11.7 Disorders of the Skeletal System
Dowager’s Hump
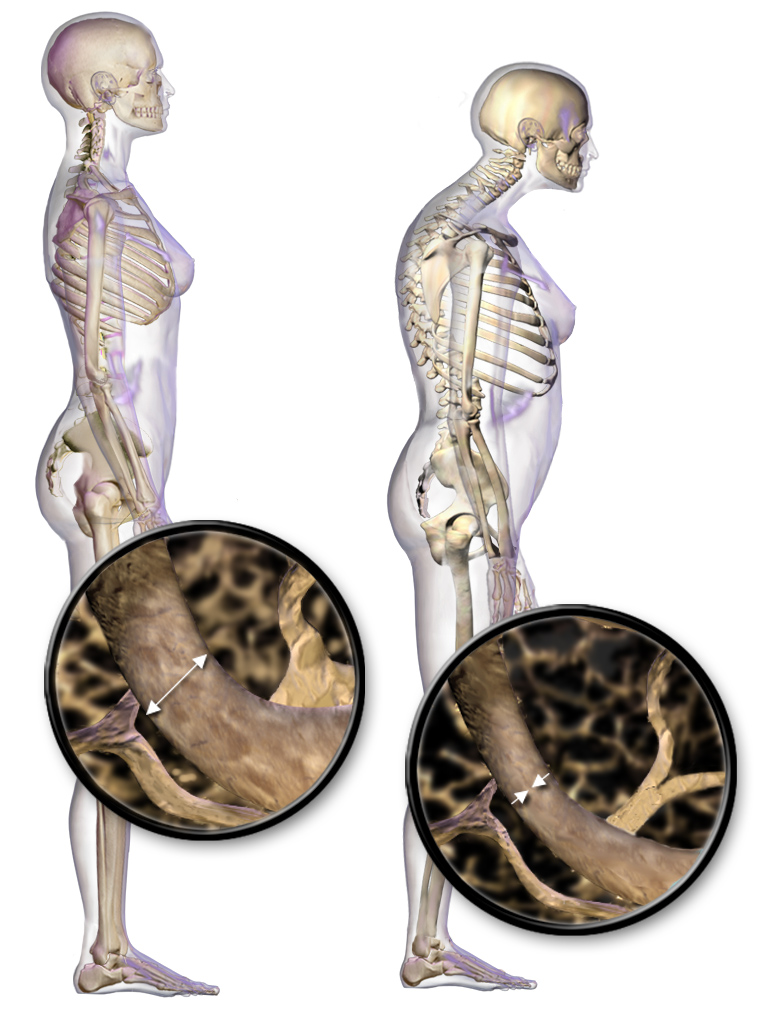
The woman on the right in Figure 11.7.1 has a deformity in her back commonly called dowager’s (widow’s) hump, because it occurs most often in elderly women. Its medical name is kyphosis, and it is defined as excessive curvature of the spinal column in the thoracic region. The curvature generally results from fractures of thoracic vertebrae. As the inset drawings suggest, these fractures may occur due to a significant decrease in bone mass, which is called osteoporosis. Osteoporosis is one of the most prevalent disorders of the skeletal system.
Common Skeletal System Disorders
A number of disorders affect the skeletal system, including bone fractures and bone cancers. However, the two most common disorders of the skeletal system are osteoporosis and osteoarthritis. At least ten million people in the United States have osteoporosis, and more than eight million of them are women. Osteoarthritis is even more common, affecting almost 1.4 million people in Canada, and 1 in 4 women over the age of 50. Because osteoporosis and osteoarthritis are so common, they are the focus of this section. These two disorders are also good examples to illustrate the structure and function of the skeletal system.
Osteoporosis
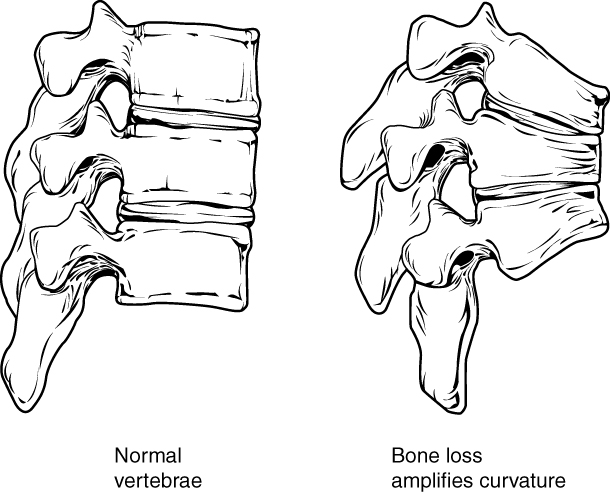
Osteoporosis is an age-related disorder in which bones lose mass, weaken, and break more easily than normal bones. Bones may weaken so much that a fracture can occur with minor stress — or even spontaneously, without any stress at all. Osteoporosis is the most common cause of broken bones in the elderly, but until a bone fracture occurs, it typically causes no symptoms. The bones that break most often include those in the wrist, hip, shoulder, and spine. When the thoracic vertebrae are affected, there can be a gradual collapse of the vertebrae due to compression fractures, as shown in Figure 11.7.2. This is what causes kyphosis, as pictured above in Figure 11.7.1.
Changes in Bone Mass with Age
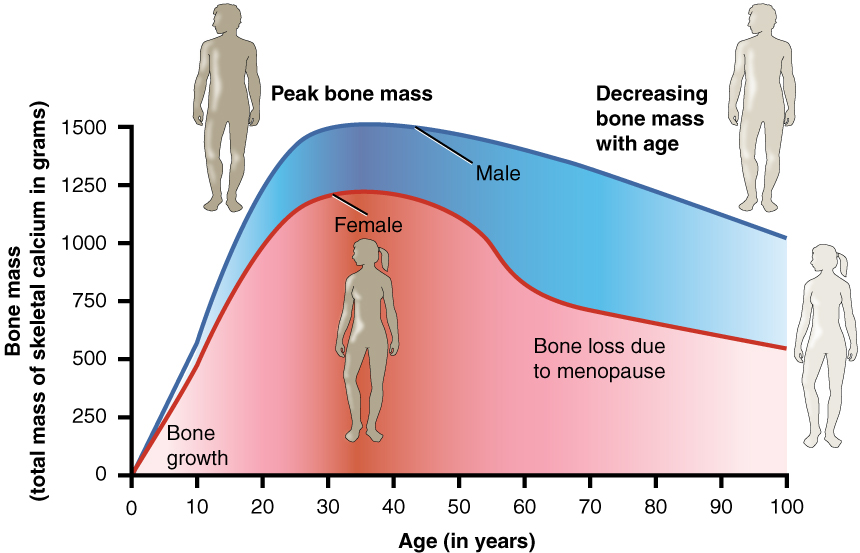
As shown in the Figure 11.7.3, bone mass in both males and females generally peaks when people are in their thirties, with males typically attaining a higher peak mass than females. In both sexes, bone mass usually decreases after that, and this tends to occur more rapidly in females, especially after menopause. The greater decrease in females is generally attributable to low levels of estrogen in the post-menopausal years.
What Causes Osteoporosis?
The underlying mechanism in all cases of osteoporosis is an imbalance between bone formation by osteoblasts and bone resorption by osteoclasts. Normally, bones are constantly being remodeled by these two processes, with up to ten per cent of all bone mass undergoing remodeling at any point in time. As long as these two processes are in balance, no net loss of bone occurs. There are three main ways that an imbalance between bone formation and bone resorption can occur and lead to a net loss of bone. All three ways may occur in the same individual. The three ways are described below:
- An individual never develops normal peak bone mass during the young adult years: If the peak level is lower than normal, then there is less bone mass to begin with, making osteoporosis more likely to develop.
- There is greater than normal bone resorption: Bone resorption normally increases after peak bone mass is reached, but age-related bone resorption may be greater than normal for a variety of reasons. One possible reason is calcium or vitamin D deficiency, which causes the parathyroid gland to release PTH, the hormone that promotes resorption by osteoclasts.
- There is inadequate formation of new bone by osteoblasts during remodeling: Lack of estrogen may decrease the normal deposition of new bone. Inadequate levels of calcium and vitamin D also lead to impaired bone formation by osteoblasts.
An imbalance between bone building and bone destruction leading to bone loss may also occur as a side effect of other disorders. For example, people with alcoholism, anorexia nervosa, or hyperthyroidism have an increased rate of bone loss. Some medications — including anti-seizure medications, chemotherapy drugs, steroid medications, and some antidepressants — also increase the rate of bone loss.
Diagnosing Osteoporosis
Osteoporosis is diagnosed by measuring a patient’s bone density and comparing it with the normal level of peak bone density in a young adult reference population of the same sex as the patient. If the patient’s bone density is too far below the normal peak level (as measured by a statistic called a T-score), then osteoporosis is diagnosed. Bone density is usually measured by a type of X-ray called dual-energy X-ray absorptiometry (or DEXA), an example of which is shown in Figure 11.7.4. Typically, the density is measured at the hip. Sometimes, other areas are also measured, because there may be variation in bone density in different parts of the skeleton. Osteoporosis Canada recommends that all women 65 years of age and older be screened with DEXA for bone density. Screening may be recommended at younger ages in people with risk factors for osteoporosis (see Risk Factors for Osteoporosis below).

Osteoporotic Fractures
Fractures are the most dangerous aspect of osteoporosis, and osteoporosis is responsible for millions of fractures annually. Debilitating pain among the elderly is often caused by fractures from osteoporosis, and it can lead to further disability and early mortality. Fractures of the long bones (such as the femur) can impair mobility and may require surgery. Hip fracture usually requires immediate surgery, as well. The immobility associated with fractures — especially of the hip — increases the risk of deep vein thrombosis, pulmonary embolism, and pneumonia. Osteoporosis is rarely fatal, but these complications of fractures often are. Older people tend to have more falls than younger people, due to such factors as poor eyesight and balance problems, increasing their risk of fractures even more. The likelihood of falls can be reduced by removing obstacles and loose carpets or rugs in the living environment.
Risk Factors for Osteoporosis
There are a number of factors that increase the risk of osteoporosis. Eleven of them are listed below. The first five factors cannot be controlled, but the remaining factors generally can be controlled by changing behaviors.
- Older age
- Female sex
- European or Asian ancestry
- Family history of osteoporosis
- Short stature and small bones
- Smoking
- Alcohol consumption
- Lack of exercise
- Vitamin D deficiency
- Poor nutrition
- Consumption of soft drinks
Treatment and Prevention of Osteoporosis
Osteoporosis is often treated with medications that may slow or even reverse bone loss. Medications called bisphosphonates, for example, are commonly prescribed. Bisphosphonates slow down the breakdown of bone, allowing bone rebuilding during remodeling to keep pace. This helps maintain bone density and decreases the risk of fractures. The medications may be more effective in patients who have already broken bones than in those who have not, significantly reducing their risk of another fracture. Generally, patients are not recommended to stay on bisphosphonates for more than three or four years. There is no evidence for continued benefit after this time — in fact, there is a potential for adverse side effects.

Preventing osteoporosis includes eliminating any risk factors that can be controlled through changes of behavior. If you smoke, stop. If you drink, reduce your alcohol consumption — or cut it out altogether. Eat a nutritious diet and make sure you are getting adequate amounts of vitamin D. You should also avoid drinking carbonated beverages.
If you’re a couch potato, get involved in regular exercise. Aerobic, weight-bearing, and resistance exercises can all help maintain or increase bone mineral density (for example hiking as in Figure 11.7.5). Exercise puts stress on bones, which stimulates bone building. Good weight-bearing exercises for bone building include weight training, dancing, stair climbing, running, and hiking (see Figure 11.7.5). Biking and swimming are less beneficial, because they don’t stress the bones. Ideally, you should exercise for at least 30 minutes a day most days of the week.
Osteoarthritis (OA) is a joint disease that results from the breakdown of joint cartilage and bone. The most common symptoms are joint pain and stiffness. Other symptoms may include joint swelling and decreased range of motion. Initially, symptoms may occur only after exercise or prolonged activity, but over time, they may become constant, negatively affecting work and normal daily activities. As shown in Figure 11.7.6, the most commonly involved joints are those near the ends of the fingers, at the bases of the thumbs, and in the neck, lower back, hips, and knees. Often, joints on one side of the body are affected more than those on the other side.
What Causes Osteoarthritis?
OA is thought to be caused by mechanical stress on the joints with insufficient self-repair of cartilage. The stress may be exacerbated by low-grade inflammation of the joints, as cells lining the joint attempt to remove breakdown products from cartilage in the synovial space. OA develops over decades as stress and inflammation cause increasing loss of articular cartilage. Eventually, bones may have no cartilage to separate them, so bones rub against one another at joints. This damages the articular surfaces of the bones and contributes to the pain and other symptoms of OA. Because of the pain, movement may be curtailed, leading to loss of muscle, as well.
Diagnosing Osteoarthritis

Diagnosis of OA is typically made on the basis of signs and symptoms. Signs include joint deformities, such as bony nodules on the finger joints or bunions on the feet (as illustrated in Figure 11.7.7). Symptoms include joint pain and stiffness. The pain is usually described as a sharp ache or burning sensation, which may be in the muscles and tendons around the affected joints, as well as in the joints themselves. The pain is usually made worse by prolonged activity, and it typically improves with rest. Stiffness is most common when first arising in the morning, and it usually improves quickly as daily activities are undertaken.
X-rays or other tests are sometimes used to either support the diagnosis of OA or to rule out other disorders. Blood tests might be done, for example, to look for factors that indicate rheumatoid arthritis (RA), an autoimmune disease in which the immune system attacks the body’s joints. If these factors are not present in the blood, then RA is unlikely, and a diagnosis of OA is more likely to be correct.
Risk Factors for Osteoarthritis
Age is the chief risk factor for osteoarthritis. By age 65, as many as 80 per cent of all people have evidence of osteoarthritis. However, people are more likely to develop OA — especially at younger ages — if they have had a joint injury. A high school football player might have a bad knee injury that damages the joint, leading to OA in the knee by the time he is in his thirties. If people have joints that are misaligned due to congenital malformations or disease, they are also more likely to develop OA. Excess body weight is another factor that increases the risk of OA, because of the added stress it places on weight-bearing joints.
Researchers have found that people with a family history of OA have a heightened risk of developing the disorder, which suggests that genetic factors are also involved in OA. It is likely that many different genes are needed for normal cartilage and cartilage repair. If such genes are defective and cartilage is abnormal or not normally repaired, OA is more likely to result.
Treatment and Prevention of Osteoarthritis
OA cannot be cured, but the symptoms — especially the pain — can often be treated successfully to maintain good quality of life for people with OA. Treatments include exercise, efforts to decrease stress on joints, pain medications, and surgery.
Exercise
Exercise helps maintain joint mobility and also increases muscle strength. Stronger muscles may help keep the bones in joints correctly aligned, and this can reduce joint stress. Good exercises for OA include swimming, water aerobics (see Figure 11.7.8 below), and biking. These activities are recommended for OA, because they put relatively little stress on the joints.

Exercising in water provides buoyancy that places less stress on joints than the same exercises would on the ground or other hard surface.
De-stressing Joints
Efforts to decrease stress on joints include resting and using mobility devices such as canes, which reduce the weight placed on weight-bearing joints and also improve stability. In people who are overweight, losing weight may also reduce joint stress.
Pain Medications
The first type of pain medication likely to be prescribed for OA is acetaminophen (e.g., Tylenol). When taken as prescribed, it has a relatively low risk of serious side effects. If this medication is inadequate to relieve the pain, non-steroidal anti-inflammatory drugs (NSAIDs, such as ibuprofen) may be prescribed. NSAIDs, however, are more likely to cause serious side effects, such as gastrointestinal bleeding, elevated blood pressure, and increased risk of stroke. Opioids usually are reserved for patients who have suffered serious side effects or for whom other medications have failed to relieve pain. Due to the risk of addiction, only short-term use of opioids is generally recommended.
Surgery
Joint-replacement surgery is the most common treatment for serious OA in the knee or hip. In fact, knee and hip replacement surgeries are among the most common of all surgeries. Although they require a long period of healing and physical rehabilitation, the results are usually worth it. The replacement “parts” are usually pain-free and fully functional for at least a couple of decades. Quality, durability, and customization of artificial joints are constantly improving.
Try out this neat Virtual Hip Resurfacing activity by Edheads (you will need to enable Flash).
Feature: Myth vs. Reality
About one out of every 5 adults in Canada suffer from osteoarthritis. The more you know about this disease, the more you can do to avoid it or slow its progression. That means knowing the facts, rather than believing the myths about osteoarthritis.
Myth |
Reality |
| “Cracking my knuckles will cause osteoarthritis.” | Cracking your knuckles may lead to inflammation of your tendons, but it will not cause osteoarthritis. |
| “My diet has no effect on my joints.” | What and how much you eat does affect your body weight, and every pound you gain translates into an additional four pounds (or more!) of stress on your knees. Being overweight, therefore, increases the chances of developing osteoarthritis — and also the rate at which it progresses. |
| “Exercise causes osteoarthritis or makes it worse, so I should avoid it.” | This is one of the biggest myths about osteoarthritis. Low-impact exercise can actually lessen the pain and improve other symptoms of osteoarthritis. If you don’t have osteoarthritis, exercise can reduce your risk of developing it. Low-impact exercise helps keep the muscles around joints strong and flexible, so they can help stabilize and protect the joints. |
| “If my mom or dad has osteoarthritis, I will also develop it.” | It is true that you are more likely to develop osteoarthritis if a parent has it, but it isn’t a sure thing. There are several things you can do to decrease your risk, such as getting regular exercise and maintaining a healthy weight. |
| “Bad weather causes osteoarthritis.” | Weather conditions do not cause osteoarthritis, although in some people who already have osteoarthritis, bad weather seems to make the symptoms worse. It is primarily low barometric pressure that increases osteoarthritis pain, probably because it leads to greater pressure inside the joints relative to the outside air pressure. Some people think their osteoarthritis pain is worse in cold weather, but systematic studies have not found convincing evidence for this. |
| “Joint pain is unavoidable as you get older, so there is no need to see a doctor for it.” | Many people with osteoarthritis think there is nothing that can be done for the pain of osteoarthritis, or that surgery is the only treatment option. In reality, osteoarthritis symptoms often can be improved with a combination of exercise, weight loss, pain management techniques, and pain medications. If osteoarthritis pain interferes with daily life and lasts more than a few days, you should see your doctor. |
| “Osteoarthritis is inevitable in seniors.” |
Although many people over 65 develop osteoarthritis, there are many people who never develop it, no matter how old they live to be. You can reduce your risk of developing osteoarthritis in later life by protecting your joints throughout life. |
11.7 Summary
- A number of disorders affect the skeletal system, including bone fractures and bone cancers. The two most common disorders of the skeletal system are osteoporosis and osteoarthritis.
- Osteoporosis is an age-related disorder in which bones lose mass, weaken, and break more easily than normal bones. The underlying mechanism in all cases of osteoporosis is an imbalance between bone formation and bone resorption in bone remodeling. Osteoporosis may also occur as a side effect of other disorders or certain medications.
- Osteoporosis is diagnosed by measuring a patient’s bone density and comparing it with the normal level of peak bone density. Fractures are the most dangerous aspect of osteoporosis. Osteoporosis is rarely fatal, but complications of fractures often are.
- Risk factors for osteoporosis include older age, female sex, European or Asian ancestry, family history of osteoporosis, short stature and small bones, smoking, alcohol consumption, lack of exercise, vitamin D deficiency, poor nutrition, and consumption of soft drinks.
- Osteoporosis is often treated with medications — such as bisphosphonates — that may slow or even reverse bone loss. Preventing osteoporosis includes eliminating any risk factors that can be controlled through changes of behavior, such as undertaking weight-bearing exercise.
- Osteoarthritis (OA) is a joint disease that results from the breakdown of joint cartilage and bone. The most common symptoms are joint pain and stiffness. OA is thought to be caused by mechanical stress on the joints with insufficient self-repair of cartilage, coupled with low-grade inflammation of the joints.
- Diagnosis of OA is typically made on the basis of signs and symptoms, such as joint deformities, pain, and stiffness. X-rays or other tests are sometimes used to either support the diagnosis or rule out other disorders. Age is the chief risk factor for OA. Other risk factors include joint injury, excess body weight, and a family history of OA.
- OA cannot be cured, but the symptoms can often be treated successfully. Treatments may include exercise, efforts to decrease stress on joints, pain medications, and surgery to replace affected hip or knee joints.
11.7 Review Questions
- Create a brochure or poster about osteoporosis to educate others about this disease. Include information about:
- A definition of osteoporosis
- Causes
- Dangers of living with the disease
- Canadian osteoporosis statistics
- Risk factors
- Diagnosis
- Treatment
-
- Why is it important to build sufficient bone mass in your young adult years?
- Explain the difference in cause between rheumatoid arthritis and osteoarthritis.
- Debunk the myth: Osteoarthritis is caused by physical activity, so people who are equally active are equally susceptible to it.
- Explain how we know that estrogen generally promotes production of new bone.
11.7 Explore More
Kevin Stone: The bio-future of joint replacement, TED, 2010.
The benefits of good posture – Murat Dalkilinç, TED-Ed, 2015.
Attributions
Figure 11.7.1
Blausen_0686_Osteoporosis_01 by BruceBlaus on Wikimedia Commons is used under a CC BY 3.0 (https://creativecommons.org/licenses/by/3.0) license.
Figure 11.7.2
Feature_Osteoprosis_of_Spine by OpenStax College on Wikimedia Commons is used under a CC BY 3.0 (https://creativecommons.org/licenses/by/3.0) license.
Figure 11.7.3
Age_and_Bone_Mass by OpenStax College on Wikimedia Commons is used under a CC BY 3.0 (https://creativecommons.org/licenses/by/3.0) license.
Figure 11.7.4
DEXA_scan_screen_ALSPAC by Nick Smith photography on Wikimedia Commons is used under a CC BY-SA 3.0 license.
Figure 11.7.5
Hiking by jake-melara-Yh6K2eTr_FY [photo] by Jake Melara on Unsplash is used under the Unsplash License (https://unsplash.com/license).
Figure 11.7.6
Areas_affected_by_osteoarthritis by National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS)/ NIH on Wikimedia Commons is in the public domain (https://en.wikipedia.org/wiki/Public_domain).
Figure 11.7.7
Hallux_valgus by Malmstajn on Wikimedia Commons is used under a CC BY 3.0 (https://creativecommons.org/licenses/by/3.0) license.
Figure 11.7.8
07-06_WtrAerob1a by Tim Ross on Wikimedia Commons is in the public domain (https://en.wikipedia.org/wiki/Public_domain).
References
Betts, J. G., Young, K.A., Wise, J.A., Johnson, E., Poe, B., Kruse, D.H., Korol, O., Johnson, J.E., Womble, M., DeSaix, P. (2013, June 19). Figure 6.23 Graph showing relationship between age and bone mass digital image]. In Anatomy and Physiology (Section 6.6). OpenStax. https://openstax.org/books/anatomy-and-physiology/pages/6-6-exercise-nutrition-hormones-and-bone-tissue
Betts, J. G., Young, K.A., Wise, J.A., Johnson, E., Poe, B., Kruse, D.H., Korol, O., Johnson, J.E., Womble, M., DeSaix, P. (2013, June 19). Figure 7.22 Osteoporosis [digital image]. In Anatomy and Physiology (Section 7.3). OpenStax. https://openstax.org/books/anatomy-and-physiology/pages/7-3-the-vertebral-column
Blausen.com staff. (2014). Medical gallery of Blausen Medical 2014. WikiJournal of Medicine 1 (2). DOI:10.15347/wjm/2014.010. ISSN 2002-4436.
Mayo Clinic Staff. (n.d.). Kyphosis [online article]. MayoClinic.org. https://www.mayoclinic.org/diseases-conditions/kyphosis/symptoms-causes/syc-20374205
Mayo Clinic Staff. (n.d.). Osteoarthritis [online article]. MayoClinic.org. https://www.mayoclinic.org/diseases-conditions/osteoarthritis/symptoms-causes/syc-20351925
TED. (2010, July 23). Kevin Stone: The bio-future of joint replacement. YouTube. https://youtu.be/DL0_gcP15Ts
TED-Ed. (2015, July 30). The benefits of good posture – Murat Dalkilinç. YouTube. https://www.youtube.com/watch?v=OyK0oE5rwFY&feature=youtu.be
Wheatley, G., Smail, S., Bort, E. (2007). Virtual hip resurfacing [online game]. EdHeads.org. https://edheads.org/page/hip_resurfacing

Created by: CK-12/Adapted by Christine Miller
Danger! Acid!
You probably know that batteries contain dangerous chemicals, including strong acids. Strong acids can hurt you if they come into contact with your skin or eyes. Therefore, it may surprise you to learn that your life depends on acids. There are many acids inside your body, and some of them are as strong as battery acid. Acids are needed for digestion and some forms of energy production. Genes are made of nucleic acids, proteins of amino acids, and lipids of fatty acids.
Water and Solutions
Acids (such as battery acid) are solutions. A solution is a mixture of two or more substances that has the same composition throughout. Many solutions are a mixture of water and some other substance. Not all solutions are acids. Some are bases and some are neither acids nor bases. To understand acids and bases, you need to know more about pure water.
In pure water (such as distilled water), a tiny fraction of water molecules naturally breaks down to form ions. An ion is an electrically charged atom or molecule. The breakdown of water is represented by the chemical equation:
2 H2O → H3O+ + OH-
The products of this reaction are a hydronium ion (H3O+) and a hydroxide ion (OH-). The hydroxide ion, which has a negative charge, forms when a water molecule gives up a positively charged hydrogen ion (H+). The hydronium ion, which has a positive charge, forms when another water molecule accepts the hydrogen ion.
Acidity and pH
The concentration of hydronium ions in a solution is known as acidity. In pure water, the concentration of hydronium ions is very low; only about one in ten million water molecules naturally breaks down to form a hydronium ion. As a result, pure water is essentially neutral. Acidity is measured on a scale called pH, as shown in Figure 3.12.2. Pure water has a pH of 7, so the point of neutrality on the pH scale is 7.
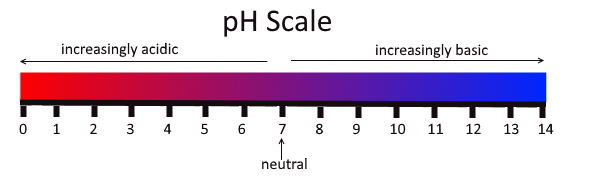
This pH scale shows the acidity of many common substances. The lower the pH value, the more acidic a substance is.
Acids
If a solution has a higher concentration of hydronium ions than pure water, it has a pH lower than 7. A solution with a pH lower than 7 is called an acid. As the hydronium ion concentration increases, the pH value decreases. Therefore, the more acidic a solution is, the lower its pH value is.
Did you ever taste vinegar? Like other acids, it tastes sour. Stronger acids can be harmful to organisms. Even stomach acid would eat through the stomach if it were not lined with a layer of mucus. Strong acids can also damage materials, even hard materials such as glass.
Bases
If a solution has a lower concentration of hydronium ions than pure water, it has a pH higher than 7. A solution with a pH higher than 7 is called a base. Bases, such as baking soda, have a bitter taste. Like strong acids, strong bases can harm organisms and damage materials. For example, lye can burn the skin, and bleach can remove the colour from clothing.
Buffers
A buffer is a solution that can resist changes in pH. Buffers are able to maintain a certain pH by by absorbing any H+ or OH- ions added to the solution. Buffers are extremely important in biological systems in order to maintain a pH conducive to life. Bicarbonate is an example of a buffer which is used to maintain pH of the blood. In this buffering system, if blood becomes too acidic, carbonic acid will convert to carbon dioxide and water. If the blood becomes too basic, carbonic acid will convert to bicarbonate and H+ ions:
CO2 + H2O ↔ H2CO3 ↔ HCO3- + H+
Acids, Bases, and Enzymes
Many acids and bases in living things provide the pH that enzymes need. Enzymes are biological catalysts that must work effectively for biochemical reactions to occur. Most enzymes can do their job only at a certain level of acidity. Cells secrete acids and bases to maintain the proper pH for enzymes to do their work.
Every time you digest food, acids and bases are at work in your digestive system. Consider the enzyme pepsin, which helps break down proteins in the stomach. Pepsin needs an acidic environment to do its job. The stomach secretes a strong acid called hydrochloric acid that allows pepsin to work. When stomach contents enter the small intestine, the acid must be neutralized, because enzymes in the small intestine need a basic environment in order to work. An organ called the pancreas secretes a base named bicarbonate into the small intestine, and this base neutralizes the acid.
Feature: My Human Body
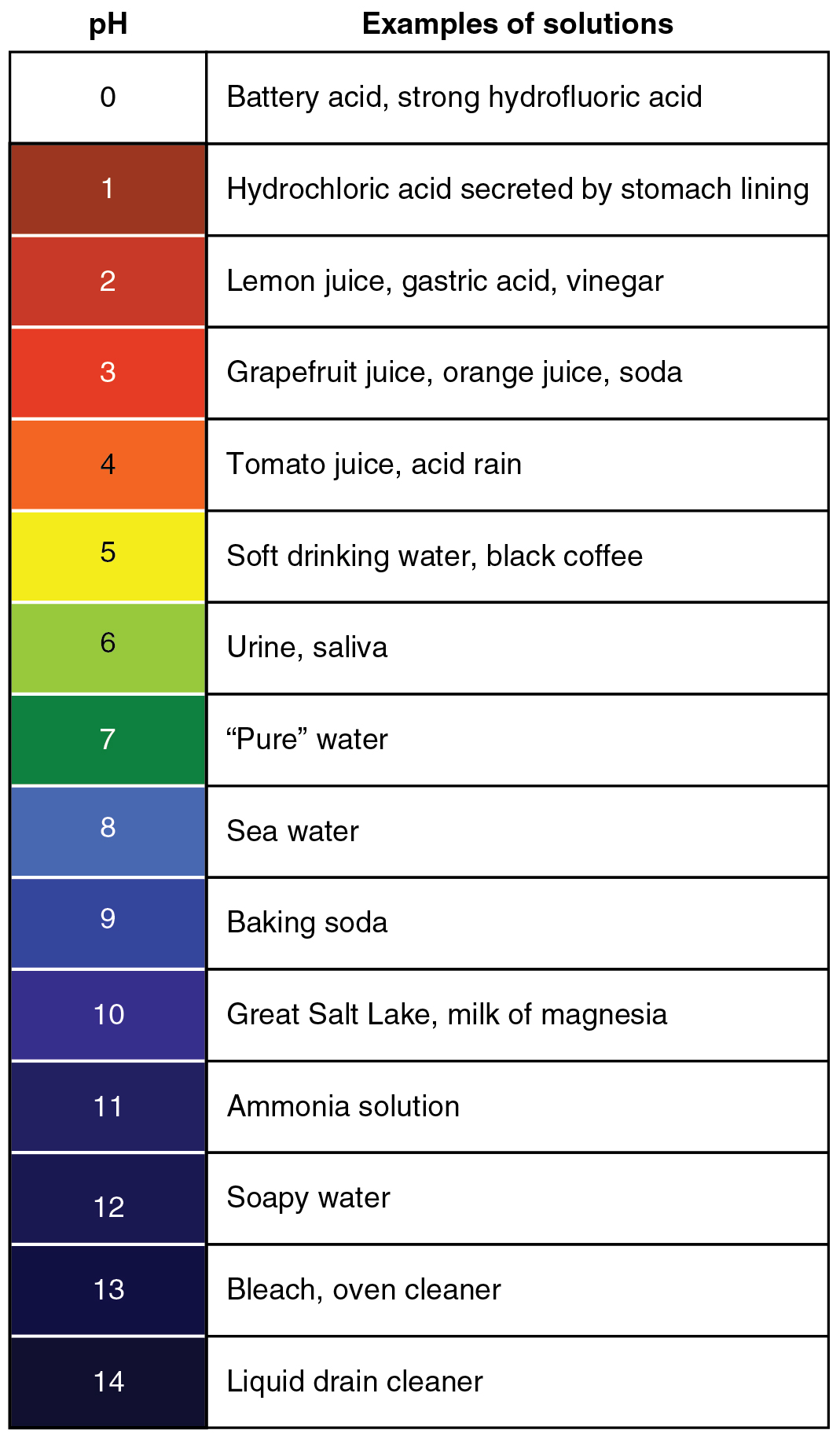
Do you ever have heartburn? The answer is probably "yes." More than 60 million Americans have heartburn at least once a month, and more than 15 million suffer from it on a daily basis. Knowing more about heartburn may help you prevent it or know when it's time to seek medical treatment.
Heartburn doesn't have anything to do with the heart, but it does cause a burning sensation in the vicinity of the chest. Normally, the acid secreted into the stomach remains in the stomach where it is needed to allow pepsin to do its job of digesting proteins. A long tube called the esophagus carries food from the mouth to the stomach. A sphincter, or valve, between the esophagus and stomach opens to allow swallowed food to enter the stomach and then closes to prevent stomach contents from backflowing into the esophagus. If this sphincter is weak or relaxes inappropriately, stomach contents flow into the esophagus. Because stomach contents are usually acidic, this causes the burning sensation known as heartburn. People who are prone to heartburn and suffer from it often may be diagnosed with GERD, which stands for gastroesophageal reflux disease.
GERD — as well as occasional heartburn — often can be improved by dietary and other lifestyle changes that decrease the amount and acidity of reflux from the stomach into the esophagus.
- Some foods and beverages seem to contribute to GERD, so these should be avoided. Problematic foods include chocolate, fatty foods, peppermint, coffee, and alcoholic beverages.
- Decreasing portion size and eating the last meal of the day at least a couple of hours before bedtime may reduce the risk of reflux occurring.
- Smoking tends to weaken the lower esophageal sphincter, so quitting the habit may help control reflux.
- GERD is often associated with being overweight. Losing weight often brings improvement.
- Some people are helped by sleeping with the head of the bed elevated. This allows gravity to help control the backflow of acids into the esophagus from the stomach.
If you have frequent heartburn and lifestyle changes don't help, you may need medication to control the condition. Over-the-counter (OTC) antacids may be all that you need to control the occasional heartburn attack. OTC medications are usually bases that neutralize stomach acids. They may also create bubbles that help block stomach contents from entering the esophagus. For some people, OTC medications are not enough, and prescription medications are instead required for the control of GERD. These prescription medications generally work by inhibiting acid secretion in the stomach.
Be sure to see a doctor if you can't control your heartburn, or you have it often. Untreated GERD not only interferes with quality of life, it may also lead to more serious complications, ranging from esophageal bleeding to esophageal cancer.
3.12 Summary
- A solution is a mixture of two or more substances that has the same composition throughout. Many solutions consist of water and one or more dissolved substances.
- Acidity is a measure of the hydronium ion concentration in a solution. Pure water has a very low concentration and a pH of 7, which is the point of neutrality on the pH scale.
- Acids have a higher hydronium ion concentration than pure water and a pH lower than 7. Bases have a lower hydronium ion concentration than pure water and a pH higher than 7.
- Many acids and bases in living things are secreted to provide the proper pH for enzymes to work properly. Enzymes are the biological catalysts (like pepsin) needed to digest protein in the stomach. Pepsin requires an acidic environment.
3.12 Review Questions
-
- What is a solution?
- Define acidity.
- Explain how acidity is measured.
- Compare and contrast acids and bases.
- Hydrochloric acid is secreted by the stomach to provide an acidic environment for the enzyme pepsin. What is the pH of this acid? How strong of an acid is it compared with other acids?
- Define an ion. Identify the ions in the equation below, and explain what makes them ions:
- 2 H2O → H3O+ + OH-
- Explain why the pancreas secretes bicarbonate into the small intestine.
- Do you think pepsin would work in the small intestine? Why or why not?
- You may have mixed vinegar and baking soda and noticed that they bubble and react with each other. Explain why this happens. Explain also what happens to the pH of this solution after you mix the vinegar and baking soda.
- Pregnancy hormones can cause the lower esophageal sphincter to relax. What effect do you think this has on pregnant women? Explain your answer.
3.12 Explore More
https://www.youtube.com/watch?v=rIvEvwViJGk&feature=youtu.be
pH and Buffers by Bozeman Science, 2014.
https://www.youtube.com/watch?v=DupXDD87oHc&feature=youtu.be
The strengths and weaknesses of acids and bases - George Zaidan and Charles Morton, TED-Ed, 2013.
Attributions
Figure 3.12.1
Leaky battery by Carbon Arc on Flickr is used under a CC BY-NC-SA 2.0 (https://creativecommons.org/licenses/by-nc-sa/2.0/) license.
Figure 3.12.2
PH_Scale by Christinelmiller on Wikimedia Commons is used under a © CC0 1.0 (https://creativecommons.org/publicdomain/zero/1.0/) public domain dedication license.
Figure 3.12.3
Ph scale with examples by OpenStax College, on Wikimedia Commons, is used under a CC BY 3.0 (https://creativecommons.org/licenses/by/3.0) license.
Figure 3.12.4
GERD by BruceBlaus on Wikimedia Commons is used under a CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0) license.
References
Betts, J.G., Young, K.A., Wise, J.A., Johnson, E., Poe, B., Kruse, D.H., Korol, O., Johnson, J.E., Womble, M., DeSaix, P. (2013, April 25). Figure 26.15 The pH Scale [digital image]. In Anatomy and Physiology. OpenStax. https://openstax.org/books/anatomy-and-physiology/pages/26-4-acid-base-balance
Bozeman Science. (2014, February 22). pH and buffers. YouTube. https://www.youtube.com/watch?v=rIvEvwViJGk&feature=youtu.be
TED-Ed. (2013, October 24). The strengths and weaknesses of acids and bases - George Zaidan and Charles Morton. YouTube. https://www.youtube.com/watch?v=DupXDD87oHc&feature=youtu.be
Created by CK-12 Foundation/Adapted by Christine Miller
Figure 18.10.1 Families all have something in common.
Family Portrait
What do all these families (Figure 18.10.1) have in common? They were born! Every person on this planet was conceived, carried in utero and then born. While families come in all shapes, sizes and styles, we all came into existence in the same way. Virtually all human societies past and present — value having children. Indeed, for many people, parenthood is an important life goal. Unfortunately, some people are unable to achieve that goal because of infertility.
What Is Infertility?
Infertility is the inability of a sexually mature adult to reproduce by natural means. For scientific and medical purposes, infertility is generally defined as the failure to achieve a successful pregnancy after at least one year of regular, unprotected sexual intercourse. Infertility may be primary or secondary. Primary infertility applies to cases in which an individual has never achieved a successful pregnancy. Secondary infertility applies to cases in which an individual has had at least one successful pregnancy, but fails to achieve another after trying for at least a year. Infertility is a common problem. The government of Canada reported that in 2019, 16% of Canadian couples experience infertility, a number which has doubled since the 1980s. If you look around at the couples you know, that means that almost 1 in 6 of them are having issues with fertility.
Causes of Infertility
Pregnancy is the result of a multi-step process. In order for a normal pregnancy to occur, a woman must release an ovum from one of her ovaries, the ovum must go through an oviduct, a man’s sperm must fertilize the ovum as it passes through the oviduct, and then the resulting zygote must implant in the uterus. If there is a problem with any of these steps, infertility can result.
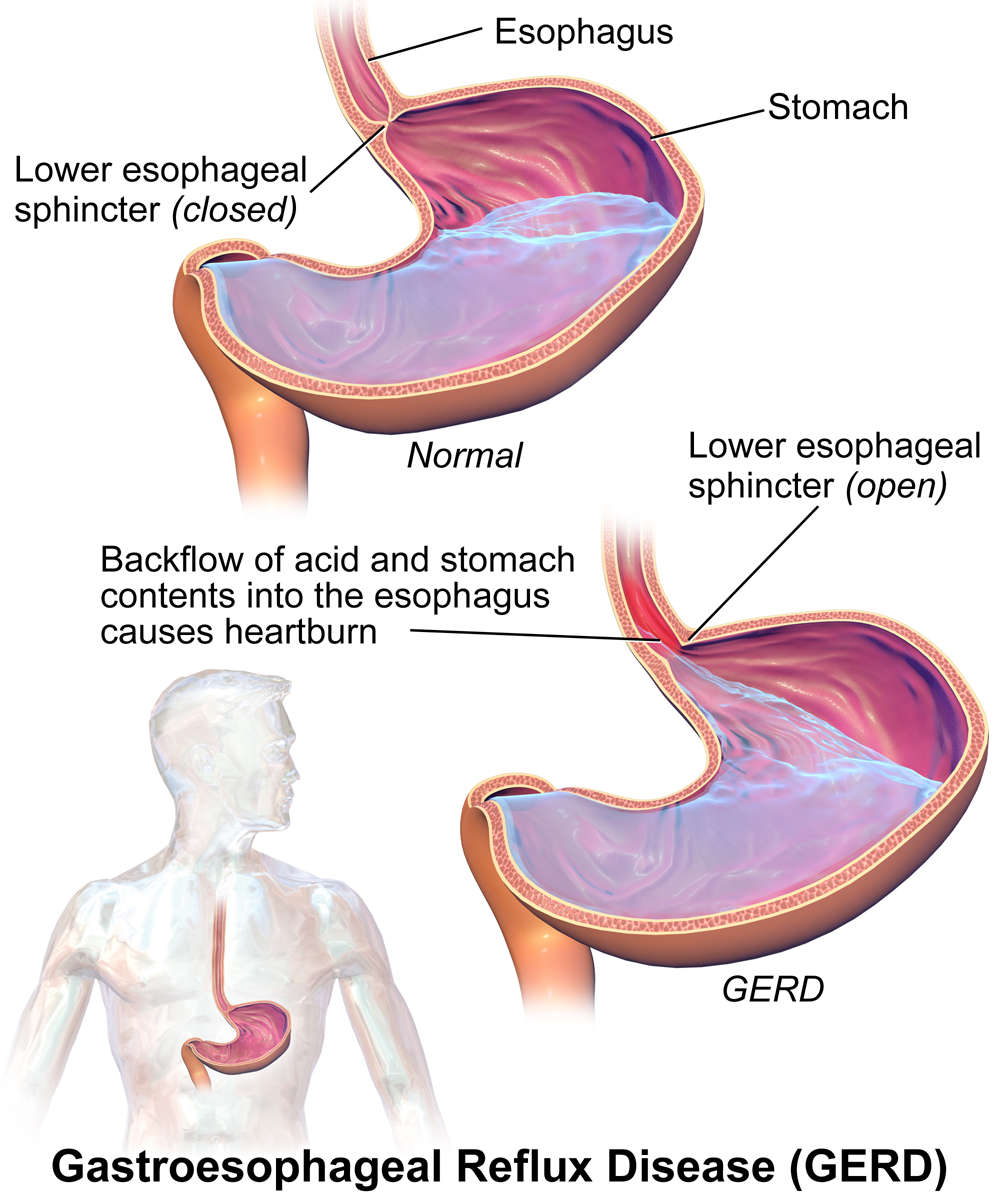
A couple’s infertility may be due to a problem with either the male or the female partner. As shown in the circle graph below (Figure 18.10.2), about 40% of infertility cases are due to female infertility, and about 30% are due to male infertility. The remaining 30% of cases are due to a combination of male and female problems or unknown causes.
Causes of Male Infertility
Male infertility occurs when there are no, or too few, sperm, or when the sperm are not healthy and motile and cannot travel through the female reproductive tract to fertilize an egg. A common cause of inadequate numbers or motility of sperm is varicocele, which is enlargement of blood vessels in the scrotum. This may raise the temperature of the testes and adversely affect sperm production. In other cases, there is no problem with the sperm, but there is a blockage in the male reproductive tract that prevents the sperm from being ejaculated.
Factors that increase a man’s risk of infertility include heavy alcohol use, drug abuse, cigarette smoking, exposure to environmental toxins (such as pesticides or lead), certain medications, serious diseases (such as kidney disease), and radiation or chemotherapy for cancer. Another risk factor is advancing age. Male fertility normally peaks in the mid-twenties and gradually declines after about age 40, although it may never actually drop to zero.
Causes of Female Infertility
Female infertility generally occurs due to one of two problems: failure to produce viable ova by the ovaries, or structural problems in the oviducts or uterus. The most common cause of female infertility is a problem with ovulation. Without ovulation, there are no ova to be fertilized. Anovulatory cycles (menstrual cycles in which ovulation does not occur) may be associated with no or irregular menstrual periods, but even regular menstrual periods may be anovulatory for a variety of reasons. The most common cause of anovulatory cycles is polycystic ovary syndrome (PCOS), which causes hormone imbalances that can interfere with normal ovulation. Another relatively common cause of anovulation is primary ovarian insufficiency. In this condition, the ovaries stop working normally and producing viable eggs at a relatively early age, generally before the age of 40.
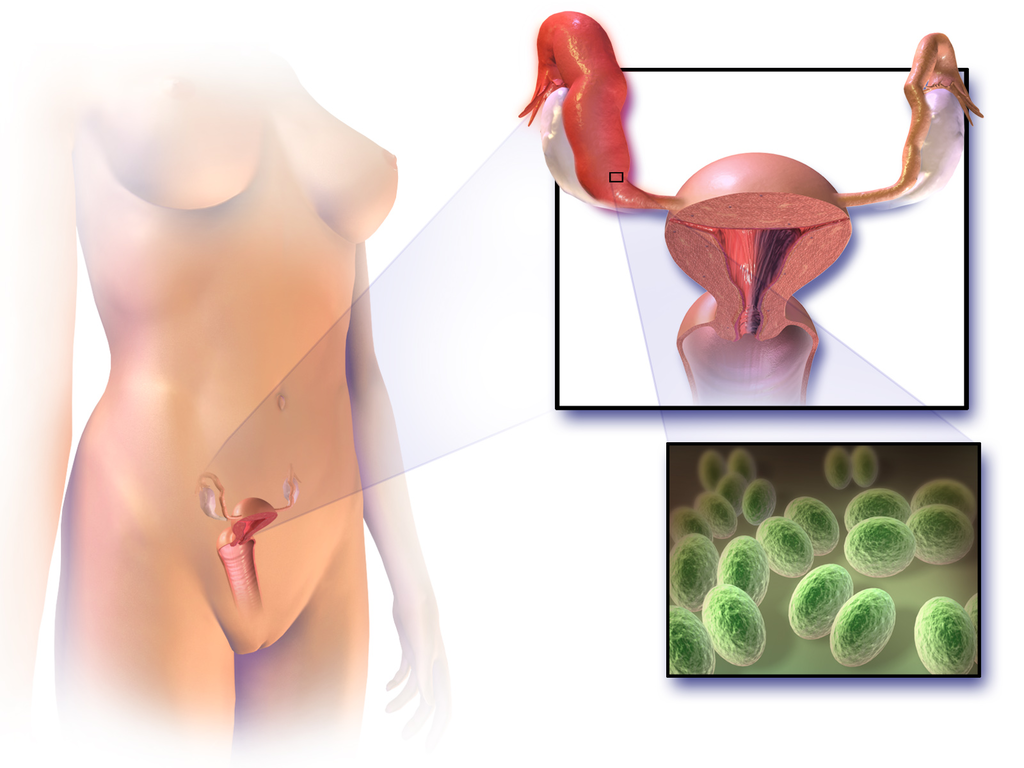
Structural problems with the oviducts or uterus are less common causes of female infertility. The oviducts may be blocked as a result of endometriosis. Another possible cause is pelvic inflammatory disease, which occurs when sexually transmitted infections spread to the oviducts or other female reproductive organs (see Figure 18.10.3). The infection may lead to scarring and blockage of the oviducts. If an ovum is produced and the oviducts are functioning — and a woman has a condition such as uterine fibroids — implantation in the uterus may not be possible. Uterine fibroids are non-cancerous clumps of tissue and muscle that form on the walls of the uterus.
Factors that increase a woman’s risk of infertility include tobacco smoking, excessive use of alcohol, stress, poor diet, strenuous athletic training, and being overweight or underweight. Advanced age is even more problematic for females than males. Female fertility normally peaks in the mid-twenties, and continuously declines after age 30 and until menopause around the age of 52, after which the ovary no longer releases eggs. About 1/3 of couples in which the woman is over age 35 have fertility problems. In older women, more cycles are likely to be anovulatory, and the eggs may not be as healthy.
Diagnosing Causes of Infertility
Diagnosing the cause(s) of a couple’s infertility often requires testing both the man and the woman for potential problems. In men, the semen is likely to be examined for the number, shape, and motility of sperm. If problems are found with sperm, further studies are likely to be done, such as medical imaging to look for structural problems with the testes or ducts.
In women, the first step is most often determining whether ovulation is occurring. This can be done at home by carefully monitoring body temperature (it rises slightly around the time of ovulation) or using a home ovulation test kit, which is available over the counter at most drugstores. Whether or not ovulation is occurring can also be detected with blood tests or ultrasound imaging of the ovaries. If ovulation is occurring normally, then the next step may be an X-ray of the oviducts and uterus to see if there are any blockages or other structural problems. Another approach to examining the female reproductive tract for potential problems is laparoscopy. In this surgical procedure, a tiny camera is inserted into the woman’s abdomen through a small incision. This allows the doctor to directly inspect the reproductive organs.
Treating Infertility
Infertility often can be treated successfully. The type of treatment depends on the cause of infertility.
Treating Male Infertility
Medical problems that interfere with sperm production may be treated with medications or other interventions that may lead to the resumption of normal sperm production. If, for example, an infection is interfering with sperm production, then antibiotics that clear up the infection may resolve the problem. If there is a blockage in the male reproductive tract that prevents the ejaculation of sperm, surgery may be able to remove the blockage. Alternatively, the man’s sperm may be removed from his body and then used for artificial insemination of his partner. In this procedure, the sperm are injected into the woman’s reproductive tract.
Treating Female Infertility
In females, it may be possible to correct blocked Fallopian tubes or uterine fibroids with surgery. Ovulation problems, on the other hand, are usually treated with hormones that act either on the pituitary gland or on the ovaries. Hormonal treatments that stimulate ovulation often result in more than one egg being ovulated at a time, thus increasing the chances of a woman having twins, triplets, or even higher multiple births. Multiple fetuses are at greater risk of being born too early or having health and developmental problems. The mother is also at greater risk of complications arising during pregnancy. Therefore, the possibility of multiple fetuses should be weighed in making a decision about this type of infertility treatment.
Assisted Reproductive Technology
Some cases of infertility are treated with assisted reproductive technology (ART). This is a collection of medical procedures in which ova are removed from the woman’s body and sperm are taken from the man’s body to be manipulated in ways that increase the chances of fertilization occurring. The eggs and sperm may be injected into one of the woman’s oviducts for fertilization to take place in vivo (in the body). More commonly, however, the eggs and sperm are mixed together outside the body so fertilization takes place in vitro (in a test tube or dish in a lab). The latter approach is illustrated in Figure 18.10.4. With in vitro fertilization, the fertilized eggs may be allowed to develop into embryos before being placed in the woman’s uterus.
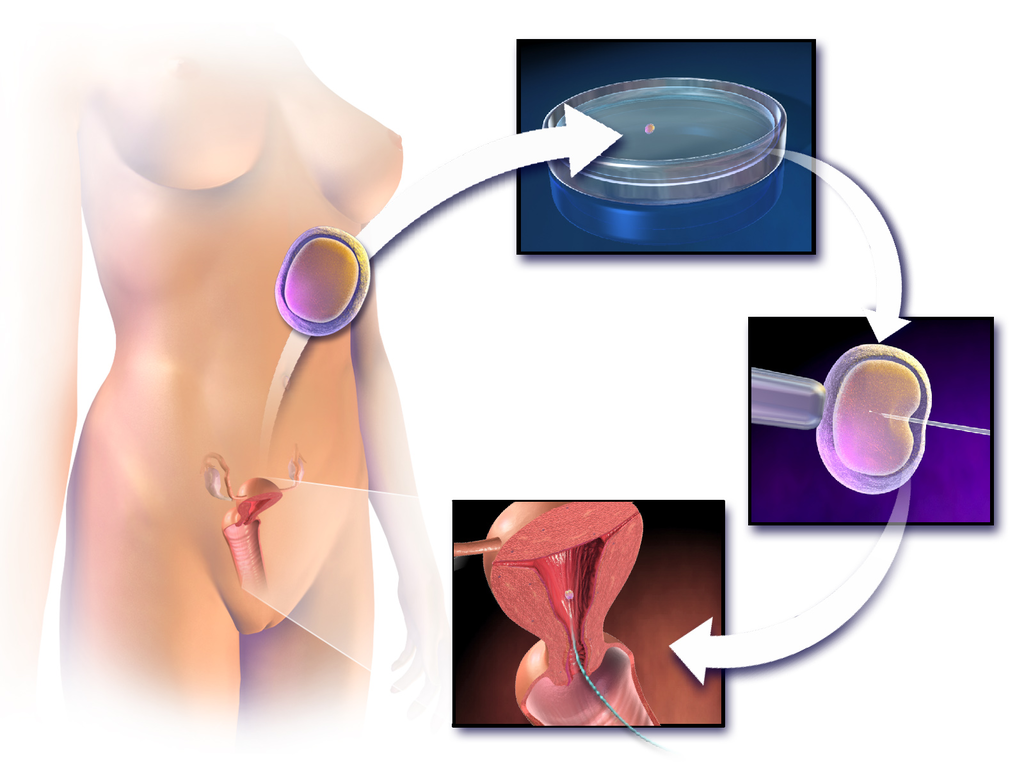
ART has about a 40% chance of leading to a live birth in women under the age of 35, but only about a 20%t chance of success in women over the age of 35. Some studies have found a higher-than-average risk of birth defects in children produced by ART procedures, but this may be due to the generally higher ages of the parent — not the technologies used.
Other Approaches
Other approaches for certain causes of infertility include the use of a surrogate mother, a gestational carrier, or sperm donation.
- A surrogate mother is a woman who agrees to become pregnant using the man’s sperm and her own egg. The child, who will be the biological offspring of the surrogate and the male partner, is given up at birth for adoption by the couple. Surrogacy might be selected by women with no eggs or unhealthy eggs. A woman who carries a mutant gene for a serious genetic disorder might choose this option to ensure that the defective gene is not passed on to the offspring.
- A gestational carrier is a woman who agrees to receive a transplanted embryo from a couple and carry it to term. The child, who will be the biological offspring of the couple, is given to the parents at birth. A gestational carrier might be used by women who have normal ovulation but no uterus, or who cannot safely carry a fetus to term because of a serious health problem (such as kidney disease or cancer).
- Sperm donation is the use of sperm from a fertile man (generally through artificial insemination) for cases in which the male partner in a couple is infertile, or in which a woman seeks to become pregnant without a male partner. A lesbian couple may use donated sperm to enable one of them to become pregnant and have a child. Sperm can be obtained from a sperm bank, which buys and stores sperm for artificial insemination, or a male friend or other individual may donate sperm to a specific woman.
Social and Ethical Issues Relating to Infertility
For people who have a strong desire for children of their own, infertility may lead to deep disappointment and depression. Individuals who are infertile may even feel biologically inadequate. Partners in infertile couples may argue and feel resentment toward each other, and married couples may get divorced because of infertility. Infertility treatments — especially ART procedures — are generally time-consuming and expensive. The high cost of the treatments can put them out of financial reach of many couples.
Ethical Concerns
Some people question whether the allocation of medical resources to infertility treatments is justified, and whether the resources could be better used in other ways. The status of embryos that are created in vitro and then not used for a pregnancy is another source of debate. Some people oppose their destruction on religious grounds, and couples may sometimes argue about what should be done with their extra embryos. Ethical issues are also raised by procedures that increase the chances of multiple births, because of the medical and developmental risks associated with multiple births.
Infertility in Developing Countries
Infertility is an under-appreciated problem in the poorer nations of the world, because of assumptions about overpopulation problems and high birth rates in developing countries. In fact, infertility is at least as great a problem in developing as in developed countries. High rates of health problems and inadequate health care in the poorer nations increase the risk of infertility. At the same time, infertility treatments are usually not available — or are far too expensive — for the vast majority of people who may need them. In addition, in many developing countries, the production of children is highly valued. Children may be needed for family income generation and economic security of the elderly. It is not uncommon for infertility to lead to social stigmatization, psychological problems, and abandonment by spouses.
18.10 Summary
- Infertility is the inability of a sexually mature adult to reproduce by natural means. It is defined scientifically and medically as the failure to achieve a successful pregnancy after at least one year of regular, unprotected sexual intercourse.
- About 40% of infertility in couples is due to female infertility, and another 30% is due to male infertility. In the remaining cases, a couple’s infertility is due to problems in both partners, or to unknown causes.
- Male infertility occurs when there are no, or too few, healthy, motile sperm. This may be caused by problems with spermatogenesis, or by blockage of the male reproductive tract that prevents sperm from being ejaculated. Risk factors for male infertility include heavy alcohol use, smoking, certain medications, and advancing age, to name just a few.
- Female infertility occurs due to failure to produce viable ova by the ovaries, or structural problems in the oviducts or uterus. Polycystic ovary syndrome (PCOS) is the most common cause of failure to produce viable ova. Endometriosis and uterine fibroids are possible causes of structural problems in the oviducts and uterus. Risk factors for female infertility include smoking, stress, poor diet, and older age, among others.
- Diagnosing the cause(s) of a couple’s infertility generally requires testing both the man and the woman for potential problems. For men, semen is likely to be examined for adequate numbers of healthy, motile sperm. For women, signs of ovulation are monitored, for example, with an ovulation test kit or ultrasound of the ovaries. For both partners, the reproductive tract may be medically imaged to look for blockages or other abnormalities.
- Treatments for infertility depend on the cause. For example, if a medical problem is interfering with sperm production, medication may resolve the underlying problem so sperm production is restored. Blockages in either the male or the female reproductive tract can often be treated surgically. If there are problems with ovulation, hormonal treatments may stimulate ovulation.
- Some cases of infertility are treated with assisted reproductive technology (ART). This is a collection of medical procedures in which ova and sperm are taken from the couple and manipulated in a lab to increase the chances of fertilization occurring and an embryo forming. Other approaches for certain causes of infertility include the use of a surrogate mother, gestational carrier, or sperm donation.
- Infertility can negatively impact a couple socially and psychologically, and it may be a major cause of marital friction or even divorce. Infertility treatments may raise ethical issues relating to the costs of the procedures and the status of embryos that are created in vitro, but not used for pregnancy. Infertility is an under-appreciated problem in developing countries, where birth rates are high and children have high economic — as well as social — value. In these countries, poor health care is likely to lead to more problems with infertility and fewer options for treatment.
18.10 Review Questions
- What is infertility? How is infertility defined scientifically and medically?
- What percentage of infertility in couples is due to male infertility? What percentage is due to female infertility?
- Identify causes of and risk factors for male infertility.
- Identify causes of and risk factors for female infertility.
- How are causes of infertility in couples diagnosed?
- How is infertility treated?
- Discuss some of the social and ethical issues associated with infertility or its treatment.
- Why is infertility an under-appreciated problem in developing countries?
- Describe two similarities between causes of male and female infertility.
- Explain the difference between males and females in terms of how age affects fertility.
-
- Do you think that taking medication to stimulate ovulation is likely to improve fertility in cases where infertility is due to endometriosis? Explain your answer.
18.10 Explore More
https://youtu.be/P27waC05Hdk
How in vitro fertilization (IVF) works - Nassim Assefi and Brian A. Levine, TED-Ed, 2015
https://youtu.be/6BBmMtVfZ4Y
A journey through infertility -- over terror's edge | Camille Preston | TEDxBeaconStreet, TEDx Talks, 2014.
https://youtu.be/iqA8uAjvEdM
Smoking Marijuana May Lower Sperm Count by 33%, David Pakman Show, 2015.
https://youtu.be/V6-v4eF9dyA
ivf embryo developing over 5 days by fertility Dr Raewyn Teirney, Fertility Specialist Sydney, 2014.
https://youtu.be/4Khn_z9FPmU
Homosexuality: It's about survival - not sex | James O'Keefe | TEDxTallaght, 2016.
Attributions
Figure 18.10.1
- Gay Pride Parade NYC 2013 - Happy Family by Bob Jagendorf on Flickr is used under a CC BY-NC 2.0 (https://creativecommons.org/licenses/by-nc/2.0/) license.
- #beaches #summer #family #blue #water by Jove Duero on Unsplash is used under the Unsplash License (https://unsplash.com/license).
- Photograph of five men near outdoor by Dollar Gill on Unsplash is used under the Unsplash License (https://unsplash.com/license).
- Família by Laercio Cavalcanti on Unsplash is used under the Unsplash License (https://unsplash.com/license).
- Happiness 🙂 by Ashwini Chaudhary on Unsplash is used under the Unsplash License (https://unsplash.com/license).
Figure 18.10.2
Causes of infertility in Canada by Christine Miller is in the Public Domain (https://creativecommons.org/publicdomain/mark/1.0/).
Figure 18.10.3
1024px-Blausen_0719_PelvicInflammatoryDisease by BruceBlaus on Wikimedia Commons is used under a CC BY 3.0 (https://creativecommons.org/licenses/by/3.0) license.
Figure 18.10.4
1024px-Blausen_0060_AssistedReproductiveTechnology by BruceBlaus on Wikimedia Commons is used under a CC BY 3.0 (https://creativecommons.org/licenses/by/3.0) license.
References
Blausen.com Staff. (2014). Medical gallery of Blausen Medical 2014. WikiJournal of Medicine 1 (2). DOI:10.15347/wjm/2014.010. ISSN 2002-4436.
David Pakman Show. (2015, September 1). Smoking marijuana may lower sperm count by 33%. YouTube. https://www.youtube.com/watch?v=iqA8uAjvEdM
Fertility Specialist Sydney. (2014, April 11). ivf embryo developing over 5 days by fertility Dr Raewyn Teirney. YouTube. https://www.youtube.com/watch?v=V6-v4eF9dyA&t=5s
Public Health Agency of Canada. (2019, May 28). Fertility. Government of Canada. https://www.canada.ca/en/public-health/services/fertility/fertility.html
TED-Ed. (2015, May 7). How in vitro fertilization (IVF) works - Nassim Assefi and Brian A. Levine. YouTube. https://www.youtube.com/watch?v=P27waC05Hdk&t=4s
TEDx Talks. (2014, June 26). A journey through infertility -- over terror's edge | Camille Preston | TEDxBeaconStreet. YouTube. https://www.youtube.com/watch?v=6BBmMtVfZ4Y&t=2s
TEDx Talks. (2016, November 15). Homosexuality: It's about survival - not sex | James O'Keefe | TEDxTallaght. YouTube. https://www.youtube.com/watch?v=4Khn_z9FPmU&t=1s
Created by CK-12 Foundation/Adapted by Christine Miller

Feel the Burn
The person in Figure 10.3.1 is no doubt feeling the burn — sunburn, that is. Sunburn occurs when the outer layer of the skin is damaged by UV light from the sun or tanning lamps. Some people deliberately allow UV light to burn their skin, because after the redness subsides, they are left with a tan. A tan may look healthy, but it is actually a sign of skin damage. People who experience one or more serious sunburns are significantly more likely to develop skin cancer. Natural pigment molecules in the skin help protect it from UV light damage. These pigment molecules are found in the layer of the skin called the epidermis.
What is the Epidermis?
The epidermis is the outer of the two main layers of the skin. The inner layer is the dermis. It averages about 0.10 mm thick, and is much thinner than the dermis. The epidermis is thinnest on the eyelids (0.05 mm) and thickest on the palms of the hands and soles of the feet (1.50 mm). The epidermis covers almost the entire body surface. It is continuous with — but structurally distinct from — the mucous membranes that line the mouth, anus, urethra, and vagina.
Structure of the Epidermis
There are no blood vessels and very few nerve cells in the epidermis. Without blood to bring epidermal cells oxygen and nutrients, the cells must absorb oxygen directly from the air and obtain nutrients via diffusion of fluids from the dermis below. However, as thin as it is, the epidermis still has a complex structure. It has a variety of cell types and multiple layers.
Cells of the Epidermis
There are several different types of cells in the epidermis. All of the cells are necessary for the important functions of the epidermis.
- The epidermis consists mainly of stacks of keratin-producing epithelial cells called keratinocytes. These cells make up at least 90 per cent of the epidermis. Near the top of the epidermis, these cells are also called squamous cells.
- Another eight per cent of epidermal cells are melanocytes. These cells produce the pigment melanin that protects the dermis from UV light.
- About one per cent of epidermal cells are Langerhans cells. These are immune system cells that detect and fight pathogens entering the skin.
- Less than one per cent of epidermal cells are Merkel cells, which respond to light touch and connect to nerve endings in the dermis.
Layers of the Epidermis
The epidermis in most parts of the body consists of four distinct layers. A fifth layer occurs in the palms of the hands and soles of the feet, where the epidermis is thicker than in the rest of the body. The layers of the epidermis are shown in Figure 10.3.2, and described in the following text.
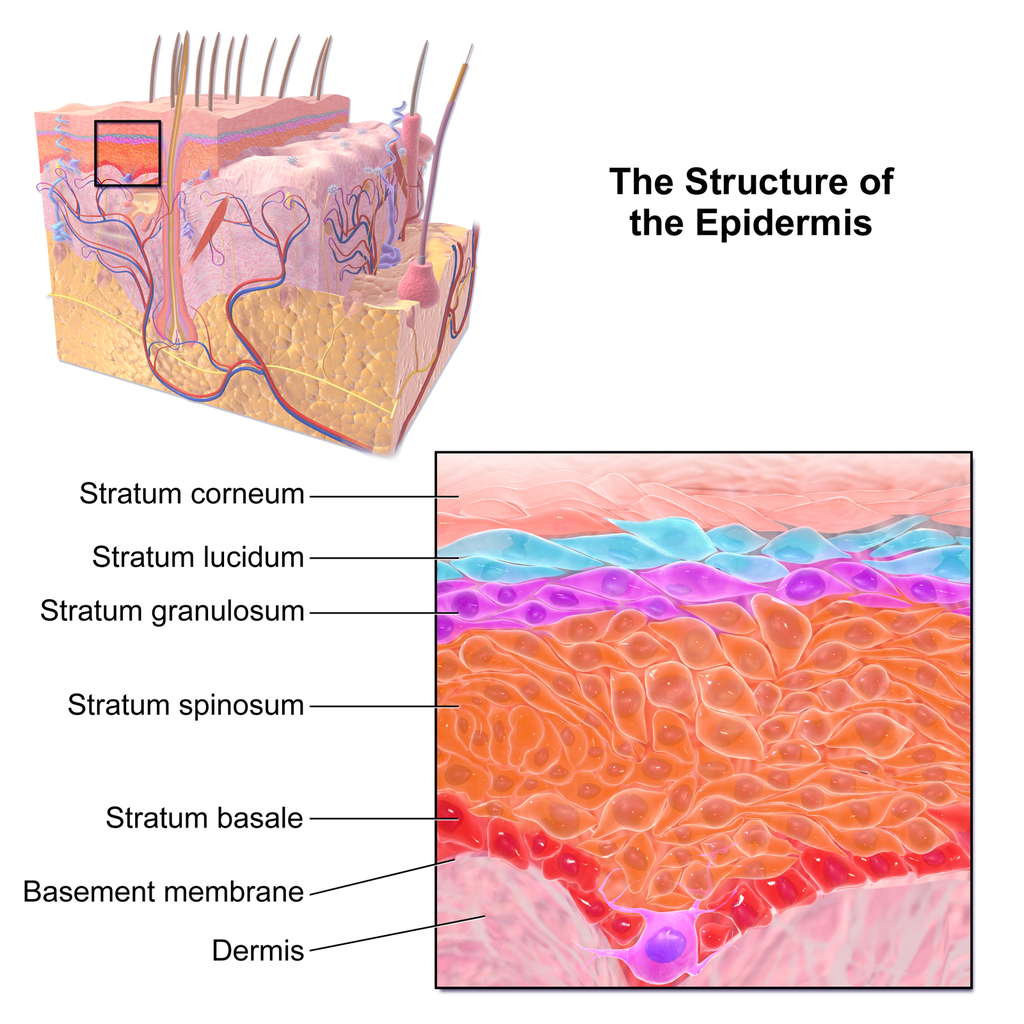
Stratum Basale
The stratum basale is the innermost (or deepest) layer of the epidermis. It is separated from the dermis by a membrane called the basement membrane. The stratum basale contains stem cells — called basal cells — which divide to form all the keratinocytes of the epidermis. When keratinocytes first form, they are cube-shaped and contain almost no keratin. As more keratinocytes are produced, previously formed cells are pushed up through the stratum basale. Melanocytes and Merkel cells are also found in the stratum basale. The Merkel cells are especially numerous in touch-sensitive areas, such as the fingertips and lips.
Stratum Spinosum
Just above the stratum basale is the stratum spinosum. This is the thickest of the four epidermal layers. The keratinocytes in this layer have begun to accumulate keratin, and they have become tougher and flatter. Spiny cellular projections form between the keratinocytes and hold them together. In addition to keratinocytes, the stratum spinosum contains the immunologically active Langerhans cells.
Stratum Granulosum
The next layer above the stratum spinosum is the stratum granulosum. In this layer, keratinocytes have become nearly filled with keratin, giving their cytoplasm a granular appearance. Lipids are released by keratinocytes in this layer to form a lipid barrier in the epidermis. Cells in this layer have also started to die, because they are becoming too far removed from blood vessels in the dermis to receive nutrients. Each dying cell digests its own nucleus and organelles, leaving behind only a tough, keratin-filled shell.
Stratum Lucidum
Only on the palms of the hands and soles of the feet, the next layer above the stratum granulosum is the stratum lucidum. This is a layer consisting of stacks of translucent, dead keratinocytes that provide extra protection to the underlying layers.
Stratum Corneum
The uppermost layer of the epidermis everywhere on the body is the stratum corneum. This layer is made of flat, hard, tightly packed dead keratinocytes that form a waterproof keratin barrier to protect the underlying layers of the epidermis. Dead cells from this layer are constantly shed from the surface of the body. The shed cells are continually replaced by cells moving up from lower layers of the epidermis. It takes a period of about 48 days for newly formed keratinocytes in the stratum basale to make their way to the top of the stratum corneum to replace shed cells.
Functions of the Epidermis
The epidermis has several crucial functions in the body. These functions include protection, water retention, and vitamin D synthesis.
Protective Functions
The epidermis provides protection to underlying tissues from physical damage, pathogens, and UV light.
Protection from Physical Damage
Most of the physical protection of the epidermis is provided by its tough outer layer, the stratum corneum. Because of this layer, minor scrapes and scratches generally do not cause significant damage to the skin or underlying tissues. Sharp objects and rough surfaces have difficulty penetrating or removing the tough, dead, keratin-filled cells of the stratum corneum. If cells in this layer are pierced or scraped off, they are quickly replaced by new cells moving up to the surface from lower skin layers.
Protection from Pathogens

When pathogens such as viruses and bacteria try to enter the body, it is virtually impossible for them to enter through intact epidermal layers. Generally, pathogens can enter the skin only if the epidermis has been breached, for example by a cut, puncture, or scrape (like the one pictured in Figure 10.3.3). That’s why it is important to clean and cover even a minor wound in the epidermis. This helps ensure that pathogens do not use the wound to enter the body. Protection from pathogens is also provided by conditions at or near the skin surface. These include relatively high acidity (pH of about 5.0), low amounts of water, the presence of antimicrobial substances produced by epidermal cells, and competition with non-pathogenic microorganisms that normally live on the epidermis.
Protection from UV Light
UV light that penetrates the epidermis can damage epidermal cells. In particular, it can cause mutations in DNA that lead to the development of skin cancer, in which epidermal cells grow out of control. UV light can also destroy vitamin B9 (in forms such as folate or folic acid), which is needed for good health and successful reproduction. In a person with light skin, just an hour of exposure to intense sunlight can reduce the body’s vitamin B9 level by 50 per cent.
Melanocytes in the stratum basale of the epidermis contain small organelles called melanosomes, which produce, store, and transport the dark brown pigment melanin. As melanosomes become full of melanin, they move into thin extensions of the melanocytes. From there, the melanosomes are transferred to keratinocytes in the epidermis, where they absorb UV light that strikes the skin. This prevents the light from penetrating deeper into the skin, where it can cause damage. The more melanin there is in the skin, the more UV light can be absorbed.
Water Retention
Skin's ability to hold water and not lose it to the surrounding environment is due mainly to the stratum corneum. Lipids arranged in an organized way among the cells of the stratum corneum form a barrier to water loss from the epidermis. This is critical for maintaining healthy skin and preserving proper water balance in the body.
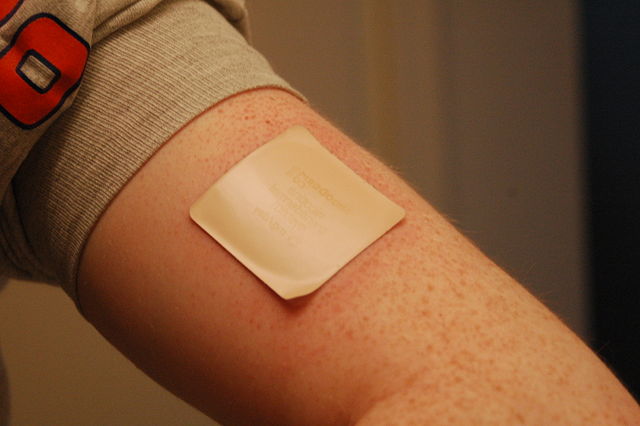
Although the skin is impermeable to water, it is not impermeable to all substances. Instead, the skin is selectively permeable, allowing certain fat-soluble substances to pass through the epidermis. The selective permeability of the epidermis is both a benefit and a risk.
- Selective permeability allows certain medications to enter the bloodstream through the capillaries in the dermis. This is the basis of medications that are delivered using topical ointments, or patches (see Figure 10.3.4) that are applied to the skin. These include steroid hormones, such as estrogen (for hormone replacement therapy), scopolamine (for motion sickness), nitroglycerin (for heart problems), and nicotine (for people trying to quit smoking).
- Selective permeability of the epidermis also allows certain harmful substances to enter the body through the skin. Examples include the heavy metal lead, as well as many pesticides.
Vitamin D Synthesis
Vitamin D is a nutrient that is needed in the human body for the absorption of calcium from food. Molecules of a lipid compound named 7-dehydrocholesterol are precursors of vitamin D. These molecules are present in the stratum basale and stratum spinosum layers of the epidermis. When UV light strikes the molecules, it changes them to vitamin D3. In the kidneys, vitamin D3 is converted to calcitriol, which is the form of vitamin D that is active in the body.
What Gives Skin Its Colour?
Melanin in the epidermis is the main substance that determines the colour of human skin. It explains most of the variation in skin colour in people around the world. Two other substances also contribute to skin colour, however, especially in light-skinned people: carotene and hemoglobin.
- The pigment carotene is present in the epidermis and gives skin a yellowish tint, especially in skin with low levels of melanin.
- Hemoglobin is a red pigment found in red blood cells. It is visible through skin as a pinkish tint, mainly in skin with low levels of melanin. The pink colour is most visible when capillaries in the underlying dermis dilate, allowing greater blood flow near the surface.
Hear what Bill Nye has to say about the subject of skin colour in the video here.
Bacteria on Skin
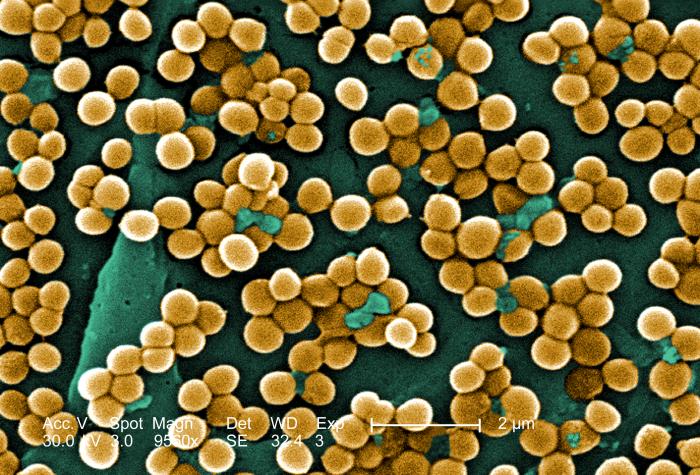
The surface of the human skin normally provides a home to countless numbers of bacteria. Just one square inch of skin normally has an average of about 50 million bacteria. These generally harmless bacteria represent roughly one thousand bacterial species (including the one in Figure 10.3.5) from 19 different bacterial phyla. Typical variations in the moistness and oiliness of the skin produce a variety of rich and diverse habitats for these microorganisms. For example, the skin in the armpits is warm and moist and often hairy, whereas the skin on the forearms is smooth and dry. These two areas of the human body are as diverse to microorganisms as rainforests and deserts are to larger organisms. The density of bacterial populations on the skin depends largely on the region of the skin and its ecological characteristics. For example, oily surfaces, such as the face, may contain over 500 million bacteria per square inch. Despite the huge number of individual microorganisms living on the skin, their total volume is only about the size of a pea.
In general, the normal microorganisms living on the skin keep one another in check, and thereby play an important role in keeping the skin healthy. If the balance of microorganisms is disturbed, however, there may be an overgrowth of certain species, and this may result in an infection. For example, when a patient is prescribed antibiotics, it may kill off normal bacteria and allow an overgrowth of single-celled yeast. Even if skin is disinfected, no amount of cleaning can remove all of the microorganisms it contains. Disinfected areas are also quickly recolonized by bacteria residing in deeper areas (such as hair follicles) and in adjacent areas of the skin.
Feature: Myth vs. Reality
Because of the negative health effects of excessive UV light exposure, it is important to know the facts about protecting the skin from UV light.
Myth |
Reality |
| "Sunblock and sunscreen are just different names for the same type of product. They both work the same way and are equally effective." | Sunscreens and sunblocks are different types of products that protect the skin from UV light in different ways. They are not equally effective. Sunblocks are opaque, so they do not let light pass through. They prevent most of the rays of UV light from penetrating to the skin surface. Sunblocks are generally stronger and more effective than sunscreens. Sunblocks also do not need to be reapplied as often as sunscreens. Sunscreens, in contrast, are transparent once they are applied the skin. Although they can prevent most UV light from penetrating the skin when first applied, the active ingredients in sunscreens tend to break down when exposed to UV light. Sunscreens, therefore, must be reapplied often to remain effective. |
| "The skin needs to be protected from UV light only on sunny days. When the sky is cloudy, UV light cannot penetrate to the ground and harm the skin." | Even on cloudy days, a significant amount of UV radiation penetrates the atmosphere to strike Earth’s surface. Therefore, using sunscreens or sunblocks to protect exposed skin is important even when there are clouds in the sky. |
| "People who have dark skin, such as African Americans, do not need to worry about skin damage from UV light." | No matter what colour skin you have, your skin can be damaged by too much exposure to UV light. Therefore, even dark-skinned people should use sunscreens or sunblocks to protect exposed skin from UV light. |
| "Sunscreens with an SPF (sun protection factor) of 15 are adequate to fully protect the skin from UV light." | Most dermatologists recommend using sunscreens with an SPF of at least 35 for adequate protection from UV light. They also recommend applying sunscreens at least 20 minutes before sun exposure and reapplying sunscreens often, especially if you are sweating or spending time in the water. |
| "Using tanning beds is safer than tanning outside in natural sunlight." | The light in tanning beds is UV light, and it can do the same damage to the skin as the natural UV light in sunlight. This is evidenced by the fact that people who regularly use tanning beds have significantly higher rates of skin cancer than people who do not. It is also the reason that the use of tanning beds is prohibited in many places in people who are under the age of 18, just as youth are prohibited from using harmful substances, such as tobacco and alcohol. |
10.3 Summary
- The epidermis is the outer of the two main layers of the skin. It is very thin, but has a complex structure.
- Cell types in the epidermis include keratinocytes that produce keratin and make up 90 per cent of epidermal cells, melanocytes that produce melanin, Langerhans cells that fight pathogens in the skin, and Merkel cells that respond to light touch.
- The epidermis in most parts of the body consists of four distinct layers. A fifth layer occurs only in the epidermis of the palms of the hands and soles of the feet.
- The innermost layer of the epidermis is the stratum basale, which contains stem cells that divide to form new keratinocytes. The next layer is the stratum spinosum, which is the thickest layer and contains Langerhans cells and spiny keratinocytes. This is followed by the stratum granulosum, in which keratinocytes are filling with keratin and starting to die. The stratum lucidum is next, but only on the palms and soles. It consists of translucent dead keratinocytes. The outermost layer is the stratum corneum, which consists of flat, dead, tightly packed keratinocytes that form a tough, waterproof barrier for the rest of the epidermis.
- Functions of the epidermis include protecting underlying tissues from physical damage and pathogens. Melanin in the epidermis absorbs and protects underlying tissues from UV light. The epidermis also prevents loss of water from the body and synthesizes vitamin D.
- Melanin is the main pigment that determines the colour of human skin. The pigments carotene and hemoglobin, however, also contribute to skin colour, especially in skin with low levels of melanin.
- The surface of healthy skin normally is covered by vast numbers of bacteria representing about one thousand species from 19 phyla. Different areas of the body provide diverse habitats for skin microorganisms. Usually, microorganisms on the skin keep each other in check unless their balance is disturbed.
10.3 Review Questions
- What is the epidermis?
- Identify the types of cells in the epidermis.
- Describe the layers of the epidermis.
-
- State one function of each of the four epidermal layers found all over the body.
- Explain three ways the epidermis protects the body.
- What makes the skin waterproof?
- Why is the selective permeability of the epidermis both a benefit and a risk?
- How is vitamin D synthesized in the epidermis?
- Identify three pigments that impart colour to skin.
- Describe bacteria that normally reside on the skin, and explain why they do not usually cause infections.
- Explain why the keratinocytes at the surface of the epidermis are dead, while keratinocytes located deeper in the epidermis are still alive.
- Which layer of the epidermis contains keratinocytes that have begun to die?
-
- Explain why our skin is not permanently damaged if we rub off some of the surface layer by using a rough washcloth.
10.3 Explore More
https://www.youtube.com/watch?v=27lMmdmy-b8
Jonathan Eisen: Meet your microbes, TED, 2015.
https://www.youtube.com/watch?v=9AcQXnOscQ8
Why Do We Blush?, SciShow, 2014.
https://www.youtube.com/watch?v=_r4c2NT4naQ
The science of skin colour - Angela Koine Flynn, TED-Ed, 2016.
Attributions
Figure 10.3.1
Sunburn by QuinnHK at English Wikipedia on Wikimedia Commons is released into the public domain (https://en.wikipedia.org/wiki/Public_domain).
Figure 10.3.2
Blausen_0353_Epidermis by BruceBlaus on Wikimedia Commons is used under a CC BY 3.0 (https://creativecommons.org/licenses/by/3.0) license.
Figure 10.3.3
Isaac's scraped knee close-up by Alpha on Flickr is used under a CC BY-NC-SA 2.0 (https://creativecommons.org/licenses/by-nc-sa/2.0/) license.
Figure 10.3.4
Nicoderm by RegBarc on Wikimedia Commons is used under a CC BY-SA 3.0 (http://creativecommons.org/licenses/by-sa/3.0/) license. (No machine-readable author provided for original.)
Figure 10.3.5
Staphylococcus aureus bacteria, MRSA by Microbe World on Flickr is used under a CC BY-NC-SA 2.0 (https://creativecommons.org/licenses/by-nc-sa/2.0/) license.
References
Blausen.com staff. (2014). Medical gallery of Blausen Medical 2014. WikiJournal of Medicine 1 (2). DOI:10.15347/wjm/2014.010. ISSN 2002-4436.
Jeff Bone 'n' Pookie. (2020, July 19). Bill Nye the science guy explains we have different skin color. Youtube. https://www.youtube.com/watch?v=zOkj5jgC4sM&feature=youtu.be
SciShow. (2014, July 15). Why do we blush? YouTube. https://www.youtube.com/watch?v=9AcQXnOscQ8
TED. (2015, July 17). Jonathan Eisen: Meet your microbes. YouTube. https://www.youtube.com/watch?v=27lMmdmy-b8
TED-Ed. (2016, February 16). The science of skin color - Angela Koine Flynn. YouTube. https://youtu.be/_r4c2NT4naQ
Created by CK-12 Foundation/Adapted by Christine Miller

Fashion Statement
This colourful hairstyle makes quite a fashion statement. Many people spend a lot of time and money on their hair, even if they don’t have an exceptional hairstyle like this one. Besides its display value, hair actually has important physiological functions.
What is Hair?
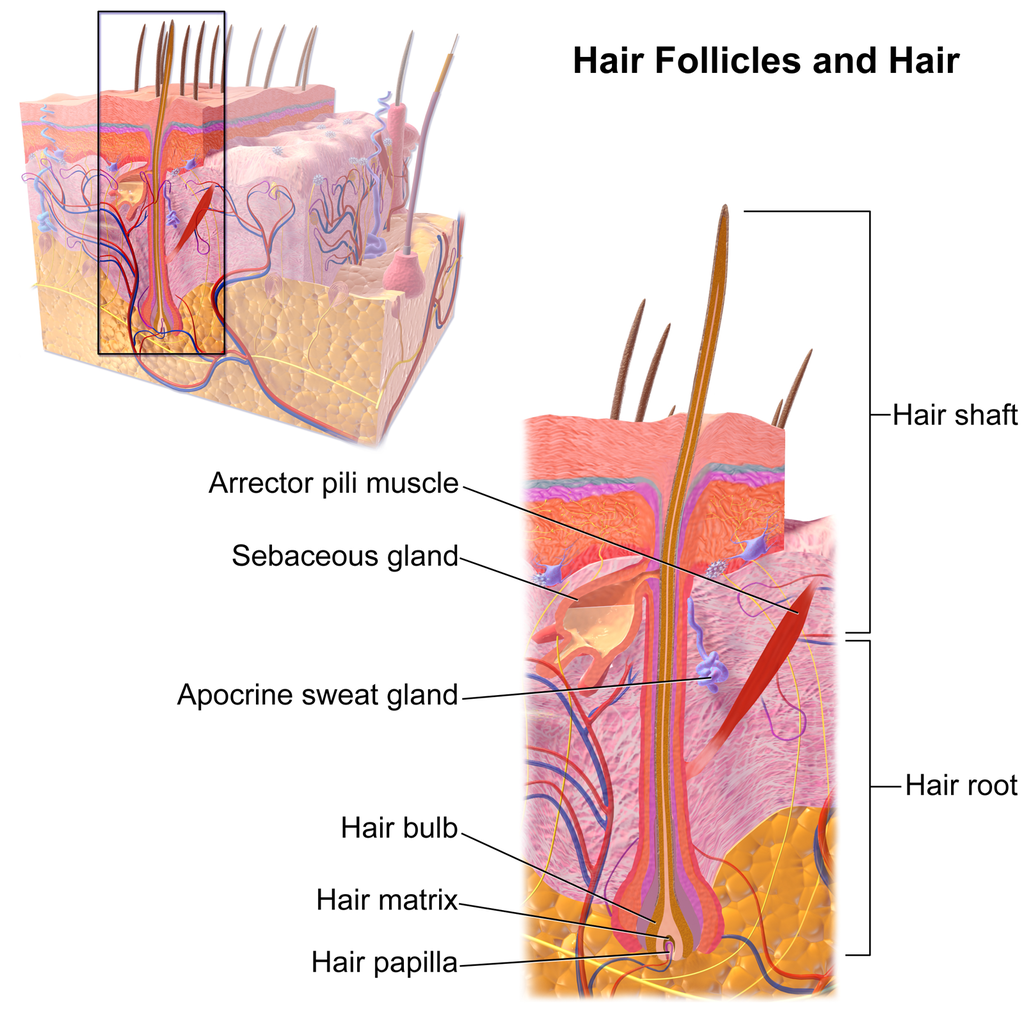
Hair is a filament that grows from a hair follicle in the dermis of the skin. It consists mainly of tightly packed, keratin-filled cells called keratinocytes. The human body is covered with hair follicles, with the exception of a few areas, including the mucous membranes, lips, palms of the hands, and soles of the feet.
Structure of Hair
The part of the hair located within the follicle is called the hair root. The root is the only living part of the hair. The part of the hair that is visible above the surface of the skin is the hair shaft. The shaft of the hair has no biochemical activity and is considered dead.
Follicle and Root
Hair growth begins inside a follicle (see Figure 10.5.2 below). Each hair follicle contains stem cells that can keep dividing, which allows hair to grow. The stem cells can also regrow a new hair after one falls out. Another structure associated with a hair follicle is a sebaceous gland that produces oily sebum. The sebum lubricates and helps to waterproof the hair. A tiny arrector pili muscle is also attached to the follicle. When it contracts, the follicle moves, and the hair in the follicle stands up.
Shaft
The hair shaft is a hard filament that may grow very long. Hair normally grows in length by about half an inch a month. In cross-section, a hair shaft can be divided into three zones, called the cuticle, cortex, and medulla.
- The cuticle (or outer coat) is the outermost zone of the hair shaft. It consists of several layers of flat, thin keratinocytes that overlap one another like shingles on a roof. This arrangement helps the cuticle repel water. The cuticle is also covered with a layer of lipids, just one molecule thick, which increases its ability to repel water. This is the zone of the hair shaft that is visible to the eye.
- The cortex is the middle zone of the hair shaft, and it is also the widest part. The cortex is highly structured and organized, consisting of keratin bundles in rod-like structures. These structures give hair its mechanical strength. The cortex also contains melanin, which gives hair its colour.
- The medulla is the innermost zone of the hair shaft. This is a small, disorganized, and more open area at the center of the hair shaft. The medulla is not always present. When it is present, it contains highly pigmented cells full of keratin.
Characteristics of Hair
Two visible characteristics of hair are its colour and texture. In adult males, the extent of balding is another visible characteristic. All three characteristics are genetically controlled.
Hair Colour
All natural hair colours are the result of melanin, which is produced in hair follicles and packed into granules in the hair. Two forms of melanin are found in human hair: eumelanin and pheomelanin. Eumelanin is the dominant pigment in brown hair and black hair, and pheomelanin is the dominant pigment in red hair. Blond hair results when you have only a small amount of melanin in the hair. Gray and white hair occur when melanin production slows down, and eventually stops.
Figure 10.5.3 Variation in hair colouration. Which types of melanin are present for each hair colour shown?
Hair Texture
Hair exists in a variety of textures. The main aspects of hair texture are the curl pattern, thickness, and consistency.
- The shape of the hair follicle determines the shape of the hair shaft. The shape of the hair shaft, in turn, determines the curl pattern of the hair. Round hair shafts produce straight hair. Hair shafts that are oval or have other shapes produce wavy or curly hair .
- The size of the hair follicle determines the thickness of hair. Thicker hair has greater volume than thinner hair.
- The consistency of hair is determined by the hair follicle volume and the condition of the hair shaft. The consistency of hair is generally classified as fine, medium, or coarse. Fine hair has the smallest circumference, and coarse hair has the largest circumference. Medium hair falls in between these two extremes. Coarse hair also has a more open cuticle than thin or medium hair does, which causes it to be more porous.

Figure 10.5.4 Curly hair has a differently shaped shaft than straight hair.
Functions of Hair
In humans, one function of head hair is to provide insulation and help the head retain heat. Head hair also protects the skin on the head from damage by UV light.
The function of hair in other locations on the body is debated. One idea is that body hair helps keep us warm in cold weather. When the body is too cold, arrector pili muscles contract and cause hairs to stand up (shown in Figure 10.5.5), trapping a layer of warm air above the epidermis. However, this is more effective in mammals that have thick hair or fur than it is in relatively hairless human beings.
Human hair has an important sensory function, as well. Sensory receptors in the hair follicles can sense when the hair moves, whether it moves because of a breeze, or because of the touch of a physical object. The receptors may also provide sensory awareness of the presence of parasites on the skin.

Some hairs, such as the eyelashes, are especially sensitive to the presence of potentially harmful matter. The eyelashes grow at the edge of the eyelid and can sense when dirt, dust, or another potentially harmful object is too close to the eye. The eye reflexively closes as a result of this sensation. The eyebrows also provide some protection to the eyes. They protect the eyes from dirt, sweat, and rain. In addition, the eyebrows play a key role in nonverbal communication (see Figure 10.5.6). They help express emotions such as sadness, anger, surprise, and excitement.
Hair in Human Evolution
Among mammals, humans are nearly unique in having undergone significant loss of body hair during their evolution. Humans are also unlike most other mammals in having curly hair as one variation in hair texture. Even non-human primates (see Figure 10.5.7) all have straight hair. This suggests that curly hair evolved at some point during human evolution.

Loss of Body Hair
One hypothesis for the loss of body hair in the human lineage is that it would have facilitated cooling of the body by the evaporation of sweat. Humans also evolved far more sweat glands than other mammals, which is consistent with this hypothesis, because sweat evaporates more quickly from less hairy skin. Another hypothesis for human hair loss is that it would have led to fewer parasites on the skin. This might have been especially important when humans started living together in larger, more crowded social groups.
These hypotheses may explain why we lost body hair, but they can’t explain why we didn’t also lose head hair and hair in the pubic region and armpits. It is possible that head hair was retained because it protected the scalp from UV light. As our bipedal ancestors walked on the open savannas of equatorial Africa, the skin on the head would have been an area exposed to the most direct rays of sunlight in an upright hominid. Pubic and armpit hair may have been retained because they served as signs of sexual maturity, which would have been important for successful mating and reproduction.
Evolution of Curly Hair
Greater protection from UV light has also been posited as a possible selective agent favoring the evolution of curly hair. Researchers have found that straight hair allows more light to pass into the body through the hair shaft via the follicle than does curly hair. In this way, human hair is like a fibre optic cable. It allows light to pass through easily when it is straight, but it impedes the passage of light when it is kinked or coiled. This is indirect evidence that UV light may have been a selective agent leading to the evolution of curly hair.
Social and Cultural Significance of Hair
Hair has great social significance for human beings. Body hair is an indicator of biological sex, because hair distribution is sexually dimorphic. Adult males are generally hairier than adult females, and facial hair in particular is a notable secondary male sex characteristic. Hair may also be an indicator of age. White hair is a sign of older age in both males and females, and male pattern baldness is a sign of older age in males. In addition, hair colour and texture can be a sign of ethnic ancestry.
Hair also has great cultural significance. Hairstyle and colour may be an indicator of social group membership and for better or worse can be associated with specific stereotypes. Head shaving has been used in many times and places as a punishment, especially for women. On the other hand, in some cultures, cutting off one’s hair symbolizes liberation from one’s past. In other cultures, it is a sign of mourning. There are also many religious-based practices involving hair. For example, the majority of Muslim women hide their hair with a headscarf. Sikh men grow their hair long and cover it with a turban. Amish men (like the one pictured in Figure 10.5.8) grow facial hair only after they marry — but just a beard, and not a mustache.

Unfortunately, sometimes hairstyle, colour and characteristics are used to apply stereotypes, particularly with respect to women. "Blonde jokes" are a good example of how negative stereotypes are maintained despite having no actual truth behind them. Many stereotypes related to hair are hidden, even from persons perpetrating the stereotype. Often a hairstyle is judged by another as having ties to gender, sexuality, worldview and/or socioeconomic status; even when these inferences are woefully inaccurate. It is important to be aware of our own biases and determine if these biases are appropriate - take a look at the collage in Figure 10.5.9. What are your initial reactions? Are these reactions founded in fact? Do you harbor an unfair bias?
Figure 10.5.9 What are your biases? Are they fair?
10.5 Summary
- Hair is a filament that grows from a hair follicle in the dermis of the skin. It consists mainly of tightly packed, keratin-filled cells called keratinocytes. The human body is almost completely covered with hair follicles.
- The part of a hair that is within the follicle is the hair root. This is the only living part of a hair. The part of a hair that is visible above the skin surface is the hair shaft. It consists of dead cells.
- Hair growth begins inside a follicle when stem cells within the follicle divide to produce new keratinocytes. An individual hair may grow to be very long.
- A hair shaft has three zones: the outermost zone called the cuticle; the middle zone called the cortex; and the innermost zone called the medulla.
- Genetically controlled, visible characteristics of hair include hair colour, hair texture, and the extent of balding in adult males. Melanin (eumelanin and/or pheomelanin) is the pigment that gives hair its colour. Aspects of hair texture include curl pattern, thickness, and consistency.
- Functions of head hair include providing insulation and protecting skin on the head from UV light. Hair everywhere on the body has an important sensory function. Hair in eyelashes and eyebrows protects the eyes from dust, dirt, sweat, and other potentially harmful substances. The eyebrows also play a role in nonverbal communication.
- Among mammals, humans are nearly unique in having undergone significant loss of body hair during their evolution, probably because sweat evaporates more quickly from less hairy skin. Curly hair also is thought to have evolved at some point during human evolution, perhaps because it provided better protection from UV light.
- Hair has social significance for human beings, because it is an indicator of biological sex, age, and ethnic ancestry. Human hair also has cultural significance. Hairstyle may be an indicator of social group membership, for example.
10.5 Review Questions
-
- Compare and contrast the hair root and hair shaft.
- Describe hair follicles.
-
-
- Explain variation in human hair colour.
- What factors determine the texture of hair?
- Describe two functions of human hair.
- What hypotheses have been proposed for the loss of body hair during human evolution?
- Discuss the social and cultural significance of human hair.
- Describe one way in which hair can be used as a method of communication in humans.
- Explain why waxing or tweezing body hair, which typically removes hair down to the root, generally keeps the skin hair-free for a longer period of time than shaving, which cuts hair off at the surface of the skin.
10.5 Explore More
https://www.youtube.com/watch?v=8diYLhl8bWU
Why do some people go bald? - Sarthak Sinha, TED-Ed, 2015.
https://www.youtube.com/watch?v=kNw8V_Fkw28
Hair Love | Oscar®-Winning Short Film (Full) | Sony Pictures Animation, 2019.
https://www.youtube.com/watch?v=hDW5e3NR1Cw
Why do we care about hair | Naomi Abigail | TEDxBaDinh, TEDx Talks, 2015.
Attributions
Figure 10.5.1
Hair by jessica-dabrowski-TETR8YLSqt4 [photo] by Jessica Dabrowski on Unsplash is used under the Unsplash License (https://unsplash.com/license).
Figure 10.5.2
Blausen_0438_HairFollicleAnatomy_02 by BruceBlaus on Wikimedia Commons is used under a CC BY 3.0 (https://creativecommons.org/licenses/by/3.0) license.
Figure 10.5.3
- Standing tall by Ilaya Raja on Unsplash is used under the Unsplash License (https://unsplash.com/license).
- Blond-haired woman smiling by Carlos Lindner on Unsplash is used under the Unsplash License (https://unsplash.com/license).
- Smith Mountain Lake redhead by Chris Ross Harris on Unsplash is used under the Unsplash License (https://unsplash.com/license).
- Through the look of experience by Laura Margarita Cedeño Peralta on Unsplash is used under the Unsplash License (https://unsplash.com/license).
Figure 10.5.4
Curly hair by chris-benson-clvEami9RN4 [photo] by Chris Benson on Unsplash is used under the Unsplash License (https://unsplash.com/license).
Figure 10.5.5
1024px-PilioerectionAnimation by AnthonyCaccese on Wikimedia Commons is used under a CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0/deed.en) license.
Figure 10.5.6
Pout by alexander-dummer-Em8I8Z_DwA4 [photo] by Alexander Dummer on Unsplash is used under the Unsplash License (https://unsplash.com/license).
Figure 10.5.7
Cotton_top_tamarin_monkey._(12046035746) by Bernard Spragg. NZ, from Christchurch, New Zealand on Wikimedia Commons is used under a CC0 1.0 Universal
Public Domain Dedication license (https://creativecommons.org/publicdomain/zero/1.0/deed.en).
Figure 10.5.8
Amish hairstyle by CK-12 Foundation is used under a CC BY-NC 3.0 (https://creativecommons.org/licenses/by-nc/3.0/) license.
 ©CK-12 Foundation Licensed under
©CK-12 Foundation Licensed under ![]() • Terms of Use • Attribution
• Terms of Use • Attribution
Figure 10.5.9
- Rainbow Hair Bubble Man by Behrouz Jafarnezhad on Unsplash is used under the Unsplash License (https://unsplash.com/license).
- Pink hair in Atlanta, United States by Tammie Allen on Unsplash is used under the Unsplash License (https://unsplash.com/license).
- Magdalena 2 by Valerie Elash on Unsplash is used under the Unsplash License (https://unsplash.com/license).
- Perfect Style by Daria Volkova on Unsplash is used under the Unsplash License (https://unsplash.com/license)
- Stay Classy by Fayiz Musthafa on Unsplash is used under the Unsplash License (https://unsplash.com/license)
- Take your time by Jan Tinneberg on Unsplash is used under the Unsplash License (https://unsplash.com/license)
References
Blausen.com staff. (2014). Medical gallery of Blausen Medical 2014. WikiJournal of Medicine 1 (2). DOI:10.15347/wjm/2014.010. ISSN 2002-4436.
Brainard, J/ CK-12 Foundation. (2016). Figure 7 This style of facial hair is adopted by most Amish men after they marry [digital image]. In CK-12 College Human Biology (Section 12.5) [online Flexbook]. CK12.org. https://www.ck12.org/book/ck-12-college-human-biology/section/12.5/
Sony Pictures Animation. (2019, December 5). Hair love | Oscar®-winning short film (Full) | Sony Pictures Animation. YouTube. https://www.youtube.com/watch?v=kNw8V_Fkw28
TED-Ed. (2015, August 25). Why do some people go bald? – Sarthak Sinha. YouTube. https://www.youtube.com/watch?v=8diYLhl8bWU
TEDx Talks. (2015, February 4). Why do we care about hair | Naomi Abigail | TEDxBaDinh. YouTube. https://www.youtube.com/watch?v=hDW5e3NR1Cw
Created by CK-12 Foundation/Adapted by Christine Miller

Tonsillitis
The white patches on either side of the throat in Figure 17.3.1 are signs of tonsillitis. The tonsils are small structures in the throat that are very common sites of infection. The white spots on the tonsils pictured here are evidence of infection. The patches consist of large amounts of dead bacteria, cellular debris, and white blood cells — in a word: pus. Children with recurrent tonsillitis may have their tonsils removed surgically to eliminate this type of infection. The tonsils are organs of the lymphatic system.
What Is the Lymphatic System?
The lymphatic system is a collection of organs involved in the production, maturation, and harboring of white blood cells called lymphocytes. It also includes a network of vessels that transport or filter the fluid known as lymph in which lymphocytes circulate. Figure 17.3.2 shows major lymphatic vessels and other structures that make up the lymphatic system. Besides the tonsils, organs of the lymphatic system include the thymus, the spleen, and hundreds of lymph nodes distributed along the lymphatic vessels.
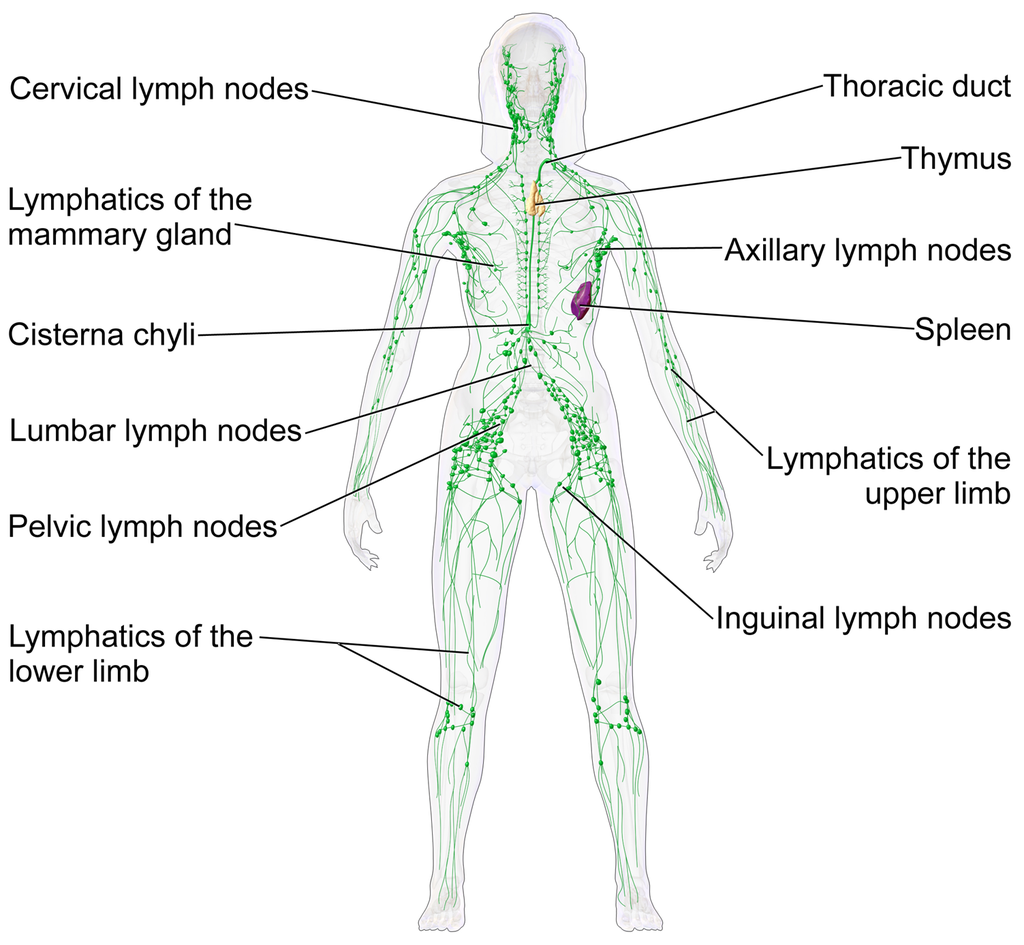
The lymphatic vessels form a transportation network similar in many respects to the blood vessels of the cardiovascular system. However, unlike the cardiovascular system, the lymphatic system is not a closed system. Instead, lymphatic vessels carry lymph in a single direction — always toward the upper chest, where the lymph empties from lymphatic vessels into blood vessels.
Cardiovascular Function of the Lymphatic System
The return of lymph to the bloodstream is one of the major functions of the lymphatic system. When blood travels through capillaries of the cardiovascular system, it is under pressure, which forces some of the components of blood (such as water, oxygen, and nutrients) through the walls of the capillaries and into the tissue spaces between cells, forming tissue fluid, also called interstitial fluid (see Figure 17.3.3). Interstitial fluid bathes and nourishes cells, and also absorbs their waste products. Much of the water from interstitial fluid is reabsorbed into the capillary blood by osmosis. Most of the remaining fluid is absorbed by tiny lymphatic vessels called lymph capillaries. Once interstitial fluid enters the lymphatic vessels, it is called lymph. Lymph is very similar in composition to blood plasma. Besides water, lymph may contain proteins, waste products, cellular debris, and pathogens. It also contains numerous white blood cells, especially the subset of white blood cells known as lymphocytes. In fact, lymphocytes are the main cellular components of lymph.
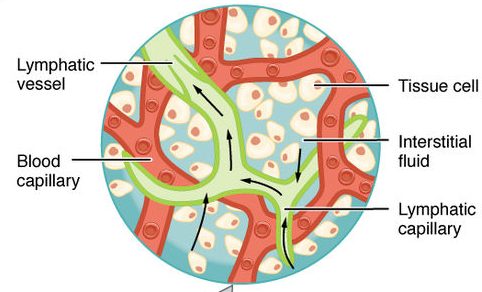
The lymph that enters lymph capillaries in tissues is transported through the lymphatic vessel network to two large lymphatic ducts in the upper chest. From there, the lymph flows into two major veins (called subclavian veins) of the cardiovascular system. Unlike blood, lymph is not pumped through its network of vessels. Instead, lymph moves through lymphatic vessels via a combination of contractions of the vessels themselves and the forces applied to the vessels externally by skeletal muscles, similarly to how blood moves through veins. Lymphatic vessels also contain numerous valves that keep lymph flowing in just one direction, thereby preventing backflow.
Digestive Function of the Lymphatic System
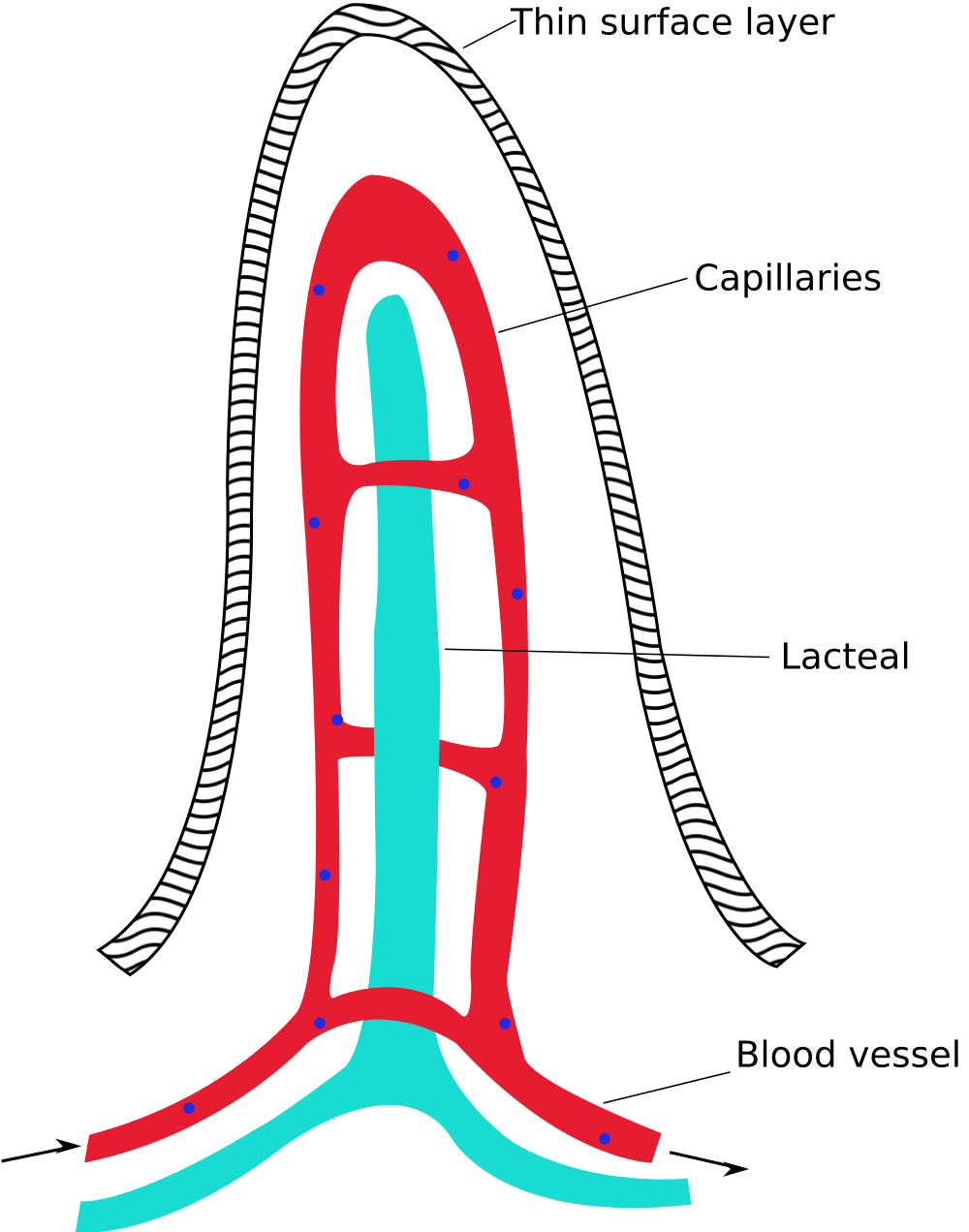
Lymphatic vessels called lacteals (see Figure 17.3.4) are present in the lining of the gastrointestinal tract, mainly in the small intestine. Each tiny villus in the lining of the small intestine has an internal bed of capillaries and lacteals. The capillaries absorb most nutrients from the digestion of food into the blood. The lacteals absorb mainly fatty acids from lipid digestion into the lymph, forming a fatty-acid-enriched fluid called chyle. Vessels of the lymphatic network then transport chyle from the small intestine to the main lymphatic ducts in the chest, from which it drains into the blood circulation. The nutrients in chyle then circulate in the blood to the liver, where they are processed along with the other nutrients that reach the liver directly via the bloodstream.
Immune Function of the Lymphatic System
The primary immune function of the lymphatic system is to protect the body against pathogens and cancerous cells. This function of the lymphatic system is centred on the production, maturation, and circulation of lymphocytes. Lymphocytes are leukocytes that are involved in the adaptive immune system. They are responsible for the recognition of — and tailored defense against — specific pathogens or tumor cells. Lymphocytes may also create a lasting memory of pathogens, so they can be attacked quickly and strongly if they ever invade the body again. In this way, lymphocytes bring about long-lasting immunity to specific pathogens.
There are two major types of lymphocytes, called B cells and T cells. Both B cells and T cells are involved in the adaptive immune response, but they play different roles.
Production and Maturation of Lymphocytes
Like all other types of blood cells (including erythrocytes), both B cells and T cells are produced from stem cells in the red marrow inside bones. After lymphocytes first form, they must go through a complicated maturation process before they are ready to search for pathogens. In this maturation process, they “learn” to distinguish self from non-self. Only those lymphocytes that successfully complete this maturation process go on to actually fight infections by pathogens.
B cells mature in the bone marrow, which is why they are called B cells. After they mature and leave the bone marrow, they travel first to the circulatory system and then enter the lymphatic system to search for pathogens. T cells, on the other hand, mature in the thymus, which is why they are called T cells. The thymus is illustrated in Figure 17.3.5. It is a small lymphatic organ in the chest that consists of an outer cortex and inner medulla, all surrounded by a fibrous capsule. After maturing in the thymus, T cells enter the rest of the lymphatic system to join B cells in the hunt for pathogens. The bone marrow and thymus are called primary lymphoid organs because of their role in the production and/or maturation of lymphocytes.
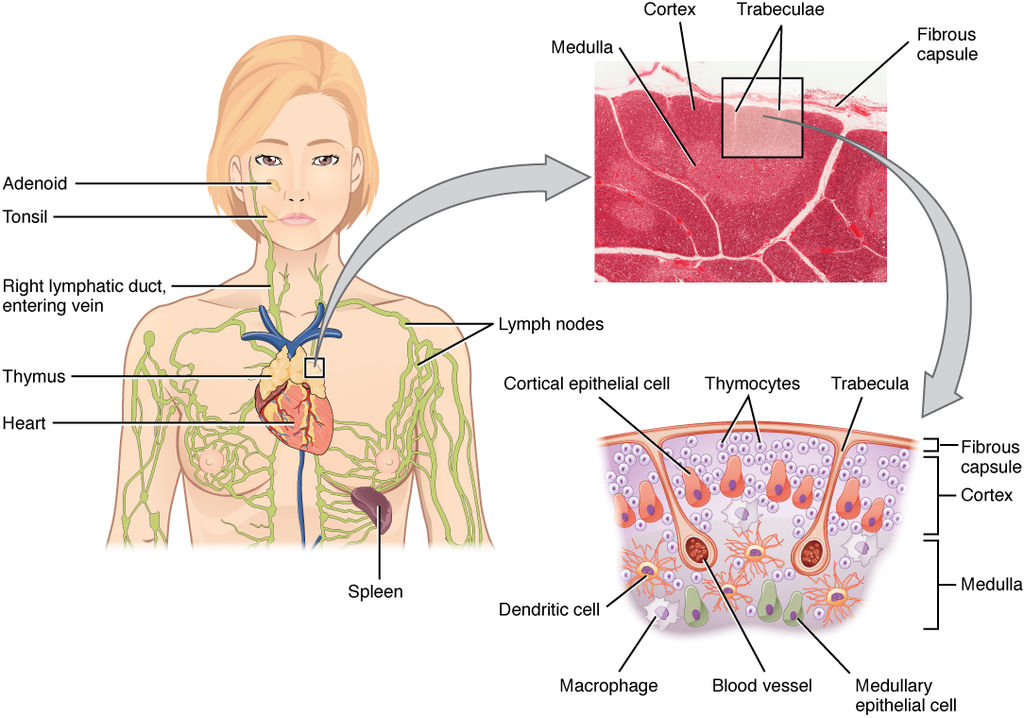
Lymphocytes in Secondary Lymphoid Organs
The tonsils, spleen, and lymph nodes are referred to as secondary lymphoid organs. These organs do not produce or mature lymphocytes. Instead, they filter lymph and store lymphocytes. It is in these secondary lymphoid organs that pathogens (or their antigens) activate lymphocytes and initiate adaptive immune responses. Activation leads to cloning of pathogen-specific lymphocytes, which then circulate between the lymphatic system and the blood, searching for and destroying their specific pathogens by producing antibodies against them.
Tonsils
There are four pairs of human tonsils. Three of the four are shown in Figure 17.3.6. The fourth pair, called tubal tonsils, is located at the back of the nasopharynx. The palatine tonsils are the tonsils that are visible on either side of the throat. All four pairs of tonsils encircle a part of the anatomy where the respiratory and gastrointestinal tracts intersect, and where pathogens have ready access to the body. This ring of tonsils is called Waldeyer's ring.
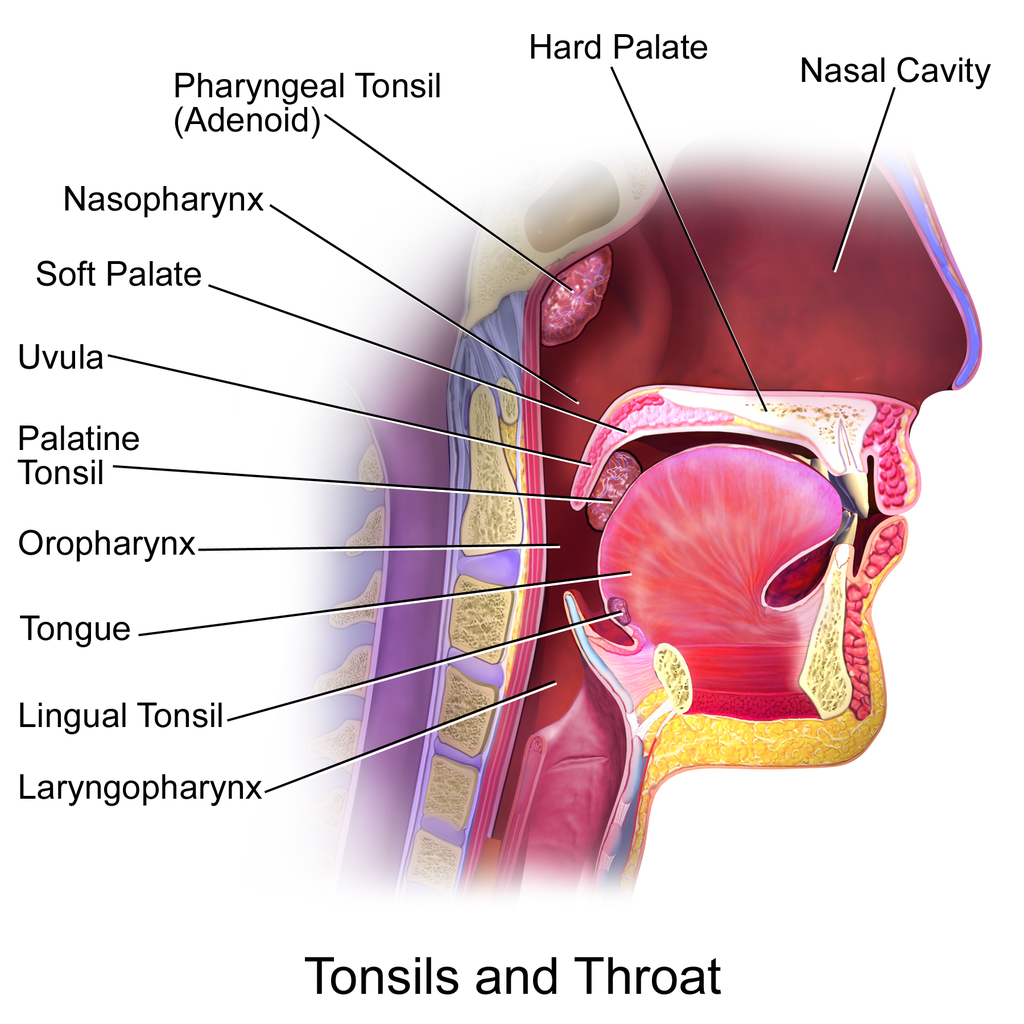
Spleen
The spleen (Figure 17.3.7) is the largest of the secondary lymphoid organs, and is centrally located in the body. Besides harboring lymphocytes and filtering lymph, the spleen also filters blood. Most dead or aged erythrocytes are removed from the blood in the red pulp of the spleen. Lymph is filtered in the white pulp of the spleen. In the fetus, the spleen has the additional function of producing red blood cells. This function is taken over by bone marrow after birth.
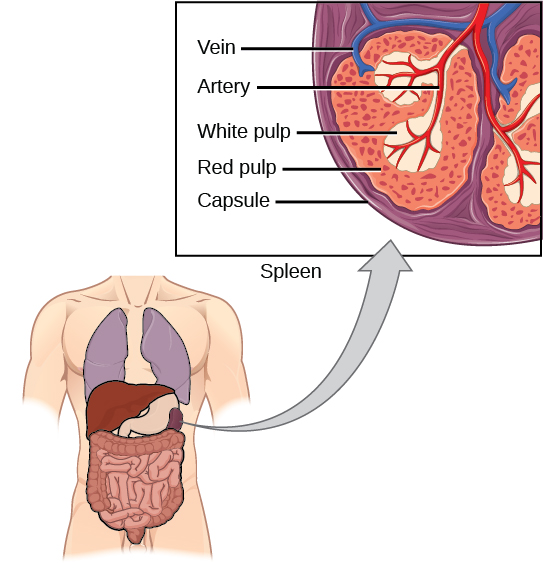
Lymph Nodes
Each lymph node is a small, but organized collection of lymphoid tissue (see Figure 17.3.8) that contains many lymphocytes. Lymph nodes are located at intervals along the lymphatic vessels, and lymph passes through them on its way back to the blood.
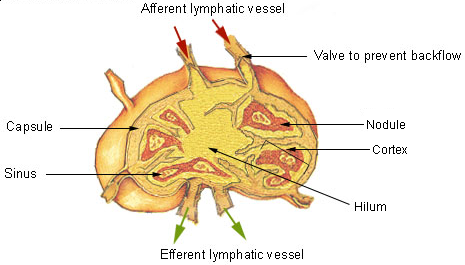
There are at least 500 lymph nodes in the human body. Many of them are clustered at the base of the limbs and in the neck. Figure 17.3.9 shows the major lymph node concentrations, and includes the spleen and the region named Waldeyer’s ring, which consists of the tonsils.
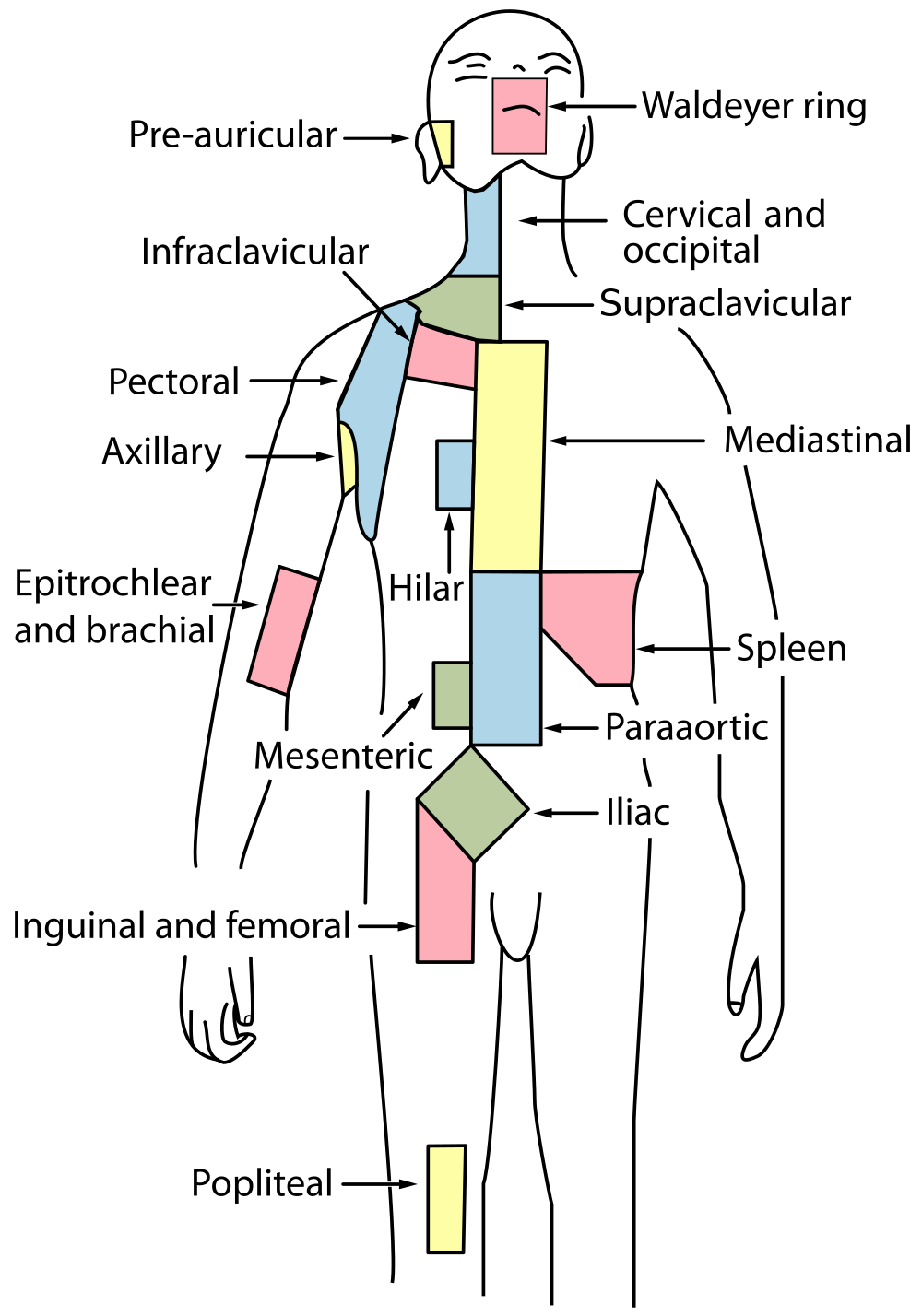
Feature: Myth vs. Reality
When lymph nodes become enlarged and tender to the touch, they are obvious signs of immune system activity. Because it is easy to see and feel swollen lymph nodes, they are one way an individual can monitor his or her own health. To be useful in this way, it is important to know the myths and realities about swollen lymph nodes.
Myth
|
Reality
|
| "You should see a doctor immediately whenever you have swollen lymph nodes." | Lymph nodes are constantly filtering lymph, so it is expected that they will change in size with varying amounts of debris or pathogens that may be present. A minor, unnoticed infection may cause swollen lymph nodes that may last for a few weeks. Generally, lymph nodes that return to their normal size within two or three weeks are not a cause for concern. |
| "Swollen lymph nodes mean you have a bacterial infection." | Although an infection is the most common cause of swollen lymph nodes, not all infections are caused by bacteria. Mononucleosis, for example, commonly causes swollen lymph nodes, and it is caused by viruses. There are also other causes of swollen lymph nodes besides infections, such as cancer and certain medications. |
| "A swollen lymph node means you have cancer." | Cancer is far less likely to be the cause of a swollen lymph node than is an infection. However, if a lymph node remains swollen longer than a few weeks — especially in the absence of an apparent infection — you should have your doctor check it. |
| "Cancer in a lymph node always originates somewhere else. There is no cancer of the lymph nodes." | Cancers do commonly spread from their site of origin to nearby lymph nodes and then to other organs, but cancer may also originate in the lymph nodes. This type of cancer is called lymphoma. |
17.3 Summary
- The lymphatic system is a collection of organs involved in the production, maturation, and harboring of leukocytes called lymphocytes. It also includes a network of vessels that transport or filter the fluid called lymph in which lymphocytes circulate.
- The return of lymph to the bloodstream is one of the functions of the lymphatic system. Lymph flows from tissue spaces — where it leaks out of blood vessels — to the subclavian veins in the upper chest, where it is returned to the cardiovascular system. Lymph is similar in composition to blood plasma. Its main cellular components are lymphocytes.
- Lymphatic vessels called lacteals are found in villi that line the small intestine. Lacteals absorb fatty acids from the digestion of lipids in the digestive system. The fatty acids are then transported through the network of lymphatic vessels to the bloodstream.
- The primary immune function of the lymphatic system is to protect the body against pathogens and cancerous cells. It is responsible for producing mature lymphocytes and circulating them in lymph. Lymphocytes, which include B cells and T cells, are the subset of white blood cells involved in adaptive immune responses. They may create a lasting memory of and immunity to specific pathogens.
- All lymphocytes are produced in bone marrow and then go through a process of maturation in which they “learn” to distinguish self from non-self. B cells mature in the bone marrow, and T cells mature in the thymus. Both the bone marrow and thymus are considered primary lymphatic organs.
- Secondary lymphatic organs include the tonsils, spleen, and lymph nodes. There are four pairs of tonsils that encircle the throat. The spleen filters blood, as well as lymph. There are hundreds of lymph nodes located in clusters along the lymphatic vessels. All of these secondary organs filter lymph and store lymphocytes, so they are sites where pathogens encounter and activate lymphocytes and initiate adaptive immune responses.
17.3 Review Questions
- What is the lymphatic system?
-
- Summarize the immune function of the lymphatic system.
- Explain the difference between lymphocyte maturation and lymphocyte activation.
17.3 Explore More
https://youtu.be/RMLPwOiYnII
What is Lymphoedema or Lymphedema? Compton Care, 2016.
https://youtu.be/ah74jT00jBA
Spleen physiology What does the spleen do in 2 minutes, Simple Nursing, 2015.
https://youtu.be/L4KexZZAdyA
How to check your lymph nodes, University Hospitals Bristol and Weston NHS FT, 2020.
Attributions
Figure 17.3.1
512px-Tonsillitis by Michaelbladon at English Wikipedia on Wikimedia Commons is in the public domain (https://en.wikipedia.org/wiki/Public_domain). (Transferred from en.wikipedia to Commons by Kauczuk)
Figure 17.3.2
Blausen_0623_LymphaticSystem_Female by BruceBlaus on Wikimedia Commons is used under a CC BY 3.0 (https://creativecommons.org/licenses/by/3.0) license.
Figure 17.3.3
2201_Anatomy_of_the_Lymphatic_System (cropped) by OpenStax College on Wikimedia Commons is used under a CC BY 3.0 (https://creativecommons.org/licenses/by/3.0) license.
Figure 17.3.4
1000px-Intestinal_villus_simplified.svg by Snow93 on Wikimedia Commons is in the public domain (https://en.wikipedia.org/wiki/Public_domain).
Figure 17.3.5
2206_The_Location_Structure_and_Histology_of_the_Thymus by OpenStax College on Wikimedia Commons is used under a CC BY 3.0 (https://creativecommons.org/licenses/by/3.0) license.
Figure 17.3.6
Blausen_0861_Tonsils&Throat_Anatomy2 by BruceBlaus on Wikimedia Commons is used under a CC BY 3.0 (https://creativecommons.org/licenses/by/3.0) license.
Figure 17.3.7
Figure_42_02_14 by CNX OpenStax on Wikimedia Commons is used under a CC BY 4.0 (https://creativecommons.org/licenses/by/4.0) license.
Figure 17.3.8
Illu_lymph_node_structure by NCI/ SEER Training on Wikimedia Commons is in the public domain (https://en.wikipedia.org/wiki/Public_domain). (Archives: https://web.archive.org/web/20070311015818/http://training.seer.cancer.gov/module_anatomy/unit8_2_lymph_compo1_nodes.html)
Figure 17.3.9
1000px-Lymph_node_regions.svg by Fred the Oyster (derivative work) on Wikimedia Commons is in the public domain (https://en.wikipedia.org/wiki/Public_domain). (Original by NCI/ SEER Training)
References
Betts, J. G., Young, K.A., Wise, J.A., Johnson, E., Poe, B., Kruse, D.H., Korol, O., Johnson, J.E., Womble, M., DeSaix, P. (2013, June 19). Figure 21.2 Anatomy of the lymphatic system [digital image]. In Anatomy and Physiology (Section 21.1). OpenStax. https://openstax.org/books/anatomy-and-physiology/pages/21-1-anatomy-of-the-lymphatic-and-immune-systems
Betts, J. G., Young, K.A., Wise, J.A., Johnson, E., Poe, B., Kruse, D.H., Korol, O., Johnson, J.E., Womble, M., DeSaix, P. (2013, June 19). Figure 21.7 Location, structure, and histology of the thymus [digital image]. In Anatomy and Physiology (Section 21.1). OpenStax. https://openstax.org/books/anatomy-and-physiology/pages/21-1-anatomy-of-the-lymphatic-and-immune-systems
Blausen.com Staff. (2014). Medical gallery of Blausen Medical 2014". WikiJournal of Medicine 1 (2). DOI:10.15347/wjm/2014.010. ISSN 2002-4436
Compton Care. (2016, March 7). What is lymphoedema or lymphedema? YouTube. https://www.youtube.com/watch?v=RMLPwOiYnII&feature=youtu.be
OpenStax. (2016, May 27) Figure 14. The spleen is similar to a lymph node but is much larger and filters blood instead of lymph [digital image]. In Open Stax, Biology (Section 42.2). OpenStax CNX. https://cnx.org/contents/GFy_h8cu@10.8:etZobsU-@6/Adaptive-Immune-Response
Simple Nursing. (2015, June 28). Spleen physiology What does the spleen do in 2 minutes. YouTube. https://www.youtube.com/watch?v=ah74jT00jBA&feature=youtu.be
University Hospitals Bristol and Weston NHS FT. (2020, May 13). How to check your lymph nodes. YouTube. https://www.youtube.com/watch?v=L4KexZZAdyA&feature=youtu.be
Created by: CK-12/Adapted by Christine Miller

Bacteria Attack!
The colourful image in Figure 4.3.1 shows a bacterial cell (in green) attacking human red blood cells. The bacterium causes a disease called relapsing fever. The bacterial and human cells look very different in size and shape. Although all living cells have certain things in common — such as a plasma membrane and cytoplasm — different types of cells, even within the same organism, may have their own unique structures and functions. Cells with different functions generally have different shapes that suit them for their particular job. Cells vary not only in shape, but also in size, as this example shows. In most organisms, however, even the largest cells are no bigger than the period at the end of this sentence. Why are cells so small?
Explaining Cell Size
Most organisms, even very large ones, have microscopic cells. Why don't cells get bigger instead of remaining tiny and multiplying? Why aren't you one giant cell rolling around school? What limits cell size?
Once you know how a cell functions, the answers to these questions are clear. To carry out life processes, a cell must be able to quickly pass substances in and out of the cell. For example, it must be able to pass nutrients and oxygen into the cell and waste products out of the cell. Anything that enters or leaves a cell must cross its outer surface. The size of a cell is limited by its need to pass substances across that outer surface.
Look at the three cubes in Figure 4.3.2. A larger cube has less surface area relative to its volume than a smaller cube. This relationship also applies to cells — a larger cell has less surface area relative to its volume than a smaller cell. A cell with a larger volume also needs more nutrients and oxygen, and produces more waste. Because all of these substances must pass through the surface of the cell, a cell with a large volume will not have enough surface area to allow it to meet its needs. The larger the cell is, the smaller its ratio of surface area to volume, and the more difficult it will be for the cell to get rid of its waste and take in necessary substances. This is what limits the size of the cell.
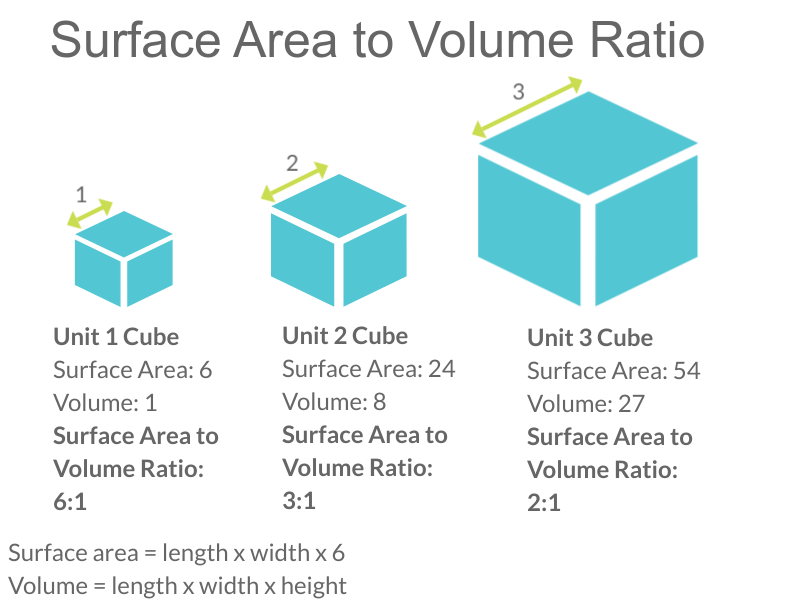
Cell Form and Function
Cells with different functions often have varying shapes. The cells pictured below (Figure 4.3.3) are just a few examples of the many different shapes that human cells may have. Each type of cell has characteristics that help it do its job. The job of the nerve cell, for example, is to carry messages to other cells. The nerve cell has many long extensions that reach out in all directions, allowing it to pass messages to many other cells at once. Do you see the tail of each tiny sperm cell? Its tail helps a sperm cell "swim" through fluids in the female reproductive tract in order to reach an egg cell. The white blood cell has the job of destroying bacteria and other pathogens. It is a large cell that can engulf foreign invaders.
Figure 4.3.3 Human cells may have many different shapes that help them to do their jobs.
Cells With and Without a Nucleus
The nucleus is a basic cell structure present in many — but not all — living cells. The nucleus of a cell is a structure in the cytoplasm that is surrounded by a membrane (the nuclear membrane) and contains DNA. Based on whether or not they have a nucleus, there are two basic types of cells: prokaryotic cells and eukaryotic cells.
Prokaryotic Cells
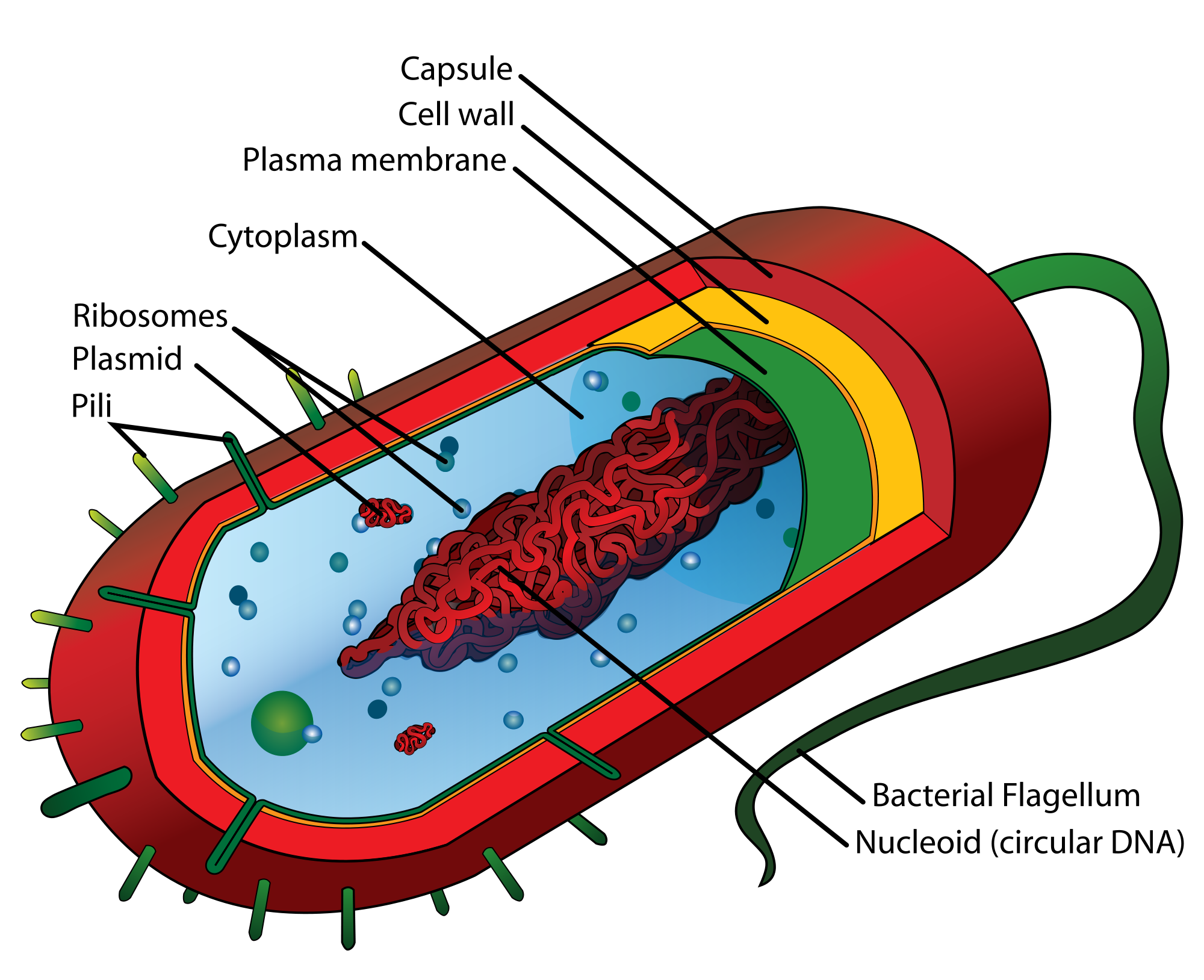
Prokaryotic cells are cells without a nucleus. The DNA in prokaryotic cells is in the cytoplasm, rather than enclosed within a nuclear membrane. In addition, these cells are typically smaller than eukaryotic cells and contain fewer organelles. Prokaryotic cells are found in single-celled organisms, such as the bacterium represented by the model in Figure 4.3.3. Organisms with prokaryotic cells are called prokaryotes. They were the first type of organisms to evolve, and they are still the most common organisms today.
Eukaryotic Cells

Eukaryotic cells are cells that contain a nucleus. A typical eukaryotic cell is represented by the model in Figure 4.3.4. Eukaryotic cells are usually larger than prokaryotic cells. They are found in some single-celled and all multicellular organisms. Organisms with eukaryotic cells are called eukaryotes, and they range from fungi to humans.
Besides a nucleus, eukaryotic cells also contain other organelles. An organelle is a structure within the cytoplasm that performs a specific job in the cell. Organelles called mitochondria, for example, provide energy to the cell, and organelles called vesicles store substances in the cell. Organelles allow eukaryotic cells to carry out more functions than prokaryotic cells can.
Interestingly, scientists think that mitochondria were once free-living prokaryotes that infected (or were engulfed by) larger cells. The two organisms developed a symbiotic relationship that was beneficial to both of them, resulting in the smaller prokaryote becoming an organelle within the larger cell. This is called endosymbiotic theory, and it is supported by a lot of evidence, including the fact that mitochondria have their own DNA separate from the DNA in the nucleus of the eukaryotic cell. Endosymbiotic theory will be described in more detail in later sections, and it's also discussed in the video below.
https://www.youtube.com/watch?v=FGnS-Xk0ZqU
Endosymbiotic Theory, Amoeba Sisters, 2017.
4.3 Summary
- Cells must be very small so they have a large enough surface area-to-volume ratio to maintain normal cell processes.
- Cells with different functions often have different shapes.
- Prokaryotic cells do not have a nucleus. Eukaryotic cells do have a nucleus, along with other organelles.
4.3 Review Questions
- Explain why most cells are very small.
- Discuss variations in the form and function of cells.
-
-
- Do human cells have organelles? Explain your answer.
- Which are usually larger – prokaryotic or eukaryotic cells? What do you think this means for their relative ability to take in needed substances and release wastes? Discuss your answer.
- DNA in eukaryotes is enclosed within the _______ ________.
- Name three different types of cells in humans.
- Which organelle provides energy in eukaryotic cells?
- What is a function of a vesicle in a cell?
4.3 Explore More
https://www.youtube.com/watch?time_continue=1&v=9i7kAt97XYU&feature=emb_logo
How we think complex cells evolved - Adam Jacobson, TED-Ed, 2015.
https://www.youtube.com/watch?v=Pxujitlv8wc
Prokaryotic vs. Eukaryotic Cells (updated), Amoeba Sisters, 2018.
Attributions
Figure 4.3.1
Borrelia_hermsii_Bacteria_(13758011613) by NAID on Wikimedia Commons is released into the public domain (https://en.wikipedia.org/wiki/Public_domain).
Figure 4.3.2
Cell Size by Christine Miller is released into the Public Domain (https://creativecommons.org/publicdomain/mark/1.0/).
Figure 4.3.3
- Chondrocyte. BioTek-Wikipedia-Image by BioTek Instruments, Inc. on Wikimedia Commons is used under a CC BY-SA 3.0 (https://creativecommons.org/licenses/by-sa/3.0/deed.en) license.
- Neutrophil with anthrax copy by Volker Brinkmann from PLOS Pathogens on Wikimedia Commons is used under a CC BY 2.5 (https://creativecommons.org/licenses/by/2.5/deed.en) license.
- PLoSBiol4.e126.Fig6fNeuron by Lee, et al. from PLOS Biology on Wikimedia Commons is used under a CC BY 2.5 (https://creativecommons.org/licenses/by/2.5/deed.en) license.
- Sperm (265 33) human by Doc. RNDr. Josef Reischig, CSc. on Wikimedia Commons is used under a CC BY-SA 3.0 (https://creativecommons.org/licenses/by-sa/3.0) license.
Figure 4.3.4
Model of a prokaryotic cell: bacterium by Mariana Ruiz Villarreal [LadyofHats] on Wikimedia Commons is released into the public domain (https://en.wikipedia.org/wiki/Public_domain).
Figure 4.3.5
Animal Cell adapted by Christine Miller is used under a CC0 1.0 (https://creativecommons.org/publicdomain/zero/1.0/deed.en) public domain dedication license. (Original image, Animal Cell Unannotated, is by Kelvin Song on Wikimedia Commons.)
References
Amoeba Sisters. (2017, May 3). Endosymbiotic theory. YouTube. https://www.youtube.com/watch?v=FGnS-Xk0ZqU&feature=youtu.be
Amoeba Sisters. (2018, July 30). Prokaryotic vs. eukaryotic cells (updated). YouTube. https://www.youtube.com/watch?v=Pxujitlv8wc&feature=youtu.be
Brinkmann, V. (November 2005). Neutrophil engulfing Bacillus anthracis. PLoS Pathogens 1 (3): Cover page [digital image]. DOI:10.1371. https://journals.plos.org/plospathogens/issue?id=10.1371/issue.ppat.v01.i03
Lee, W.C.A., Huang, H., Feng, G., Sanes, J.R., Brown, E.N., et al. (2005, December 27) Figure 6f, slightly altered (plus scalebar, minus letter "f".) [digital image]. Dynamic Remodeling of Dendritic Arbors in GABAergic Interneurons of Adult Visual Cortex. PLoS Biology, 4(2), e29. doi:10.1371/journal.pbio.0040029. https://journals.plos.org/plosbiology/article?id=10.1371/journal.pbio.0040029
TED-Ed. (2015, February 17). How we think complex cells evolved - Adam Jacobson. https://www.youtube.com/watch?v=9i7kAt97XYU&feature=youtu.be
A group of diseases involving abnormal cell growth with the potential to invade or spread to other parts of the body.

