8.7 Human Senses
Seeing Is Believing
At first glance, Figure 8.7.1 appears to be just random dots of colour, but hidden within it is the three-dimensional shape of a bee. Can you see it among the dots? This figure is an example of a stereogram, which is a two-dimensional picture that, when viewed correctly, reveals a three-dimensional object. If you can’t see the hidden image, it doesn’t mean that there is anything wrong with your eyes. It’s all in how your brain interprets what your eyes are sensing. The eyes are special sensory organs, and vision is one of our special senses.
Special and General Senses
The human body has two basic types of senses, called special senses and general senses. Special senses have specialized sense organs that gather sensory information and change it into nerve impulses. Special senses include vision (for which the eyes are the specialized sense organs), hearing (ears), balance (ears), taste (tongue), and smell (nasal passages). General senses, in contrast, are all associated with the sense of touch. They lack special sense organs. Instead, sensory information about touch is gathered by the skin and other body tissues, all of which have important functions besides gathering sense information. Whether the senses are special or general, however, they all depend on cells called sensory receptors.
Sensory Receptors
A sensory receptor is a specialized nerve cell that responds to a stimulus in the internal or external environment by generating a nerve impulse. The nerve impulse then travels along the sensory (afferent) nerve to the central nervous system for processing and to form a response.
There are several different types of sensory receptors that respond to different kinds of stimuli:
- Mechanoreceptors respond to mechanical forces, such as pressure, roughness, vibration, and stretching. Most mechanoreceptors are found in the skin and are needed for the sense of touch. Mechanoreceptors are also found in the inner ear, where they are needed for the senses of hearing and balance.
- Thermoreceptors respond to variations in temperature. They are found mostly in the skin and detect temperatures that are above or below body temperature.
- Nociceptors respond to potentially damaging stimuli, which are generally perceived as pain. They are found in internal organs, as well as on the surface of the body. Different nociceptors are activated depending on the particular stimulus. Some detect damaging heat or cold, others detect excessive pressure, and still others detect painful chemicals (such as very hot spices in food).
- Photoreceptors detect and respond to light. Most photoreceptors are found in the eyes and are needed for the sense of vision.
- Chemoreceptors respond to certain chemicals. They are found mainly in taste buds on the tongue — where they are needed for the sense of taste — and in nasal passages, where they are needed for the sense of smell.
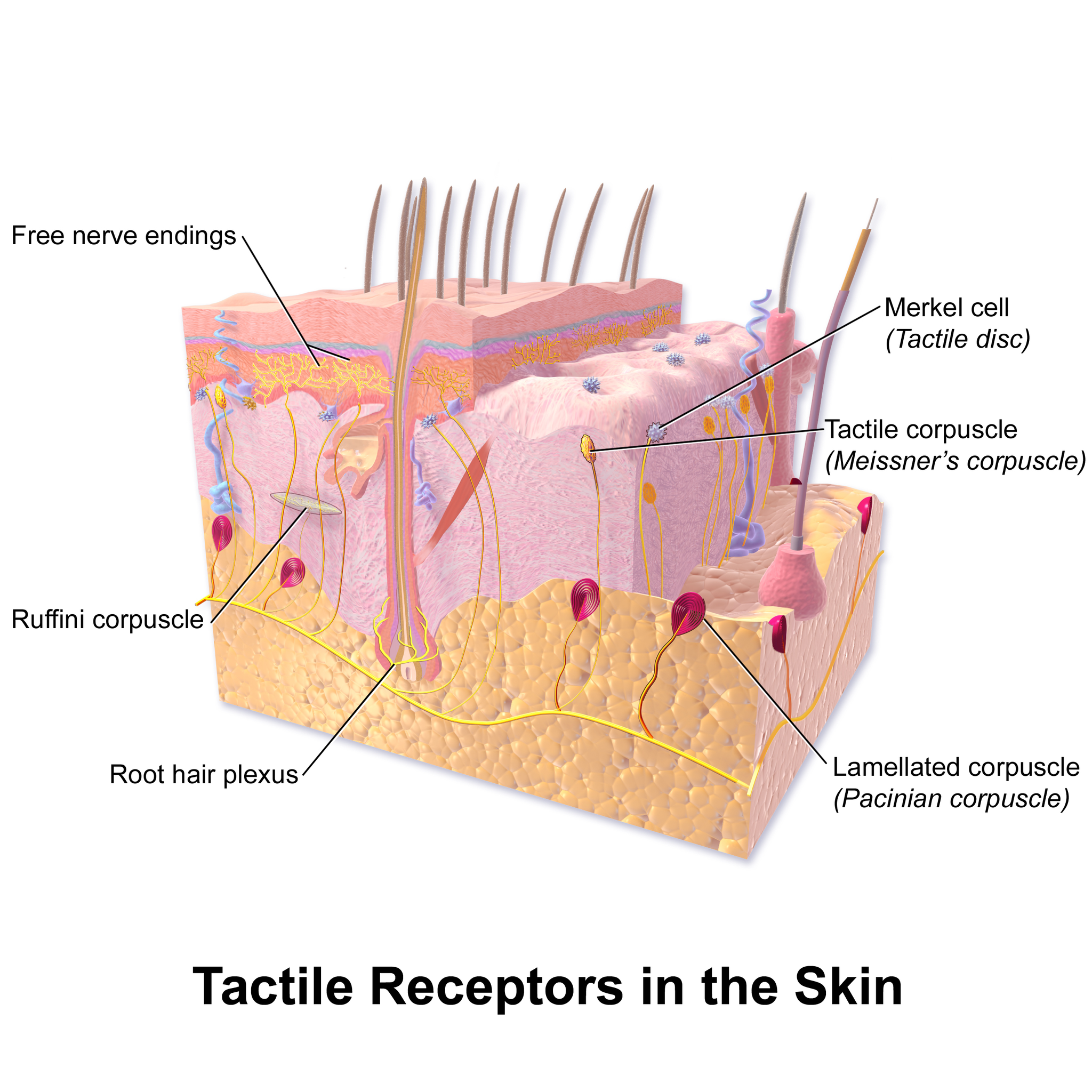
Touch
Touch is the ability to sense pressure, vibration, temperature, pain, and other tactile stimuli. These types of stimuli are detected by mechanoreceptors, thermoreceptors, and nociceptors all over the body, most noticeably in the skin. These receptors are especially concentrated on the tongue, lips, face, palms of the hands, and soles of the feet. Various types of tactile receptors in the skin are shown in Figure 8.7.2.

Vision
Vision (or sight) is the ability to sense light and see. The eye is the special sensory organ that collects and focuses light and forms images. The eye, however, is not sufficient for us to see. The brain also plays a necessary role in vision. Vision is our primary sense and more than 50 per cent of the cerebral cortex is devoted to processing visual information. A person with normal colour vision can differentiate between hundreds of thousands of different colours, hues, and shades.
How the Eye Works
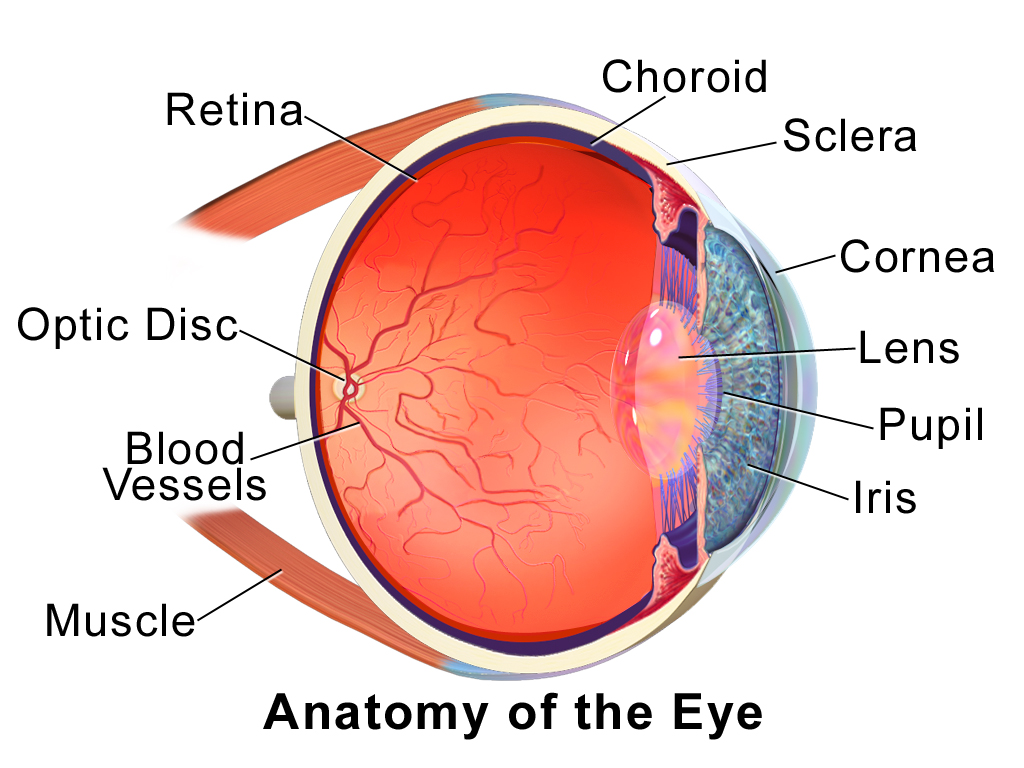
Figure 8.7.4 (below) shows the anatomy of the human eye in cross-section. The eye gathers and focuses light to form an image, and then changes the image to nerve impulses that travel to the brain. The eye’s functions are summarized in the following steps.
- Light passes first through the cornea, which is a clear outer layer that protects the eye and helps to focus the light by refracting (or bending) it.
- Next, light enters the interior of the eye through an opening called the pupil. The size of this opening is controlled by the coloured part of the eye (called the iris), which adjusts the size based on the brightness of the light. The iris causes the pupil to narrow in bright light and widen in dim light. Filling the space between the cornea and the iris is a semi-gelatinous fluid called aqueous humor and functions to maintain the shape of the eye.
- The light then passes through the lens, which refracts the light even more and focuses it on the retina at the back of the eye, as an inverted image. Sitting behind the lens is a gelatinous fluid called vitreous humor, which functions to maintain the shape of the eye.
- The retina contains two types of photoreceptors: rod and cone cells . Rod cells, which are found mainly in all areas of the retina other than the very center, are particularly sensitive to low levels of light. Cone cells, which are found mainly in the center of the retina, are sensitive to light of different colours, and allow colour vision. The rods and cones convert the light that strikes them to nerve impulses.
- The nerve impulses from the rods and cones travel to the optic nerve via the optic disc (also known as the optic nerve), which is a circular area at the back of the eye where the optic nerve connects to the retina.
Colour Vision
Humans have colour vision because we have three types of cone cells: blue, green and red. Each of these types of cone cell detects a specific wavelength of light, for which they are named. The combined stimulus is then perceived as a specific colour, based on the ratio of the amount stimulus coming from each of the three types of cone cells. Do you know what else uses these same three pieces of information to communicate colour? Your computer monitor! When working in a creative program, such as Paint, these three reference points of red (R), green (G), and blue (B), can be used to create any of the million colours the human eye can perceive, as illustrated in Figure 8.7.5. Take a look at each of the numerical values for red, green, and blue and what colour their combined values create:
Figure 8.7.5 RGB colours.
Role of the Brain in Vision
The optic nerves from both eyes meet and cross just below the bottom of the hypothalamus in the brain. The information from both eyes is sent to the visual cortex in the occipital lobe of the cerebrum, which is part of the cerebral cortex. The visual cortex is the largest system in the human brain, and is responsible for processing visual images. It interprets messages from both eyes and “tells” us what we are seeing.
Vision Problems
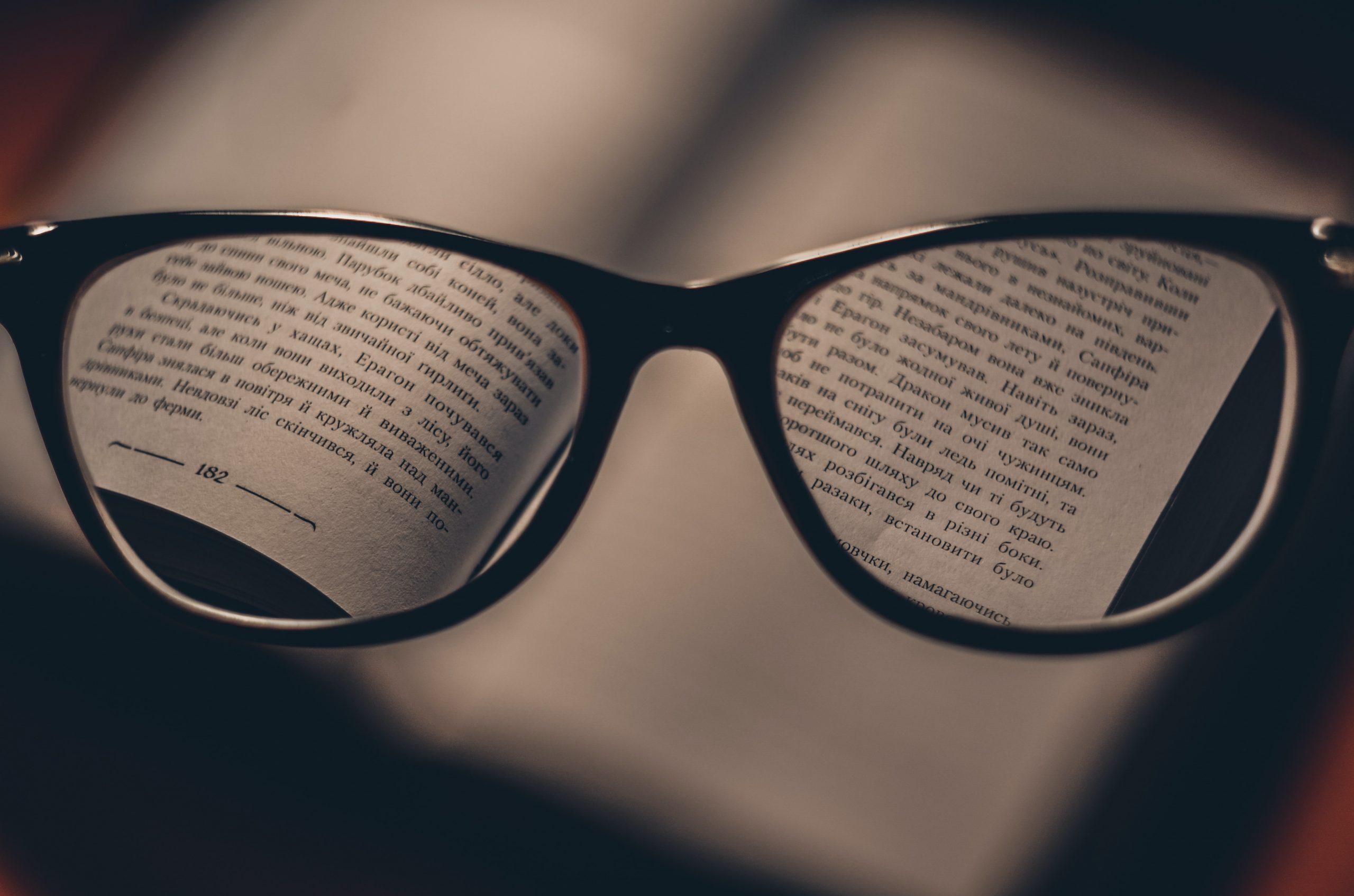
Vision problems are very common. Two of the most common are myopia and hyperopia, and they often start in childhood or adolescence. Another common problem, called presbyopia, occurs in most people, beginning in middle adulthood. In all three conditions, the eyes fail to focus images correctly on the retina, resulting in blurred vision.
Myopia
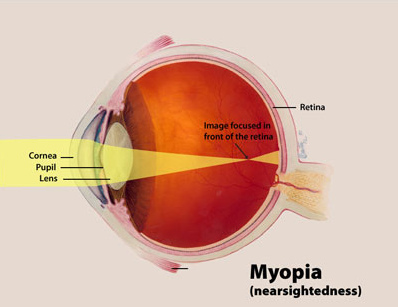
Myopia (or nearsightedness) occurs when the light that comes into the eye does not directly focus on the retina, but in front of it, as shown in Figure 8.7.7. As a result, distant objects may appear out of focus, but the focus of close objects is not affected. Myopia may occur because the eyeball is elongated from front to back, or because the cornea is too curved. Myopia can be corrected with the use of corrective lenses, either eyeglasses or contact lenses. Myopia can also be corrected by refractive surgery performed with a laser.
Hyperopia
Hyperopia (or farsightedness) happens when the light coming into the eye does not directly focus on the retina but behind it, as shown in Figure 8.7.8. This causes close objects to appear out of focus, but does not affect the focus of distant objects. Hyperopia may occur because the eyeball is too short from front to back, or because the lens is not curved enough. Hyperopia can be corrected through the use of corrective lenses or laser surgery.
Presbyopia
Presbyopia is a vision problem associated with aging, in which the eye gradually loses its ability to focus on close objects. The precise origin of presbyopia is not known for certain, but evidence suggests that the lens may become less elastic with age, causing the muscles that control the lens to lose power as people grow older. The first signs of presbyopia — eyestrain, difficulty seeing in dim light, problems focusing on small objects and fine print — are usually first noticed between the ages of 40 and 50. Most older people with this problem use corrective lenses to focus on close objects, because surgical procedures to correct presbyopia have not been as successful as those for myopia and hyperopia.
Hearing
Hearing is the ability to sense sound waves, and the ear is the organ that senses sound. Sound waves enter the ear through the ear canal and travel to the eardrum (see the diagram of the ear Figure 8.7.9). The sound waves strike the eardrum, and make it vibrate. The vibrations then travel through the three tiny bones (incus, malleus and stapes) of the middle ear, which amplify the vibrations. From the middle ear, the vibrations pass to the cochlea in the inner ear. The cochlea is a coiled tube filled with liquid. The liquid moves in response to the vibrations, causing tiny hair cells(which are mechanoreceptors) lining the cochlea to bend. In response, the hair cells send nerve impulses to the auditory nerve, which carries the impulses to the brain. The brain interprets the impulses and “tells” us what we are hearing.
Balance
The ears are also responsible for the sense of balance. Balance is the ability to sense and maintain an appropriate body position. The semicircular canals inside the ear (see the figure above) contain fluid that moves when the head changes position. Tiny hairs lining the semicircular canals sense movement of the fluid. In response, they send nerve impulses to the vestibular nerve, which carries the impulses to the brain. The brain interprets the impulses and sends messages to the peripheral nervous system, which triggers contractions of skeletal muscles as needed to maintain balance.
Taste and Smell
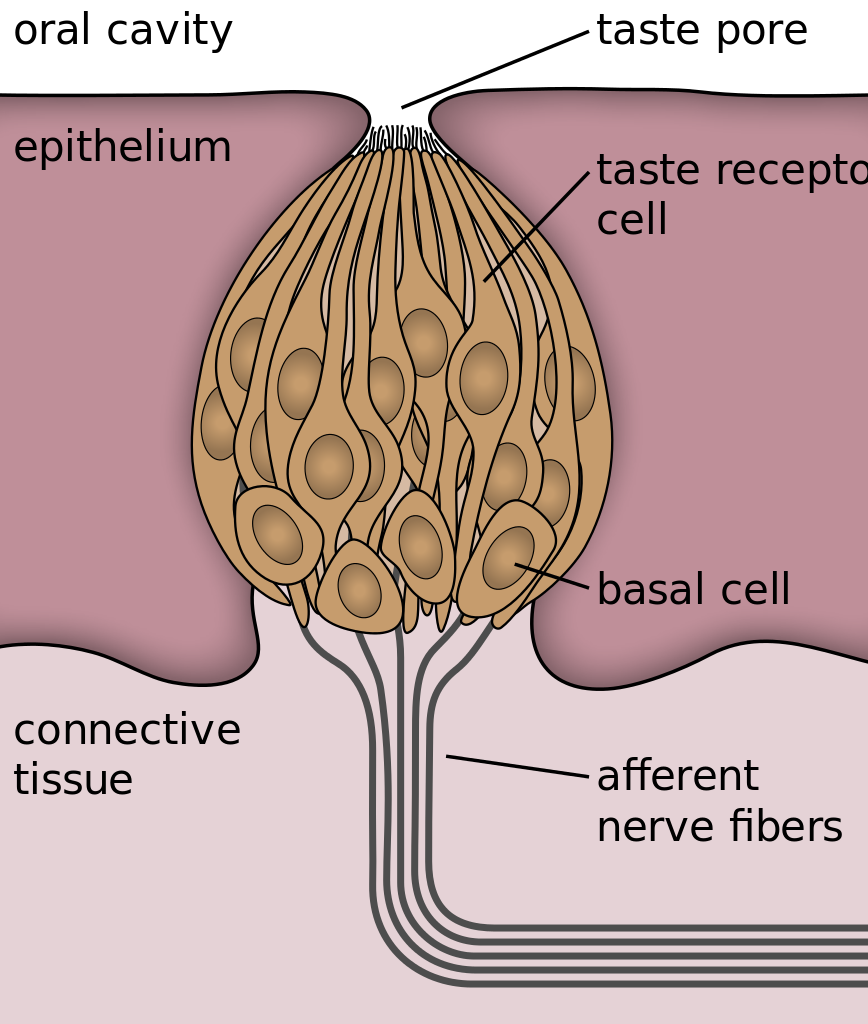
Taste and smell are both abilities to sense chemicals, so both taste and olfactory (odor) receptors are chemoreceptors. Both types of chemoreceptors send nerve impulses to the brain along sensory nerves, and the brain “tells” us what we are tasting or smelling.
Taste receptors are found in tiny bumps on the tongue called taste buds.You can see a diagram of a taste receptor cell and related structures in Figure 8.7.10. Taste receptor cells make contact with chemicals in food through tiny openings called taste pores. When certain chemicals bind with taste receptor cells, it generates nerve impulses that travel through afferent nerves to the CNS. There are separate taste receptors for sweet, salty, sour, bitter, and meaty tastes. The meaty — or savory — taste is called umami.
Feature: Human Biology in the News
The most common cause of blindness in the Western hemisphere is age-related macular degeneration (AMD). Approximately 1.4 million people in Canada have this type of blindness, and 196 million people are affected worldwide and is expected to increase to 288 millions people by the year 2040. At present, there is no cure for AMD. The disease occurs with the death of a layer of cells called retinal pigment epithelium, which normally provides nutrients and other support to the macula of the eye. The macula is an oval-shaped pigmented area near the center of the retina that is specialized for high visual acuity and has the retina’s greatest concentration of cones. When the epithelial cells die and the macula is no longer supported or nourished, the macula also starts to die. Patients experience a black spot in the center of their vision, and as the disease progresses, the black spot grows outward. Patients eventually lose the ability to read and even to recognize familiar faces before developing total blindness.
In 2016, a landmark surgery was performed as a trial on a patient with severe AMD. In the first ever operation of its kind, Dr. Pete Coffey of the University of London implanted a tiny patch of cells behind the retina in each of the patient’s eyes. The cells were retinal pigmented epithelial cells that had been grown in a lab from stem cells, which are undifferentiated cells that can develop into other cell types. Within six months of the operation, the new cells were still surviving, and the doctor was hopeful that the patient’s vision loss would stop and even be reversed. At that point, several other operations had already been planned to test the new procedure. If these cases are a success, Dr. Coffey predicts that the surgery will become as routine as cataract surgery, and that it will prevent millions of patients from losing their vision.
8.7 Summary
- The human body has two major types of senses: special senses and general senses. Special senses have specialized sense organs and include vision (eyes), hearing (ears), balance (ears), taste (tongue), and smell (nasal passages). General senses are all associated with touch and lack special sense organs. Touch receptors are found throughout the body, but particularly in the skin.
- All senses depend on sensory receptor cells to detect sensory stimuli and transform them into nerve impulses. Types of sensory receptors include mechanoreceptors (mechanical forces), thermoreceptors (temperature), nociceptors (pain), photoreceptors (light), and chemoreceptors (chemicals).
- Touch is the ability to sense pressure, vibration, temperature, pain, and other tactile stimuli. The skin includes several different types of touch receptor cells.
- Vision is the ability to sense light and see. The eye is the special sensory organ that collects and focuses light, forms images, and changes them to nerve impulses. Optic nerves send information from the eyes to the brain, which processes the visual information and “tells” us what we are seeing.
- Common vision problems include myopia (nearsightedness), hyperopia (farsightedness), and presbyopia (age-related decline in close vision). Vision problems can be corrected with lenses (eyeglasses or contacts) or — in many cases — with laser surgery.
- Hearing is the ability to sense sound waves, and the ear is the organ that senses sound. It changes sound waves to vibrations that trigger nerve impulses, which travel to the brain through the auditory nerve. The brain processes the information and “tells” us what we are hearing.
- The ear is also the organ responsible for the sense of balance, which is the ability to sense and maintain an appropriate body position. The ears send impulses about head position to the brain, which sends messages to skeletal muscles via the peripheral nervous system. The muscles respond by contracting to maintain balance.
- Taste and smell are both abilities to sense chemicals. Taste receptors in taste buds on the tongue sense chemicals in food, while olfactory receptors in the nasal passages sense chemicals in the air. Sense of smell contributes significantly to sense of taste.
8.7 Review Questions
-
- Compare and contrast special senses and general senses.
- What are sensory receptors?
-
- Describe the range of tactile stimuli detected in the sense of touch.
- Explain how the eye collects and focuses light to form an image, and how it converts it to nerve impulses.
- Identify two common vision problems,along with their causes and their effects on vision.
-
- Explain how structures of the ear collect and amplify sound waves and transform them to nerve impulses.
- What role does the ear play in balance? Which structures of the ear are involved in balance?
- Describe two ways that the body senses chemicals. What are the special sense organs involved in these senses?
- Explain why your skin can detect different types of stimuli, such as pressure and temperature.
- Is sensory information sent to the central nervous system via efferent or afferent nerves?
- Identify a mechanoreceptor used in two different human senses. Describe the type of mechanical stimuli that each detects.
- If a person is blind, but their retina is functioning properly, where do you think the damage might be? Explain your answer.
- When you see colours, what receptor cells are activated? Where are these receptors located? What lobe of the brain is primarily used to process visual information?
- The auditory nerve carries _______________.
-
-
- smell information
- taste information
- balance information
- sound information
-
8.7 Explore More
What color is Tuesday? Exploring synesthesia – Richard E. Cytowic, TED-Ed, 2013.
What Is Vertigo & Why Do We Get It?, Seeker, 2016.
How do animals see in the dark? – Anna Stöckl, TED-Ed, 2016.
What are those floaty things in your eye? – Michael Mauser, TED-Ed, 2014.
Attributions
Figure 8.7.1
Bee Stereogram by Be Mosaic on Flickr is used under a CC BY-NC-SA 2.0 (https://creativecommons.org/licenses/by-nc-sa/2.0/) license.
Figure 8.7.2
Skin_TactileReceptors by BruceBlaus on Wikimedia Commons is used under a CC BY 3.0 (https://creativecommons.org/licenses/by/3.0) license.
Figure 8.7.3
Macro shot photograph of someone’s right eye [photo] by Jordan Whitfield on Unsplash is used under the Unsplash License (https://unsplash.com/license).
Figure 8.7.4
EyeAnatomy_01 by BruceBlaus on Wikimedia Commons is used under a CC BY 3.0 (https://creativecommons.org/licenses/by/3.0) license.
Figure 8.7.5
RGB colours [screenshots] from Microsoft Paint.
Figure 8.7.6
Through the reading glasses [photo] by Dmitry Ratushny on Unsplash is used under the Unsplash License (https://unsplash.com/license).
Figure 8.7.7
Myopia_Diagram by National Eye Institute/ National Institutes of Health on Wikimedia Commons is used under a CC BY 2.0 (https://creativecommons.org/licenses/by/2.0) license.
Figure 8.7.8
Hyperopia by National Institute of Health/NIH on Wikimedia Commons is in the public domain (https://en.wikipedia.org/wiki/Public_domain).
Figure 8.7.9
AnatomyHumanEar by unknown author from Occupational Safety & Health Administration on Wikimedia Commons is in the public domain (https://en.wikipedia.org/wiki/Public_domain).
Figure 8.7.10
Taste_bud_2_eng.svg by Jonas Töle on Wikimedia Commons is used under a CC0 1.0 Universal Public Domain Dedication license (https://creativecommons.org/publicdomain/zero/1.0/deed.en).
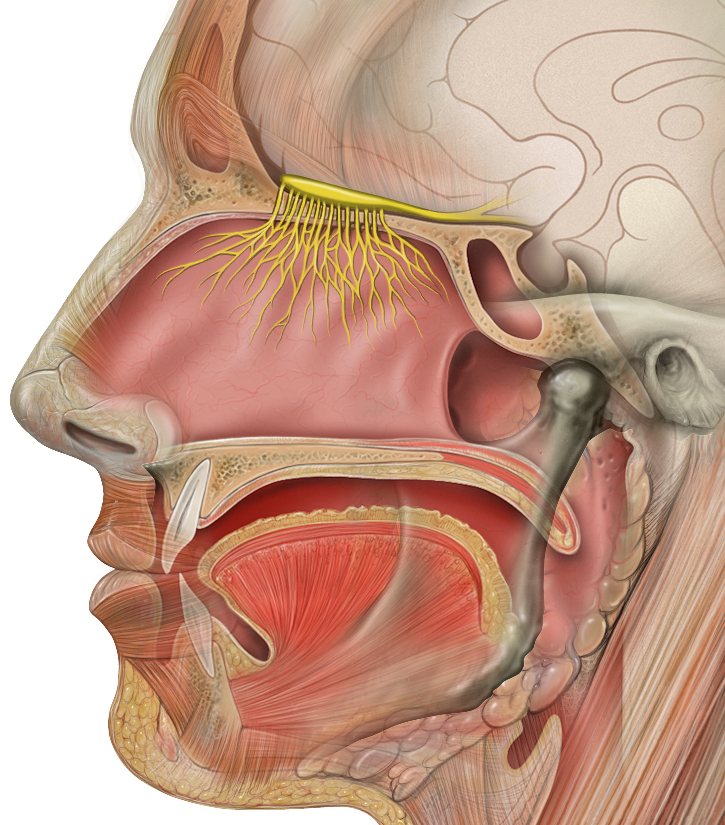
Figure 8.7.11
Head_olfactory_nerve by Patrick.lynch, medical illustrator on Wikimedia Commons is used under a CC BY 2.5 (https://creativecommons.org/licenses/by/2.5/deed.en) license.
References
Age-Related Macular Degeneration. (n.d.). WebMD. https://www.webmd.com/eye-health/macular-degeneration/age-related-macular-degeneration-overview#3 (Reviewed by Alan Kozarsky, MD on October 26, 2019)
Blausen.com Staff. (2014). Medical gallery of Blausen Medical 2014. WikiJournal of Medicine 1 (2). DOI:10.15347/wjm/2014.010. ISSN 2002-4436.
da Cruz, L., Fynes, K., Georgiadis, O. et al. (2018, March 19). Phase 1 clinical study of an embryonic stem cell–derived retinal pigment epithelium patch in age-related macular degeneration. Natural Biotechnology, 36, 328–337. https://doi.org/10.1038/nbt.4114
File:Eye Diagram without text.gif. (2018, February 9). Wikimedia Commons. https://commons.wikimedia.org/w/index.php?title=File:Eye_Diagram_without_text.gif&oldid=286008241 (original image from National Eye Institute – modified by User:Nordelch) [public domain (https://en.wikipedia.org/wiki/Public_domain)]
Occupational Health and Safety Administration. (n.d.). Figure 7. Anatomy of the human ear [diagram]. In OSHA Technical Manual (Section III, Chapter 5 – Noise). United States Department of Labour [online]. https://www.osha.gov/dts/osta/otm/new_noise/
Seeker. (2016, March 18). What is vertigo & why do we get it? YouTube. https://www.youtube.com/watch?v=UL8YSLhqa5U&feature=youtu.be
TED-Ed. (2013, June 10). What color is Tuesday? Exploring synesthesia – Richard E. Cytowic. YouTube. https://www.youtube.com/watch?v=rkRbebvoYqI&feature=youtu.be
TED-Ed. (2014, December 1). What are those floaty things in your eye? – Michael Mauser. YouTube. https://www.youtube.com/watch?v=Y6e_m9iq-4Q&feature=youtu.be
TED-Ed. (2016, August 25). How do animals see in the dark? – Anna Stöckl. YouTube. https://www.youtube.com/watch?v=t3CjTU7TaNA&feature=youtu.be
Created by CK-12 Foundation/Adapted by Christine Miller

Getting Rid of Wastes
The many chimneys on these houses are one way that the inhabitants of the home get rid of the wastes they produce. The chimneys expel waste gases that are created when they burn fuel in their furnace or fireplace. Think about the other wastes that people create in their homes and how we dispose of them. Solid trash and recyclables may go to the curb in a trash can, or in a recycling bin for pick up and transport to a landfill or recycling centre. Wastewater from sinks, showers, toilets, and the washing machine goes into a main sewer pipe and out of the house to join the community’s sanitary sewer system.
Like a busy home, your body also produces a lot of wastes that must be eliminated. Like a home, the way your body gets rid of wastes depends on the nature of the waste products. Some human body wastes are gases, some are solids, and some are in a liquid state. Getting rid of body wastes is called excretion, and there are a number of different organs of excretion in the human body.
Excretion
Excretion is the process of removing wastes and excess water from the body. It is an essential process in all living things, and it is one of the major ways the human body maintains homeostasis. It also helps prevent damage to the body. Wastes include by-products of metabolism — some of which are toxic — and other non-useful materials, such as used up and broken down components. Some of the specific waste products that must be excreted from the body include carbon dioxide from cellular respiration, ammonia and urea from protein catabolism, and uric acid from nucleic acid catabolism.
Excretory Organs
Organs of excretion include the skin, liver, large intestine, lungs, and kidneys (see Figure 16.2.2). Together, these organs make up the excretory system. They all excrete wastes, but they don’t work together in the same way that organs do in most other body systems. Each of the excretory organs “does its own thing” more-or-less independently of the others, but all are necessary to successfully excrete the full range of wastes from the human body.
Figure 16.2.2 Internal organs of excretion are identified in this illustration. They include the skin, liver, large intestine, lungs, and kidneys.
Skin

The skin is part of the integumentary system, but it also plays a role in excretion through the production of sweat by sweat glands in the dermis. Although the main role of sweat production is to cool the body and maintain temperature homeostasis, sweating also eliminates excess water and salts, as well as a small amount of urea. When sweating is copious, as in Figure 16.2.3, ingestion of salts and water may be helpful to maintain homeostasis in the body.
Liver
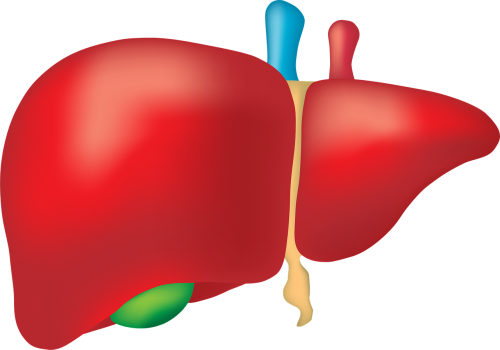
The liver (shown in Figure 16.2.4) has numerous major functions, including secreting bile for digestion of lipids, synthesizing many proteins and other compounds, storing glycogen and other substances, and secreting endocrine hormones. In addition to all of these functions, the liver is a very important organ of excretion. The liver breaks down many substances in the blood, including toxins. For example, the liver transforms ammonia — a poisonous by-product of protein catabolism — into urea, which is filtered from the blood by the kidneys and excreted in urine. The liver also excretes in its bile the protein bilirubin, a byproduct of hemoglobin catabolism that forms when red blood cells die. Bile travels to the small intestine and is then excreted in feces by the large intestine.
Large Intestine
The large intestine is an important part of the digestive system and the final organ in the gastrointestinal tract. As an organ of excretion, its main function is to eliminate solid wastes that remain after the digestion of food and the extraction of water from indigestible matter in food waste. The large intestine also collects wastes from throughout the body. Bile secreted into the gastrointestinal tract, for example, contains the waste product bilirubin from the liver. Bilirubin is a brown pigment that gives human feces its characteristic brown colour.
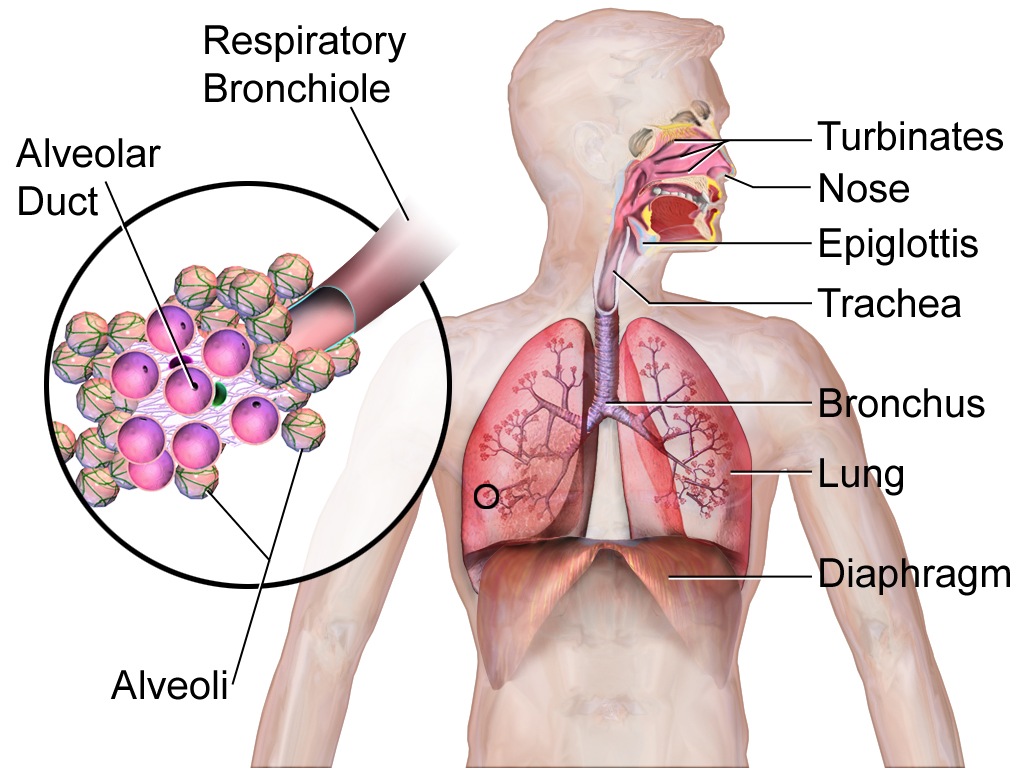
Lungs
The lungs are part of the respiratory system (shown in Figure 16.2.5), but they are also important organs of excretion. They are responsible for the excretion of gaseous wastes from the body. The main waste gas excreted by the lungs is carbon dioxide, which is a waste product of cellular respiration in cells throughout the body. Carbon dioxide is diffused from the blood into the air in the tiny air sacs called alveoli in the lungs (shown in the inset diagram). By expelling carbon dioxide from the blood, the lungs help maintain acid-base homeostasis. In fact, it is the pH of blood that controls the rate of breathing. Water vapor is also picked up from the lungs and other organs of the respiratory tract as the exhaled air passes over their moist linings, and the water vapor is excreted along with the carbon dioxide. Trace levels of some other waste gases are exhaled, as well.
Kidneys
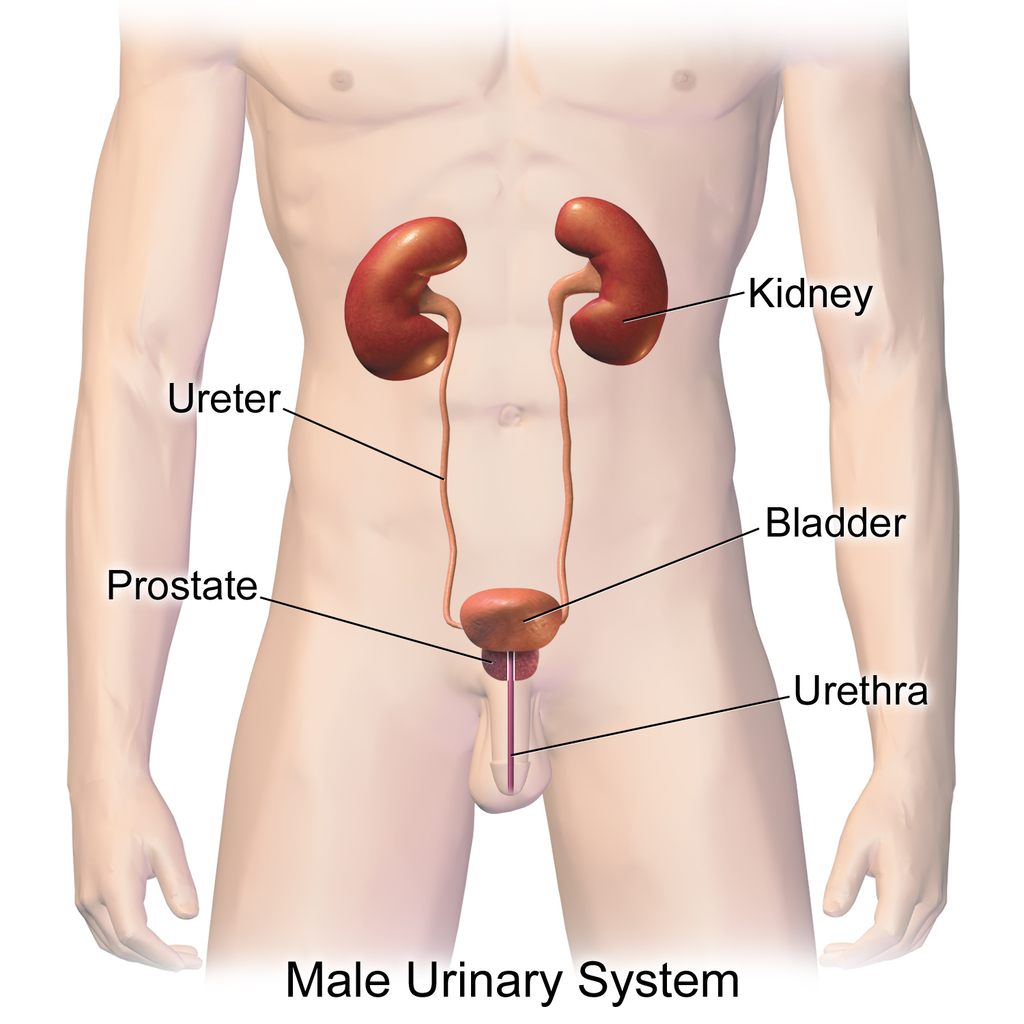
The paired kidneys are often considered the main organs of excretion. The primary function of the kidneys is the elimination of excess water and wastes from the bloodstream by the production of the liquid waste known as urine. The main structural and functional units of the kidneys are tiny structures called nephrons. Nephrons filter materials out of the blood, return to the blood what is needed, and excrete the rest as urine. As shown in Figure 16.2.6, the kidneys are organs of the urinary system, which also includes the ureters, bladder, and urethra — organs that transport, store, and eliminate urine, respectively.
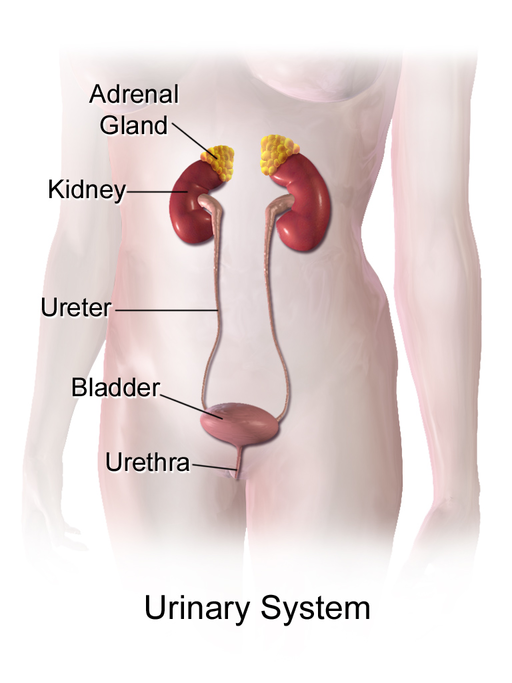
By producing and excreting urine, the kidneys play vital roles in body-wide homeostasis. They maintain the correct volume of extracellular fluid, which is all the fluid in the body outside of cells, including the blood and lymph. The kidneys also maintain the correct balance of salts and pH in extracellular fluid. In addition, the kidneys function as endocrine glands, secreting hormones into the blood that control other body processes. You can read much more about the kidneys in section 16.4 Kidneys.
16.2 Summary
- Excretion is the process of removing wastes and excess water from the body. It is an essential process in all living things and a major way the human body maintains homeostasis.
- Organs of excretion include the skin, liver, large intestine, lungs, and kidneys. All of them excrete wastes, and together they make up the excretory system.
- The skin plays a role in excretion through the production of sweat by sweat glands. Sweating eliminates excess water and salts, as well as a small amount of urea, a byproduct of protein catabolism.
- The liver is a very important organ of excretion. The liver breaks down many substances in the blood, including toxins. The liver also excretes bilirubin — a waste product of hemoglobin catabolism — in bile. Bile then travels to the small intestine, and is eventually excreted in feces by the large intestine.
- The main excretory function of the large intestine is to eliminate solid waste that remains after food is digested and water is extracted from the indigestible matter. The large intestine also collects and excretes wastes from throughout the body, including bilirubin in bile.
- The lungs are responsible for the excretion of gaseous wastes, primarily carbon dioxide from cellular respiration in cells throughout the body. Exhaled air also contains water vapor and trace levels of some other waste gases.
- The paired kidneys are often considered the main organs of excretion. Their primary function is the elimination of excess water and wastes from the bloodstream by the production of urine. The kidneys contain tiny structures called nephrons that filter materials out of the blood, return to the blood what is needed, and excrete the rest as urine. The kidneys are part of the urinary system, which also includes the ureters, urinary bladder, and urethra.
16.2 Review Questions
- What is excretion, and what is its significance?
-
- Describe the excretory functions of the liver.
- What are the main excretory functions of the large intestine?
- List organs of the urinary system.
- Describe the physical states in which the wastes from the human body are excreted.
- Give one example of why ridding the body of excess water is important.
- What gives feces its brown colour? Why is that substance produced?
16.2 Explore More
https://www.youtube.com/watch?v=erMCADOJcHk&feature=youtu.be
Why Can We Regrow A Liver (But Not A Limb)? MITK12Videos, 2015.
https://www.youtube.com/watch?v=SeK0zFB9yHg&feature=youtu.be
Are Sports Drinks Good For You? | Fit or Fiction, POPSUGAR Fitness, 2014.
https://www.youtube.com/watch?v=fctH_1NuqCQ&feature=youtu.be
Why do we sweat? - John Murnan, TED-Ed, 2018.
Attributions
Figure 16.2.1
Chimneys/ Kingston upon Hull, England [photo] by Angela Baker on Unsplash is used under the Unsplash License (https://unsplash.com/license).
Figure 16.2.2
- Sweat or rain? by Kullez on Flickr is used under a CC BY 2.0 (https://creativecommons.org/licenses/by/2.0/).
- Kidney front - white from www.medicalgraphics.de is used under a CC BY-ND 4.0 (https://creativecommons.org/licenses/by-nd/4.0/) license.
- File:Liver Cirrhosis.png by BruceBlaus on Wikimedia Commons is used under a CC BY SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0/deed.en) license.
- File:Human lungs.png by Sharanyaudupa on Wikimedia Commons is used under a CC BY SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0/deed.en) license.
- Tags: Offal Marking Medical Intestine Liver by Elionas2 on Pixabay is used under the Pixabay license (https://pixabay.com/service/license/).
Figure 16.2.3
gym_room_fitness_equipment_cardiovascular_exercise_elliptical_bike_cardio_training_sports_equipment_bodybuilding-825364 from Pxhere is used under a CC0 1.0 Universal public domain dedication license (https://creativecommons.org/publicdomain/zero/1.0/).
Figure 16.2.4
Tags: Liver Organ Anatomy by zachvanstone8 on Pixabay is used under the Pixabay License (https://pixabay.com/service/license/).
Figure 16.2.5
Lung_and_diaphragm by Terese Winslow/ National Cancer Institute on Wikimedia Commons is in the public domain (https://en.wikipedia.org/wiki/Public_domain).
Figure 16.2.6
512px-Urinary_System_(Female) by BruceBlaus on Wikimedia Commons is used under a CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0) license.
References
MITK12Videos. (2015, June 4). Why can we regrow a liver (but not a limb)? https://www.youtube.com/watch?v=erMCADOJcHk&feature=youtu.be
POPSUGAR Fitness. (2014, February 7). Are sports drinks good for you? | Fit or Fiction. YouTube. https://www.youtube.com/watch?v=SeK0zFB9yHg&feature=youtu.be
TED-Ed. (2018, May 15). Why do we sweat? - John Murnan. YouTube. https://www.youtube.com/watch?v=fctH_1NuqCQ&feature=youtu.be
As per caption
Image shows a detailed labelled diagram of a kidney. There is a tough outer layer called the capsule. The cortex contains blood vessels and the medulla contains nephrons. The renal artery brings blood from the heart to the kidney, and this blood is returned to the heart via the renal vein.
Created by CK-12 Foundation/Adapted by Christine Miller

Vampires
From Bram Stoker’s famous novel about Count Dracula, to films such as Van Helsing and the Twilight Saga, fantasies featuring vampires (like the one in Figure 14.5.1) have been popular for decades. Vampires, in fact, are found in centuries-old myths from many cultures. In such myths, vampires are generally described as creatures that drink blood — preferably of the human variety — for sustenance. Dracula, for example, is based on Eastern European folklore about a human who attains immortality (and eternal damnation) by drinking the blood of others.
What Is Blood?
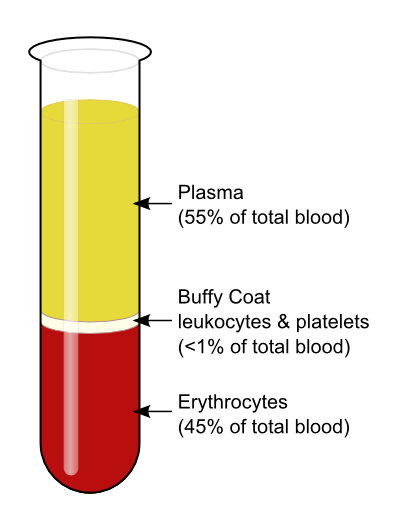
The average adult body contains between 4.7 and 5.7 litres of blood. More than half of that amount is fluid. Most of the rest of that amount consists of blood cells. The relative amounts of the various components in blood are illustrated in Figure 14.5.2. The components are also described in detail below.
Blood is a fluid connective tissue that circulates throughout the body through blood vessels of the cardiovascular system. What makes blood so special that it features in widespread myths? Although blood accounts for less than 10% of human body weight, it is quite literally the elixir of life. As blood travels through the vessels of the cardiovascular system, it delivers vital substances (such as nutrients and oxygen) to all of the cells, and carries away their metabolic wastes. It is no exaggeration to say that without blood, cells could not survive. Indeed, without the oxygen carried in blood, cells of the brain start to die within a matter of minutes.
Functions of Blood
Blood performs many important functions in the body. Major functions of blood include:
- Supplying tissues with oxygen, which is needed by all cells for aerobic cellular respiration.
- Supplying cells with nutrients, including glucose, amino acids, and fatty acids.
- Removing metabolic wastes from cells, including carbon dioxide, urea, and lactic acid.
- Helping to defend the body from pathogens and other foreign substances.
- Forming clots to seal broken blood vessels and stop bleeding.
- Transporting hormones and other messenger molecules.
- Regulating the pH of the body, which must be kept within a narrow range (7.35 to 7.45).
- Helping regulate body temperature (through vasoconstriction and vasodilation).
Blood Plasma
Plasma is the liquid component of human blood. It makes up about 55% of blood by volume. It is about 92% water, and contains many dissolved substances. Most of these substances are proteins, but plasma also contains trace amounts of glucose, mineral ions, hormones, carbon dioxide, and other substances. In addition, plasma contains blood cells. When the cells are removed from plasma, as in Figure 14.5.2 above, the remaining liquid is clear but yellow in colour.
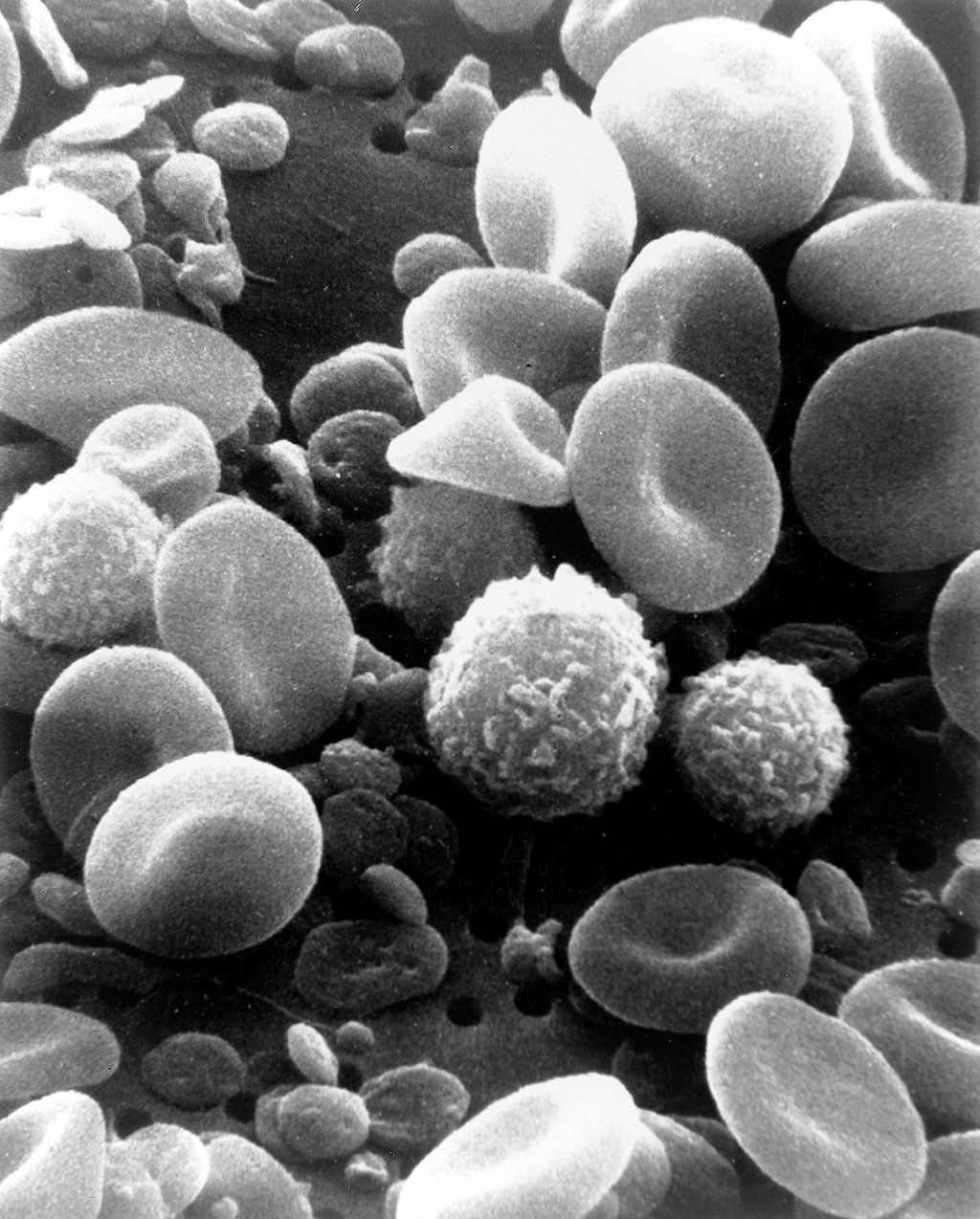
Blood Cells
The cells in blood include erythrocytes, leukocytes, and thrombocytes. These different types of blood cells are shown in the photomicrograph (Figure 14.5.3) and described in the sections that follow.
Erythrocytes
The most numerous cells in blood are red blood cells, also called erythrocytes. One microlitre of blood contains between 4.2 and 6.1 million red blood cells, and red blood cells make up about 25% of all the cells in the human body. The cytoplasm of a mature erythrocyte is almost completely filled with hemoglobin, the iron-containing protein that binds with oxygen and gives the cell its red colour. In order to provide maximum space for hemoglobin, mature erythrocytes lack a cell nucleus and most organelles. They are little more than sacks of hemoglobin.
Erythrocytes also carry proteins called antigens that determine blood type. Blood type is a genetic characteristic. The best known human blood type systems are the ABO and Rhesus systems.
- In the ABO system, there are two common antigens, called antigen A and antigen B. There are four ABO blood types, A (only A antigen), B (only B antigen), AB (both A and B antigens), and O (neither A nor B antigen). The ABO antigens are illustrated in Figure 14.5.4.
- In the Rhesus system, there is just one common antigen. A person may either have the antigen (Rh+) or lack the antigen (Rh-).
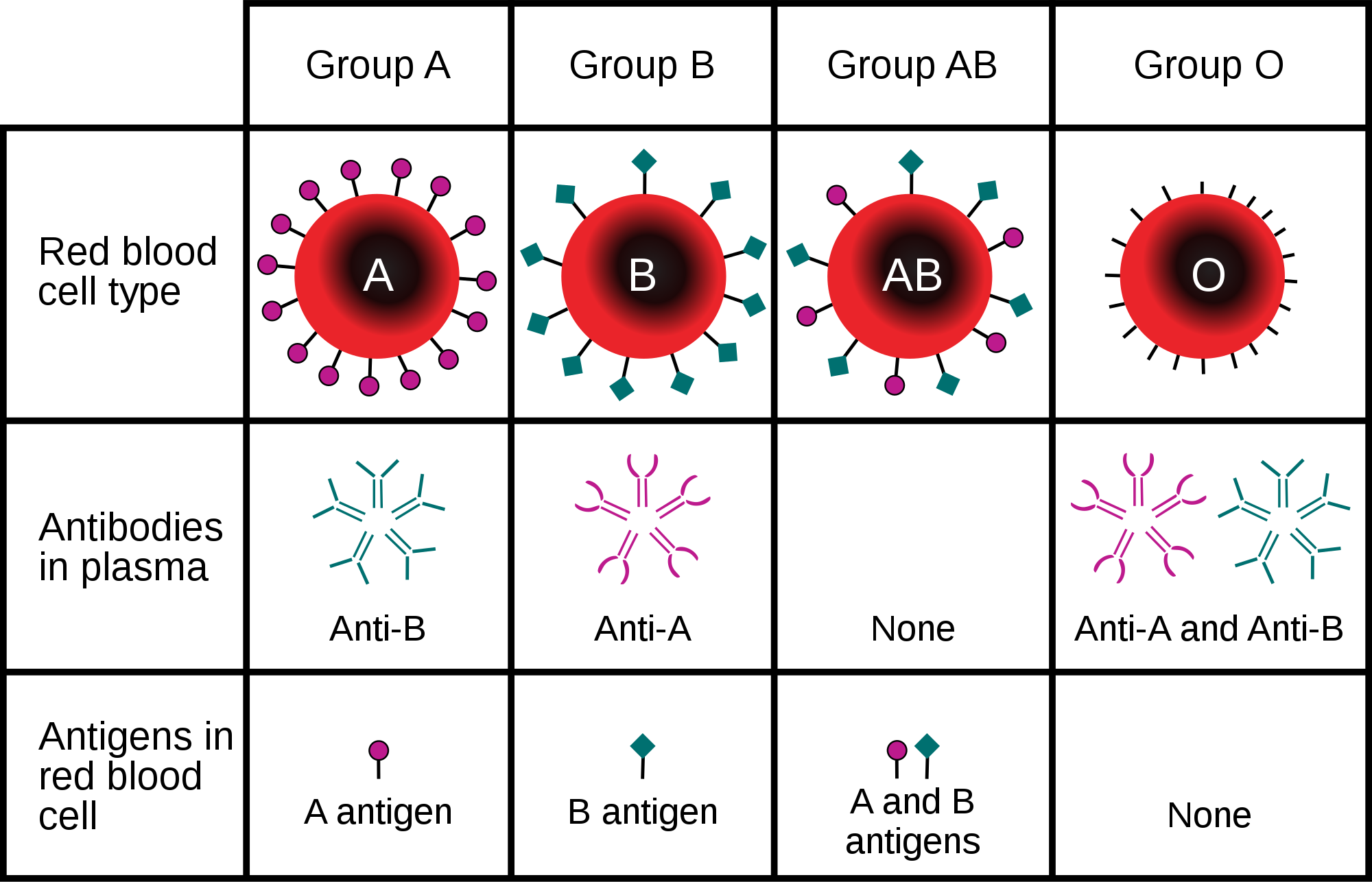
Blood type is important for medical reasons. A person who needs a blood transfusion must receive blood of a compatible type. Blood that is compatible lacks antigens that the patient's own blood also lacks. For example, for a person with type A blood (no B antigen), compatible types include any type of blood that lacks the B antigen. This would include type A blood or type O blood, but not type AB or type B blood. If incompatible blood is transfused, it may cause a potentially life-threatening reaction in the patient’s blood.
Leukocytes
Leukocytes (also called white blood cells) are cells in blood that defend the body against invading microorganisms and other threats. There are far fewer leukocytes than red blood cells in blood. There are normally only about 1,000 to 11,000 white blood cells per microlitre of blood. Unlike erythrocytes, leukocytes have a nucleus. White blood cells are part of the body’s immune system. They destroy and remove old or abnormal cells and cellular debris, as well as attack pathogens and foreign substances. There are five main types of white blood cells, which are described in Table 14.5.1: neutrophils, eosinophils, basophils, lymphocytes, and monocytes. The five types differ in their specific immune functions.
| Type of Leukocyte | Per cent of All Leukocytes | Main Function(s) |
|---|---|---|
| Neutrophil | 62% | Phagocytize (engulf and destroy) bacteria and fungi in blood. |
| Eosinophil | 2% | Attack and kill large parasites; carry out allergic responses. |
| Basophil | less than 1% | Release histamines in inflammatory responses. |
| Lymphocyte | 30% | Attack and destroy virus-infected and tumor cells; create lasting immunity to specific pathogens. |
| Monocyte | 5% | Phagocytize pathogens and debris in tissues. |
Thrombocytes
Thrombocytes, also called platelets, are actually cell fragments. Like erythrocytes, they lack a nucleus and are more numerous than white blood cells. There are about 150 thousand to 400 thousand thrombocytes per microlitre of blood.
The main function of thrombocytes is blood clotting, or coagulation. This is the process by which blood changes from a liquid to a gel, forming a plug in a damaged blood vessel. If blood clotting is successful, it results in hemostasis, which is the cessation of blood loss from the damaged vessel. A blood clot consists of both platelets and proteins, especially the protein fibrin. You can see a scanning electron microscope photomicrograph of a blood clot in Figure 14.5.5.
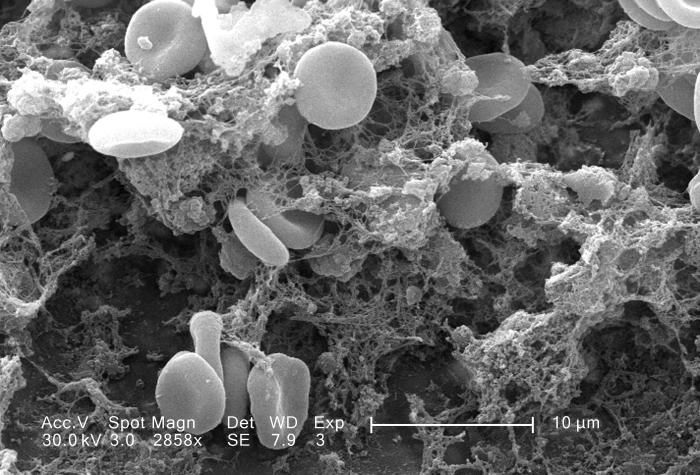
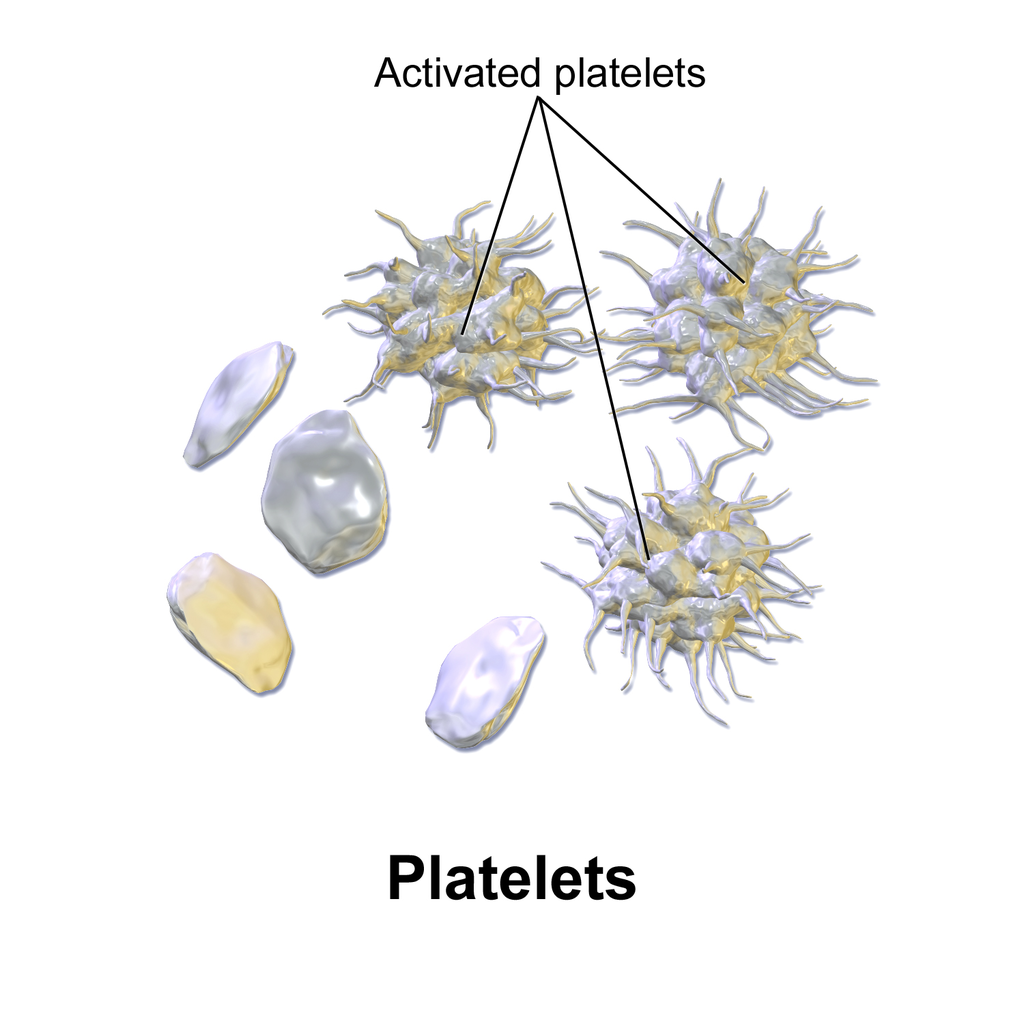
Coagulation begins almost instantly after an injury occurs to the endothelium of a blood vessel. Thrombocytes become activated and change their shape from spherical to star-shaped, as shown in Figure 14.5.6. This helps them aggregate with one another (stick together) at the site of injury to start forming a plug in the vessel wall. Activated thrombocytes also release substances into the blood that activate additional thrombocytes and start a sequence of reactions leading to fibrin formation. Strands of fibrin crisscross the platelet plug and strengthen it, much as rebar strengthens concrete.
Formation and Degradation of Blood Cells
Blood is considered a connective tissue, because blood cells form inside bones. All three types of blood cells are made in red marrow within the medullary cavity of bones in a process called hematopoiesis. Formation of blood cells occurs by the proliferation of stem cells in the marrow. These stem cells are self-renewing — when they divide, some of the daughter cells remain stem cells, so the pool of stem cells is not used up. Other daughter cells follow various pathways to differentiate into the variety of blood cell types. Once the cells have differentiated, they cannot divide to form copies of themselves.
Eventually, blood cells die and must be replaced through the formation of new blood cells from proliferating stem cells. After blood cells die, the dead cells are phagocytized (engulfed and destroyed) by white blood cells, and removed from the circulation. This process most often takes place in the spleen and liver.
Blood Disorders
Many human disorders primarily affect the blood. They include cancers, genetic disorders, poisoning by toxins, infections, and nutritional deficiencies.
- Leukemia is a group of cancers of the blood-forming tissues in the bone marrow. It is the most common type of cancer in children, although most cases occur in adults. Leukemia is generally characterized by large numbers of abnormal leukocytes. Symptoms may include excessive bleeding and bruising, fatigue, fever, and an increased risk of infections. Leukemia is thought to be caused by a combination of genetic and environmental factors.
- Hemophilia refers to any of several genetic disorders that cause dysfunction in the blood clotting process. People with hemophilia are prone to potentially uncontrollable bleeding, even with otherwise inconsequential injuries. They also commonly suffer bleeding into the spaces between joints, which can cause crippling.
- Carbon monoxide poisoning occurs when inhaled carbon monoxide (in fumes from a faulty home furnace or car exhaust, for example) binds irreversibly to the hemoglobin in erythrocytes. As a result, oxygen cannot bind to the red blood cells for transport throughout the body, and this can quickly lead to suffocation. Carbon monoxide is extremely dangerous, because it is colourless and odorless, so it cannot be detected in the air by human senses.
- HIV is a virus that infects certain types of leukocytes and interferes with the body’s ability to defend itself from pathogens and other causes of illness. HIV infection may eventually lead to AIDS (acquired immunodeficiency syndrome). AIDS is characterized by rare infections and cancers that people with a healthy immune system almost never acquire.
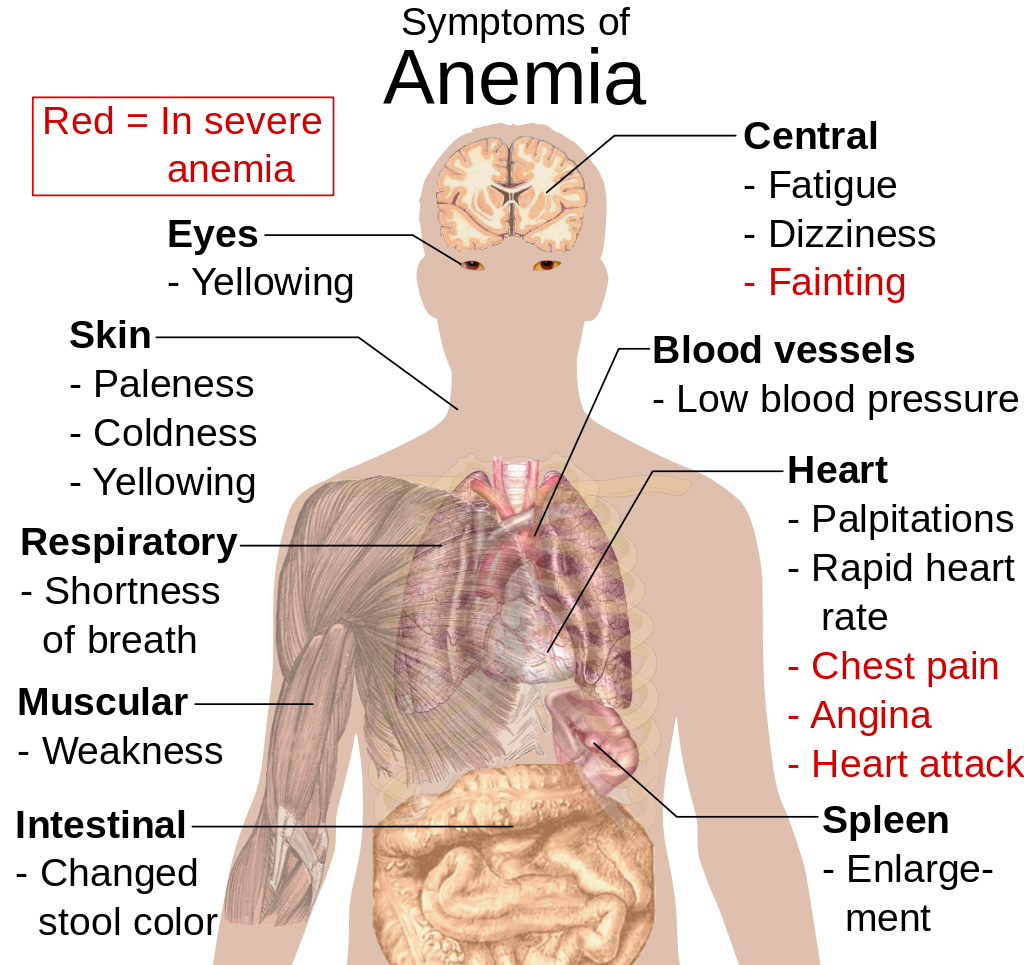
- Anemia is a disorder in which the blood has an inadequate volume of erythrocytes, reducing the amount of oxygen that the blood can carry, and potentially causing weakness and fatigue. These and other signs and symptoms of anemia are shown in Figure 14.5.8. Anemia has many possible causes, including excessive bleeding, inherited disorders (such as sickle cell hemoglobin), or nutritional deficiencies (iron, folate, or B12). Severe anemia may require transfusions of donated blood.
Feature: Myth vs. Reality
Donating blood saves lives. In fact, with each blood donation, as many as three lives may be saved. According to Government Canada, up to 52% of Canadians have reported that they or a family member have needed blood or blood products at some point in their lifetime. Many donors agree that the feeling that comes from knowing you have saved lives is well worth the short amount of time it takes to make a blood donation. Nonetheless, only a minority of potential donors actually donate blood. There are many myths about blood donation that may help explain the small percentage of donors. Knowing the facts may reaffirm your decision to donate if you are already a donor — and if you aren’t a donor already, getting the facts may help you decide to become one.
| Myth | Reality |
|---|---|
| "Your blood might become contaminated with an infection during the donation." | There is no risk of contamination because only single-use, disposable catheters, tubing, and other equipment are used to collect blood for a donation. |
| "You are too old (or too young) to donate blood." | There is no upper age limit on donating blood, as long as you are healthy. The minimum age is 16 years. |
| "You can’t donate blood if you have high blood pressure." | As long as your blood pressure is below 180/100 at the time of donation, you can give blood. Even if you take blood pressure medication to keep your blood pressure below this level, you can donate. |
| "You can’t give blood if you have high cholesterol." | Having high cholesterol does not affect your ability to donate blood. Taking cholesterol-lowering medication also does not disqualify you. |
| "You can’t donate blood if you have had a flu shot." | Having a flu shot has no effect on your ability to donate blood. You can even donate on the same day that you receive a flu shot. |
| "You can’t donate blood if you take medication." | As long as you are healthy, in most cases, taking medication does not preclude you from donating blood. |
| "Your blood isn’t needed if it’s a common blood type." | All types of blood are in constant demand. |
14.5 Summary
- Blood is a fluid connective tissue that circulates throughout the body in the cardiovascular system. Blood supplies tissues with oxygen and nutrients and removes their metabolic wastes. Blood helps defend the body from pathogens and other threats, transports hormones and other substances, and helps keep the body’s pH and temperature in homeostasis.
- Plasma is the liquid component of blood, and it makes up more than half of blood by volume. It consists of water and many dissolved substances. It also contains blood cells, including erythrocytes, leukocytes and thrombocytes.
- Erythrocytes, (also known as red blood cells) are the most numerous cells in blood. They consist mostly of hemoglobin, which carries oxygen. Erythrocytes also carry antigens that determine blood type.
- Leukocytes (also referred to as white blood cells) are less numerous than erythrocytes and are part of the body’s immune system. There are several different types of leukocytes that differ in their specific immune functions. They protect the body from abnormal cells, microorganisms, and other harmful substances.
- Thrombocytes (also called platelets) are cell fragments that play important roles in blood clotting, or coagulation. They stick together at breaks in blood vessels to form a clot and stimulate the production of fibrin, which strengthens the clot.
- All blood cells form by proliferation of stem cells in red bone marrow in a process called hematopoiesis. When blood cells die, they are phagocytized by leukocytes and removed from the circulation.
- Disorders of the blood include leukemia, which is cancer of the bone-forming cells; hemophilia, which is any of several genetic blood-clotting disorders; carbon monoxide poisoning, which prevents erythrocytes from binding with oxygen and causes suffocation; HIV infection, which destroys certain types of leukocytes and can cause AIDS; and anemia, in which there are not enough erythrocytes to carry adequate oxygen to body tissues.
14.5 Review Questions
- What is blood? Why is blood considered a connective tissue?
- Identify four physiological roles of blood in the body.
- Describe plasma and its components.
-
14.5 Explore More
https://youtu.be/e-5wqwp64MM
Joe Landolina: This gel can make you stop bleeding instantly, TED, 2014.
https://youtu.be/hgp8LtwFSBA
Can Synthetic Blood Help The World's Blood Shortage? Science Plus, 2016.
https://youtu.be/1Qfmkd6C8u8
How bones make blood - Melody Smith, TED-Ed, 2020.
Attributions
Figure 14.5.1
vampire_PNG32 from pngimg.com is used under a CC BY-NC 4.0 (https://creativecommons.org/licenses/by-nc/4.0/) license.
Figure 14.5.2
Blood-centrifugation-scheme by KnuteKnudsen at English Wikipedia on Wikimedia Commons is used under a CC BY 3.0 (https://creativecommons.org/licenses/by/3.0) license.
Figure 14.5.3
SEM_blood_cells by Bruce Wetzel and Harry Schaefer (Photographers)/ NCI AV-8202-3656 on Wikimedia Commons is in the public domain (https://en.wikipedia.org/wiki/en:Public_domain).
Figure 14.5.4
ABO_blood_type.svg by InvictaHOG on Wikimedia Commons is in the public domain (https://en.wikipedia.org/wiki/en:Public_domain).
Figure 14.5.5
Blood_clot_in_scanning_electron_microscopy by Janice Carr from CDC/ Public Health Image LIbrary (PHIL) ID #7308 on Wikimedia Commons is in the public domain (https://en.wikipedia.org/wiki/en:Public_domain).
Figure 14.5.6
Blausen_0740_Platelets by BruceBlaus on Wikimedia Commons is used under a CC BY 3.0 (https://creativecommons.org/licenses/by/3.0) license.
Figure 14.5.7
Platelet_Party_900x by Awkward Yeti (used with permission of the author) © All Rights Reserved
Figure 14.5.8
Symptoms_of_anemia.svg by Mikael Häggström on Wikimedia Commons is in the public domain (https://en.wikipedia.org/wiki/en:public_domain).
References
Blausen.com Staff. (2014). Medical gallery of Blausen Medical 2014. WikiJournal of Medicine 1 (2). DOI:10.15347/wjm/2014.010. ISSN 2002-4436.
Blood, organ and tissue donation. (2020, April 28). Government of Canada. https://www.canada.ca/en/public-health/services/healthy-living/blood-organ-tissue-donation.html#a3
Canadian Blood Services. (n.d.). There is an immediate need for blood as demand is rising. https://www.blood.ca
Science Plus. (2016, March 2). Can synthetic blood help the world's blood shortage? https://www.youtube.com/watch?v=hgp8LtwFSBA&feature=youtu.be
TED. (2014, November 20). Joe Landolina: This gel can make you stop bleeding instantly. YouTube. https://www.youtube.com/watch?v=e-5wqwp64MM&feature=youtu.be
TED-Ed. (2020, January 27). How bones make blood - Melody Smith. YouTube. https://www.youtube.com/watch?v=1Qfmkd6C8u8&feature=youtu.be
As per caption
Image shows a diagram of the bladder. There is smooth muscle in the bladder walls which are under involuntary control. There is a sphincter between the bladder and the urethra which can inhibit urination.
Created by CK-12 Foundation/Adapted by Christine Miller
Figure 16.3.1 The surprising uses of pee.
Surprising Uses
What do gun powder, leather, fabric dyes and laundry service have in common? This may be surprising, but they all historically involved urine. One of the main components in gun powder, potassium nitrate, was difficult to come by pre-1900s, so ingenious gun-owners would evaporate urine to concentrate the nitrates it contains. The ammonium in urine was excellent in breaking down tissues, making it a prime candidate for softening leathers and removing stains in laundry. Ammonia in urine also helps dyes penetrate fabrics, so it was used to make colours stay brighter for longer.
What is the Urinary System?
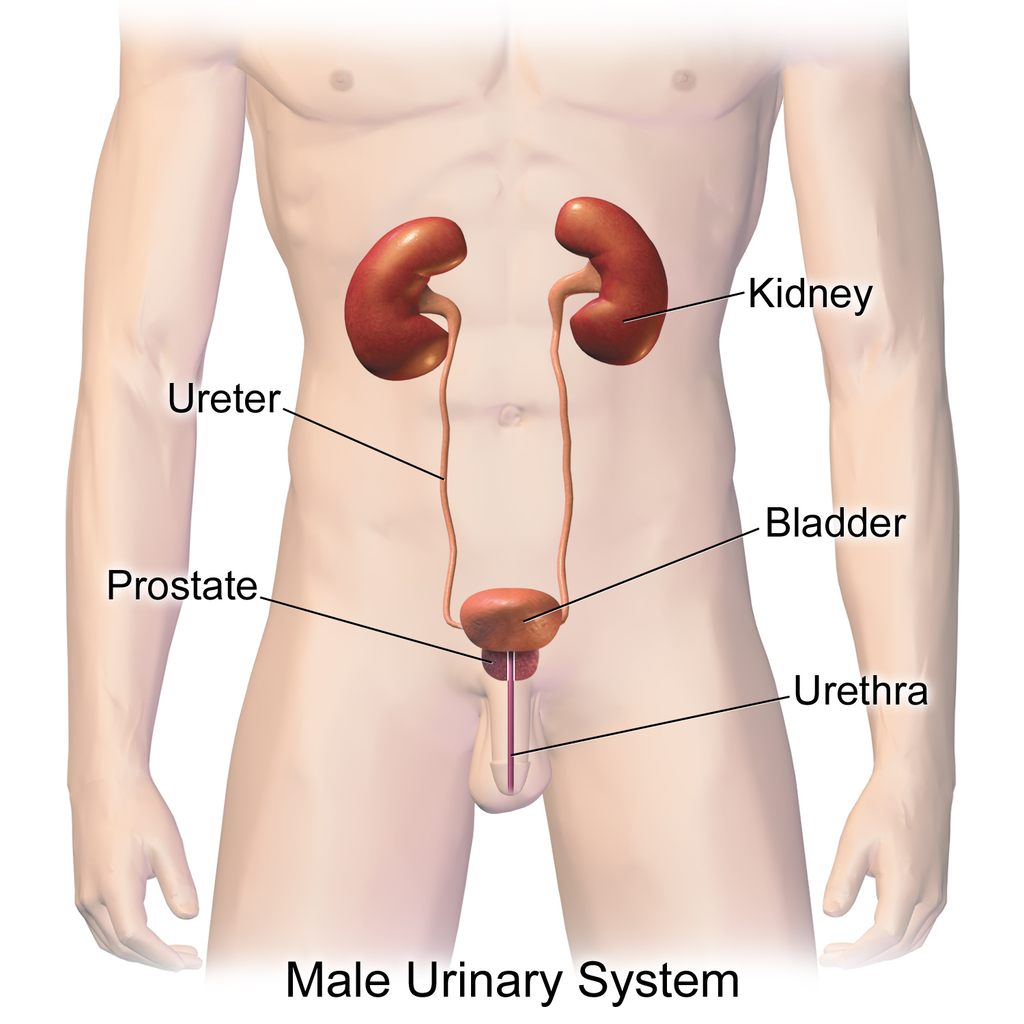
The actual human urinary system, also known as the renal system, is shown in Figure 16.3.2. The system consists of the kidneys, ureters, bladder, and urethra. The main function of the urinary system is to eliminate the waste products of metabolism from the body by forming and excreting urine. Typically, between one and two litres of urine are produced every day in a healthy individual.
Organs of the Urinary System
The urinary system is all about urine. It includes organs that form urine, and also those that transport, store, or excrete urine.
Kidneys
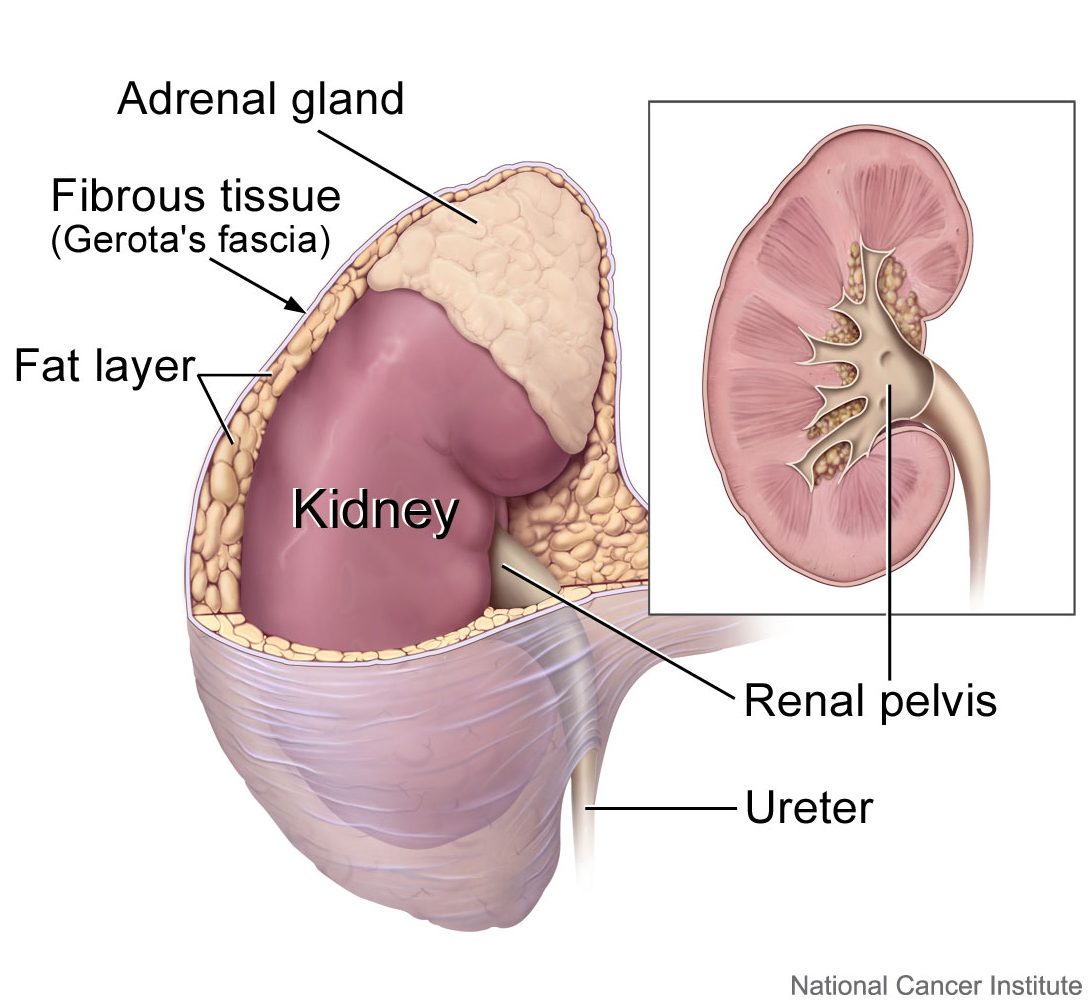
Urine is formed by the kidneys, which filter many substances out of the blood, allow the blood to reabsorb needed materials, and use the remaining materials to form urine. The human body normally has two paired kidneys, although it is possible to get by quite well with just one. As you can see in Figure 16.3.3, each kidney is well supplied with blood vessels by a major artery and vein. Blood to be filtered enters the kidney through the renal artery, and the filtered blood leaves the kidney through the renal vein. The kidney itself is wrapped in a fibrous capsule, and consists of a thin outer layer called the cortex, and a thicker inner layer called the medulla.
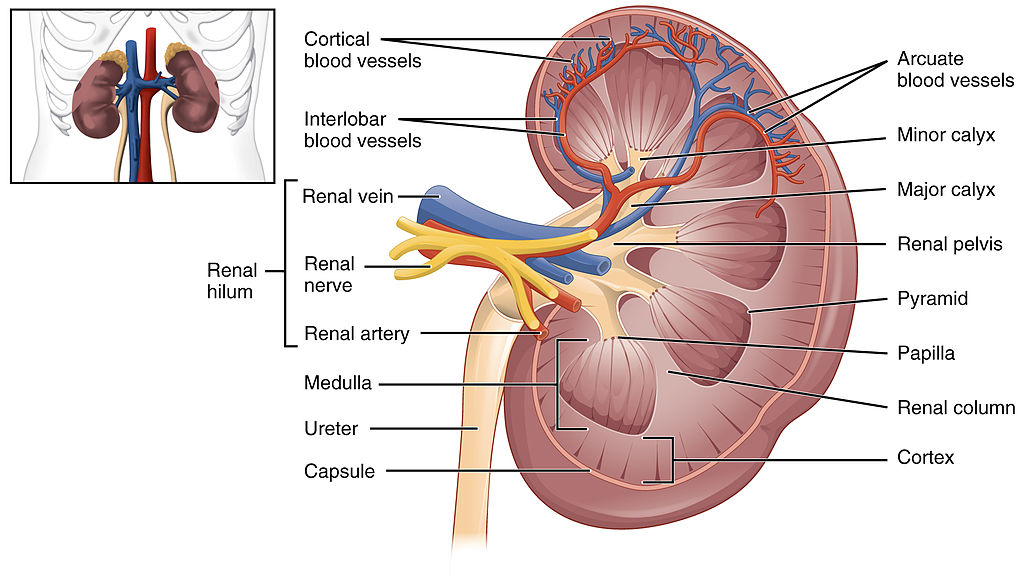
Blood is filtered and urine is formed by tiny filtering units called nephrons. Each kidney contains at least a million nephrons, and each nephron spans the cortex and medulla layers of the kidney. After urine forms in the nephrons, it flows through a system of converging collecting ducts. The collecting ducts join together to form minor calyces (or chambers) that join together to form major calyces (see Figure 16.3.3 above). Ultimately, the major calyces join the renal pelvis, which is the funnel-like end of the ureter where it enters the kidney.
Ureters, Bladder, Urethra
After urine forms in the kidneys, it is transported through the ureters (one per kidney) via peristalsis to the sac-like urinary bladder, which stores the urine until urination. During urination, the urine is released from the bladder and transported by the urethra to be excreted outside the body through the external urethral opening.
Functions of the Urinary System
Waste products removed from the body with the formation and elimination of urine include many water-soluble metabolic products. The main waste products are urea — a by-product of protein catabolism — and uric acid, a by-product of nucleic acid catabolism. Excess water and mineral ions are also eliminated in urine.
Besides the elimination of waste products such as these, the urinary system has several other vital functions. These include:
- Maintaining homeostasis of mineral ions in extracellular fluid: These ions are either excreted in urine or returned to the blood as needed to maintain the proper balance.
- Maintaining homeostasis of blood pH: When pH is too low (blood is too acidic), for example, the kidneys excrete less bicarbonate (which is basic) in urine. When pH is too high (blood is too basic), the opposite occurs, and more bicarbonate is excreted in urine.
- Maintaining homeostasis of extracellular fluids, including the blood volume, which helps maintain blood pressure: The kidneys control fluid volume and blood pressure by excreting more or less salt and water in urine.
Control of the Urinary System
The formation of urine must be closely regulated to maintain body-wide homeostasis. Several endocrine hormones help control this function of the urinary system, including antidiuretic hormone, parathyroid hormone, and aldosterone.
- Antidiuretic hormone (ADH), also called vasopressin, is secreted by the posterior pituitary gland. One of its main roles is conserving body water. It is released when the body is dehydrated, and it causes the kidneys to excrete less water in urine.
- Parathyroid hormone is secreted by the parathyroid glands. It works to regulate the balance of mineral ions in the body via its effects on several organs, including the kidneys. Parathyroid hormone stimulates the kidneys to excrete less calcium and more phosphorus in urine.
- Aldosterone is secreted by the cortex of the adrenal glands, which rest atop the kidneys, as shown in Figure 16.3.4. Through its effect on the kidneys, it plays a central role in regulating blood pressure. It causes the kidneys to excrete less sodium and water in urine.
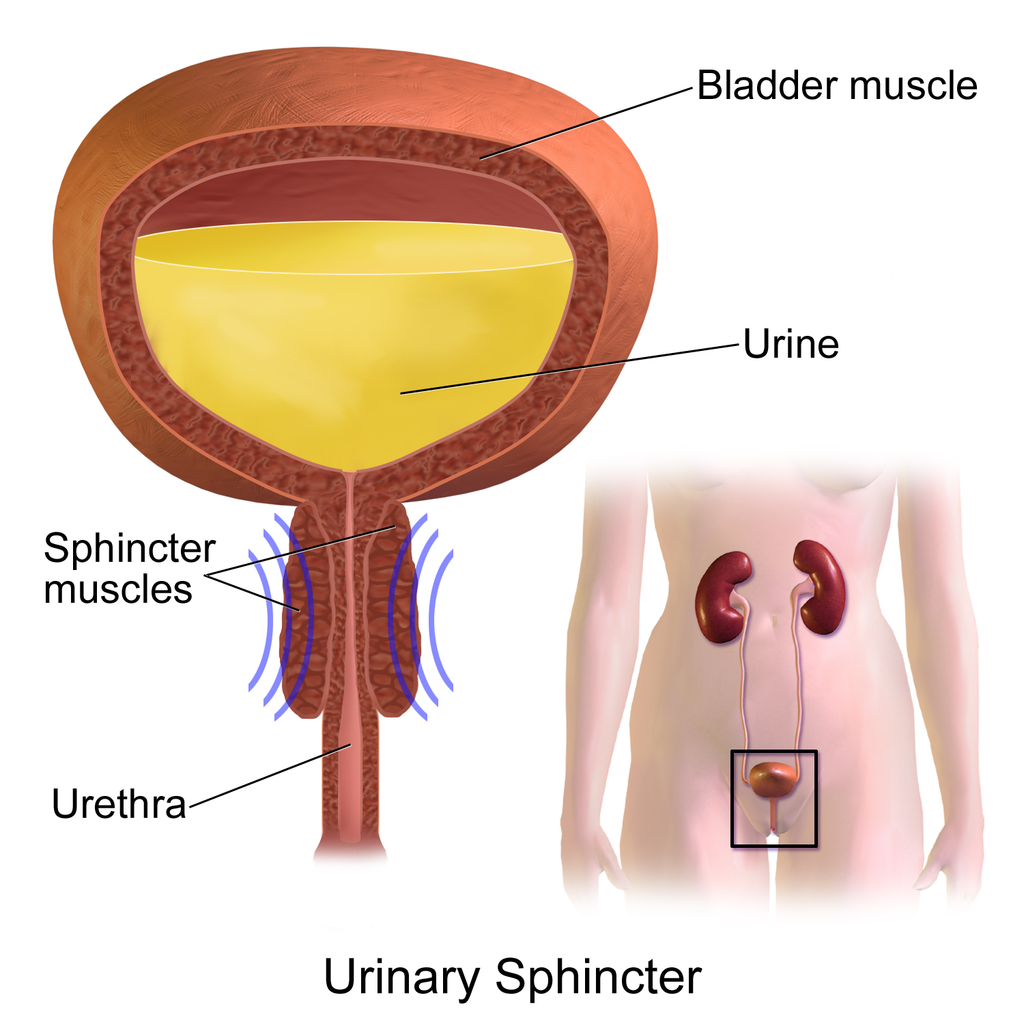
Once urine forms, it is excreted from the body in the process of urination, also sometimes referred to as micturition. This process is controlled by both the autonomic and the somatic nervous systems. As the bladder fills with urine, it causes the autonomic nervous system to signal smooth muscle in the bladder wall to contract (as shown in Figure 16.3.5), and the sphincter between the bladder and urethra to relax and open. This forces urine out of the bladder and through the urethra. Another sphincter at the distal end of the urethra is under voluntary control. When it relaxes under the influence of the somatic nervous system, it allows urine to leave the body through the external urethral opening.
16.3 Summary
- The urinary system consists of the kidneys, ureters, bladder, and urethra. The main function of the urinary system is to eliminate the waste products of metabolism from the body by forming and excreting urine.
- Urine is formed by the kidneys, which filter many substances out of blood, allow the blood to reabsorb needed materials, and use the remaining materials to form urine. Blood to be filtered enters the kidney through the renal artery, and filtered blood leaves the kidney through the renal vein.
- Within each kidney, blood is filtered and urine is formed by tiny filtering units called nephrons, of which there are at least a million in each kidney.
- After urine forms in the kidneys, it is transported through the ureters via peristalsis to the urinary bladder. The bladder stores the urine until urination, when urine is transported by the urethra to be excreted outside the body.
- Besides the elimination of waste products (such as urea, uric acid, excess water, and mineral ions), the urinary system has other vital functions. These include maintaining homeostasis of mineral ions in extracellular fluid, regulating acid-base balance in the blood, regulating the volume of extracellular fluids, and controlling blood pressure.
- The formation of urine must be closely regulated to maintain body-wide homeostasis. Several endocrine hormones help control this function of the urinary system, including antidiuretic hormone from the posterior pituitary gland, parathyroid hormone from the parathyroid glands, and aldosterone from the adrenal glands.
- The process of urination is controlled by both the autonomic and the somatic nervous systems. The autonomic system causes the bladder to empty, but conscious relaxation of the sphincter at the distal end of the urethra allows urine to leave the body.
16.3 Review Questions
-
- State the main function of the urinary system.
- What are nephrons?
- Other than the elimination of waste products, identify functions of the urinary system.
- How is the formation of urine regulated?
- Explain why it is important to have voluntary control over the sphincter at the end of the urethra.
- In terms of how they affect the kidneys, compare aldosterone to antidiuretic hormone.
- If your body needed to retain more calcium, which of the hormones described in this concept is most likely to increase? Explain your reasoning.
16.3 Explore More
https://youtu.be/dxecGD0m0Xc
The Urinary System - An Introduction | Physiology | Biology | FuseSchool, 2017.
https://youtu.be/pyMcTUQYMQw
Maple Syrup Urine Disease, Alexandria Doody, 2016.
https://youtu.be/3z-xjfdJWAI
How Accurate Are Drug Tests? Seeker, 2016.
https://youtu.be/xt1Tj5eeS0k
Three Ways Pee Could Change the World, Gross Science, 2015.
Attributions
Figure 16.3.1
- File:Pyrodex powder ffg.jpg by Hustvedt on Wikimedia Commons is used under a CC BY SA 3.0 (https://creativecommons.org/licenses/by-sa/3.0/deed.en).
- Brown leather satchel bag by Álvaro Serrano on Unsplash is used under the Unsplash Licence (https://unsplash.com/license).
- Laundry basket by Andy Fitzsimon on Unsplash is used under the Unsplash Licence (https://unsplash.com/license).
- Tags: Wool Skeins Natural Dyed Colorful Himalayan Weavers by on Pixabay is used under the Pixabay License (https://pixabay.com/service/license/).
Figure 16.3.2
Urinary_System_(Male) by BruceBlaus on Wikimedia Commons is used under a CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0) license.
Figure 16.3.3
2610_The_Kidney by OpenStax College on Wikimedia Commons is used under a CC BY 3.0 (https://creativecommons.org/licenses/by/3.0) license.
Figure 16.3.4
Adrenal glands on Kidney by Alan Hoofring (Illustrator)/ NCI Visuals Online is in the public domain (https://en.wikipedia.org/wiki/Public_domain).
Figure 16.3.5
Urinary_Sphincter by BruceBlaus on Wikimedia Commons is used under a CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0) license.
References
Alexandria Doody. (2016, March 29). Maple syrup urine disease. YouTube. https://www.youtube.com/watch?v=pyMcTUQYMQw&feature=youtu.be
Betts, J. G., Young, K.A., Wise, J.A., Johnson, E., Poe, B., Kruse, D.H., Korol, O., Johnson, J.E., Womble, M., DeSaix, P. (2013, June 19). Figure 25.8 Left kidney [digital image]. In Anatomy and Physiology (Section 25.3). OpenStax. https://openstax.org/books/anatomy-and-physiology/pages/25-3-gross-anatomy-of-the-kidney
FuseSchool. (2017, June 19). The urinary system - An introduction | Physiology | Biology | FuseSchool. YouTube. https://www.youtube.com/watch?v=dxecGD0m0Xc&feature=youtu.be
Gross Science. (2015, September 15). Three ways pee could change the world. YouTube. https://www.youtube.com/watch?v=xt1Tj5eeS0k&feature=youtu.be
Seeker. (2016, January 16). How accurate are drug tests? YouTube. https://www.youtube.com/watch?v=3z-xjfdJWAI&feature=youtu.be
Created by CK-12 Foundation/Adapted by Christine Miller
Figure 16.3.1 The surprising uses of pee.
Surprising Uses
What do gun powder, leather, fabric dyes and laundry service have in common? This may be surprising, but they all historically involved urine. One of the main components in gun powder, potassium nitrate, was difficult to come by pre-1900s, so ingenious gun-owners would evaporate urine to concentrate the nitrates it contains. The ammonium in urine was excellent in breaking down tissues, making it a prime candidate for softening leathers and removing stains in laundry. Ammonia in urine also helps dyes penetrate fabrics, so it was used to make colours stay brighter for longer.
What is the Urinary System?
The actual human urinary system, also known as the renal system, is shown in Figure 16.3.2. The system consists of the kidneys, ureters, bladder, and urethra. The main function of the urinary system is to eliminate the waste products of metabolism from the body by forming and excreting urine. Typically, between one and two litres of urine are produced every day in a healthy individual.
Organs of the Urinary System
The urinary system is all about urine. It includes organs that form urine, and also those that transport, store, or excrete urine.
Kidneys
Urine is formed by the kidneys, which filter many substances out of the blood, allow the blood to reabsorb needed materials, and use the remaining materials to form urine. The human body normally has two paired kidneys, although it is possible to get by quite well with just one. As you can see in Figure 16.3.3, each kidney is well supplied with blood vessels by a major artery and vein. Blood to be filtered enters the kidney through the renal artery, and the filtered blood leaves the kidney through the renal vein. The kidney itself is wrapped in a fibrous capsule, and consists of a thin outer layer called the cortex, and a thicker inner layer called the medulla.
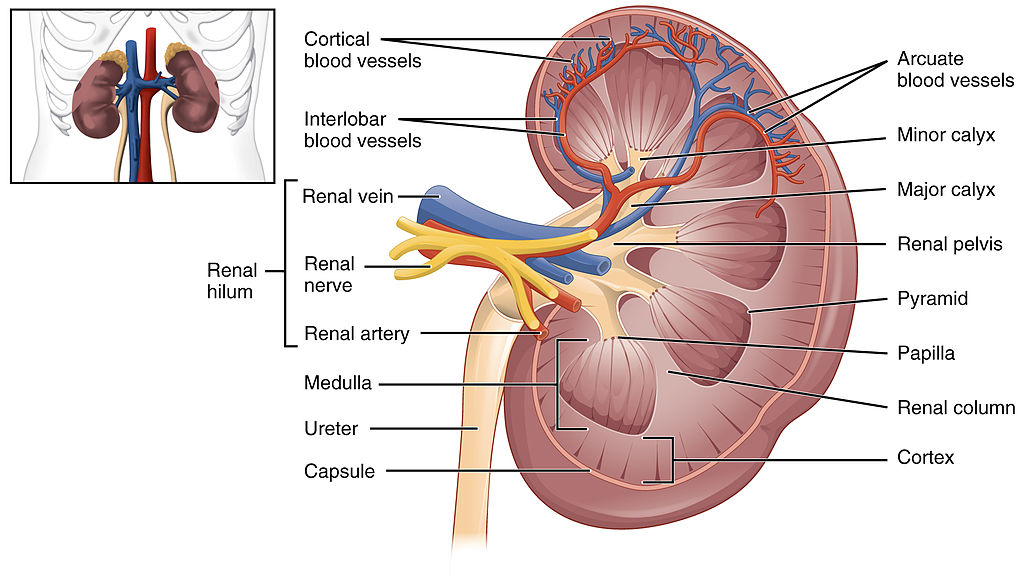
Blood is filtered and urine is formed by tiny filtering units called nephrons. Each kidney contains at least a million nephrons, and each nephron spans the cortex and medulla layers of the kidney. After urine forms in the nephrons, it flows through a system of converging collecting ducts. The collecting ducts join together to form minor calyces (or chambers) that join together to form major calyces (see Figure 16.3.3 above). Ultimately, the major calyces join the renal pelvis, which is the funnel-like end of the ureter where it enters the kidney.
Ureters, Bladder, Urethra
After urine forms in the kidneys, it is transported through the ureters (one per kidney) via peristalsis to the sac-like urinary bladder, which stores the urine until urination. During urination, the urine is released from the bladder and transported by the urethra to be excreted outside the body through the external urethral opening.
Functions of the Urinary System
Waste products removed from the body with the formation and elimination of urine include many water-soluble metabolic products. The main waste products are urea — a by-product of protein catabolism — and uric acid, a by-product of nucleic acid catabolism. Excess water and mineral ions are also eliminated in urine.
Besides the elimination of waste products such as these, the urinary system has several other vital functions. These include:
- Maintaining homeostasis of mineral ions in extracellular fluid: These ions are either excreted in urine or returned to the blood as needed to maintain the proper balance.
- Maintaining homeostasis of blood pH: When pH is too low (blood is too acidic), for example, the kidneys excrete less bicarbonate (which is basic) in urine. When pH is too high (blood is too basic), the opposite occurs, and more bicarbonate is excreted in urine.
- Maintaining homeostasis of extracellular fluids, including the blood volume, which helps maintain blood pressure: The kidneys control fluid volume and blood pressure by excreting more or less salt and water in urine.
Control of the Urinary System
The formation of urine must be closely regulated to maintain body-wide homeostasis. Several endocrine hormones help control this function of the urinary system, including antidiuretic hormone, parathyroid hormone, and aldosterone.
- Antidiuretic hormone (ADH), also called vasopressin, is secreted by the posterior pituitary gland. One of its main roles is conserving body water. It is released when the body is dehydrated, and it causes the kidneys to excrete less water in urine.
- Parathyroid hormone is secreted by the parathyroid glands. It works to regulate the balance of mineral ions in the body via its effects on several organs, including the kidneys. Parathyroid hormone stimulates the kidneys to excrete less calcium and more phosphorus in urine.
- Aldosterone is secreted by the cortex of the adrenal glands, which rest atop the kidneys, as shown in Figure 16.3.4. Through its effect on the kidneys, it plays a central role in regulating blood pressure. It causes the kidneys to excrete less sodium and water in urine.
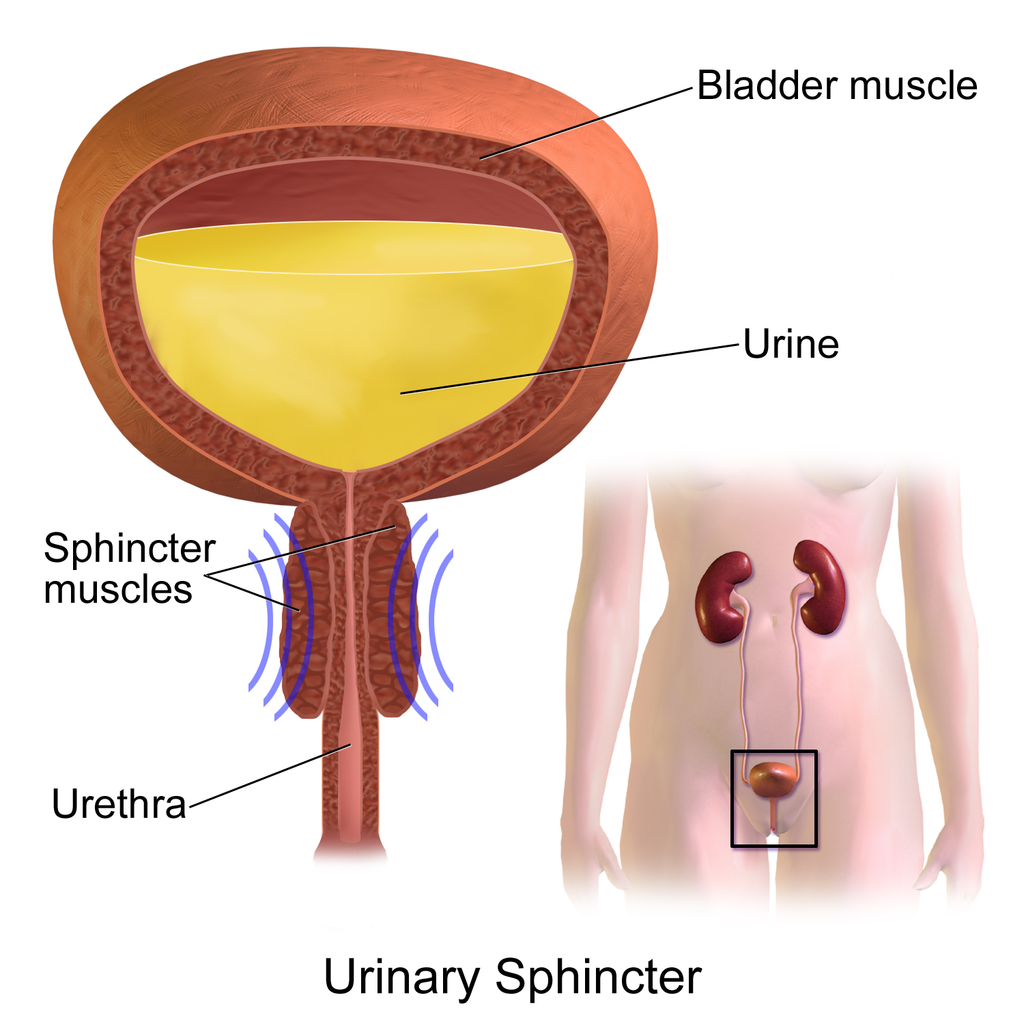
Once urine forms, it is excreted from the body in the process of urination, also sometimes referred to as micturition. This process is controlled by both the autonomic and the somatic nervous systems. As the bladder fills with urine, it causes the autonomic nervous system to signal smooth muscle in the bladder wall to contract (as shown in Figure 16.3.5), and the sphincter between the bladder and urethra to relax and open. This forces urine out of the bladder and through the urethra. Another sphincter at the distal end of the urethra is under voluntary control. When it relaxes under the influence of the somatic nervous system, it allows urine to leave the body through the external urethral opening.
16.3 Summary
- The urinary system consists of the kidneys, ureters, bladder, and urethra. The main function of the urinary system is to eliminate the waste products of metabolism from the body by forming and excreting urine.
- Urine is formed by the kidneys, which filter many substances out of blood, allow the blood to reabsorb needed materials, and use the remaining materials to form urine. Blood to be filtered enters the kidney through the renal artery, and filtered blood leaves the kidney through the renal vein.
- Within each kidney, blood is filtered and urine is formed by tiny filtering units called nephrons, of which there are at least a million in each kidney.
- After urine forms in the kidneys, it is transported through the ureters via peristalsis to the urinary bladder. The bladder stores the urine until urination, when urine is transported by the urethra to be excreted outside the body.
- Besides the elimination of waste products (such as urea, uric acid, excess water, and mineral ions), the urinary system has other vital functions. These include maintaining homeostasis of mineral ions in extracellular fluid, regulating acid-base balance in the blood, regulating the volume of extracellular fluids, and controlling blood pressure.
- The formation of urine must be closely regulated to maintain body-wide homeostasis. Several endocrine hormones help control this function of the urinary system, including antidiuretic hormone from the posterior pituitary gland, parathyroid hormone from the parathyroid glands, and aldosterone from the adrenal glands.
- The process of urination is controlled by both the autonomic and the somatic nervous systems. The autonomic system causes the bladder to empty, but conscious relaxation of the sphincter at the distal end of the urethra allows urine to leave the body.
16.3 Review Questions
-
- State the main function of the urinary system.
- What are nephrons?
- Other than the elimination of waste products, identify functions of the urinary system.
- How is the formation of urine regulated?
- Explain why it is important to have voluntary control over the sphincter at the end of the urethra.
- In terms of how they affect the kidneys, compare aldosterone to antidiuretic hormone.
- If your body needed to retain more calcium, which of the hormones described in this concept is most likely to increase? Explain your reasoning.
16.3 Explore More
https://youtu.be/dxecGD0m0Xc
The Urinary System - An Introduction | Physiology | Biology | FuseSchool, 2017.
https://youtu.be/pyMcTUQYMQw
Maple Syrup Urine Disease, Alexandria Doody, 2016.
https://youtu.be/3z-xjfdJWAI
How Accurate Are Drug Tests? Seeker, 2016.
https://youtu.be/xt1Tj5eeS0k
Three Ways Pee Could Change the World, Gross Science, 2015.
Attributions
Figure 16.3.1
- File:Pyrodex powder ffg.jpg by Hustvedt on Wikimedia Commons is used under a CC BY SA 3.0 (https://creativecommons.org/licenses/by-sa/3.0/deed.en).
- Brown leather satchel bag by Álvaro Serrano on Unsplash is used under the Unsplash Licence (https://unsplash.com/license).
- Laundry basket by Andy Fitzsimon on Unsplash is used under the Unsplash Licence (https://unsplash.com/license).
- Tags: Wool Skeins Natural Dyed Colorful Himalayan Weavers by on Pixabay is used under the Pixabay License (https://pixabay.com/service/license/).
Figure 16.3.2
Urinary_System_(Male) by BruceBlaus on Wikimedia Commons is used under a CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0) license.
Figure 16.3.3
2610_The_Kidney by OpenStax College on Wikimedia Commons is used under a CC BY 3.0 (https://creativecommons.org/licenses/by/3.0) license.
Figure 16.3.4
Adrenal glands on Kidney by Alan Hoofring (Illustrator)/ NCI Visuals Online is in the public domain (https://en.wikipedia.org/wiki/Public_domain).
Figure 16.3.5
Urinary_Sphincter by BruceBlaus on Wikimedia Commons is used under a CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0) license.
References
Alexandria Doody. (2016, March 29). Maple syrup urine disease. YouTube. https://www.youtube.com/watch?v=pyMcTUQYMQw&feature=youtu.be
Betts, J. G., Young, K.A., Wise, J.A., Johnson, E., Poe, B., Kruse, D.H., Korol, O., Johnson, J.E., Womble, M., DeSaix, P. (2013, June 19). Figure 25.8 Left kidney [digital image]. In Anatomy and Physiology (Section 25.3). OpenStax. https://openstax.org/books/anatomy-and-physiology/pages/25-3-gross-anatomy-of-the-kidney
FuseSchool. (2017, June 19). The urinary system - An introduction | Physiology | Biology | FuseSchool. YouTube. https://www.youtube.com/watch?v=dxecGD0m0Xc&feature=youtu.be
Gross Science. (2015, September 15). Three ways pee could change the world. YouTube. https://www.youtube.com/watch?v=xt1Tj5eeS0k&feature=youtu.be
Seeker. (2016, January 16). How accurate are drug tests? YouTube. https://www.youtube.com/watch?v=3z-xjfdJWAI&feature=youtu.be
Image shows a freshly baked Steak and Kidney Pie.
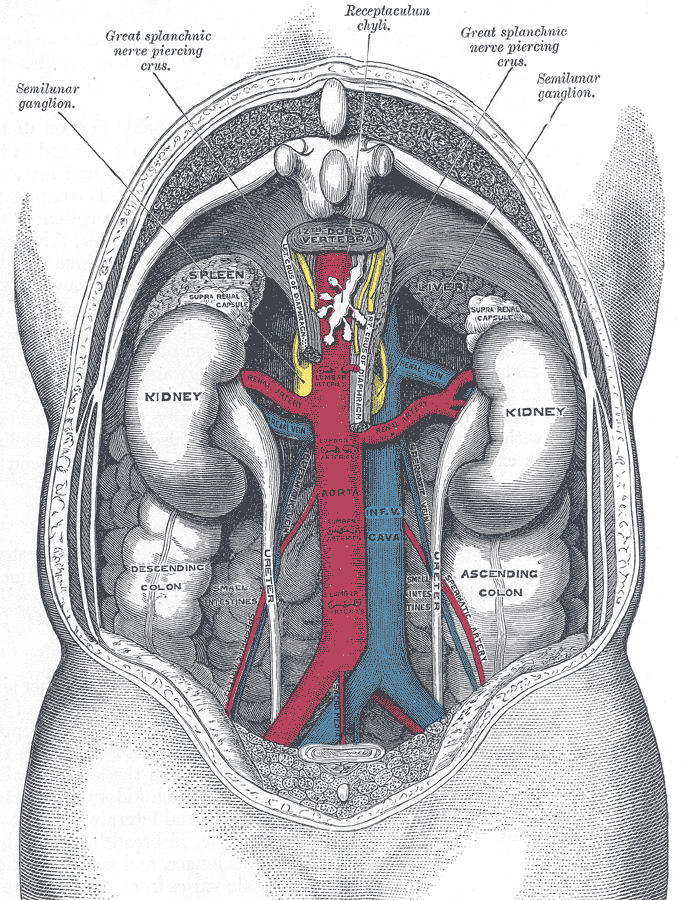
Image shows a labelled diagram of the posterior (from the back) view of the kidneys. The aorta and renal arteries are clearly visible bringing blood to each kidney. The left kidney sits a bit higher than the right kidney.
The transparent front part of the eye that covers the iris, pupil, and anterior chamber.
Image shows a diagram of a renal tubule and which substances are secreted or absorbed at each location along the tubule. Most secretion happens at the proximal convoluted tubule, although it does take place at all locations on the renal tubule. Reabsorption occurs mainly in the loop of Henle when balancing water and in the distal convoluted tubule when balancing pH.
As per caption
A transparent watery fluid similar to plasma, but containing low protein concentrations. It is secreted from the ciliary epithelium, a structure supporting the lens.
Created by CK-12 Foundation/Adapted by Christine Miller

Kidneys on the Menu
Pictured in Figure 16.4.1 is a steak and kidney pie; this savory dish is a British favorite. When kidneys are on a menu, they typically come from sheep, pigs, or cows. In these animals (as in the human animal), kidneys are the main organs of excretion.
Location of the Kidneys
The two bean-shaped kidneys are located high in the back of the abdominal cavity, one on each side of the spine. Both kidneys sit just below the diaphragm, the large breathing muscle that separates the abdominal and thoracic cavities. As you can see in the following figure, the right kidney is slightly smaller and lower than the left kidney. The right kidney is behind the liver, and the left kidney is behind the spleen. The location of the liver explains why the right kidney is smaller and lower than the left.
Kidney Anatomy
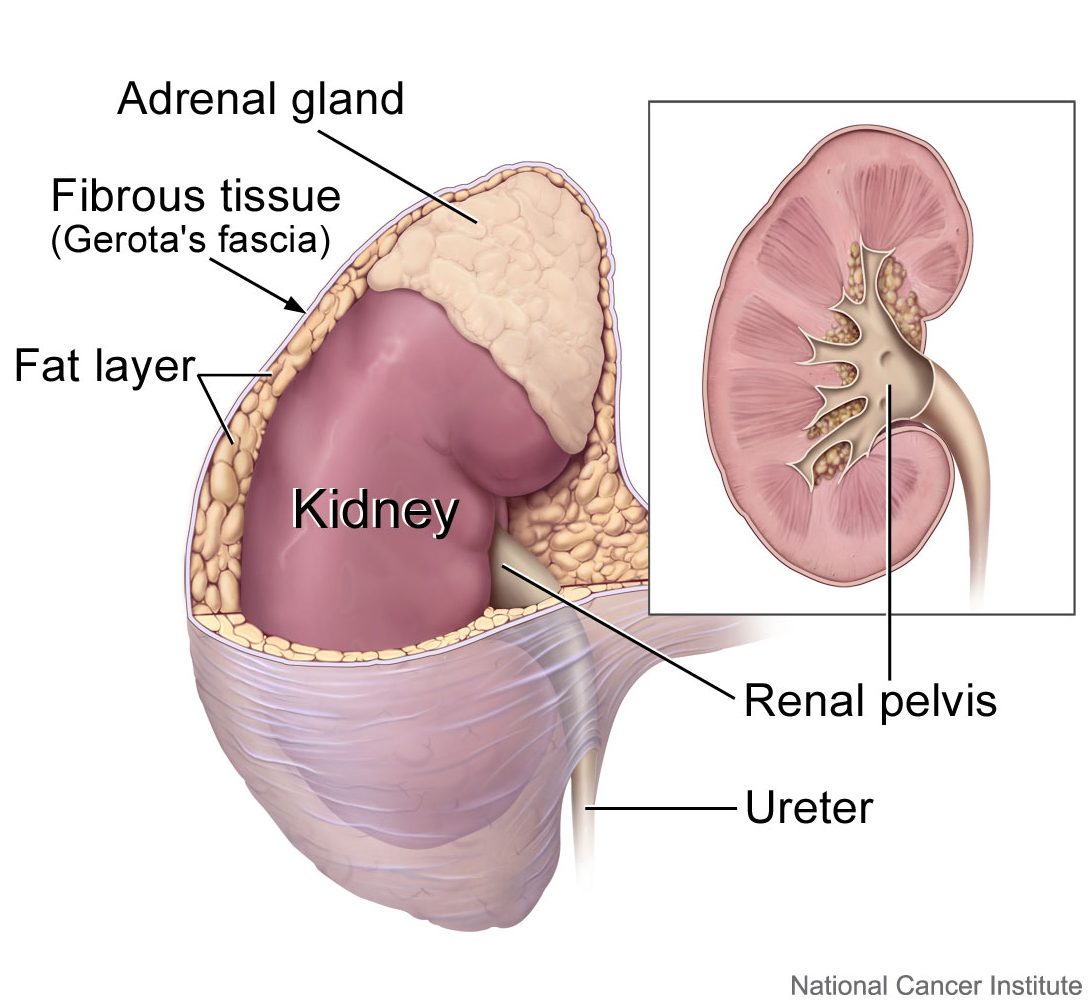
The shape of each kidney gives it a convex side (curving outward) and a concave side (curving inward). You can see this clearly in the detailed diagram of kidney anatomy shown in Figure 16.4.3. The concave side is where the renal artery enters the kidney, as well as where the renal vein and ureter leave the kidney. This area of the kidney is called the hilum. The entire kidney is surrounded by tough fibrous tissue — called the renal capsule — which, in turn, is surrounded by two layers of protective, cushioning fat.
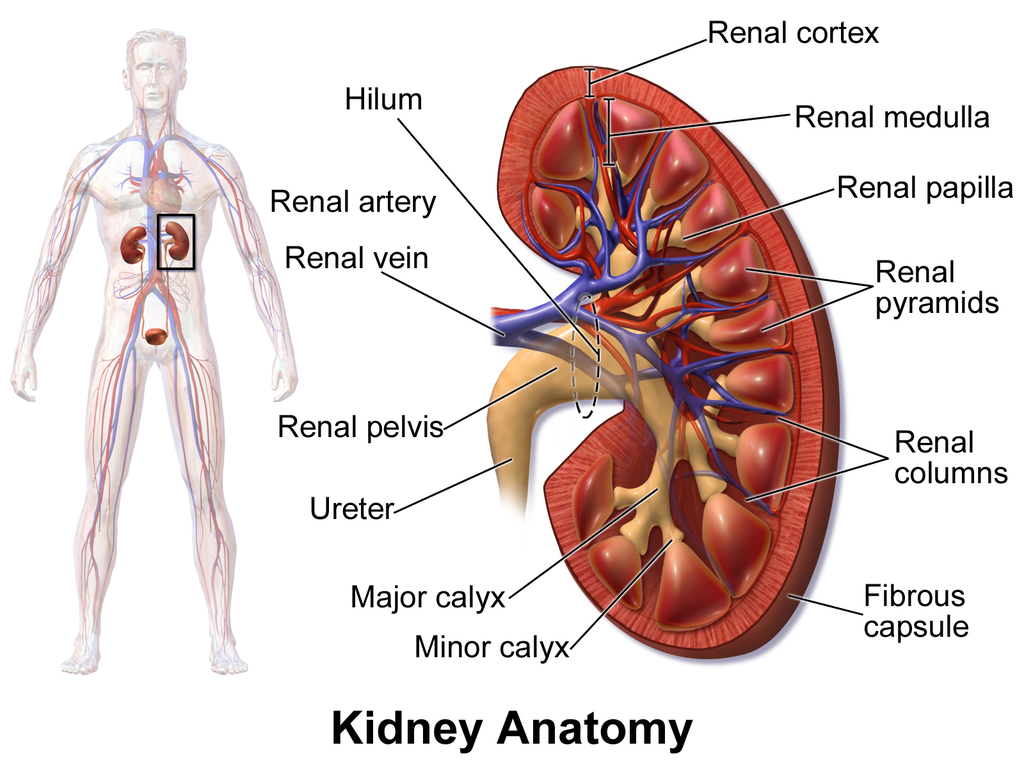
Internally, each kidney is divided into two major layers: the outer renal cortex and the inner renal medulla (see Figure 16.4.3 above). These layers take the shape of many cone-shaped renal lobules, each containing renal cortex surrounding a portion of medulla called a renal pyramid. Within the renal pyramids are the structural and functional units of the kidneys, the tiny nephrons. Between the renal pyramids are projections of cortex called renal columns. The tip, or papilla, of each pyramid empties urine into a minor calyx (chamber). Several minor calyces empty into a major calyx, and the latter empty into the funnel-shaped cavity called the renal pelvis, which becomes the ureter as it leaves the kidney.
Renal Circulation
The renal circulation is an important part of the kidney’s primary function of filtering waste products from the blood. Blood is supplied to the kidneys via the renal arteries. The right renal artery supplies the right kidney, and the left renal artery supplies the left kidney. These two arteries branch directly from the aorta, which is the largest artery in the body. Each kidney is only about 11 cm (4.4 in) long, and has a mass of just 150 grams (5.3 oz), yet it receives about ten per cent of the total output of blood from the heart. Blood is filtered through the kidneys every 3 minutes, 24 hours a day, every day of your life.
As indicated in Figure 16.4.4, each renal artery carries blood with waste products into the kidney. Within the kidney, the renal artery branches into increasingly smaller arteries that extend through the renal columns between the renal pyramids. These arteries, in turn, branch into arterioles that penetrate the renal pyramids. Blood in the arterioles passes through nephrons, the structures that actually filter the blood. After blood passes through the nephrons and is filtered, the clean blood moves through a network of venules that converge into small veins. Small veins merge into increasingly larger ones, and ultimately into the renal vein, which carries clean blood away from the kidney to the inferior vena cava.
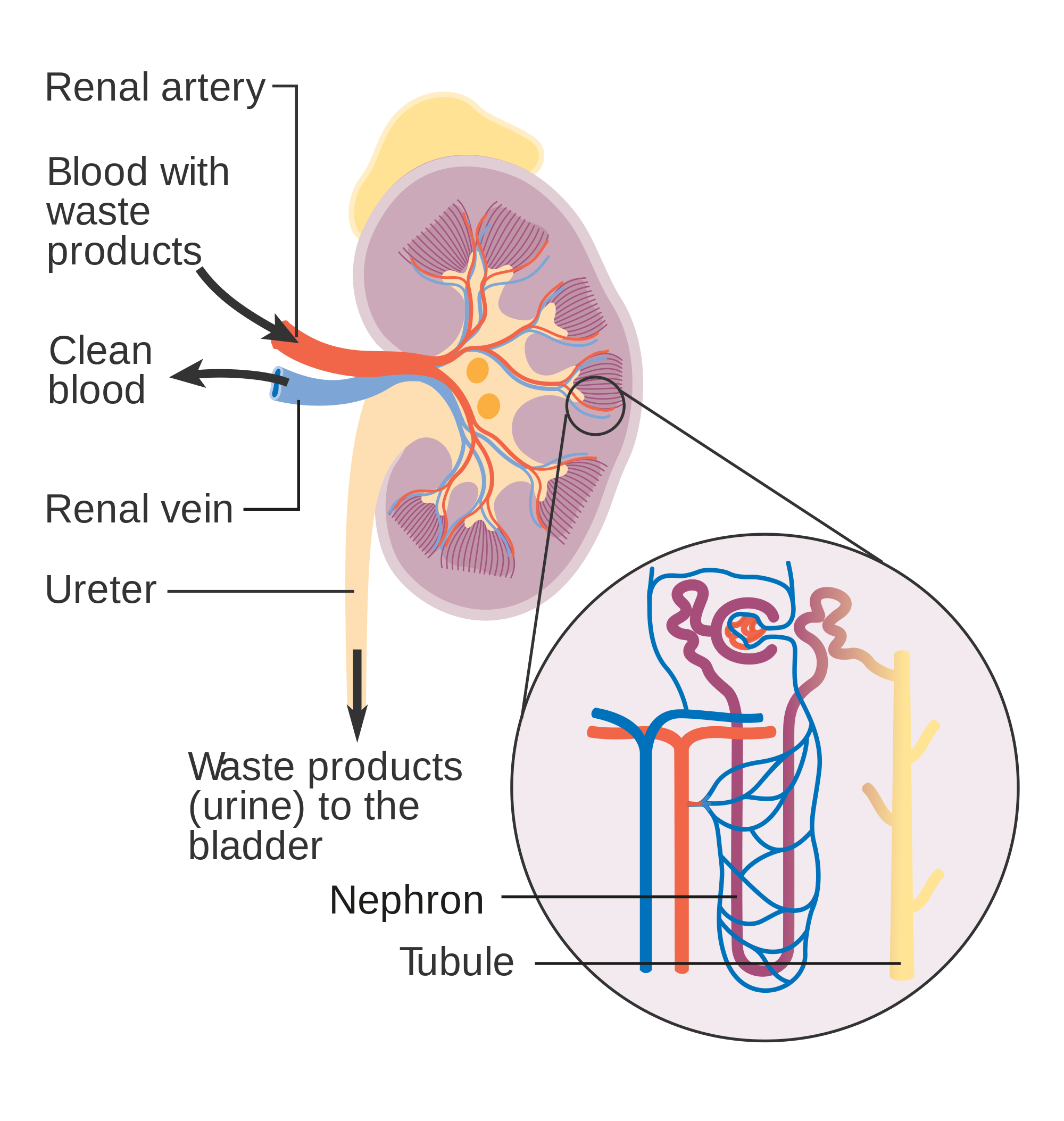
Nephron Structure and Function
Figure 16.4.4 gives an indication of the complex structure of a nephron. The nephron is the basic structural and functional unit of the kidney, and each kidney typically contains at least a million of them. As blood flows through a nephron, many materials are filtered out of the blood, needed materials are returned to the blood, and the remaining materials form urine. Most of the waste products removed from the blood and excreted in urine are byproducts of metabolism. At least half of the waste is urea, a waste product produced by protein catabolism. Another important waste is uric acid, produced in nucleic acid catabolism.
Components of a Nephron
Figure 16.4.5 shows in greater detail the components of a nephron. Each nephron is composed of an initial filtering component that consists of a network of capillaries called the glomerulus (plural, glomeruli), which is surrounded by a space within a structure called glomerular capsule (also known as the Bowman's capsule). Extending from glomerular capsule is the renal tubule. The proximal end (nearest glomerular capsule) of the renal tubule is called the proximal convoluted (coiled) tubule. From here, the renal tubule continues as a loop (known as the loop of Henle) (also known as the loop of the nephron), which in turn becomes the distal convoluted tubule. The latter finally joins with a collecting duct. As you can see in the diagram, arterioles surround the total length of the renal tubule in a mesh called the peritubular capillary network.
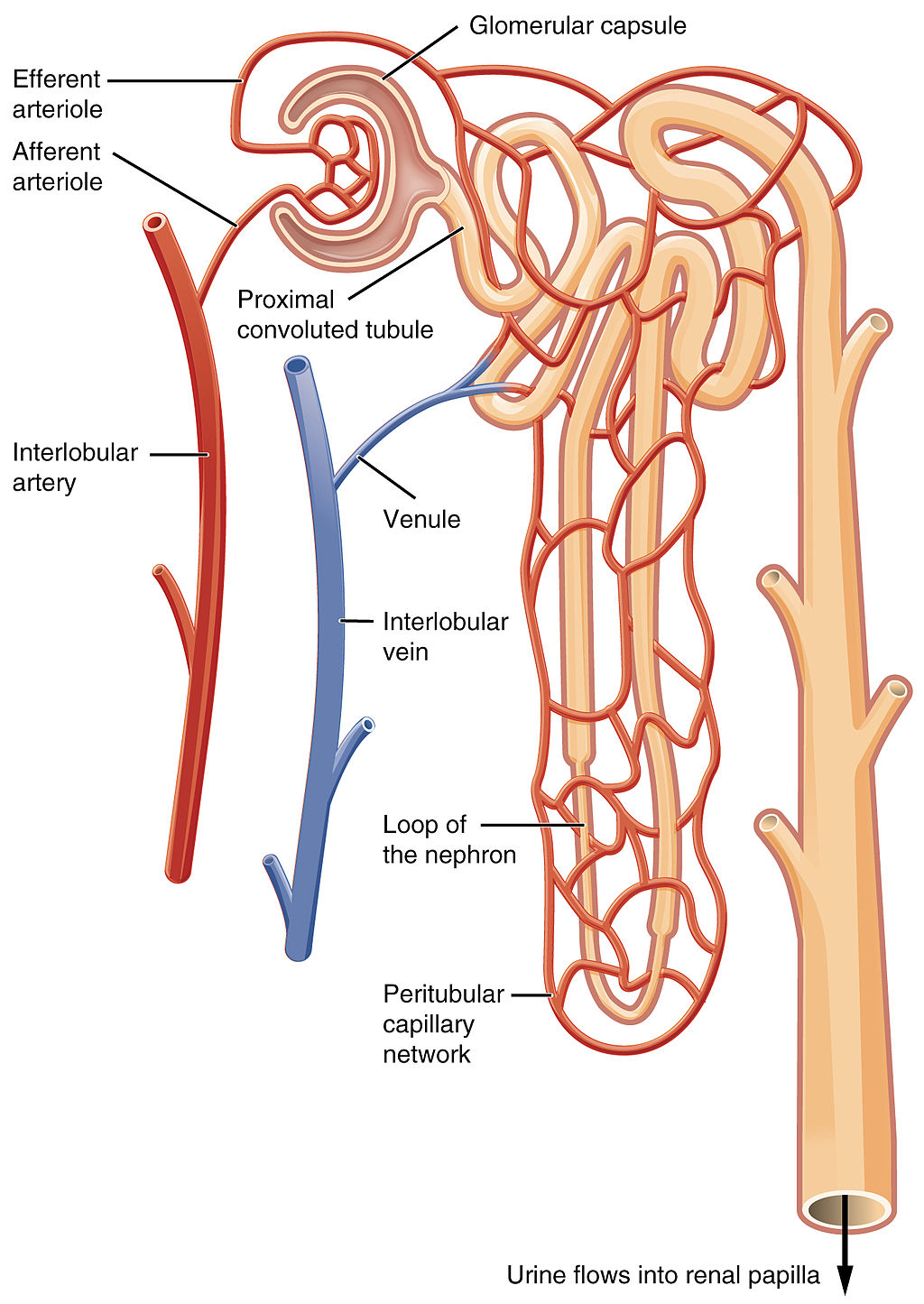
Function of a Nephron
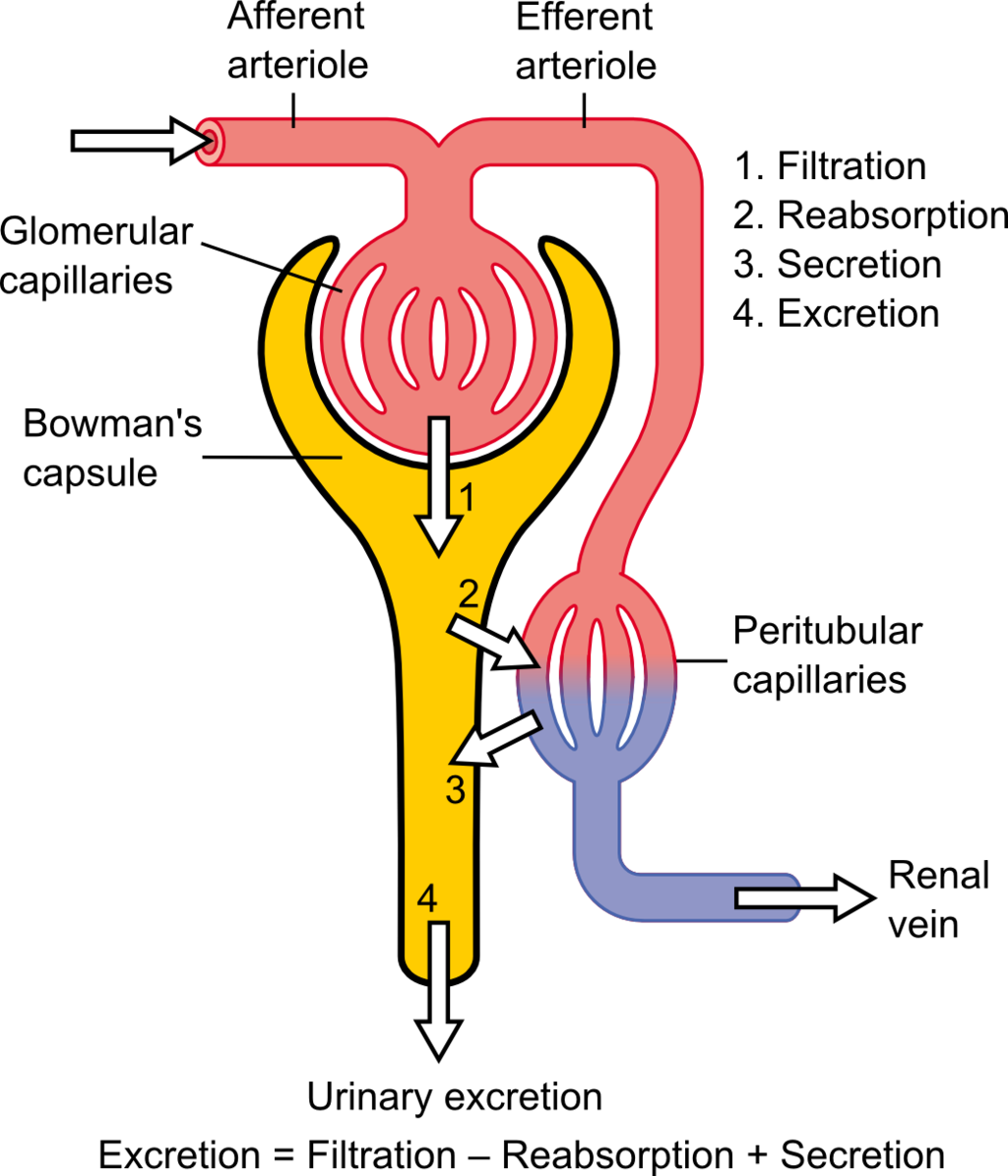
The simplified diagram of a nephron in Figure 16.4.6 shows an overview of how the nephron functions. Blood enters the nephron through an arteriole called the afferent arteriole. Next, some of the blood passes through the capillaries of the glomerulus. Any blood that doesn’t pass through the glomerulus — as well as blood after it passes through the glomerular capillaries — continues on through an arteriole called the efferent arteriole. The efferent arteriole follows the renal tubule of the nephron, where it continues playing a role in nephron functioning.
Filtration
As blood from the afferent arteriole flows through the glomerular capillaries, it is under pressure. Because of the pressure, water and solutes are filtered out of the blood and into the space made by glomerular capsule, almost like the water you cook pasta is is filtered out through a strainer. This is the filtration stage of nephron function. The filtered substances — called filtrate — pass into glomerular capsule, and from there into the proximal end of the renal tubule. Anything too large to move through the pores in the glomerulus, such as blood cells, large proteins, etc., stay in the cardiovascular system. At this stage, filtrate (fluid in the nephron) includes water, salts, organic solids (such as nutrients), and waste products of metabolism (such as urea).
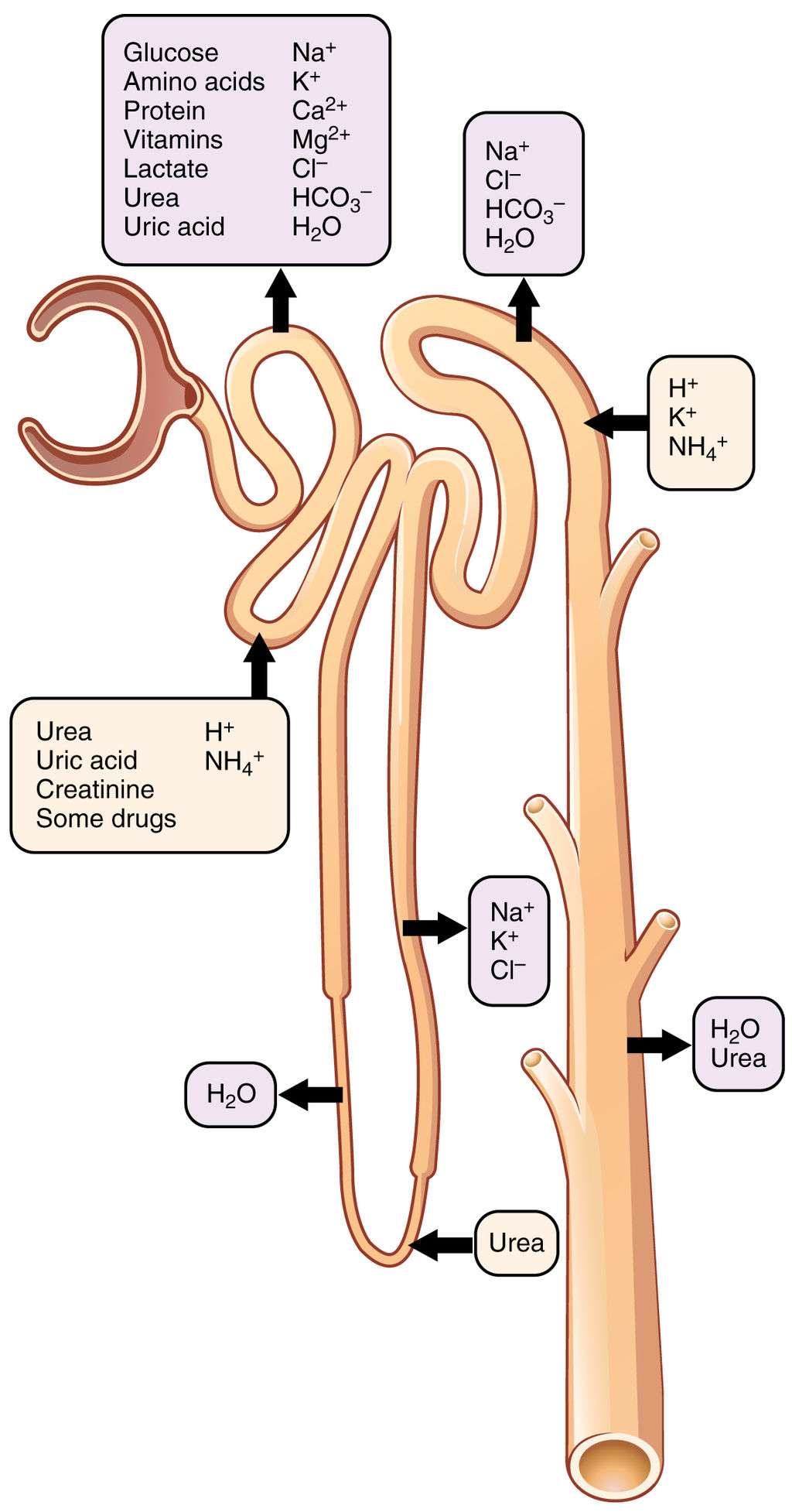
Reabsorption and Secretion
As filtrate moves through the renal tubule, some of the substances it contains are reabsorbed from the filtrate back into the blood in the efferent arteriole (via peritubular capillary network). This is the reabsorption stage of nephron function and it is about returning "the good stuff" back to the blood so that it doesn't exit the body in urine. About two-thirds of the filtered salts and water, and all of the filtered organic solutes (mainly glucose and amino acids) are reabsorbed from the filtrate by the blood in the peritubular capillary network. Reabsorption occurs mainly in the proximal convoluted tubule and the loop of Henle, as seen in Figure 16.4.7.
At the distal end of the renal tubule, some additional reabsorption generally occurs. This is also the region of the tubule where other substances from the blood are added to the filtrate in the tubule. The addition of other substances to the filtrate from the blood is called secretion. Both reabsorption and secretion (shown in Figure 16.4.7) in the distal convoluted tubule are largely under the control of endocrine hormones that maintain homeostasis of water and mineral salts in the blood. These hormones work by controlling what is reabsorbed into the blood from the filtrate and what is secreted from the blood into the filtrate to become urine. For example, parathyroid hormone causes more calcium to be reabsorbed into the blood and more phosphorus to be secreted into the filtrate.
Collection of Urine and Excretion

By the time the filtrate has passed through the entire renal tubule, it has become the liquid waste known as urine. Urine empties from the distal end of the renal tubule into a collecting duct. From there, the urine flows into increasingly larger collecting ducts. As urine flows through the system of collecting ducts, more water may be reabsorbed from it. This will occur in the presence of antidiuretic hormone from the posterior pituitary gland. This hormone makes the collecting ducts permeable to water, allowing water molecules to pass through them into capillaries by osmosis, while preventing the passage of ions or other solutes. As much as 75% of the water may be reabsorbed from urine in the collecting ducts, making the urine more concentrated.
Urine finally exits the largest collecting ducts through the renal papillae. It empties into the renal calyces, and finally into the renal pelvis. From there, it travels through the ureter to the urinary bladder for eventual excretion from the body. An average of roughly 1.5 litres (a little over 6 cups) of urine is excreted each day. Normally, urine is yellow or amber in colour (see Figure 16.4.8). The darker the colour, generally speaking, the more concentrated the urine is.
Besides filtering blood and forming urine for excretion of soluble wastes, the kidneys have several vital functions in maintaining body-wide homeostasis. Most of these functions are related to the composition or volume of urine formed by the kidneys. The kidneys must maintain the proper balance of water and salts in the body, normal blood pressure, and the correct range of blood pH. Through the processes of absorption and secretion by nephrons, more or less water, salt ions, acids, or bases are returned to the blood or excreted in urine, as needed, to maintain homeostasis.
Blood Pressure Regulation
The kidneys do not control homeostasis all alone. As indicated above, endocrine hormones are also involved. Consider the regulation of blood pressure by the kidneys. Blood pressure is the pressure exerted by blood on the walls of the arteries. The regulation of blood pressure is part of a complex system, called the renin-angiotensin-aldosterone system. This system regulates the concentration of sodium in the blood to control blood pressure.
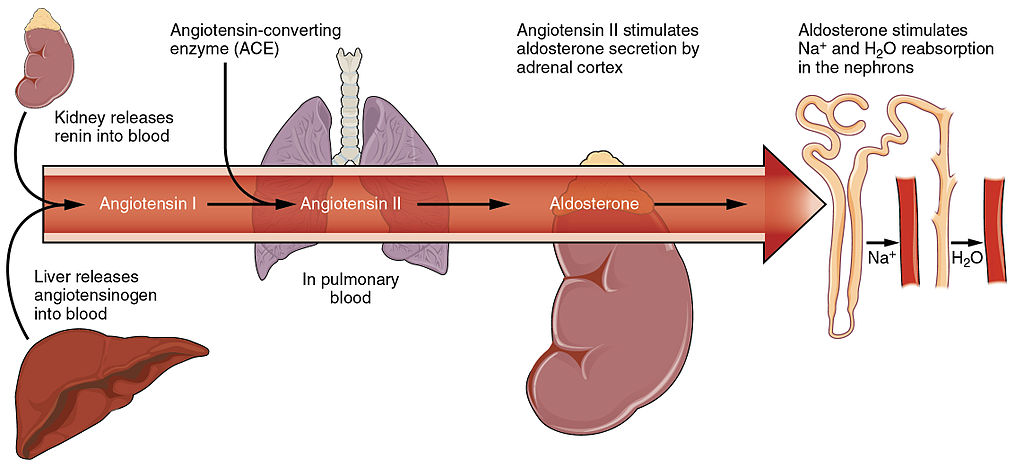
The renin-angiotensin-aldosterone system is put into play when the concentration of sodium ions in the blood falls lower than normal. This causes the kidneys to secrete an enzyme called renin into the blood. It also causes the liver to secrete a protein called angiotensinogen. Renin changes angiotensinogen into a proto-hormone called angiotensin I. This is converted to angiotensin II by an enzyme (angiotensin-converting enzyme) in lung capillaries.
Angiotensin II is a potent hormone that causes arterioles to constrict. This, in turn, increases blood pressure. Angiotensin II also stimulates the secretion of the hormone aldosterone from the adrenal cortex. Aldosterone causes the kidneys to increase the reabsorption of sodium ions and water from the filtrate into the blood. This returns the concentration of sodium ions in the blood to normal. The increased water in the blood also increases blood volume and blood pressure.
Other Kidney Hormones
Hormones other than renin are also produced and secreted by the kidneys. These include calcitriol and erythropoietin.
- Calcitriol is secreted by the kidneys in response to low levels of calcium in the blood. This hormone stimulates uptake of calcium by the intestine, thus raising blood levels of calcium.
- Erythropoietin is secreted by the kidneys in response to low levels of oxygen in the blood. This hormone stimulates erythropoiesis, which is the production of erythrocytes in bone marrow. Extra red blood cells increase the level of oxygen carried in the blood.
Feature: Human Biology in the News
Kidney failure is a complication of common disorders including diabetes mellitus and hypertension. It is estimated that approximately 12.5% of Canadians have some form of kidney disease. If the disease is serious, the patient must either receive a donated kidney or have frequent hemodialysis, a medical procedure in which the blood is artificially filtered through a machine. Transplant generally results in better outcomes than hemodialysis, but demand for organs far outstrips the supply. The average time on the organ donation waitlist for a kidney is four years. There are over 3,000 Canadians on the wait list for a kidney transplant and some will die waiting for a kidney to become available.
For the past decade, Dr. William Fissell, a kidney specialist at Vanderbilt University, has been working to create an implantable part-biological and part-artificial kidney. Using microchips like those used in computers, he has produced an artificial kidney small enough to implant in the patient’s body in place of the failed kidney. According to Dr. Fissell, the artificial kidney is “... a bio-hybrid device that can mimic a kidney to remove enough waste products, salt, and water to keep a patient off [hemo]dialysis.”
The filtration system in the artificial kidney consists of a stack of 15 microchips. Tiny pores in the microchips act as a scaffold for the growth of living kidney cells that can mimic the natural functions of the kidney. The living cells form a membrane to filter the patient’s blood as a biological kidney would, but with less risk of rejection by the patient’s immune system, because they are embedded within the device. The new kidney doesn’t need a power source, because it uses the natural pressure of blood flowing through arteries to push the blood through the filtration system. A major part of the design of the artificial organ was devoted to fine tuning the fluid dynamics so blood flows through the device without clotting.
Because of the potential life-saving benefits of the device, the implantable kidney was given fast-track approval for testing in people by the U.S. Food and Drug Administration. The artificial kidney is expected to be tested in pilot trials by 2018. Dr. Fissell says he has a long list of patients eager to volunteer for the trials.
16.4 Summary
- The two bean-shaped kidneys are located high in the back of the abdominal cavity on either side of the spine. A renal artery connects each kidney with the aorta, and transports unfiltered blood to the kidney. A renal vein connects each kidney with the inferior vena cava and transports filtered blood back to the circulation.
- The kidney has two main layers involved in the filtration of blood and formation of urine: the outer cortex and inner medulla. At least a million nephrons — which are the tiny functional units of the kidney — span the cortex and medulla. The entire kidney is surrounded by a fibrous capsule and protective fat layers.
- As blood flows through a nephron, many materials are filtered out of the blood, needed materials are returned to the blood, and the remaining materials are used to form urine.
- In each nephron, the glomerulus and surrounding Bowman’s capsule form the unit that filters blood. From Bowman’s capsule, the material filtered from blood (called filtrate) passes through the long renal tubule. As it does, some substances are reabsorbed into the blood, and other substances are secreted from the blood into the filtrate, finally forming urine. The urine empties into collecting ducts, where more water may be reabsorbed.
- The kidneys control homeostasis with the help of endocrine hormones. The kidneys, for example, are part of the renin-angiotensin-aldosterone system that regulates the concentration of sodium in the blood to control blood pressure. In this system, the enzyme renin secreted by the kidneys works with hormones from the liver and adrenal gland to stimulate nephrons to reabsorb more sodium and water from urine.
- The kidneys also secrete endocrine hormones, including calcitriol — which helps control the level of calcium in the blood — and erythropoietin, which stimulates bone marrow to produce red blood cells.
16.4 Review Questions
-
- Contrast the renal artery and renal vein.
- Identify the functions of a nephron. Describe in detail what happens to fluids (blood, filtrate, and urine) as they pass through the parts of a nephron.
- Identify two endocrine hormones secreted by the kidneys, along with the functions they control.
- Name two regions in the kidney where water is reabsorbed.
- Is the blood in the glomerular capillaries more or less filtered than the blood in the peritubular capillaries? Explain your answer.
- What do you think would happen if blood flow to the kidneys is blocked?
16.4 Explore More
https://youtu.be/FN3MFhYPWWo
How do your kidneys work? - Emma Bryce, TED-Ed, 2015.
https://youtu.be/es-t8lO1KpA
Urine Formation, Hamada Abass, 2013.
https://youtu.be/bX3C201O4MA
Printing a human kidney - Anthony Atala, TED-Ed, 2013.
Attributions
Figure 16.4.1
Steak and Kidney Pie by Charles Haynes on Flickr is used under a CC BY-SA 2.0 (https://creativecommons.org/licenses/by-sa/2.0/) license.
Figure 16.4.2
Gray Kidneys by Henry Vandyke Carter (1831-1897) on Wikimedia Commons is in the public domain (https://en.wikipedia.org/wiki/public_domain). (Bartleby.com: Gray’s Anatomy, Plate 1120).
Figure 16.4.3
Blausen_0592_KidneyAnatomy_01 by BruceBlaus on Wikimedia Commons is used under a CC BY 3.0 (https://creativecommons.org/licenses/by/3.0) license.
Figure 16.4.4
Diagram_showing_how_the_kidneys_work_CRUK_138.svg by Cancer Research UK on Wikimedia Commons is used under a CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0) license.
Figure 16.4.5
Blood_Flow_in_the_Nephron by OpenStax College on Wikimedia Commons is used under a CC BY 3.0 (https://creativecommons.org/licenses/by/3.0) license.
Figure 16.4.6
1024px-Physiology_of_Nephron by Madhero88 on Wikimedia Commons is used under a CC BY 3.0 (https://creativecommons.org/licenses/by/3.0) license.
Figure 16.4.7
Nephron_Secretion_Reabsorption by OpenStax College on Wikimedia Commons is used under a CC BY 3.0 (https://creativecommons.org/licenses/by/3.0) license.
Figure 16.4.8
Urine by User:Markhamilton at English Wikipedia on Wikimedia Commons is in the public domain (https://en.wikipedia.org/wiki/Public_domain).
Figure 16.4.9
Renin_Angiotensin_System-01 by OpenStax College on Wikimedia Commons is used under a CC BY 3.0 (https://creativecommons.org/licenses/by/3.0) license.
References
Betts, J. G., Young, K.A., Wise, J.A., Johnson, E., Poe, B., Kruse, D.H., Korol, O., Johnson, J.E., Womble, M., DeSaix, P. (2013, June 19). Figure 25.10 Blood flow in the nephron [digital image]. In Anatomy and Physiology (Section 25.3). OpenStax. https://openstax.org/books/anatomy-and-physiology/pages/25-3-gross-anatomy-of-the-kidney
Betts, J. G., Young, K.A., Wise, J.A., Johnson, E., Poe, B., Kruse, D.H., Korol, O., Johnson, J.E., Womble, M., DeSaix, P. (2013, June 19). Figure 25.17 Locations of secretion and reabsorption in the nephron [digital image]. In Anatomy and Physiology (Section 25.6). OpenStax. https://openstax.org/books/anatomy-and-physiology/pages/25-6-tubular-reabsorption
Betts, J. G., Young, K.A., Wise, J.A., Johnson, E., Poe, B., Kruse, D.H., Korol, O., Johnson, J.E., Womble, M., DeSaix, P. (2013, June 19). Figure 26.14 The renin-angiotensin system [digital image]. In Anatomy and Physiology (Section 26.3). OpenStax. https://openstax.org/books/anatomy-and-physiology/pages/26-3-electrolyte-balance
Blausen.com Staff. (2014). Medical gallery of Blausen Medical 2014. WikiJournal of Medicine 1 (2). DOI:10.15347/wjm/2014.010. ISSN 2002-4436
Hamada Abass. (2013). Urine formation. YouTube. https://www.youtube.com/watch?v=es-t8lO1KpA&feature=youtu.be
TED-Ed. (2015, February 9). How do your kidneys work? - Emma Bryce. YouTube. https://www.youtube.com/watch?v=FN3MFhYPWWo&feature=youtu.be
TED-Ed. (2013, March 15). Printing a human kidney - Anthony Atala. YouTube. https://www.youtube.com/watch?v=bX3C201O4MA&feature=youtu.be
Created by CK-12 Foundation/Adapted by Christine Miller

Kidneys on the Menu
Pictured in Figure 16.4.1 is a steak and kidney pie; this savory dish is a British favorite. When kidneys are on a menu, they typically come from sheep, pigs, or cows. In these animals (as in the human animal), kidneys are the main organs of excretion.
Location of the Kidneys
The two bean-shaped kidneys are located high in the back of the abdominal cavity, one on each side of the spine. Both kidneys sit just below the diaphragm, the large breathing muscle that separates the abdominal and thoracic cavities. As you can see in the following figure, the right kidney is slightly smaller and lower than the left kidney. The right kidney is behind the liver, and the left kidney is behind the spleen. The location of the liver explains why the right kidney is smaller and lower than the left.
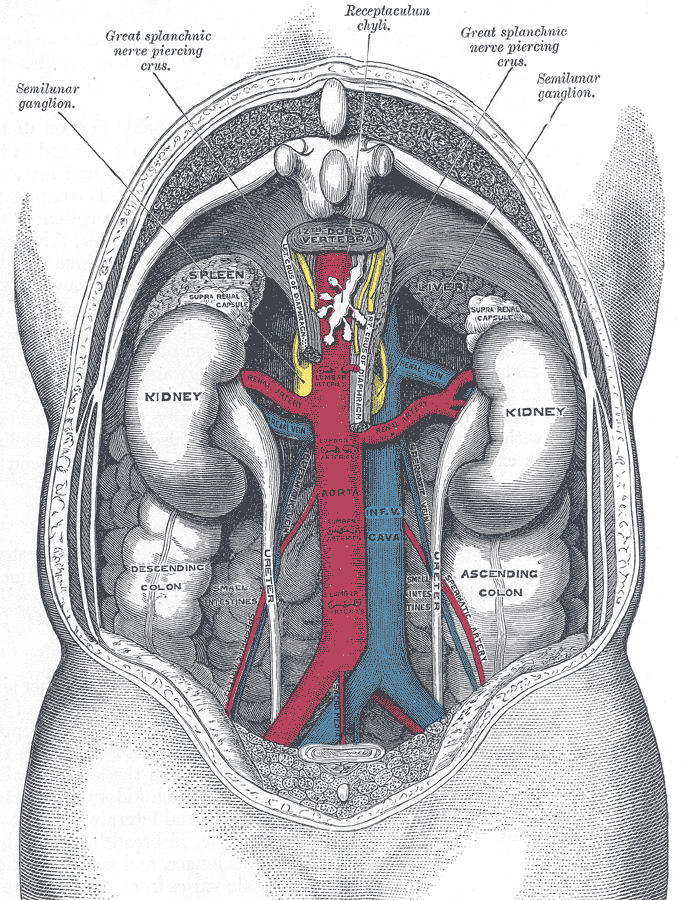
Kidney Anatomy
The shape of each kidney gives it a convex side (curving outward) and a concave side (curving inward). You can see this clearly in the detailed diagram of kidney anatomy shown in Figure 16.4.3. The concave side is where the renal artery enters the kidney, as well as where the renal vein and ureter leave the kidney. This area of the kidney is called the hilum. The entire kidney is surrounded by tough fibrous tissue — called the renal capsule — which, in turn, is surrounded by two layers of protective, cushioning fat.
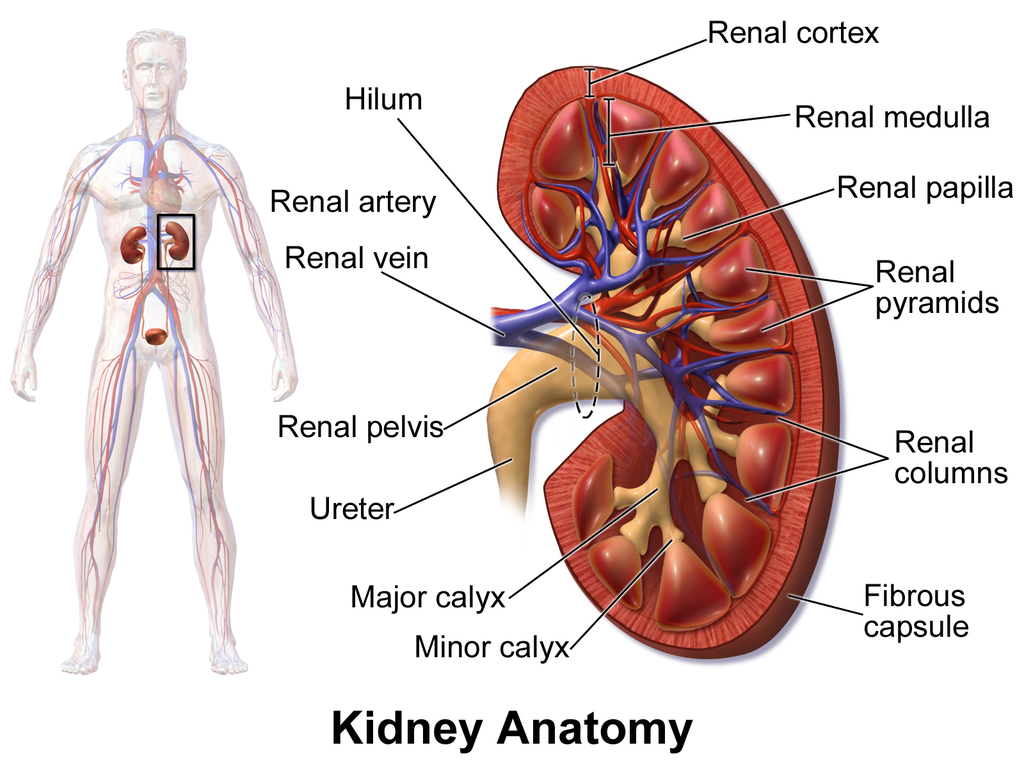
Internally, each kidney is divided into two major layers: the outer renal cortex and the inner renal medulla (see Figure 16.4.3 above). These layers take the shape of many cone-shaped renal lobules, each containing renal cortex surrounding a portion of medulla called a renal pyramid. Within the renal pyramids are the structural and functional units of the kidneys, the tiny nephrons. Between the renal pyramids are projections of cortex called renal columns. The tip, or papilla, of each pyramid empties urine into a minor calyx (chamber). Several minor calyces empty into a major calyx, and the latter empty into the funnel-shaped cavity called the renal pelvis, which becomes the ureter as it leaves the kidney.
Renal Circulation
The renal circulation is an important part of the kidney’s primary function of filtering waste products from the blood. Blood is supplied to the kidneys via the renal arteries. The right renal artery supplies the right kidney, and the left renal artery supplies the left kidney. These two arteries branch directly from the aorta, which is the largest artery in the body. Each kidney is only about 11 cm (4.4 in) long, and has a mass of just 150 grams (5.3 oz), yet it receives about ten per cent of the total output of blood from the heart. Blood is filtered through the kidneys every 3 minutes, 24 hours a day, every day of your life.
As indicated in Figure 16.4.4, each renal artery carries blood with waste products into the kidney. Within the kidney, the renal artery branches into increasingly smaller arteries that extend through the renal columns between the renal pyramids. These arteries, in turn, branch into arterioles that penetrate the renal pyramids. Blood in the arterioles passes through nephrons, the structures that actually filter the blood. After blood passes through the nephrons and is filtered, the clean blood moves through a network of venules that converge into small veins. Small veins merge into increasingly larger ones, and ultimately into the renal vein, which carries clean blood away from the kidney to the inferior vena cava.
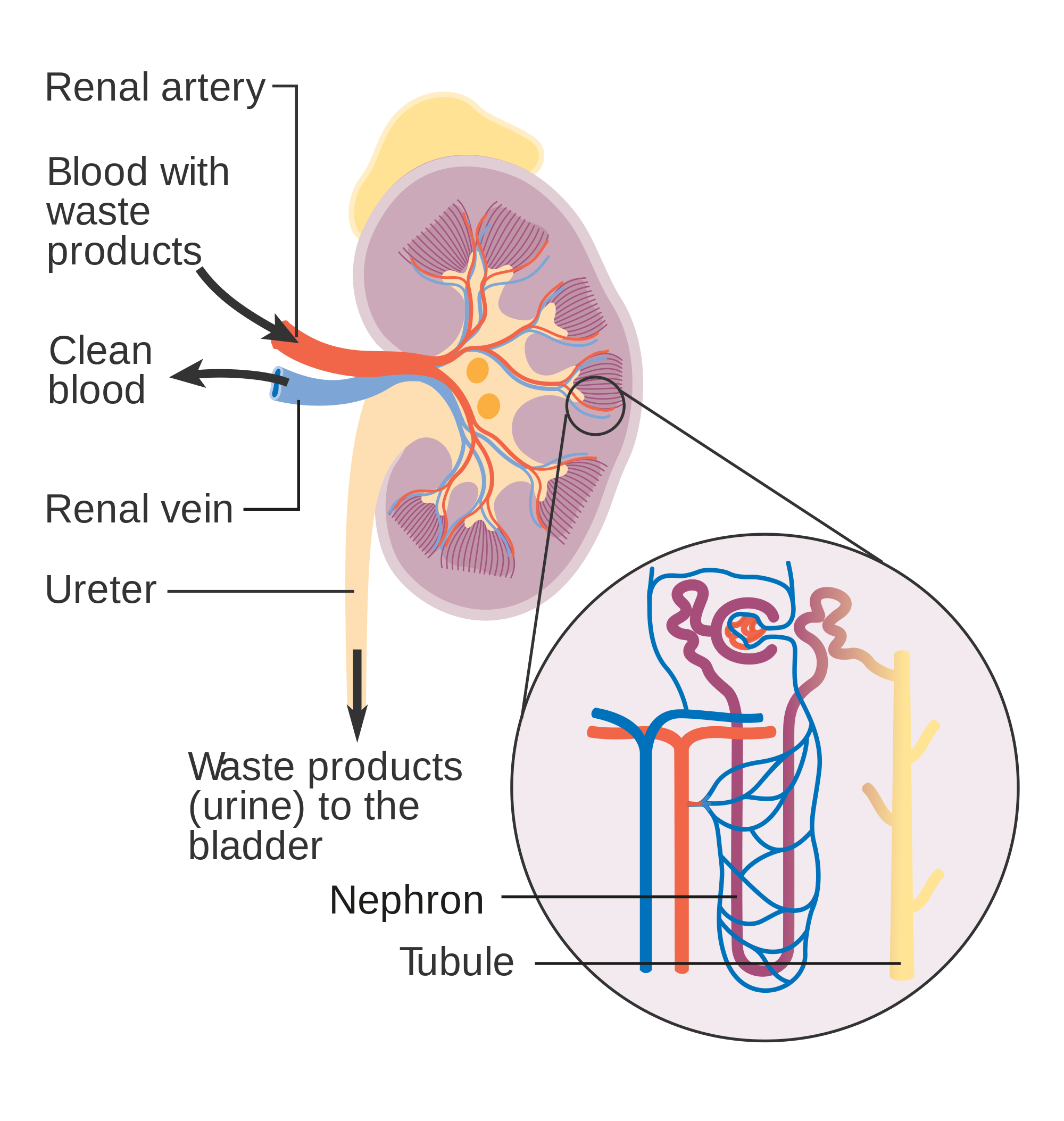
Nephron Structure and Function
Figure 16.4.4 gives an indication of the complex structure of a nephron. The nephron is the basic structural and functional unit of the kidney, and each kidney typically contains at least a million of them. As blood flows through a nephron, many materials are filtered out of the blood, needed materials are returned to the blood, and the remaining materials form urine. Most of the waste products removed from the blood and excreted in urine are byproducts of metabolism. At least half of the waste is urea, a waste product produced by protein catabolism. Another important waste is uric acid, produced in nucleic acid catabolism.
Components of a Nephron
Figure 16.4.5 shows in greater detail the components of a nephron. Each nephron is composed of an initial filtering component that consists of a network of capillaries called the glomerulus (plural, glomeruli), which is surrounded by a space within a structure called glomerular capsule (also known as the Bowman's capsule). Extending from glomerular capsule is the renal tubule. The proximal end (nearest glomerular capsule) of the renal tubule is called the proximal convoluted (coiled) tubule. From here, the renal tubule continues as a loop (known as the loop of Henle) (also known as the loop of the nephron), which in turn becomes the distal convoluted tubule. The latter finally joins with a collecting duct. As you can see in the diagram, arterioles surround the total length of the renal tubule in a mesh called the peritubular capillary network.
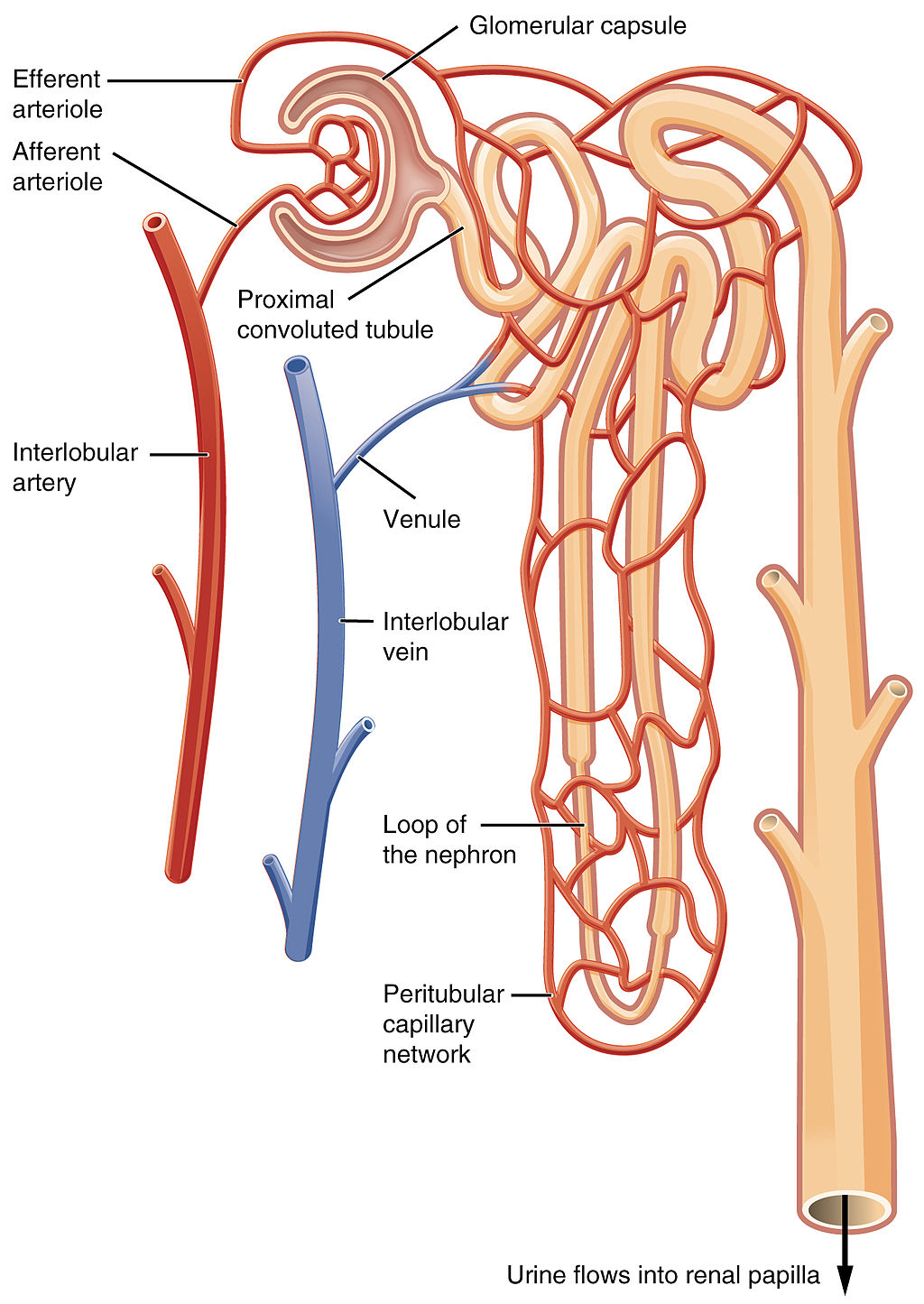
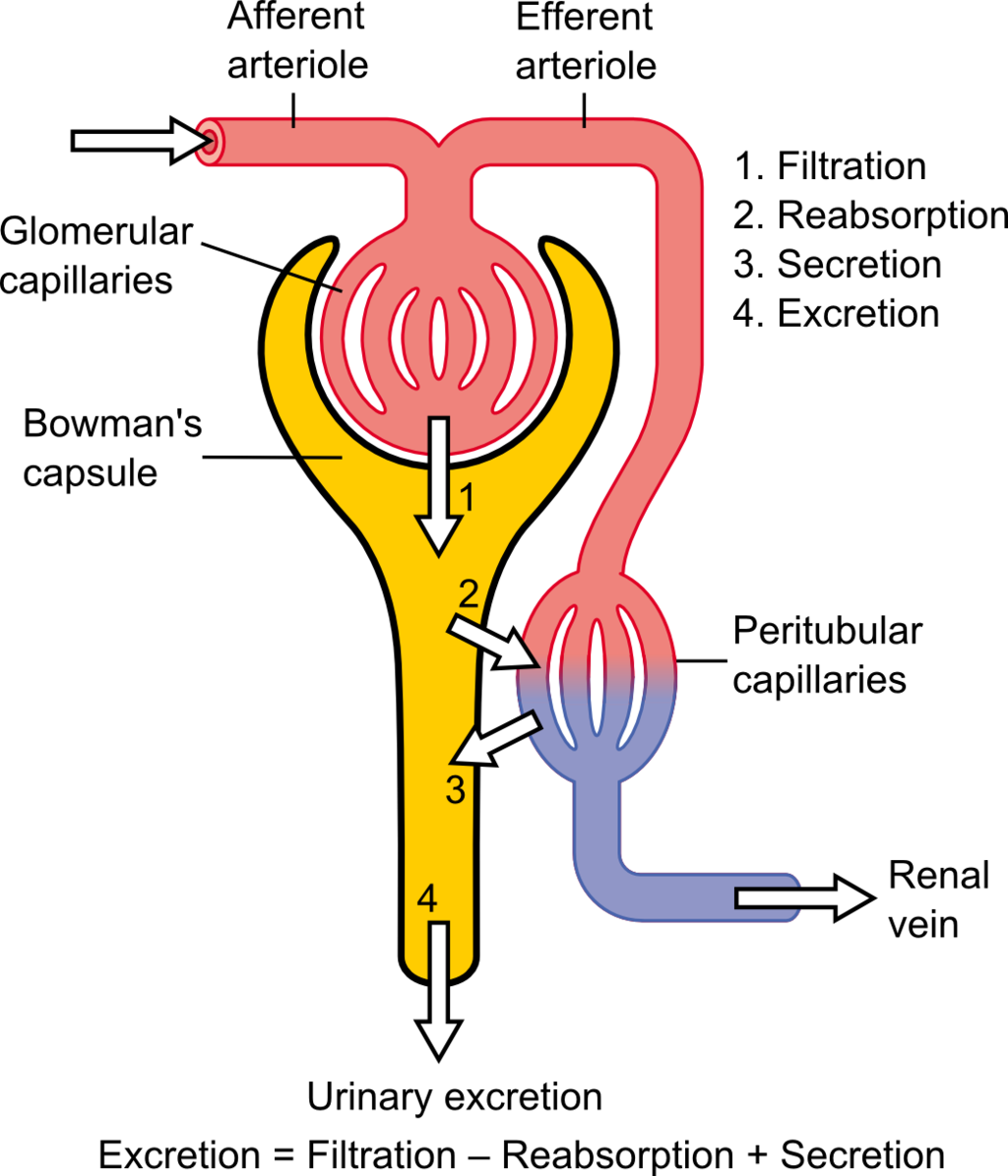
Function of a Nephron
The simplified diagram of a nephron in Figure 16.4.6 shows an overview of how the nephron functions. Blood enters the nephron through an arteriole called the afferent arteriole. Next, some of the blood passes through the capillaries of the glomerulus. Any blood that doesn’t pass through the glomerulus — as well as blood after it passes through the glomerular capillaries — continues on through an arteriole called the efferent arteriole. The efferent arteriole follows the renal tubule of the nephron, where it continues playing a role in nephron functioning.
Filtration
As blood from the afferent arteriole flows through the glomerular capillaries, it is under pressure. Because of the pressure, water and solutes are filtered out of the blood and into the space made by glomerular capsule, almost like the water you cook pasta is is filtered out through a strainer. This is the filtration stage of nephron function. The filtered substances — called filtrate — pass into glomerular capsule, and from there into the proximal end of the renal tubule. Anything too large to move through the pores in the glomerulus, such as blood cells, large proteins, etc., stay in the cardiovascular system. At this stage, filtrate (fluid in the nephron) includes water, salts, organic solids (such as nutrients), and waste products of metabolism (such as urea).
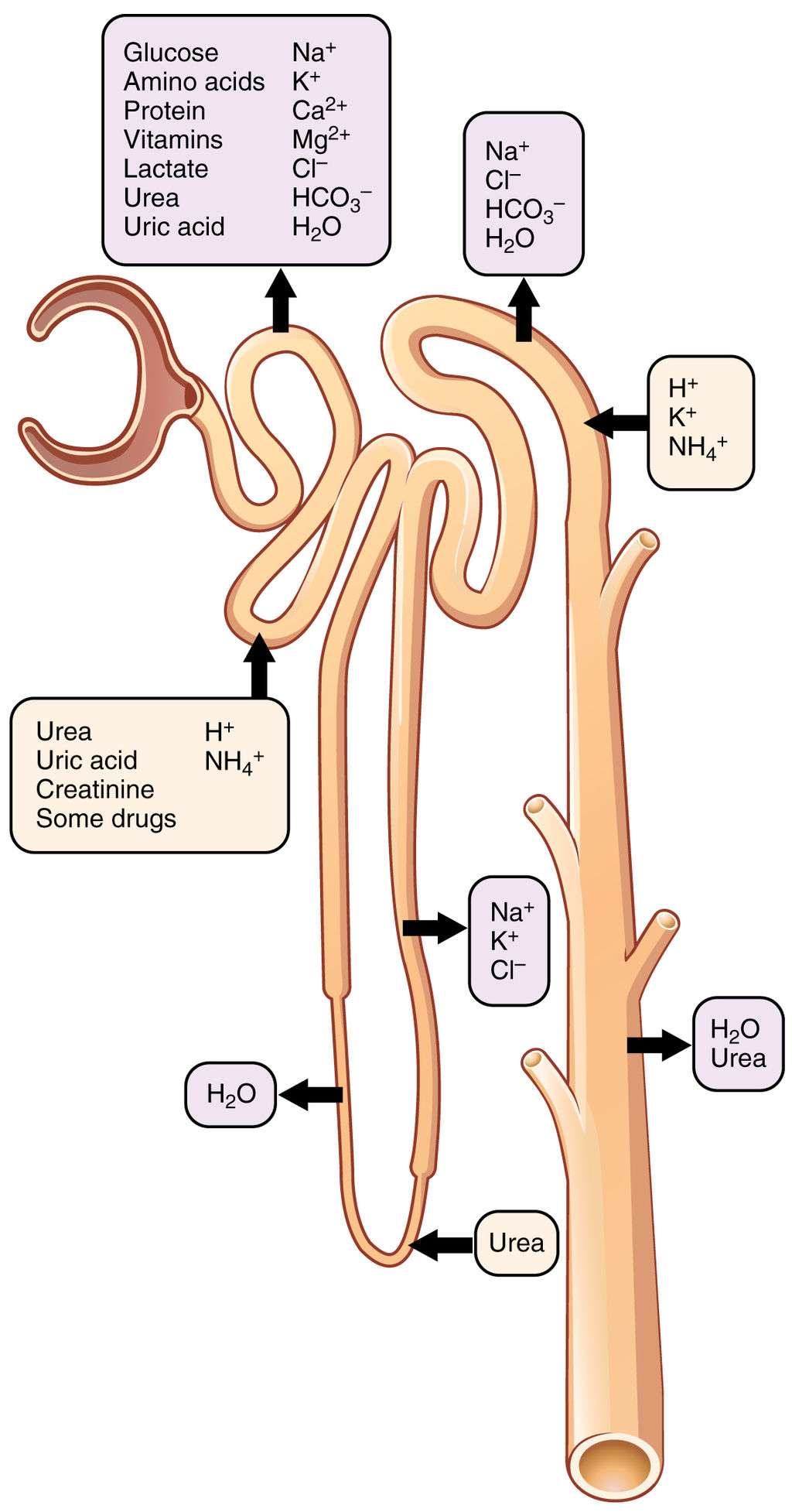
Reabsorption and Secretion
As filtrate moves through the renal tubule, some of the substances it contains are reabsorbed from the filtrate back into the blood in the efferent arteriole (via peritubular capillary network). This is the reabsorption stage of nephron function and it is about returning "the good stuff" back to the blood so that it doesn't exit the body in urine. About two-thirds of the filtered salts and water, and all of the filtered organic solutes (mainly glucose and amino acids) are reabsorbed from the filtrate by the blood in the peritubular capillary network. Reabsorption occurs mainly in the proximal convoluted tubule and the loop of Henle, as seen in Figure 16.4.7.
At the distal end of the renal tubule, some additional reabsorption generally occurs. This is also the region of the tubule where other substances from the blood are added to the filtrate in the tubule. The addition of other substances to the filtrate from the blood is called secretion. Both reabsorption and secretion (shown in Figure 16.4.7) in the distal convoluted tubule are largely under the control of endocrine hormones that maintain homeostasis of water and mineral salts in the blood. These hormones work by controlling what is reabsorbed into the blood from the filtrate and what is secreted from the blood into the filtrate to become urine. For example, parathyroid hormone causes more calcium to be reabsorbed into the blood and more phosphorus to be secreted into the filtrate.
Collection of Urine and Excretion

By the time the filtrate has passed through the entire renal tubule, it has become the liquid waste known as urine. Urine empties from the distal end of the renal tubule into a collecting duct. From there, the urine flows into increasingly larger collecting ducts. As urine flows through the system of collecting ducts, more water may be reabsorbed from it. This will occur in the presence of antidiuretic hormone from the posterior pituitary gland. This hormone makes the collecting ducts permeable to water, allowing water molecules to pass through them into capillaries by osmosis, while preventing the passage of ions or other solutes. As much as 75% of the water may be reabsorbed from urine in the collecting ducts, making the urine more concentrated.
Urine finally exits the largest collecting ducts through the renal papillae. It empties into the renal calyces, and finally into the renal pelvis. From there, it travels through the ureter to the urinary bladder for eventual excretion from the body. An average of roughly 1.5 litres (a little over 6 cups) of urine is excreted each day. Normally, urine is yellow or amber in colour (see Figure 16.4.8). The darker the colour, generally speaking, the more concentrated the urine is.
Besides filtering blood and forming urine for excretion of soluble wastes, the kidneys have several vital functions in maintaining body-wide homeostasis. Most of these functions are related to the composition or volume of urine formed by the kidneys. The kidneys must maintain the proper balance of water and salts in the body, normal blood pressure, and the correct range of blood pH. Through the processes of absorption and secretion by nephrons, more or less water, salt ions, acids, or bases are returned to the blood or excreted in urine, as needed, to maintain homeostasis.
Blood Pressure Regulation
The kidneys do not control homeostasis all alone. As indicated above, endocrine hormones are also involved. Consider the regulation of blood pressure by the kidneys. Blood pressure is the pressure exerted by blood on the walls of the arteries. The regulation of blood pressure is part of a complex system, called the renin-angiotensin-aldosterone system. This system regulates the concentration of sodium in the blood to control blood pressure.
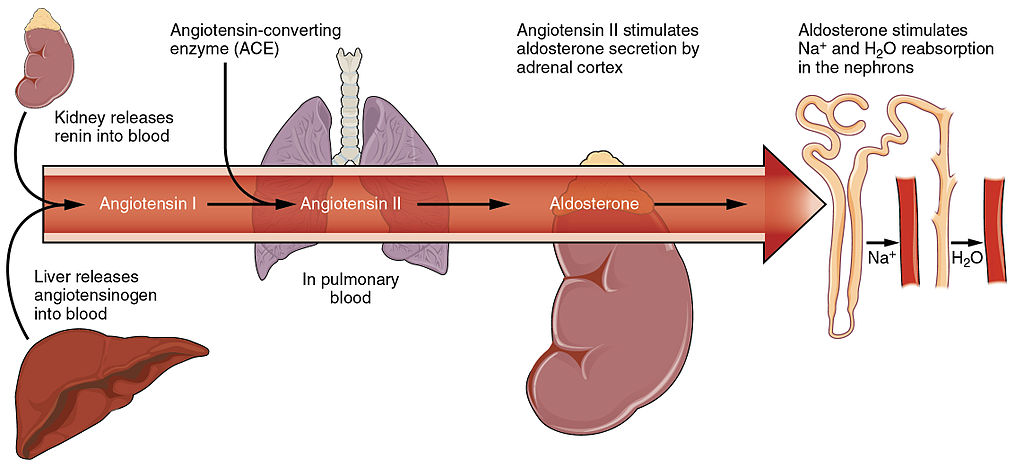
The renin-angiotensin-aldosterone system is put into play when the concentration of sodium ions in the blood falls lower than normal. This causes the kidneys to secrete an enzyme called renin into the blood. It also causes the liver to secrete a protein called angiotensinogen. Renin changes angiotensinogen into a proto-hormone called angiotensin I. This is converted to angiotensin II by an enzyme (angiotensin-converting enzyme) in lung capillaries.
Angiotensin II is a potent hormone that causes arterioles to constrict. This, in turn, increases blood pressure. Angiotensin II also stimulates the secretion of the hormone aldosterone from the adrenal cortex. Aldosterone causes the kidneys to increase the reabsorption of sodium ions and water from the filtrate into the blood. This returns the concentration of sodium ions in the blood to normal. The increased water in the blood also increases blood volume and blood pressure.
Other Kidney Hormones
Hormones other than renin are also produced and secreted by the kidneys. These include calcitriol and erythropoietin.
- Calcitriol is secreted by the kidneys in response to low levels of calcium in the blood. This hormone stimulates uptake of calcium by the intestine, thus raising blood levels of calcium.
- Erythropoietin is secreted by the kidneys in response to low levels of oxygen in the blood. This hormone stimulates erythropoiesis, which is the production of erythrocytes in bone marrow. Extra red blood cells increase the level of oxygen carried in the blood.
Feature: Human Biology in the News
Kidney failure is a complication of common disorders including diabetes mellitus and hypertension. It is estimated that approximately 12.5% of Canadians have some form of kidney disease. If the disease is serious, the patient must either receive a donated kidney or have frequent hemodialysis, a medical procedure in which the blood is artificially filtered through a machine. Transplant generally results in better outcomes than hemodialysis, but demand for organs far outstrips the supply. The average time on the organ donation waitlist for a kidney is four years. There are over 3,000 Canadians on the wait list for a kidney transplant and some will die waiting for a kidney to become available.
For the past decade, Dr. William Fissell, a kidney specialist at Vanderbilt University, has been working to create an implantable part-biological and part-artificial kidney. Using microchips like those used in computers, he has produced an artificial kidney small enough to implant in the patient’s body in place of the failed kidney. According to Dr. Fissell, the artificial kidney is “... a bio-hybrid device that can mimic a kidney to remove enough waste products, salt, and water to keep a patient off [hemo]dialysis.”
The filtration system in the artificial kidney consists of a stack of 15 microchips. Tiny pores in the microchips act as a scaffold for the growth of living kidney cells that can mimic the natural functions of the kidney. The living cells form a membrane to filter the patient’s blood as a biological kidney would, but with less risk of rejection by the patient’s immune system, because they are embedded within the device. The new kidney doesn’t need a power source, because it uses the natural pressure of blood flowing through arteries to push the blood through the filtration system. A major part of the design of the artificial organ was devoted to fine tuning the fluid dynamics so blood flows through the device without clotting.
Because of the potential life-saving benefits of the device, the implantable kidney was given fast-track approval for testing in people by the U.S. Food and Drug Administration. The artificial kidney is expected to be tested in pilot trials by 2018. Dr. Fissell says he has a long list of patients eager to volunteer for the trials.
16.4 Summary
- The two bean-shaped kidneys are located high in the back of the abdominal cavity on either side of the spine. A renal artery connects each kidney with the aorta, and transports unfiltered blood to the kidney. A renal vein connects each kidney with the inferior vena cava and transports filtered blood back to the circulation.
- The kidney has two main layers involved in the filtration of blood and formation of urine: the outer cortex and inner medulla. At least a million nephrons — which are the tiny functional units of the kidney — span the cortex and medulla. The entire kidney is surrounded by a fibrous capsule and protective fat layers.
- As blood flows through a nephron, many materials are filtered out of the blood, needed materials are returned to the blood, and the remaining materials are used to form urine.
- In each nephron, the glomerulus and surrounding Bowman’s capsule form the unit that filters blood. From Bowman’s capsule, the material filtered from blood (called filtrate) passes through the long renal tubule. As it does, some substances are reabsorbed into the blood, and other substances are secreted from the blood into the filtrate, finally forming urine. The urine empties into collecting ducts, where more water may be reabsorbed.
- The kidneys control homeostasis with the help of endocrine hormones. The kidneys, for example, are part of the renin-angiotensin-aldosterone system that regulates the concentration of sodium in the blood to control blood pressure. In this system, the enzyme renin secreted by the kidneys works with hormones from the liver and adrenal gland to stimulate nephrons to reabsorb more sodium and water from urine.
- The kidneys also secrete endocrine hormones, including calcitriol — which helps control the level of calcium in the blood — and erythropoietin, which stimulates bone marrow to produce red blood cells.
16.4 Review Questions
-
- Contrast the renal artery and renal vein.
- Identify the functions of a nephron. Describe in detail what happens to fluids (blood, filtrate, and urine) as they pass through the parts of a nephron.
- Identify two endocrine hormones secreted by the kidneys, along with the functions they control.
- Name two regions in the kidney where water is reabsorbed.
- Is the blood in the glomerular capillaries more or less filtered than the blood in the peritubular capillaries? Explain your answer.
- What do you think would happen if blood flow to the kidneys is blocked?
16.4 Explore More
https://youtu.be/FN3MFhYPWWo
How do your kidneys work? - Emma Bryce, TED-Ed, 2015.
https://youtu.be/es-t8lO1KpA
Urine Formation, Hamada Abass, 2013.
https://youtu.be/bX3C201O4MA
Printing a human kidney - Anthony Atala, TED-Ed, 2013.
Attributions
Figure 16.4.1
Steak and Kidney Pie by Charles Haynes on Flickr is used under a CC BY-SA 2.0 (https://creativecommons.org/licenses/by-sa/2.0/) license.
Figure 16.4.2
Gray Kidneys by Henry Vandyke Carter (1831-1897) on Wikimedia Commons is in the public domain (https://en.wikipedia.org/wiki/public_domain). (Bartleby.com: Gray’s Anatomy, Plate 1120).
Figure 16.4.3
Blausen_0592_KidneyAnatomy_01 by BruceBlaus on Wikimedia Commons is used under a CC BY 3.0 (https://creativecommons.org/licenses/by/3.0) license.
Figure 16.4.4
Diagram_showing_how_the_kidneys_work_CRUK_138.svg by Cancer Research UK on Wikimedia Commons is used under a CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0) license.
Figure 16.4.5
Blood_Flow_in_the_Nephron by OpenStax College on Wikimedia Commons is used under a CC BY 3.0 (https://creativecommons.org/licenses/by/3.0) license.
Figure 16.4.6
1024px-Physiology_of_Nephron by Madhero88 on Wikimedia Commons is used under a CC BY 3.0 (https://creativecommons.org/licenses/by/3.0) license.
Figure 16.4.7
Nephron_Secretion_Reabsorption by OpenStax College on Wikimedia Commons is used under a CC BY 3.0 (https://creativecommons.org/licenses/by/3.0) license.
Figure 16.4.8
Urine by User:Markhamilton at English Wikipedia on Wikimedia Commons is in the public domain (https://en.wikipedia.org/wiki/Public_domain).
Figure 16.4.9
Renin_Angiotensin_System-01 by OpenStax College on Wikimedia Commons is used under a CC BY 3.0 (https://creativecommons.org/licenses/by/3.0) license.
References
Betts, J. G., Young, K.A., Wise, J.A., Johnson, E., Poe, B., Kruse, D.H., Korol, O., Johnson, J.E., Womble, M., DeSaix, P. (2013, June 19). Figure 25.10 Blood flow in the nephron [digital image]. In Anatomy and Physiology (Section 25.3). OpenStax. https://openstax.org/books/anatomy-and-physiology/pages/25-3-gross-anatomy-of-the-kidney
Betts, J. G., Young, K.A., Wise, J.A., Johnson, E., Poe, B., Kruse, D.H., Korol, O., Johnson, J.E., Womble, M., DeSaix, P. (2013, June 19). Figure 25.17 Locations of secretion and reabsorption in the nephron [digital image]. In Anatomy and Physiology (Section 25.6). OpenStax. https://openstax.org/books/anatomy-and-physiology/pages/25-6-tubular-reabsorption
Betts, J. G., Young, K.A., Wise, J.A., Johnson, E., Poe, B., Kruse, D.H., Korol, O., Johnson, J.E., Womble, M., DeSaix, P. (2013, June 19). Figure 26.14 The renin-angiotensin system [digital image]. In Anatomy and Physiology (Section 26.3). OpenStax. https://openstax.org/books/anatomy-and-physiology/pages/26-3-electrolyte-balance
Blausen.com Staff. (2014). Medical gallery of Blausen Medical 2014. WikiJournal of Medicine 1 (2). DOI:10.15347/wjm/2014.010. ISSN 2002-4436
Hamada Abass. (2013). Urine formation. YouTube. https://www.youtube.com/watch?v=es-t8lO1KpA&feature=youtu.be
TED-Ed. (2015, February 9). How do your kidneys work? - Emma Bryce. YouTube. https://www.youtube.com/watch?v=FN3MFhYPWWo&feature=youtu.be
TED-Ed. (2013, March 15). Printing a human kidney - Anthony Atala. YouTube. https://www.youtube.com/watch?v=bX3C201O4MA&feature=youtu.be
Image shows a photograph of a toy poodle peeing on a fire hydrant
As per caption
As per caption
Image shows a diagram of the bladder, the locations where the ureters enter, the internal and external sphincters that keep urine in the bladder and the urethra. There is also an inset pictomicrograph of the layers of the bladder wall with include transitional epithelia and mucose
Created by: CK-12/Adapted by Christine Miller

Oh, the Agony!
Wearing braces can be very uncomfortable, but it is usually worth it. Braces and other orthodontic treatments can re-align the teeth and jaws to improve bite and appearance. Braces can change the position of the teeth and the shape of the jaws because the human body is malleable. Many phenotypic traits — even those that have a strong genetic basis — can be molded by the environment. Changing the phenotype in response to the environment is just one of several ways we respond to environmental stress.
Types of Responses to Environmental Stress
There are four different types of responses that humans may make to cope with environmental stress:
- Adaptation
- Developmental adjustment
- Acclimatization
- Cultural responses
The first three types of responses are biological in nature, and the fourth type is cultural. Only adaptation involves genetic change and occurs at the level of the population or species. The other three responses do not require genetic change, and they occur at the individual level.
Adaptation
An adaptation is a genetically-based trait that has evolved because it helps living things survive and reproduce in a given environment. Adaptations generally evolve in a population over many generations in response to stresses that last for a long period of time. Adaptations come about through natural selection. Those individuals who inherit a trait that confers an advantage in coping with an environmental stress are likely to live longer and reproduce more. As a result, more of their genes pass on to the next generation. Over many generations, the genes and the trait they control become more frequent in the population.
A Classic Example: Hemoglobin S and Malaria
Probably the most frequently-cited example of a genetic adaptation to an environmental stress is sickle cell trait. As you read in the previous section, people with sickle cell trait have one abnormal allele (S) and one normal allele (A) for hemoglobin, the red blood cell protein that carries oxygen in the blood. Sickle cell trait is an adaptation to the environmental stress of malaria, because people with the trait have resistance to this parasitic disease. In areas where malaria is endemic (present year-round), the sickle cell trait and its allele have evolved to relatively high frequencies. It is a classic example of natural selection favoring heterozygotes for a gene with two alleles. This type of selection keeps both alleles at relatively high frequencies in a population.
To Taste or Not to Taste
Another example of an adaptation in humans is the ability to taste bitter compounds. Plants produce a variety of toxic compounds in order to protect themselves from being eaten, and these toxic compounds often have a bitter taste. The ability to taste bitter compounds is thought to have evolved as an adaptation, because it prevented people from eating poisonous plants. Humans have many different genes that code for bitter taste receptors, allowing us to taste a wide variety of bitter compounds.
A harmless bitter compound called phenylthiocarbamide (PTC) is not found naturally in plants, but it is similar to toxic bitter compounds that are found in plants. Humans' ability to taste this harmless substance has been tested in many different populations. In virtually every population studied, there are some people who can taste PTC (called tasters), and some people who cannot taste PTC, (called nontasters). The ratio of tasters to non-tasters varies among populations, but on average, 75 per cent of people can taste PTC and 25 per cent cannot.

Like many scientific discoveries, human variation in PTC-taster status was discovered by chance. Around 1930, a chemist named Arthur Fox was working with powdered PTC in his lab. Some of the powder accidentally blew into the air. Another lab worker noticed that the powdered PTC tasted bitter, but Fox couldn't detect any taste at all. Fox wondered how to explain this difference in PTC-tasting ability. Geneticists soon determined that PTC-taster status is controlled by a single gene with two common alleles, usually represented by the letters T and t. The T allele encodes a chemical receptor protein (found in taste buds on the tongue, as illustrated in Figure 6.4.2) that can strongly bind to PTC. The other allele, t, encodes a version of the receptor protein that cannot bind as strongly to PTC. The particular combination of these two alleles that a person inherits determines whether the person finds PTC to taste very bitter (TT), somewhat bitter (Tt), or not bitter at all (tt).
If the ability to taste bitter compounds is advantageous, why does every human population studied contain a significant percentage of people who are nontasters? Why has the nontasting allele been preserved in human populations at all? Some scientists hypothesize that the nontaster allele actually confers the ability to taste some other, yet-to-be identified, bitter compound in plants. People who inherit both alleles would presumably be able to taste a wider range of bitter compounds, so they would have the greatest ability to avoid plant toxins. In other words, the heterozygote genotype for the taster gene would be the most fit and favored by natural selection.
Most people no longer have to worry whether the plants they eat contain toxins. The produce you grow in your garden or buy at the supermarket consists of known varieties that are safe to eat. However, natural selection may still be at work in human populations for the PTC-taster gene, because PTC tasters may be more sensitive than nontasters to bitter compounds in tobacco and vegetables in the cabbage family (that is, cruciferous vegetables, such as the broccoli, cauliflower, and cabbage pictured in Figure 6.4.3).
- People who find PTC to taste very bitter are less likely to smoke tobacco, presumably because tobacco smoke has a stronger bitter taste to these individuals. In this case, selection would favor taster genotypes, because tasters would be more likely to avoid smoking and its serious health risks.
- Strong tasters find cruciferous vegetables to taste bitter. As a result, they may avoid eating these vegetables (and perhaps other foods, as well), presumably resulting in a diet that is less varied and nutritious. In this scenario, natural selection might work against taster genotypes.
Figure 6.4.3 Cruciferous vegetables.
Developmental Adjustment
It takes a relatively long time for genetic change in response to environmental stress to produce a population with adaptations. Fortunately, we can adjust to some environmental stresses more quickly by changing in nongenetic ways. One type of nongenetic response to stress is developmental adjustment. This refers to phenotypic change that occurs during development in infancy or childhood, and that may persist into adulthood. This type of change may be irreversible by adulthood.
Phenotypic Plasticity
Developmental adjustment is possible because humans have a high degree of phenotypic plasticity, which is the ability to alter the phenotype in response to changes in the environment. Phenotypic plasticity allows us to respond to changes that occur within our lifetime, and it is particularly important for species (like our own) that have a long generation time. With long generations, evolution of genetic adaptations may occur too slowly to keep up with changing environmental stresses.
Developmental Adjustment and Cultural Practices
Developmental adjustment may be the result of naturally occurring environmental stresses or cultural practices, including medical or dental treatments. Like our example at the beginning of this section, using braces to change the shape of the jaw and the position of the teeth is an example of a dental practice that brings about a developmental adjustment. Another example of developmental adjustment is the use of a back brace to treat scoliosis (see images in Figure 6.4.4). Scoliosis is an abnormal curvature from side to side in the spine. If the problem is not too severe, a brace, if worn correctly, should prevent the curvature from worsening as a child grows, although it cannot straighten a curve that is already present. Surgery may be required to do that.
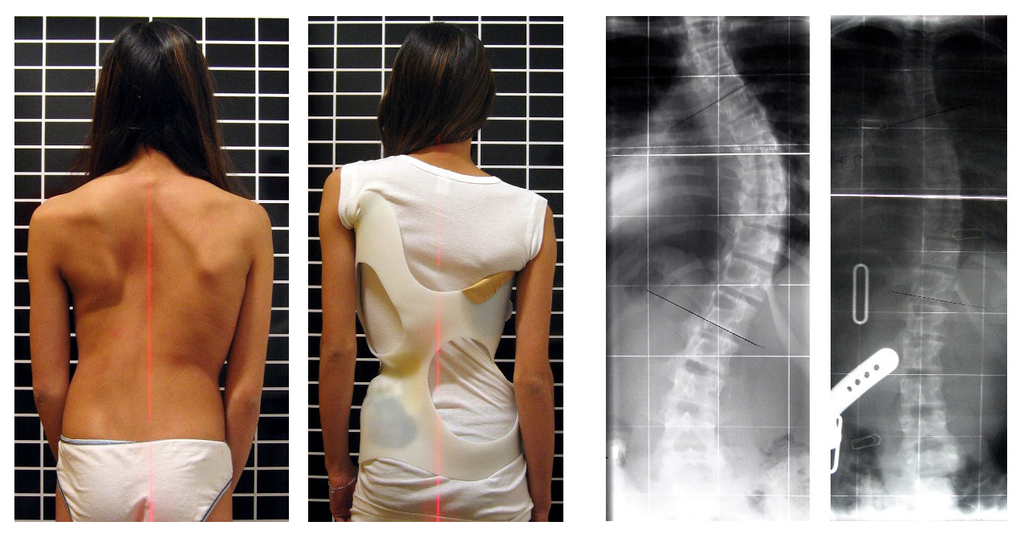
Developmental Adjustment and Nutritional Stress
An important example of developmental adjustment that results from a naturally occurring environmental stress is the cessation of physical growth that occurs in children who are under nutritional stress. Children who lack adequate food to fuel both growth and basic metabolic processes are likely to slow down in their growth rate — or even to stop growing entirely. Shunting all available calories and nutrients into essential life functions may keep the child alive at the expense of increasing body size.
Table 6.4.1 shows the effects of inadequate diet on children's' growth in several countries worldwide. For each country, the table gives the prevalence of stunting in children under the age of five. Children are considered stunted if their height is at least two standard deviations below the median height for their age in an international reference population.
Table 6.4.1
Percentage of Stunting in Young Children in Selected Countries (2011-2015)
| Percentage of Stunting in Young Children in Selected Countries (2011-2015) | |
| Country | Per cent of Children Under Age 5 with Stunting |
| United States | 2.1 |
| Turkey | 9.5 |
| Mexico | 13.6 |
| Thailand | 16.3 |
| Iraq | 22.6 |
| Philippines | 33.6 |
| Pakistan | 45.0 |
| Papua New Guinea | 49.5 |
After a growth slow-down occurs and if adequate food becomes available, a child may be able to make up the loss of growth. If food is plentiful, the child may grow more rapidly than normal until the original, genetically-determined growth trajectory is reached. If the inadequate diet persists, however, the failure of growth may become chronic, and the child may never reach his or her full potential adult size.
Phenotypic plasticity of body size in response to dietary change has been observed in successive generations within populations. For example, children in Japan were taller, on average, in each successive generation after the end of World War II. Boys aged 14-15 years old in 1986 were an average of about 18 cm (7 in.) taller than boys of the same age in 1959, a generation earlier. This is a highly significant difference, and it occurred too quickly to be accounted for by genetic change. Instead, the increase in height is a developmental adjustment, thought to be largely attributable to changes in the Japanese diet since World War II. During this period, there was an increase in the amount of animal protein and fat, as well as in the total calories consumed.
Acclimatization
Other responses to environmental stress are reversible and not permanent, whether they occur in childhood or adulthood. The development of reversible changes to environmental stress is called acclimatization. Acclimatization generally develops over a relatively short period of time. It may take just a few days or weeks to attain a maximum response to a stress. When the stress is no longer present, the acclimatized state declines, and the body returns to its normal baseline state. Generally, the shorter the time for acclimatization to occur, the more quickly the condition is reversed when the environmental stress is removed.
Acclimatization to UV Light
A common example of acclimatization is tanning of the skin (see Figure 6.4.5). This occurs in many people in response to exposure to ultraviolet radiation from the sun. Special pigment cells in the skin, called melanocytes, produce more of the brown pigment melanin when exposed to sunlight. The melanin collects near the surface of the skin where it absorbs UV radiation so it cannot penetrate and potentially damage deeper skin structures. Tanning is a reversible change in the phenotype that helps the body deal temporarily with the environmental stress of high levels of UV radiation. When the skin is no longer exposed to the sun’s rays, the tan fades, generally over a period of a few weeks or months.
Figure 6.4.5 Tanning of the skin occurs in many people in response to exposure to ultraviolet radiation from the sun.
Acclimatization to Heat
Another common example of acclimatization occurs in response to heat. Changes that occur with heat acclimatization include increased sweat output and earlier onset of sweat production, which helps the body stay cool because evaporation of sweat takes heat from the body’s surface in a process called evaporative cooling. It generally takes a couple of weeks for maximum heat acclimatization to come about by gradually working out harder and longer at high air temperatures. The changes that occur with acclimatization just as quickly subside when the body is no longer exposed to excessive heat.
Acclimatization to High Altitude

Short term acclimatization to high altitude occurs as a response to low levels of oxygen in the blood. This reduced level of oxygen is detected by carotid bodies, which will trigger in increase in breathing and heart rate. Over a period of weeks the body will compensate by increasing red blood cell production, thereby improving the oxygen-carrying capacity of the blood. This is why mountaineers wishing to climb to the peak of Mount Everest must complete the full climb in portions; it is recommended that climbers spend 2-3 days acclimatizing for every 600 metres of elevation increase. In addition, the higher to altitude, the longer it make take to acclimatize; climbers are advised to spend 4-5 days acclimatizing at base camp (whether the base camp in Nepal or China) before completing the final leg of the climb to the peak. The concentration of red blood cells gradually decreases to normal levels once a climber returns to their normal elevation.
Cultural Responses
More than any other species, humans respond to environmental stresses with learned behaviors and technology. These cultural responses allow us to change our environments to control stresses, rather than changing our bodies genetically or physiologically to cope with the stresses. Even archaic humans responded to some environmental stresses in this way. For example, Neanderthals used shelters, fires, and animal hides as clothing to stay warm in the cold climate in Europe during the last ice age. Today, we use more sophisticated technologies to stay warm in cold climates while retaining our essentially tropical-animal anatomy and physiology. We also use technology (such as furnaces and air conditioners) to avoid temperature stress and stay comfortable in hot or cold climates.
6.4 Summary
- Humans may respond to environmental stress in four different ways: adaptation, developmental adjustment, acclimatization, and cultural responses.
- An adaptation is a genetically based trait that has evolved because it helps living things survive and reproduce in a given environment. Adaptations evolve by natural selection in populations over a relatively long period to time. Examples of adaptations include sickle cell trait as an adaptation to the stress of endemic malaria and the ability to taste bitter compounds as an adaptation to the stress of bitter-tasting toxins in plants.
- A developmental adjustment is a non-genetic response to stress that occurs during infancy or childhood, and that may persist into adulthood. This type of change may be irreversible. Developmental adjustment is possible because humans have a high degree of phenotypic plasticity. It may be the result of environmental stresses (such as inadequate food), which may stunt growth, or cultural practices (such as orthodontic treatments), which re-align the teeth and jaws.
- Acclimatization is the development of reversible changes to environmental stress that develop over a relatively short period of time. The changes revert to the normal baseline state after the stress is removed. Examples of acclimatization include tanning of the skin and physiological changes (such as increased sweating) that occur with heat acclimatization.
- More than any other species, humans respond to environmental stress with learned behaviors and technology, which are cultural responses. These responses allow us to change our environment to control stress, rather than changing our bodies genetically or physiologically to cope with stress. Examples include using shelter, fire, and clothing to cope with a cold climate.
6.4 Review Questions
- List four different types of responses that humans may make to cope with environmental stress.
- Define adaptation.
-
- Explain how natural selection may have resulted in most human populations having people who can and people who cannot taste PTC.
- What is a developmental adjustment?
- Define phenotypic plasticity.
- Explain why phenotypic plasticity may be particularly important in a species with a long generation time.
- Why may stunting of growth occur in children who have an inadequate diet? Why is stunting preferable to the alternative?
- What is acclimatization?
- How does acclimatization to heat come about, and what are two physiological changes that occur in heat acclimatization?
- Give an example of a cultural response to heat stress.
- Which is more likely to be reversible — a change due to acclimatization, or a change due to developmental adjustment? Explain your answer.
6.4 Explore More
https://www.youtube.com/watch?v=upp9-w6GPhU
Could we survive prolonged space travel? - Lisa Nip, TED-Ed, 2016.
https://www.youtube.com/watch?v=hRnrIpUMyZQ&t=182s
How this disease changes the shape of your cells - Amber M. Yates, TED-Ed, 2019.
Attributions
Figure 6.4.1
Free_Awesome_Girl_With_Braces_Close_Up by D. Sharon Pruitt from Hill Air Force Base, Utah, USA on Wikimedia Commons is used under a CC BY 2.0 (https://creativecommons.org/licenses/by/2.0/deed.en) license.
Figure 6.4.2
Tongue by Mahdiabbasinv on Wikimedia Commons is used under a CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0/deed.en) license.
Figure 6.4.3
- White cauliflower on brown wooden chopping board by Louis Hansel @shotsoflouis on Unsplash is used under the Unsplash License (https://unsplash.com/license).
- Broccoli on wooden chopping board by Louis Hansel @shotsoflouis on Unsplash is used under the Unsplash License (https://unsplash.com/license).
- Green cabbage close up by Craig Dimmick on Unsplash is used under the Unsplash License (https://unsplash.com/license).
- Cabbage hybrid/ brussel sprouts by Solstice Hannan on Unsplash is used under the Unsplash License (https://unsplash.com/license).
- Kale by Laura Johnston on Unsplash is used under the Unsplash License (https://unsplash.com/license).
- Tiny bok choy at the Asian market by Jodie Morgan on Unsplash is used under the Unsplash License (https://unsplash.com/license).
Figure 6.4.4
Scoliosis_patient_in_cheneau_brace_correcting_from_56_to_27_deg by Weiss H.R. from Scoliosis Journal/BioMed Central Ltd. on Wikimedia Commons is used under a CC BY 2.0 (https://creativecommons.org/licenses/by/2.0) license.
Figure 6.4.5
- Tan Lines by k.steudel on Flickr is used under a CC BY 2.0 (https://creativecommons.org/licenses/by/2.0/) license.
- Twin tan lines (all sizes) by Quinn Dombrowski on Flickr is used under a CC BY-SA 2.0 (https://creativecommons.org/licenses/by-sa/2.0/) license.
- Wedding ring tan line by Quinn Dombrowski on Flickr is used under a CC BY-SA 2.0 (https://creativecommons.org/licenses/by-sa/2.0/) license.
- Tan by Evil Erin on Flickr is used under a CC BY 2.0 (https://creativecommons.org/licenses/by/2.0/) license.
Figure 6.4.6
Nepalese base camp by Mark Horrell on Flickr is used under a CC BY-NC-SA 2.0 (https://creativecommons.org/licenses/by-nc-sa/2.0/) license.
References
TED-Ed. (2016, October 4). Could we survive prolonged space travel? - Lisa Nip. YouTube. https://www.youtube.com/watch?v=upp9-w6GPhU&feature=youtu.be
TED-Ed. (2019, May 6). How this disease changes the shape of your cells - Amber M. Yates. YouTube. https://www.youtube.com/watch?v=hRnrIpUMyZQ&feature=youtu.be
Weiss, H. (2007). Is there a body of evidence for the treatment of patients with Adolescent Idiopathic Scoliosis (AIS)? [Figure 2 - digital photograph], Scoliosis, 2(19). https://doi.org/10.1186/1748-7161-2-19
Image shows a diagram of the location of the liver (large organ which sits below the diaphragm), the gallbladder (small sac-like organ which is tucked under the liver) and the pancreas (long flat organ which sits in front of and just under the stomach).
The largest part of the brain that controls conscious functions such as reasoning and sight.
The highly folded, thin outer layer of the cerebrum where most information processing in the brain takes place.
Created by CK-12 Foundation/Adapted by Christine Miller

Communicating with Urine
Why do dogs pee on fire hydrants? Besides “having to go,” they are marking their territory with chemicals in their urine called pheromones. It’s a form of communication, in which they are “saying” with odors that the yard is theirs and other dogs should stay away. In addition to fire hydrants, dogs may urinate on fence posts, trees, car tires, and many other objects. Urination in dogs, as in people, is usually a voluntary process controlled by the brain. The process of forming urine — which occurs in the kidneys — occurs constantly, and is not under voluntary control. What happens to all the urine that forms in the kidneys? It passes from the kidneys through the other organs of the urinary system, starting with the ureters.
Ureters
As shown in Figure 16.5.2, ureters are tube-like structures that connect the kidneys with the urinary bladder. They are paired structures, with one ureter for each kidney. In adults, ureters are between 25 and 30 cm (about 10–12 in) long and about 3 to 4 mm in diameter.
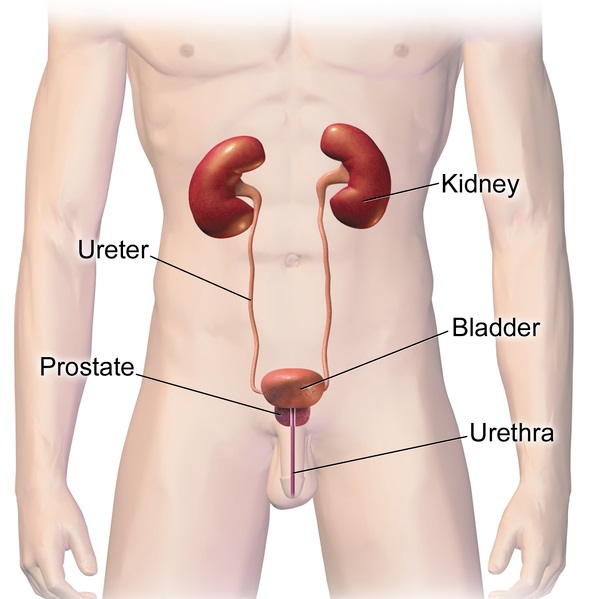
Each ureter arises in the pelvis of a kidney (the renal pelvis in Figure 16.5.3). It then passes down the side of the kidney, and finally enters the back of the bladder. At the entrance to the bladder, the ureters have sphincters that prevent the backflow of urine.
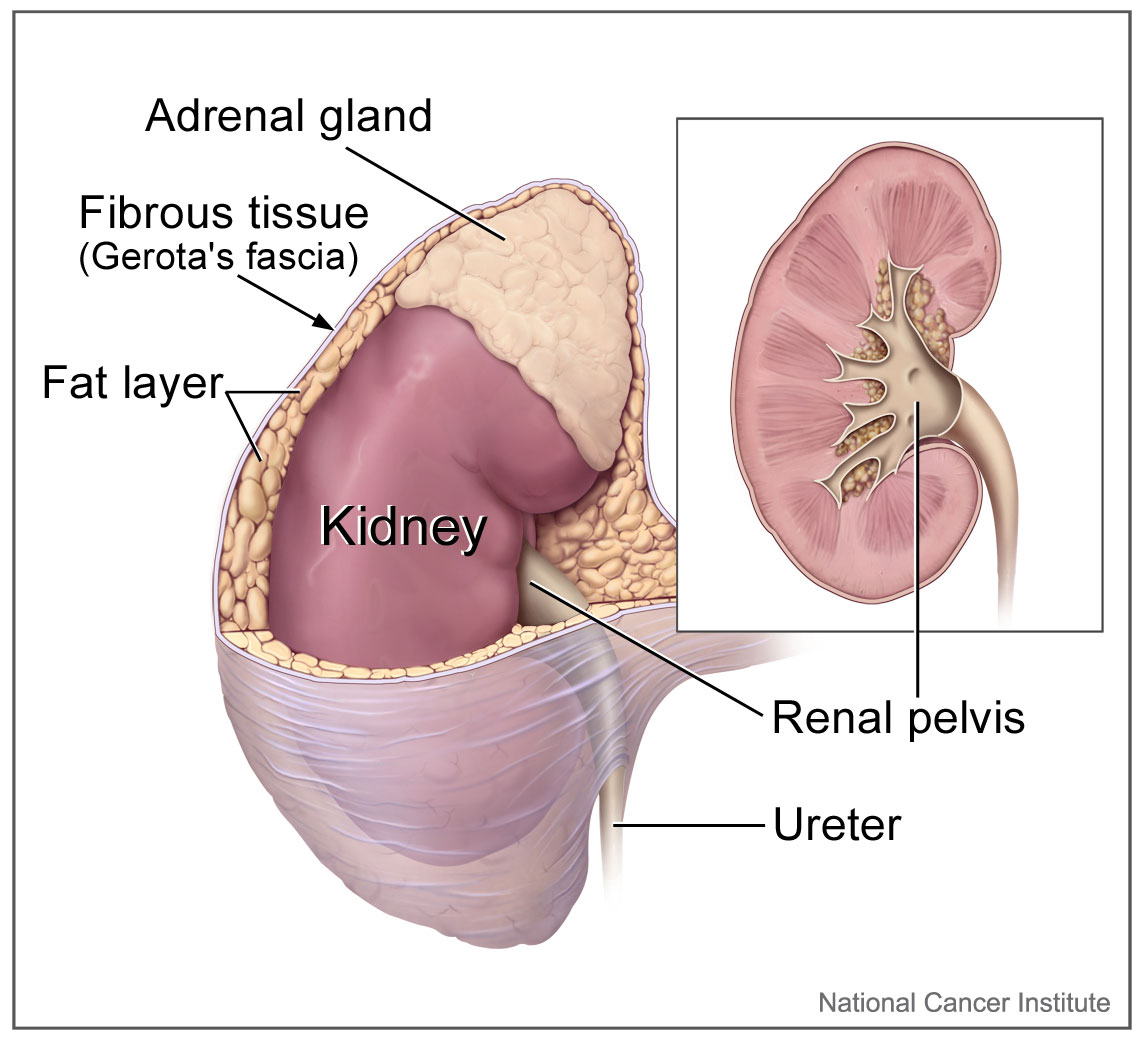
The walls of the ureters are composed of multiple layers of different types of tissues. The innermost layer is a special type of epithelium, called transitional epithelium. Unlike the epithelium lining most organs, transitional epithelium is capable of stretching and does not produce mucus. It lines much of the urinary system, including the renal pelvis, bladder, and much of the urethra, in addition to the ureters. Transitional epithelium allows these organs to stretch and expand as they fill with urine or allow urine to pass through. The next layer of the ureter walls is made up of loose connective tissue containing elastic fibres, nerves, and blood and lymphatic vessels. After this layer are two layers of smooth muscles, an inner circular layer, and an outer longitudinal layer. The smooth muscle layers can contract in waves of peristalsis to propel urine down the ureters from the kidneys to the urinary bladder. The outermost layer of the ureter walls consists of fibrous tissue.
Urinary Bladder
The urinary bladder is a hollow, muscular, and stretchy organ that rests on the pelvic floor. It collects and stores urine from the kidneys before the urine is eliminated through urination. As shown in Figure 16.5.4, urine enters the urinary bladder from the ureters through two ureteral openings on either side of the back wall of the bladder. Urine leaves the bladder through a sphincter called the internal urethral sphincter. When the sphincter relaxes and opens, it allows urine to flow out of the bladder and into the urethra.
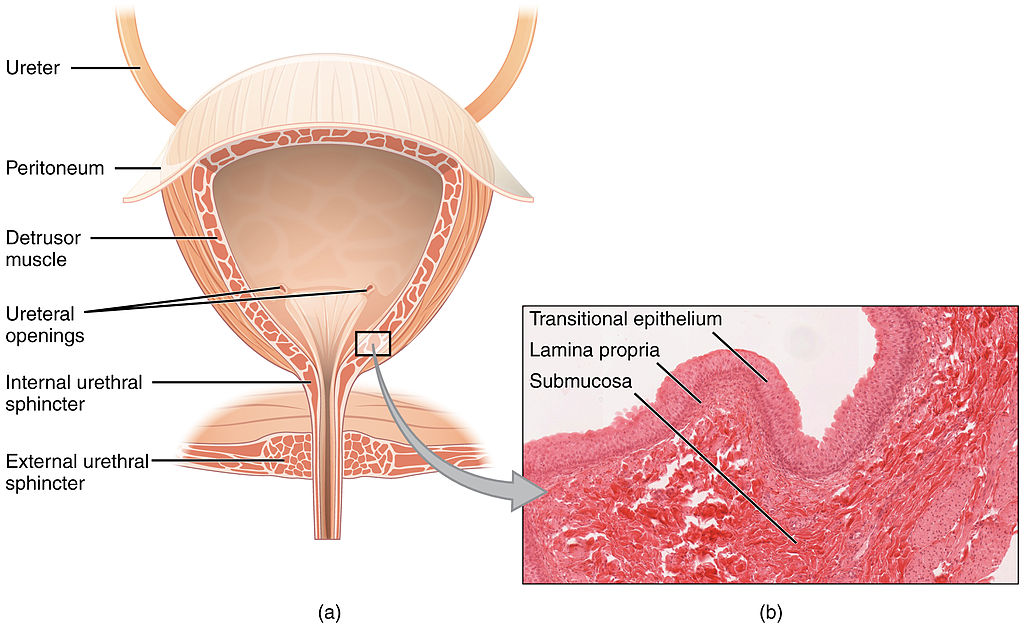
Like the ureters, the bladder is lined with transitional epithelium, which can flatten out and stretch as needed as the bladder fills with urine. The next layer (lamina propria) is a layer of loose connective tissue, nerves, and blood and lymphatic vessels. This is followed by a submucosa layer, which connects the lining of the bladder with the detrusor muscle in the walls of the bladder. The outer covering of the bladder is peritoneum, which is a smooth layer of epithelial cells that lines the abdominal cavity and covers most abdominal organs.
The detrusor muscle in the wall of the bladder is made of smooth muscle fibres controlled by both the autonomic and somatic nervous systems. As the bladder fills, the detrusor muscle automatically relaxes to allow it to hold more urine. When the bladder is about half full, the stretching of the walls triggers the sensation of needing to urinate. When the individual is ready to void, conscious nervous signals cause the detrusor muscle to contract, and the internal urethral sphincter to relax and open. As a result, urine is forcefully expelled out of the bladder and into the urethra.
Urethra
The urethra is a tube that connects the urinary bladder to the external urethral orifice, which is the opening of the urethra on the surface of the body. As shown in Figure 16.5.5, the urethra in males travels through the penis, so it is much longer than the urethra in females. In males, the urethra averages about 20 cm (about 7.8 in) long, whereas in females, it averages only about 4.8 cm (about 1.9 in) long. In males, the urethra carries semen (as well as urine), but in females, it carries only urine. In addition, in males, the urethra passes through the prostate gland (part of the reproductive system) which is absent in women.
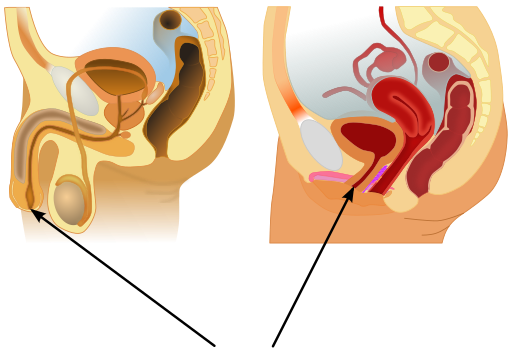
Like the ureters and bladder, the proximal (closer to the bladder) two-thirds of the urethra are lined with transitional epithelium. The distal (farther from the bladder) third of the urethra is lined with mucus-secreting epithelium. The mucus helps protect the epithelium from urine, which is corrosive. Below the epithelium is loose connective tissue, and below that are layers of smooth muscle that are continuous with the muscle layers of the urinary bladder. When the bladder contracts to forcefully expel urine, the smooth muscle of the urethra relaxes to allow the urine to pass through.
In order for urine to leave the body through the external urethral orifice, the external urethral sphincter must relax and open. This sphincter is a striated muscle that is controlled by the somatic nervous system, so it is under conscious, voluntary control in most people (exceptions are infants, some elderly people, and patients with certain injuries or disorders). The muscle can be held in a contracted state and hold in the urine until the person is ready to urinate. Following urination, the smooth muscle lining the urethra automatically contracts to re-establish muscle tone, and the individual consciously contracts the external urethral sphincter to close the external urethral opening.
16.5 Summary
- Ureters are tube-like structures that connect the kidneys with the urinary bladder. Each ureter arises at the renal pelvis of a kidney and travels down through the abdomen to the urinary bladder. The walls of the ureter contain smooth muscle that can contract to push urine through the ureter by peristalsis. The walls are lined with transitional epithelium that can expand and stretch.
- The urinary bladder is a hollow, muscular organ that rests on the pelvic floor. It is also lined with transitional epithelium. The function of the bladder is to collect and store urine from the kidneys before the urine is eliminated through urination. Filling of the bladder triggers the sensation of needing to urinate. When a conscious decision to urinate is made, the detrusor muscle in the bladder wall contracts and forces urine out of the bladder and into the urethra.
- The urethra is a tube that connects the urinary bladder to the external urethral orifice. Somatic nerves control the sphincter at the distal end of the urethra. This allows the opening of the sphincter for urination to be under voluntary control.
16.5 Review Questions
- What are ureters? Describe the location of the ureters relative to other urinary tract organs.
- Identify layers in the walls of a ureter. How do they contribute to the ureter’s function?
- Describe the urinary bladder. What is the function of the urinary bladder?
-
- How does the nervous system control the urinary bladder?
- What is the urethra?
- How does the nervous system control urination?
- Identify the sphincters that are located along the pathway from the ureters to the external urethral orifice.
- What are two differences between the male and female urethra?
- When the bladder muscle contracts, the smooth muscle in the walls of the urethra _________ .
16.5 Explore More
https://youtu.be/2Brajdazp1o
The taboo secret to better health | Molly Winter, TED. 2016.
https://youtu.be/dg4_deyHLvQ
What Happens When You Hold Your Pee? SciShow, 2016.
Attributions
Figure 16.5.1
Cliche by Jackie on Wikimedia Common s is used under a CC BY 2.0 (https://creativecommons.org/licenses/by/2.0) license.
Figure 16.5.2
Urinary System Male by BruceBlaus on Wikimedia Commons is used under a CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0) license.
Figure 16.5.3
Adrenal glands on Kidney by NCI Public Domain by Alan Hoofring (Illustrator) /National Cancer Institute (photo ID 4355) on Wikimedia Commons is in the public domain (https://en.wikipedia.org/wiki/Public_domain).
Figure 16.5.4
2605_The_Bladder by OpenStax College on Wikimedia Commons is used under a CC BY 3.0 (https://creativecommons.org/licenses/by/3.0) license. (Micrograph originally provided by the Regents of the University of Michigan Medical School © 2012.)
Figure 16.5.5
512px-Male_and_female_urethral_openings.svg by andrybak (derivative work) on Wikimedia Commons is used under a CC BY-SA 3.0 (https://creativecommons.org/licenses/by-sa/3.0) license. (Original: Male anatomy blank.svg: alt.sex FAQ, derivative work: Tsaitgaist Female anatomy with g-spot.svg: Tsaitgaist.)
References
Betts, J. G., Young, K.A., Wise, J.A., Johnson, E., Poe, B., Kruse, D.H., Korol, O., Johnson, J.E., Womble, M., DeSaix, P. (2013, June 19). Figure 25.4 Bladder (a) Anterior cross section of the bladder. (b) The detrusor muscle of the bladder (source: monkey tissue) LM × 448 [digital image]. In Anatomy and Physiology (Section 7.3). OpenStax. https://openstax.org/books/anatomy-and-physiology/pages/25-2-gross-anatomy-of-urine-transport
SciShow. (2016, January 22). What happens when you hold your pee? YouTube. https://www.youtube.com/watch?v=dg4_deyHLvQ&feature=youtu.be
TED. (2016, September 2). The taboo secret to better health | Molly Winter. YouTube. https://www.youtube.com/watch?v=2Brajdazp1o&feature=youtu.be
Created by CK-12 Foundation/Adapted by Christine Miller

Communicating with Urine
Why do dogs pee on fire hydrants? Besides “having to go,” they are marking their territory with chemicals in their urine called pheromones. It’s a form of communication, in which they are “saying” with odors that the yard is theirs and other dogs should stay away. In addition to fire hydrants, dogs may urinate on fence posts, trees, car tires, and many other objects. Urination in dogs, as in people, is usually a voluntary process controlled by the brain. The process of forming urine — which occurs in the kidneys — occurs constantly, and is not under voluntary control. What happens to all the urine that forms in the kidneys? It passes from the kidneys through the other organs of the urinary system, starting with the ureters.
Ureters
As shown in Figure 16.5.2, ureters are tube-like structures that connect the kidneys with the urinary bladder. They are paired structures, with one ureter for each kidney. In adults, ureters are between 25 and 30 cm (about 10–12 in) long and about 3 to 4 mm in diameter.
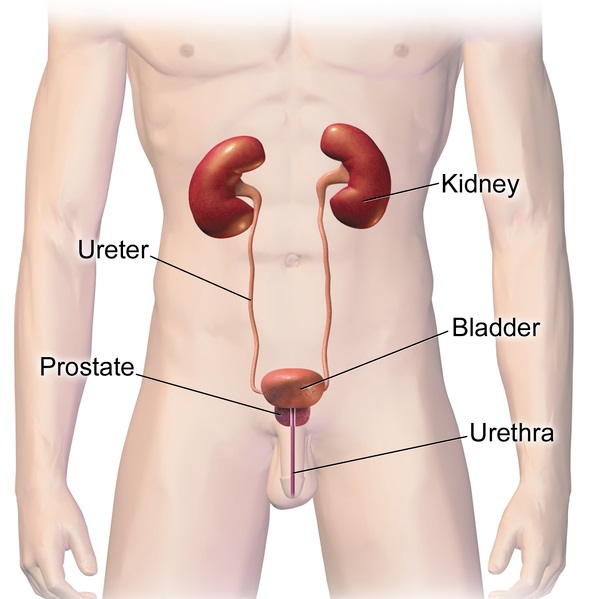
Each ureter arises in the pelvis of a kidney (the renal pelvis in Figure 16.5.3). It then passes down the side of the kidney, and finally enters the back of the bladder. At the entrance to the bladder, the ureters have sphincters that prevent the backflow of urine.
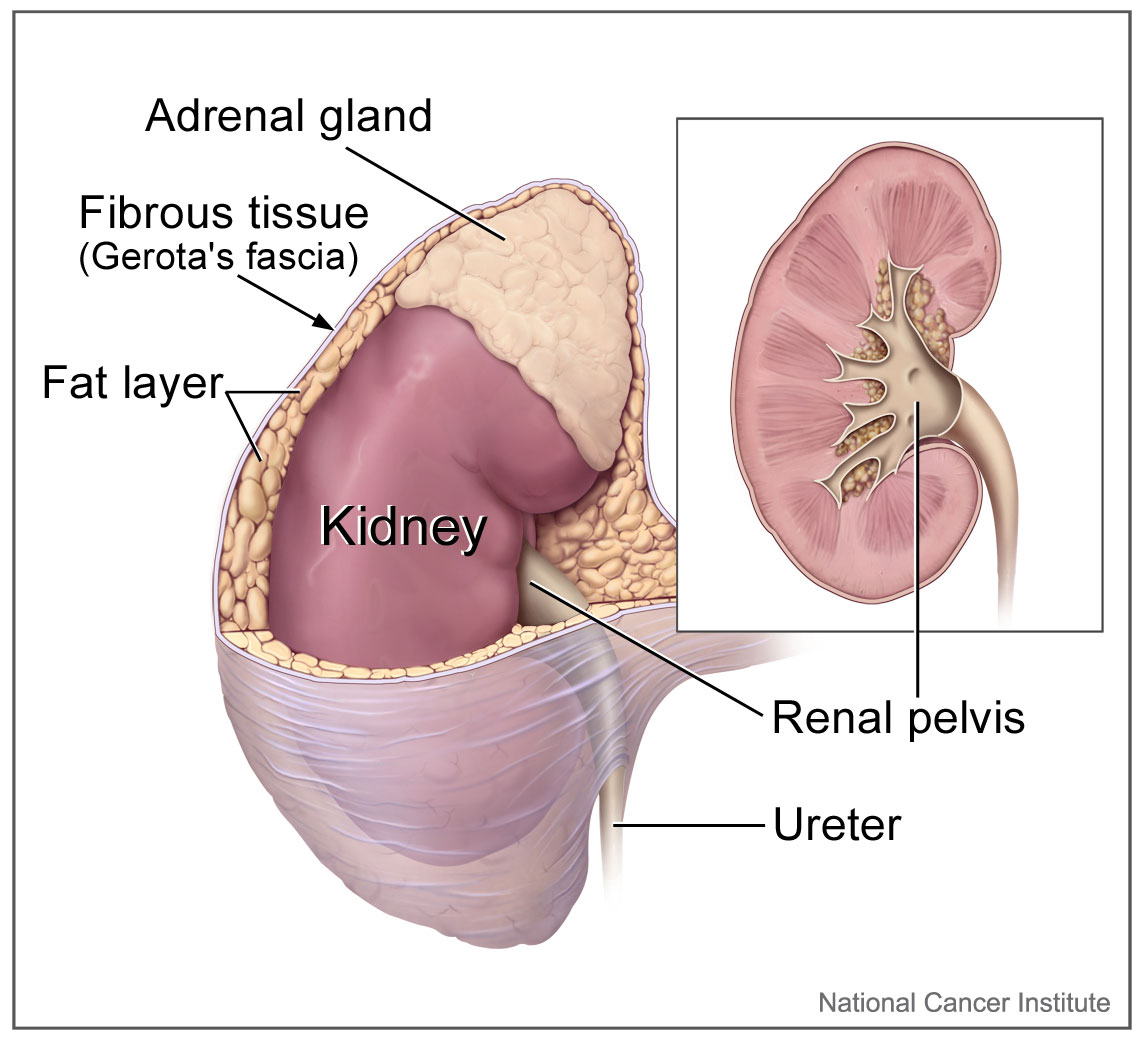
The walls of the ureters are composed of multiple layers of different types of tissues. The innermost layer is a special type of epithelium, called transitional epithelium. Unlike the epithelium lining most organs, transitional epithelium is capable of stretching and does not produce mucus. It lines much of the urinary system, including the renal pelvis, bladder, and much of the urethra, in addition to the ureters. Transitional epithelium allows these organs to stretch and expand as they fill with urine or allow urine to pass through. The next layer of the ureter walls is made up of loose connective tissue containing elastic fibres, nerves, and blood and lymphatic vessels. After this layer are two layers of smooth muscles, an inner circular layer, and an outer longitudinal layer. The smooth muscle layers can contract in waves of peristalsis to propel urine down the ureters from the kidneys to the urinary bladder. The outermost layer of the ureter walls consists of fibrous tissue.
Urinary Bladder
The urinary bladder is a hollow, muscular, and stretchy organ that rests on the pelvic floor. It collects and stores urine from the kidneys before the urine is eliminated through urination. As shown in Figure 16.5.4, urine enters the urinary bladder from the ureters through two ureteral openings on either side of the back wall of the bladder. Urine leaves the bladder through a sphincter called the internal urethral sphincter. When the sphincter relaxes and opens, it allows urine to flow out of the bladder and into the urethra.
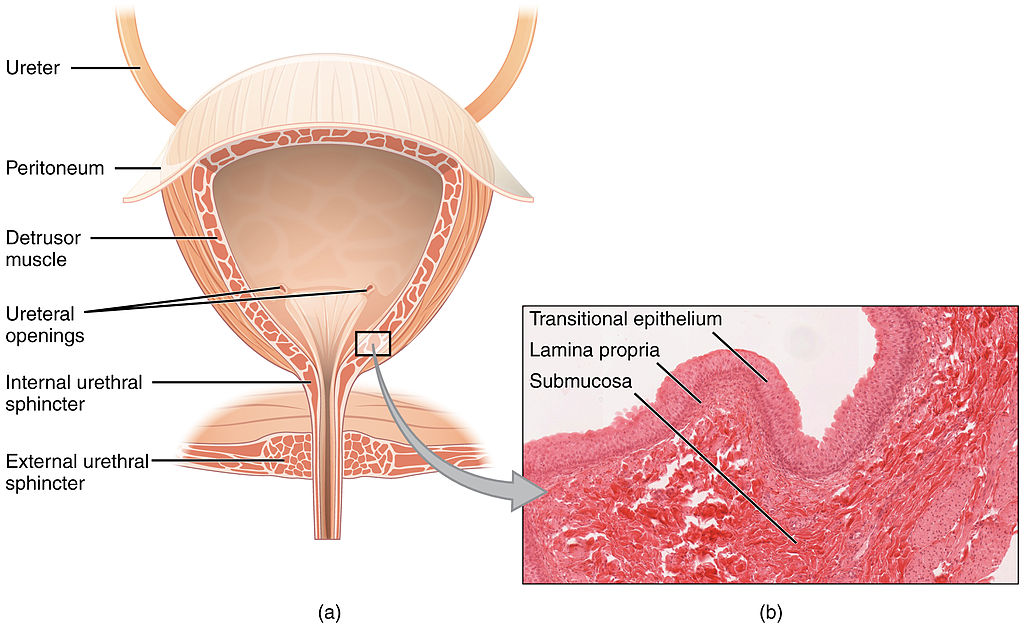
Like the ureters, the bladder is lined with transitional epithelium, which can flatten out and stretch as needed as the bladder fills with urine. The next layer (lamina propria) is a layer of loose connective tissue, nerves, and blood and lymphatic vessels. This is followed by a submucosa layer, which connects the lining of the bladder with the detrusor muscle in the walls of the bladder. The outer covering of the bladder is peritoneum, which is a smooth layer of epithelial cells that lines the abdominal cavity and covers most abdominal organs.
The detrusor muscle in the wall of the bladder is made of smooth muscle fibres controlled by both the autonomic and somatic nervous systems. As the bladder fills, the detrusor muscle automatically relaxes to allow it to hold more urine. When the bladder is about half full, the stretching of the walls triggers the sensation of needing to urinate. When the individual is ready to void, conscious nervous signals cause the detrusor muscle to contract, and the internal urethral sphincter to relax and open. As a result, urine is forcefully expelled out of the bladder and into the urethra.
Urethra
The urethra is a tube that connects the urinary bladder to the external urethral orifice, which is the opening of the urethra on the surface of the body. As shown in Figure 16.5.5, the urethra in males travels through the penis, so it is much longer than the urethra in females. In males, the urethra averages about 20 cm (about 7.8 in) long, whereas in females, it averages only about 4.8 cm (about 1.9 in) long. In males, the urethra carries semen (as well as urine), but in females, it carries only urine. In addition, in males, the urethra passes through the prostate gland (part of the reproductive system) which is absent in women.
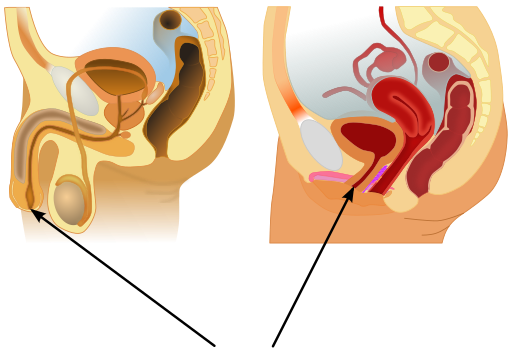
Like the ureters and bladder, the proximal (closer to the bladder) two-thirds of the urethra are lined with transitional epithelium. The distal (farther from the bladder) third of the urethra is lined with mucus-secreting epithelium. The mucus helps protect the epithelium from urine, which is corrosive. Below the epithelium is loose connective tissue, and below that are layers of smooth muscle that are continuous with the muscle layers of the urinary bladder. When the bladder contracts to forcefully expel urine, the smooth muscle of the urethra relaxes to allow the urine to pass through.
In order for urine to leave the body through the external urethral orifice, the external urethral sphincter must relax and open. This sphincter is a striated muscle that is controlled by the somatic nervous system, so it is under conscious, voluntary control in most people (exceptions are infants, some elderly people, and patients with certain injuries or disorders). The muscle can be held in a contracted state and hold in the urine until the person is ready to urinate. Following urination, the smooth muscle lining the urethra automatically contracts to re-establish muscle tone, and the individual consciously contracts the external urethral sphincter to close the external urethral opening.
16.5 Summary
- Ureters are tube-like structures that connect the kidneys with the urinary bladder. Each ureter arises at the renal pelvis of a kidney and travels down through the abdomen to the urinary bladder. The walls of the ureter contain smooth muscle that can contract to push urine through the ureter by peristalsis. The walls are lined with transitional epithelium that can expand and stretch.
- The urinary bladder is a hollow, muscular organ that rests on the pelvic floor. It is also lined with transitional epithelium. The function of the bladder is to collect and store urine from the kidneys before the urine is eliminated through urination. Filling of the bladder triggers the sensation of needing to urinate. When a conscious decision to urinate is made, the detrusor muscle in the bladder wall contracts and forces urine out of the bladder and into the urethra.
- The urethra is a tube that connects the urinary bladder to the external urethral orifice. Somatic nerves control the sphincter at the distal end of the urethra. This allows the opening of the sphincter for urination to be under voluntary control.
16.5 Review Questions
- What are ureters? Describe the location of the ureters relative to other urinary tract organs.
- Identify layers in the walls of a ureter. How do they contribute to the ureter’s function?
- Describe the urinary bladder. What is the function of the urinary bladder?
-
- How does the nervous system control the urinary bladder?
- What is the urethra?
- How does the nervous system control urination?
- Identify the sphincters that are located along the pathway from the ureters to the external urethral orifice.
- What are two differences between the male and female urethra?
- When the bladder muscle contracts, the smooth muscle in the walls of the urethra _________ .
16.5 Explore More
https://youtu.be/2Brajdazp1o
The taboo secret to better health | Molly Winter, TED. 2016.
https://youtu.be/dg4_deyHLvQ
What Happens When You Hold Your Pee? SciShow, 2016.
Attributions
Figure 16.5.1
Cliche by Jackie on Wikimedia Common s is used under a CC BY 2.0 (https://creativecommons.org/licenses/by/2.0) license.
Figure 16.5.2
Urinary System Male by BruceBlaus on Wikimedia Commons is used under a CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0) license.
Figure 16.5.3
Adrenal glands on Kidney by NCI Public Domain by Alan Hoofring (Illustrator) /National Cancer Institute (photo ID 4355) on Wikimedia Commons is in the public domain (https://en.wikipedia.org/wiki/Public_domain).
Figure 16.5.4
2605_The_Bladder by OpenStax College on Wikimedia Commons is used under a CC BY 3.0 (https://creativecommons.org/licenses/by/3.0) license. (Micrograph originally provided by the Regents of the University of Michigan Medical School © 2012.)
Figure 16.5.5
512px-Male_and_female_urethral_openings.svg by andrybak (derivative work) on Wikimedia Commons is used under a CC BY-SA 3.0 (https://creativecommons.org/licenses/by-sa/3.0) license. (Original: Male anatomy blank.svg: alt.sex FAQ, derivative work: Tsaitgaist Female anatomy with g-spot.svg: Tsaitgaist.)
References
Betts, J. G., Young, K.A., Wise, J.A., Johnson, E., Poe, B., Kruse, D.H., Korol, O., Johnson, J.E., Womble, M., DeSaix, P. (2013, June 19). Figure 25.4 Bladder (a) Anterior cross section of the bladder. (b) The detrusor muscle of the bladder (source: monkey tissue) LM × 448 [digital image]. In Anatomy and Physiology (Section 7.3). OpenStax. https://openstax.org/books/anatomy-and-physiology/pages/25-2-gross-anatomy-of-urine-transport
SciShow. (2016, January 22). What happens when you hold your pee? YouTube. https://www.youtube.com/watch?v=dg4_deyHLvQ&feature=youtu.be
TED. (2016, September 2). The taboo secret to better health | Molly Winter. YouTube. https://www.youtube.com/watch?v=2Brajdazp1o&feature=youtu.be
Image shows a diagram of the kidney with several kidney stones, which have accumulated in the renal pelvis and are blocking the exit to the ureter.
A special sensory organ that collects and amplifies sound waves and information on body position and transforms them into nerve impulses that travel to the brain.
A coiled, fluid-filled tube in the inner ear that changes mechanical sound vibrations and positional information to nerve impulses that travel to the brain.
Image shows a photograph of several wine bottles on a shelf. The image has been deliberately blurred to simulate the effects of drunkeness.
Created by CK-12 Foundation/Adapted by Christine Miller

Case Study Conclusion: Drink and Flush
You are probably aware that, because of its effects on the brain, drinking alcohol can cause visual disturbances, slurred speech, drowsiness, impaired judgment, and loss of coordination. Although it may be less obvious, alcohol also can have serious effects on the functioning of the excretory system.
As you learned from the conversation between Talia and Shae — who were in line for the restroom at the beginning of this chapter — alcohol consumption inhibits a hormone that causes our bodies to retain water. As a result, more water is released in urine, increasing the frequency of restroom trips, as well as the risk of dehydration.
Which hormone discussed in this chapter does this? If you answered antidiuretic hormone (ADH; also called vasopressin) — you are correct! ADH is secreted by the posterior pituitary gland and acts on the kidneys. As you have learned, the kidneys filter the blood, reabsorb needed substances, and produce urine. ADH helps the body conserve water by influencing this process. ADH makes the collecting ducts in the kidneys permeable to water, allowing water molecules to be reabsorbed from the urine back into the blood through osmosis into capillaries.
Alcohol is thought to produce more dilute urine by inhibiting the release of ADH. This causes the collecting ducts to be more impermeable to water, so less water can be reabsorbed, and more is excreted in urine. Because the volume of urine is increased, the bladder fills up more quickly, and the urge to urinate occurs more frequently. This is part of the reason why you often see a long line for the restroom in situations where many people are drinking alcohol. In addition to producing more dilute urine, simply consuming many beverages can also increase urine output.
In most cases, moderate drinking causes only a minor and temporary effect on kidney function. However, when people consume a large quantity of alcohol in a short period of time, or abuse alcohol over long time periods, there can be serious effects on the kidney. Binge drinking (consuming roughly four to five drinks in two hours) can cause a condition called “acute kidney injury,” a serious and sudden impairment of kidney function that requires immediate medical attention. As with the other cases of kidney failure that you learned about in this chapter, the treatment is to artificially filter the blood using hemodialysis. While normal kidney function may eventually return, acute kidney injury can sometimes cause long-term damage to the kidneys.
In cases where people abuse alcohol, particularly for an extended period of time, there can be many serious effects on the kidneys and other parts of the excretory system. The dehydrating effect of alcohol on the body can impair the function of many organs, including the kidneys themselves. Additionally, because of alcohol’s effect on kidney function, water balance, and ion balance, chronic alcohol consumption can cause abnormalities in blood ion concentration and acid-base balance, which can be very dangerous.
Drinking more than two alcoholic beverages a day can increase your risk for high blood pressure, too. As you have learned, high blood pressure is a risk factor for some kidney disorders, as well as a common cause of kidney failure. Drinking too much alcohol can damage the kidneys by raising blood pressure.
Finally, chronic excessive consumption of alcohol can cause liver disease. The liver is an important organ of the excretory system that breaks down toxic substances in the blood. The liver and kidneys work together to remove wastes from the bloodstream. You may remember, for example, the liver transforms ammonia into urea, which is then filtered and excreted by the kidneys. When the liver is not functioning normally, it puts added strain on the kidneys, which can result in kidney dysfunction. This association between alcohol, liver disease, and kidney dysfunction is so strong that most of the patients in Canada with both liver disease and related kidney dysfunction are alcoholics.
As you have learned, the excretory system is essential in removing toxic wastes from the body and regulating homeostasis. Having an occasional drink can temporarily alter these functions, but excessive alcohol exposure can seriously and permanently damage this system in many ways. Limiting alcohol consumption can help preserve the normal functioning of the excretory system, so that it can protect your health.
Chapter 16 Summary
In this chapter you learned about the excretory system. Specifically, you learned that:
- Excretion is the process of removing wastes and excess water from the body. It is an essential process in all living things, and a major way in which the human body maintains homeostasis.
- Organs of the excretory system include the skin, liver, large intestine, lungs, and kidneys.
-
- The skin plays a role in excretion through the production of sweat by sweat glands. Sweating eliminates excess water and salts, as well as a small amount of urea, a byproduct of protein catabolism.
- The liver is a very important organ of excretion. The liver breaks down many substances — including toxins — in the blood. The liver also excretes bilirubin (a waste product of hemoglobin catabolism) in bile. Bile then travels to the small intestine and is eventually excreted in feces by the large intestine.
- The main excretory function of the large intestine is to eliminate solid waste that remains after food is digested and water is extracted from the indigestible matter. The large intestine also collects and excretes wastes from throughout the body.
- The lungs are responsible for the excretion of gaseous wastes — primarily carbon dioxide — from cellular respiration in cells throughout the body. Exhaled air also contains water vapor and trace levels of some other waste gases.
- The paired kidneys are often considered the main organs of excretion. Their primary function is the elimination of excess water and wastes from the bloodstream by the production of urine. The kidneys filter many substances out of blood, allow the blood to reabsorb needed materials, and use the remaining materials to form urine.
-
- The two bean-shaped kidneys are located high in the back of the abdominal cavity on either side of the spine. A renal artery connects each kidney with the aorta, and transports unfiltered blood to the kidney. A renal vein connects each kidney with the inferior vena cava and transports filtered blood back to the circulation.
- The kidney has two main layers involved in the filtration of blood and formation of urine: the outer cortex and inner medulla. At least a million nephrons — which are the tiny functional units of the kidney — span the cortex and medulla. The entire kidney is surrounded by a fibrous capsule and protective fat layers.
- As blood flows through a nephron, many materials are filtered out of the blood, needed materials are returned to the blood, and the remaining materials are used to form urine.
-
-
- In each nephron, the glomerulus and the surrounding glomerular capsule form the unit that filters blood. From the glomerular capsule, the material filtered from blood (called filtrate) passes through the long renal tubule. As it does, some substances are reabsorbed into the blood, and other substances are secreted from the blood into the filtrate, finally forming urine. The urine empties into collecting ducts, where more water may be reabsorbed.
-
- The kidneys are part of the urinary system, which also includes the ureters, urinary bladder, and urethra. The main function of the urinary system is to eliminate the waste products of metabolism from the body by forming and excreting urine. After urine forms in the kidneys, it is transported through the ureters to the bladder. The bladder stores the urine until urination, when urine is transported by the urethra to be excreted outside the body.
-
- Besides the elimination of waste products such as urea, uric acid, excess water, and mineral ions, the urinary system has other vital functions. These include maintaining homeostasis of mineral ions in extracellular fluid, regulating acid-base balance in the blood, regulating the volume of extracellular fluids, and controlling blood pressure.
-
-
- The formation of urine must be closely regulated to maintain body-wide homeostasis. Several endocrine hormones help control this function of the urinary system, including antidiuretic hormone secreted from the posterior pituitary gland, parathyroid hormone from the parathyroid glands, and aldosterone from the adrenal glands.
-
-
-
-
- For example, the kidneys are part of the renin-angiotensin-aldosterone system that regulates the concentration of sodium in the blood to control blood pressure. In this system, the enzyme renin secreted by the kidneys works with hormones from the liver and adrenal gland to stimulate nephrons to reabsorb more sodium and water from urine.
- The kidneys also secrete endocrine hormones, including calcitriol — which helps control the level of calcium in the blood — and erythropoietin, which stimulates bone marrow to produce red blood cells.
-
- The process of urination is controlled by both the autonomic and the somatic nervous systems. The autonomic system causes the detrusor muscle in the bladder wall to relax as the bladder fills with urine, but conscious contraction of the detrusor muscle expels urine from the bladder during urination.
- Ureters are tube-like structures that connect the kidneys with the urinary bladder. Each ureter arises at the renal pelvis of a kidney and travels down through the abdomen to the urinary bladder. The walls of the ureter contain smooth muscle that can contract to push urine through the ureter by peristalsis. The walls are lined with transitional epithelium that can expand and stretch.
- The urinary bladder is a hollow, muscular organ that rests on the pelvic floor. It is also lined with transitional epithelium. The function of the bladder is to collect and store urine from the kidneys before the urine is eliminated through urination. Filling of the bladder triggers the autonomic nervous system to stimulate the detrusor muscle in the bladder wall to contract. This forces urine out of the bladder and into the urethra.
- The urethra is a tube that connects the urinary bladder to the external urethral orifice. Somatic nerves control the sphincter at the distal end of the urethra. This allows the opening of the sphincter for urination to be under voluntary control.
-
- Diabetic nephropathy is a progressive kidney disease caused by damage to the capillaries in the glomeruli of the kidneys due to long-standing diabetes mellitus. Years of capillary damage may occur before symptoms first appear.
- Polycystic kidney disease (PKD) is a genetic disorder (autosomal dominant or recessive) in which multiple abnormal cysts grow in the kidneys.
- Diabetic nephropathy, PKD, or chronic hypertension may lead to kidney failure, in which the kidneys are no longer able to adequately filter metabolic wastes from the blood. Kidneys may fail to such a degree that kidney transplantation or repeated, frequent hemodialysis is needed to support life. In hemodialysis, the patient’s blood is filtered artificially through a machine and then returned to the patient’s circulation.
- A kidney stone is a solid crystal that forms in a kidney from minerals in urine. A small stone may pass undetected through the ureters and the rest of the urinary tract. A larger stone may cause pain when it passes or be too large to pass, causing blockage of a ureter. Large kidney stones may be shattered with high-intensity ultrasound into pieces small enough to pass through the urinary tract, or they may be removed surgically.
- A bladder infection is generally caused by bacteria that reach the bladder from the GI tract and multiply. Bladder infections are much more common in females than males because the female urethra is much shorter and closer to the anus. Treatment generally includes antibiotic drugs.
- Urinary incontinence is a chronic problem of uncontrolled leakage of urine. It is very common, especially at older ages and in women. In men, urinary incontinence is usually caused by an enlarged prostate gland. In women, it is usually caused by stretching of pelvic floor muscles during childbirth (stress incontinence) or by an “overactive bladder” that empties without warning (urge incontinence).
You have learned that, through the removal of toxic wastes and the maintenance of homeostasis, the excretory system protects your body. But how does your body protect itself against pathogens and other threats? Read the next chapter on the immune system to find out.
Chapter 16 Review
-
- In what ways can the alveoli of the lungs be considered analogous to the nephrons of the kidney?
- What is urea? Where is urea produced, and what is it produced from? How is urea excreted from the body?
- If a person has a large kidney stone preventing urine that has left the kidney from reaching the bladder, where do you think this kidney stone is located? Explain your answer.
- As it relates to urine production, explain what is meant by “Excretion = Filtration – Reabsorption + Secretion."
- Which disease discussed in the chapter specifically affects the glomerular capillaries of the kidneys? Where are the glomerular capillaries located within the kidneys, and what is their function?
- Describe one way in which the excretory system helps maintain homeostasis in the body.
- High blood pressure can both contribute to the development of kidney disorders and be a symptom of kidney disorders. What is a kidney disorder that can be caused by high blood pressure? What is a kidney disorder that has high blood pressure as a symptom? How does blood pressure generally relate to the function of the kidney?
- If the body is dehydrated, what do the kidneys do? What does this do to the appearance of the urine produced?
- Identify three risk factors for the development of kidney stones.
Attribution
Figure 16.7.1
Tags: Alcohol Drink Alkolismus Bottles Glass Container by Gerd Altmann [geralt] on Pixabay is used under the Pixabay License (https://pixabay.com/service/license/).
Created by CK-12 Foundation/Adapted by Christine Miller

Case Study Conclusion: Drink and Flush
You are probably aware that, because of its effects on the brain, drinking alcohol can cause visual disturbances, slurred speech, drowsiness, impaired judgment, and loss of coordination. Although it may be less obvious, alcohol also can have serious effects on the functioning of the excretory system.
As you learned from the conversation between Talia and Shae — who were in line for the restroom at the beginning of this chapter — alcohol consumption inhibits a hormone that causes our bodies to retain water. As a result, more water is released in urine, increasing the frequency of restroom trips, as well as the risk of dehydration.
Which hormone discussed in this chapter does this? If you answered antidiuretic hormone (ADH; also called vasopressin) — you are correct! ADH is secreted by the posterior pituitary gland and acts on the kidneys. As you have learned, the kidneys filter the blood, reabsorb needed substances, and produce urine. ADH helps the body conserve water by influencing this process. ADH makes the collecting ducts in the kidneys permeable to water, allowing water molecules to be reabsorbed from the urine back into the blood through osmosis into capillaries.
Alcohol is thought to produce more dilute urine by inhibiting the release of ADH. This causes the collecting ducts to be more impermeable to water, so less water can be reabsorbed, and more is excreted in urine. Because the volume of urine is increased, the bladder fills up more quickly, and the urge to urinate occurs more frequently. This is part of the reason why you often see a long line for the restroom in situations where many people are drinking alcohol. In addition to producing more dilute urine, simply consuming many beverages can also increase urine output.
In most cases, moderate drinking causes only a minor and temporary effect on kidney function. However, when people consume a large quantity of alcohol in a short period of time, or abuse alcohol over long time periods, there can be serious effects on the kidney. Binge drinking (consuming roughly four to five drinks in two hours) can cause a condition called “acute kidney injury,” a serious and sudden impairment of kidney function that requires immediate medical attention. As with the other cases of kidney failure that you learned about in this chapter, the treatment is to artificially filter the blood using hemodialysis. While normal kidney function may eventually return, acute kidney injury can sometimes cause long-term damage to the kidneys.
In cases where people abuse alcohol, particularly for an extended period of time, there can be many serious effects on the kidneys and other parts of the excretory system. The dehydrating effect of alcohol on the body can impair the function of many organs, including the kidneys themselves. Additionally, because of alcohol’s effect on kidney function, water balance, and ion balance, chronic alcohol consumption can cause abnormalities in blood ion concentration and acid-base balance, which can be very dangerous.
Drinking more than two alcoholic beverages a day can increase your risk for high blood pressure, too. As you have learned, high blood pressure is a risk factor for some kidney disorders, as well as a common cause of kidney failure. Drinking too much alcohol can damage the kidneys by raising blood pressure.
Finally, chronic excessive consumption of alcohol can cause liver disease. The liver is an important organ of the excretory system that breaks down toxic substances in the blood. The liver and kidneys work together to remove wastes from the bloodstream. You may remember, for example, the liver transforms ammonia into urea, which is then filtered and excreted by the kidneys. When the liver is not functioning normally, it puts added strain on the kidneys, which can result in kidney dysfunction. This association between alcohol, liver disease, and kidney dysfunction is so strong that most of the patients in Canada with both liver disease and related kidney dysfunction are alcoholics.
As you have learned, the excretory system is essential in removing toxic wastes from the body and regulating homeostasis. Having an occasional drink can temporarily alter these functions, but excessive alcohol exposure can seriously and permanently damage this system in many ways. Limiting alcohol consumption can help preserve the normal functioning of the excretory system, so that it can protect your health.
Chapter 16 Summary
In this chapter you learned about the excretory system. Specifically, you learned that:
- Excretion is the process of removing wastes and excess water from the body. It is an essential process in all living things, and a major way in which the human body maintains homeostasis.
- Organs of the excretory system include the skin, liver, large intestine, lungs, and kidneys.
-
- The skin plays a role in excretion through the production of sweat by sweat glands. Sweating eliminates excess water and salts, as well as a small amount of urea, a byproduct of protein catabolism.
- The liver is a very important organ of excretion. The liver breaks down many substances — including toxins — in the blood. The liver also excretes bilirubin (a waste product of hemoglobin catabolism) in bile. Bile then travels to the small intestine and is eventually excreted in feces by the large intestine.
- The main excretory function of the large intestine is to eliminate solid waste that remains after food is digested and water is extracted from the indigestible matter. The large intestine also collects and excretes wastes from throughout the body.
- The lungs are responsible for the excretion of gaseous wastes — primarily carbon dioxide — from cellular respiration in cells throughout the body. Exhaled air also contains water vapor and trace levels of some other waste gases.
- The paired kidneys are often considered the main organs of excretion. Their primary function is the elimination of excess water and wastes from the bloodstream by the production of urine. The kidneys filter many substances out of blood, allow the blood to reabsorb needed materials, and use the remaining materials to form urine.
-
- The two bean-shaped kidneys are located high in the back of the abdominal cavity on either side of the spine. A renal artery connects each kidney with the aorta, and transports unfiltered blood to the kidney. A renal vein connects each kidney with the inferior vena cava and transports filtered blood back to the circulation.
- The kidney has two main layers involved in the filtration of blood and formation of urine: the outer cortex and inner medulla. At least a million nephrons — which are the tiny functional units of the kidney — span the cortex and medulla. The entire kidney is surrounded by a fibrous capsule and protective fat layers.
- As blood flows through a nephron, many materials are filtered out of the blood, needed materials are returned to the blood, and the remaining materials are used to form urine.
-
-
- In each nephron, the glomerulus and the surrounding glomerular capsule form the unit that filters blood. From the glomerular capsule, the material filtered from blood (called filtrate) passes through the long renal tubule. As it does, some substances are reabsorbed into the blood, and other substances are secreted from the blood into the filtrate, finally forming urine. The urine empties into collecting ducts, where more water may be reabsorbed.
-
- The kidneys are part of the urinary system, which also includes the ureters, urinary bladder, and urethra. The main function of the urinary system is to eliminate the waste products of metabolism from the body by forming and excreting urine. After urine forms in the kidneys, it is transported through the ureters to the bladder. The bladder stores the urine until urination, when urine is transported by the urethra to be excreted outside the body.
-
- Besides the elimination of waste products such as urea, uric acid, excess water, and mineral ions, the urinary system has other vital functions. These include maintaining homeostasis of mineral ions in extracellular fluid, regulating acid-base balance in the blood, regulating the volume of extracellular fluids, and controlling blood pressure.
-
-
- The formation of urine must be closely regulated to maintain body-wide homeostasis. Several endocrine hormones help control this function of the urinary system, including antidiuretic hormone secreted from the posterior pituitary gland, parathyroid hormone from the parathyroid glands, and aldosterone from the adrenal glands.
-
-
-
-
- For example, the kidneys are part of the renin-angiotensin-aldosterone system that regulates the concentration of sodium in the blood to control blood pressure. In this system, the enzyme renin secreted by the kidneys works with hormones from the liver and adrenal gland to stimulate nephrons to reabsorb more sodium and water from urine.
- The kidneys also secrete endocrine hormones, including calcitriol — which helps control the level of calcium in the blood — and erythropoietin, which stimulates bone marrow to produce red blood cells.
-
- The process of urination is controlled by both the autonomic and the somatic nervous systems. The autonomic system causes the detrusor muscle in the bladder wall to relax as the bladder fills with urine, but conscious contraction of the detrusor muscle expels urine from the bladder during urination.
- Ureters are tube-like structures that connect the kidneys with the urinary bladder. Each ureter arises at the renal pelvis of a kidney and travels down through the abdomen to the urinary bladder. The walls of the ureter contain smooth muscle that can contract to push urine through the ureter by peristalsis. The walls are lined with transitional epithelium that can expand and stretch.
- The urinary bladder is a hollow, muscular organ that rests on the pelvic floor. It is also lined with transitional epithelium. The function of the bladder is to collect and store urine from the kidneys before the urine is eliminated through urination. Filling of the bladder triggers the autonomic nervous system to stimulate the detrusor muscle in the bladder wall to contract. This forces urine out of the bladder and into the urethra.
- The urethra is a tube that connects the urinary bladder to the external urethral orifice. Somatic nerves control the sphincter at the distal end of the urethra. This allows the opening of the sphincter for urination to be under voluntary control.
-
- Diabetic nephropathy is a progressive kidney disease caused by damage to the capillaries in the glomeruli of the kidneys due to long-standing diabetes mellitus. Years of capillary damage may occur before symptoms first appear.
- Polycystic kidney disease (PKD) is a genetic disorder (autosomal dominant or recessive) in which multiple abnormal cysts grow in the kidneys.
- Diabetic nephropathy, PKD, or chronic hypertension may lead to kidney failure, in which the kidneys are no longer able to adequately filter metabolic wastes from the blood. Kidneys may fail to such a degree that kidney transplantation or repeated, frequent hemodialysis is needed to support life. In hemodialysis, the patient’s blood is filtered artificially through a machine and then returned to the patient’s circulation.
- A kidney stone is a solid crystal that forms in a kidney from minerals in urine. A small stone may pass undetected through the ureters and the rest of the urinary tract. A larger stone may cause pain when it passes or be too large to pass, causing blockage of a ureter. Large kidney stones may be shattered with high-intensity ultrasound into pieces small enough to pass through the urinary tract, or they may be removed surgically.
- A bladder infection is generally caused by bacteria that reach the bladder from the GI tract and multiply. Bladder infections are much more common in females than males because the female urethra is much shorter and closer to the anus. Treatment generally includes antibiotic drugs.
- Urinary incontinence is a chronic problem of uncontrolled leakage of urine. It is very common, especially at older ages and in women. In men, urinary incontinence is usually caused by an enlarged prostate gland. In women, it is usually caused by stretching of pelvic floor muscles during childbirth (stress incontinence) or by an “overactive bladder” that empties without warning (urge incontinence).
You have learned that, through the removal of toxic wastes and the maintenance of homeostasis, the excretory system protects your body. But how does your body protect itself against pathogens and other threats? Read the next chapter on the immune system to find out.
Chapter 16 Review
-
- In what ways can the alveoli of the lungs be considered analogous to the nephrons of the kidney?
- What is urea? Where is urea produced, and what is it produced from? How is urea excreted from the body?
- If a person has a large kidney stone preventing urine that has left the kidney from reaching the bladder, where do you think this kidney stone is located? Explain your answer.
- As it relates to urine production, explain what is meant by “Excretion = Filtration – Reabsorption + Secretion."
- Which disease discussed in the chapter specifically affects the glomerular capillaries of the kidneys? Where are the glomerular capillaries located within the kidneys, and what is their function?
- Describe one way in which the excretory system helps maintain homeostasis in the body.
- High blood pressure can both contribute to the development of kidney disorders and be a symptom of kidney disorders. What is a kidney disorder that can be caused by high blood pressure? What is a kidney disorder that has high blood pressure as a symptom? How does blood pressure generally relate to the function of the kidney?
- If the body is dehydrated, what do the kidneys do? What does this do to the appearance of the urine produced?
- Identify three risk factors for the development of kidney stones.
Attribution
Figure 16.7.1
Tags: Alcohol Drink Alkolismus Bottles Glass Container by Gerd Altmann [geralt] on Pixabay is used under the Pixabay License (https://pixabay.com/service/license/).
Image shows a female doctor checking the lymph nodes in the neck of a patient.
Created by CK-12 Foundation/Adapted by Christine Miller

Case Study: Defending Your Defenses

Twenty-six-year-old Hakeem wasn’t feeling well. He was more tired than usual, dragging through his workdays despite going to bed earlier, and napping on the weekends. He didn’t have much of an appetite, and had started losing weight. When he pressed on the side of his neck, like the doctor is doing in Figure 17.1.1, he noticed an unusual lump.
Hakeem went to his doctor, who performed a physical exam and determined that the lump was a swollen lymph node. Lymph nodes are part of the immune system, and they will often become enlarged when the body is fighting off an infection. Dr. Hayes thinks that the swollen lymph node and fatigue could be signs of a viral or bacterial infection, although he is concerned about Hakeem’s lack of appetite and weight loss. All of those symptoms combined can indicate a type of cancer called lymphoma. An infection, however, is a more likely cause, particularly in a young person like Hakeem. Dr. Hayes prescribes an antibiotic in case Hakeem has a bacterial infection, and advises him to return in a few weeks if his lymph node does not shrink, or if he is not feeling better.
Hakeem returns a few weeks later. He is not feeling better and his lymph node is still enlarged. Dr. Hayes is concerned, and orders a biopsy of the enlarged lymph node. A lymph node biopsy for suspected lymphoma often involves the surgical removal of all or part of a lymph node. This helps to determine whether the tissue contains cancerous cells.

The initial results of the biopsy indicate that Hakeem does have lymphoma. Although lymphoma is more common in older people, young adults and even children can get this disease. There are many types of lymphoma, with the two main types being Hodgkin's lymphoma and non-Hodgkin's lymphoma. Non-Hodgkin lymphoma (NHL), in turn, has many subtypes. The subtype depends on several factors, including which cell types are affected. Some subtypes of NHL, for example, affect immune system cells called B cells, while others affect different immune system cells called T cells.
Dr. Hayes explains to Hakeem that it is important to determine which type of lymphoma he has, in order to choose the best course of treatment. Hakeem’s biopsied tissue will be further examined and tested to see which cell types are affected, as well as which specific cell-surface proteins — called antigens — are present. This should help identify his specific type of lymphoma.
As you read this chapter, you will learn about the functions of the immune system, and the specific roles that its cells and organs — such as B and T cells and lymph nodes — play in defending the body. At the end of this chapter, you will learn what type of lymphoma Hakeem has and what some of his treatment options are, including treatments that make use of the biochemistry of the immune system to fight cancer with the immune system itself.
Chapter Overview: Immune System
In this chapter, you will learn about the immune system — the system that defends the body against infections and other causes of disease, such as cancerous cells. Specifically, you will learn about:
- How the immune system identifies normal cells of the body as “self” and pathogens and damaged cells as “non-self.”
- The two major subsystems of the general immune system: the innate immune system — which provides a quick, but non-specific response — and the adaptive immune system, which is slower, but provides a specific response that often results in long-lasting immunity.
- The specialized immune system that protects the brain and spinal cord, called the neuroimmune system.
- The organs, cells, and responses of the innate immune system, which includes physical barriers (such as skin and mucus), chemical and biological barriers, inflammation, activation of the complement system of molecules, and non-specific cellular responses (such as phagocytosis).
- The lymphatic system — which includes white blood cells called lymphocytes, lymphatic vessels (which transport a fluid called lymph), and organs (such as the spleen, tonsils, and lymph nodes) — and its important role in the adaptive immune system.
- Specific cells of the immune system and their functions, including B cells, T cells, plasma cells, and natural killer cells.
- How the adaptive immune system can generate specific and often long-lasting immunity against pathogens through the production of antibodies.
- How vaccines work to generate immunity.
- How cells in the immune system detect and kill cancerous cells.
- Some strategies that pathogens employ to evade the immune system.
- Disorders of the immune system, including allergies, autoimmune diseases (such as diabetes and multiple sclerosis), and immunodeficiency resulting from conditions such as HIV infection.
As you read the chapter, think about the following questions:
- What are the functions of lymph nodes?
- What are B and T cells? How do they relate to lymph nodes?
- What are cell-surface antigens? How do they relate to the immune system and to cancer?
Attributions
Figure 17.1.1
Lymph nodes/Is it a Cold or the Flu by Lee Health on Vimeo is used under Vimeo's Terms of Service (https://vimeo.com/terms#licenses).
Figure 17.1.2
mitchell-luo-ymo_yC_N_2o-unsplash [photo] by Mitchell Luo on Unsplash is used under the Unsplash License (https://unsplash.com/license).
Figure 17.1.3
Lymph node biopsy by US Army Africa on Flickr is used under a CC BY 2.0 (https://creativecommons.org/licenses/by/2.0/) license.
References
Mayo Clinic Staff. (n.d.). Hodgkin's lymphoma [online article]. MayoClinic.org. https://www.mayoclinic.org/diseases-conditions/hodgkins-lymphoma/symptoms-causes/syc-20352646
Mayo Clinic Staff. (n.d.). Non-Hodgkin's lymphoma [online article]. MayoClinic.org. https://www.mayoclinic.org/diseases-conditions/non-hodgkins-lymphoma/symptoms-causes/syc-20375680
Created by CK-12 Foundation/Adapted by Christine Miller

Case Study: Defending Your Defenses

Twenty-six-year-old Hakeem wasn’t feeling well. He was more tired than usual, dragging through his workdays despite going to bed earlier, and napping on the weekends. He didn’t have much of an appetite, and had started losing weight. When he pressed on the side of his neck, like the doctor is doing in Figure 17.1.1, he noticed an unusual lump.
Hakeem went to his doctor, who performed a physical exam and determined that the lump was a swollen lymph node. Lymph nodes are part of the immune system, and they will often become enlarged when the body is fighting off an infection. Dr. Hayes thinks that the swollen lymph node and fatigue could be signs of a viral or bacterial infection, although he is concerned about Hakeem’s lack of appetite and weight loss. All of those symptoms combined can indicate a type of cancer called lymphoma. An infection, however, is a more likely cause, particularly in a young person like Hakeem. Dr. Hayes prescribes an antibiotic in case Hakeem has a bacterial infection, and advises him to return in a few weeks if his lymph node does not shrink, or if he is not feeling better.
Hakeem returns a few weeks later. He is not feeling better and his lymph node is still enlarged. Dr. Hayes is concerned, and orders a biopsy of the enlarged lymph node. A lymph node biopsy for suspected lymphoma often involves the surgical removal of all or part of a lymph node. This helps to determine whether the tissue contains cancerous cells.

The initial results of the biopsy indicate that Hakeem does have lymphoma. Although lymphoma is more common in older people, young adults and even children can get this disease. There are many types of lymphoma, with the two main types being Hodgkin's lymphoma and non-Hodgkin's lymphoma. Non-Hodgkin lymphoma (NHL), in turn, has many subtypes. The subtype depends on several factors, including which cell types are affected. Some subtypes of NHL, for example, affect immune system cells called B cells, while others affect different immune system cells called T cells.
Dr. Hayes explains to Hakeem that it is important to determine which type of lymphoma he has, in order to choose the best course of treatment. Hakeem’s biopsied tissue will be further examined and tested to see which cell types are affected, as well as which specific cell-surface proteins — called antigens — are present. This should help identify his specific type of lymphoma.
As you read this chapter, you will learn about the functions of the immune system, and the specific roles that its cells and organs — such as B and T cells and lymph nodes — play in defending the body. At the end of this chapter, you will learn what type of lymphoma Hakeem has and what some of his treatment options are, including treatments that make use of the biochemistry of the immune system to fight cancer with the immune system itself.
Chapter Overview: Immune System
In this chapter, you will learn about the immune system — the system that defends the body against infections and other causes of disease, such as cancerous cells. Specifically, you will learn about:
- How the immune system identifies normal cells of the body as “self” and pathogens and damaged cells as “non-self.”
- The two major subsystems of the general immune system: the innate immune system — which provides a quick, but non-specific response — and the adaptive immune system, which is slower, but provides a specific response that often results in long-lasting immunity.
- The specialized immune system that protects the brain and spinal cord, called the neuroimmune system.
- The organs, cells, and responses of the innate immune system, which includes physical barriers (such as skin and mucus), chemical and biological barriers, inflammation, activation of the complement system of molecules, and non-specific cellular responses (such as phagocytosis).
- The lymphatic system — which includes white blood cells called lymphocytes, lymphatic vessels (which transport a fluid called lymph), and organs (such as the spleen, tonsils, and lymph nodes) — and its important role in the adaptive immune system.
- Specific cells of the immune system and their functions, including B cells, T cells, plasma cells, and natural killer cells.
- How the adaptive immune system can generate specific and often long-lasting immunity against pathogens through the production of antibodies.
- How vaccines work to generate immunity.
- How cells in the immune system detect and kill cancerous cells.
- Some strategies that pathogens employ to evade the immune system.
- Disorders of the immune system, including allergies, autoimmune diseases (such as diabetes and multiple sclerosis), and immunodeficiency resulting from conditions such as HIV infection.
As you read the chapter, think about the following questions:
- What are the functions of lymph nodes?
- What are B and T cells? How do they relate to lymph nodes?
- What are cell-surface antigens? How do they relate to the immune system and to cancer?
Attributions
Figure 17.1.1
Lymph nodes/Is it a Cold or the Flu by Lee Health on Vimeo is used under Vimeo's Terms of Service (https://vimeo.com/terms#licenses).
Figure 17.1.2
mitchell-luo-ymo_yC_N_2o-unsplash [photo] by Mitchell Luo on Unsplash is used under the Unsplash License (https://unsplash.com/license).
Figure 17.1.3
Lymph node biopsy by US Army Africa on Flickr is used under a CC BY 2.0 (https://creativecommons.org/licenses/by/2.0/) license.
References
Mayo Clinic Staff. (n.d.). Hodgkin's lymphoma [online article]. MayoClinic.org. https://www.mayoclinic.org/diseases-conditions/hodgkins-lymphoma/symptoms-causes/syc-20352646
Mayo Clinic Staff. (n.d.). Non-Hodgkin's lymphoma [online article]. MayoClinic.org. https://www.mayoclinic.org/diseases-conditions/non-hodgkins-lymphoma/symptoms-causes/syc-20375680
Image shows a Scanning electron micrograph of a parasite. It looks quite scary, with a creepy sucker-type thing on its neck

