted by food, contaminated water, or human saliva (for example, by kissing or sharing eating utensils). Surprisingly, the bacterial cause of peptic ulcers was not discovered until the 1980s. The scientists who made the discovery are Australians Robin Warren and Barry J. Marshall. Although the two scientists eventually won a Nobel Prize for their discovery, their hypothesis was poorly received at first. To demonstrate the validity of their discovery, Marshall used himself in an experiment. He drank a culture of bacteria from a peptic ulcer patient and developed symptoms of peptic ulcer in a matter of days. His symptoms resolved on their own within a couple of weeks, but, at his wife’s urging, he took antibiotics to kill any remaining bacteria. Marshall’s self-experiment was published in the Australian Medical Journal, and is among the most cited articles ever published in the journal. Figure 15.7.4 shows how H. pylori cause peptic ulcers.
Another relatively common cause of peptic ulcers is chronic use of non-steroidal anti-inflammatory drugs (NSAIDs), such as aspirin or ibuprofen. Additional contributing factors may include tobacco smoking and stress, although these factors have not been demonstrated conclusively to cause peptic ulcers independent of H. pylori infection. Contrary to popular belief, diet does not appear to play a role in either causing or preventing peptic ulcers. Eating spicy foods and drinking coffee and alcohol were once thought to cause peptic ulcers. These lifestyle choices are no longer thought to have much (if any) of an effect on the development of peptic ulcers.
Peptic ulcers are typically diagnosed on the basis of symptoms or the presence of H. pylori in the GI tract. However, endoscopy (shown in Figure 15.7.5), which allows direct visualization of the stomach and duodenum with a camera, may be required for a definitive diagnosis. Peptic ulcers are usually treated with antibiotics to kill H. pylori, along with medications to temporarily decrease stomach acid and aid in healing. Unfortunately, H. pylori has developed resistance to commonly used antibiotics, so treatment is not always effective. If a peptic ulcer has penetrated so deep into the tissues that it causes a perforation of the wall of the stomach or duodenum, then emergency surgery is needed to repair the damage.

Gastroenteritis
Gastroenteritis, also known as infectious diarrhea or stomach flu, is an acute and usually self-limiting infection of the GI tract by pathogens. Symptoms typically include some combination of diarrhea, vomiting, and abdominal pain. Fever, lack of energy, and dehydration may also occur. The illness generally lasts less than two weeks, even without treatment, but in young children it is potentially deadly. Gastroenteritis is very common, especially in poorer nations. Worldwide, up to five billion cases occur each year, resulting in about 1.4 million deaths.
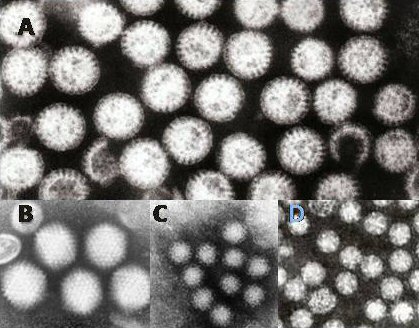
Commonly called “stomach flu,” gastroenteritis is unrelated to the influenza virus, although viruses are the most common cause of the disease (see Figure 15.7.6). In children, rotavirus is most often the cause which is why the British Columbia immunization schedule now includes a rotovirus vaccine. Norovirus is more likely to be the cause of gastroenteritis in adults. Besides viruses, other potential causes of gastroenteritis include fungi, bacteria (most often E. coli or Campylobacter jejuni), and protozoa(including Giardia lamblia, more commonly called Beaver Fever, described below). Transmission of pathogens may occur due to eating improperly prepared foods or foods left to stand at room temperature, drinking contaminated water, or having close contact with an infected individual.
Gastroenteritis is less common in adults than children, partly because adults have acquired immunity after repeated exposure to the most common infectious agents. Adults also tend to have better hygiene than children. If children have frequent repeated incidents of gastroenteritis, they may suffer from malnutrition, stunted growth, and developmental delays. Many cases of gastroenteritis in children can be avoided by giving them a rotavirus vaccine. Frequent and thorough handwashing can cut down on infections caused by other pathogens.
Treatment of gastroenteritis generally involves increasing fluid intake to replace fluids lost in vomiting or diarrhea. Oral rehydration solution, which is a combination of water, salts, and sugar, is often recommended. In severe cases, intravenous fluids may be needed. Antibiotics are not usually prescribed, because they are ineffective against viruses that cause most cases of gastroenteritis.
Giardiasis
Giardiasis, popularly known as beaver fever, is a type of gastroenteritis caused by a GI tract parasite, the single-celled protozoan Giardia lamblia (pictured in Figure 15.7.7). In addition to human beings, the parasite inhabits the digestive tract of a wide variety of domestic and wild animals, including cows, rodents, and sheep, as well as beavers (hence its popular name). Giardiasis is one of the most common parasitic infections in people the world over, with hundreds of millions of people infected worldwide each year.

Transmission of G. lamblia is via a fecal-oral route (as in, you got feces in your food). Those at greatest risk include travelers to countries where giardiasis is common, people who work in child-care settings, backpackers and campers who drink untreated water from lakes or rivers, and people who have close contact with infected people or animals in other settings. In Canada, Giardia is the most commonly identified intestinal parasite and approximately 3,000 Canadians will contract the parasite annually.
Symptoms of giardiasis can vary widely. About one-third third of people with the infection have no symptoms, whereas others have severe diarrhea with poor absorption of nutrients. Problems with absorption occur because the parasites inhibit intestinal digestive enzyme production, cause detrimental changes in microvilli lining the small intestine, and kill off small intestinal epithelial cells. The illness can result in weakness, loss of appetite, stomach cramps, vomiting, and excessive gas. Without treatment, symptoms may continue for several weeks. Treatment with anti-parasitic medications may be needed if symptoms persist longer or are particularly severe.
15.7 Summary
- Inflammatory bowel disease is a collection of inflammatory conditions primarily affecting the intestines. The diseases involve the immune system attacking the GI tract, and they have multiple genetic and environmental causes. Typical symptoms include abdominal pain and diarrhea, which show a pattern of repeated flare-ups interrupted by periods of remission. Lifestyle changes and medications may control flare-ups and extend remission. Surgery is sometimes required.
- The two principal inflammatory bowel diseases are Crohn’s disease and ulcerative colitis. Crohn’s disease may affect any part of the GI tract from the mouth to the anus, among other body tissues. Ulcerative colitis affects the colon and/or rectum.
- Some people have little pouches, called diverticula, in the lining of their large intestine, a condition called diverticulosis. People with diverticulosis may develop diverticulitis, in which one or more of the diverticula become infected and inflamed. Diverticulitis is generally treated with antibiotics and bowel rest. Sometimes, surgery is required.
- A peptic ulcer is a sore in the lining of the stomach (gastric ulcer) or duodenum (duodenal ulcer). The most common cause is infection with the bacterium Helicobacter pylori. NSAIDs (such as aspirin) can also cause peptic ulcers, and some lifestyle factors may play contributing roles. Antibiotics and acid reducers are typically prescribed, and surgery is not often needed.
- Gastroenteritis, or infectious diarrhea, is an acute and usually self-limiting infection of the GI tract by pathogens, most often viruses. Symptoms typically include diarrhea, vomiting, and/or abdominal pain. Treatment includes replacing lost fluids. Antibiotics are not usually effective.
- Giardiasis is a type of gastroenteritis caused by infection of the GI tract with the protozoa parasite Giardia lamblia. It may cause malnutrition. Generally self-limiting, severe or long-lasting cases may require antibiotics.
15.7 Review Questions
-
-
- Compare and contrast Crohn’s disease and ulcerative colitis.
- How are diverticulosis and diverticulitis related?
- Identify the cause of giardiasis. Why may it cause malabsorption?
- Name three disorders of the GI tract that can be caused by bacteria.
- Name one disorder of the GI tract that can be helped by anti-inflammatory medications, and one that can be caused by chronic use of anti-inflammatory medications.
- Describe one reason why it can be dangerous to drink untreated water.
15.7 Explore More
Who’s at risk for colon cancer? – Amit H. Sachdev and Frank G. Gress, TED-Ed, 2018.
The surprising cause of stomach ulcers – Rusha Modi, TED-Ed, 2017.
Attributions
Figure 15.7.1
BADAS_Crohn by Dayavathi Ashok and Patrick Kiely/ Journal of medical case reports on Wikimedia Commons is used under a CC BY 2.0 (https://creativecommons.org/licenses/by/2.0) license.
Figure 15.7.2
512px-Ds00070_an01934_im00887_divert_s_gif.webp by Lfreeman04 on Wikimedia Commons is used under a CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0) license.
Figure 15.7.3
Colon_diverticulum by melvil on Wikimedia Commons is used under a CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0) license.
Figure 15.7.4
H_pylori_ulcer_diagram by Y_tambe on Wikimedia Commons is used under a CC BY-SA 3.0 (http://creativecommons.org/licenses/by-sa/3.0/) license.
Figure 15.7.5
1024px-Endoscopy_training by Yuya Tamai on Wikimedia Commons is used under a CC BY 2.0 (https://creativecommons.org/licenses/by/2.0) license.
Figure 15.7.6
Gastroenteritis_viruses by Dr. Graham Beards [en:User:Graham Beards] at en.wikipedia on Wikimedia Commons is used under a CC BY 3.0 (https://creativecommons.org/licenses/by/3.0) license.
Figure 15.7.7
Giardia_lamblia_SEM_8698_lores by Janice Haney Carr from CDC/ Public Health Image Library (PHIL) ID# 8698 on Wikimedia Commons is in the public domain (https://en.wikipedia.org/wiki/public_domain).
References
Ashok, D., & Kiely, P. (2007). Bowel associated dermatosis – arthritis syndrome: a case report. Journal of medical case reports, 1, 81. https://doi.org/10.1186/1752-1947-1-81
Marshall, B. J., Armstrong, J. A., McGechie, D. B., & Glancy, R. J. (1985). Attempt to fulfil Koch’s postulates for pyloric Campylobacter. The Medical Journal of Australia, 142(8), 436–439.
Marshall, B. J., McGechie, D. B., Rogers, P. A., & Glancy, R. J. (1985). Pyloric campylobacter infection and gastroduodenal disease. The Medical Journal of Australia, 142(8), 439–444.
TED-Ed. (2017, September 28). The surprising cause of stomach ulcers – Rusha Modi. YouTube. https://www.youtube.com/watch?v=V_U6czbDHLE&feature=youtu.be
TED-Ed. (2018, January 4). Who’s at risk for colon cancer? – Amit H. Sachdev and Frank G. Gress. YouTube. https://www.youtube.com/watch?v=H5zin8jKeT0&feature=youtu.be
Figure 6.7.1 Men from Maasai Mara, Kenya.
Built for Heat
These tall, slender men live near the equator in Kenya, East Africa — one of the hottest regions of the world. These and the other people of his tribal group, called the Maasai, are among the tallest, most linear people on the planet. Their body build is thought to be an adaptation to their climate, which is hot year-round.
Climate Extremes
Climate refers to the average weather conditions in a region over a long period of time. One of the main determinants of climate is temperature. Both hot and cold temperatures are serious environmental stresses on the human body.
In the cold, there is risk of hypothermia, which is a dangerous decrease in core body temperature. The normal temperature of the human body is 37 degrees C (98.6 degrees F). Hypothermia sets in when body temperature drops to 34.4 degrees C (94 degrees F). If body temperature falls below 29.4 degrees C (85 degrees F), it starts to cool very rapidly because the body’s temperature regulation mechanism starts to fail.
The opposite problem occurs in the heat, where the risk is hyperthermia, which is a dangerous increase in core body temperature. If human body temperature rises above about 40.6 degrees C (105 degrees F), hyperthermia may become life threatening. If a temperature this high persists more than a few days, it generally damages the brain and other internal organs, leading to death.
Human Adaptation to Heat and Cold
Humans are the most widespread species on the planet, and they have lived in extreme climates for tens of thousands of years. As a result, many human populations have had to cope with extreme temperatures for hundreds of generations, which has forced them to develop genetic adaptations to these climate extremes.
The size and proportions of the human body may play an important role in how well an individual is able to handle hot or cold temperatures. In general, people with a tall, slender build, like the Maasai man pictured in Figure 6.7.1, are well adapted to heat, whereas people with a short, stocky build (like the Indigenous North American Inuit pictured in Figure 6.7.2) are well adapted to cold. These relationships between body build and climate were first noticed in other animal species in the 1800s by biologists Carl Bergmann and Joel Allen. These scientists formulated what are now known as Bergmann’s and Allen’s rules.
Figure 6.7.2 Indigenous North American Inuit.
Bergmann’s Rule
Bergmann's rule states that within a broadly distributed taxonomic group, populations or species of larger size are found in colder environments, whereas populations or species of smaller size are found in warmer environments. Bergmann’s rule has been shown to generally apply to widespread species of mammals and birds, although there are also many exceptions to the rule.
What explains Bergmann’s rule? Larger animals have a lower surface area to volume ratio than smaller animals, which is illustrated in Table 6.7.1 for a simple shape, a cube. From the table, you can see how the surface area to volume ratio of a cube decreases dramatically as the size of the cube increases. Because heat is lost through the surface of the body, an animal with a smaller surface area to volume ratio radiates less body heat per unit of mass. The larger body mass also allows the animal to generate more heat. A larger animal has more cells, so it can produce more body heat as a byproduct of cellular metabolism. Both of these factors allow a larger animal to stay warmer in a cold climate.
Table 6.7.1
Relationship of Surface Area to Volume in Cubes of Different Sizes
| Relationship of Surface Area to Volume in Cubes of Different Sizes | |||
| Side of Cube (cm) | Surface Area of Cube (cm2) | Volume of Cube (cm3) | Surface Area:Volume Ratio |
| 2 | 24 | 8 | 3:1 |
| 4 | 96 | 64 | 3:2 |
| 6 | 216 | 216 | 3:3 |
| 12 | 864 | 1728 | 3:6 |
| 20 | 2400 | 8000 | 3:10 |
Warmer climates impose the opposite problem: body heat generated by metabolism needs to be dissipated quickly rather than stored within the body. Smaller animals have a higher surface area to volume ratio that maximizes heat loss through the surface of the body and helps cool the body. With less mass and fewer cells, smaller animals also generate less heat due to cellular metabolism.

Anthropologists have found that many human populations tend to follow Bergmann’s rule. For example, a study of 100 human populations in the 1950s found a strong negative correlation between mean body mass and average yearly temperature. In other words, higher body mass was generally found in colder places, and lower body mass was generally found in hotter places.
There are also exceptions to the rule, in part because we use cultural responses to temper environmental stresses so we do not need to change genetically or physiologically in order to cope. Humans, for example, use clothing and heated buildings to stay warm in cold climates, which tends to counter the effects of natural selection changing human body shape in cold climates.
Allen’s Rule
Allen’s rule is a corollary of Bergmann’s rule. It states that animals living in hotter climates generally have longer extremities (such as limbs, tails, snouts, and ears) than closely related animals living in colder climates. The explanation for Allen’s rule is similar to the rationale behind Bergmann’s rule. Longer extremities maximize an animal’s surface area, allowing greater heat loss through the surface of the body. Therefore, having long extremities is adaptive in hot climates where the main challenge is dissipating body heat.
Anthropologists have noted that, in populations that have lived in tropical regions for long periods of time, the limbs of people tend to be longer in proportion to overall body height. The Maasai man pictured in Figure 6.7.1 is a clear example. His exceptionally long limbs — like those of other members of his population — are optimally proportioned for the hot climate in Kenya. The shorter-limbed body proportions of the Inuit people (Figure 6.7.2) suit them well for their cold climate. Marked differences in limb length have also been observed in related populations that have lived for long periods of time at different altitudes. High altitudes have colder climates than lower altitudes and — consistent with Allen's rule —people tend to have shorter limbs at higher altitudes.
Other Human Responses to Heat
Humans exhibit several other responses to high temperatures that are generally considered either short-term physiological responses or examples of longer-term acclimatization.
Sweating and Humidity

Because humans are basically tropical animals, we generally have an easier time dealing with excessive heat than excessive cold. Evaporation of sweat is the main way we cool the body. The dancer in Figure 6.7.4 is sweating copiously while working out in a hot environment. Why does sweating cool us? When sweat evaporates from the skin, it requires heat. The heat comes from the surface of the body, resulting in evaporative cooling.
How well we can deal with high air temperatures depends in large part on the humidity of the air. We have a harder time losing excess body heat when the humidity is high because our sweat does not evaporate as well as it does when the humidity is low. Instead, the sweat stays on the skin, making us feel clammy and warmer than we would feel if the humidity were lower. If the air is dry, on the other hand, sweat evaporates readily, and we feel more comfortable. For this reason, we are able to tolerate higher temperatures when the humidity is low. This is the basis of the common aphorism, “It’s not the heat, but the humidity.”
The heat index (HI) is a number that combines air temperature and relative humidity to indicate how hot the air feels due to the humidity. The heat index is also called "apparent temperature.” Figure 6.7.5 shows the heat index at different combinations of air temperature and relative humidity. As you can see, when the humidity is very high, even a 90-degree F (32 degrees C) temperature can be very dangerous.
Acclimatization to Heat

If humidity is low, evaporation of sweat can be an effective way to keep the body from overheating. However, the loss of water and salts in sweat can also be dangerous. In very hot conditions, an adult may lose up to four litres of sweat per hour and up to 14 litres per day. Such water losses may cause severe dehydration if the water is not replaced by drinking much more than usual. The loss of salts may also upset the normal salt balance in the body, which can be dangerous. Becoming acclimatized to heat by gradually increasing the exposure time to high temperatures — particularly while exercising or doing physical work — can reduce the risk of these effects.
It may take up to 14 days to attain maximum heat acclimatization. As the body becomes acclimatized, sweat output increases, and sweating begins sooner. The salt content of the sweat also declines, as does the output of urine. These and other physiological changes help the body lose heat through the evaporation of sweat, while maintaining the proper balance of salts and fluids in the body. There may also be increased blood flow to the body surface through the widening of blood vessels near the skin. This is called vasodilation. This brings more heat from the body core to the skin, and from there it may be radiated out into the environment.
Becoming acclimatized to heat allows one to safely perform more exercise or work in the heat. It also helps prevent heat-related illnesses by reducing strain on the body. Heat-related illnesses — from least to most serious — include heat cramps, heat exhaustion, and heat stroke.
- Heat cramps are muscle spasms caused by loss of water and salts. They often follow prolonged sweating brought on by over-exertion in hot weather.
- Heat exhaustion is a condition in which over-heating of the body causes dizziness, headache, profuse sweating, rapid heartbeat. and other symptoms. Without prompt treatment, heat exhaustion can lead to heat stroke.
- Heat stroke is potentially life threatening and a medical emergency. Heat stroke results from prolonged exposure to high temperatures, usually in combination with dehydration. It leads to failure of the body's temperature control system and is diagnosed when the core body temperature exceeds 105 degrees F (40 degrees C). Symptoms may include nausea, seizures, confusion, disorientation, and coma.
Acclimatization to heat, like other types of acclimatization, is a reversible process. Just as quickly as heat acclimatization occurs, the physiological changes fade away in the absence of heat exposure. The body returns to its baseline state within a week or two of no longer exercising or working at high temperatures.
Other Human Responses to Cold
Besides genetic difference in body build, there are two major ways the human body can respond to the cold. One way is by producing more body heat, and the other way is by conserving more body heat. An immediate response to cooling of the body is shivering. This is an involuntary and simultaneous contraction of many tiny muscles in the body. These muscle contractions generate a small amount of heat. Another early response to cold temperature is a narrowing of blood vessels near the skin. This is called vasoconstriction. This helps to shunt blood away from the body surface so more heat is held at the body core. The skin cools down and radiates less heat into the environment.
Hunting Response
At temperatures below freezing, vasoconstriction can be dangerous if it lasts too long. The extremities become too cold because of lack of blood flow, and cold injury (such as frostbite) may occur. Frostbite is tissue destruction that occurs when tissue freezes. You can see a mild-to-moderate case of frostbite of the fingers in Figure 6.7.7. If frostbite is severe, it may lead to gangrene and amputation of the affected extremities.

The body counters the possibility of cold injury with a reaction called the hunting response. This is a process of alternating vasoconstriction and vasodilation in extremities exposed to cold. About five to ten minutes after the start of cold exposure, the blood vessels in the extremities suddenly dilate, which increases blood flow and subsequently the temperature of the extremities. This is soon followed by another phase of vasoconstriction, and then the process repeats.
The hunting response occurs in most people, but several factors may influence the strength of the response. People who live or work regularly in cold environments show an increased hunting response. Through acclimatization, however, tropical residents can develop an increased response, which is indistinguishable from that of arctic residents. Genetic factors may play a role in the hunting response, but this is uncertain because it is difficult to differentiate between adaptation and acclimatization.
Persistent Vasoconstriction
Where temperatures rarely fall below freezing but are repeatedly very chilly, the hunting response may not occur. Instead, vasoconstriction may persist to keep heat within the body at the expense of cooling the skin. As long as the temperature stays above freezing, cold injury (such as frostbite) will not occur. This type of response has been shown to occur in indigenous desert dwellers in southern Africa and Australia, where the temperature is hot during the day and very cold at night. People in these populations also tend to deposit fat around the organs in their chest and abdomen. The fat serves as insulation, protecting vital structures from the cold.
High-Fat Diet
Besides shivering, another way to increase body heat is to raise the basal metabolic rate. The basal metabolic rate (BMR) is the amount of energy that a person needs to keep the body functioning at rest. The higher the BMR, the more heat the body generates, even without exercise or physical labor. The BMR can be increased by consuming large quantities of high-calorie fatty foods. People living in very cold subarctic regions, including the Inuit, traditionally ate whale and seal blubber and other high-fat foods, which helped them maintain a high BMR and stay warm.
Figure 6.7.8 Whale and seal blubber (mainly on abundant ring seals) is an important part of the traditional Inuit diet.
Feature: Human Biology in the News
Too many news stories report young children being seriously injured or dying from heat stroke in hot vehicles. On average, 38 children die in hot vehicles each year from heat-related deaths after being trapped inside. Most often, this happens by accident, when a parent or caregiver unknowingly leaves a sleeping child in a car. In other cases, children get into cars on their own, and then cannot get out again.
A child’s thermoregulatory system is not as efficient as that of an adult, and a child’s body temperature may increase as much as five times faster. This makes children prime candidates for heat stroke. A motor vehicle is also easily heated by direct sun. The windows of the vehicle allow solar radiation to pass through and heat up objects inside. A dark-coloured dashboard or seat may quickly reach a temperature of more than 180 degrees F (82 degrees C)! These hot surfaces can just as quickly heat the adjacent air, rapidly increasing the temperature of the air trapped inside the vehicle.
Here are several simple tips that parents and caregivers can follow to prevent heat stroke tragedies:
- Never leave children alone in or around cars — not even for a minute.
- Always open the back door and check the back seat before leaving your vehicle to be sure no child has been left behind.
- Put something you will need, such as your cell phone or handbag, in the back seat so you will have to open the back door to retrieve it whenever you park the car.
- Keep a large stuffed animal in the child's car seat, and when the child is placed in the car seat, put the stuffed animal in the front passenger seat as a visual reminder that the child is in the back.
- Make sure you have a strict policy in place with everyone involved in the care of your child that you should always be called whenever your child does not show up at daycare or school as scheduled.
- Keep vehicles locked at all times, even in driveways and garages. Ask home visitors, child care providers, and neighbors to do the same.
- Keep car keys and remote vehicle openers out of reach of children.
- If a child is missing, immediately check the inside passenger compartments and trunks of all vehicles in the area. Check vehicles even if they are locked, because a child may lock a vehicle after entering and not be able to unlock it again to get out.
- If you see a child alone in a vehicle, call 911 immediately. If the child seems hot or sick, get them out of the vehicle as quickly as possible.
- Pay for gas at the pump and use drive-throughs at the bank, pharmacy, or wherever else they are available.
6.7 Summary
- Both hot and cold temperatures are serious environmental stresses on the human body. In the cold, there is risk of hypothermia, which is a dangerous decrease in core body temperature. In the heat, there is risk of hyperthermia, which is a dangerous increase in core body temperature.
- According to Bergmann’s rule, body size tends to be negatively correlated with temperature, because larger body size increases heat production and decreases heat loss. The opposite holds true for small body size. Bergmann’s rule applies to many human populations that are hot- or cold-adapted.
- According to Allen’s rule, the length of body extremities is positively correlated with temperature, because longer extremities are better at dissipating excess body heat. The opposite applies to shorter extremities. Allen’s rule applies to relative limb lengths in many human populations that have adapted to heat or cold.
- Sweating is the primary way that humans lose body heat. The evaporation of sweat from the skin cools the body. This only works well when the relative humidity is fairly low. At high relative humidity, sweat does not readily evaporate to cool us down. The heat index (HI) indicates how hot it feels due to the humidity.
- Gradually working longer and harder in the heat can bring about heat acclimatization, in which the body has improved responses to heat stress. For example, sweating starts earlier, sweat contains less salt, and vasodilation brings heat to the surface to help cool the body. Full acclimatization takes up to 14 days and reverses just as quickly when the heat stress is removed.
- The human body can respond to cold by producing more heat (by shivering or increasing the basal metabolic rate) or by conserving heat (by vasoconstriction at the body surface or a layer of fat-insulating internal organs).
- At temperatures below freezing, the hunting response occurs to prevent cold injury, such as frostbite. This is a process of alternating vasoconstriction and vasodilation in extremities that are exposed to dangerous cold. Where temperatures are repeatedly cold but rarely below freezing, the hunting response may not occur, and the skin may remain cold due to vasoconstriction alone.
6.7 Review Questions
- Compare and contrast hypothermia and hyperthermia.
- State Bergmann’s and Allen’s rules.
- How do the Maasai and Inuit match the predictions based on Bergmann’s and Allen’s rules?
- Explain how sweating cools the body.
- What is the heat index?
- Relate the heat index to evaporative cooling of the body.
- Identify three heat-related illnesses, from least to most serious.
- How does heat acclimatization occur?
- State two major ways the human body can respond to the cold, and give an example of each.
- Explain how and why the hunting response occurs.
- Define basal metabolic rate.
- How does a high-fat diet help prevent hypothermia?
- Explain why frostbite most commonly occurs in the extremities, such as the fingers and toes.
6.7 Explore More
https://www.youtube.com/watch?v=PpHM4DfPZQU
What happens when you get heat stroke? - Douglas J. Casa, TED-Ed, 2014.
https://youtu.be/_Ifq73REJiM
Hailstones' Inupiaq Traditions | Life Below Zero, National Geographic, 2014.
https://www.youtube.com/watch?v=1L7EI0vKVuU
How An Igloo Keeps You Warm, It's Okay To Be Smart, 2017.
https://www.youtube.com/watch?v=fctH_1NuqCQ&t=
Why do we sweat? - John Murnan, TED-Ed, 2018.
https://www.youtube.com/watch?time_continue=44&v=j3sY67aGFXY&feature=emb_logo
Wim Hof Method, Wim Hof, 2011.
Attributions
Figure 6.7.1
- Maasai warrior by Ninaras on Wikimedia Commons is used under a CC BY 4.0 (https://creativecommons.org/licenses/by/4.0/deed.en) license.
- Smiling man from Maasai Mara, Kenya by Sneha on Unsplash is used under the Unsplash License (https://unsplash.com/license).
Figure 6.7.2
- Inuit-Kleidung women by Ansgar Walk on Wikimedia Commons is used under a CC BY-SA 3.0 (https://creativecommons.org/licenses/by-sa/3.0/deed.lv) license.
- Kulusuk, Tunumiit Inuit couple by Arian Zwegers on Wikimedia Commons is used under a CC BY 2.0 (https://creativecommons.org/licenses/by/2.0/deed.en) license.
-
Inuit girls by Susan van Gelder on Flickr is used under a CC BY-NC-SA 2.0 (https://creativecommons.org/licenses/by-nc-sa/2.0/) license.
Figure 6.7.3
Bergmann’s_rule_-_Canis_lupus by Dhaval Vargiya at Yellowstone National Park on Wikimedia Commons is in the public domain (https://en.wikipedia.org/wiki/Public_domain).
Figure 6.7.4
Sweating [photo] by Avi Richards on Unsplash is used under the Unsplash License (https://unsplash.com/license).
Figure 6.7.5
Heat_Index by U.S. National Oceanic and Atmospheric Administration (NOAA) on Wikimedia Commons is in the public domain (https://en.wikipedia.org/wiki/Public_domain).
Figure 6.7.6
Thirsty [photo] by Dylan Alcock on Unsplash is used under the Unsplash License (https://unsplash.com/license).
Figure 6.7.7
Frostbitten_hands by Winky from Oxford, UK on Wikimedia Commons is used under a CC BY 2.0 (https://creativecommons.org/licenses/by/2.0/deed.en) license.
Figure 6.7.8
- Ringed seal preparation by Ansgar Walk on Wikimedia Commons is used under a CC BY-SA 2.5 (https://creativecommons.org/licenses/by-sa/2.5/deed.en) license.
- Butchering a narwhal by Spencer & Carole on Flickr is used under a CC BY-NC-SA 2.0 (https://creativecommons.org/licenses/by-nc-sa/2.0/) license.
- Inuit children playing while the family is on seal hunt, by GRID-Arendal on Flickr is used under a CC BY-NC-SA 2.0 (https://creativecommons.org/licenses/by-nc-sa/2.0/) license.
References
It's Okay To Be Smart. (2017, January 9). How an igloo keeps you warm. YouTube. https://www.youtube.com/watch?v=1L7EI0vKVuU&feature=youtu.be
National Geographic. (2014, April 7). Hailstones' Inupiaq traditions | Life below zero. YouTube. https://www.youtube.com/watch?v=_Ifq73REJiM&feature=youtu.be
TED-Ed. (2014, July 21). What happens when you get heat stroke? - Douglas J. Casa. YouTube. https://www.youtube.com/watch?v=PpHM4DfPZQU&feature=youtu.be
TED-Ed. (2018, May 15). Why do we sweat? - John Murnan. YouTube. https://www.youtube.com/watch?v=fctH_1NuqCQ&feature=youtu.be
Wim Hof. (2011, June 19). Wim Hof Method. YouTube. https://www.youtube.com/watch?v=j3sY67aGFXY&feature=youtu.be
Created by: CK-12/Adapted by Christine Miller
Figure 6.7.1 Men from Maasai Mara, Kenya.
Built for Heat
These tall, slender men live near the equator in Kenya, East Africa — one of the hottest regions of the world. These and the other people of his tribal group, called the Maasai, are among the tallest, most linear people on the planet. Their body build is thought to be an adaptation to their climate, which is hot year-round.
Climate Extremes
Climate refers to the average weather conditions in a region over a long period of time. One of the main determinants of climate is temperature. Both hot and cold temperatures are serious environmental stresses on the human body.
In the cold, there is risk of hypothermia, which is a dangerous decrease in core body temperature. The normal temperature of the human body is 37 degrees C (98.6 degrees F). Hypothermia sets in when body temperature drops to 34.4 degrees C (94 degrees F). If body temperature falls below 29.4 degrees C (85 degrees F), it starts to cool very rapidly because the body’s temperature regulation mechanism starts to fail.
The opposite problem occurs in the heat, where the risk is hyperthermia, which is a dangerous increase in core body temperature. If human body temperature rises above about 40.6 degrees C (105 degrees F), hyperthermia may become life threatening. If a temperature this high persists more than a few days, it generally damages the brain and other internal organs, leading to death.
Human Adaptation to Heat and Cold
Humans are the most widespread species on the planet, and they have lived in extreme climates for tens of thousands of years. As a result, many human populations have had to cope with extreme temperatures for hundreds of generations, which has forced them to develop genetic adaptations to these climate extremes.
The size and proportions of the human body may play an important role in how well an individual is able to handle hot or cold temperatures. In general, people with a tall, slender build, like the Maasai man pictured in Figure 6.7.1, are well adapted to heat, whereas people with a short, stocky build (like the Indigenous North American Inuit pictured in Figure 6.7.2) are well adapted to cold. These relationships between body build and climate were first noticed in other animal species in the 1800s by biologists Carl Bergmann and Joel Allen. These scientists formulated what are now known as Bergmann’s and Allen’s rules.
Figure 6.7.2 Indigenous North American Inuit.
Bergmann’s Rule
Bergmann's rule states that within a broadly distributed taxonomic group, populations or species of larger size are found in colder environments, whereas populations or species of smaller size are found in warmer environments. Bergmann’s rule has been shown to generally apply to widespread species of mammals and birds, although there are also many exceptions to the rule.
What explains Bergmann’s rule? Larger animals have a lower surface area to volume ratio than smaller animals, which is illustrated in Table 6.7.1 for a simple shape, a cube. From the table, you can see how the surface area to volume ratio of a cube decreases dramatically as the size of the cube increases. Because heat is lost through the surface of the body, an animal with a smaller surface area to volume ratio radiates less body heat per unit of mass. The larger body mass also allows the animal to generate more heat. A larger animal has more cells, so it can produce more body heat as a byproduct of cellular metabolism. Both of these factors allow a larger animal to stay warmer in a cold climate.
Table 6.7.1
Relationship of Surface Area to Volume in Cubes of Different Sizes
| Relationship of Surface Area to Volume in Cubes of Different Sizes | |||
| Side of Cube (cm) | Surface Area of Cube (cm2) | Volume of Cube (cm3) | Surface Area:Volume Ratio |
| 2 | 24 | 8 | 3:1 |
| 4 | 96 | 64 | 3:2 |
| 6 | 216 | 216 | 3:3 |
| 12 | 864 | 1728 | 3:6 |
| 20 | 2400 | 8000 | 3:10 |
Warmer climates impose the opposite problem: body heat generated by metabolism needs to be dissipated quickly rather than stored within the body. Smaller animals have a higher surface area to volume ratio that maximizes heat loss through the surface of the body and helps cool the body. With less mass and fewer cells, smaller animals also generate less heat due to cellular metabolism.

Anthropologists have found that many human populations tend to follow Bergmann’s rule. For example, a study of 100 human populations in the 1950s found a strong negative correlation between mean body mass and average yearly temperature. In other words, higher body mass was generally found in colder places, and lower body mass was generally found in hotter places.
There are also exceptions to the rule, in part because we use cultural responses to temper environmental stresses so we do not need to change genetically or physiologically in order to cope. Humans, for example, use clothing and heated buildings to stay warm in cold climates, which tends to counter the effects of natural selection changing human body shape in cold climates.
Allen’s Rule
Allen’s rule is a corollary of Bergmann’s rule. It states that animals living in hotter climates generally have longer extremities (such as limbs, tails, snouts, and ears) than closely related animals living in colder climates. The explanation for Allen’s rule is similar to the rationale behind Bergmann’s rule. Longer extremities maximize an animal’s surface area, allowing greater heat loss through the surface of the body. Therefore, having long extremities is adaptive in hot climates where the main challenge is dissipating body heat.
Anthropologists have noted that, in populations that have lived in tropical regions for long periods of time, the limbs of people tend to be longer in proportion to overall body height. The Maasai man pictured in Figure 6.7.1 is a clear example. His exceptionally long limbs — like those of other members of his population — are optimally proportioned for the hot climate in Kenya. The shorter-limbed body proportions of the Inuit people (Figure 6.7.2) suit them well for their cold climate. Marked differences in limb length have also been observed in related populations that have lived for long periods of time at different altitudes. High altitudes have colder climates than lower altitudes and — consistent with Allen's rule —people tend to have shorter limbs at higher altitudes.
Other Human Responses to Heat
Humans exhibit several other responses to high temperatures that are generally considered either short-term physiological responses or examples of longer-term acclimatization.
Sweating and Humidity

Because humans are basically tropical animals, we generally have an easier time dealing with excessive heat than excessive cold. Evaporation of sweat is the main way we cool the body. The dancer in Figure 6.7.4 is sweating copiously while working out in a hot environment. Why does sweating cool us? When sweat evaporates from the skin, it requires heat. The heat comes from the surface of the body, resulting in evaporative cooling.
How well we can deal with high air temperatures depends in large part on the humidity of the air. We have a harder time losing excess body heat when the humidity is high because our sweat does not evaporate as well as it does when the humidity is low. Instead, the sweat stays on the skin, making us feel clammy and warmer than we would feel if the humidity were lower. If the air is dry, on the other hand, sweat evaporates readily, and we feel more comfortable. For this reason, we are able to tolerate higher temperatures when the humidity is low. This is the basis of the common aphorism, “It’s not the heat, but the humidity.”
The heat index (HI) is a number that combines air temperature and relative humidity to indicate how hot the air feels due to the humidity. The heat index is also called "apparent temperature.” Figure 6.7.5 shows the heat index at different combinations of air temperature and relative humidity. As you can see, when the humidity is very high, even a 90-degree F (32 degrees C) temperature can be very dangerous.
Acclimatization to Heat

If humidity is low, evaporation of sweat can be an effective way to keep the body from overheating. However, the loss of water and salts in sweat can also be dangerous. In very hot conditions, an adult may lose up to four litres of sweat per hour and up to 14 litres per day. Such water losses may cause severe dehydration if the water is not replaced by drinking much more than usual. The loss of salts may also upset the normal salt balance in the body, which can be dangerous. Becoming acclimatized to heat by gradually increasing the exposure time to high temperatures — particularly while exercising or doing physical work — can reduce the risk of these effects.
It may take up to 14 days to attain maximum heat acclimatization. As the body becomes acclimatized, sweat output increases, and sweating begins sooner. The salt content of the sweat also declines, as does the output of urine. These and other physiological changes help the body lose heat through the evaporation of sweat, while maintaining the proper balance of salts and fluids in the body. There may also be increased blood flow to the body surface through the widening of blood vessels near the skin. This is called vasodilation. This brings more heat from the body core to the skin, and from there it may be radiated out into the environment.
Becoming acclimatized to heat allows one to safely perform more exercise or work in the heat. It also helps prevent heat-related illnesses by reducing strain on the body. Heat-related illnesses — from least to most serious — include heat cramps, heat exhaustion, and heat stroke.
- Heat cramps are muscle spasms caused by loss of water and salts. They often follow prolonged sweating brought on by over-exertion in hot weather.
- Heat exhaustion is a condition in which over-heating of the body causes dizziness, headache, profuse sweating, rapid heartbeat. and other symptoms. Without prompt treatment, heat exhaustion can lead to heat stroke.
- Heat stroke is potentially life threatening and a medical emergency. Heat stroke results from prolonged exposure to high temperatures, usually in combination with dehydration. It leads to failure of the body's temperature control system and is diagnosed when the core body temperature exceeds 105 degrees F (40 degrees C). Symptoms may include nausea, seizures, confusion, disorientation, and coma.
Acclimatization to heat, like other types of acclimatization, is a reversible process. Just as quickly as heat acclimatization occurs, the physiological changes fade away in the absence of heat exposure. The body returns to its baseline state within a week or two of no longer exercising or working at high temperatures.
Other Human Responses to Cold
Besides genetic difference in body build, there are two major ways the human body can respond to the cold. One way is by producing more body heat, and the other way is by conserving more body heat. An immediate response to cooling of the body is shivering. This is an involuntary and simultaneous contraction of many tiny muscles in the body. These muscle contractions generate a small amount of heat. Another early response to cold temperature is a narrowing of blood vessels near the skin. This is called vasoconstriction. This helps to shunt blood away from the body surface so more heat is held at the body core. The skin cools down and radiates less heat into the environment.
Hunting Response
At temperatures below freezing, vasoconstriction can be dangerous if it lasts too long. The extremities become too cold because of lack of blood flow, and cold injury (such as frostbite) may occur. Frostbite is tissue destruction that occurs when tissue freezes. You can see a mild-to-moderate case of frostbite of the fingers in Figure 6.7.7. If frostbite is severe, it may lead to gangrene and amputation of the affected extremities.

The body counters the possibility of cold injury with a reaction called the hunting response. This is a process of alternating vasoconstriction and vasodilation in extremities exposed to cold. About five to ten minutes after the start of cold exposure, the blood vessels in the extremities suddenly dilate, which increases blood flow and subsequently the temperature of the extremities. This is soon followed by another phase of vasoconstriction, and then the process repeats.
The hunting response occurs in most people, but several factors may influence the strength of the response. People who live or work regularly in cold environments show an increased hunting response. Through acclimatization, however, tropical residents can develop an increased response, which is indistinguishable from that of arctic residents. Genetic factors may play a role in the hunting response, but this is uncertain because it is difficult to differentiate between adaptation and acclimatization.
Persistent Vasoconstriction
Where temperatures rarely fall below freezing but are repeatedly very chilly, the hunting response may not occur. Instead, vasoconstriction may persist to keep heat within the body at the expense of cooling the skin. As long as the temperature stays above freezing, cold injury (such as frostbite) will not occur. This type of response has been shown to occur in indigenous desert dwellers in southern Africa and Australia, where the temperature is hot during the day and very cold at night. People in these populations also tend to deposit fat around the organs in their chest and abdomen. The fat serves as insulation, protecting vital structures from the cold.
High-Fat Diet
Besides shivering, another way to increase body heat is to raise the basal metabolic rate. The basal metabolic rate (BMR) is the amount of energy that a person needs to keep the body functioning at rest. The higher the BMR, the more heat the body generates, even without exercise or physical labor. The BMR can be increased by consuming large quantities of high-calorie fatty foods. People living in very cold subarctic regions, including the Inuit, traditionally ate whale and seal blubber and other high-fat foods, which helped them maintain a high BMR and stay warm.
Figure 6.7.8 Whale and seal blubber (mainly on abundant ring seals) is an important part of the traditional Inuit diet.
Feature: Human Biology in the News
Too many news stories report young children being seriously injured or dying from heat stroke in hot vehicles. On average, 38 children die in hot vehicles each year from heat-related deaths after being trapped inside. Most often, this happens by accident, when a parent or caregiver unknowingly leaves a sleeping child in a car. In other cases, children get into cars on their own, and then cannot get out again.
A child’s thermoregulatory system is not as efficient as that of an adult, and a child’s body temperature may increase as much as five times faster. This makes children prime candidates for heat stroke. A motor vehicle is also easily heated by direct sun. The windows of the vehicle allow solar radiation to pass through and heat up objects inside. A dark-coloured dashboard or seat may quickly reach a temperature of more than 180 degrees F (82 degrees C)! These hot surfaces can just as quickly heat the adjacent air, rapidly increasing the temperature of the air trapped inside the vehicle.
Here are several simple tips that parents and caregivers can follow to prevent heat stroke tragedies:
- Never leave children alone in or around cars — not even for a minute.
- Always open the back door and check the back seat before leaving your vehicle to be sure no child has been left behind.
- Put something you will need, such as your cell phone or handbag, in the back seat so you will have to open the back door to retrieve it whenever you park the car.
- Keep a large stuffed animal in the child's car seat, and when the child is placed in the car seat, put the stuffed animal in the front passenger seat as a visual reminder that the child is in the back.
- Make sure you have a strict policy in place with everyone involved in the care of your child that you should always be called whenever your child does not show up at daycare or school as scheduled.
- Keep vehicles locked at all times, even in driveways and garages. Ask home visitors, child care providers, and neighbors to do the same.
- Keep car keys and remote vehicle openers out of reach of children.
- If a child is missing, immediately check the inside passenger compartments and trunks of all vehicles in the area. Check vehicles even if they are locked, because a child may lock a vehicle after entering and not be able to unlock it again to get out.
- If you see a child alone in a vehicle, call 911 immediately. If the child seems hot or sick, get them out of the vehicle as quickly as possible.
- Pay for gas at the pump and use drive-throughs at the bank, pharmacy, or wherever else they are available.
6.7 Summary
- Both hot and cold temperatures are serious environmental stresses on the human body. In the cold, there is risk of hypothermia, which is a dangerous decrease in core body temperature. In the heat, there is risk of hyperthermia, which is a dangerous increase in core body temperature.
- According to Bergmann’s rule, body size tends to be negatively correlated with temperature, because larger body size increases heat production and decreases heat loss. The opposite holds true for small body size. Bergmann’s rule applies to many human populations that are hot- or cold-adapted.
- According to Allen’s rule, the length of body extremities is positively correlated with temperature, because longer extremities are better at dissipating excess body heat. The opposite applies to shorter extremities. Allen’s rule applies to relative limb lengths in many human populations that have adapted to heat or cold.
- Sweating is the primary way that humans lose body heat. The evaporation of sweat from the skin cools the body. This only works well when the relative humidity is fairly low. At high relative humidity, sweat does not readily evaporate to cool us down. The heat index (HI) indicates how hot it feels due to the humidity.
- Gradually working longer and harder in the heat can bring about heat acclimatization, in which the body has improved responses to heat stress. For example, sweating starts earlier, sweat contains less salt, and vasodilation brings heat to the surface to help cool the body. Full acclimatization takes up to 14 days and reverses just as quickly when the heat stress is removed.
- The human body can respond to cold by producing more heat (by shivering or increasing the basal metabolic rate) or by conserving heat (by vasoconstriction at the body surface or a layer of fat-insulating internal organs).
- At temperatures below freezing, the hunting response occurs to prevent cold injury, such as frostbite. This is a process of alternating vasoconstriction and vasodilation in extremities that are exposed to dangerous cold. Where temperatures are repeatedly cold but rarely below freezing, the hunting response may not occur, and the skin may remain cold due to vasoconstriction alone.
6.7 Review Questions
- Compare and contrast hypothermia and hyperthermia.
- State Bergmann’s and Allen’s rules.
- How do the Maasai and Inuit match the predictions based on Bergmann’s and Allen’s rules?
- Explain how sweating cools the body.
- What is the heat index?
- Relate the heat index to evaporative cooling of the body.
- Identify three heat-related illnesses, from least to most serious.
- How does heat acclimatization occur?
- State two major ways the human body can respond to the cold, and give an example of each.
- Explain how and why the hunting response occurs.
- Define basal metabolic rate.
- How does a high-fat diet help prevent hypothermia?
- Explain why frostbite most commonly occurs in the extremities, such as the fingers and toes.
6.7 Explore More
https://www.youtube.com/watch?v=PpHM4DfPZQU
What happens when you get heat stroke? - Douglas J. Casa, TED-Ed, 2014.
https://youtu.be/_Ifq73REJiM
Hailstones' Inupiaq Traditions | Life Below Zero, National Geographic, 2014.
https://www.youtube.com/watch?v=1L7EI0vKVuU
How An Igloo Keeps You Warm, It's Okay To Be Smart, 2017.
https://www.youtube.com/watch?v=fctH_1NuqCQ&t=
Why do we sweat? - John Murnan, TED-Ed, 2018.
https://www.youtube.com/watch?time_continue=44&v=j3sY67aGFXY&feature=emb_logo
Wim Hof Method, Wim Hof, 2011.
Attributions
Figure 6.7.1
- Maasai warrior by Ninaras on Wikimedia Commons is used under a CC BY 4.0 (https://creativecommons.org/licenses/by/4.0/deed.en) license.
- Smiling man from Maasai Mara, Kenya by Sneha on Unsplash is used under the Unsplash License (https://unsplash.com/license).
Figure 6.7.2
- Inuit-Kleidung women by Ansgar Walk on Wikimedia Commons is used under a CC BY-SA 3.0 (https://creativecommons.org/licenses/by-sa/3.0/deed.lv) license.
- Kulusuk, Tunumiit Inuit couple by Arian Zwegers on Wikimedia Commons is used under a CC BY 2.0 (https://creativecommons.org/licenses/by/2.0/deed.en) license.
-
Inuit girls by Susan van Gelder on Flickr is used under a CC BY-NC-SA 2.0 (https://creativecommons.org/licenses/by-nc-sa/2.0/) license.
Figure 6.7.3
Bergmann’s_rule_-_Canis_lupus by Dhaval Vargiya at Yellowstone National Park on Wikimedia Commons is in the public domain (https://en.wikipedia.org/wiki/Public_domain).
Figure 6.7.4
Sweating [photo] by Avi Richards on Unsplash is used under the Unsplash License (https://unsplash.com/license).
Figure 6.7.5
Heat_Index by U.S. National Oceanic and Atmospheric Administration (NOAA) on Wikimedia Commons is in the public domain (https://en.wikipedia.org/wiki/Public_domain).
Figure 6.7.6
Thirsty [photo] by Dylan Alcock on Unsplash is used under the Unsplash License (https://unsplash.com/license).
Figure 6.7.7
Frostbitten_hands by Winky from Oxford, UK on Wikimedia Commons is used under a CC BY 2.0 (https://creativecommons.org/licenses/by/2.0/deed.en) license.
Figure 6.7.8
- Ringed seal preparation by Ansgar Walk on Wikimedia Commons is used under a CC BY-SA 2.5 (https://creativecommons.org/licenses/by-sa/2.5/deed.en) license.
- Butchering a narwhal by Spencer & Carole on Flickr is used under a CC BY-NC-SA 2.0 (https://creativecommons.org/licenses/by-nc-sa/2.0/) license.
- Inuit children playing while the family is on seal hunt, by GRID-Arendal on Flickr is used under a CC BY-NC-SA 2.0 (https://creativecommons.org/licenses/by-nc-sa/2.0/) license.
References
It's Okay To Be Smart. (2017, January 9). How an igloo keeps you warm. YouTube. https://www.youtube.com/watch?v=1L7EI0vKVuU&feature=youtu.be
National Geographic. (2014, April 7). Hailstones' Inupiaq traditions | Life below zero. YouTube. https://www.youtube.com/watch?v=_Ifq73REJiM&feature=youtu.be
TED-Ed. (2014, July 21). What happens when you get heat stroke? - Douglas J. Casa. YouTube. https://www.youtube.com/watch?v=PpHM4DfPZQU&feature=youtu.be
TED-Ed. (2018, May 15). Why do we sweat? - John Murnan. YouTube. https://www.youtube.com/watch?v=fctH_1NuqCQ&feature=youtu.be
Wim Hof. (2011, June 19). Wim Hof Method. YouTube. https://www.youtube.com/watch?v=j3sY67aGFXY&feature=youtu.be
Image shows a photograph of a young child drinking milk from a cup. He has milk on his upper lip. It is adorable.
Created by: CK-12/Adapted by Christine Miller

Polly Who?
Each hand in the Figure 5.15.1 photo has an extra pinky finger. This is a condition called polydactyly, which literally means "many digits." People with polydactyly may have extra fingers and/or toes, and the condition may affect just one hand or foot, or both hands and feet. Polydactyly is often genetic in origin and may be part of a genetic disorder associated with other abnormalities.
What Are Genetic Disorders?
Genetic disorders are diseases, syndromes, or other abnormal conditions caused by mutations in one or more genes, or by chromosomal alterations. Genetic disorders are typically present at birth, but they should not be confused with congenital disorders, a category that includes any disorder present at birth, regardless of cause. Some congenital disorders are not caused by genetic mutations or chromosomal alterations. Instead, they are caused by problems that arise during embryonic or fetal development, or during the process of birth. An example of a nongenetic congenital disorder is fetal alcohol syndrome. This is a collection of birth defects, including facial anomalies and intellectual disability, caused by maternal alcohol consumption during pregnancy.
Genetic Disorders Caused by Mutations
Table 5.15.1 lists several genetic disorders caused by mutations in just one gene. Some of the disorders are caused by mutations in autosomal genes, others by mutations in X-linked genes. Which disorders would you expect to be more common in males than females?
| Genetic Disorder | Direct Effect of Mutation | Signs and Symptoms of the Disorder | Mode of Inheritance |
|---|---|---|---|
| Marfan syndrome | Defective protein in connective tissue | Heart and bone defects and unusually long, slender limbs and fingers | Autosomal dominant |
| Sickle cell anemia | Abnormal hemoglobin protein in red blood cells | Sickle-shaped red blood cells that clog tiny blood vessels, causing pain and damaging organs and joints | Autosomal recessive |
| Hypophosphatemic (Vitamin D-resistant) rickets | Lack of a substance needed for bones to absorb minerals | Soft bones that easily become deformed, leading to bowed legs and other skeletal deformities | X-linked dominant |
| Hemophilia A | Reduced activity of a protein needed for blood clotting | Internal and external bleeding that occurs easily and is difficult to control | X-linked recessive |
Very few genetic disorders are controlled by dominant mutant [pHypophosphatemicb_glossary id="2119"]alleles[/pb_glossary]. A dominant allele is expressed in every individual who inherits even one copy of it. If it causes a serious disorder, affected people may die young and fail to reproduce. Therefore, the mutant dominant allele is likely to die out of a population.
A recessive mutant allele — such as the allele that causes sickle cell anemia or cystic fibrosis — is not expressed in people who inherit just one copy of it. These people are called carriers. They do not have the disorder themselves, but they carry the mutant allele and their offspring can inherit it. Thus, the allele is likely to pass on to the next generation, rather than die out.
Genetic Disorders Caused by Chromosomal Alterations
Mistakes may occur during meiosis that result in nondisjunction. This is the failure of replicated chromosomes to separate properly during meiosis. Some of the resulting gametes will be missing all or part of a chromosome, while others will have an extra copy of all or part of the chromosome. If such gametes are fertilized and form zygotes, they usually do not survive. If they do survive, the individuals are likely to have serious genetic disorders.
Table 5.15.2 lists several genetic disorders that are caused by abnormal numbers of chromosomes. Most chromosomal disorders involve the X chromosome. The X and Y chromosomes are the only chromosome pair in which the two chromosomes are very different in size. This explains why nondisjunction tends to occur more frequently in sex chromosomes than in autosomes.
| Genetic Disorder | Genotype | Phenotypic Effects |
|---|---|---|
| Down syndrome | Extra copy (complete or partial) of chromosome 21 (see Figure 5.15.3) | Developmental delays, distinctive facial appearance, and other abnormalities (see Figure 5.15.2) |
| Turner syndrome | One X chromosome but no other sex chromosome (XO) | Female with short height and infertility(inability to reproduce) |
| Triple X syndrome | Three X chromosomes (XXX) | Female with mild developmental delays and menstrual irregularities |
| Klinefelter syndrome | One Y chromosome and two or more X chromosomes (XXY, XXXY) | Male with problems in sexual development and reduced levels of the male hormone testosterone |
 |
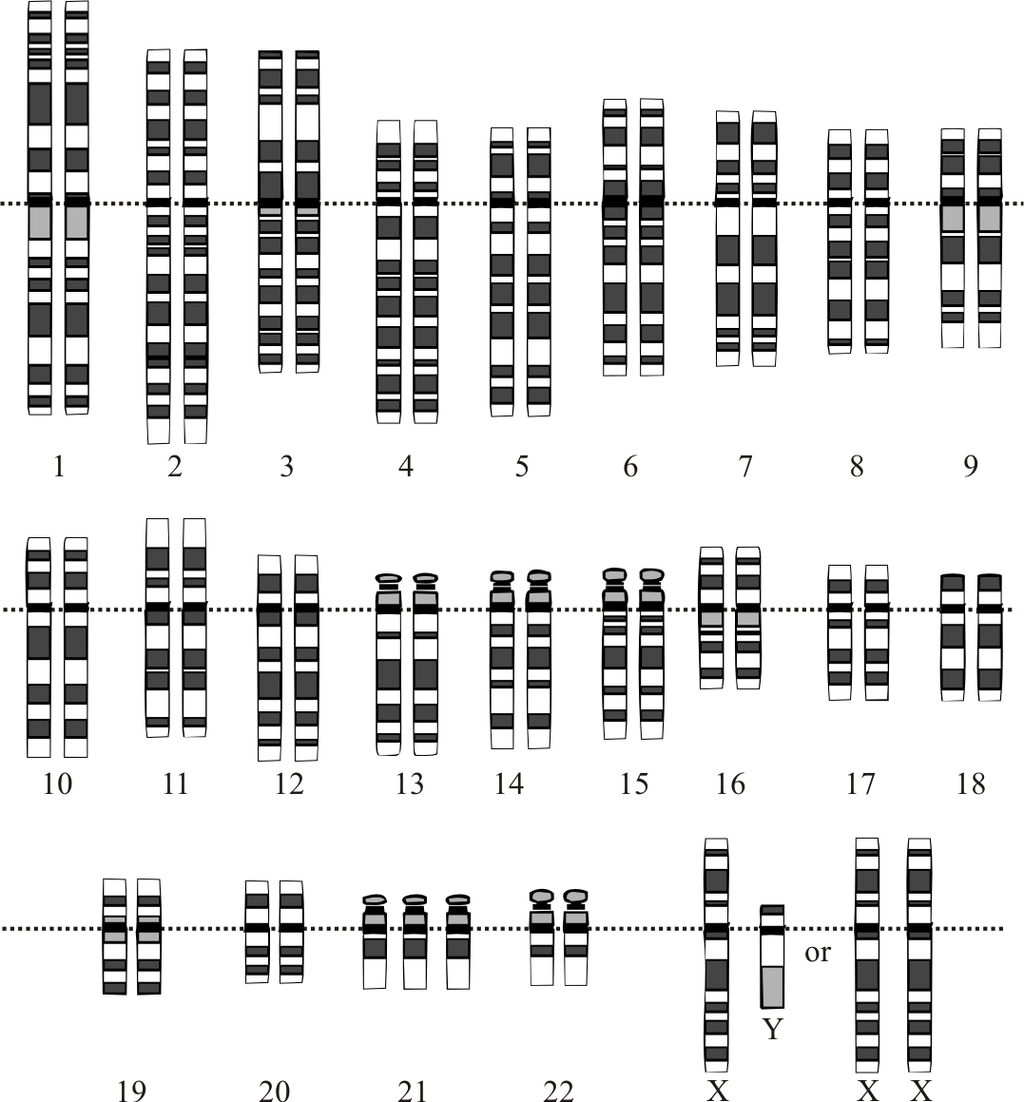 |
A karyotype is a picture of a cell's chromosomes. In Figure 5.15.3, note the extra chromosome 21. In Figure 5.15.2, a young man with Down syndrome exhibits the characteristic facial appearance.
Diagnosing and Treating Genetic Disorders
A genetic disorder that is caused by a mutation can be inherited. Therefore, people with a genetic disorder in their family may be concerned about having children with the disorder. A genetic counselor can help them understand the risks of their children being affected. If they decide to have children, they may be advised to have prenatal (“before birth”) testing to see if the fetus has any genetic abnormalities. One method of prenatal testing is amniocentesis. In this procedure, a few fetal cells are extracted from the fluid surrounding the fetus in utero, and the fetal chromosomes are examined. Down syndrome and other chromosomal alterations can be detected in this way.

The symptoms of genetic disorders can sometimes be treated or prevented. In the genetic disorder called phenylketonuria (PKU), for example, the amino acid phenylalanine builds up in the body to harmful levels. PKU is caused by a mutation in a gene that normally codes for an enzyme needed to break down phenylalanine. When a person with PKU consumes foods high in phenylalanine (including many high-protein foods), the buildup of PKU can lead to serious health problems. In infants and young children, the build-up of phenylalanine can cause intellectual disability and delayed development, along with other serious problems. All babies in Canada and the United States and many other countries are screened for PKU soon after birth. As shown in Figure 5.15.3, the PKU test involves collecting a small amount of blood from the infant, typically from the heel using a small lancet. The blood is collected on a special type of filter paper and then brought to a laboratory for analysis. If PKU is diagnosed, the infant can be fed a low-phenylalanine diet, which prevents the buildup of phenylalanine and the health problems associated with it, including intellectual disability. As long as a low-phenylalanine diet is followed throughout life, most symptoms of the disorder can be prevented.
Curing Genetic Disorders
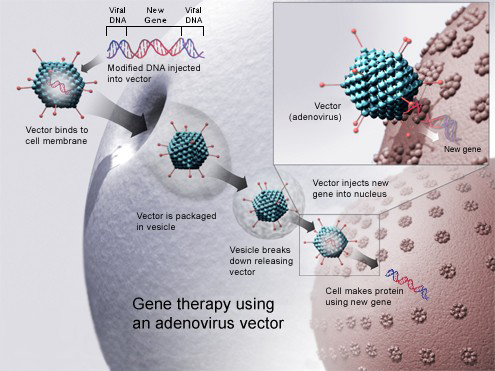
Cures for genetic disorders are still in the early stages of development. One potential cure is gene therapy. Gene therapy is an experimental technique that uses genes to treat or prevent disease. In gene therapy, normal genes are introduced into cells to compensate for abnormal genes. If a mutated gene causes a necessary protein to be nonfunctional or missing, gene therapy may be able to introduce a normal copy of the gene to produce the needed functional protein.
A gene inserted directly into a cell usually does not function, so a carrier called a vector is genetically engineered to deliver the gene (see Figure 5.15.4 illustration). Certain viruses, such as adenoviruses, are often used as vectors. They can deliver the new gene by infecting cells. The viruses are modified so they do not cause disease when used in people. If the treatment is successful, the new gene delivered by the vector will allow the synthesis of a functioning protein. Researchers still must overcome many technical challenges before gene therapy will be a practical approach to curing genetic disorders.
Feature: Human Biology in the News

Down syndrome is the most common genetic cause of intellectual disability. It occurs in about one in every 700 live births, and it currently affects nearly half a million Americans. Until recently, scientists thought that the changes leading to intellectual disability in people with Down syndrome all happen before birth.
Even more recently, researchers discovered a genetic abnormality that affects brain development in people with Down syndrome throughout childhood and into adulthood. The newly discovered genetic abnormality changes communication between nerve cells in the brain, resulting in slower transmission of nerve impulses. This finding may eventually allow the development of strategies to promote brain functioning in Down syndrome patients, and it may also be applicable to other development disabilities, such as autism. The results of this promising study were published in the March 16, 2016 issue of the scientific journal Neuron.
5.15 Summary
- Genetic disorders are diseases, syndromes, or other abnormal conditions that are caused by mutations in one or more genes, or by chromosomal alterations.
- Examples of genetic disorders caused by single-gene mutations include Marfan syndrome (autosomal dominant), sickle cell anemia (autosomal recessive), vitamin D-resistant rickets (X-linked dominant), and hemophilia A (X-linked recessive). Very few genetic disorders are caused by dominant mutations because these alleles are less likely to be passed on to successive generations.
- Nondisjunction is the failure of replicated chromosomes to separate properly during meiosis. This may result in genetic disorders caused by abnormal numbers of chromosomes. An example is Down syndrome, in which the individual inherits an extra copy of chromosome 21. Most chromosomal disorders involve the X chromosome. An example is Klinefelter's syndrome (XXY, XXXY).
- Prenatal genetic testing (by amniocentesis, for example) can detect chromosomal alterations in utero. The symptoms of some genetic disorders can be treated or prevented. For example, symptoms of phenylketonuria (PKU) can be prevented by following a low-phenylalanine diet throughout life.
- Cures for genetic disorders are still in the early stages of development. One potential cure is gene therapy, in which normal genes are introduced into cells by a vector such as a virus to compensate for mutated genes.
5.15 Review Questions
- Define genetic disorder.
- Identify three genetic disorders caused by mutations in a single gene.
- Why are single-gene genetic disorders more commonly controlled by recessive than dominant mutant alleles?
- What is nondisjunction? Why can it cause genetic disorders?
- Explain why genetic disorders caused by abnormal numbers of chromosomes most often involve the X chromosome.
- How is Down syndrome detected in utero?
- Use the example of PKU to illustrate how the symptoms of a genetic disorder can sometimes be prevented.
- Explain how gene therapy works.
- Compare and contrast genetic disorders and congenital disorders.
- Explain why parents that do not have Down syndrome can have a child with Down syndrome.
- Hemophilia A and Turner’s syndrome both involve problems with the X chromosome. In terms of how the X chromosome is affected, what is the major difference between these two types of disorders?
- Can you be a carrier of Marfan syndrome and not have the disorder? Explain your answer.
5.15 Explore More
https://www.youtube.com/watch?v=6tw_JVz_IEc
How CRISPR lets you edit DNA - Andrea M. Henle, TED-Ed, 2019.
https://youtu.be/1BXYSGepx7Q
What you need to know about CRISPR | Ellen Jorgensen, TED, 2016.
https://youtu.be/nOHbn8Q1fBM
The ethical dilemma of designer babies | Paul Knoepfler, TED, 2017.
Attributions
Figure 5.15.1
Polydactyly_ECS by Baujat G, Le Merrer M. on Wikimedia Commons is used under a CC BY 2.0 (https://creativecommons.org/licenses/by/2.0) license.
Figure 5.15.2
Downs/ All the Family [photo] by Nathan Anderson on Unsplash is used under the Unsplash License (https://unsplash.com/license).
Figure 5.15.3
Phenylketonuria_testing by U.S. Air Force photo/Staff Sgt Eric T. Sheler in the US Air Force National Archives on Wikimedia Commons is in the public domain (https://en.wikipedia.org/wiki/Public_domain).
Figure 5.15.4
Gene_therapy by National Institutes of Health (NIH) on Wikimedia Commons is in the public domain (https://en.wikipedia.org/wiki/Public_domain).
Figure 5.15.5
Boy_with_Down_Syndrome by Vanellus Foto on Wikimedia Commons is used under a CC BY-SA 3.0 (https://creativecommons.org/licenses/by-sa/3.0/deed.en) license.
References
Baujat, G., Le Merrer, M. (2007, January 23). Ellis-Van Creveld syndrome. Orphanet Journal of Rare Diseases, 2, 27. https://doi.org/10.1186/1750-1172-2-27
Hecht, M. (2019, June 26). What is polydactyly? [online article]. Healthline. https://www.healthline.com/health/polydactyly
Genetic and Rare Diseases Information Center (GARD). (2016). Hypophosphatemic rickets (previously called vitamin D-resistant rickets) [online article]. NIH. https://rarediseases.info.nih.gov/diseases/6735/hypophosphatemic-rickets [last updated 7/1/2020]
Mayo Clinic Staff. (n.d.). Cystic fibrosis [online article]. MayoClinic.org. https://www.mayoclinic.org/diseases-conditions/cystic-fibrosis/symptoms-causes/syc-20353700
Mayo Clinic Staff. (n.d.). Down syndrome [online article]. MayoClinic.org. https://www.mayoclinic.org/diseases-conditions/down-syndrome/diagnosis-treatment/drc-20355983
Mayo Clinic Staff. (n.d.). Hemophilia [online article]. MayoClinic.org. https://www.mayoclinic.org/diseases-conditions/hemophilia/symptoms-causes/syc-20373327
Mayo Clinic Staff. (n.d.). Klinefelter syndrome [online article]. MayoClinic.org. https://www.mayoclinic.org/diseases-conditions/klinefelter-syndrome/symptoms-causes/syc-20353949
Mayo Clinic Staff. (n.d.). Marfan syndrome [online article]. MayoClinic.org. https://www.mayoclinic.org/diseases-conditions/marfan-syndrome/symptoms-causes/syc-20350782
Mayo Clinic Staff. (n.d.). Phenylketonuria (PKU) [online article]. MayoClinic.org. https://www.mayoclinic.org/diseases-conditions/phenylketonuria/symptoms-causes/syc-20376302
Mayo Clinic Staff. (n.d.). Sickle cell anemia [online article]. MayoClinic.org. https://www.mayoclinic.org/diseases-conditions/sickle-cell-anemia/symptoms-causes/syc-20355876
Mayo Clinic Staff. (n.d.). Turner syndrome [online article]. MayoClinic.org. https://www.mayoclinic.org/diseases-conditions/turner-syndrome/symptoms-causes/syc-20360782
Mayo Clinic Staff. (n.d.). Triple X syndrome [online article]. MayoClinic.org. https://www.mayoclinic.org/diseases-conditions/triple-x-syndrome/symptoms-causes/syc-20350977
National Center on Birth Defects and Developmental Disabilities. (2020). Fetal alcohol spectrum disorders (FASDs): Basics about FASDs [webpage]. Centers for Disease Control and Prevention (CDC). https://www.cdc.gov/ncbddd/fasd/facts.html
TED-Ed. (2019, January 24). How CRISPR lets you edit DNA - Andrea M. Henle. YouTube. https://www.youtube.com/watch?v=6tw_JVz_IEc
TED. (2016, October 24). What you need to know about CRISPR | Ellen Jorgensen. YouTube. https://www.youtube.com/watch?v=1BXYSGepx7Q&feature=youtu.be
TED. (2017, February 10). The ethical dilemma of designer babies | Paul Knoepfler. YouTube. https://www.youtube.com/watch?v=nOHbn8Q1fBM&t=3s
A group of diseases involving abnormal cell growth with the potential to invade or spread to other parts of the body.
A condition in which you don't have enough healthy red blood cells to carry adequate oxygen to the body's tissues resulting in symptoms including weakness and fatigue.
The image shows a diagram of lactose conversion to galactose and glucose by the help of the enzyme lactase.
Image shows a worldwide map of lactose intolerance. In east asia, south africa and southern south america, lactose intolerance rates are highest (80-100%). In Northern Asia, Europe, and North America, lactose intolerance rates are the loweest (0-40%)

Got Lactase?
Do you remember the American “got milk?” slogan from the 1990s? It was used in advertisements for milk in which celebrities were pictured wearing milk “mustaches.” While the purpose of the “got milk?” ads was to sell more milk, there is no denying that drinking milk can actually be good for one’s health. Milk is naturally high in protein and minerals. It can also be low in fat or even fat-free if treated to remove the lipids that naturally occur in milk. However, before you reach for a tall, cold glass of milk, you might want to ask yourself another question: “got lactase?”
Adaptation to Lactose
Do you drink milk? Or do you avoid drinking milk and consuming milk products because they cause you discomfort? If the latter is the case, then you may have trouble digesting milk.
Milk, Lactose, and Lactase
Milk naturally contains more than just proteins and lipids — it also contains carbohydrates. Specifically, milk contains the sugar lactose, which is a disaccharide (two-sugar) compound that consists of one molecule each of galactose and glucose, as shown in the structural formula below (Figure 6.8.2). Lactose makes up between two and eight per cent of milk by weight. The exact amount varies both within and between species.
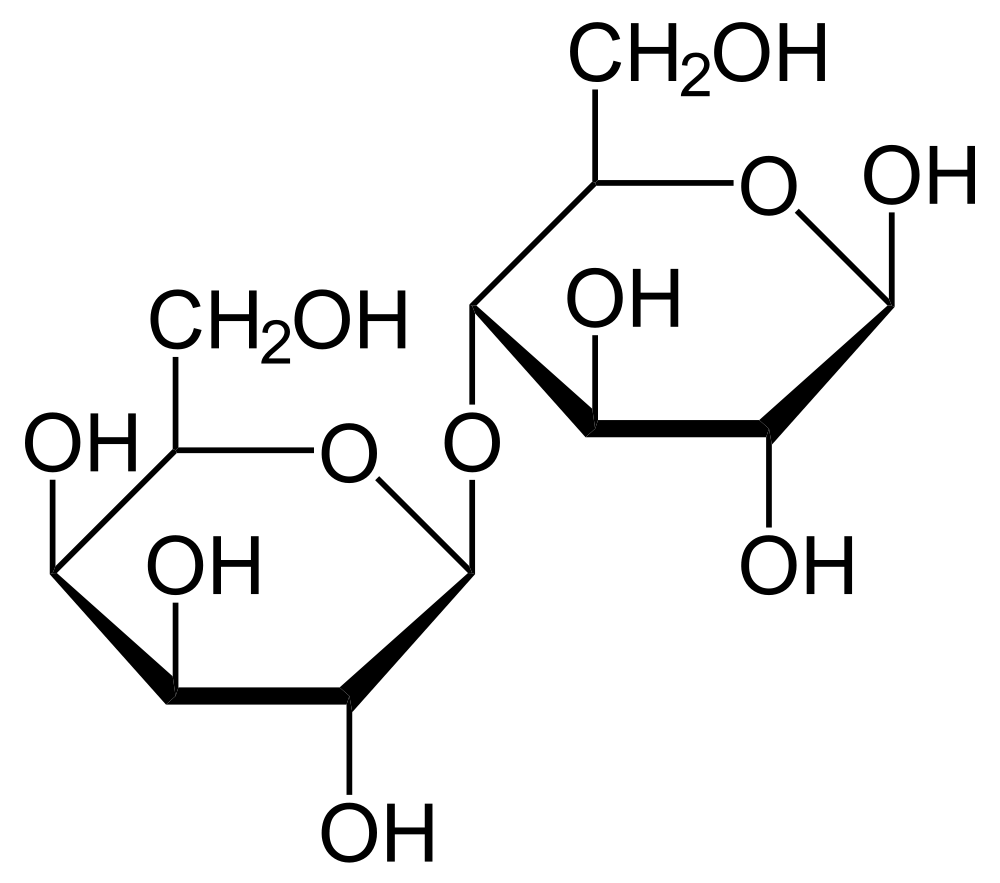
Lactose in milk must be broken down into its two component sugars to be absorbed by the small intestine. The enzyme lactase is needed for this process, as shown in Figure 6.8.3. Human infants are almost always born with the ability to synthesize lactase. This allows them to readily digest the lactose in their mother’s milk (or infant formula). In the majority of children, however, lactase synthesis begins to decline at about two years of age, and less and less lactase is produced throughout childhood.
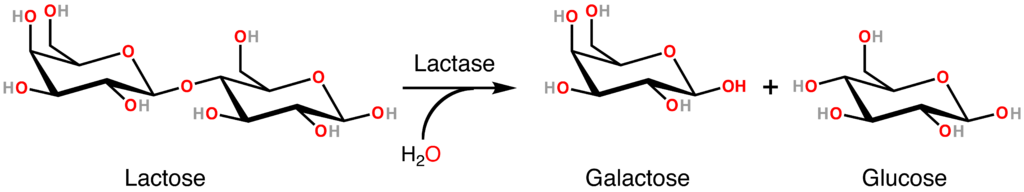
Lactose Intolerance
Lactose intolerance is the inability of older children and adults to digest lactose in milk. People who are lactose intolerant may be able to drink small quantities of milk without any problems, but if they try to consume larger amounts, they are likely to suffer adverse effects. For example, they may have abdominal bloating and cramping, flatulence (gas), diarrhea, nausea, and vomiting. The symptoms may occur from 30 minutes to two hours after milk is consumed, and they're generally worse when the quantity of milk consumed is greater. The symptoms result from the small intestine's inability to digest and absorb lactose, so the lactose is passed on to the large intestine, where normal intestinal bacteria start breaking it down through the process of fermentation. This process releases gas and causes the other symptoms of lactose intolerance.
Lactose intolerance is actually the original and normal condition of the human species, as well as all other mammalian species. Early humans were hunter-gatherers that subsisted on wild plant and animal foods. The animal foods may have included meat and eggs, but did not include milk because animals had not been domesticated. Therefore, beyond the weaning period, milk was not available for people to drink in early human populations. It makes good biological sense to stop synthesizing an enzyme that the body does not need. After a young child is weaned, it is a waste of materials and energy to keep producing lactase when milk is no longer likely to be consumed.
Overall, an estimated 60 per cent of the world’s adult human population is thought to be lactose intolerant today. You can see the geographic distribution of modern human lactose intolerance on the map in Figure 6.8.4. Lactose intolerance (dark blue) approaches 100 per cent in populations throughout southern South America, southern Africa, and East and Southeast Asia.
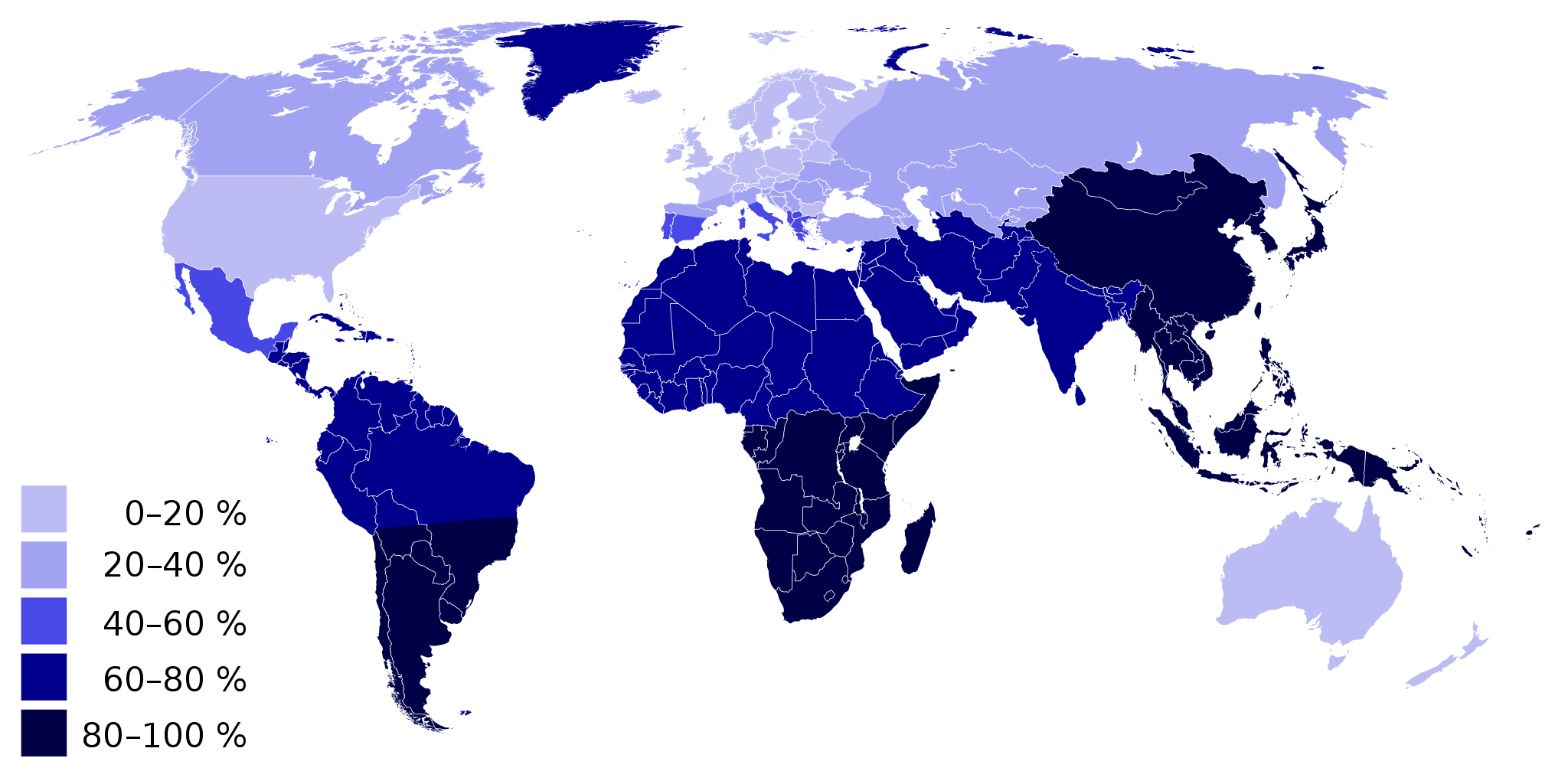
Lactose intolerance is not considered a medical problem, because its symptoms can be avoided by avoiding milk or milk products. Dietary control of lactose intolerance may be a matter of trial and error, however, because different people may be able to consume different quantities of milk or milk products before symptoms occur. If you are lactose intolerant, be aware that low-fat and fat-free milk may contain somewhat more lactose than full-fat milk because the former often have added milk solids that are relatively high in lactose.
Lactase Persistence
Lactase persistence is the opposite of lactose intolerance. People who are lactase persistent continue to produce the enzyme lactase beyond infancy and generally throughout life. As a consequence they are able to digest lactose and drink milk at older ages without adverse effects. The map in Figure 6.8.4 can also be read to show where lactase persistence occurs today. Populations with a low percentage of lactose intolerance (including most North Americans and Western and Northern Europeans) have high percentages of lactase-persistent people.
Lactase persistence is a uniquely human trait that is not found in any other mammalian species. Why did lactase persistence evolve in humans? When some human populations began domesticating and keeping herds of animals, animal milk became a potential source of food. Animals such as cows, sheep, goats, camels, and even reindeer (see Figure 6.8.5) can be kept for their milk. These animal milks also contain lactose, so natural selection would be strong for any individuals who kept producing lactase beyond infancy and could make use of this nutritious food. Eventually, the trait of lactase persistence would increase in frequency and come to be the predominant trait in dairying populations.

It is likely that lactase persistence occurs as a result of both genes and environment. Some people inherit genes that help them keep producing lactase after infancy. Geneticists think that several different mutations for lactase persistence arose independently in different populations within the last ten thousand years. Part of lactase persistence may be due to continued exposure to milk in the childhood and adulthood diet. In other words, a person may be genetically predisposed to synthesize lactase at older ages because of a mutation, but they may need the continued stimulation of milk drinking to keep producing lactase.
Thrifty Gene or Drifty Gene?
Besides variation in lactase persistence, human populations may vary in how efficiently they use calories in the foods they consume. People in some populations seem able to get by on quantities of food that would be inadequate for others, so they tend to gain weight easily. What explains these differences in people?
Thrifty Gene Hypothesis
In 1962, human geneticist James Neel proposed the thrifty gene hypothesis. According to this hypothesis, so-called “thrifty genes” evolved in some human populations because they allowed people to get by on fewer calories and store the rest as body fat when food was plentiful. According to Neel’s hypothesis, thrifty genes would have increased in frequency through natural selection, because they would help people survive during times of famine. People with the genes would be fatter and able to rely on their stored body fat for calories when food was scarce.
Such thrifty genes would have been advantageous in early human populations of hunter-gatherers if food scarcity was a recurrent stress. However, in modern times, when most people have access to enough food year-round, thrifty genes would no longer be advantageous. In fact, under conditions of plentiful food, having thrifty genes would predispose people to gain weight and develop obesity. They would also tend to develop the chronic diseases associated with obesity, particularly type II diabetes. Diabetes mellitus is a disease that occurs when there are problems with the pancreatic hormone insulin, which normally helps cells take up glucose from the blood and controls blood glucose levels. In type II diabetes, body cells become relatively resistant to insulin, leading to high blood glucose. This causes symptoms like excessive thirst and urination. Without treatment, diabetes can lead to serious consequences, such as blindness and kidney failure.
Neel proposed his thrifty gene hypothesis not on the basis of genetic evidence for thrifty genes, but as a possible answer to the mystery of why genes that seem to promote diabetes have not been naturally selected out of some populations. The mystery arose from observations that certain populations — such as South Pacific Islanders, sub-Saharan Africans, and southwestern Native Americans — developed high levels of obesity and diabetes after they abandoned traditional diets and adopted Western diets.
Assessing the Thrifty Gene Hypothesis
One of the assumptions underlying the thrifty gene hypothesis is that human populations that recently developed high rates of obesity and diabetes after Western contact had a long history of recurrent famine. Anthropological evidence contradicts this assumption for at least some of the populations in question. South Pacific Islanders, for example, have long lived in a “land of plenty,” with lush tropical forests year-round on islands surrounded by warm waters full of fish. Another assumption underlying the thrifty gene hypothesis is that hunter-gatherer people became significantly fatter during periods of plenty. Again, there is little or no evidence that hunter-gatherers traditionally deposited large fat stores when food was readily available.
Some geneticists have searched directly for so-called thrifty genes. Studies have revealed many genes with small effects associated with obesity or diabetes. However, these genes can explain only a few percentage points of the total population variation in obesity or diabetes.
The Drifty Gene and Other Hypotheses
Given the lack of evidence for the thrifty gene hypothesis, several researchers have suggested alternative hypotheses to explain population variation in obesity and diabetes. One hypothesis posits that susceptibility to obesity and diabetes may be a side effect of heat adaptation. According to this idea, some populations evolved lower metabolic rates as an adaptation to heat stress, because lower metabolic rates reduced the amount of heat that the body produced. The lower metabolic rates also predisposed people to gain excess weight and develop obesity and diabetes.
A thrifty phenotype hypothesis has also been proposed. This hypothesis suggests that individuals who have inadequate nutrition during fetal development might develop an insulin-resistant phenotype. The insulin-resistant phenotype would supposedly prepare these individuals for a life of famine, based on the environment within the womb. In a famine-free environment, however, the thrifty phenotype would lead to the development of diabetes.
The most recent alternative to the thrifty gene hypothesis is the drifty gene hypothesis, which was proposed by biologist John Speakman. He argues that genes protecting humans from obesity were under strong natural selection pressure for a very long period of time while human ancestors were subject to the risk of predation. According to this view, being able to outrun predators would have been an important factor selecting against fatness. When the risk of predation was lessened — perhaps as early as two million years ago — genes keeping fatness in check would no longer be selected for. Without selective pressure for these genes, their frequencies could change randomly due to genetic drift. In some populations, by chance, frequencies of the genes could decrease to relatively low levels, whereas in other populations the frequencies could be much higher.
Feature: Myth vs. Reality

Myth: Lactose intolerance is an allergy to milk.
Reality: Lactose intolerance is not an allergy because it is not an immune system response. It is a sensitivity to milk caused by lactase deficiency so the sugar in milk cannot be digested. Milk allergy does exist, but it is a different condition that occurs in only about four per cent of people. It results when milk proteins (not milk sugar) trigger an immune reaction. How can you determine whether you have lactose intolerance or milk allergy? If you can drink lactose-free milk without symptoms, it is likely that you are lactose intolerant and not allergic to milk. However, if lactose-free milk also produces symptoms, it is likely that you have milk allergy. Note that it is possible to have both conditions.
Myth: If you are lactose intolerant, you will never be able to drink milk or consume other dairy products without suffering adverse physical symptoms.
Reality: Lactose intolerance does not mean that consuming milk and other dairy products is out of the question. Besides lactose-free milk, which is widely available, many dairy products have relatively low levels of lactose, so you may be able to consume at least small amounts of them without discomfort. You may be able to consume milk in the form of yogurt without any problems because the bacteria in yogurt produce lactase that breaks down the lactose. Greek yogurt may be your best bet, because it is lower in lactose to begin with. Aged cheeses also tend to have relatively low levels of lactose, because of the cheese-making process. Finally, by gradually adding milk or milk products to your diet, you may be able to increase your tolerance to lactose.
6.8 Summary
- Milk contains the sugar lactose, a disaccharide. Lactose must be broken down into its two component sugars to be absorbed by the small intestine, and the enzyme lactase is needed for this process.
- In about 60 per cent of people worldwide, the ability to synthesize lactase and digest lactose declines after the first two years of life. These people become lactose intolerant and cannot consume much milk without suffering symptoms of bloating, cramps, and diarrhea.
- In populations that herded milking animals for thousands of years, lactase persistence evolved. People who were able to synthesize lactase and digest lactose throughout life were strongly favored by natural selection. People — including many Europeans and European-Americans — who descended from these early herders generally still have lactase persistence.
- Human populations may vary in how efficiently they use calories in food. Some people (especially South Pacific Islanders, Native Americans, and sub-Saharan Africans) seem to be able to get by on fewer calories than would be adequate for others, so they tend to easily gain weight, become obese, and develop diseases such as diabetes.
- The thrifty gene hypothesis answers the question of how genes for this ability could have evolved. It proposes that “thrifty genes” were selected for because they allowed people to use calories efficiently and store body fat when food was plentiful so they had a reserve to use when food was scarce. Thrifty genes become detrimental and lead to obesity and diabetes when food is consistently plentiful.
- Several assumptions underlying the thrifty gene hypothesis have been called into question, and genetic research has been unable to actually identify thrifty genes. Alternate hypotheses to the thrifty gene hypothesis have been proposed, including the drifty gene hypothesis. The latter hypothesis explains variation in the tendency to become obese by genetic drift on neutral genes.
6.8 Review Questions
-
- Distinguish between the terms lactose and lactase.
- What is lactose intolerance, and what percentage of all people have it?
- Where and why did lactase persistence evolve?
- What is the thrifty gene hypothesis?
- How well is the thrifty gene hypothesis supported by evidence?
- Describe an alternative hypothesis to the thrifty gene hypothesis.
- Do you think that a lack of exposure to dairy products might affect a person’s lactase level? Why or why not?
- Describe an experiment you would want to do or data you would want to analyze that would help to test the thrifty phenotype hypothesis. Remember, you are studying people, so be sure it is ethical! Discuss possible confounding factors that you should control for, or that might affect the interpretation of your results.
- Explain the relationship between insulin, blood glucose, and type II diabetes.
6.8 Explore More
https://www.youtube.com/watch?v=G1NGzycaQV0&feature=emb_logo
Why Are People Lactose Intolerant?, Super Scienced, 2016.
https://www.youtube.com/watch?v=UMhLBPPtlrY
Peter Attia: What if we're wrong about diabetes?, TED, 2013.
https://www.youtube.com/watch?v=4O8k9qe8fjI
The Last Nomadic Reindeer Herders in the World, Great Big Story, 2018.
https://www.youtube.com/watch?v=XIYag5MWhPU
Experience a Traditional Whale Hunt in Northern Alaska | Short Film Showcase, National Geographic, 2018.
Attributions
Figure 6.8.1
IMG_4325 Milk Mustache licking 3 by Cedar Summit Farm on Flickr is used under a CC BY SA 2.0 (https://creativecommons.org/licenses/by-sa/2.0/) license.
Figure 6.8.2
Lactose Haworth by NEUROtiker on Wikimedia Commons is in the public domain (https://en.wikipedia.org/wiki/Public_domain).
Figure 6.8.3
Lactase by Boghog2 on Wikimedia Commons is released into the public domain (https://en.wikipedia.org/wiki/Public_domain).
Figure 6.8.4
Lactose Intolerance by Rainer Z ... on Wikimedia Commons is released into the public domain (https://en.wikipedia.org/wiki/Public_domain).
Figure 6.8.5
Reindeer_herding by Mats Andersson on Wikimedia Commons is used under a CC BY 2.0 (https://creativecommons.org/licenses/by/2.0/deed.en) license.
Figure 6.8.6
Milk Photo [photo] by Eiliv-Sonas Aceron on Unsplash is used under the Unsplash License (https://unsplash.com/license).
References
Great Big Story. (2018, November 29). The last nomadic reindeer herders in the world. YouTube. https://www.youtube.com/watch?v=4O8k9qe8fjI&feature=youtu.be
Super Scienced. (2016, February 26). Why are people lactose intolerant? YouTube. https://www.youtube.com/watch?v=G1NGzycaQV0&feature=youtu.be
National Geographic. (2018, November 27). Experience a traditional whale hunt in northern Alaska | Short film showcase. YouTube. https://www.youtube.com/watch?v=XIYag5MWhPU&feature=youtu.be
TED. (2013, June 25). Peter Attia: What if we're wrong about diabetes? YouTube. https://www.youtube.com/watch?v=UMhLBPPtlrY&feature=youtu.be
Wikipedia contributors. (2019, December 15). James V. Neel. In Wikipedia. https://en.wikipedia.org/w/index.php?title=James_V._Neel&oldid=930860629
Wikipedia contributors. (2020, June 9). John Speakman. In Wikipedia. https://en.wikipedia.org/w/index.php?title=John_Speakman&oldid=961610417

Case Study Conclusion: Your Genes May Help You Save a Life
As you have learned in this chapter, humans are much more genetically similar to each other than they are different. Any two people on Earth are 99.9 per cent genetically identical to each other — but the mere 0.1 per cent that is different can be very important, as in the case of bone marrow donation to treat diseases such as leukemia. A good match must exist between a bone marrow donor and recipient in genes that encode for human leukocyte antigen (HLA) proteins. As you have learned, antigens are molecules — often on the surface of cells — that the immune system uses to identify foreign invaders. If a patient receives a bone marrow transplant from a donor that has different types of HLAs than the patient does, antibodies in their immune system will identify the antigens as nonself and will launch an attack on the transplanted cells. Also, since bone marrow produces immune cells, antibodies in the transplanted tissue can actually attack the patient’s own cells using the same mechanism.
As you have also learned, a good HLA match is often difficult to find, even between full siblings. Finding a match in the registries is particularly hard for non-Caucasian people — and even harder for people from multiethnic backgrounds, such as seven-year-old Mateo, who you read about in the beginning of this chapter. Mateo is of African, Japanese, and Caucasian descent — a relatively rare combination. Because HLA matches are more likely to occur between people of the same ethnicity, the donor registries would ideally have sufficient potential donors from every ethnicity and ethnic combination. Unfortunately, some ethnicities are not sufficiently represented in the donor registry. According to the U.S. National Marrow Donor Program, while 97 per cent of Caucasian patients find a match, the match rate drops to 83 per cent for Hispanic or Latino patients and 76 per cent for African American or black patients. Multi-ethnic patients generally have an even harder time finding a match because the relative rareness of their particular ethnic combination in the general population makes it less likely that enough people of their same ancestry are registered donors.
As you learned in this chapter, human variation has historically been classified in several different ways, some of which resulted from or have contributed to racism. Most biological traits in humans exist on a continuum, and attempting to create biological categories of race based on discrete categories using a handful of traits is generally arbitrary and inaccurate. Gene flow through migration and mating between populations, genetic drift, and natural selection results in a gradual, clinal distribution of many human traits, rather than discrete categories. Mateo, for example, cannot be neatly placed into one racial category or another. Race and ethnic identity, however, remain important social and cultural concepts.
Mateo’s ancestry does play a role in determining his specific types of HLA proteins, and he is more likely to find a bone marrow match with a donor of an ethnic background similar to his own. Although there is much more genetic variation within races than between races, HLA types tend to correlate with ethnicity more than some other traits. As you have seen throughout this chapter, some environmental factors in different geographic regions have provided strong natural selection pressures, resulting in the development of genetic differences between people whose ancestors came from different areas. For example, adaptations to differing UV levels, diseases, altitudes, and climates all likely led to the evolution of human variations in skin colour, blood cells, and body morphology. This type of association between race and ethnicity and genetic variation is similar to the link between ethnicity and HLA type.
Mateo’s family was not able to find a match for him in the bone marrow registries, unlike the little boy pictured in Figure 6.9.1, but they are not giving up hope. His parents have started working with organizations to host bone marrow drives, where potential donors can provide cheek swabs to add themselves to the donor registry. His parents have contacted the news media with Mateo’s story, and family and friends are getting the word out on social media that more donors are needed, particular those with Mateo’s specific combination of ethnicities. They hope that even if they are unable to find a match for Mateo, bringing awareness to the issue may increase the ethnic diversity of the donor registry to save other lives.
You Can Help!
According to the Canadian Blood Services, more donors are needed to join the bone marrow registry. Currently, there is a need for more young male donors: male stem cell donors are more likely to be matched with recipients because they offer better patient outcomes after transplant. There is also a need for donors with diverse ethnic backgrounds, particularly Aboriginal, Hispanic, African-Canadian, Filipino, and more. DIverse donors are needed to acheive the closest possible match for HLA between the donor and the recipient.
Leukemia is not the only disease in which treatment involves bone marrow transplant — this course of action is often taken for conditions such as:
- Aplastic anemia
- Inherited immune system disorders
- Inherited metabolic disorders
- Bone marrow diseases
- Lymphomas
Are you registered? If not, it is a relatively simple process that could save someone’s life. A cheek swab is all that is initially needed. Only about one in 430 potential donors will actually be matched with a patient, and if you are chosen, it means that you are one of the only people on Earth who can donate to this patient because of your genetic similarity! If you decide to donate, bone marrow will either be surgically removed from the back of your pelvic bone, or blood-forming cells will be removed non-surgically from your bloodstream. Most donors are able to return to their normal activities one to seven days after donation — a small price to pay for potentially saving someone’s life!
https://www.youtube.com/watch?v=FyriQibRhLA
Stem cell donation: Step by step, hemaquebec1998, 2015.
https://www.youtube.com/watch?v=rLO0Usg8vcY&feature=emb_logo
Marrow donors talk about donating and the donation process, Be The Match, 2012.
Chapter 6 Summary
In this chapter, you learned about human variation and its origins. Specifically, you learned that:
- No two human individuals are genetically identical (except for monozygotic twins), but the human species as a whole exhibits relatively little genetic diversity relative to other mammalian species. Genetically, two people chosen at random are likely to be 99.9 per cent identical.
- Of the total genetic variation in humans, about 90 per cent occurs between people within continental populations, and only about 10 per cent occurs between people from different continents. Older, larger populations tend to have greater genetic variation, because there's been more time and there are more people in which to accumulate mutations.
- Single nucleotide polymorphisms account for most human genetic differences. Allele frequencies for polymorphic genes generally have a clinal, rather than discrete, distribution. A minority of alleles seem to cluster in particular geographic areas, such as the allele for no antigen in the Duffy blood group. Such alleles may be useful as genetic markers to establish the ancestry of individuals.
- Knowledge of genetic variation can help us understand our similarities and differences. It can also help us reconstruct our evolutionary origins and history as a species. For example, the distribution of modern human genetic variation is consistent with the out-of-Africa hypothesis for the origin of modern humans.
- An important benefit of studying human genetic variation is learning more about the genetic basis of human diseases. This should help us find more effective treatments and cures.
- Humans seem to have a need to classify and label people based on their similarities and differences. Three approaches to classifying human variation are typological, populational, and clinal approaches.
-
- The typological approach involves creating a system of discrete categories, or races (no longer used). This approach was widely used by scientists until the early 20th century. Racial categories are based on observable phenotypic traits (such as skin colour), but other traits and behaviors are often mistakenly assumed to apply to racial groups, as well. The use of racial classifications often leads to racism.
- By the mid-20th century, scientists started advocating a population approach (no longer used). This assumes that the breeding population, which is the unit of evolution, is the only biologically meaningful group. While this approach makes sense in theory, in reality, it can rarely be applied to actual human populations. With few exceptions, most human populations are not closed breeding populations.
- By the 1960s, scientists began to use a clinal approach to classify human variation. This approach maps variation in the frequency of traits or alleles over geographic regions or worldwide. Clinal maps for many genetic traits show variation that changes gradually from one geographic area to another. Gene flow and/or natural selection can cause this type of distribution.
- Humans may respond to environmental stress in four different ways: adaptation, developmental adjustment, acclimatization, and cultural responses.
-
- An adaptation is a genetically based trait that has evolved because it helps living things survive and reproduce in a given environment. Adaptations evolve by natural selection in populations over a relatively long period to time. Examples of adaptations include sickle cell trait as an adaptation to endemic malaria and the ability to taste bitter compounds as an adaptation to bitter-tasting toxins in plants.
- A developmental adjustment is a nongenetic response to stress that occurs during infancy or childhood. It may persist into adulthood and may be irreversible. Developmental adjustment is possible because humans have a high degree of phenotypic plasticity. It may be the result of environmental stresses, such as inadequate food — which may stunt growth — or cultural practices, such as orthodontic treatments, which re-align the teeth and jaws.
- Acclimatization is the development of reversible changes to environmental stress that develop over a relatively short period of time. The changes revert to the normal baseline state after the stress is removed. Examples of acclimatization include tanning of the skin and physiological changes (such as increased sweating) that occur with heat acclimatization.
- Cultural responses consist of learned behaviors and technology that allow us to change our environment to control stress, rather than changing our bodies genetically or physiologically to cope with stress. Examples include using shelter, fire, and clothing to cope with a cold climate.
- Blood type is a genetic characteristic associated with the presence or absence of antigens on the surface of red blood cells. A blood group system refers to all of the gene(s), alleles, and possible genotypes and phenotypes that exist for a particular set of blood type antigens.
-
- Antigens are molecules that the immune system identifies as either self or nonself. If antigens are identified as nonself, the immune system responds by forming antibodies that are specific to the nonself antigens, leading to the destruction of cells bearing the antigens.
- The ABO blood group system is a system of red blood cell antigens controlled by a single gene with three common alleles on chromosome 9. There are four possible ABO blood types: A, B, AB, and O. The ABO system is the most important blood group system in blood transfusions. People with type O blood are universal donors, and people with type AB blood are universal recipients.
- The frequencies of ABO blood type alleles and blood groups vary around the world. The allele for the B antigen is least common, and blood type O is the most common. Evolutionary forces of founder effect, genetic drift, and natural selection are responsible for the geographic distribution of ABO alleles and blood types. For example, people with type O blood may be somewhat resistant to malaria, possibly giving them a selective advantage where malaria is endemic.
- The Rhesus blood group system is a system of red blood cell antigens controlled by two genes with many alleles on chromosome 1. There are five common Rhesus antigens, of which antigen D is the most significant. Individuals who have antigen D are called Rh+, and individuals who lack antigen D are called Rh-. Rh- mothers of Rh+ fetuses may produce antibodies against the D antigen in the fetal blood, causing hemolytic disease of the newborn (HDN).
- The majority of people worldwide are Rh+, but there is regional variation in this blood group system. This variation may be explained by natural selection that favors heterozygotes for the D antigen, because this genotype seems to be protected against some of the neurological consequences of the common parasitic infection toxoplasmosis.
- At high altitudes, humans face the stress of hypoxia, or a lack of oxygen. Hypoxia occurs at high altitude because there is less oxygen in each breath of air and lower air pressure, which prevents adequate absorption of oxygen from the lungs.
- Initial responses to hypoxia include hyperventilation and elevated heart rate, but these responses are stressful to the body. Continued exposure to high altitude may cause high altitude sickness, with symptoms such as fatigue, shortness of breath, and loss of appetite. At higher altitudes, there is greater risk of serious illness.
- After several days at high altitude, acclimatization starts to occur in someone from a lowland population. More red blood cells and capillaries form, along with other changes. Full acclimatization may take several weeks. Returning to low altitude causes a reversal of the changes to the pre-high altitude state in a matter of weeks.
- Well over 100 million people live at altitudes higher than 2,500 metres above sea level. Some indigenous populations of Tibet, Peru, and Ethiopia have been living above 2,500 metres for thousands of years, and have evolved genetic adaptations to high altitude hypoxia. Different high altitude populations have evolved different adaptations to the same hypoxic stress. Tibetan highlanders, for example, have a faster rate of breathing and wider arteries, whereas Peruvian highlanders have larger red blood cells and a greater concentration of the oxygen-carrying protein hemoglobin.
- Both hot and cold temperatures are serious environmental stresses on the human body. In the cold, there is risk of hypothermia, which is a dangerous decrease in core body temperature. In the heat, there is risk of hyperthermia, which is a dangerous increase in core body temperature.
- According to Bergmann’s rule, body size tends to be negatively correlated with temperature, because larger body size increases heat production and decreases heat loss. The opposite holds true for small body size. Bergmann’s rule applies to many human populations that are hot or cold adapted.
- According Allen’s rule, the length of body extremities is positively correlated with temperature, because longer extremities are better at dissipating excess body heat. The opposite applies to shorter extremities. Allen’s rule applies to relative limb lengths in many human populations that have adapted to heat or cold.
- Sweating is the primary way humans lose body heat. The evaporation of sweat from the skin cools the body. This only works well when the relative humidity is fairly low. At high relative humidity, sweat does not readily evaporate to cool us down. The heat index (HI) indicates how hot it feels due to the humidity.
- Gradually working longer and harder in the heat can bring about heat acclimatization, in which the body has improved responses to heat stress. Sweating starts earlier, sweat contains less salt, and vasodilation brings heat to the surface to help cool the body. Full acclimatization takes up to 14 days and reverses just as quickly when the heat stress is removed.
- The human body can respond to cold by producing more heat (by shivering or increasing the basal metabolic rate) or by conserving heat (by vasoconstriction at the body surface or a layer of fat-insulating internal organs).
- At temperatures below freezing, the hunting response occurs to prevent cold injury (such as frostbite). This is a process of alternating vasoconstriction and vasodilation in extremities that are exposed to dangerous cold. Where temperatures are repeatedly cold but rarely below freezing, the hunting response may not occur, and the skin may remain cold due to vasoconstriction alone.
- Milk contains the sugar lactose, a disaccharide. Lactose must be broken down into its two component sugars to be absorbed by the small intestine, and the enzyme lactase is needed for this process.
- In about 60 per cent of people worldwide, the ability to synthesize lactase and digest lactose declines after the first two years of life. These people become lactose intolerant, and cannot consume much milk without suffering symptoms such as bloating, cramps, and diarrhea.
- In populations that herded milking animals for thousands of years, lactase persistence evolved. People who were able to synthesize lactase and digest lactose throughout life were strongly favored by natural selection. People who descended from these early herders generally still have lactase persistence. That includes many Europeans and European-Americans.
- Human populations may vary in how efficiently they use calories in food. Some people (especially South Pacific Islanders, Native Americans, and sub-Saharan Africans) may be able to get by on fewer calories than would be adequate for others, so they tend to easily gain weight, become obese, and develop diseases such as diabetes.
- The thrifty gene hypothesis proposes that “thrifty genes” were selected for because they allowed people to use calories efficiently and store body fat when food was plentiful so they had a reserve to use when food was scarce. According to the hypothesis, thrifty genes become detrimental and lead to obesity and diabetes when food is plentiful all of the time.
- Several assumptions underlying the thrifty gene hypothesis have been called into question, and genetic research has been unable to actually identify thrifty genes. Alternate hypotheses to the thrifty gene hypothesis have been proposed, including the drifty gene hypothesis. The latter hypothesis explains variation in the tendency to become obese by genetic drift on neutral genes.
In this chapter, you learned about how genetic variation can lead to differences in human characteristics. Genes encode for proteins, which carry out our bodies’ life processes. In the next chapter, you will learn about how proteins and other molecules make up the cells, tissues, and organs of the human body, and how these units work together in interacting systems to allow us to function.
Chapter 6 Review
- Explain why an evolutionarily older population is likely to have more genetic variation than a similarly-sized younger population.
- The genetic difference between any two people on Earth is only about 0.1 percent. Based on our evolutionary history, describe one reason why humans are relatively homogeneous genetically.
- What aspect(s) of human skin colour are due to adaptation? Be sure to define adaptation in your answer. What aspect(s) of human skin colour are due to acclimatization? Be sure to define acclimatization in your answer.
- For each of the following human responses to the environment, list whether it can be best described as an example of adaptation, acclimatization, or developmental adjustment:
- Reduction in height due to lack of food in childhood
- Resistance to malaria
- Shivering in the cold
- Changes in body size and dimensions to better tolerate heat or cold
- Give an example of a human response to environmental stress that involves changes in behavior, instead of changes in physiology.
- What are two types of environmental stresses that caused genetic changes related to hemoglobin in some populations of humans?
- The ability of an organism to change their phenotype in response to the environment is called phenotypic __________ .
- List three natural selection pressures that differ geographically across the world and contributed to the evolution of human genetic variation in different regions.
-
- You may have noticed that when a sudden hot day occurs during a cool period, it can feel even more uncomfortable than higher temperatures during a hot period — even with the same humidity levels. Using what you learned in this chapter, explain why you think that happens.
- Out of all mammals, why are humans the only ones that evolved lactase persistence?
- If the Inuit people who live in the Arctic were not able to get enough vitamin D from their diet, what do you think might happen to their skin colour over a long period of time? Explain your answer.
- Explain why malaria has been such a strong force of natural selection on human populations.
- Give one example of “heterozygote advantage” (i.e. when the heterozygous genotype has higher relative fitness than the dominant or recessive homozygous genotype) in humans.
- What is one way in which humans have evolved genetic adaptations in response to their food sources?
- Do you think adaptation to high altitude evolved once or several times? Explain your reasoning.
Attribution
Figure 6.9.1
Give Life - Donner la vie by Andrew Scheer on Wikimedia Commons is used under a CC0 1.0 Universal Public Domain Dedication (https://creativecommons.org/publicdomain/zero/1.0/deed.en) license.
References
Be The Match. (2012, December 19). Marrow donors talk about donating and the donation process. YouTube. https://www.youtube.com/watch?v=rLO0Usg8vcY&feature=youtu.be
Canadian Blood Services. (n.d.). There is an immediate need for blood as demand is rising. https://www.blood.ca/en
hemaquebec1998. (2015, August 27).Stem cell donation: Step by step. YouTube. https://www.youtube.com/watch?v=FyriQibRhLA&feature=youtu.be
A microorganism which causes disease.
Created by: CK-12/Adapted by Christine Miller

Case Study Conclusion: Your Genes May Help You Save a Life
As you have learned in this chapter, humans are much more genetically similar to each other than they are different. Any two people on Earth are 99.9 per cent genetically identical to each other — but the mere 0.1 per cent that is different can be very important, as in the case of bone marrow donation to treat diseases such as leukemia. A good match must exist between a bone marrow donor and recipient in genes that encode for human leukocyte antigen (HLA) proteins. As you have learned, antigens are molecules — often on the surface of cells — that the immune system uses to identify foreign invaders. If a patient receives a bone marrow transplant from a donor that has different types of HLAs than the patient does, antibodies in their immune system will identify the antigens as nonself and will launch an attack on the transplanted cells. Also, since bone marrow produces immune cells, antibodies in the transplanted tissue can actually attack the patient’s own cells using the same mechanism.
As you have also learned, a good HLA match is often difficult to find, even between full siblings. Finding a match in the registries is particularly hard for non-Caucasian people — and even harder for people from multiethnic backgrounds, such as seven-year-old Mateo, who you read about in the beginning of this chapter. Mateo is of African, Japanese, and Caucasian descent — a relatively rare combination. Because HLA matches are more likely to occur between people of the same ethnicity, the donor registries would ideally have sufficient potential donors from every ethnicity and ethnic combination. Unfortunately, some ethnicities are not sufficiently represented in the donor registry. According to the U.S. National Marrow Donor Program, while 97 per cent of Caucasian patients find a match, the match rate drops to 83 per cent for Hispanic or Latino patients and 76 per cent for African American or black patients. Multi-ethnic patients generally have an even harder time finding a match because the relative rareness of their particular ethnic combination in the general population makes it less likely that enough people of their same ancestry are registered donors.
As you learned in this chapter, human variation has historically been classified in several different ways, some of which resulted from or have contributed to racism. Most biological traits in humans exist on a continuum, and attempting to create biological categories of race based on discrete categories using a handful of traits is generally arbitrary and inaccurate. Gene flow through migration and mating between populations, genetic drift, and natural selection results in a gradual, clinal distribution of many human traits, rather than discrete categories. Mateo, for example, cannot be neatly placed into one racial category or another. Race and ethnic identity, however, remain important social and cultural concepts.
Mateo’s ancestry does play a role in determining his specific types of HLA proteins, and he is more likely to find a bone marrow match with a donor of an ethnic background similar to his own. Although there is much more genetic variation within races than between races, HLA types tend to correlate with ethnicity more than some other traits. As you have seen throughout this chapter, some environmental factors in different geographic regions have provided strong natural selection pressures, resulting in the development of genetic differences between people whose ancestors came from different areas. For example, adaptations to differing UV levels, diseases, altitudes, and climates all likely led to the evolution of human variations in skin colour, blood cells, and body morphology. This type of association between race and ethnicity and genetic variation is similar to the link between ethnicity and HLA type.
Mateo’s family was not able to find a match for him in the bone marrow registries, unlike the little boy pictured in Figure 6.9.1, but they are not giving up hope. His parents have started working with organizations to host bone marrow drives, where potential donors can provide cheek swabs to add themselves to the donor registry. His parents have contacted the news media with Mateo’s story, and family and friends are getting the word out on social media that more donors are needed, particular those with Mateo’s specific combination of ethnicities. They hope that even if they are unable to find a match for Mateo, bringing awareness to the issue may increase the ethnic diversity of the donor registry to save other lives.
You Can Help!
According to the Canadian Blood Services, more donors are needed to join the bone marrow registry. Currently, there is a need for more young male donors: male stem cell donors are more likely to be matched with recipients because they offer better patient outcomes after transplant. There is also a need for donors with diverse ethnic backgrounds, particularly Aboriginal, Hispanic, African-Canadian, Filipino, and more. DIverse donors are needed to acheive the closest possible match for HLA between the donor and the recipient.
Leukemia is not the only disease in which treatment involves bone marrow transplant — this course of action is often taken for conditions such as:
- Aplastic anemia
- Inherited immune system disorders
- Inherited metabolic disorders
- Bone marrow diseases
- Lymphomas
Are you registered? If not, it is a relatively simple process that could save someone’s life. A cheek swab is all that is initially needed. Only about one in 430 potential donors will actually be matched with a patient, and if you are chosen, it means that you are one of the only people on Earth who can donate to this patient because of your genetic similarity! If you decide to donate, bone marrow will either be surgically removed from the back of your pelvic bone, or blood-forming cells will be removed non-surgically from your bloodstream. Most donors are able to return to their normal activities one to seven days after donation — a small price to pay for potentially saving someone’s life!
https://www.youtube.com/watch?v=FyriQibRhLA
Stem cell donation: Step by step, hemaquebec1998, 2015.
https://www.youtube.com/watch?v=rLO0Usg8vcY&feature=emb_logo
Marrow donors talk about donating and the donation process, Be The Match, 2012.
Chapter 6 Summary
In this chapter, you learned about human variation and its origins. Specifically, you learned that:
- No two human individuals are genetically identical (except for monozygotic twins), but the human species as a whole exhibits relatively little genetic diversity relative to other mammalian species. Genetically, two people chosen at random are likely to be 99.9 per cent identical.
- Of the total genetic variation in humans, about 90 per cent occurs between people within continental populations, and only about 10 per cent occurs between people from different continents. Older, larger populations tend to have greater genetic variation, because there's been more time and there are more people in which to accumulate mutations.
- Single nucleotide polymorphisms account for most human genetic differences. Allele frequencies for polymorphic genes generally have a clinal, rather than discrete, distribution. A minority of alleles seem to cluster in particular geographic areas, such as the allele for no antigen in the Duffy blood group. Such alleles may be useful as genetic markers to establish the ancestry of individuals.
- Knowledge of genetic variation can help us understand our similarities and differences. It can also help us reconstruct our evolutionary origins and history as a species. For example, the distribution of modern human genetic variation is consistent with the out-of-Africa hypothesis for the origin of modern humans.
- An important benefit of studying human genetic variation is learning more about the genetic basis of human diseases. This should help us find more effective treatments and cures.
- Humans seem to have a need to classify and label people based on their similarities and differences. Three approaches to classifying human variation are typological, populational, and clinal approaches.
-
- The typological approach involves creating a system of discrete categories, or races (no longer used). This approach was widely used by scientists until the early 20th century. Racial categories are based on observable phenotypic traits (such as skin colour), but other traits and behaviors are often mistakenly assumed to apply to racial groups, as well. The use of racial classifications often leads to racism.
- By the mid-20th century, scientists started advocating a population approach (no longer used). This assumes that the breeding population, which is the unit of evolution, is the only biologically meaningful group. While this approach makes sense in theory, in reality, it can rarely be applied to actual human populations. With few exceptions, most human populations are not closed breeding populations.
- By the 1960s, scientists began to use a clinal approach to classify human variation. This approach maps variation in the frequency of traits or alleles over geographic regions or worldwide. Clinal maps for many genetic traits show variation that changes gradually from one geographic area to another. Gene flow and/or natural selection can cause this type of distribution.
- Humans may respond to environmental stress in four different ways: adaptation, developmental adjustment, acclimatization, and cultural responses.
-
- An adaptation is a genetically based trait that has evolved because it helps living things survive and reproduce in a given environment. Adaptations evolve by natural selection in populations over a relatively long period to time. Examples of adaptations include sickle cell trait as an adaptation to endemic malaria and the ability to taste bitter compounds as an adaptation to bitter-tasting toxins in plants.
- A developmental adjustment is a nongenetic response to stress that occurs during infancy or childhood. It may persist into adulthood and may be irreversible. Developmental adjustment is possible because humans have a high degree of phenotypic plasticity. It may be the result of environmental stresses, such as inadequate food — which may stunt growth — or cultural practices, such as orthodontic treatments, which re-align the teeth and jaws.
- Acclimatization is the development of reversible changes to environmental stress that develop over a relatively short period of time. The changes revert to the normal baseline state after the stress is removed. Examples of acclimatization include tanning of the skin and physiological changes (such as increased sweating) that occur with heat acclimatization.
- Cultural responses consist of learned behaviors and technology that allow us to change our environment to control stress, rather than changing our bodies genetically or physiologically to cope with stress. Examples include using shelter, fire, and clothing to cope with a cold climate.
- Blood type is a genetic characteristic associated with the presence or absence of antigens on the surface of red blood cells. A blood group system refers to all of the gene(s), alleles, and possible genotypes and phenotypes that exist for a particular set of blood type antigens.
-
- Antigens are molecules that the immune system identifies as either self or nonself. If antigens are identified as nonself, the immune system responds by forming antibodies that are specific to the nonself antigens, leading to the destruction of cells bearing the antigens.
- The ABO blood group system is a system of red blood cell antigens controlled by a single gene with three common alleles on chromosome 9. There are four possible ABO blood types: A, B, AB, and O. The ABO system is the most important blood group system in blood transfusions. People with type O blood are universal donors, and people with type AB blood are universal recipients.
- The frequencies of ABO blood type alleles and blood groups vary around the world. The allele for the B antigen is least common, and blood type O is the most common. Evolutionary forces of founder effect, genetic drift, and natural selection are responsible for the geographic distribution of ABO alleles and blood types. For example, people with type O blood may be somewhat resistant to malaria, possibly giving them a selective advantage where malaria is endemic.
- The Rhesus blood group system is a system of red blood cell antigens controlled by two genes with many alleles on chromosome 1. There are five common Rhesus antigens, of which antigen D is the most significant. Individuals who have antigen D are called Rh+, and individuals who lack antigen D are called Rh-. Rh- mothers of Rh+ fetuses may produce antibodies against the D antigen in the fetal blood, causing hemolytic disease of the newborn (HDN).
- The majority of people worldwide are Rh+, but there is regional variation in this blood group system. This variation may be explained by natural selection that favors heterozygotes for the D antigen, because this genotype seems to be protected against some of the neurological consequences of the common parasitic infection toxoplasmosis.
- At high altitudes, humans face the stress of hypoxia, or a lack of oxygen. Hypoxia occurs at high altitude because there is less oxygen in each breath of air and lower air pressure, which prevents adequate absorption of oxygen from the lungs.
- Initial responses to hypoxia include hyperventilation and elevated heart rate, but these responses are stressful to the body. Continued exposure to high altitude may cause high altitude sickness, with symptoms such as fatigue, shortness of breath, and loss of appetite. At higher altitudes, there is greater risk of serious illness.
- After several days at high altitude, acclimatization starts to occur in someone from a lowland population. More red blood cells and capillaries form, along with other changes. Full acclimatization may take several weeks. Returning to low altitude causes a reversal of the changes to the pre-high altitude state in a matter of weeks.
- Well over 100 million people live at altitudes higher than 2,500 metres above sea level. Some indigenous populations of Tibet, Peru, and Ethiopia have been living above 2,500 metres for thousands of years, and have evolved genetic adaptations to high altitude hypoxia. Different high altitude populations have evolved different adaptations to the same hypoxic stress. Tibetan highlanders, for example, have a faster rate of breathing and wider arteries, whereas Peruvian highlanders have larger red blood cells and a greater concentration of the oxygen-carrying protein hemoglobin.
- Both hot and cold temperatures are serious environmental stresses on the human body. In the cold, there is risk of hypothermia, which is a dangerous decrease in core body temperature. In the heat, there is risk of hyperthermia, which is a dangerous increase in core body temperature.
- According to Bergmann’s rule, body size tends to be negatively correlated with temperature, because larger body size increases heat production and decreases heat loss. The opposite holds true for small body size. Bergmann’s rule applies to many human populations that are hot or cold adapted.
- According Allen’s rule, the length of body extremities is positively correlated with temperature, because longer extremities are better at dissipating excess body heat. The opposite applies to shorter extremities. Allen’s rule applies to relative limb lengths in many human populations that have adapted to heat or cold.
- Sweating is the primary way humans lose body heat. The evaporation of sweat from the skin cools the body. This only works well when the relative humidity is fairly low. At high relative humidity, sweat does not readily evaporate to cool us down. The heat index (HI) indicates how hot it feels due to the humidity.
- Gradually working longer and harder in the heat can bring about heat acclimatization, in which the body has improved responses to heat stress. Sweating starts earlier, sweat contains less salt, and vasodilation brings heat to the surface to help cool the body. Full acclimatization takes up to 14 days and reverses just as quickly when the heat stress is removed.
- The human body can respond to cold by producing more heat (by shivering or increasing the basal metabolic rate) or by conserving heat (by vasoconstriction at the body surface or a layer of fat-insulating internal organs).
- At temperatures below freezing, the hunting response occurs to prevent cold injury (such as frostbite). This is a process of alternating vasoconstriction and vasodilation in extremities that are exposed to dangerous cold. Where temperatures are repeatedly cold but rarely below freezing, the hunting response may not occur, and the skin may remain cold due to vasoconstriction alone.
- Milk contains the sugar lactose, a disaccharide. Lactose must be broken down into its two component sugars to be absorbed by the small intestine, and the enzyme lactase is needed for this process.
- In about 60 per cent of people worldwide, the ability to synthesize lactase and digest lactose declines after the first two years of life. These people become lactose intolerant, and cannot consume much milk without suffering symptoms such as bloating, cramps, and diarrhea.
- In populations that herded milking animals for thousands of years, lactase persistence evolved. People who were able to synthesize lactase and digest lactose throughout life were strongly favored by natural selection. People who descended from these early herders generally still have lactase persistence. That includes many Europeans and European-Americans.
- Human populations may vary in how efficiently they use calories in food. Some people (especially South Pacific Islanders, Native Americans, and sub-Saharan Africans) may be able to get by on fewer calories than would be adequate for others, so they tend to easily gain weight, become obese, and develop diseases such as diabetes.
- The thrifty gene hypothesis proposes that “thrifty genes” were selected for because they allowed people to use calories efficiently and store body fat when food was plentiful so they had a reserve to use when food was scarce. According to the hypothesis, thrifty genes become detrimental and lead to obesity and diabetes when food is plentiful all of the time.
- Several assumptions underlying the thrifty gene hypothesis have been called into question, and genetic research has been unable to actually identify thrifty genes. Alternate hypotheses to the thrifty gene hypothesis have been proposed, including the drifty gene hypothesis. The latter hypothesis explains variation in the tendency to become obese by genetic drift on neutral genes.
In this chapter, you learned about how genetic variation can lead to differences in human characteristics. Genes encode for proteins, which carry out our bodies’ life processes. In the next chapter, you will learn about how proteins and other molecules make up the cells, tissues, and organs of the human body, and how these units work together in interacting systems to allow us to function.
Chapter 6 Review
- Explain why an evolutionarily older population is likely to have more genetic variation than a similarly-sized younger population.
- The genetic difference between any two people on Earth is only about 0.1 percent. Based on our evolutionary history, describe one reason why humans are relatively homogeneous genetically.
- What aspect(s) of human skin colour are due to adaptation? Be sure to define adaptation in your answer. What aspect(s) of human skin colour are due to acclimatization? Be sure to define acclimatization in your answer.
- For each of the following human responses to the environment, list whether it can be best described as an example of adaptation, acclimatization, or developmental adjustment:
- Reduction in height due to lack of food in childhood
- Resistance to malaria
- Shivering in the cold
- Changes in body size and dimensions to better tolerate heat or cold
- Give an example of a human response to environmental stress that involves changes in behavior, instead of changes in physiology.
- What are two types of environmental stresses that caused genetic changes related to hemoglobin in some populations of humans?
- The ability of an organism to change their phenotype in response to the environment is called phenotypic __________ .
- List three natural selection pressures that differ geographically across the world and contributed to the evolution of human genetic variation in different regions.
-
- You may have noticed that when a sudden hot day occurs during a cool period, it can feel even more uncomfortable than higher temperatures during a hot period — even with the same humidity levels. Using what you learned in this chapter, explain why you think that happens.
- Out of all mammals, why are humans the only ones that evolved lactase persistence?
- If the Inuit people who live in the Arctic were not able to get enough vitamin D from their diet, what do you think might happen to their skin colour over a long period of time? Explain your answer.
- Explain why malaria has been such a strong force of natural selection on human populations.
- Give one example of “heterozygote advantage” (i.e. when the heterozygous genotype has higher relative fitness than the dominant or recessive homozygous genotype) in humans.
- What is one way in which humans have evolved genetic adaptations in response to their food sources?
- Do you think adaptation to high altitude evolved once or several times? Explain your reasoning.
Attribution
Figure 6.9.1
Give Life - Donner la vie by Andrew Scheer on Wikimedia Commons is used under a CC0 1.0 Universal Public Domain Dedication (https://creativecommons.org/publicdomain/zero/1.0/deed.en) license.
References
Be The Match. (2012, December 19). Marrow donors talk about donating and the donation process. YouTube. https://www.youtube.com/watch?v=rLO0Usg8vcY&feature=youtu.be
Canadian Blood Services. (n.d.). There is an immediate need for blood as demand is rising. https://www.blood.ca/en
hemaquebec1998. (2015, August 27).Stem cell donation: Step by step. YouTube. https://www.youtube.com/watch?v=FyriQibRhLA&feature=youtu.be
Created by CK-12/Adapted by Christine Miller

Looking at this photo of a football game (Figure 7.1.1), you can see why it is so important that the players wear helmets. As players tackle each other, football often involves forceful impact to the head. This can cause damage to the brain — temporarily (as in the case of a concussion) or long-term and more severe. Helmets are critical in reducing the incidence of traumatic brain injuries (TBIs), but they do not fully prevent them.
As a former professional football player who also played in college and high school, 43-year-old Jayson sustained many high-impact head injuries over the course of his football playing years. A few years ago, Jayson began experiencing a variety of troubling symptoms, including the loss of bladder control (the involuntary leakage of urine), memory loss, and difficulty walking. Symptoms like these are often signs of damage to the nervous system, which includes the brain, spinal cord, and nerves, but they can result from many different types of injuries or diseases that affect the nervous system. In order to treat him properly, Jayson’s doctors needed to do several tests to determine the exact cause of his symptoms. The doctors ordered a spinal tap to see if he had an infection, and an MRI (magnetic resonance imaging) to see if there were any observable problems in and around his brain.
The MRI revealed the cause of Jayson’s symptoms. There are fluid-filled spaces within the brain called ventricles, and compared to normal ventricles, Jayson’s ventricles were enlarged. Based on this observation, along with the results of other tests, Jayson’s doctor diagnosed him with hydrocephalus, a term that literally means “water head.” Hydrocephalus occurs when the fluid that fills the ventricles — called cerebrospinal fluid — builds up excessively, causing the ventricles to become enlarged. This puts pressure on the brain, which can cause a variety of neurological symptoms, including the ones Jayson was experiencing. In Figure 7.1.2, you can see the difference between normal ventricles and ventricles that are enlarged due to hydrocephalus. Notice in the image on the right how the brain becomes “squeezed” due to hydrocephalus.
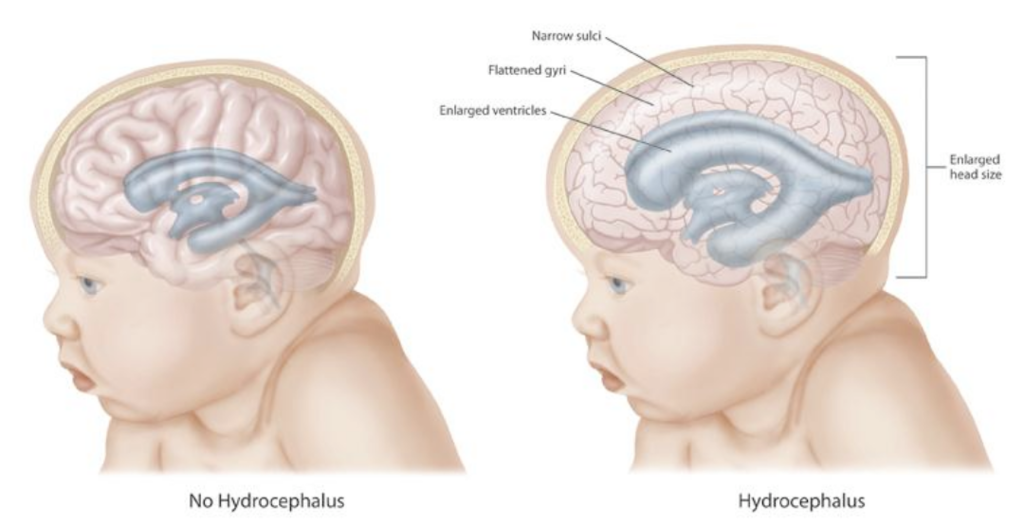
Hydrocephalus often occurs at birth, as a result of genetic factors or events that occurred during fetal development. Because babies are born with skull bones that are not fully fused, the skull of a baby born with hydrocephalus can expand and relieve some of the pressure on the brain, as reflected in the enlarged head size shown in Figure 7.1.2. Adults have fully fused, inflexible skulls, so when hydrocephalus occurs in an adult, the brain experiences all of the increased pressure.
Why did Jayson develop hydrocephalus? There are many possible causes of hydrocephalus in adults, including tumors, infections, hemorrhages, and TBIs. Given his repeated and long history of football-related TBIs and the absence of any evidence of infection, tumor, or other cause, Jayson’s doctor thinks his head injuries were most likely responsible for his hydrocephalus.
Although hydrocephalus is serious, there are treatments. Read the rest of this chapter to learn about the cells, tissues, organs, cavities, and systems of the body, how they are interconnected, and the importance of keeping the body in a state of homeostasis (or balance). The amount of cerebrospinal fluid in the ventricles is normally kept at a relatively steady level, and the potentially devastating symptoms of hydrocephalus are an example of what can happen when a system in the body becomes unbalanced. At the end of the chapter, you will learn about Jayson’s treatment and prognosis.
Chapter Overview: Introduction to the Human Body
In this chapter, you will learn about the general organization and functions of the human body. Specifically, you will learn about:
- The organization of the body from atoms and molecules up through cells, tissues, organs, and organ systems.
- How organ systems work together to carry out the functions of life.
- The variety of different specialized cell types in humans, the four major types of human tissues, and some of their functions.
- The five vital organs and the 11 major organ systems of the human body.
- Spaces in the body called body cavities, and the organs they hold and protect.
- The tissues and fluid that protect the brain and spinal cord.
- How organ systems communicate and interact in body processes, such as cellular respiration, digestion, the fight-or-flight response to stressors, and physical activities (such as sports).
- How homeostasis is maintained to keep the body in a relatively steady state, and the problems that can be caused by loss of homeostasis, such as diabetes.
As you read the chapter, think about the following questions:
- What is the normal function of cerebrospinal fluid?
- What is a spinal tap and how does it test for infection?
- In Jayson’s case, what organs and organ systems are probably affected by his hydrocephalus? What are some ways in which these organ systems interact?
- The level of cerebrospinal fluid is normally kept in a state of homeostasis. What are other examples of types of homeostasis that keep your body functioning properly?
Attributions
Figure 7.1.1.
Football tackel [photo] by John Torcasio on Unsplash is used under the Unsplash License (https://unsplash.com/license).
Figure 7.1.2
Hydrocephalus by Centers for Disease Control and Prevention (CDC) on Wikimedia Commons is in the public domain (https://en.wikipedia.org/wiki/Public_domain).
References
Mayo Clinic Staff. (n.d.). Hydrocephalus [online article]. MayoClinic.org. https://www.mayoclinic.org/diseases-conditions/hydrocephalus/symptoms-causes/syc-20373604
Mayo Clinic Staff. (n.d.). Traumatic brain injury [online article]. MayoClinic.org. https://www.mayoclinic.org/diseases-conditions/traumatic-brain-injury/symptoms-causes/syc-20378557

