9.7 Pancreas

A Shot in the Arm
Giving yourself an injection can be difficult, but for someone with diabetes, it may be a matter of life or death. The person in the photo has diabetes and is injecting themselves with insulin, the hormone that helps control the level of glucose in the blood. Insulin is produced by the pancreas.
Introduction to the Pancreas
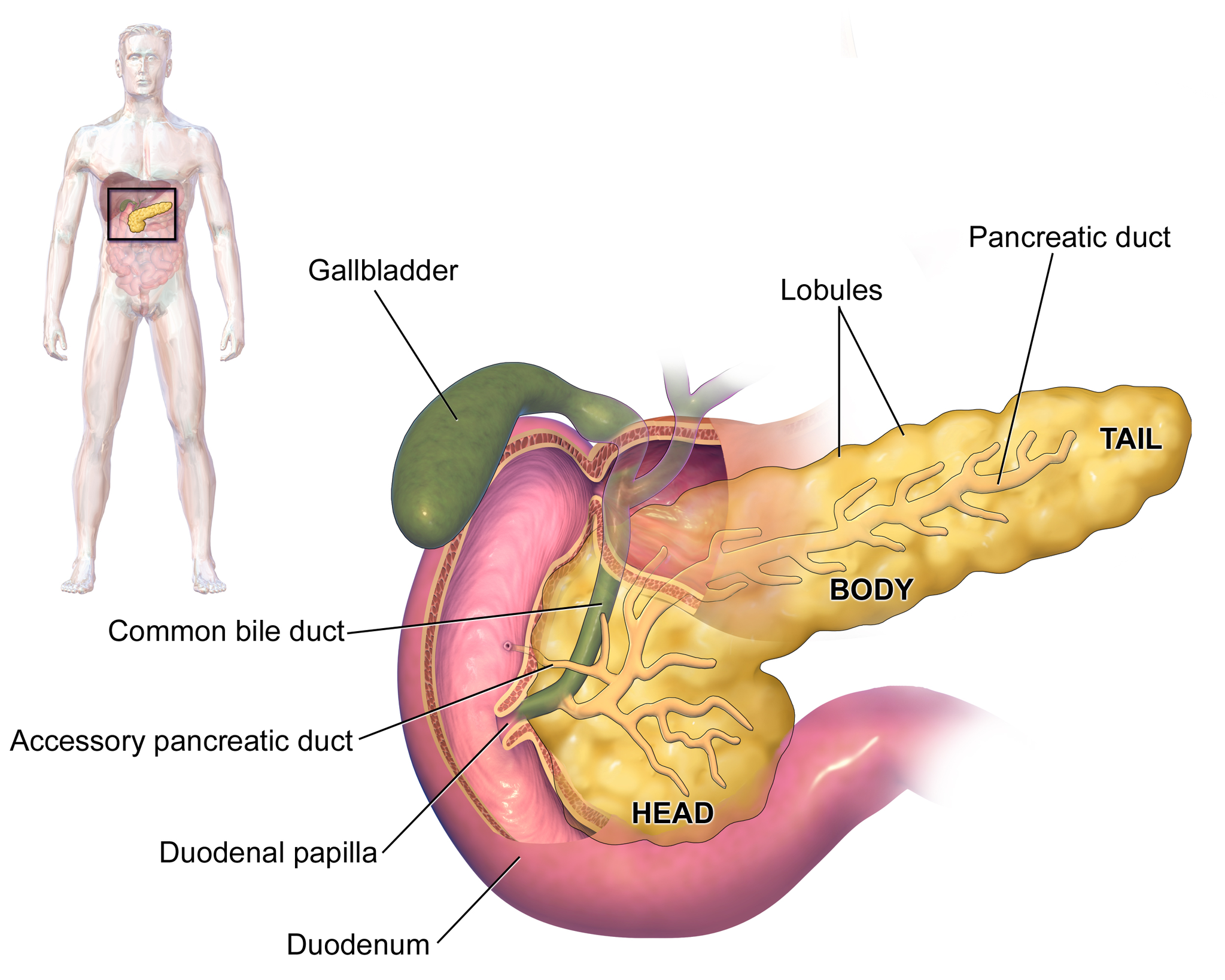
The pancreas is a large gland located in the upper left abdomen behind the stomach, as shown in Figure 9.7.2. The pancreas is about 15 cm (6 in) long, and it has a flat, oblong shape. Structurally, the pancreas is divided into a head, body, and tail. Functionally, the pancreas serves as both an endocrine gland and an exocrine gland.
- As an endocrine gland, the pancreas is part of the endocrine system. As such, it releases hormones (such as insulin) directly into the bloodstream for transport to cells throughout the body.
- As an exocrine gland, the pancreas is part of the digestive system. As such, it releases digestive enzymes into ducts that carry the enzymes to the gastrointestinal tract, where they assist with digestion. In this concept, the focus is on the pancreas as an endocrine gland. You can read about the pancreas as an exocrine gland in Chapter 15 Digestive System.
The Pancreas as an Endocrine Gland
The tissues within the pancreas that have an endocrine role exist as clusters of cells called pancreatic islets. They are also called the islets of Langerhans. You can see pancreatic tissue, including islets, in Figure 9.7.3. There are approximately three million pancreatic islets, and they are crisscrossed by a dense network of capillaries. The capillaries are lined by layers of islet cells that have direct contact with the blood vessels, into which they secrete their endocrine hormones.
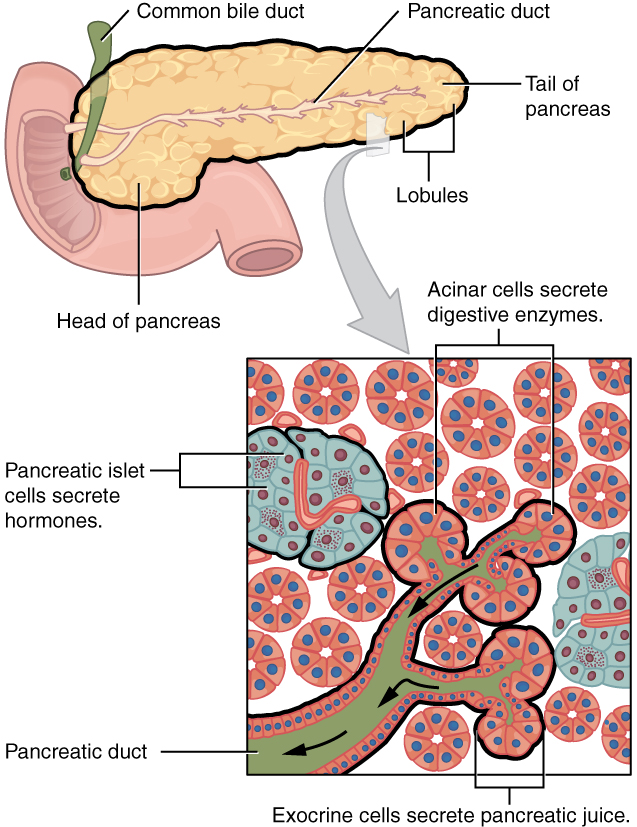
The pancreatic islets consist of four main types of cells, each of which secretes a different endocrine hormone. All of the hormones produced by the pancreatic islets, however, play crucial roles in glucose metabolism and the regulation of blood glucose levels, among other functions.
- Islet cells called alpha (α) cells secrete the hormone glucagon. The function of glucagon is to increase the level of glucose in the blood. It does this by stimulating the liver to convert stored glycogen into glucose, which is released into the bloodstream.
- Islets cells called beta (β) cells secrete the hormone insulin. The function of insulin is to decrease the level of glucose in the blood. It does this by promoting the absorption of glucose from the blood into fat, liver, and skeletal muscle cells. In these tissues, the absorbed glucose is converted into glycogen, fats (triglycerides), or both.
- Islet cells called delta (δ) cells secrete the hormone somatostatin. This hormone is also called growth hormone inhibiting hormone, because it inhibits the anterior lobe of the pituitary gland from producing growth hormone. Somatostatin also inhibits the secretion of pancreatic endocrine hormones and pancreatic exocrine enzymes.
- Islet cells called gamma (γ) cells secrete the hormone pancreatic polypeptide. The function of pancreatic polypeptide is to help regulate the secretion of both endocrine and exocrine substances by the pancreas.
Disorders of the Pancreas
There are a variety of disorders that affect the pancreas. They include pancreatitis, pancreatic cancer, and diabetes mellitus.
Pancreatitis

Pancreatitis is inflammation of the pancreas. It has a variety of possible causes, including gallstones, chronic alcohol use, infections (such as measles or mumps), and certain medications. Pancreatitis occurs when digestive enzymes produced by the pancreas damage the gland’s tissues, which causes problems with fat digestion. The disorder is usually associated with intense pain in the central abdomen, and the pain may radiate to the back. Yellowing of the skin and whites of the eyes (see Figure 9.7.4), which is called jaundice, is a common sign of pancreatitis. People with pancreatitis may also have pale stools and dark urine. Treatment of pancreatitis includes administering drugs to manage pain, and addressing the underlying cause of the disease, for example, by removing gallstones.
Pancreatic Cancer
There are several different types of pancreatic cancer that may affect either the endocrine or the exocrine tissues of the gland. Cancers affecting the endocrine tissues are all relatively rare. However, their incidence has been rising sharply. It is unclear to what extent this reflects increased detection, especially through medical imaging techniques. Unfortunately, pancreatic cancer is usually diagnosed at a relatively late stage when it is too late for surgery, which is the only way to cure the disorder. In 2020 it is estimated that 6,000 Canadians will be newly diagnosed with pancreatic cancer, and that during this same year, 5,300 will die of pancreatic cancer.
While it is rare before the age of 40, pancreatic cancer occurs most often after the age of 60. Factors that increase the risk of developing pancreatic cancer include smoking, obesity, diabetes, and a family history of the disease. About one in four cases of pancreatic cancer are attributable to smoking. Certain rare genetic conditions are also risk factors for pancreatic cancer.
Diabetes Mellitus
By far the most common type of pancreatic disorder is diabetes mellitus, more commonly called simply diabetes. There are many different types of diabetes, but diabetes mellitus is the most common. It occurs in two major types, type 1 diabetes and type 2 diabetes. The two types have different causes and may also have different treatments, but they generally produce the same initial symptoms, which include excessive urination and thirst. These symptoms occur because the kidneys excrete more urine in an attempt to rid the blood of excess glucose. Loss of water in urine stimulates greater thirst. Other signs and symptoms of diabetes are listed in Figure 9.7.5.
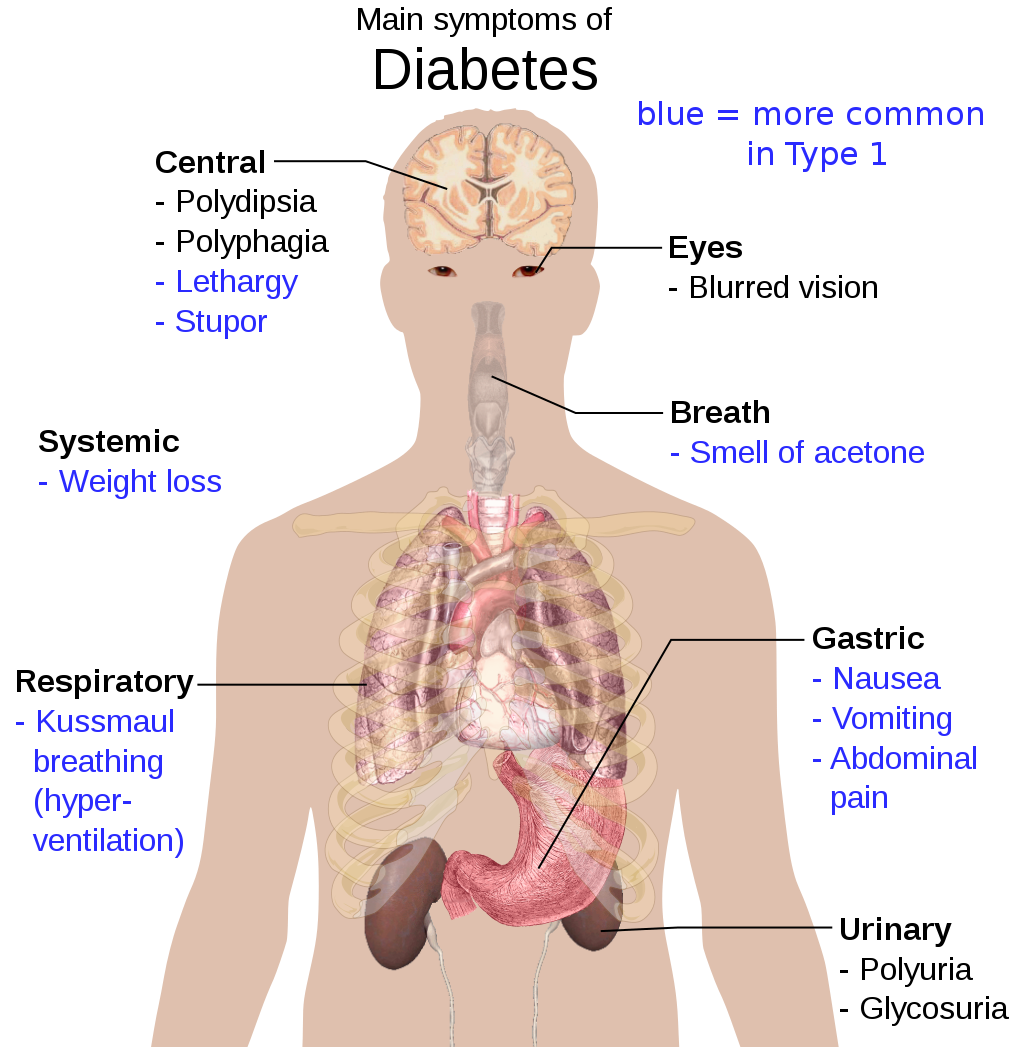
When diabetes is not well controlled, it is likely to have several serious long-term consequences. Most of these consequences are due to damage to small blood vessels caused by high glucose levels in the blood. Damage to blood vessels, in turn, may lead to increased risk of coronary artery disease and stroke. Damage to blood vessels in the retina of the eye can result in gradual vision loss and blindness. Damage to blood vessels in the kidneys can lead to chronic kidney disease, sometimes requiring dialysis or kidney transplant. Long-term consequences of diabetes may also include damage to the nerves of the body, known as diabetic neuropathy. In fact, this is the most common complication of diabetes. Symptoms of diabetic neuropathy may include numbness, tingling, and pain in the extremities.
Type 1 Diabetes
Type 1 diabetes is a chronic autoimmune disorder in which the immune system attacks the insulin-secreting beta cells of the pancreas. As a result, people with type 1 diabetes lack the insulin needed to keep blood glucose levels within the normal range. Type 1 diabetes may develop in people of any age, but is most often diagnosed before adulthood. For type 1 diabetics, insulin injections are critical for survival.
Type 2 Diabetes
Type 2 diabetes is the single most common form of diabetes. The cause of high blood glucose in this form of diabetes usually includes a combination of insulin resistance and impaired insulin secretion. Both genetic and environmental factors play roles in the development of type 2 diabetes. Type 2 diabetes can be managed with changes in diet and physical activity, which may increase insulin sensitivity and help reduce blood glucose levels to normal ranges. Medications may also be used as part of the treatment, as may insulin injections.
Feature: Human Biology in the News
Some patients with type 1 diabetes have been given pancreatic islet cells transplants from other human donors. If the transplanted cells are not rejected by the recipient’s immune system, they can cure the patient of diabetes. However, because of a shortage of appropriate human donors, only about one thousand such surgeries have been performed over the past ten years.
In June of 2016, a research team led by Dr. David K.C. Cooper at the Thomas E. Starzl Transplantation Institute in Pittsburgh, Pennsylvania, reported on their work developing pig islet cells for transplant into human diabetes patients. The researchers genetically engineered the pig islet cells to be protected from the human immune response. As a result, patients receiving the transplanted cells would require only minimal suppression of their immune system after the surgery. The pig islet cells would also be less likely to transmit pathogenic agents, because the animals could be raised in a controlled environment.
The researchers have successfully transplanted the pig islet cells into monkey models of type 1 diabetes. As of June 2016, the scientists were looking for funding to undertake clinical trials in humans with type 1 diabetes. Dr. Cooper predicted then that if the human trials go as well as expected, the pig islet cells could be available for curing patients in as little as two years.
9.7 Summary
- The pancreas is a gland located in the upper left abdomen behind the stomach that functions as both an endocrine gland and an exocrine gland. As an endocrine gland, the pancreas releases hormones (such as insulin) directly into the bloodstream. As an exocrine gland, the pancreas releases digestive enzymes into ducts that carry them to the gastrointestinal tract.
- Tissues in the pancreas that have an endocrine role exist as clusters of cells called pancreatic islets. The islets consist of four main types of cells, each of which secretes a different endocrine hormone. Alpha (α) cells secrete glucagon, beta (β) cells secrete insulin, delta (δ) cells secrete somatostatin, and gamma (γ) cells secrete pancreatic polypeptide.
- The endocrine hormones secreted by the pancreatic islets all play a role, either directly or indirectly, in glucose metabolism and homeostasis of blood glucose levels. For example, insulin stimulates the uptake of glucose by cells and decreases the level of glucose in the blood, whereas glucagon stimulates the conversion of glycogen to glucose and increases the level of glucose in the blood.
- Disorders of the pancreas include pancreatitis, pancreatic cancer, and diabetes mellitus. Pancreatitis is painful inflammation of the pancreas that has many possible causes. Pancreatic cancer of the endocrine tissues is rare, but increasing in frequency. It is generally discovered too late to cure surgically. Smoking is a major risk factor for pancreatic cancer.
- Diabetes mellitus is the most common type of pancreatic disorder. In diabetes, inadequate activity of insulin results in high blood levels of glucose. Type 1 diabetes is a chronic autoimmune disorder in which the immune system attacks the insulin-secreting beta cells of the pancreas. Type 2 diabetes is usually caused by a combination of insulin resistance and impaired insulin secretion due to a variety of environmental and genetic factors.
9.7 Review Questions
- Describe the structure and location of the pancreas.
- Distinguish between the endocrine and exocrine functions of the pancreas.
-
-
- What is pancreatitis? What are possible causes and effects of pancreatitis?
- Describe the incidence, prognosis, and risk factors of cancer of the endocrine tissues of the pancreas.
- Compare and contrast type 1 and type 2 diabetes.
- If the alpha islet cells of the pancreas were damaged to the point that they no longer functioned, how would this affect blood glucose levels? Assume that no outside regulation of this system is occurring and explain your answer. Further, would administration of insulin be more likely to help or hurt this condition? Explain your answer.
- Explain why diabetes causes excessive thirst.
9.7 Explore More
What does the pancreas do? – Emma Bryce, TED-Ed, 2015.
Type 2 diabetes in children, Children’s Health, 2008.
Reversing Type 2 diabetes starts with ignoring the guidelines | Sarah Hallberg | TEDxPurdueU, TEDx Talks, 2015.
Attributions
Figure 9.7.1
Insulin_Application by Mr Hyde at Czech Wikipedia (Original text: moje foto) on Wikimedia Commons is released into the public domain (https://en.wikipedia.org/wiki/Public_domain).
Figure 9.7.2
Blausen_0699_PancreasAnatomy2 by BruceBlaus on Wikimedia Commons is used under a CC BY 3.0 (https://creativecommons.org/licenses/by/3.0) license.
Figure 9.7.3
Exocrine_and_Endocrine_Pancreas by OpenStax College is used under a CC BY 3.0 (https://creativecommons.org/licenses/by/3.0/deed.en) license.
Figure 9.7.4
Jaundice_eye_new by Info-farmer on Wikimedia Commons is in the public domain (https://en.wikipedia.org/wiki/Public_domain). (Original image, File:Jaundice eye.jpg, is from Centers for Disease Control and Prevention‘s Public Health Image Library (PHIL), with identification number #2860)
Figure 9.7.5
Main_symptoms_of_diabetes.svg by Mikael Häggström on Wikimedia Commons is released into the public domain (https://en.wikipedia.org/wiki/Public_domain).
Betts, J. G., Young, K.A., Wise, J.A., Johnson, E., Poe, B., Kruse, D.H., Korol, O., Johnson, J.E., Womble, M., DeSaix, P. (2013, July 19). Figure 23.26 Exocrine and endocrine pancreas [digital image]. In Anatomy and Physiology (Section 23.6). OpenStax. https://openstax.org/books/anatomy-and-physiology/pages/23-6-accessory-organs-in-digestion-the-liver-pancreas-and-gallbladder
Blausen.com Staff. (2014). Medical gallery of Blausen Medical 2014. WikiJournal of Medicine 1 (2). DOI:10.15347/wjm/2014.010. ISSN 2002-4436.
Children’s Health. (2008, June 13). Type 2 diabetes in children. YouTube. https://www.youtube.com/watch?v=qlzLSbAGMqA&feature=youtu.be
, , , , , , . (2016, March 4). First update of the International Xenotransplantation Association consensus statement on conditions for undertaking clinical trials of porcine islet products in type 1 diabetes—Executive summary. Xenotransplantation 2016, 23: 3– 13. https://doi.org/10.1111/xen.12231
TED-Ed. (2015, February 19). What does the pancreas do? – Emma Bryce. YouTube. https://www.youtube.com/watch?v=8dgoeYPoE-0&feature=youtu.be
TEDx Talks. (2015, May 4). Reversing Type 2 diabetes starts with ignoring the guidelines | Sarah Hallberg | TEDxPurdueU. YouTube. https://www.youtube.com/watch?v=da1vvigy5tQ&feature=youtu.be
Created by CK-12 Foundation/Adapted by Christine Miller

Fashion Statement
This colourful hairstyle makes quite a fashion statement. Many people spend a lot of time and money on their hair, even if they don’t have an exceptional hairstyle like this one. Besides its display value, hair actually has important physiological functions.
What is Hair?
Hair is a filament that grows from a hair follicle in the dermis of the skin. It consists mainly of tightly packed, keratin-filled cells called keratinocytes. The human body is covered with hair follicles, with the exception of a few areas, including the mucous membranes, lips, palms of the hands, and soles of the feet.
Structure of Hair
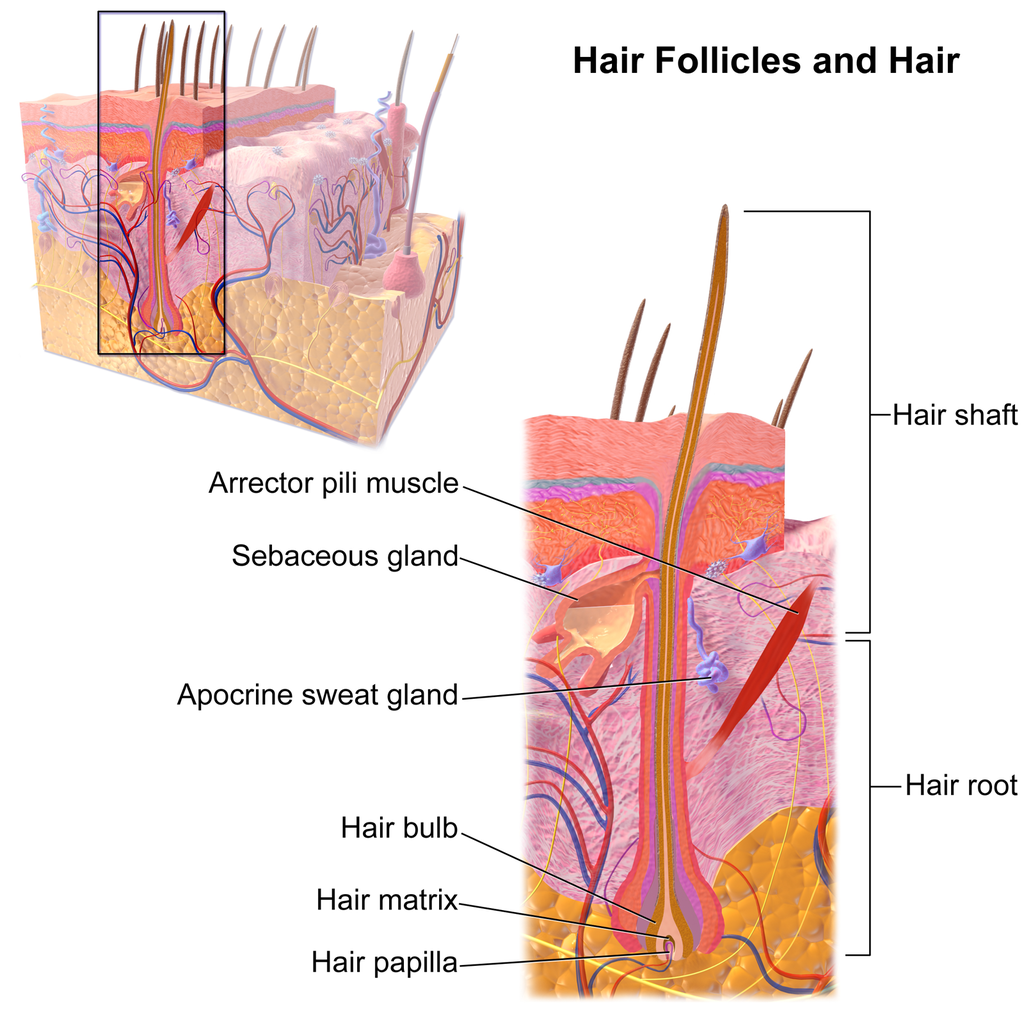
The part of the hair located within the follicle is called the hair root. The root is the only living part of the hair. The part of the hair that is visible above the surface of the skin is the hair shaft. The shaft of the hair has no biochemical activity and is considered dead.
Follicle and Root
Hair growth begins inside a follicle (see Figure 10.5.2 below). Each hair follicle contains stem cells that can keep dividing, which allows hair to grow. The stem cells can also regrow a new hair after one falls out. Another structure associated with a hair follicle is a sebaceous gland that produces oily sebum. The sebum lubricates and helps to waterproof the hair. A tiny arrector pili muscle is also attached to the follicle. When it contracts, the follicle moves, and the hair in the follicle stands up.
Shaft
The hair shaft is a hard filament that may grow very long. Hair normally grows in length by about half an inch a month. In cross-section, a hair shaft can be divided into three zones, called the cuticle, cortex, and medulla.
- The cuticle (or outer coat) is the outermost zone of the hair shaft. It consists of several layers of flat, thin keratinocytes that overlap one another like shingles on a roof. This arrangement helps the cuticle repel water. The cuticle is also covered with a layer of lipids, just one molecule thick, which increases its ability to repel water. This is the zone of the hair shaft that is visible to the eye.
- The cortex is the middle zone of the hair shaft, and it is also the widest part. The cortex is highly structured and organized, consisting of keratin bundles in rod-like structures. These structures give hair its mechanical strength. The cortex also contains melanin, which gives hair its colour.
- The medulla is the innermost zone of the hair shaft. This is a small, disorganized, and more open area at the center of the hair shaft. The medulla is not always present. When it is present, it contains highly pigmented cells full of keratin.
Characteristics of Hair
Two visible characteristics of hair are its colour and texture. In adult males, the extent of balding is another visible characteristic. All three characteristics are genetically controlled.
Hair Colour
All natural hair colours are the result of melanin, which is produced in hair follicles and packed into granules in the hair. Two forms of melanin are found in human hair: eumelanin and pheomelanin. Eumelanin is the dominant pigment in brown hair and black hair, and pheomelanin is the dominant pigment in red hair. Blond hair results when you have only a small amount of melanin in the hair. Gray and white hair occur when melanin production slows down, and eventually stops.
Figure 10.5.3 Variation in hair colouration. Which types of melanin are present for each hair colour shown?
Hair Texture
Hair exists in a variety of textures. The main aspects of hair texture are the curl pattern, thickness, and consistency.
- The shape of the hair follicle determines the shape of the hair shaft. The shape of the hair shaft, in turn, determines the curl pattern of the hair. Round hair shafts produce straight hair. Hair shafts that are oval or have other shapes produce wavy or curly hair .
- The size of the hair follicle determines the thickness of hair. Thicker hair has greater volume than thinner hair.
- The consistency of hair is determined by the hair follicle volume and the condition of the hair shaft. The consistency of hair is generally classified as fine, medium, or coarse. Fine hair has the smallest circumference, and coarse hair has the largest circumference. Medium hair falls in between these two extremes. Coarse hair also has a more open cuticle than thin or medium hair does, which causes it to be more porous.

Figure 10.5.4 Curly hair has a differently shaped shaft than straight hair.
Functions of Hair
In humans, one function of head hair is to provide insulation and help the head retain heat. Head hair also protects the skin on the head from damage by UV light.
The function of hair in other locations on the body is debated. One idea is that body hair helps keep us warm in cold weather. When the body is too cold, arrector pili muscles contract and cause hairs to stand up (shown in Figure 10.5.5), trapping a layer of warm air above the epidermis. However, this is more effective in mammals that have thick hair or fur than it is in relatively hairless human beings.
Human hair has an important sensory function, as well. Sensory receptors in the hair follicles can sense when the hair moves, whether it moves because of a breeze, or because of the touch of a physical object. The receptors may also provide sensory awareness of the presence of parasites on the skin.

Some hairs, such as the eyelashes, are especially sensitive to the presence of potentially harmful matter. The eyelashes grow at the edge of the eyelid and can sense when dirt, dust, or another potentially harmful object is too close to the eye. The eye reflexively closes as a result of this sensation. The eyebrows also provide some protection to the eyes. They protect the eyes from dirt, sweat, and rain. In addition, the eyebrows play a key role in nonverbal communication (see Figure 10.5.6). They help express emotions such as sadness, anger, surprise, and excitement.
Hair in Human Evolution
Among mammals, humans are nearly unique in having undergone significant loss of body hair during their evolution. Humans are also unlike most other mammals in having curly hair as one variation in hair texture. Even non-human primates (see Figure 10.5.7) all have straight hair. This suggests that curly hair evolved at some point during human evolution.

Loss of Body Hair
One hypothesis for the loss of body hair in the human lineage is that it would have facilitated cooling of the body by the evaporation of sweat. Humans also evolved far more sweat glands than other mammals, which is consistent with this hypothesis, because sweat evaporates more quickly from less hairy skin. Another hypothesis for human hair loss is that it would have led to fewer parasites on the skin. This might have been especially important when humans started living together in larger, more crowded social groups.
These hypotheses may explain why we lost body hair, but they can’t explain why we didn’t also lose head hair and hair in the pubic region and armpits. It is possible that head hair was retained because it protected the scalp from UV light. As our bipedal ancestors walked on the open savannas of equatorial Africa, the skin on the head would have been an area exposed to the most direct rays of sunlight in an upright hominid. Pubic and armpit hair may have been retained because they served as signs of sexual maturity, which would have been important for successful mating and reproduction.
Evolution of Curly Hair
Greater protection from UV light has also been posited as a possible selective agent favoring the evolution of curly hair. Researchers have found that straight hair allows more light to pass into the body through the hair shaft via the follicle than does curly hair. In this way, human hair is like a fibre optic cable. It allows light to pass through easily when it is straight, but it impedes the passage of light when it is kinked or coiled. This is indirect evidence that UV light may have been a selective agent leading to the evolution of curly hair.
Social and Cultural Significance of Hair
Hair has great social significance for human beings. Body hair is an indicator of biological sex, because hair distribution is sexually dimorphic. Adult males are generally hairier than adult females, and facial hair in particular is a notable secondary male sex characteristic. Hair may also be an indicator of age. White hair is a sign of older age in both males and females, and male pattern baldness is a sign of older age in males. In addition, hair colour and texture can be a sign of ethnic ancestry.
Hair also has great cultural significance. Hairstyle and colour may be an indicator of social group membership and for better or worse can be associated with specific stereotypes. Head shaving has been used in many times and places as a punishment, especially for women. On the other hand, in some cultures, cutting off one’s hair symbolizes liberation from one’s past. In other cultures, it is a sign of mourning. There are also many religious-based practices involving hair. For example, the majority of Muslim women hide their hair with a headscarf. Sikh men grow their hair long and cover it with a turban. Amish men (like the one pictured in Figure 10.5.8) grow facial hair only after they marry — but just a beard, and not a mustache.

Unfortunately, sometimes hairstyle, colour and characteristics are used to apply stereotypes, particularly with respect to women. "Blonde jokes" are a good example of how negative stereotypes are maintained despite having no actual truth behind them. Many stereotypes related to hair are hidden, even from persons perpetrating the stereotype. Often a hairstyle is judged by another as having ties to gender, sexuality, worldview and/or socioeconomic status; even when these inferences are woefully inaccurate. It is important to be aware of our own biases and determine if these biases are appropriate - take a look at the collage in Figure 10.5.9. What are your initial reactions? Are these reactions founded in fact? Do you harbor an unfair bias?
Figure 10.5.9 What are your biases? Are they fair?
10.5 Summary
- Hair is a filament that grows from a hair follicle in the dermis of the skin. It consists mainly of tightly packed, keratin-filled cells called keratinocytes. The human body is almost completely covered with hair follicles.
- The part of a hair that is within the follicle is the hair root. This is the only living part of a hair. The part of a hair that is visible above the skin surface is the hair shaft. It consists of dead cells.
- Hair growth begins inside a follicle when stem cells within the follicle divide to produce new keratinocytes. An individual hair may grow to be very long.
- A hair shaft has three zones: the outermost zone called the cuticle; the middle zone called the cortex; and the innermost zone called the medulla.
- Genetically controlled, visible characteristics of hair include hair colour, hair texture, and the extent of balding in adult males. Melanin (eumelanin and/or pheomelanin) is the pigment that gives hair its colour. Aspects of hair texture include curl pattern, thickness, and consistency.
- Functions of head hair include providing insulation and protecting skin on the head from UV light. Hair everywhere on the body has an important sensory function. Hair in eyelashes and eyebrows protects the eyes from dust, dirt, sweat, and other potentially harmful substances. The eyebrows also play a role in nonverbal communication.
- Among mammals, humans are nearly unique in having undergone significant loss of body hair during their evolution, probably because sweat evaporates more quickly from less hairy skin. Curly hair also is thought to have evolved at some point during human evolution, perhaps because it provided better protection from UV light.
- Hair has social significance for human beings, because it is an indicator of biological sex, age, and ethnic ancestry. Human hair also has cultural significance. Hairstyle may be an indicator of social group membership, for example.
10.5 Review Questions
-
- Compare and contrast the hair root and hair shaft.
- Describe hair follicles.
-
-
- Explain variation in human hair colour.
- What factors determine the texture of hair?
- Describe two functions of human hair.
- What hypotheses have been proposed for the loss of body hair during human evolution?
- Discuss the social and cultural significance of human hair.
- Describe one way in which hair can be used as a method of communication in humans.
- Explain why waxing or tweezing body hair, which typically removes hair down to the root, generally keeps the skin hair-free for a longer period of time than shaving, which cuts hair off at the surface of the skin.
10.5 Explore More
https://www.youtube.com/watch?v=8diYLhl8bWU
Why do some people go bald? - Sarthak Sinha, TED-Ed, 2015.
https://www.youtube.com/watch?v=kNw8V_Fkw28
Hair Love | Oscar®-Winning Short Film (Full) | Sony Pictures Animation, 2019.
https://www.youtube.com/watch?v=hDW5e3NR1Cw
Why do we care about hair | Naomi Abigail | TEDxBaDinh, TEDx Talks, 2015.
Attributions
Figure 10.5.1
Hair by jessica-dabrowski-TETR8YLSqt4 [photo] by Jessica Dabrowski on Unsplash is used under the Unsplash License (https://unsplash.com/license).
Figure 10.5.2
Blausen_0438_HairFollicleAnatomy_02 by BruceBlaus on Wikimedia Commons is used under a CC BY 3.0 (https://creativecommons.org/licenses/by/3.0) license.
Figure 10.5.3
- Standing tall by Ilaya Raja on Unsplash is used under the Unsplash License (https://unsplash.com/license).
- Blond-haired woman smiling by Carlos Lindner on Unsplash is used under the Unsplash License (https://unsplash.com/license).
- Smith Mountain Lake redhead by Chris Ross Harris on Unsplash is used under the Unsplash License (https://unsplash.com/license).
- Through the look of experience by Laura Margarita Cedeño Peralta on Unsplash is used under the Unsplash License (https://unsplash.com/license).
Figure 10.5.4
Curly hair by chris-benson-clvEami9RN4 [photo] by Chris Benson on Unsplash is used under the Unsplash License (https://unsplash.com/license).
Figure 10.5.5
1024px-PilioerectionAnimation by AnthonyCaccese on Wikimedia Commons is used under a CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0/deed.en) license.
Figure 10.5.6
Pout by alexander-dummer-Em8I8Z_DwA4 [photo] by Alexander Dummer on Unsplash is used under the Unsplash License (https://unsplash.com/license).
Figure 10.5.7
Cotton_top_tamarin_monkey._(12046035746) by Bernard Spragg. NZ, from Christchurch, New Zealand on Wikimedia Commons is used under a CC0 1.0 Universal
Public Domain Dedication license (https://creativecommons.org/publicdomain/zero/1.0/deed.en).
Figure 10.5.8
Amish hairstyle by CK-12 Foundation is used under a CC BY-NC 3.0 (https://creativecommons.org/licenses/by-nc/3.0/) license.
 ©CK-12 Foundation Licensed under
©CK-12 Foundation Licensed under ![]() • Terms of Use • Attribution
• Terms of Use • Attribution
Figure 10.5.9
- Rainbow Hair Bubble Man by Behrouz Jafarnezhad on Unsplash is used under the Unsplash License (https://unsplash.com/license).
- Pink hair in Atlanta, United States by Tammie Allen on Unsplash is used under the Unsplash License (https://unsplash.com/license).
- Magdalena 2 by Valerie Elash on Unsplash is used under the Unsplash License (https://unsplash.com/license).
- Perfect Style by Daria Volkova on Unsplash is used under the Unsplash License (https://unsplash.com/license)
- Stay Classy by Fayiz Musthafa on Unsplash is used under the Unsplash License (https://unsplash.com/license)
- Take your time by Jan Tinneberg on Unsplash is used under the Unsplash License (https://unsplash.com/license)
References
Blausen.com staff. (2014). Medical gallery of Blausen Medical 2014. WikiJournal of Medicine 1 (2). DOI:10.15347/wjm/2014.010. ISSN 2002-4436.
Brainard, J/ CK-12 Foundation. (2016). Figure 7 This style of facial hair is adopted by most Amish men after they marry [digital image]. In CK-12 College Human Biology (Section 12.5) [online Flexbook]. CK12.org. https://www.ck12.org/book/ck-12-college-human-biology/section/12.5/
Sony Pictures Animation. (2019, December 5). Hair love | Oscar®-winning short film (Full) | Sony Pictures Animation. YouTube. https://www.youtube.com/watch?v=kNw8V_Fkw28
TED-Ed. (2015, August 25). Why do some people go bald? – Sarthak Sinha. YouTube. https://www.youtube.com/watch?v=8diYLhl8bWU
TEDx Talks. (2015, February 4). Why do we care about hair | Naomi Abigail | TEDxBaDinh. YouTube. https://www.youtube.com/watch?v=hDW5e3NR1Cw
Image shows a diagram of Killer T Cell funtion. An infected cell displays a pathogen antigen on an MHC. The Killer T Cell interacts with the MHC and in response produces perforin ( a protein that pokes holes in cell membranes) and granzymes (proteins that instruct a cell to carry out programmed cell death). The infected cell dies from the combination of these substances, and as it dies, so does the pathogen inside the infected cell. The Killer T Cell is free to move on and find and destroy other infected cells.
An intentional deception for the purpose of humour or malice.
The smallest type of blood vessel that connects arterioles and venules and that transfers substances between blood and tissues.
Glucose (also called dextrose) is a simple sugar with the molecular formula C6H12O6. Glucose is the most abundant monosaccharide, a subcategory of carbohydrates. Glucose is mainly made by plants and most algae during photosynthesis from water and carbon dioxide, using energy from sunlight.
The chemical processes that occur in a living organism to sustain life.
A peptide hormone, produced by alpha cells of the pancreas. It works to raise the concentration of glucose and fatty acids in the bloodstream, and is considered to be the main catabolic hormone of the body. It is also used as a medication to treat a number of health conditions.
Created by CK-12 Foundation/Adapted by Christine Miller

Case Study: Flight Risk
Nineteen-year-old Malcolm is about to take his first plane flight. Shortly after he boards the plane and sits down, a man in his late sixties sits next to him in the aisle seat. About half an hour after the plane takes off, the pilot announces that she is turning the seat belt light off, and that it is safe to move around the cabin.
The man in the aisle seat — who has introduced himself to Malcolm as Willie — immediately unbuckles his seat belt and paces up and down the aisle a few times before returning to his seat. After about 45 minutes, Willie gets up again, walks some more, then sits back down and does some foot and leg exercises. After the third time Willie gets up and paces the aisles, Malcolm asks him whether he is walking so much to accumulate steps on a pedometer or fitness tracking device. Willie laughs and says no. He is actually trying to do something even more important for his health — prevent a blood clot from forming in his legs.
Willie explains that he has a chronic condition: heart failure. Although it sounds scary, his condition is currently well-managed, and he is able to lead a relatively normal lifestyle. However, it does put him at risk of developing other serious health conditions, such as deep vein thrombosis (DVT), which is when a blood clot occurs in the deep veins, usually in the legs. Air travel — and other situations where a person has to sit for a long period of time — increases the risk of DVT. Willie’s doctor said that he is healthy enough to fly, but that he should walk frequently and do leg exercises to help avoid a blood clot.
As you read this chapter, you will learn about the heart, blood vessels, and blood that make up the cardiovascular system, as well as disorders of the cardiovascular system, such as heart failure. At the end of the chapter you will learn more about why DVT occurs, why Willie has to take extra precautions when he flies, and what can be done to lower the risk of DVT and its potentially deadly consequences.
Chapter Overview: Cardiovascular System
In this chapter, you will learn about the cardiovascular system, which transports substances throughout the body. Specifically, you will learn about:
- The major components of the cardiovascular system: the heart, blood vessels, and blood.
- The functions of the cardiovascular system, including transporting needed substances (such as oxygen and nutrients) to the cells of the body, and picking up waste products.
- How blood is oxygenated through the pulmonary circulation, which transports blood between the heart and lungs.
- How blood is circulated throughout the body through the systemic circulation.
- The components of blood — including plasma, red blood cells, white blood cells, and platelets — and their specific functions.
- Types of blood vessels — including arteries, veins, and capillaries — and their functions, similarities, and differences.
- The structure of the heart, how it pumps blood, and how contractions of the heart are controlled.
- What blood pressure is and how it is regulated.
- Blood disorders, including anemia, HIV, and leukemia.
- Cardiovascular diseases (including heart attack, stroke, and angina), and the risk factors and precursors — such as high blood pressure and atherosclerosis — that contribute to them.
As you read the chapter, think about the following questions:
- What is heart failure?Why do you think it increases the risk of DVT?
- What is a blood clot? What are possible health consequences of blood clots?
- Why do you think sitting for long periods of time increases the risk of DVT? Why does walking and exercising the legs help reduce this risk?
Attribution
Figure 14.1.1
aircraft-1583871_1920 [photo] by olivier89 from Pixabay is used under the Pixabay License (https://pixabay.com/de/service/license/).
The evolutionary development and history of a species or trait of a species or of a higher taxonomic grouping of organisms.
The evolutionary development and history of a species or trait of a species or of a higher taxonomic grouping of organisms.
A thin polar membrane made of two layers of phospholipid molecules. These membranes are flat sheets that form a continuous barrier around all cells.
Gland such as a sweat gland, salivary gland, or mammary gland that secretes a substance into a duct that carries the secretion to the outside of the body.
Created by: CK-12/Adapted by Christine Miller

Like Father, Like Son
This father-son duo share some similarities. The shape of their faces and their facial features look very similar. If you saw them together, you might well guess that they are father and son. People have long known that the characteristics of living things are similar between parents and their offspring. However, it wasn’t until the experiments of Gregor Mendel that scientists understood how those traits are inherited.
The Father of Genetics
Mendel did experiments with pea plants to show how traits such as seed shape and flower colour are inherited. Based on his research, he developed his two well known laws of inheritance: the law of segregation and the law of independent assortment. When Mendel died in 1884, his work was still virtually unknown. In 1900, three other researchers working independently came to the same conclusions that Mendel had drawn almost half a century earlier. Only then was Mendel's work rediscovered.
Mendel knew nothing about genes, because they were discovered after his death. He did think, however, that some type of "factors" controlled traits, and that those "factors" were passed from parents to offspring. We now call these "factors" genes. Mendel's laws of inheritance, now expressed in terms of genes, form the basis of genetics, the science of heredity. For this reason, Mendel is often called the father of genetics.
The Language of Genetics
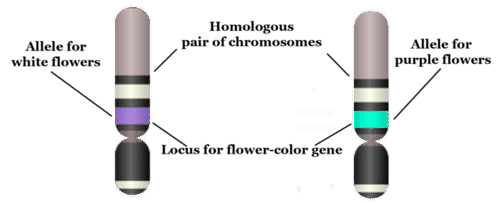
Today, we know that traits of organisms are controlled by genes on chromosomes. To talk about inheritance in terms of genes and chromosomes, you need to know the language of genetics. The terms below serve as a good starting point. They are illustrated in the figure that follows.
- A gene is the part of a chromosome that contains the genetic code for a given protein. For example, in pea plants, a given gene might code for flower colour.
- The position of a given gene on a chromosome is called its locus (plural, loci). A gene might be located near the center, or at one end or the other of a chromosome.
- A given gene may have different normal versions, which are called alleles. For example, in pea plants, there is a purple-flower allele (B) and a white-flower allele (b) for the flower-colour gene. Different alleles account for much of the variation in the traits of organisms, including people.
- In sexually reproducing organisms, each individual has two copies of each type of chromosome. Paired chromosomes of the same type are called homologous chromosomes. They are about the same size and shape, and they have all the same genes at the same loci.
Genotype
When sexual reproduction occurs, sex cells (called gametes) unite during fertilization to form a single cell called a zygote. The zygote inherits two of each type of chromosome, with one chromosome of each type coming from the father, and the other coming from the mother. Because homologous chromosomes have the same genes at the same loci, each individual also inherits two copies of each gene. The two copies may be the same allele or different alleles. The alleles an individual inherits for a given gene make up the individual’s genotype. As shown in Table 5.11.1, an organism with two of the same allele (for example, BB or bb) is called a homozygote. An organism with two different alleles (in this example, Bb) is called a heterozygote.
Table 5.11.1
Allele Combinations Associated With the Terms Homozygous and Heterozygous
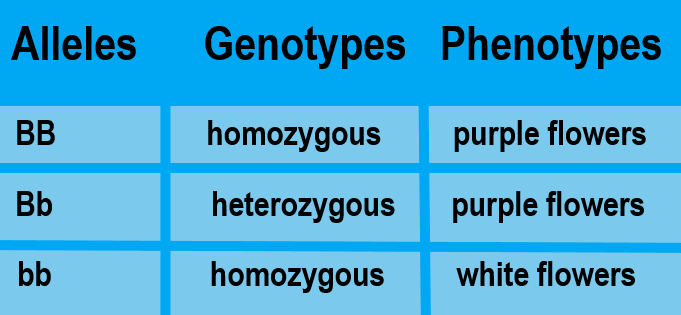
Phenotype
The expression of an organism’s genotype is referred to as its phenotype, and it refers to the organism’s traits, such as purple or white flowers in pea plants. As you can see from Table 5.11.1, different genotypes may produce the same phenotype. In this example, both BB and Bb genotypes produce plants with the same phenotype, purple flowers. Why does this happen? In a Bb heterozygote, only the B allele is expressed, so the b allele doesn’t influence the phenotype. In general, when only one of two alleles is expressed in the phenotype, the expressed allele is called dominant, and the allele that isn’t expressed is called recessive.
The terms dominant and recessive may also be used to refer to phenotypic traits. For example, purple flower colour in pea plants is a dominant trait. It shows up in the phenotype whenever a plant inherits even one dominant allele for the trait. Similarly, white flower colour is a recessive trait. Like other recessive traits, it shows up in the phenotype only when a plant inherits two recessive alleles for the trait.
5.11 Summary
- Mendel's laws of inheritance, now expressed in terms of genes, form the basis of genetics, which is the science of heredity. This is why Mendel is often called the father of genetics.
- A gene is the part of a chromosome that codes for a given protein. The position of a gene on a chromosome is its locus. A given gene may have different versions, called alleles. Paired chromosomes of the same type are called homologous chromosomes. They have the same size and shape, and they have the same genes at the same loci.
- The alleles an individual inherits for a given gene make up the individual's genotype. An organism with two of the same allele is called a homozygote, and an individual with two different alleles is called a heterozygote.
- The expression of an organism's genotype is referred to as its phenotype. A dominant allele is always expressed in the phenotype, even when just one dominant allele has been inherited. A recessive allele is expressed in the phenotype only when two recessive alleles have been inherited.
5.11 Review Questions
- Define genetics.
- Why is Gregor Mendel called the father of genetics if genes were not discovered until after his death?
-
- Imagine that there are two alleles, R and r, for a given gene. R is dominant to r. Answer the following questions about this gene:
- What are the possible homozygous and heterozygous genotypes?
- Which genotype or genotypes express the dominant R phenotype? Explain your answer.
- Are R and r on different loci? Why or why not?
- Can R and r be on the same exact chromosome? Why or why not? If not, where are they located?
5.11 Explore More
https://www.youtube.com/watch?v=pv3Kj0UjiLE
Alleles and Genes, Amoeba Sisters, 2018.
https://www.youtube.com/watch?v=OaovnS7BAoc
Genotypes and Phenotypes, Bozeman Science, 2011.
Attributions
Figure 5.11.1
Father holding his baby boy with matching haircut [photo] by Kelly Sikkema on Unsplash is used under the Unsplash License (https://unsplash.com/license).
Figure 5.11.2
Chromosome, Gene, Locus, and Allele by CK-12 Foundation is used under a CC BY-NC 3.0 (https://creativecommons.org/licenses/by-nc/3.0/) license.
 ©CK-12 Foundation Licensed under
©CK-12 Foundation Licensed under ![]() • Terms of Use • Attribution
• Terms of Use • Attribution
Table 5.11.1
Allele Combinations Associated With the Terms Homozygous and Heterozygous by Christine Miller is released into the public domain (https://en.wikipedia.org/wiki/Public_domain).
References
Amoeba Sisters. (2018, February 1). Alleles and genes. YouTube. https://www.youtube.com/watch?v=pv3Kj0UjiLE&feature=youtu.be
Bozeman Science. (2011, August 4). Genotypes and phenotypes. YouTube. https://www.youtube.com/watch?v=OaovnS7BAoc&feature=youtu.be
Brainard, J/ CK-12 Foundation. (2016). Figure 2 Chromosome, gene, locus, and allele [digital image]. In CK-12 College Human Biology (Section 5.10) [online Flexbook]. CK12.org. https://www.ck12.org/book/ck-12-human-biology/section/5.9/
A groups of mammals characterized by flexible hands and feet, each with five digits, including humans, great apes, monkeys, and lemurs.
Image shows a cartoon from The Awkward Yeti. It depicts a cartoon-ized platelet with a mustache telling another platelet that there has been blood loss in an area. Thee "younger" platelet, upon hearing this gets very excited and declares a "platelet party" and the last frame of the comic is a bunch of platelets with happy faces all stuck to each other.
Image shows a photograph of a toy poodle peeing on a fire hydrant
Any gland of the endocrine system, which is the system of glands that releases hormones directly into the blood.
The ability of an organism to maintain constant internal conditions despite external changes.
A group of diseases involving abnormal cell growth with the potential to invade or spread to other parts of the body.

