10.7 Skin Cancer

Bathing in Sunshine
Summer sun may feel good on your body, but its invisible UV rays wreak havoc on your skin. Exposing the skin to UV light causes photo-aging: premature wrinkling, brown discolourations, and other unattractive signs of sun exposure. Even worse, UV light increases your risk of skin cancer.
What Is Skin Cancer?
Skin cancer is a disease in which skin cells grow out of control. It is caused mainly by excessive exposure to UV light, which damages DNA. Therefore, skin cancer most often develops on areas of the skin that are frequently exposed to UV light. However, it can also occur on areas that are rarely exposed to UV light. Skin cancer affects people of all skin colours, including those with dark skin. It also affects more people altogether than all other cancers combined. One in five Canadians develops skin cancer in his or her lifetime.
Types of Skin Cancer
Skin cancer begins in the outer layer of skin, the epidermis. There are three common types of skin cancer: basal cell carcinoma, squamous cell carcinoma, and melanoma.
Basal Cell Carcinoma

Basal cell carcinoma occurs in basal cells of the epidermis. Basal cells are stem cells in the stratum basale layer that divide to form all the keratinocytes of the epidermis. Basal cell carcinoma is the most common form of skin cancer and 1 in 8 Canadians will develop basal cell carcinoma during their lifetime. A basal cell carcinoma may appear as a pearly or waxy sore, like the one shown in Figure 10.7.2. Basal cell carcinomas rarely spread (or undergo metastasis), so they can generally be cured with a biopsy, in which the lesion is cut out of the skin and analyzed in a medical lab.
Squamous Cell Carcinoma

Squamous cell carcinoma occurs in squamous cells of the epidermis. Squamous cells are flattened, keratin-filled cells in upper layers of the epidermis. Squamous cell carcinoma is the second most common form of skin cancer. More than two million cases occur in the United States each year. A squamous cell carcinoma may appear as a firm, red nodule, or as a flat lesion with a scaly or crusty surface, like the one pictured in Figure 10.7.3. Squamous cell carcinomas are generally localized and unlikely to metastasize, so they are usually curable surgically.
Melanoma

Melanoma occurs in melanocytes of the epidermis. Melanocytes are the melanin-producing cells in the stratum basale of the epidermis. Melanoma is the rarest type of skin cancer, accounting for less than one per cent of all skin cancer cases. Melanoma, however, is the most deadly type of skin cancer. It causes the vast majority of skin cancer deaths, because melanoma is malignant. If not treated, it will metastasize and spread to other parts of the body. If melanoma is detected early and while it is still localized in the skin, most patients survive for at least five years. If melanoma is discovered only after it has already metastasized to distant organs, there is only a 17% of patients surviving for five years. You can see an example of a melanoma in Figure 10.7.4.
Melanoma can develop anywhere on the body. It may develop in otherwise normal skin, or an existing mole may become cancerous. Signs of melanoma may include a:
- Mole that changes in size, feel, or colour.
- Mole that bleeds.
- Large brown spot on the skin sprinkled with darker specks.
- Small lesion with an irregular border and parts that appear red, white, blue, or blue-black.
- Dark lesion on the palms, soles, fingertips, toes, or mucous membranes.
Skin Cancer Risk Factors
Exposure to UV radiation causes about 90 per cent of all skin cancer cases. The connection between skin cancer and UV light is so strong that the World Health Organization has classified UV radiation (whether from tanning beds or the sun) as a Group 1 carcinogen (cancer-causing agent). Group 1 carcinogens are those carcinogens that are known with virtual certainty to cause cancer. In addition to UV light, Group 1 carcinogens include tobacco and plutonium. In terms of numbers of cancers caused, UV radiation is far worse than tobacco. More people develop skin cancer because of UV light exposure than develop lung cancer because of smoking. The increase in cancer risk due to UV light is especially great if you have ever had blistering sunburns as a child or teen.
Besides UV light exposure, other risk factors for skin cancer include:
- Having light coloured skin.
- Having a lot of moles.
- Being diagnosed with precancerous skin lesions.
- Having a family history of skin cancer.
- Having a personal history of skin cancer.
- Having a weakened immune system.
- Being exposed to other forms of radiation or to certain toxic substances such as arsenic.
Feature: My Human Body
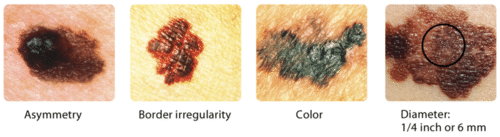
As with most types of cancer, skin cancer is easiest to treat and most likely to be cured the earlier it is detected. The skin is one of the few organs that you can monitor for cancer yourself, as long as you know what to look for. A brown spot on the skin is likely to be a harmless mole, but it could be a sign of skin cancer. As shown in Figure 10.7.5 below, unlike moles, skin cancers may be asymmetrical, have irregular borders, may be very dark in colour, and may have a relatively great diameter. These characteristics can be remembered with the acronym ABCD.
With the help of mirrors, you should check all of your skin regularly. Look for new skin growths or changes in any existing moles, freckles, bumps, or birthmarks. Report anything suspicious or different to your doctor.
If you have risk factors for skin cancer, it’s a good idea to have an annual skin check by a dermatologist. This helps ensure that cancerous or precancerous lesions will be detected before they grow too large and become difficult to cure, or in the case of melanoma, before they metastasize.
10.7 Summary
- Skin cancer is a disease in which skin cells grow out of control. It is caused mainly by excessive exposure to UV light, which damages DNA. Skin cancer affects more Canadians than all other cancers combined. There are three common types of skin cancer: basal cell carcinoma, squamous cell carcinoma, and melanoma. Carcinomas are more common and unlikely to metastasize. Melanoma is rare and likely to metastasize. It causes most skin cancer deaths.
- Besides exposure to UV light, risk factors for skin cancer include having light coloured skin, having lots of moles, and a family history of skin cancer, among several others.
10.7 Review Questions
- What is skin cancer?
- How common is skin cancer?
-
- Compare and contrast the three common types of skin cancer.
- Identify factors that increase the risk of skin cancer.
- How does exposure to UV light cause skin cancer?
- In which layer of the skin does skin cancer normally start?
- Which two skin cancers described in this section start in the same sub-layer? Include the name of the sub-layer and the cells affected in each of these cancers.
- Which type of skin cancer is most likely to spread to other organs? Explain your answer.
- Which form of skin cancer is the most deadly?
- What are some ways people can reduce their risk of getting skin cancer? Explain your answer.
10.7 Explore More
The skin ‘beauty’ and the sun ‘beast’: Charareh Pourzand at TEDxBathUniveristy, TEDx Talks, 2014.
Cancer of the Vulva, Robert Miller, 2014.
How do cancer cells behave differently from healthy ones? – George Zaidan, TED-Ed, 2012.
Attributions
Figure 10.7.1
Stolen_Moment_in_the_Sun by Angie Garrett on Wikimedia Commons is used under a CC BY 2.0 (https://creativecommons.org/licenses/by/2.0) license.
Figure 10.7.2
Basal_cell_carcinoma,_ulcerated by Kelly Nelson (Photographer) from National Cancer Institute (part of the National Institutes of Health) with the ID 9237 on Wikimedia Commons was released into the public domain (https://en.wikipedia.org/wiki/Public_domain).
Figure 10.7.3
Squamous_cell_carcinoma_(1) by Kelly Nelson (Photographer) from National Cancer Institute (part of the National Institutes of Health) with the ID 9248 on Wikimedia Commons was released into the public domain (https://en.wikipedia.org/wiki/Public_domain).
Figure 10.7.4
Melanoma by Unknown author (Photographer) from National Cancer Institute (part of the National Institutes of Health) with the AV-8500-3850/ ID 9186 on Wikimedia Commons was released into the public domain (https://en.wikipedia.org/wiki/Public_domain).
Figure 10.7.5
ABCDs of skin cancer by CK-12 Foundation is used under a CC BY-NC 3.0 (https://creativecommons.org/licenses/by-nc/3.0/) license. (Original images courtesy of NCI: ID numbers 2362; 2363; 2364; and 2184)
References
Brainard, J/ CK-12 Foundation. (2016). Figure 5 ABCDs of skin cancer[digital image]. In CK-12 College Human Biology (Section 12.7) [online Flexbook]. CK12.org. https://www.ck12.org/book/ck-12-college-human-biology/section/12.7/
Public Health Agency of Canada. (2019, December 9). Non melanoma skin cancer. Canada.ca. https://www.canada.ca/en/public-health/services/chronic-diseases/cancer/non-melanoma-skin-cancer.html
Robert Miller. (2014, July 22). Cancer of the vulva. YouTube. https://www.youtube.com/watch?v=ID-O-Ion3EQ
TED-Ed. (2012, December 5). How do cancer cells behave differently from healthy ones? – George Zaidan. YouTube. https://www.youtube.com/watch?v=BmFEoCFDi-w
TEDx Talks. (2014, March 28). The skin ‘beauty’ and the sun ‘beast’: Charareh Pourzand at TEDxBathUniveristy. YouTube. https://www.youtube.com/watch?v=60e-t4zglBk
The space occurring between two or more membranes. In cell biology, it's most commonly described as the region between the inner membrane and the outer membrane of a mitochondrion or a chloroplast.
A group of diseases involving abnormal cell growth with the potential to invade or spread to other parts of the body.
The outer layer of skin that consists mainly of epithelial cells and lacks nerve endings, blood vessels, and other structures.
A genetic mutation caused by a deletion or insertion in a DNA sequence that shifts the way the sequence is read.
Created by CK-12 Foundation/Adapted by Christine Miller

Case Study: Defending Your Defenses

Twenty-six-year-old Hakeem wasn’t feeling well. He was more tired than usual, dragging through his workdays despite going to bed earlier, and napping on the weekends. He didn’t have much of an appetite, and had started losing weight. When he pressed on the side of his neck, like the doctor is doing in Figure 17.1.1, he noticed an unusual lump.
Hakeem went to his doctor, who performed a physical exam and determined that the lump was a swollen lymph node. Lymph nodes are part of the immune system, and they will often become enlarged when the body is fighting off an infection. Dr. Hayes thinks that the swollen lymph node and fatigue could be signs of a viral or bacterial infection, although he is concerned about Hakeem’s lack of appetite and weight loss. All of those symptoms combined can indicate a type of cancer called lymphoma. An infection, however, is a more likely cause, particularly in a young person like Hakeem. Dr. Hayes prescribes an antibiotic in case Hakeem has a bacterial infection, and advises him to return in a few weeks if his lymph node does not shrink, or if he is not feeling better.
Hakeem returns a few weeks later. He is not feeling better and his lymph node is still enlarged. Dr. Hayes is concerned, and orders a biopsy of the enlarged lymph node. A lymph node biopsy for suspected lymphoma often involves the surgical removal of all or part of a lymph node. This helps to determine whether the tissue contains cancerous cells.

The initial results of the biopsy indicate that Hakeem does have lymphoma. Although lymphoma is more common in older people, young adults and even children can get this disease. There are many types of lymphoma, with the two main types being Hodgkin's lymphoma and non-Hodgkin's lymphoma. Non-Hodgkin lymphoma (NHL), in turn, has many subtypes. The subtype depends on several factors, including which cell types are affected. Some subtypes of NHL, for example, affect immune system cells called B cells, while others affect different immune system cells called T cells.
Dr. Hayes explains to Hakeem that it is important to determine which type of lymphoma he has, in order to choose the best course of treatment. Hakeem’s biopsied tissue will be further examined and tested to see which cell types are affected, as well as which specific cell-surface proteins — called antigens — are present. This should help identify his specific type of lymphoma.
As you read this chapter, you will learn about the functions of the immune system, and the specific roles that its cells and organs — such as B and T cells and lymph nodes — play in defending the body. At the end of this chapter, you will learn what type of lymphoma Hakeem has and what some of his treatment options are, including treatments that make use of the biochemistry of the immune system to fight cancer with the immune system itself.
Chapter Overview: Immune System
In this chapter, you will learn about the immune system — the system that defends the body against infections and other causes of disease, such as cancerous cells. Specifically, you will learn about:
- How the immune system identifies normal cells of the body as “self” and pathogens and damaged cells as “non-self.”
- The two major subsystems of the general immune system: the innate immune system — which provides a quick, but non-specific response — and the adaptive immune system, which is slower, but provides a specific response that often results in long-lasting immunity.
- The specialized immune system that protects the brain and spinal cord, called the neuroimmune system.
- The organs, cells, and responses of the innate immune system, which includes physical barriers (such as skin and mucus), chemical and biological barriers, inflammation, activation of the complement system of molecules, and non-specific cellular responses (such as phagocytosis).
- The lymphatic system — which includes white blood cells called lymphocytes, lymphatic vessels (which transport a fluid called lymph), and organs (such as the spleen, tonsils, and lymph nodes) — and its important role in the adaptive immune system.
- Specific cells of the immune system and their functions, including B cells, T cells, plasma cells, and natural killer cells.
- How the adaptive immune system can generate specific and often long-lasting immunity against pathogens through the production of antibodies.
- How vaccines work to generate immunity.
- How cells in the immune system detect and kill cancerous cells.
- Some strategies that pathogens employ to evade the immune system.
- Disorders of the immune system, including allergies, autoimmune diseases (such as diabetes and multiple sclerosis), and immunodeficiency resulting from conditions such as HIV infection.
As you read the chapter, think about the following questions:
- What are the functions of lymph nodes?
- What are B and T cells? How do they relate to lymph nodes?
- What are cell-surface antigens? How do they relate to the immune system and to cancer?
Attributions
Figure 17.1.1
Lymph nodes/Is it a Cold or the Flu by Lee Health on Vimeo is used under Vimeo's Terms of Service (https://vimeo.com/terms#licenses).
Figure 17.1.2
mitchell-luo-ymo_yC_N_2o-unsplash [photo] by Mitchell Luo on Unsplash is used under the Unsplash License (https://unsplash.com/license).
Figure 17.1.3
Lymph node biopsy by US Army Africa on Flickr is used under a CC BY 2.0 (https://creativecommons.org/licenses/by/2.0/) license.
References
Mayo Clinic Staff. (n.d.). Hodgkin's lymphoma [online article]. MayoClinic.org. https://www.mayoclinic.org/diseases-conditions/hodgkins-lymphoma/symptoms-causes/syc-20352646
Mayo Clinic Staff. (n.d.). Non-Hodgkin's lymphoma [online article]. MayoClinic.org. https://www.mayoclinic.org/diseases-conditions/non-hodgkins-lymphoma/symptoms-causes/syc-20375680
The process by which a parent cell divides into two or more daughter cells. Cell division usually occurs as part of a larger cell cycle.
A genetic mutation caused by a deletion or insertion in a DNA sequence that shifts the way the sequence is read.
A part of each hemisphere of the cerebrum that controls executive functions such as reasoning and language.
A mature haploid male or female germ cell which is able to unite with another of the opposite sex in sexual reproduction to form a zygote.
Respiration using electron acceptors other than molecular oxygen. Although oxygen is not the final electron acceptor, the process still uses a respiratory electron transport chain.
The process whereby a haploid cell (n) is formed from a diploid cell (2n) through meiosis and cell differentiation. Gametogenesis in the male is known as spermatogenesis and produces spermatozoa. Gametogenesis in the female is known as oogenesis and result in the formation of ova.
Respiration using electron acceptors other than molecular oxygen. Although oxygen is not the final electron acceptor, the process still uses a respiratory electron transport chain.


