8.3 Neurons and Neuroglia
Life as Art
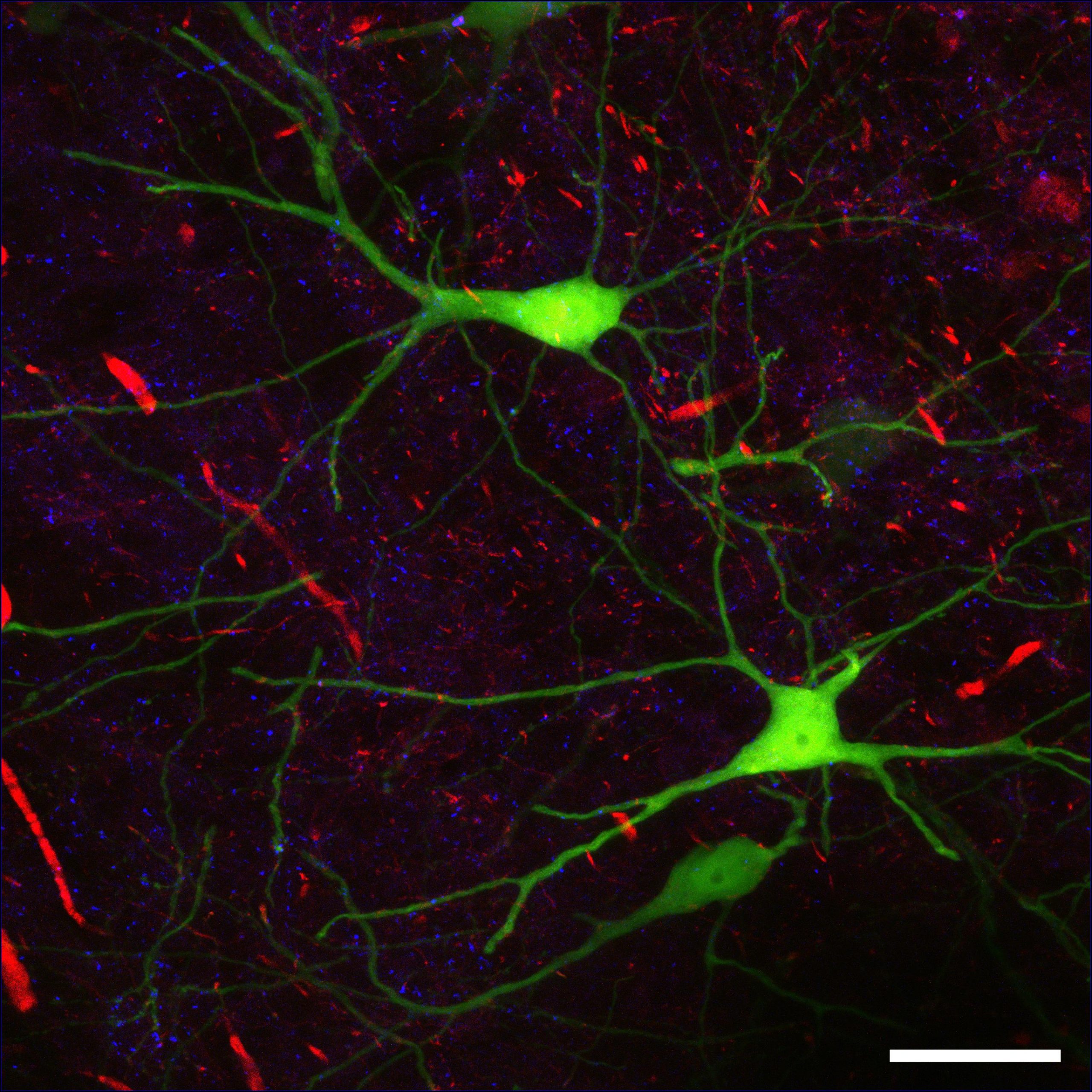
This colourful picture (Figure 8.3.1) could be an abstract work of modern art. You might imagine it hanging in an art museum or art gallery. In fact, the picture illustrates real life — not artistic creation. It is a micrograph of human nervous tissue. The neon green structures in the picture are neurons. The neuron is one of two basic types of cells in the nervous system. The other type is the neuroglial cell.
Neurons
Neurons — also called nerve cells — are electrically excitable cells that are the main functional units of the nervous system. Their function is to transmit nerve impulses, and they are the only type of human cells that can carry out this function.
Neuron Structure
Figure 8.3.2 shows the structure of a typical neuron. Click on each of the main parts to learn about their functions.
Figure 8.3.2 The structure of a typical neuron.
Neurogenesis
Fully differentiated neurons, with all their special structures, cannot divide and form new daughter neurons. Until recently, scientists thought that new neurons could no longer be formed after the brain developed prenatally. In other words, they thought that people were born with all the brain neurons they would ever have, and as neurons died, they would not be replaced. However, new evidence shows that additional neurons can form in the brain, even in adults, from the division of undifferentiated neural stem cells found throughout the brain. The production of new neurons is called neurogenesis. The extent to which it can occur is not known, but it is not likely to be very great in humans.
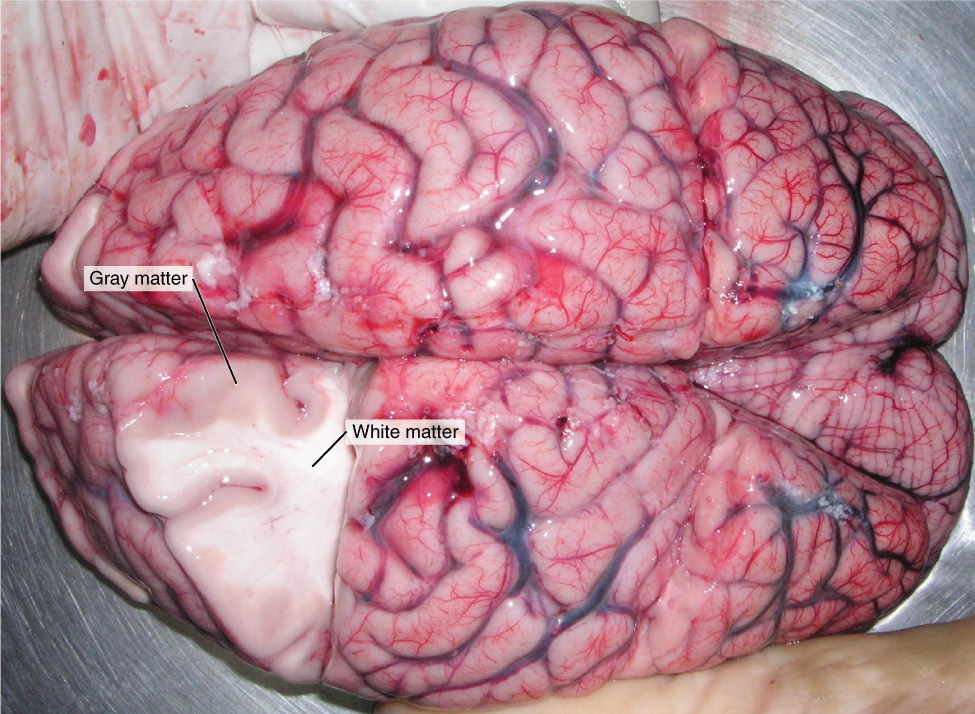
Neurons in Nervous Tissues
The nervous tissue in the brain and spinal cord consists of gray matter and white matter. Gray matter contains mainly non-myelinated structures, including the cell bodies and dendrites of neurons. It is gray only in cadavers. Living gray matter is actually more pink than gray (see Figure 8.3.3) White matter consists mainly of axons covered with a myelin sheath, which gives them their white colour. White matter also makes up the nerves of the peripheral nervous system. Nerves consist of long bundles of myelinated axons that extend to muscles, organs, or glands throughout the body. The axons in each nerve are bundled together like wires in a cable. Axons in nerves may be more than a metre long in an adult. The longest nerve runs from the base of the spine to the toes.
Types of Neurons
There are hundreds of different types of neurons in the human nervous system that exhibit a variety of structures and functions. Nonetheless, many neurons can be classified functionally based on the direction in which they carry nerve impulses.
- Sensory (also called afferent) neurons carry nerve impulses from sensory receptors in tissues and organs to the central nervous system. They change physical stimuli (such as touch, light, and sound) into nerve impulses.
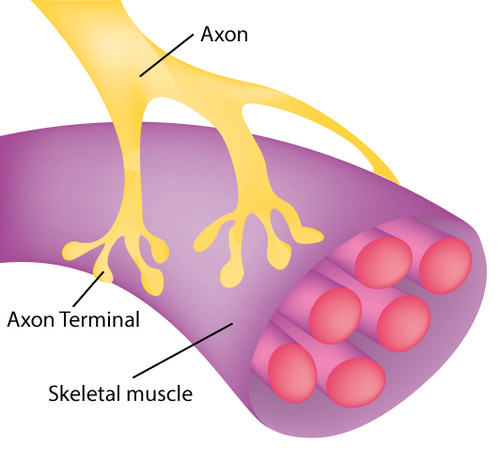
- Motor (also called efferent) neurons, like the one in the diagram below (Figure 8.3.4), carry nerve impulses from the central nervous system to muscles and glands. They change nerve signals into the activation of these structures.
- Within the spinal cord or brain, interneurons carry nerve impulses back and forth, often between sensory and motor neurons.
Neuroglia
In addition to neurons, nervous tissues also consist of neuroglia, also called glial cells. The root of the word glial comes from a Greek word meaning “glue,” which reflects earlier ideas about the role of neuroglia in nervous tissues. Neuroglia were thought to be little more than “glue” holding together the all-important neurons, but this is no longer the case. They are now known to play many vital roles in the nervous system. There are several different types of neuroglia, each with a different function. You can see six types of neuroglia in Figure 8.3.5.
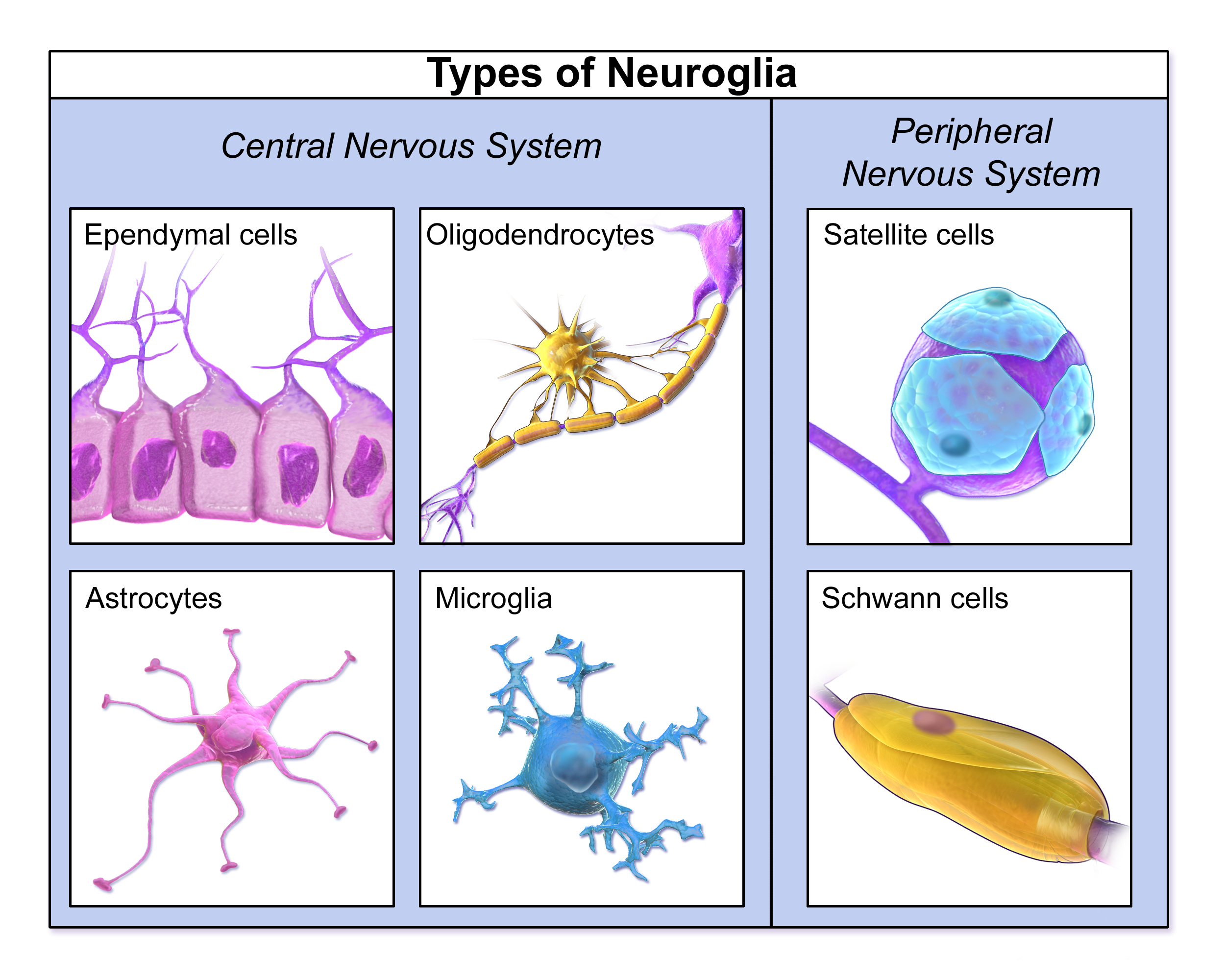
In general, neuroglia provide support for neurons and help them carry out the basic function of nervous tissues, which is to transmit nerve impulses. For example, oligodendrocytes in the central nervous system and Schwann cells in the peripheral nervous system generate the lipids that make up myelin sheaths, which increase the speed of nerve impulses’ transmission. Functions of other neuroglia cells include holding neurons in place, supplying neurons with nutrients, regulating the repair of neurons, destroying pathogens, removing dead neurons, and directing axons to their targets. Neuroglia may also play a role in the transmission of nerve impulses, but this is still under study. Unlike mature neurons, mature glial cells retain the ability to divide by undergoing mitosis.
In the human brain, there are generally roughly equal numbers of neurons and neuroglia. If you think intelligence depends on how many neurons you have, think again. Having a relatively high number of neuroglia is actually associated with higher intelligence. When Einstein’s brain was analyzed, researchers discovered a significantly higher-than-normal ratio of neuroglia to neurons in areas of the brain associated with mathematical processing and language. On an evolutionary scale, as well, an increase in the ratio of neuroglia to neurons is associated with greater intelligence in species.
Feature: My Human Body
Would you like your brain to make new neurons that could help you become a better learner? When it comes to learning new things, what college student wouldn’t want a little more brain power? If research about rats applies to humans, then sustained aerobic exercise (such as running) can increase neurogenesis in the adult brain, and specifically in the hippocampus, a brain structure important for learning temporally and/or spatially complex tasks, as well as memory. Although the research is still at the beginning stages, it suggests that exercise may actually lead to a “smarter” brain. Even if the research results are not ultimately confirmed for humans, though, it can’t hurt to get more aerobic exercise. It is certainly beneficial for your body, if not your brain!
8.3 Summary
- Neurons are one of two major types of nervous system cells. They are electrically excitable cells that transmit nerve impulses.
- Neuroglia are the other major type of nervous system cells. There are many types of neuroglia and they have many specific functions. In general, neuroglia function to support, protect, and nourish neurons.
- The main parts of a neuron include the cell body, dendrites, and axon. The cell body contains the nucleus. Dendrites receive nerve impulses from other cells, and the axon transmits nerve impulses to other cells at axon terminals. A synapse is a complex membrane junction at the end of an axon terminal that transmits signals to another cell.
- Axons are often wrapped in an electrically-insulating myelin sheath, which is produced by neuroglia. Electrical signals occur at gaps in the myelin sheath, called nodes of Ranvier, which speeds the conduction of nerve impulses down the axon.
- Neurogenesis, or the formation of new neurons by cell division, may occur in a mature human brain, but only to a limited extent.
- The nervous tissue in the brain and spinal cord consists of gray matter (which contains unmyelinated cell bodies and dendrites of neurons) and white matter (which contains mainly myelinated axons of neurons). Nerves of the peripheral nervous system consist of long bundles of myelinated axons that extend throughout the body.
- There are hundreds of types of neurons in the human nervous system, but many can be classified on the basis of the direction in which they carry nerve impulses. Sensory neurons carry nerve impulses away from the body and toward the central nervous system, motor neurons carry them away from the central nervous system and toward the body, and interneurons often carry them between sensory and motor neurons.
8.3 Review Questions
-
- Describe the myelin sheath and nodes of Ranvier. How does their arrangement allow nerve impulses to travel very rapidly along axons?
- Define neurogenesis. What is the potential for neurogenesis in the human brain?
- Relate neurons to different types of nervous tissues.
- Compare and contrast sensory and motor neurons.
- Identify the role of interneurons.
- Identify four specific functions of neuroglia.
- What is the relationship between the proportion of neuroglia to neurons and intelligence?
-
-
8.3 Explore More
Thriving in the Face of Adversity | Stephanie Buxhoeveden | TEDxHerndon, TEDx Talks, 2015.
You can grow new brain cells. Here’s how | Sandrine Thuret,
TED, 2015.
Attributions
Figure 8.3.1
Nervous Tissue Confocal Microscopy/ Mouse brain, confocal microscopy by ZEISS Microscopy on Flickr is used under a CC BY-NC-ND 2.0 (https://creativecommons.org/licenses/by-nc-nd/2.0/) license.
Figure 8.3.2
Parts of a Neuron by Open Stax on Wikimedia Commons is used and adapted by Christine Miller under the CC BY 4.0 (https://creativecommons.org/licenses/by/4.0/) license.
Figure 8.3.3
White_and_Gray_Matter by OpenStax on Wikimedia Commons is used under a CC BY 4.0 (https://creativecommons.org/licenses/by/4.0/) license.
Figure 8.3.4
Neuromuscular Junction by CK-12 Foundation is used under a CC BY-NC 3.0 (https://creativecommons.org/licenses/by-nc/3.0/) license.
Figure 8.3.5
TypesofNeuroglia by BruceBlaus on Wikimedia Commons is used under a CC BY 3.0 (https://creativecommons.org/licenses/by/3.0/deed.en) license.
References
Betts, J. G., Young, K.A., Wise, J.A., Johnson, E., Poe, B., Kruse, D.H., Korol, O., Johnson, J.E., Womble, M., DeSaix, P. (2016, May 18). Figure 12.3 Gray matter and white matter [digital image]. In Anatomy and Physiology (Section 12.1). OpenStax. https://openstax.org/books/anatomy-and-physiology/pages/12-1-basic-structure-and-function-of-the-nervous-system
Betts, J. G., Young, K.A., Wise, J.A., Johnson, E., Poe, B., Kruse, D.H., Korol, O., Johnson, J.E., Womble, M., DeSaix, P. (2016, May 18). Figure 12.8 Parts of a neuron [digital image]. In Anatomy and Physiology (Section 12.2). OpenStax. https://openstax.org/books/anatomy-and-physiology/pages/12-2-nervous-tissue
Blausen.com staff. (2014). Types of neuroglia cells [digital image]. Medical gallery of Blausen Medical 2014. WikiJournal of Medicine, 1 (2). DOI:10.15347/wjm/2014.010. ISSN 2002-4436. Wikiversity.org. https://en.wikiversity.org/wiki/WikiJournal_of_Medicine/Medical_gallery_of_Blausen_Medical_2014
Brainard, J/ CK-12 Foundation. (2016). Figure 3 The axon in this diagram is part of a motor neuron. [digital image]. In CK-12 College Human Biology (Section 10.3) [online Flexbook]. CK12.org. https://www.ck12.org/book/ck-12-college-human-biology/section/10.3/
TED. (2015, October 30). You can grow new brain cells. Here’s how | Sandrine Thuret. YouTube. https://www.youtube.com/watch?v=B_tjKYvEziI&feature=youtu.be
TEDx Talks. (2015, April 3). Thriving in the face of adversity | Stephanie Buxhoeveden | TEDxHerndon. YouTube. https://www.youtube.com/watch?v=zuLOT6GsAxw&feature=youtu.be
Created by CK-12 Foundation/Adapted by Christine Miller

Bathing in Sunshine
Summer sun may feel good on your body, but its invisible UV rays wreak havoc on your skin. Exposing the skin to UV light causes photo-aging: premature wrinkling, brown discolourations, and other unattractive signs of sun exposure. Even worse, UV light increases your risk of skin cancer.
What Is Skin Cancer?
Skin cancer is a disease in which skin cells grow out of control. It is caused mainly by excessive exposure to UV light, which damages DNA. Therefore, skin cancer most often develops on areas of the skin that are frequently exposed to UV light. However, it can also occur on areas that are rarely exposed to UV light. Skin cancer affects people of all skin colours, including those with dark skin. It also affects more people altogether than all other cancers combined. One in five Canadians develops skin cancer in his or her lifetime.
Types of Skin Cancer
Skin cancer begins in the outer layer of skin, the epidermis. There are three common types of skin cancer: basal cell carcinoma, squamous cell carcinoma, and melanoma.
Basal Cell Carcinoma

Basal cell carcinoma occurs in basal cells of the epidermis. Basal cells are stem cells in the stratum basale layer that divide to form all the keratinocytes of the epidermis. Basal cell carcinoma is the most common form of skin cancer and 1 in 8 Canadians will develop basal cell carcinoma during their lifetime. A basal cell carcinoma may appear as a pearly or waxy sore, like the one shown in Figure 10.7.2. Basal cell carcinomas rarely spread (or undergo metastasis), so they can generally be cured with a biopsy, in which the lesion is cut out of the skin and analyzed in a medical lab.
Squamous Cell Carcinoma

Squamous cell carcinoma occurs in squamous cells of the epidermis. Squamous cells are flattened, keratin-filled cells in upper layers of the epidermis. Squamous cell carcinoma is the second most common form of skin cancer. More than two million cases occur in the United States each year. A squamous cell carcinoma may appear as a firm, red nodule, or as a flat lesion with a scaly or crusty surface, like the one pictured in Figure 10.7.3. Squamous cell carcinomas are generally localized and unlikely to metastasize, so they are usually curable surgically.
Melanoma

Melanoma occurs in melanocytes of the epidermis. Melanocytes are the melanin-producing cells in the stratum basale of the epidermis. Melanoma is the rarest type of skin cancer, accounting for less than one per cent of all skin cancer cases. Melanoma, however, is the most deadly type of skin cancer. It causes the vast majority of skin cancer deaths, because melanoma is malignant. If not treated, it will metastasize and spread to other parts of the body. If melanoma is detected early and while it is still localized in the skin, most patients survive for at least five years. If melanoma is discovered only after it has already metastasized to distant organs, there is only a 17% of patients surviving for five years. You can see an example of a melanoma in Figure 10.7.4.
Melanoma can develop anywhere on the body. It may develop in otherwise normal skin, or an existing mole may become cancerous. Signs of melanoma may include a:
- Mole that changes in size, feel, or colour.
- Mole that bleeds.
- Large brown spot on the skin sprinkled with darker specks.
- Small lesion with an irregular border and parts that appear red, white, blue, or blue-black.
- Dark lesion on the palms, soles, fingertips, toes, or mucous membranes.
Skin Cancer Risk Factors
Exposure to UV radiation causes about 90 per cent of all skin cancer cases. The connection between skin cancer and UV light is so strong that the World Health Organization has classified UV radiation (whether from tanning beds or the sun) as a Group 1 carcinogen (cancer-causing agent). Group 1 carcinogens are those carcinogens that are known with virtual certainty to cause cancer. In addition to UV light, Group 1 carcinogens include tobacco and plutonium. In terms of numbers of cancers caused, UV radiation is far worse than tobacco. More people develop skin cancer because of UV light exposure than develop lung cancer because of smoking. The increase in cancer risk due to UV light is especially great if you have ever had blistering sunburns as a child or teen.
Besides UV light exposure, other risk factors for skin cancer include:
- Having light coloured skin.
- Having a lot of moles.
- Being diagnosed with precancerous skin lesions.
- Having a family history of skin cancer.
- Having a personal history of skin cancer.
- Having a weakened immune system.
- Being exposed to other forms of radiation or to certain toxic substances such as arsenic.
Feature: My Human Body
As with most types of cancer, skin cancer is easiest to treat and most likely to be cured the earlier it is detected. The skin is one of the few organs that you can monitor for cancer yourself, as long as you know what to look for. A brown spot on the skin is likely to be a harmless mole, but it could be a sign of skin cancer. As shown in Figure 10.7.5 below, unlike moles, skin cancers may be asymmetrical, have irregular borders, may be very dark in colour, and may have a relatively great diameter. These characteristics can be remembered with the acronym ABCD.
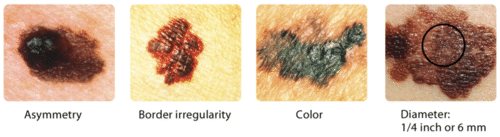
With the help of mirrors, you should check all of your skin regularly. Look for new skin growths or changes in any existing moles, freckles, bumps, or birthmarks. Report anything suspicious or different to your doctor.
If you have risk factors for skin cancer, it’s a good idea to have an annual skin check by a dermatologist. This helps ensure that cancerous or precancerous lesions will be detected before they grow too large and become difficult to cure, or in the case of melanoma, before they metastasize.
10.7 Summary
- Skin cancer is a disease in which skin cells grow out of control. It is caused mainly by excessive exposure to UV light, which damages DNA. Skin cancer affects more Canadians than all other cancers combined. There are three common types of skin cancer: basal cell carcinoma, squamous cell carcinoma, and melanoma. Carcinomas are more common and unlikely to metastasize. Melanoma is rare and likely to metastasize. It causes most skin cancer deaths.
- Besides exposure to UV light, risk factors for skin cancer include having light coloured skin, having lots of moles, and a family history of skin cancer, among several others.
10.7 Review Questions
- What is skin cancer?
- How common is skin cancer?
-
- Compare and contrast the three common types of skin cancer.
- Identify factors that increase the risk of skin cancer.
- How does exposure to UV light cause skin cancer?
- In which layer of the skin does skin cancer normally start?
- Which two skin cancers described in this section start in the same sub-layer? Include the name of the sub-layer and the cells affected in each of these cancers.
- Which type of skin cancer is most likely to spread to other organs? Explain your answer.
- Which form of skin cancer is the most deadly?
- What are some ways people can reduce their risk of getting skin cancer? Explain your answer.
10.7 Explore More
https://www.youtube.com/watch?v=60e-t4zglBk&feature=emb_logo
The skin 'beauty' and the sun 'beast': Charareh Pourzand at TEDxBathUniveristy, TEDx Talks, 2014.
https://www.youtube.com/watch?v=ID-O-Ion3EQ&feature=emb_logo
Cancer of the Vulva, Robert Miller, 2014.
https://www.youtube.com/watch?v=BmFEoCFDi-w
How do cancer cells behave differently from healthy ones? - George Zaidan, TED-Ed, 2012.
Attributions
Figure 10.7.1
Stolen_Moment_in_the_Sun by Angie Garrett on Wikimedia Commons is used under a CC BY 2.0 (https://creativecommons.org/licenses/by/2.0) license.
Figure 10.7.2
Basal_cell_carcinoma,_ulcerated by Kelly Nelson (Photographer) from National Cancer Institute (part of the National Institutes of Health) with the ID 9237 on Wikimedia Commons was released into the public domain (https://en.wikipedia.org/wiki/Public_domain).
Figure 10.7.3
Squamous_cell_carcinoma_(1) by Kelly Nelson (Photographer) from National Cancer Institute (part of the National Institutes of Health) with the ID 9248 on Wikimedia Commons was released into the public domain (https://en.wikipedia.org/wiki/Public_domain).
Figure 10.7.4
Melanoma by Unknown author (Photographer) from National Cancer Institute (part of the National Institutes of Health) with the AV-8500-3850/ ID 9186 on Wikimedia Commons was released into the public domain (https://en.wikipedia.org/wiki/Public_domain).
Figure 10.7.5
ABCDs of skin cancer by CK-12 Foundation is used under a CC BY-NC 3.0 (https://creativecommons.org/licenses/by-nc/3.0/) license. (Original images courtesy of NCI: ID numbers 2362; 2363; 2364; and 2184)
References
Brainard, J/ CK-12 Foundation. (2016). Figure 5 ABCDs of skin cancer[digital image]. In CK-12 College Human Biology (Section 12.7) [online Flexbook]. CK12.org. https://www.ck12.org/book/ck-12-college-human-biology/section/12.7/
Public Health Agency of Canada. (2019, December 9). Non melanoma skin cancer. Canada.ca. https://www.canada.ca/en/public-health/services/chronic-diseases/cancer/non-melanoma-skin-cancer.html
Robert Miller. (2014, July 22). Cancer of the vulva. YouTube. https://www.youtube.com/watch?v=ID-O-Ion3EQ
TED-Ed. (2012, December 5). How do cancer cells behave differently from healthy ones? - George Zaidan. YouTube. https://www.youtube.com/watch?v=BmFEoCFDi-w
TEDx Talks. (2014, March 28). The skin 'beauty' and the sun 'beast': Charareh Pourzand at TEDxBathUniveristy. YouTube. https://www.youtube.com/watch?v=60e-t4zglBk
Created by CK-12 Foundation/Adapted by Christine Miller

Stroller Moms
These moms (Figure 12.5.1) are setting a great example for their children by engaging in physical exercise. Adopting a habit of regular physical exercise is one of the most important ways to maintain fitness and good health. From higher self-esteem to a healthier heart, physical exercise can have a positive effect on virtually all aspects of health, including physical, mental, and emotional health.
What Is Physical Exercise?
Physical exercise is any bodily activity that enhances or maintains physical fitness and overall health and wellness. We generally think of physical exercise as activities that are undertaken for the main purpose of improving physical fitness and health. However, physical activities that are undertaken for other purposes may also count as physical exercise. Scrubbing a floor, raking a lawn, or playing active games with young children or a pet are all activities that can have fitness and health benefits, even though they generally are not done mainly for this purpose.
How much physical exercise should people get? In the Canada, both the Canadian Food Guide and the Canadian Society for Exercise Physiology recommend that every child and adult who is able should participate in moderate exercise for a minimum of 60 minutes a day. This might include walking, swimming, and/or household or yard work.
Types of Physical Exercise
Physical exercise can be classified into three types, depending on the effects it has on the body: aerobic exercise, anaerobic exercise, and flexibility exercise. Many specific examples of physical exercise (including playing soccer and rock climbing) can be classified as more than one type.
Aerobic Exercise

Aerobic exerciseis any physical activity in which muscles are used at well below their maximum contraction strength, but for long periods of time. Aerobic exercise uses a relatively high percentage of slow-twitch muscle fibres that consume a large amount of oxygen. The main goal of aerobic exercise is to increase cardiovascular endurance, although it can have many other benefits, including muscle toning. Examples of aerobic exercise include cycling, swimming, brisk walking, jumping rope, rowing, hiking, tennis, and kayaking as shown in Figure 12.5.2 .
Anaerobic Exercise
Anaerobic exercise is any physical activity in which muscles are used at close to their maximum contraction strength, but for relatively short periods of time. Anaerobic exercise uses a relatively high percentage of fast-twitch muscle fibres that consume a small amount of oxygen. Goals of anaerobic exercise include building and strengthening muscles, as well as improving bone strength, balance, and coordination. Examples of anaerobic exercise include push-ups, lunges, sprinting, interval training, resistance training, and weight training (such as biceps curls with a dumbbell, as pictured in Figure 12.5.3).

Flexibility Exercise

Flexibility exercise is any physical activity that stretches and lengthens muscles. Goals of flexibility exercise include increasing joint flexibility, keeping muscles limber, and improving the range of motion, all of which can reduce the risk of injury. Examples of flexibility exercise include stretching, yoga (as in Figure 12.5.4), and tai chi.
Health Benefits of Physical Exercise
Many studies have shown that physical exercise is positively correlated with a diversity of health benefits. Some of these benefits include maintaining physical fitness, losing weight and maintaining a healthy weight, regulating digestive health, building and maintaining healthy bone density, increasing muscle strength, improving joint mobility, strengthening the immune system, boosting cognitive ability, and promoting psychological well-being. Some studies have also found a significant positive correlation between exercise and both quality of life and life expectancy. People who participate in moderate to high levels of physical activity have been shown to have lower mortality rates than people of the same ages who are not physically active and daily exercise has been shown to increase life expectancy up to an average of five years.
The underlying physiological mechanisms explaining why exercise has these positive health benefits are not completely understood. However, developing research suggests that many of the benefits of exercise may come about because of the role of skeletal muscles as endocrine organs. Contracting muscles release hormones called myokines, which promote tissue repair and the growth of new tissue. Myokines also have anti-inflammatory effects, which, in turn, reduce the risk of developing inflammatory diseases. Exercise also reduces levels of cortisol, the adrenal cortex stress hormone that may cause many health problems — both physical and mental — at sustained high levels.
Cardiovascular Benefits of Physical Exercise
The beneficial effects of exercise on the cardiovascular system are well documented. Physical inactivity has been identified as a risk factor for the development of coronary artery disease. There is also a direct correlation between physical inactivity and cardiovascular disease mortality. Physical exercise, in contrast, has been demonstrated to reduce several risk factors for cardiovascular disease, including hypertension (high blood pressure), “bad” cholesterol (low-density lipoproteins), high total cholesterol, and excess body weight. Physical exercise has also been shown to increase “good” cholesterol (high-density lipoproteins), insulin sensitivity, the mechanical efficiency of the heart, and exercise tolerance, which is the ability to perform physical activity without undue stress and fatigue.
Cognitive Benefits of Physical Exercise
Physical exercise has been shown to help protect people from developing neurodegenerative disorders, such as dementia. A 30-year study of almost 2,400 men found that those who exercised regularly had a 59 per cent reduction in dementia when compared with those who did not exercise. Similarly, a review of cognitive enrichment therapies for the elderly found that physical activity — in particular, aerobic exercise — can enhance the cognitive function of older adults. Anecdotal evidence suggests that frequent exercise may even help reverse alcohol-induced brain damage. There are several possible reasons why exercise is so beneficial for the brain. Physical exercise:
- Increases blood flow and oxygen availability to the brain.
- Increases growth factors that promote new brain cells and new neuronal pathways in the brain.
- Increases levels of neurotransmitters (such as serotonin), which increase memory retention, information processing, and cognition.
Mental Health Benefits of Physical Exercise
Numerous studies suggest that regular aerobic exercise works as well as pharmaceutical antidepressants in treating mild-to-moderate depression. A possible reason for this effect is that exercise increases the biosynthesis of at least three neurochemicals that may act as euphoriants. The euphoric effect of exercise is well known. Distance runners may refer to it as “runner’s high,” and people who participate in crew (as in Figure 12.5.5) may refer to it as “rower’s high.” Because of these effects, health care providers often promote the use of aerobic exercise as a treatment for depression.

Additional mental health benefits of physical exercise include reducing stress, improving body image, and promoting positive self-esteem. Conversely, there is evidence to suggest that being sedentary is associated with increased risk of anxiety.
Sleep Benefits of Physical Exercise
A recent review of published scientific research suggests that exercise generally improves sleep for most people, and helps sleep disorders, such as insomnia. In fact, exercise is the most recommended alternative to sleeping pills for people with insomnia. For sleep benefits, the optimum time to exercise may be four to eight hours before bedtime, although exercise at any time of day seems to be beneficial. The only possible exception is heavy exercise undertaken shortly before bedtime, which may actually interfere with sleep.
Other Benefits of Physical Exercise
Some studies suggest that physical activity may benefit the immune system. For example, moderate exercise has been found to be associated with a decreased incidence of upper respiratory tract infections. Evidence from many studies has found a correlation between physical exercise and reduced death rates from cancer, specifically breast cancer and colon cancer. Physical exercise has also been shown to reduce the risk of type 2 diabetes and obesity.
Variation in Responses to Physical Exercise

Not everyone benefits equally from physical exercise. When participating in aerobic exercise, most people will have a moderate increase in their endurance, but some people will as much as double their endurance. Some people, on the other hand, will show little or no increase in endurance from aerobic exercise. Genetic differences in slow-twitch and fast-twitch skeletal muscle fibres may play a role in these different results. People with more slow-twitch fibres may be able to develop greater endurance, because these muscle fibres have more capillaries, mitochondria, and myoglobin than fast-twitch fibres. As a result, slow-twitch fibres can carry more oxygen and sustain aerobic activity for a longer period of time than fast-twitch fibres. Studies show that endurance athletes (like the marathoner pictured in Figure 12.5.6) generally do tend to have a higher proportion of slow-twitch fibres than other people.
There is also great variation in individual responses to muscle building as a result of anaerobic exercise. Some people have a much greater capacity to increase muscle size and strength, whereas other people never develop large muscles, no matter how much they exercise them. People who have more fast-twitch than slow-twitch muscle fibres may be able to develop bigger, stronger muscles, because fast-twitch muscle fibres contribute more to muscle strength and have greater potential to increase in mass. Evidence suggests that athletes who excel at power activities (such as throwing and jumping) tend to have a higher proportion of fast-twitch fibres than do endurance athletes.
Can You “Overdose” on Physical Exercise?
Is it possible to exercise too much? Can too much exercise be harmful? Evidence suggests that some adverse effects may occur if exercise is extremely intense and the body is not given proper rest between exercise sessions. Athletes who train for multiple marathons have been shown to develop scarring of the heart and heart rhythm abnormalities. Doing too much exercise without prior conditioning also increases the risk of injuries to muscles and joints. Damage to muscles due to overexertion is often seen in new military recruits (see Figure 12.5.7). Too much exercise in females may cause amenorrhea, which is a cessation of menstrual periods. When this occurs, it generally indicates that a woman is pushing her body too hard.

Many people develop delayed onset muscle soreness (DOMS), which is pain or discomfort in muscles that is felt one to three days after exercising, and generally subsides two or three days later. DOMS was once thought to be caused by the buildup of lactic acid in the muscles. Lactic acid is a product of anaerobic respiration in muscle tissues. However, lactic acid disperses fairly rapidly, so it is unlikely to explain pain experienced several days after exercise. The current theory is that DOMS is caused by tiny tears in muscle fibres, which occur when muscles are used at too high a level of intensity.
Feature: My Human Body
Most people know that exercise is important for good health, and it’s easy to find endless advice about exercise programs and fitness plans. What is not so easy to find is the motivation to start exercising — and to stick with it. This is the main reason why so many people fail to get regular exercise. Practical concerns like a busy schedule and bad weather can certainly make exercising more of a challenge, but the biggest barriers to adopting a regular exercise routine are mental. If you want to exercise but find yourself making excuses or getting discouraged and giving up, here are some tips that may help you get started and stay moving:
- Avoid an all-or-nothing point of view. Don’t think you need to spend hours sweating at the gym or training for a marathon to get healthy. Even a little bit of exercise is better than nothing at all. Start out with ten or 15 minutes of moderate activity each day. Taking a walk around your neighborhood is a great way to begin! From there, gradually increase the amount of time until you are exercising to at least 30 minutes a day, five days a week. Make it a routine.
- Be kind to yourself, and reinforce positive behaviors with rewards. Don’t be down on yourself because you are overweight or out of shape. Don’t beat yourself up because of a supposed lack of willpower. Instead, look at any past failures as opportunities to learn and do better. When you do achieve even small exercise goals, treat yourself to something special. Did you just complete your first workout? Reward yourself with a relaxing bath or other treat.
- Don’t make excuses for not exercising. Common complaints include being too busy or tired or not athletic enough. Such excuses are not valid reasons to avoid exercising, and they will sabotage any plans to improve your fitness. If you can’t find a 30-minute period to work out, try to find ten minutes, three times a day. If you’re feeling tired, know that exercise can actually reduce fatigue and boost your energy level. If you feel clumsy and uncoordinated, remind yourself that you don’t need to be athletic to take a walk or engage in vigorous house or yard work.
- Find an activity that you truly enjoy doing. Don’t think you have to lift weights or run on a treadmill to exercise your muscles. If you find such activities boring or unpleasant, you won’t stick with them. Any activity that increases your heart rate and uses large muscles can provide a workout, especially if you’re not in the habit of exercising, so find something you like to do. Do you like to dance? Put on some music and dance up a sweat! Do you enjoy gardening? Get out in the yard and dig up some dirt! Still not interested? Try an activity-based video game, such as Wii or Kinect. You may find it so much fun that it doesn’t seem like exercise until you realize you’ve worked up a sweat.
- Make yourself accountable. Tell friends and family members that you’re going to start exercising. You’ll be letting them — as well as yourself — down if you don’t follow through. Some people find that keeping an exercise log to track their progress is a good way to be accountable and stick to an exercise program. Perhaps the best way to keep at it is to find an exercise partner. If you’ve got someone waiting to exercise with you, you will be less likely to make excuses for not exercising.
- Add more physical activity to your daily life. You don’t need to follow a structured exercise program to increase your activity level. Do your house or yard work briskly for a workout. Park your car further than necessary from work or the mall, and walk the extra distance. If you live close enough, leave the car at home and walk to and from your destination. Rather than taking elevators or escalators, walk up and down stairs. When you take breaks at work, take a walk instead of sitting. Every time a commercial comes on while you’re watching TV, take a quick exercise break — run in place or do some curls with hand weights.
12.5 Summary
- Physical exercise is any bodily activity that enhances or maintains physical fitness and overall health. Activities such as household chores may count as physical exercise, even if they are not done for their health benefits. Current recommendations for adults are 30 minutes a day of moderate exercise.
- Aerobic exercise is any physical activity that uses muscles at less than their maximum contraction strength, but for long periods of time. This type of exercise uses a relatively high percentage of slow-twitch muscle fibres that consume large amounts of oxygen. Aerobic exercises increase cardiovascular endurance and include cycling and brisk walking.
- Anaerobic exercise is any physical activity that uses muscles at close to their maximum contraction strength, but for short periods of time. This type of exercise uses a relatively high percentage of fast-twitch muscle fibres that consume small amounts of oxygen. Anaerobic exercises increase muscle and bone mass and strength, and they include push-ups and sprinting.
- Flexibility exercise is any physical activity that stretches and lengthens muscles, thereby improving range of motion and reducing risk of injury. Examples include stretching and yoga.
- Many studies have shown that physical exercise is positively correlated with a diversity of physical, mental, and emotional health benefits. Physical exercise also increases quality of life and life expectancy.
- Many of the benefits of exercise may come about because contracting muscles release hormones called myokines, which promote tissue repair and growth and have anti-inflammatory effects.
- Physical exercise can reduce risk factors for cardiovascular disease, including hypertension and excess body weight. Physical exercise can also increase factors associated with cardiovascular health, such as mechanical efficiency of the heart.
- Physical exercise has been shown to offer protection from dementia and other cognitive problems, perhaps because it increases blood flow or neurotransmitters in the brain, among other potential effects.
- Numerous studies suggest that regular aerobic exercise works as well as pharmaceutical antidepressants in treating mild-to-moderate depression, possibly because it increases synthesis of natural euphoriants in the brain.
- Research shows that physical exercise generally improves sleep for most people and helps sleep disorders, such as insomnia. Other health benefits of physical exercise include better immune system function and reduced risk of type 2 diabetes and obesity.
- There is great variation in individual responses to exercise, partly due to genetic differences in proportions of slow-twitch and fast-twitch skeletal muscle fibres. People with more slow-twitch fibres may be able to develop greater endurance from aerobic exercise, whereas people with more fast-twitch fibres may be able to develop greater muscle size and strength from anaerobic exercise.
- Some adverse effects may occur if exercise is extremely intense and the body is not given proper rest between exercise sessions. Many people who overwork their muscles develop delayed onset muscle soreness (DOMS), which may be caused by tiny tears in muscle fibres.
12.5 Review Questions
- How do we define physical exercise?
- What are current recommendations for physical exercise for adults?
-
- Define flexibility exercise, and state its benefits. What are two examples of flexibility exercises?
- In general, how does physical exercise affect health, quality of life, and longevity?
- What mechanism may underlie many of the general health benefits of physical exercise?
- Relate physical exercise to cardiovascular disease risk.
- What may explain the positive benefits of physical exercise on cognition?
- How does physical exercise compare with antidepressant drugs in the treatment of depression?
- Identify several other health benefits of physical exercise.
- Explain how genetics may influence the way individuals respond to physical exercise.
- Can too much physical exercise be harmful?
12.5 Explore More
https://www.youtube.com/watch?v=hmFQqjMF_f0
How playing sports benefits your body ... and your brain - Leah Lagos and Jaspal Ricky Singh, TED-Ed, 2016.
https://www.youtube.com/watch?v=rLsimrBoYXc&t=12s
The surprising reason our muscles get tired - Christian Moro, TED-Ed, 2019.
https://youtu.be/2tM1LFFxeKg
What makes muscles grow? - Jeffrey Siegel, TED-Ed, 2015.
https://www.youtube.com/watch?v=QeIrdqU0o9s
Why some people find exercise harder than others | Emily Balcetis, TED, 2014.
Attributions
Figure 12.5.1
stroller fit by Serge Melki from Indianapolis, USA on Wikimedia Commons is used under a CC BY 2.0 (https://creativecommons.org/licenses/by/2.0) license.
Figure 12.5.2
Children kayaking young sport by Hagerty Ryan, USFWS on Pixnio is used under a public domain (CC0) Certification (https://creativecommons.org/licenses/publicdomain/).
Figure 12.5.3
Bicep curls [photo] by Senior Airman Jarrod Grammel from U.S. Moody Air Force Base is released into the public domain (https://en.wikipedia.org/wiki/Public_domain).
Figure 12.5.4
Flexibility exercise by carl-barcelo-nqUHQkuVj3c [photo] by Carl Barcelo on Unsplash is used under the Unsplash License (https://unsplash.com/license).
Figure 12.5.5
Canadian women’s double scull silver Rio 2016 by Gerhard Pratt on Flickr is used under a CC BY-NC 2.0 (https://creativecommons.org/licenses/by-nc/2.0/) license.
Figure 12.5.6
Toronto Marathon 2012 by Marc Roberts on Flickr is used under a CC BY-NC-SA 2.0 (https://creativecommons.org/licenses/by-nc-sa/2.0/) license.
Figure 12.5.7
Muscle damage in military recruits by Lance Cpl. Bridget M. Keane from the United States Marine Corps Recruit Depot is in the public domain (https://en.wikipedia.org/wiki/Public_domain).
References
Elwood, P., Galante, J., Pickering, J., Palmer, S., Bayer, A., Ben-Shlomo, Y., Longley, M., & Gallacher, J. (2013). Healthy lifestyles reduce the incidence of chronic diseases and dementia: evidence from the Caerphilly cohort study. PloS one, 8(12), e81877. https://doi.org/10.1371/journal.pone.0081877
Mayo Clinic Staff. (n.d.). Amenorrhea [online article]. MayoClinic.org. https://www.mayoclinic.org/diseases-conditions/amenorrhea/symptoms-causes/syc-20369299#
Mayo Clinic Staff. (n.d.). Coronary artery disease [online article]. MayoClinic.org. https://www.mayoclinic.org/diseases-conditions/coronary-artery-disease/symptoms-causes/syc-20350613
TED-Ed. (2016, June 28). How playing sports benefits your body ... and your brain - Leah Lagos and Jaspal Ricky Singh. YouTube. https://www.youtube.com/watch?v=hmFQqjMF_f0&feature=youtu.be
TED-Ed. (2019, April 18). The surprising reason our muscles get tired - Christian Moro. YouTube. https://www.youtube.com/watch?v=rLsimrBoYXc&feature=youtu.be
TED-Ed. (2015, November 3). What makes muscles grow? - Jeffrey Siegel. YouTube https://www.youtube.com/watch?v=2tM1LFFxeKg&feature=youtu.be
TED. (2014, November 14). Why some people find exercise harder than others | Emily Balcetis, YouTube. https://www.youtube.com/watch?v=QeIrdqU0o9s&feature=youtu.be
Wikipedia contributors. (2020, August 1). Delayed onset muscle soreness. In Wikipedia. https://en.wikipedia.org/w/index.php?title=Delayed_onset_muscle_soreness&oldid=970682631
Image shows a diagram of locations in the body where the effects of anemia are experienced. Some of these include: Central nervous system: fatigue, dizziness and possibly fainting. Low blood pressure. In the heart: heart palpitations, rapid heart rate, chest palpitations, in extreme cases chest pain, angina and heart attack. Enlargement of the spleen. Changed stool (poo) colour. Muscular weakness. Shortness of breath. Pale, cold and/or yellowing skin. Yellowing eyes.
Created by: CK-12/Adapted by Christine Miller

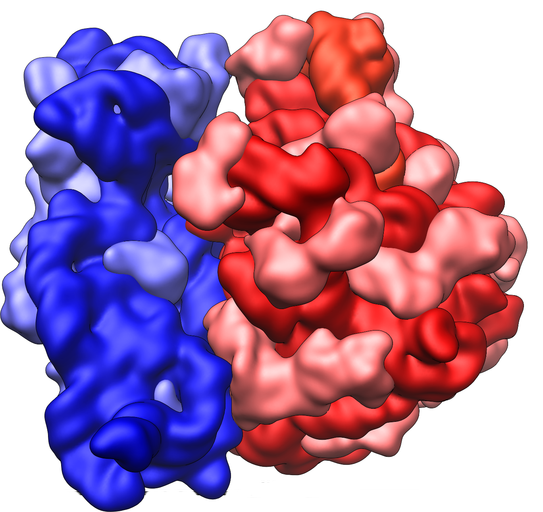
Ribosome Review
The 25-metre long sculpture shown in Figure 4.6.1 is a recognition of the beauty of one of the metabolic functions that takes place in the cells in your body. This artwork brings to life an important structure in living cells: the ribosome, the cell structure where proteins are synthesized. The slender silver strand is the messenger RNA(mRNA) bringing the code for a protein out into the cytoplasm. The purple and green structures are ribosomal subunits (which together form a single ribosome), which can "read" the code on the mRNA and direct the bonding of the correct sequence of amino acids to create a protein. All living cells — whether they are prokaryotic or eukaryotic — contain ribosomes, but only eukaryotic cells also contain a nucleus and several other types of organelles.
What Are Organelles?
An organelle is a structure within the cytoplasm of a eukaryotic cell that is enclosed within a membrane and performs a specific job. Organelles are involved in many vital cell functions. Organelles in animal cells include the nucleus, mitochondria, endoplasmic reticulum, Golgi apparatus, vesicles, and vacuoles. Ribosomes are not enclosed within a membrane, but they are still commonly referred to as organelles in eukaryotic cells.
The Nucleus
The nucleus is the largest organelle in a eukaryotic cell, and it's considered the cell’s control center. It contains most of the cell’s DNA(which makes up chromosomes), and it is encoded with the genetic instructions for making proteins. The function of the nucleus is to regulate gene expression, including controlling which proteins the cell makes. In addition to DNA, the nucleus contains a thick liquid called nucleoplasm, which is similar in composition to the cytosol found in the cytoplasm outside the nucleus. Most eukaryotic cells contain just a single nucleus, but some types of cells (such as red blood cells) contain no nucleus and a few other types of cells (such as muscle cells) contain multiple nuclei.
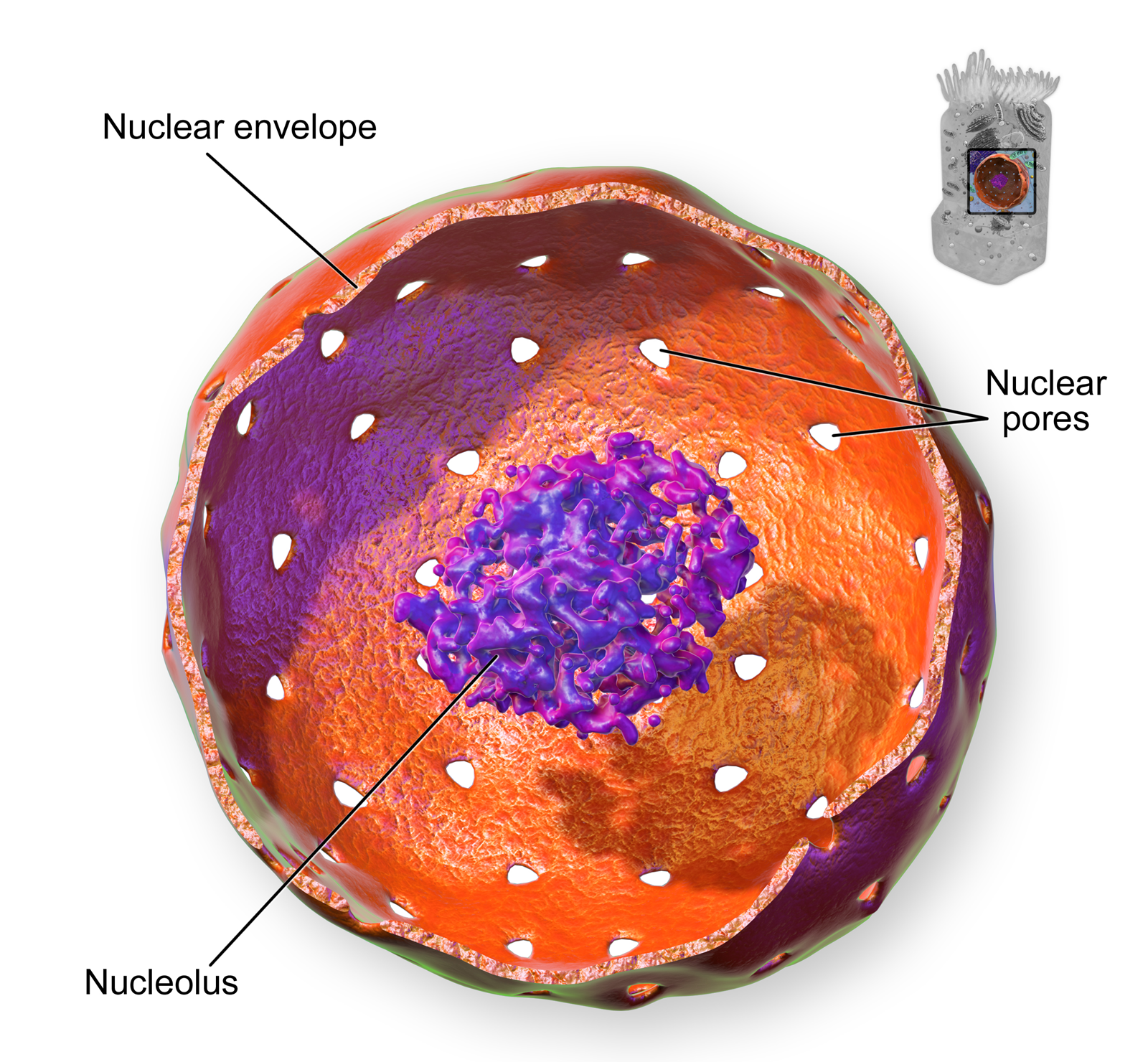
As you can see in the model pictured in Figure 4.6.2, the membrane enclosing the nucleus is called the nuclear envelope. This is actually a double membrane that encloses the entire organelle and isolates its contents from the cellular cytoplasm. Tiny holes called nuclear pores allow large molecules to pass through the nuclear envelope, with the help of special proteins. Large proteins and RNA molecules must be able to pass through the nuclear envelope so proteins can be synthesized in the cytoplasm and the genetic material can be maintained inside the nucleus. The nucleolus shown in the model below is mainly involved in the assembly of ribosomes. After being produced in the nucleolus, ribosomes are exported to the cytoplasm, where they are involved in the synthesis of proteins.
Mitochondria
The mitochondrion (plural, mitochondria) is an organelle that makes energy available to the cell. This is why mitochondria are sometimes referred to as the "power plants of the cell." They use energy from organic compounds (such as glucose) to make molecules of ATP (adenosine triphosphate), an energy-carrying molecule that is used almost universally inside cells for energy.
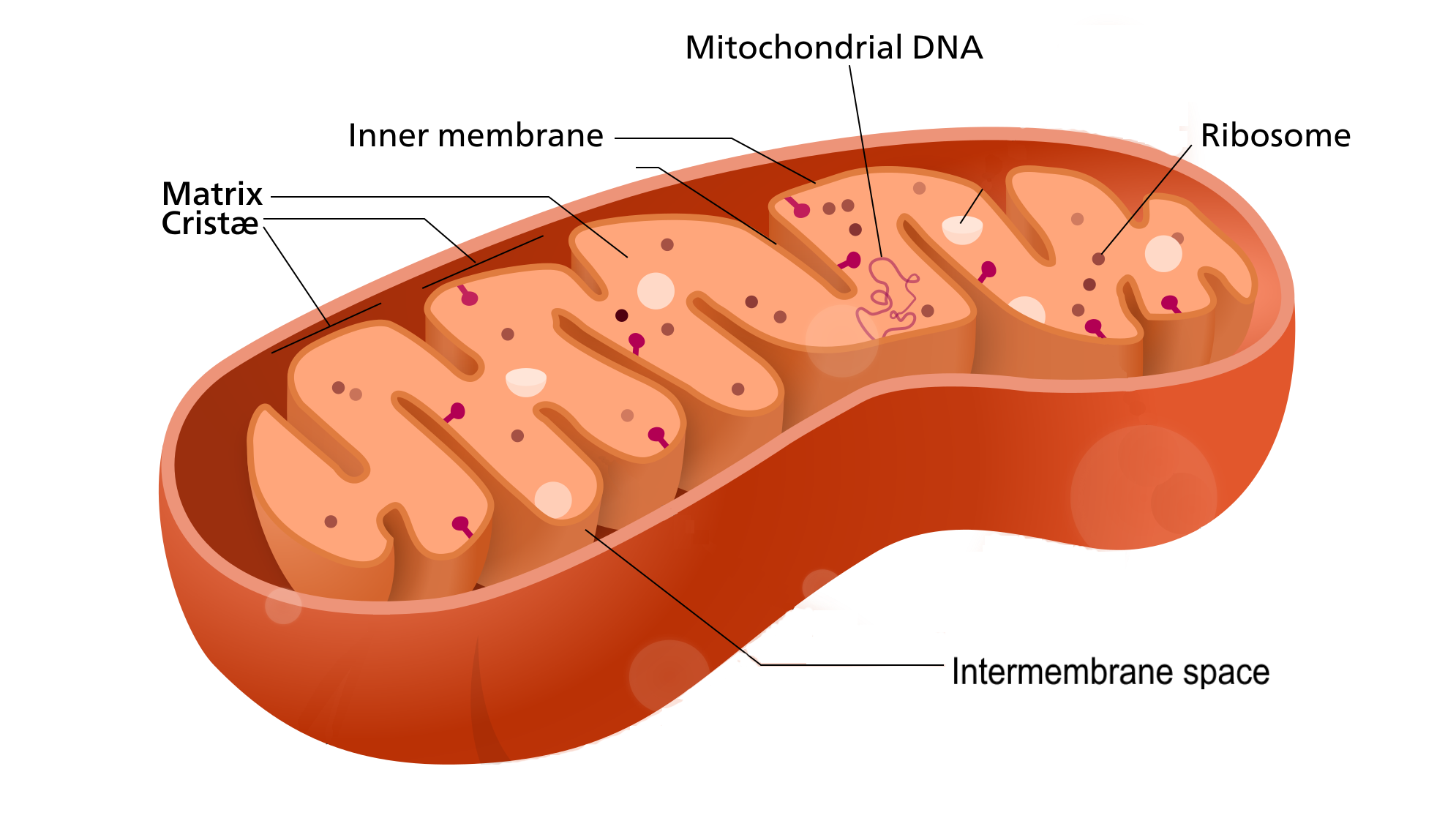
Mitochondria (as in the Figure 4.6.3 diagram) have a complex structure including an inner and out membrane. In addition, mitochondria have their own DNA, ribosomes, and a version of cytoplasm, called matrix. Does this sound similar to the requirements to be considered a cell? That's because they are!
Scientists think that mitochondria were once free-living organisms because they contain their own DNA. They theorize that ancient prokaryotes infected (or were engulfed by) larger prokaryotic cells, and the two organisms evolved a symbiotic relationship that benefited both of them. The larger cells provided the smaller prokaryotes with a place to live. In return, the larger cells got extra energy from the smaller prokaryotes. Eventually, the smaller prokaryotes became permanent guests of the larger cells, as organelles inside them. This theory is called endosymbiotic theory, and it is widely accepted by biologists today. (See the video in section 4.3 to learn all about endosymbiotic theory.)
Endoplasmic Reticulum
The endoplasmic reticulum (ER) is an organelle that helps make and transport proteins and lipids. There are two types of endoplasmic reticulum: rough endoplasmic reticulum (rER) and smooth endoplasmic reticulum (sER). Both types are shown in Figure 4.6.4.
- rER looks rough because it is studded with ribosomes. It provides a framework for the ribosomes, which make proteins. Bits of its membrane pinch off to form tiny sacs called vesicles, which carry proteins away from the ER.
- sER looks smooth because it does not have ribosomes. sER makes lipids, stores substances, and plays other roles.
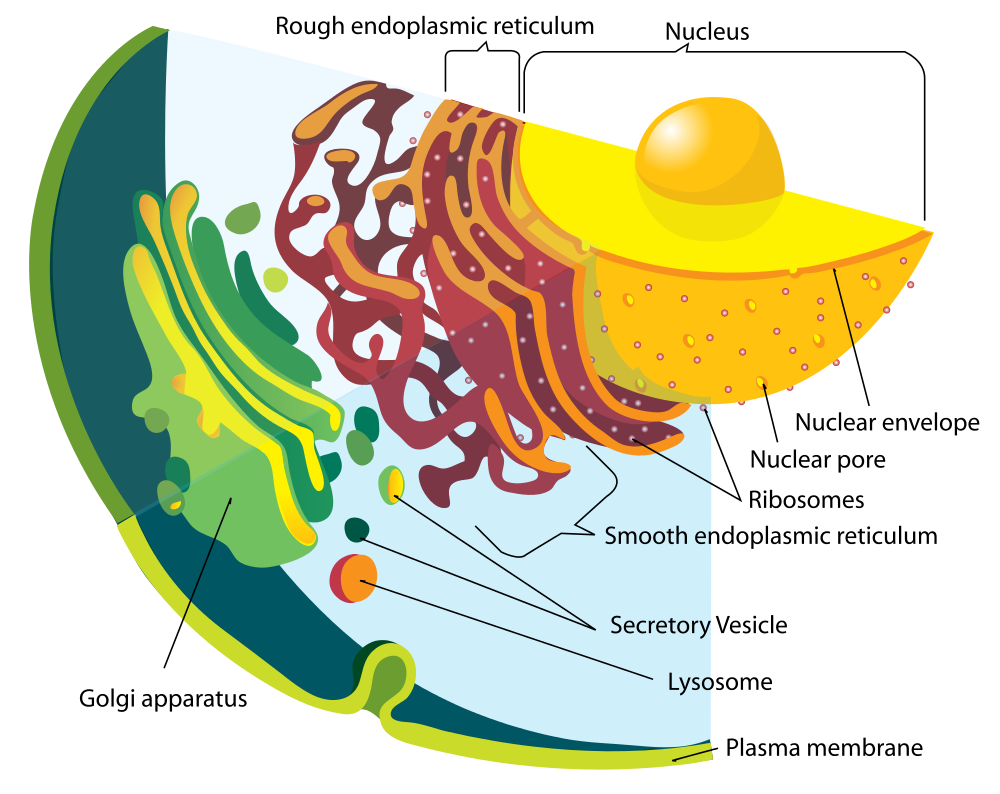
The Figure 4.6.4 drawing includes the nucleus, rER, sER, and Golgi apparatus. From the drawing, you can see how all these organelles work together to make and transport proteins.
Golgi Apparatus
The Golgi apparatus (shown in the Figure 4.6.4 diagram) is a large organelle that processes proteins and prepares them for use both inside and outside the cell. You can see the Golgi apparatus in the figure above. The Golgi apparatus is something like a post office. It receives items (proteins from the ER), then packages and labels them before sending them on to their destinations (to different parts of the cell or to the cell membrane for transport out of the cell). The Golgi apparatus is also involved in the transport of lipids around the cell.
Vesicles and Vacuoles
Both vesicles and vacuoles are sac-like organelles made of phospholipid bilayer that store and transport materials in the cell. Vesicles are much smaller than vacuoles and have a variety of functions. The vesicles that pinch off from the membranes of the ER and Golgi apparatus store and transport protein and lipid molecules. You can see an example of this type of transport vesicle in the Figure 4.6.4. Some vesicles are used as chambers for biochemical reactions.
There are some vesicles which are specialized to carry out specific functions. Lysosomes, which use enzymes to break down foreign matter and dead cells, have a double membrane to make sure their contents don't leak into the rest of the cell. Peroxisomes are another type of specialized vesicle with the main function of breaking down fatty acids and some toxins.
Centrioles
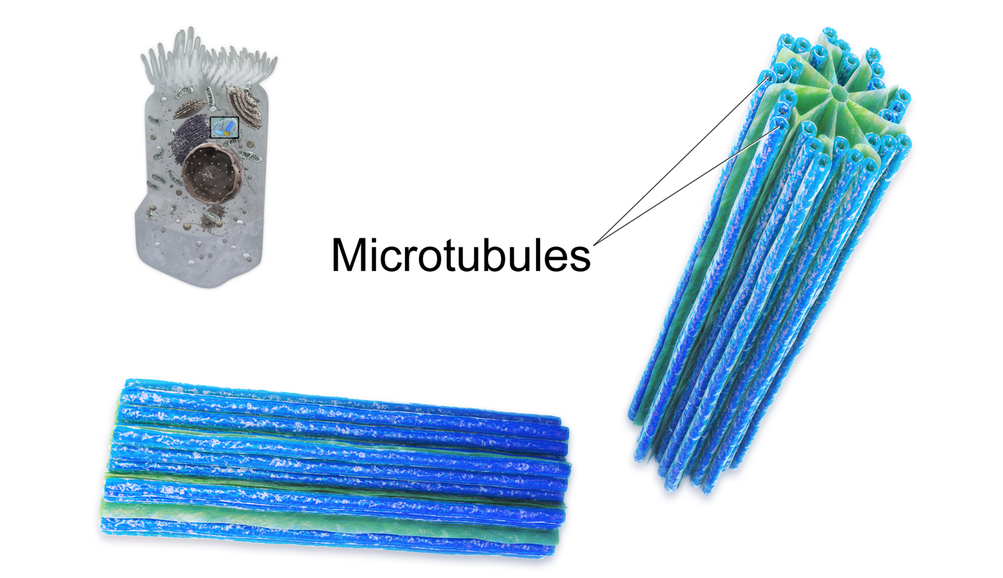
Centrioles are organelles involved in cell division. The function of centrioles is to help organize the chromosomes before cell division occurs so that each daughter cell has the correct number of chromosomes after the cell divides. Centrioles are found only in animal cells, and are located near the nucleus. Each centriole is made mainly of a protein named tubulin. The centriole is cylindrical in shape and consists of many microtubules, as shown in the model pictured in Figure 4.6.5.
Ribosomes
Ribosomes are small structures where proteins are made. Although they are not enclosed within a membrane, they are frequently considered organelles. Each ribosome is formed of two subunits, like the ones pictured at the beginning of this section (Figure 4.6.1) and in Figure 4.6.6. Both subunits consist of proteins and RNA. mRNA from the nucleus carries the genetic code, copied from DNA, which remains in the nucleus. At the ribosome, the genetic code in mRNA is used to assemble and join together amino acids to make proteins. Ribosomes can be found alone or in groups within the cytoplasm, as well as on the rER.
4.6 Summary
- An organelle is a structure within the cytoplasm of a eukaryotic cell that is enclosed within a membrane and performs a specific job. Although ribosomes are not enclosed within a membrane, they are still commonly referred to as organelles in eukaryotic cells.
- The nucleus is the largest organelle in a eukaryotic cell, and it is considered to be the cell's control center. It controls gene expression, including controlling which proteins the cell makes.
- The mitochondrion (plural, mitochondria) is an organelle that makes energy available to the cells. It is like the power plant of the cell. According to the widely accepted endosymbiotic theory, mitochondria evolved from prokaryotic cells that were once free-living organisms that infected or were engulfed by larger prokaryotic cells.
- The endoplasmic reticulum (ER) is an organelle that helps make and transport proteins and lipids. Rough endoplasmic reticulum (rER) is studded with ribosomes. Smooth endoplasmic reticulum (sER) has no ribosomes.
- The Golgi apparatus is a large organelle that processes proteins and prepares them for use both inside and outside the cell. It is also involved in the transport of lipids around the cell.
- Both vesicles and vacuoles are sac-like organelles that may be used to store and transport materials in the cell or as chambers for biochemical reactions. Lysosomes and peroxisomes are special types of vesicles that break down foreign matter, dead cells, or poisons.
- Centrioles are organelles located near the nucleus that help organize the chromosomes before cell division so each daughter cell receives the correct number of chromosomes.
- Ribosomes are small structures where proteins are made. They are found in both prokaryotic and eukaryotic cells. They may be found alone or in groups within the cytoplasm or on the rER.
4.6 Review Questions
- What is an organelle?
- Describe the structure and function of the nucleus.
- Explain how the nucleus, ribosomes, rough endoplasmic reticulum, and Golgi apparatus work together to make and transport proteins.
- Why are mitochondria referred to as the "power plants of the cell"?
- What roles are played by vesicles and vacuoles?
- Why do all cells need ribosomes — even prokaryotic cells that lack a nucleus and other cell organelles?
- Explain endosymbiotic theory as it relates to mitochondria. What is one piece of evidence that supports this theory?
-
4.6 Explore More
https://www.youtube.com/watch?v=URUJD5NEXC8&t=121s
Biology: Cell Structure I Nucleus Medical Media, Nucleus Medical Media, 2015.
https://www.youtube.com/watch?v=Id2rZS59xSE&feature=youtu.be
David Bolinsky: Visualizing the wonder of a living cell, TED, 2007.
Attributes
Figure 4.6.1
Ribosomes at Work by Pedrik on Flickr is used under a CC BY-NC-SA 2.0 (https://creativecommons.org/licenses/by-nc-sa/2.0/) license.
Figure 4.6.2
Nucleus by BruceBlaus on Wikimedia Commons is used under a CC BY 3.0 (https://creativecommons.org/licenses/by/3.0) license.
Figure 4.6.3
Mitochondrion_structure.svg by Kelvinsong; modified by Sowlos on Wikimedia Commons is used and adapted by Christine Miller under a CC BY-SA 3.0 (https://creativecommons.org/licenses/by-sa/3.0) license.
Figure 4.6.4
Endomembrane_system_diagram_en.svg by Mariana Ruiz [LadyofHats] on Wikimedia Commons is released into the public domain (https://en.wikipedia.org/wiki/Public_domain).
Figure 4.6.5
Centrioles by BruceBlaus on Wikimedia Commons is used under a CC BY 3.0 (https://creativecommons.org/licenses/by/3.0) license.
Figure 4.6.6
Ribosome_shape by Vossman on Wikimedia Commons is used and adapted by Christine Miller under a CC BY-SA 3.0 (https://creativecommons.org/licenses/by-sa/3.0) license.
References
Blausen.com staff. (2014). Nucleus - Medical gallery of Blausen Medical 2014. WikiJournal of Medicine 1 (2). DOI:10.15347/wjm/2014.010. ISSN 2002-4436. https://en.wikiversity.org/wiki/WikiJournal_of_Medicine/Medical_gallery_of_Blausen_Medical_2014
Blausen.com staff (2014). Centrioles - Medical gallery of Blausen Medical 2014. WikiJournal of Medicine 1 (2). DOI:10.15347/wjm/2014.010. ISSN 2002-4436.https://en.wikiversity.org/wiki/WikiJournal_of_Medicine/Medical_gallery_of_Blausen_Medical_2014
Nucleus Medical Media. (2015, March 18). Biology: Cell structure I Nucleus Medical Media. YouTube. https://www.youtube.com/watch?v=URUJD5NEXC8&feature=youtu.be
TED. (2007, July 24). David Bolinsky: Visualizing the wonder of a living cell. YouTube. https://www.youtube.com/watch?v=Id2rZS59xSE&feature=youtu.be
A signal transmitted along a nerve fiber.
Created by CK-12 Foundation/Adapted by Christine Miller

Fertility Symbol
The geometric design on the ancient stone carving in Figure 18.6.1 represents a powerful symbol of female fertility: the vagina. The symbol is called yoni in Hindu, and it reflects the value placed by Hindu culture on the ability of females to give birth. The vagina is one of several organs in the female reproductive system.
Female Reproductive Organs
The female reproductive system is made up of internal and external organs that function to produce haploid female gametes called ova (or oocytes), secrete female sex hormones (such as estrogen), and carry and give birth to a fetus. The internal female reproductive organs include the vagina, uterus, oviducts, and ovaries. The external organs — collectively called the vulva — include the clitoris and labia.
The vagina is an elastic, muscular canal leading from its opening in the vulva to the neck of the uterus, called the cervix. It is about 7.5 cm (about 3 in) long at the front, and about 9 cm (3.5 in) long at the back. The vagina accommodates the penis and is the site where sperm are usually ejaculated during sexual intercourse. In the context of pregnancy and natural (vaginal) childbirth, the vagina is referred to as the birth canal. In addition, it channels the flow of menstrual blood from the uterus.
Structure of the Vagina
Muscles and ligaments support the vagina within the pelvic cavity. The vagina itself is made up of several layers of fibrous and muscular tissues and lined with mucous membranes. Folds in the mucosa provide the vagina with extra surface area so it can stretch in both length and width during intercourse or childbirth. The elasticity of the vagina and the extra mucosa allow it to stretch to many times its normal diameter in order to deliver a baby.
Bacteria and pH in the Vagina
A healthy vagina is home to many symbiotic bacteria that help prevent pathogens (such as yeast) from colonizing the vagina. The pH in the vagina is normally between 3.8 and 4.5, and this acidity also helps keep pathogenic microorganisms from colonizing it. The vagina constantly sheds its epithelium, so it is considered self-cleaning. As a consequence, there is no need for douching to clean it. Physicians actually discourage the practice, as it may upset the normal bacterial and pH balance in the vagina, although washing the vulva with a mild soap is good practice.
Uterus
The uterus (commonly called the womb) is a pear-shaped, muscular organ that is about 7.6 cm (about 3 in) long. It is located above the vagina and behind the bladder in the centre of the pelvis. The position of the uterus in the pelvis is stabilized by several ligaments and bands of supportive tissue. The uterus is where a fetus develops during gestation, and the organ provides mechanical protection and support for the developing offspring. Contractions of the muscular wall of the uterus are responsible for pushing the fetus out of the uterus during childbirth.
Parts of the Uterus
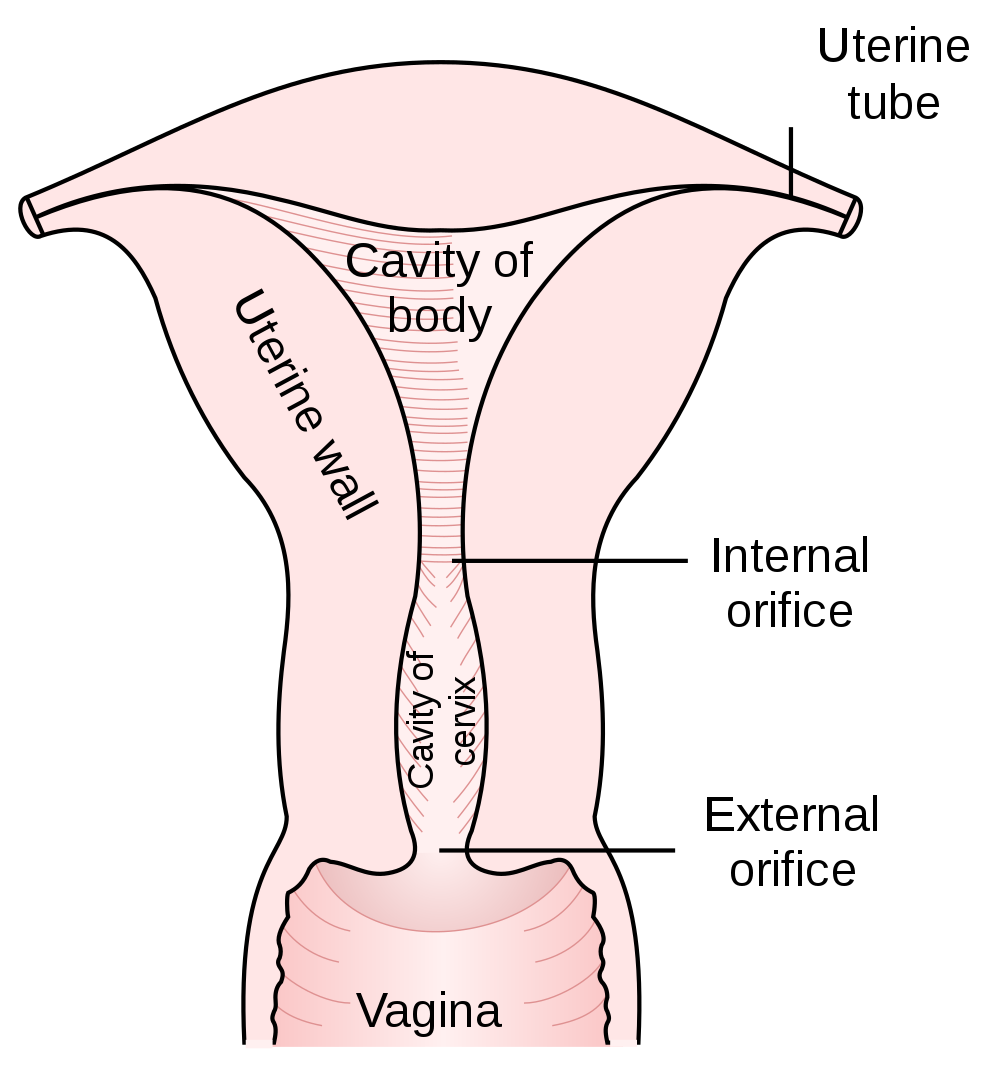
As shown in Figure 18.6.2, the lower end of the uterus forms the cervix, which is also called the neck of the uterus. The cervix is about 2.5 cm (almost 1 in) long and protrudes downward into the vagina. A small canal runs the length of the cervix, connecting the uterine cavity with the lumen of the vagina. This allows semen deposited in the vagina to enter the uterus, and a baby to pass from the uterus into the vagina during birth. Glands in the cervix secrete mucus that varies in water content and thickness, so it can function either as a barrier to keep microorganisms out of the uterus during pregnancy, or as a transport medium to help sperm enter the uterus around the time of ovulation. The rest of the uterus above the cervix is called the body of the uterus. The upper end of the uterus is connected with the two oviducts.
Tissues of the Uterus
As indicated in Figure 18.6.3, the uterus consists of three tissue layers, called the endometrium, myometrium, and perimetrium.
- The endometrium is the innermost tissue layer of the uterus. It consists of epithelial tissue, including mucous membranes. This layer thickens during each menstrual cycle and, unless an egg is fertilized, sloughs off during the following menstrual period. If an ovum is fertilized, the thickened endometrium is maintained by hormones and provides nourishment to the embryo. As gestation progresses, the endometrium develops into the maternal portion of the placenta.
- The placenta is a temporary organ that consists of a mass of maternal and fetal blood vessels through which the mother’s and fetus’s blood exchange substances.
- The myometrium is the middle layer of the uterus. It consists mostly of a thick layer of smooth muscle tissue. Powerful contractions of the smooth muscle allow the uterus to contract and expel an infant during childbirth.
- The perimetrium is the outermost layer of the uterus. It covers the outer surface of the uterus. This layer actually consists of two layers of epithelium that secrete fluid into the space between them. The fluid allows for small movements of the uterus within the pelvis, without causing it to rub against other organs.
Oviducts
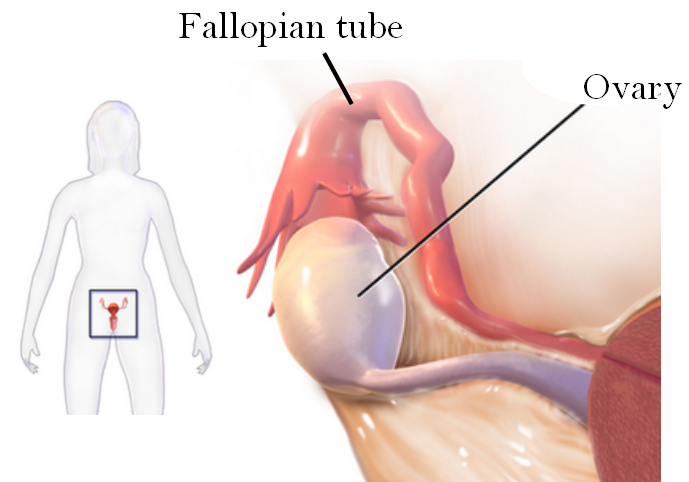
The oviducts (often referred to as Fallopian tubes) are two thin tubes that lie between the ovaries and the uterus. The oviducts are not attached to the ovaries, but their broad upper ends — called infundibula — lie very close to the ovaries. The infundibula also have fringe-like extensions called fimbriae that move in a waving motion to help guide eggs from the ovaries into the oviducts. The lower ends of the oviducts are attached to the upper part of the body of the uterus on either side of the body. They open into the uterus.
The oviducts are made up of multiple tissue layers. The innermost layer consists of mucosal epithelium. The epithelium is covered with cilia, which can move in a sweeping motion to help ova move through the tube from the ovary to the uterus. In between the ciliated cells of the epithelium are cells that secrete a fluid called tubular fluid. This fluid contains nutrients for sperm, ova, and zygotes. The secretions in tubular fluid also remove certain molecules from the plasma membrane of sperm so they are better able to penetrate an egg. Other layers of the oviducts consist of connective tissue and smooth muscle. Contractions of the smooth muscle allow peristalsis to help move eggs through the tubes.
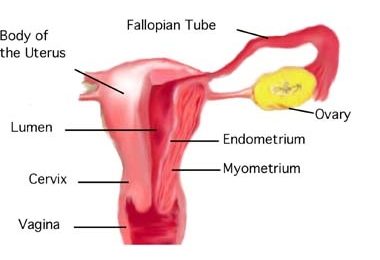
Ovaries
Like the testes in males, the ovaries in females are gonads that produce gametes and secrete sex hormones. The gametes produced by the ovaries are called ova, or oocytes. The main sex hormone secreted by the ovaries is estrogen. The position of the paired ovaries relative to the other reproductive system organs is shown in Figure 18.6.4. Each ovary lies along one side of the uterus and is about 4 cm (a little more than 1.5 in) long. Fibrous ligaments attach one end of each ovary to its nearby oviduct and the other and to its side of the uterus. These ligaments keep the ovaries in place within the pelvis.
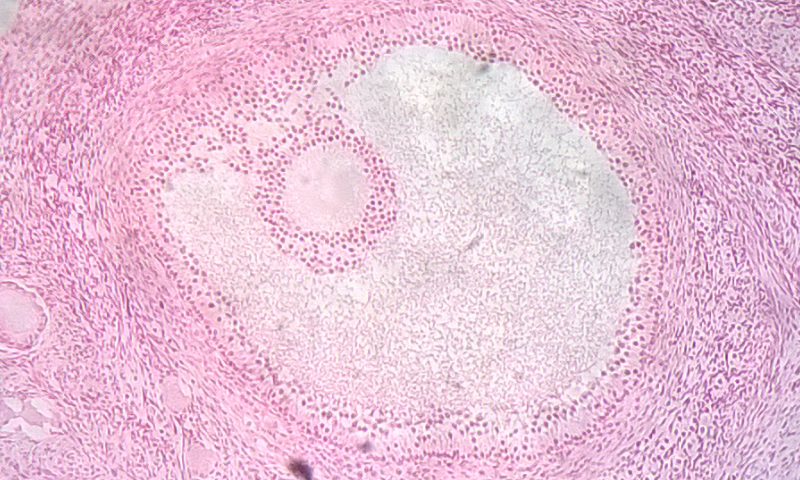
Ovarian Follicles
The ovary consists of two main layers, called the ovarian medulla (the inner layer) and the ovarian cortex (the outer layer). The ovary also contains blood and lymphatic vessels. The ovarian cortex consists primarily of the functional units of the ovaries, which are called ovarian follicles. The follicles are nests of epithelial cells, within each of which is an ovum. The photomicrograph in Figure 18.6.5 shows an ovarian follicle and the developing ovum inside it. If an ovum and follicle complete maturation, the follicle ruptures and the ovum is released from the ovary. This event is called ovulation.
Ova in the Ovaries
Whereas the male testes produce sperm continuously after puberty, the female ovary already contains all the ova it will ever produce by the time a female is born. At birth, a baby girl’s ovaries contain at least a million eggs, each of which is contained within a follicle. Only about 500 of these eggs will eventually mature and be ovulated. This process starts at puberty and typically continues at monthly intervals until menopause occurs around age 52. The remaining eggs never mature, and their number declines as the woman ages. By menopause, a woman’s reserve of eggs is nearly depleted, and ovulation no longer occurs.
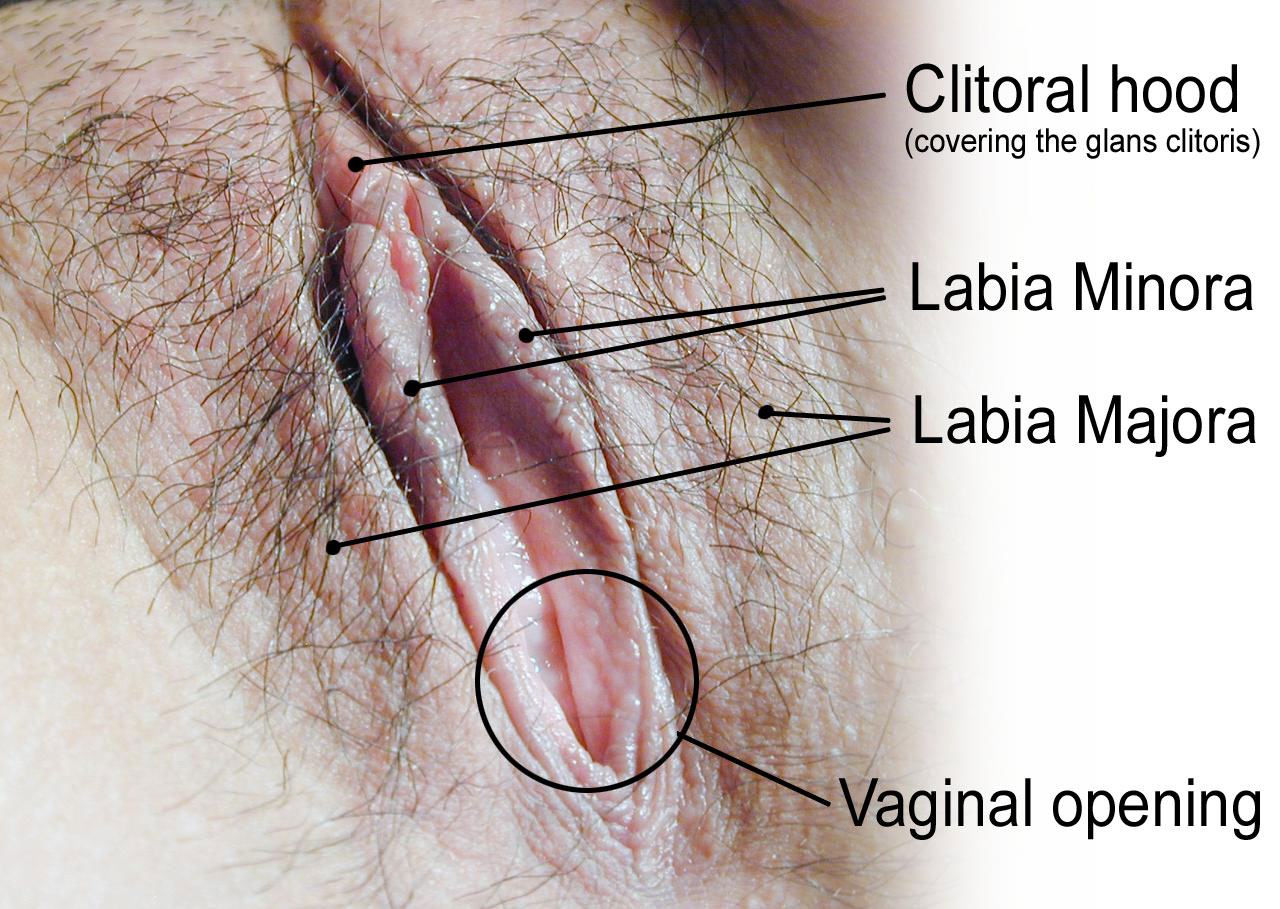
Vulva
The vulva is a general term for all of the external female reproductive organs. The vulva includes the clitoris, labia, and external openings for the urethra and vagina.
Labia
The labia (singular, labium) refer to the “lips” of the vulva, which are folds of tissue that contain and protect the other, more delicate structures of the vulva (as shown in Figure 18.6.6). There are two pairs of labia: the outer and larger labia majora, and the inner and smaller labia minora. The labia minora contain numerous sebaceous glands. These glands release secretions that help lubricate the labia and vulvar area.
Clitoris
The clitoris, is located at the front of the vulva where the labia minora meet. The visible portion of the clitoris is called the glans clitoris. It is roughly the size and shape of a pea. It is highly sensitive, because it contains many nerve endings. A hood of tissue called the clitoral hood (shown in Figure 18.6.5 above), or prepuce, normally covers and protects the clitoris. The clitoris is the homologue to the male penis, and they both contain spongy tissue. Stimulation of the glans clitoris during sexual activity generally results in sexual arousal in females, and may lead to orgasm. The glans clitoris is the only part of the overall clitoris visible externally, but this spongy tissue extends down either side of the openings to the urethra and vagina, as seen in Figure 18.6.7.
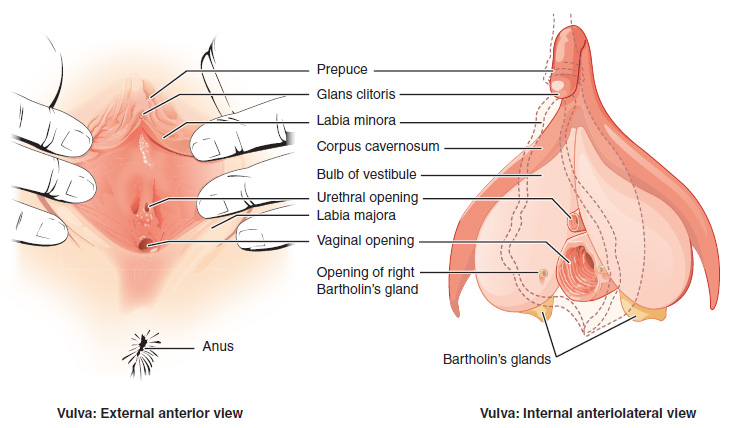
Other Vulvar Structures
The area between the two labia minora is called the vestibule of the vulva. Both the urethra and vagina have openings to the outside of the body in the vestibule. As you can see in Figure 18.6.7 above, the urethral opening (or meatus) is located just in front of, and is much smaller than, the vaginal opening. Both openings are protected by the labia. Two glands — called Bartholin’s glands — open on either side of the vaginal opening. These glands secrete mucus and a vaginal and vulvar lubricant.
Breasts
The breasts are not directly involved in reproduction, but because they contain mammary glands, they can provide nourishment to an infant after birth. The breasts overlay major muscles in the chest from which they project outward in a conical shape. The two main types of tissues in the breast are adipose (fat) tissue and glandular tissue that produces milk. As shown in Figure 18.6.8, each mature breast contains many lobules, where milk is produced and stored during pregnancy. During breastfeeding (or lactation), the milk drains into ducts and sacs, which in turn converge at the nipple. Milk exits the breast through the nipple in response to the suckling action of an infant and is regulated by a positive feedback loop. The nipple is surrounded by a more darkly pigmented area called the areola. The areola contains glands that secrete an oily fluid, which lubricates and protects the nipple during breastfeeding.
18.6 Summary
- The female reproductive system is made up of internal and external organs that function to produce haploid female gametes called ova, secrete female sex hormones (such as estrogen), and carry and give birth to a fetus.
- The vagina is an elastic, muscular canal that can accommodate the penis. It is also where sperm are usually ejaculated during sexual intercourse. The vagina is the birth canal, and it channels the flow of menstrual blood from the uterus. A healthy vagina has a balance of symbiotic bacteria and an acidic pH.
- The uterus is a muscular organ above the vagina where a fetus develops. Its muscular walls contract to push out the fetus during childbirth. The cervix is the neck of the uterus that extends down into the vagina. It contains a canal connecting the vagina and uterus for sperm, or for an infant to pass through. The innermost layer of the uterus — the endometrium — thickens each month in preparation for an embryo, but is shed in the following menstrual period if fertilization does not occur.
- The oviducts extend from the uterus to the ovaries. Waving fimbriae at the ovary ends of the oviducts guide ovulated eggs into the tubes where fertilization may occur as the ova travel to the uterus. Cilia and peristalsis help ova move through the tubes. Tubular fluid helps nourish sperm as they swim up the tubes toward ova.
- The ovaries are gonads that produce ova and secrete sex hormones, including estrogen. Nests of cells called follicles in the ovarian cortex are the functional units of ovaries. Each follicle surrounds an immature ovum. At birth, a baby girl’s ovaries contain at least a million ova, and they will not produce any more during her lifetime. During a woman’s reproductive years, one ova typically matures and is ovulated each month.
- The vulva is a general term for external female reproductive organs. The vulva includes the clitoris, two pairs of labia, and openings for the urethra and vagina. Secretions from mucosal glands near the vaginal opening lubricate the vulva.
- The breasts are not technically reproductive organs, but their mammary glands produce milk to feed an infant after birth. Milk drains through ducts and sacs, and out through the nipple when a baby sucks during breastfeeding.
18.6 Review Questions
-
- State the general functions of the female reproductive system.
- Describe the vagina and its reproductive functions.
- Outline the structure and basic functions of the uterus.
- What is the endometrium? How does it change during the monthly cycle?
- Why are breasts included in discussions of reproduction, if they are not organs of the female reproductive system?
- What is the function of the folds in the mucous membrane lining of the vagina?
- What are two ways in which the female reproductive system protects itself from pathogens?
18.6 Explore More
https://youtu.be/SkB4gG8ke7Q
The uncomplicated truth about women's sexuality | Sarah Barmak, TED, 2019.
https://youtu.be/9rs2gNchQig
Human Physiology - Functional Anatomy of the Female Reproductive System, Janux, 2015.
Attributes
Figure 18.6.1
1024px-Cattien_stone_yoni by Binh Giang on Wikimedia Commons is in the public domain (https://en.wikipedia.org/wiki/en:public_domain).
Figure 18.6.2
1000px-Gray1167.svg by Henry Vandyke Carter (1831-1897) on Wikimedia Commons is in the public domain (https://en.wikipedia.org/wiki/public_domain). (Bartleby.com: Gray’s Anatomy, Plate 1167).
Figure 18.6.3
Uterine_anatomy. from Uterine Stem cells by The Stem Cell Research Community, StemBook on Wikimedia Commons is used under a CC BY 3.0 (https://creativecommons.org/licenses/by/3.0) license.
Figure 18.6.4
Sites_of_tubo_ovarian_abscess by Bfpage on Wikimedia Commons is used under a CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0) license.
Figure 18.6.5
Ovarian_follicle by TiagoLubiana on Wikimedia Commons is used under a CC BY 4.0 (https://creativecommons.org/licenses/by-sa/4.0) license.
Figure 18.6.6
HumanVulva-NewText-PhiloViv by Amphis (edited) on Wikimedia Commons is used under a CC BY-SA 3.0 (https://creativecommons.org/licenses/by-sa/3.0/deed.en) license. (Original en:Image:HumanVulva-NoText-PhiloVivero.jpg by en:user:PhiloVivero)
Figure 18.6.7
Vulva by OpenStax College on Wikimedia Commons is used under a CC BY 3.0 (https://creativecommons.org/licenses/by/3.0) license.
Figure 18.6.8
Breast-Diagram by Women's Health (NCI/ NIH) on Wikimedia Commons is in the public domain (https://en.wikipedia.org/wiki/en:Public_domain).
References
Betts, J. G., Young, K.A., Wise, J.A., Johnson, E., Poe, B., Kruse, D.H., Korol, O., Johnson, J.E., Womble, M., DeSaix, P. (2013, June 19). Figure 27.10 The vulva [digital image]. In Anatomy and Physiology (Section 27.2). OpenStax. https://openstax.org/books/anatomy-and-physiology/pages/27-2-anatomy-and-physiology-of-the-female-reproductive-system
Janux. (2015, January 10). Human physiology - Functional anatomy of the female reproductive system. YouTube. https://www.youtube.com/watch?v=9rs2gNchQig&feature=youtu.be
TED. (2019, March 22). The uncomplicated truth about women's sexuality | Sarah Barmak. YouTube. https://www.youtube.com/watch?v=SkB4gG8ke7Q&feature=youtu.be
Teixeira, J., Rueda, B.R., and Pru, J.K. (September 30, 2008). Figure 1 Uterine anatomy. In Uterine Stem Cells (StemBook, ed.). The Stem Cell Research Community, StemBook, doi/10.3824/stembook.1.16.1, http://www.stembook.org
The central nervous system organ inside the skull that is the control center of the nervous system.
Created by CK-12 Foundation/Adapted by Christine Miller

Kidneys on the Menu
Pictured in Figure 16.4.1 is a steak and kidney pie; this savory dish is a British favorite. When kidneys are on a menu, they typically come from sheep, pigs, or cows. In these animals (as in the human animal), kidneys are the main organs of excretion.
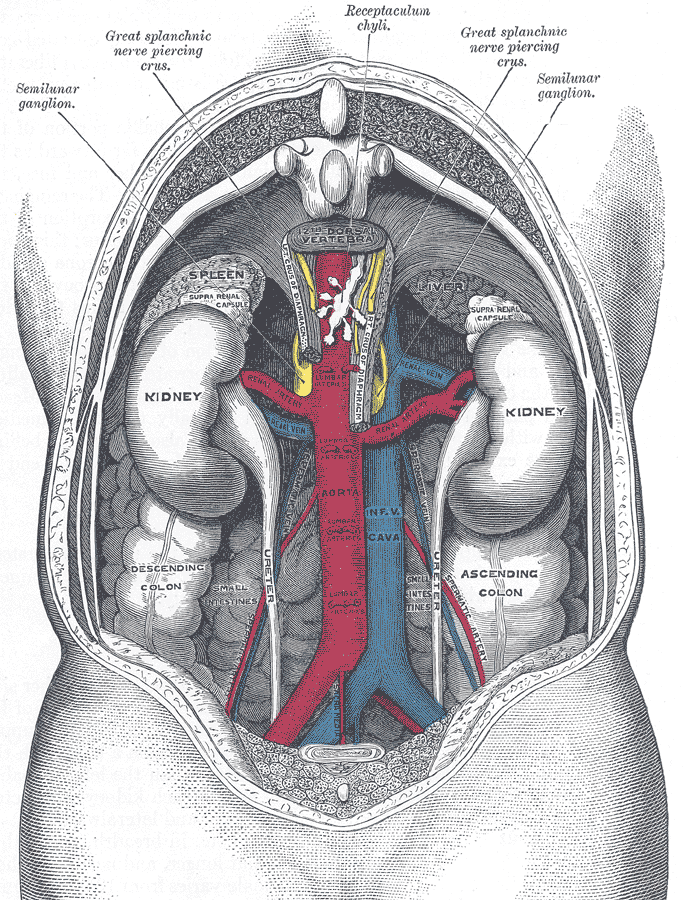
Location of the Kidneys
The two bean-shaped kidneys are located high in the back of the abdominal cavity, one on each side of the spine. Both kidneys sit just below the diaphragm, the large breathing muscle that separates the abdominal and thoracic cavities. As you can see in the following figure, the right kidney is slightly smaller and lower than the left kidney. The right kidney is behind the liver, and the left kidney is behind the spleen. The location of the liver explains why the right kidney is smaller and lower than the left.
Kidney Anatomy
The shape of each kidney gives it a convex side (curving outward) and a concave side (curving inward). You can see this clearly in the detailed diagram of kidney anatomy shown in Figure 16.4.3. The concave side is where the renal artery enters the kidney, as well as where the renal vein and ureter leave the kidney. This area of the kidney is called the hilum. The entire kidney is surrounded by tough fibrous tissue — called the renal capsule — which, in turn, is surrounded by two layers of protective, cushioning fat.
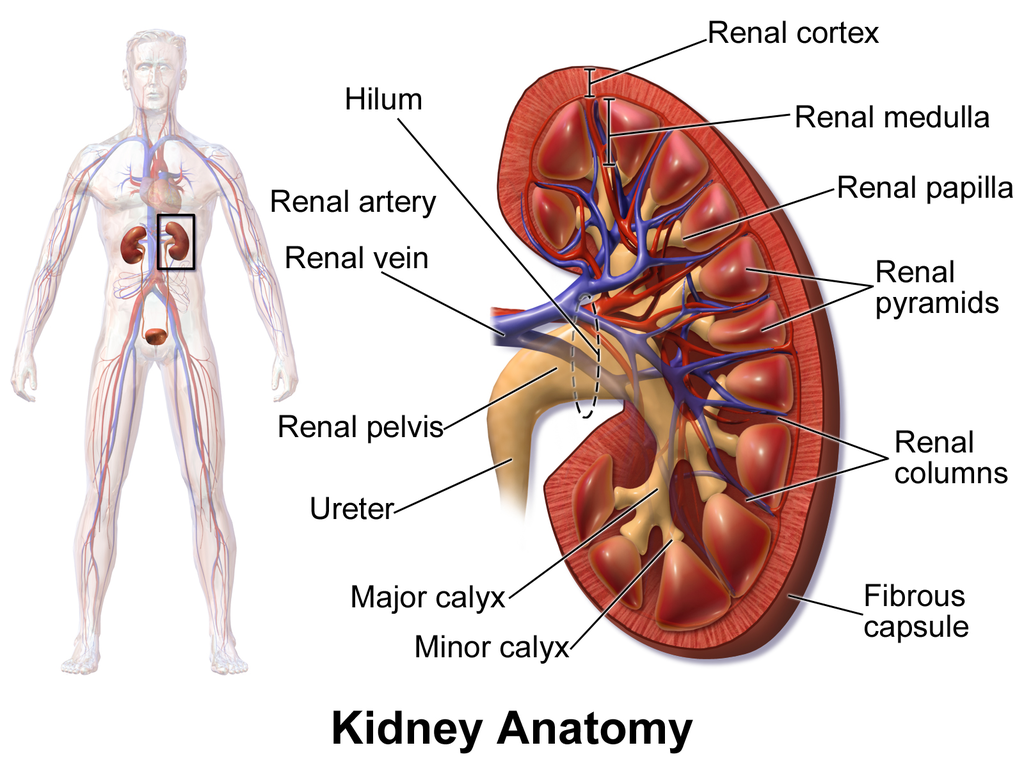
Internally, each kidney is divided into two major layers: the outer renal cortex and the inner renal medulla (see Figure 16.4.3 above). These layers take the shape of many cone-shaped renal lobules, each containing renal cortex surrounding a portion of medulla called a renal pyramid. Within the renal pyramids are the structural and functional units of the kidneys, the tiny nephrons. Between the renal pyramids are projections of cortex called renal columns. The tip, or papilla, of each pyramid empties urine into a minor calyx (chamber). Several minor calyces empty into a major calyx, and the latter empty into the funnel-shaped cavity called the renal pelvis, which becomes the ureter as it leaves the kidney.
Renal Circulation
The renal circulation is an important part of the kidney’s primary function of filtering waste products from the blood. Blood is supplied to the kidneys via the renal arteries. The right renal artery supplies the right kidney, and the left renal artery supplies the left kidney. These two arteries branch directly from the aorta, which is the largest artery in the body. Each kidney is only about 11 cm (4.4 in) long, and has a mass of just 150 grams (5.3 oz), yet it receives about ten per cent of the total output of blood from the heart. Blood is filtered through the kidneys every 3 minutes, 24 hours a day, every day of your life.
As indicated in Figure 16.4.4, each renal artery carries blood with waste products into the kidney. Within the kidney, the renal artery branches into increasingly smaller arteries that extend through the renal columns between the renal pyramids. These arteries, in turn, branch into arterioles that penetrate the renal pyramids. Blood in the arterioles passes through nephrons, the structures that actually filter the blood. After blood passes through the nephrons and is filtered, the clean blood moves through a network of venules that converge into small veins. Small veins merge into increasingly larger ones, and ultimately into the renal vein, which carries clean blood away from the kidney to the inferior vena cava.
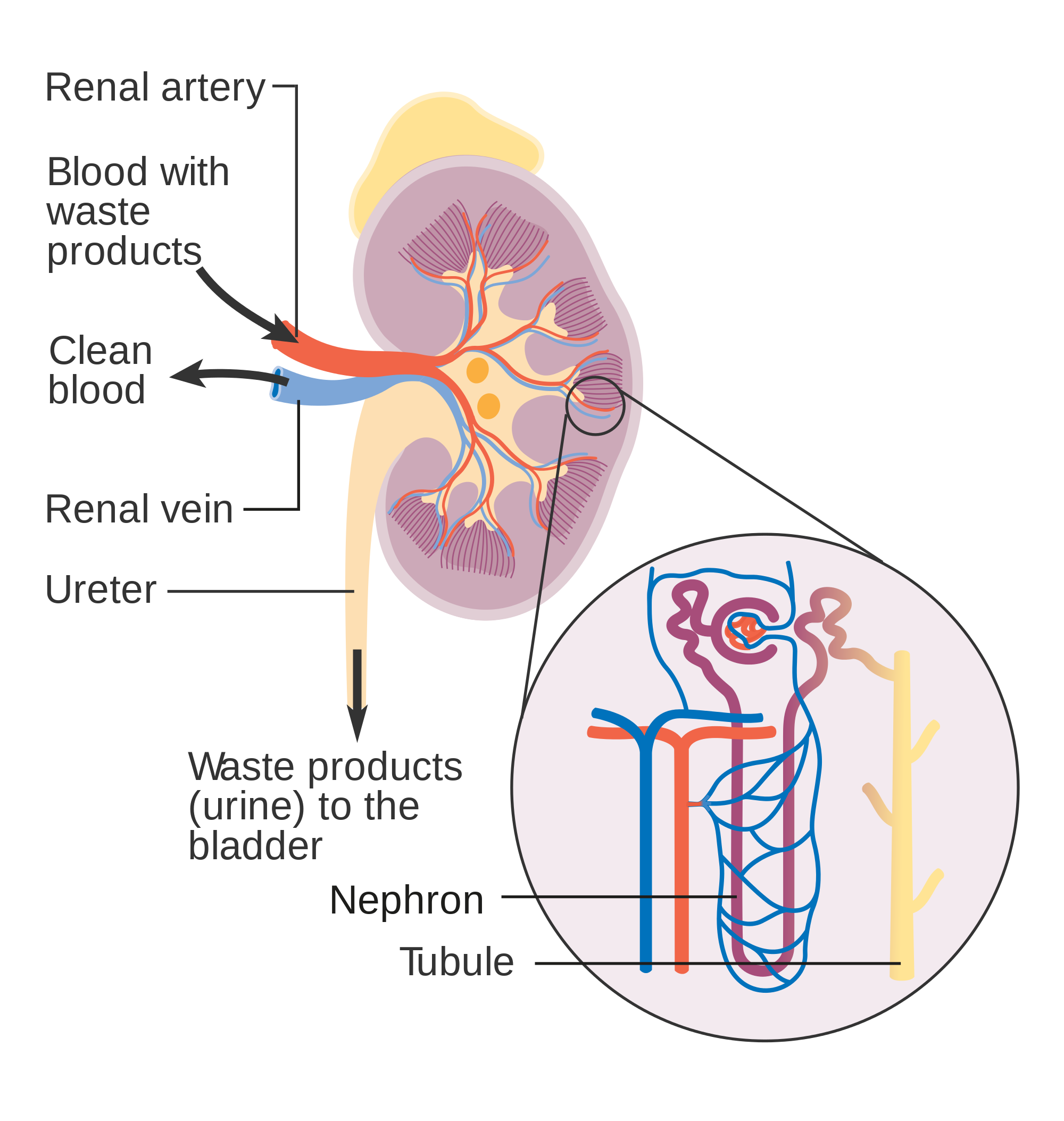
Nephron Structure and Function
Figure 16.4.4 gives an indication of the complex structure of a nephron. The nephron is the basic structural and functional unit of the kidney, and each kidney typically contains at least a million of them. As blood flows through a nephron, many materials are filtered out of the blood, needed materials are returned to the blood, and the remaining materials form urine. Most of the waste products removed from the blood and excreted in urine are byproducts of metabolism. At least half of the waste is urea, a waste product produced by protein catabolism. Another important waste is uric acid, produced in nucleic acid catabolism.
Components of a Nephron
Figure 16.4.5 shows in greater detail the components of a nephron. Each nephron is composed of an initial filtering component that consists of a network of capillaries called the glomerulus (plural, glomeruli), which is surrounded by a space within a structure called glomerular capsule (also known as the Bowman's capsule). Extending from glomerular capsule is the renal tubule. The proximal end (nearest glomerular capsule) of the renal tubule is called the proximal convoluted (coiled) tubule. From here, the renal tubule continues as a loop (known as the loop of Henle) (also known as the loop of the nephron), which in turn becomes the distal convoluted tubule. The latter finally joins with a collecting duct. As you can see in the diagram, arterioles surround the total length of the renal tubule in a mesh called the peritubular capillary network.
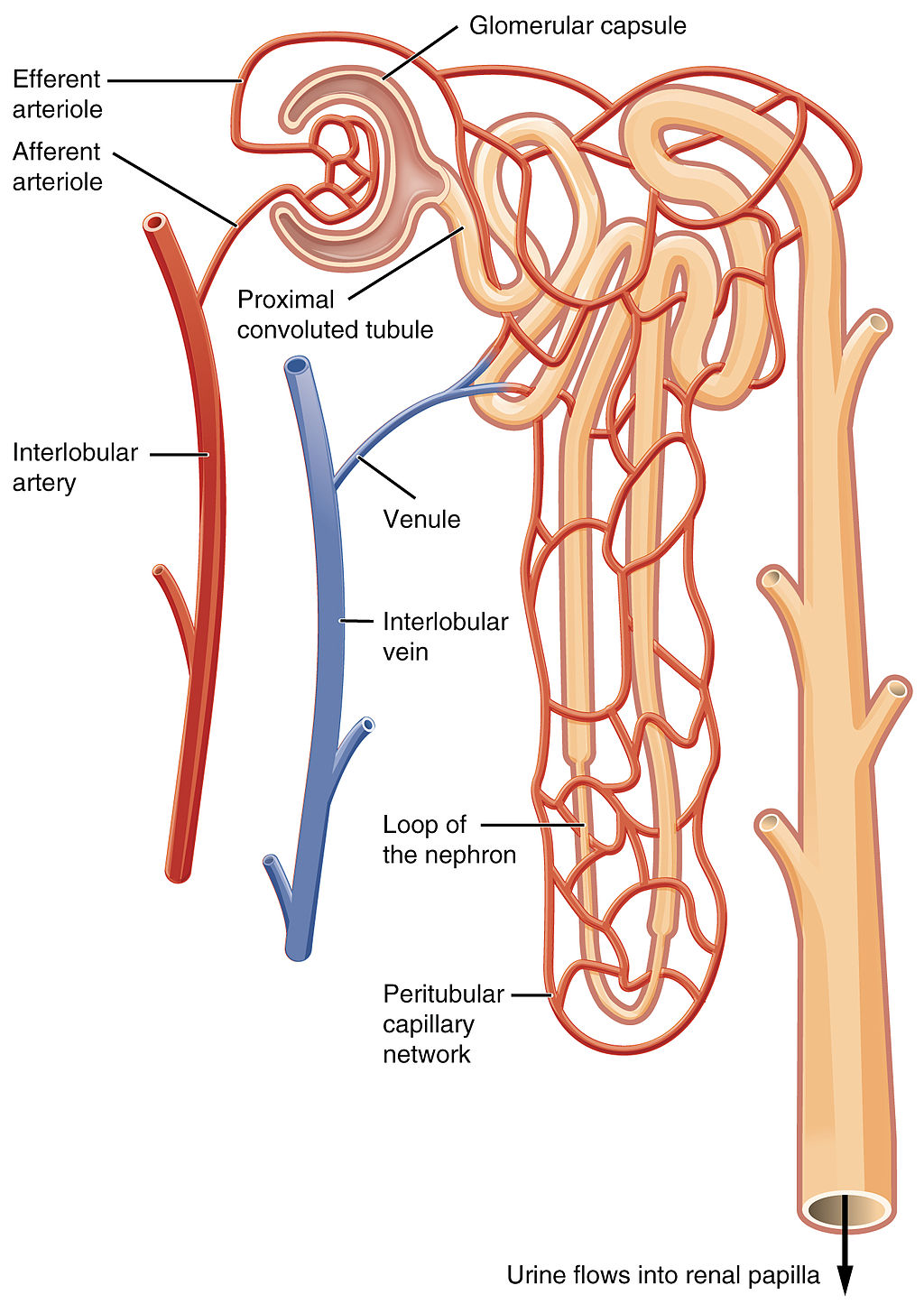
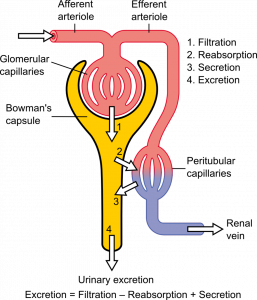
Function of a Nephron
The simplified diagram of a nephron in Figure 16.4.6 shows an overview of how the nephron functions. Blood enters the nephron through an arteriole called the afferent arteriole. Next, some of the blood passes through the capillaries of the glomerulus. Any blood that doesn’t pass through the glomerulus — as well as blood after it passes through the glomerular capillaries — continues on through an arteriole called the efferent arteriole. The efferent arteriole follows the renal tubule of the nephron, where it continues playing a role in nephron functioning.
Filtration
As blood from the afferent arteriole flows through the glomerular capillaries, it is under pressure. Because of the pressure, water and solutes are filtered out of the blood and into the space made by glomerular capsule, almost like the water you cook pasta is is filtered out through a strainer. This is the filtration stage of nephron function. The filtered substances — called filtrate — pass into glomerular capsule, and from there into the proximal end of the renal tubule. Anything too large to move through the pores in the glomerulus, such as blood cells, large proteins, etc., stay in the cardiovascular system. At this stage, filtrate (fluid in the nephron) includes water, salts, organic solids (such as nutrients), and waste products of metabolism (such as urea).
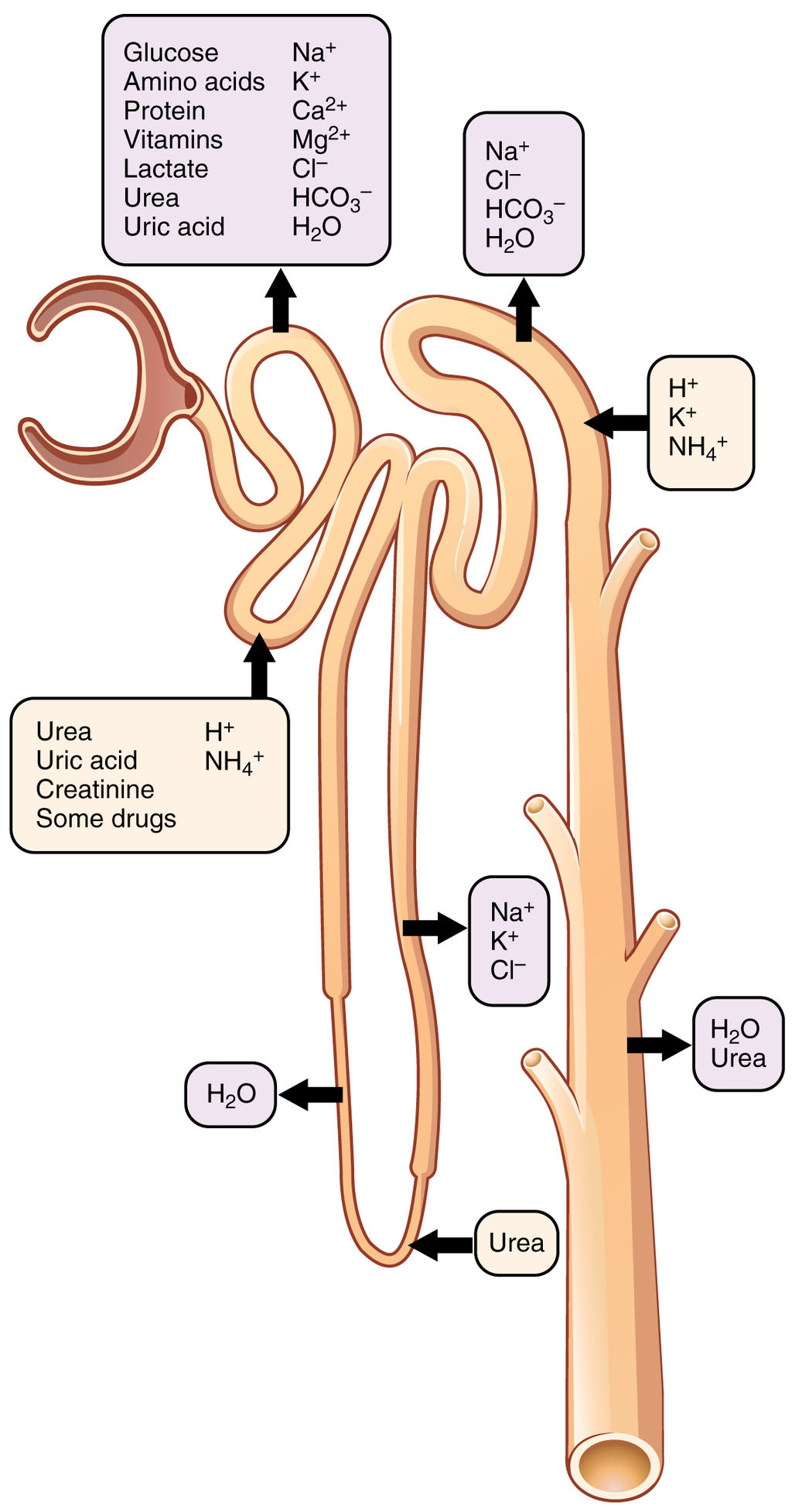
Reabsorption and Secretion
As filtrate moves through the renal tubule, some of the substances it contains are reabsorbed from the filtrate back into the blood in the efferent arteriole (via peritubular capillary network). This is the reabsorption stage of nephron function and it is about returning "the good stuff" back to the blood so that it doesn't exit the body in urine. About two-thirds of the filtered salts and water, and all of the filtered organic solutes (mainly glucose and amino acids) are reabsorbed from the filtrate by the blood in the peritubular capillary network. Reabsorption occurs mainly in the proximal convoluted tubule and the loop of Henle, as seen in Figure 16.4.7.
At the distal end of the renal tubule, some additional reabsorption generally occurs. This is also the region of the tubule where other substances from the blood are added to the filtrate in the tubule. The addition of other substances to the filtrate from the blood is called secretion. Both reabsorption and secretion (shown in Figure 16.4.7) in the distal convoluted tubule are largely under the control of endocrine hormones that maintain homeostasis of water and mineral salts in the blood. These hormones work by controlling what is reabsorbed into the blood from the filtrate and what is secreted from the blood into the filtrate to become urine. For example, parathyroid hormone causes more calcium to be reabsorbed into the blood and more phosphorus to be secreted into the filtrate.
Collection of Urine and Excretion

By the time the filtrate has passed through the entire renal tubule, it has become the liquid waste known as urine. Urine empties from the distal end of the renal tubule into a collecting duct. From there, the urine flows into increasingly larger collecting ducts. As urine flows through the system of collecting ducts, more water may be reabsorbed from it. This will occur in the presence of antidiuretic hormone from the posterior pituitary gland. This hormone makes the collecting ducts permeable to water, allowing water molecules to pass through them into capillaries by osmosis, while preventing the passage of ions or other solutes. As much as 75% of the water may be reabsorbed from urine in the collecting ducts, making the urine more concentrated.
Urine finally exits the largest collecting ducts through the renal papillae. It empties into the renal calyces, and finally into the renal pelvis. From there, it travels through the ureter to the urinary bladder for eventual excretion from the body. An average of roughly 1.5 litres (a little over 6 cups) of urine is excreted each day. Normally, urine is yellow or amber in colour (see Figure 16.4.8). The darker the colour, generally speaking, the more concentrated the urine is.
Besides filtering blood and forming urine for excretion of soluble wastes, the kidneys have several vital functions in maintaining body-wide homeostasis. Most of these functions are related to the composition or volume of urine formed by the kidneys. The kidneys must maintain the proper balance of water and salts in the body, normal blood pressure, and the correct range of blood pH. Through the processes of absorption and secretion by nephrons, more or less water, salt ions, acids, or bases are returned to the blood or excreted in urine, as needed, to maintain homeostasis.
Blood Pressure Regulation
The kidneys do not control homeostasis all alone. As indicated above, endocrine hormones are also involved. Consider the regulation of blood pressure by the kidneys. Blood pressure is the pressure exerted by blood on the walls of the arteries. The regulation of blood pressure is part of a complex system, called the renin-angiotensin-aldosterone system. This system regulates the concentration of sodium in the blood to control blood pressure.
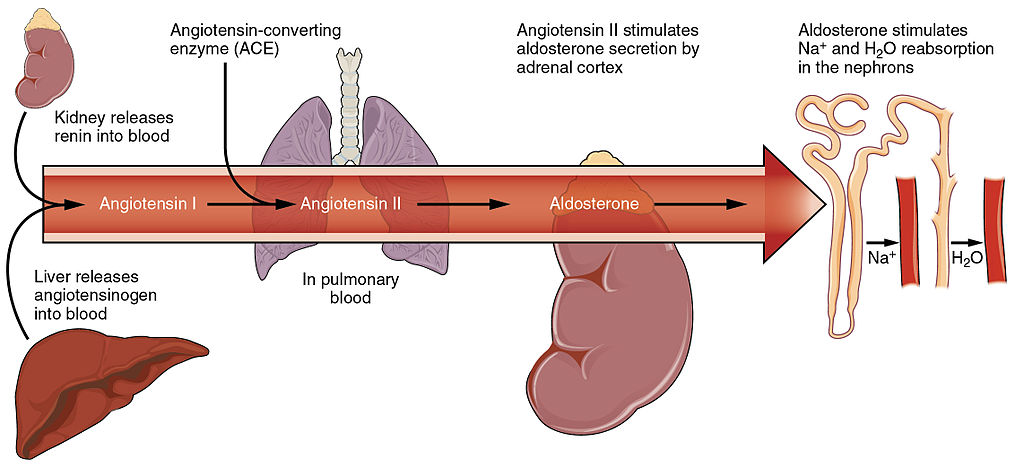
The renin-angiotensin-aldosterone system is put into play when the concentration of sodium ions in the blood falls lower than normal. This causes the kidneys to secrete an enzyme called renin into the blood. It also causes the liver to secrete a protein called angiotensinogen. Renin changes angiotensinogen into a proto-hormone called angiotensin I. This is converted to angiotensin II by an enzyme (angiotensin-converting enzyme) in lung capillaries.
Angiotensin II is a potent hormone that causes arterioles to constrict. This, in turn, increases blood pressure. Angiotensin II also stimulates the secretion of the hormone aldosterone from the adrenal cortex. Aldosterone causes the kidneys to increase the reabsorption of sodium ions and water from the filtrate into the blood. This returns the concentration of sodium ions in the blood to normal. The increased water in the blood also increases blood volume and blood pressure.
Other Kidney Hormones
Hormones other than renin are also produced and secreted by the kidneys. These include calcitriol and erythropoietin.
- Calcitriol is secreted by the kidneys in response to low levels of calcium in the blood. This hormone stimulates uptake of calcium by the intestine, thus raising blood levels of calcium.
- Erythropoietin is secreted by the kidneys in response to low levels of oxygen in the blood. This hormone stimulates erythropoiesis, which is the production of erythrocytes in bone marrow. Extra red blood cells increase the level of oxygen carried in the blood.
Feature: Human Biology in the News
Kidney failure is a complication of common disorders including diabetes mellitus and hypertension. It is estimated that approximately 12.5% of Canadians have some form of kidney disease. If the disease is serious, the patient must either receive a donated kidney or have frequent hemodialysis, a medical procedure in which the blood is artificially filtered through a machine. Transplant generally results in better outcomes than hemodialysis, but demand for organs far outstrips the supply. The average time on the organ donation waitlist for a kidney is four years. There are over 3,000 Canadians on the wait list for a kidney transplant and some will die waiting for a kidney to become available.
For the past decade, Dr. William Fissell, a kidney specialist at Vanderbilt University, has been working to create an implantable part-biological and part-artificial kidney. Using microchips like those used in computers, he has produced an artificial kidney small enough to implant in the patient’s body in place of the failed kidney. According to Dr. Fissell, the artificial kidney is “... a bio-hybrid device that can mimic a kidney to remove enough waste products, salt, and water to keep a patient off [hemo]dialysis.”
The filtration system in the artificial kidney consists of a stack of 15 microchips. Tiny pores in the microchips act as a scaffold for the growth of living kidney cells that can mimic the natural functions of the kidney. The living cells form a membrane to filter the patient’s blood as a biological kidney would, but with less risk of rejection by the patient’s immune system, because they are embedded within the device. The new kidney doesn’t need a power source, because it uses the natural pressure of blood flowing through arteries to push the blood through the filtration system. A major part of the design of the artificial organ was devoted to fine tuning the fluid dynamics so blood flows through the device without clotting.
Because of the potential life-saving benefits of the device, the implantable kidney was given fast-track approval for testing in people by the U.S. Food and Drug Administration. The artificial kidney is expected to be tested in pilot trials by 2018. Dr. Fissell says he has a long list of patients eager to volunteer for the trials.
16.4 Summary
- The two bean-shaped kidneys are located high in the back of the abdominal cavity on either side of the spine. A renal artery connects each kidney with the aorta, and transports unfiltered blood to the kidney. A renal vein connects each kidney with the inferior vena cava and transports filtered blood back to the circulation.
- The kidney has two main layers involved in the filtration of blood and formation of urine: the outer cortex and inner medulla. At least a million nephrons — which are the tiny functional units of the kidney — span the cortex and medulla. The entire kidney is surrounded by a fibrous capsule and protective fat layers.
- As blood flows through a nephron, many materials are filtered out of the blood, needed materials are returned to the blood, and the remaining materials are used to form urine.
- In each nephron, the glomerulus and surrounding Bowman’s capsule form the unit that filters blood. From Bowman’s capsule, the material filtered from blood (called filtrate) passes through the long renal tubule. As it does, some substances are reabsorbed into the blood, and other substances are secreted from the blood into the filtrate, finally forming urine. The urine empties into collecting ducts, where more water may be reabsorbed.
- The kidneys control homeostasis with the help of endocrine hormones. The kidneys, for example, are part of the renin-angiotensin-aldosterone system that regulates the concentration of sodium in the blood to control blood pressure. In this system, the enzyme renin secreted by the kidneys works with hormones from the liver and adrenal gland to stimulate nephrons to reabsorb more sodium and water from urine.
- The kidneys also secrete endocrine hormones, including calcitriol — which helps control the level of calcium in the blood — and erythropoietin, which stimulates bone marrow to produce red blood cells.
16.4 Review Questions
-
- Contrast the renal artery and renal vein.
- Identify the functions of a nephron. Describe in detail what happens to fluids (blood, filtrate, and urine) as they pass through the parts of a nephron.
- Identify two endocrine hormones secreted by the kidneys, along with the functions they control.
- Name two regions in the kidney where water is reabsorbed.
- Is the blood in the glomerular capillaries more or less filtered than the blood in the peritubular capillaries? Explain your answer.
- What do you think would happen if blood flow to the kidneys is blocked?
16.4 Explore More
https://youtu.be/FN3MFhYPWWo
How do your kidneys work? - Emma Bryce, TED-Ed, 2015.
https://youtu.be/es-t8lO1KpA
Urine Formation, Hamada Abass, 2013.
https://youtu.be/bX3C201O4MA
Printing a human kidney - Anthony Atala, TED-Ed, 2013.
Attributions
Figure 16.4.1
Steak and Kidney Pie by Charles Haynes on Flickr is used under a CC BY-SA 2.0 (https://creativecommons.org/licenses/by-sa/2.0/) license.
Figure 16.4.2
Gray Kidneys by Henry Vandyke Carter (1831-1897) on Wikimedia Commons is in the public domain (https://en.wikipedia.org/wiki/public_domain). (Bartleby.com: Gray’s Anatomy, Plate 1120).
Figure 16.4.3
Blausen_0592_KidneyAnatomy_01 by BruceBlaus on Wikimedia Commons is used under a CC BY 3.0 (https://creativecommons.org/licenses/by/3.0) license.
Figure 16.4.4
Diagram_showing_how_the_kidneys_work_CRUK_138.svg by Cancer Research UK on Wikimedia Commons is used under a CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0) license.
Figure 16.4.5
Blood_Flow_in_the_Nephron by OpenStax College on Wikimedia Commons is used under a CC BY 3.0 (https://creativecommons.org/licenses/by/3.0) license.
Figure 16.4.6
1024px-Physiology_of_Nephron by Madhero88 on Wikimedia Commons is used under a CC BY 3.0 (https://creativecommons.org/licenses/by/3.0) license.
Figure 16.4.7
Nephron_Secretion_Reabsorption by OpenStax College on Wikimedia Commons is used under a CC BY 3.0 (https://creativecommons.org/licenses/by/3.0) license.
Figure 16.4.8
Urine by User:Markhamilton at English Wikipedia on Wikimedia Commons is in the public domain (https://en.wikipedia.org/wiki/Public_domain).
Figure 16.4.9
Renin_Angiotensin_System-01 by OpenStax College on Wikimedia Commons is used under a CC BY 3.0 (https://creativecommons.org/licenses/by/3.0) license.
References
Betts, J. G., Young, K.A., Wise, J.A., Johnson, E., Poe, B., Kruse, D.H., Korol, O., Johnson, J.E., Womble, M., DeSaix, P. (2013, June 19). Figure 25.10 Blood flow in the nephron [digital image]. In Anatomy and Physiology (Section 25.3). OpenStax. https://openstax.org/books/anatomy-and-physiology/pages/25-3-gross-anatomy-of-the-kidney
Betts, J. G., Young, K.A., Wise, J.A., Johnson, E., Poe, B., Kruse, D.H., Korol, O., Johnson, J.E., Womble, M., DeSaix, P. (2013, June 19). Figure 25.17 Locations of secretion and reabsorption in the nephron [digital image]. In Anatomy and Physiology (Section 25.6). OpenStax. https://openstax.org/books/anatomy-and-physiology/pages/25-6-tubular-reabsorption
Betts, J. G., Young, K.A., Wise, J.A., Johnson, E., Poe, B., Kruse, D.H., Korol, O., Johnson, J.E., Womble, M., DeSaix, P. (2013, June 19). Figure 26.14 The renin-angiotensin system [digital image]. In Anatomy and Physiology (Section 26.3). OpenStax. https://openstax.org/books/anatomy-and-physiology/pages/26-3-electrolyte-balance
Blausen.com Staff. (2014). Medical gallery of Blausen Medical 2014. WikiJournal of Medicine 1 (2). DOI:10.15347/wjm/2014.010. ISSN 2002-4436
Hamada Abass. (2013). Urine formation. YouTube. https://www.youtube.com/watch?v=es-t8lO1KpA&feature=youtu.be
TED-Ed. (2015, February 9). How do your kidneys work? - Emma Bryce. YouTube. https://www.youtube.com/watch?v=FN3MFhYPWWo&feature=youtu.be
TED-Ed. (2013, March 15). Printing a human kidney - Anthony Atala. YouTube. https://www.youtube.com/watch?v=bX3C201O4MA&feature=youtu.be
Created by CK-12 Foundation/Adapted by Christine Miller

Waiting Expectantly
A mother-to-be waits patiently for her baby to grow as her belly gradually swells. Reproduction is all about making babies, and the female reproductive system is specialized for this purpose. Its functions include producing female gametes called ova, secreting female sex hormones (such as estrogen), providing a site for fertilization, gestating a fetus if fertilization occurs, giving birth to a baby, and breastfeeding a baby after birth. The only thing missing is sperm.
Ova Production
At birth, a female’s ovaries contain all the ova she will ever produce, which may include a million or more ova. The ova don't start to mature, however, until she enters puberty and attains sexual maturity. After that, one ovum typically matures each month, and is released from an ovary. This continues until a woman reaches menopause (cessation of monthly periods), typically by age 52. By then, viable eggs may be almost depleted, and hormone levels can no longer support the monthly cycle. During the reproductive years, which of the two ovaries releases an egg in a given month seems to be a matter of chance. Occasionally, both ovaries will release an egg at the same time. If both eggs are fertilized, the offspring are fraternal twins (dizygotic, or "two-zygote," twins), and they are no more alike genetically than non-twin siblings.
Oogenesis
The process of producing ova in the ovaries of a female fetus is called oogenesis. Ova are haploid gametes, and their production occurs in several steps that involve different types of cells, as summarized in Figure 18.7.2. Oogenesis is completed long before birth. It occurs when diploid germ cells called oogonia (singular, oogonium) undergo mitosis. Each such cell division produces two diploid daughter cells. One is called the primary oocyte, and the other is retained to help maintain a reserve of oogonia. The primary oocyte, in turn, starts to go through the first cell division of meiosis (meiosis I). However, it does not complete meiosis I until much later. Instead, it remains in a resting state, nestled within a tiny, immature follicle in the ovary until the female goes through puberty.
Maturation of a Follicle
Beginning in puberty, about once a month, one of the follicles in an ovary undergoes maturation, and an egg is released. As the follicle matures, it goes through changes in the numbers and types of its cells, as shown in Figure 18.7.2. The primary oocyte within the follicle also resumes meiosis. It completes meiosis I, which began long before birth, to form a secondary oocyte and a smaller cell, called the first polar body. Both the secondary oocyte and the first polar body are haploid cells. The secondary oocyte has most of the cytoplasm from the primary oocyte and is much larger than the first polar body, which soon disintegrates and disappears. The secondary oocyte begins meiosis II, but only completes it if the egg is fertilized.
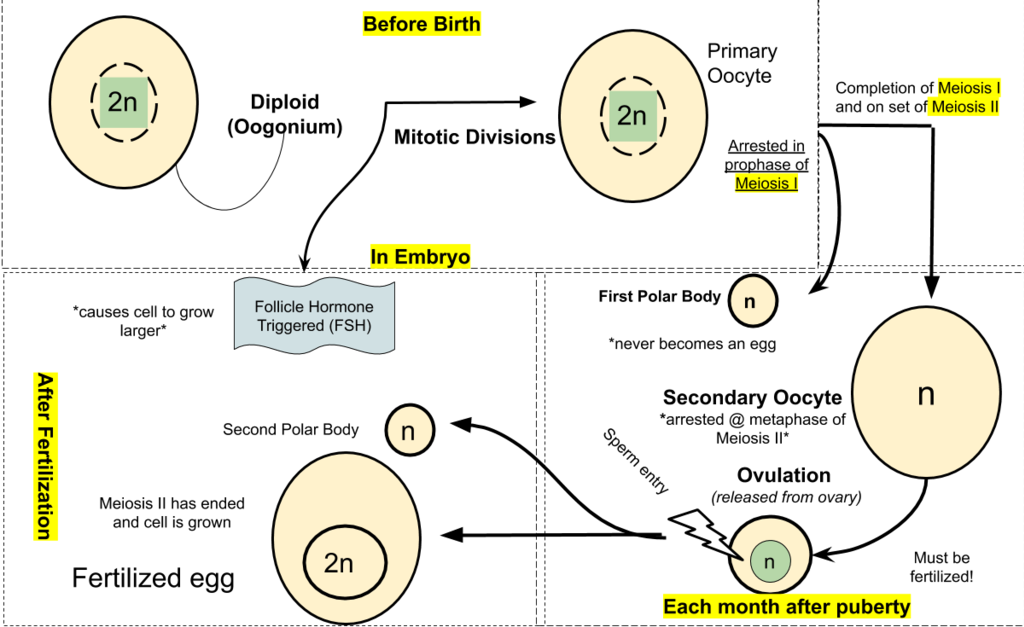
Release of an Egg
It typically takes 12 to 14 days for a follicle to mature in an ovary, and for the secondary oocyte to form. Then, the follicle bursts open and the ovary ruptures, releasing the secondary oocyte from the ovary. This event is called ovulation. The now-empty follicle starts to change into a structure called a corpus luteum. The expelled secondary oocyte is usually swept into the nearby oviduct by its waving, fringe-like fimbriae.
Uterine Changes
While the follicle is maturing in the ovary, the uterus is also undergoing changes to prepare it for an embryo if fertilization occurs. For example, the endometrium gets thicker and becomes more vascular. Around the time of ovulation, the cervix undergoes changes that help sperm reach the ovum to fertilize it. The cervical canal widens, and cervical mucus becomes thinner and more alkaline. These changes help promote the passage of sperm from the vagina into the uterus and make the environment more hospitable to sperm.
Fertilization — or Not
Fertilization of an ovum by a sperm normally occurs in an oviduct, most often in the part of the tube that passes above the ovary (see Figure 18.7.3). In order for fertilization to occur, sperm must “swim” from the vagina where they are deposited, through the cervical canal to the uterus, and then through the body of the uterus to one of the oviducts. Once sperm enter a oviduct, tubular fluids help carry them through the tube toward the secondary oocyte at the other end. The secondary oocyte also functions to promote fertilization. It releases molecules that guide the sperm and allow the surface of the ovum to attach to the surface of the sperm. The ovum can then absorb the sperm, allowing fertilization to occur.
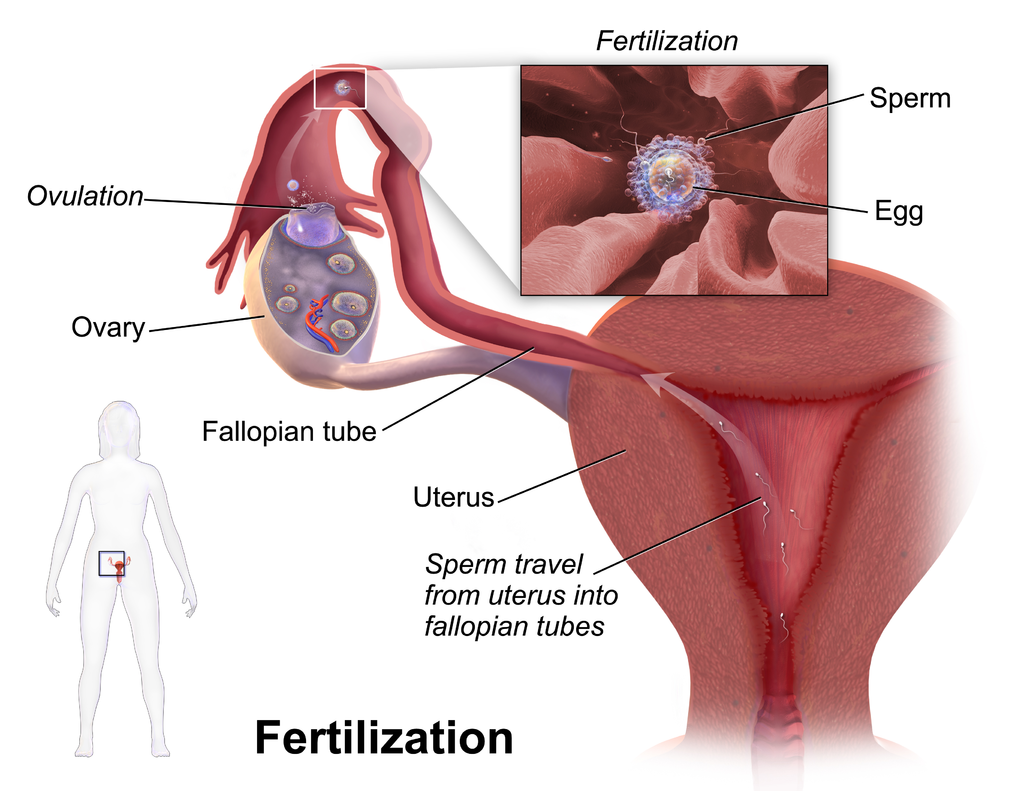
If Fertilization Occurs
If the secondary oocyte is fertilized by a sperm as it passes through the oviduct, the secondary oocyte quickly completes meiosis II, forming a diploid zygote and another polar body. This second polar body, like the first, normally breaks down and disappears. The zygote then continues the journey through the oviduct to the uterus, during which it undergoes several mitotic cell divisions. By the time it reaches the uterus up to five days after fertilization, it consists of a ball of cells called a blastocyst. Within another day or two, the blastocyst implants itself in the endometrium lining the uterus, and gestation begins.
If Fertilization Does Not Occur
What happens if the secondary oocyte is not fertilized by a sperm as it passes through the oviduct? It continues on its way to the uterus without ever completing meiosis II. It is likely to disintegrate within a few days while still in the oviduct. Any remaining material will be shed from the woman’s body during the next menstrual period.
Pregnancy and Childbirth
Pregnancy is the carrying of one or more offspring from fertilization until birth. This is one of the major functions of the female reproductive system. It involves virtually every other body system including the cardiovascular, urinary, and respiratory systems, to name just three. The maternal organism plays a critical role in the development of the offspring. She must provide all the nutrients and other substances needed for normal growth and development of the offspring, and she must also remove the wastes excreted by the offspring. Most nutrients are needed in greater amounts by a pregnant woman to meet fetal needs, but some are especially important, including folic acid, calcium, iron, and omega-3 fatty acids. A healthy diet (see photo in Figure 18.7.4), along with prenatal vitamin supplements, is recommended for the best pregnancy outcome. A pregnant woman should also avoid ingesting substances (such as alcohol) that can damage the developing offspring, especially early in the pregnancy when all of the major organs and organ systems are forming.

Trimesters of Pregnancy
When counted from the first day of the last menstrual period, the average duration of pregnancy is about 40 weeks (38 weeks when counted from the time of fertilization), but a pregnancy that lasts between 37 and 42 weeks is still considered within the normal range. From the point of view of the maternal organism, the total duration of pregnancy is typically divided into three periods, called trimesters, each of which lasts about three months. This division of the total period of gestation is useful for summarizing the typical changes a woman can expect during pregnancy. From the point of view of the developing offspring, however, the major divisions are different. They are the embryonic and fetal stages. The offspring is called an embryo from the time it implants in the uterus through the first eight weeks of life. After that, it is called a fetus for the duration of the pregnancy.
First Trimester
The first trimester begins at the time of fertilization and lasts for the next 12 weeks. Even before she knows she is pregnant, a woman in the first trimester is likely to experience signs and symptoms of pregnancy. She may notice a missed menstrual period, and she may also experience tender breasts, increased appetite, and more frequent urination. Many women also experience nausea and vomiting in the first trimester. This is often called “morning sickness,” because it commonly occurs in the morning, but it may occur at any time of day. Some women may lose weight during the first trimester because of morning sickness.
Second Trimester
The second trimester occurs during weeks 13 to 28 of pregnancy. A pregnant woman may feel more energized during this trimester. If she experienced nausea and vomiting during the first trimester, these symptoms often subside during the second trimester. Weight gain starts occurring during this trimester, as well. By about week 20, the fetus is getting large enough that the mother can feel its movements. The photo in Figure 18.7.5 shows a pregnant woman at week 26, toward the end of the second trimester. (For comparison, the same woman is shown on the right at the end of the third trimester.)

Third Trimester
The third trimester occurs during weeks 29 through birth (at about 40 weeks). During this trimester, the uterus expands rapidly, making up a larger and larger portion of the woman's abdomen. Weight gain is also more rapid. During the third trimester, the movements of the fetus become stronger and more frequent, and they may become disruptive to the mother. As the fetus grows larger, its weight and the space it takes up may lead to symptoms in the mother such as back pain, swelling of the lower extremities, more frequent urination, varicose veins, and heartburn. By the end of the third trimester, the woman's abdomen often will transform in shape as it drops, due to the fetus turning to a downward position before birth so its head rests on the cervix. This relieves pressure on the upper abdomen, but reduces bladder capacity and increases pressure on the pelvic floor and rectum.
Childbirth
Near the time of birth, the amniotic sac — a fluid-filled membrane that encloses the fetus within the uterus — breaks in a gush of fluid. This is commonly called “breaking water.” Labour usually begins within a day of this event, although it may begin prior to it. Labour is the general term for the process of childbirth in which regular uterine contractions push the fetus and placenta out of the body. Labour can be divided into three stages, which are illustrated in Figure 18.7.6: dilation, birth, and afterbirth.
- During the dilation stage of labour, uterine contractions begin and become increasingly frequent and intense. The contractions push the baby’s head (most often) against the cervix, causing the cervical canal to dilate, or become wider. This lasts until the cervical canal has dilated to about 10 cm (almost 4 in.) in width, which may take 12 to 20 hours — or even longer. The cervical canal must be dilated to this extent in order for the baby’s head to fit through it.
- During birth, the baby descends (usually headfirst) through the cervical canal and vagina, and into the world outside. This is the stage when the mother generally starts bearing down during the contractions to help push out the fetus. This stage may last from about 20 minutes to two hours or more. Usually, within a minute or less of birth, the umbilical cord is cut, so the baby is no longer connected to the placenta.
- During the afterbirth stage, the placenta is delivered. This stage may last from a few minutes to a half hour.
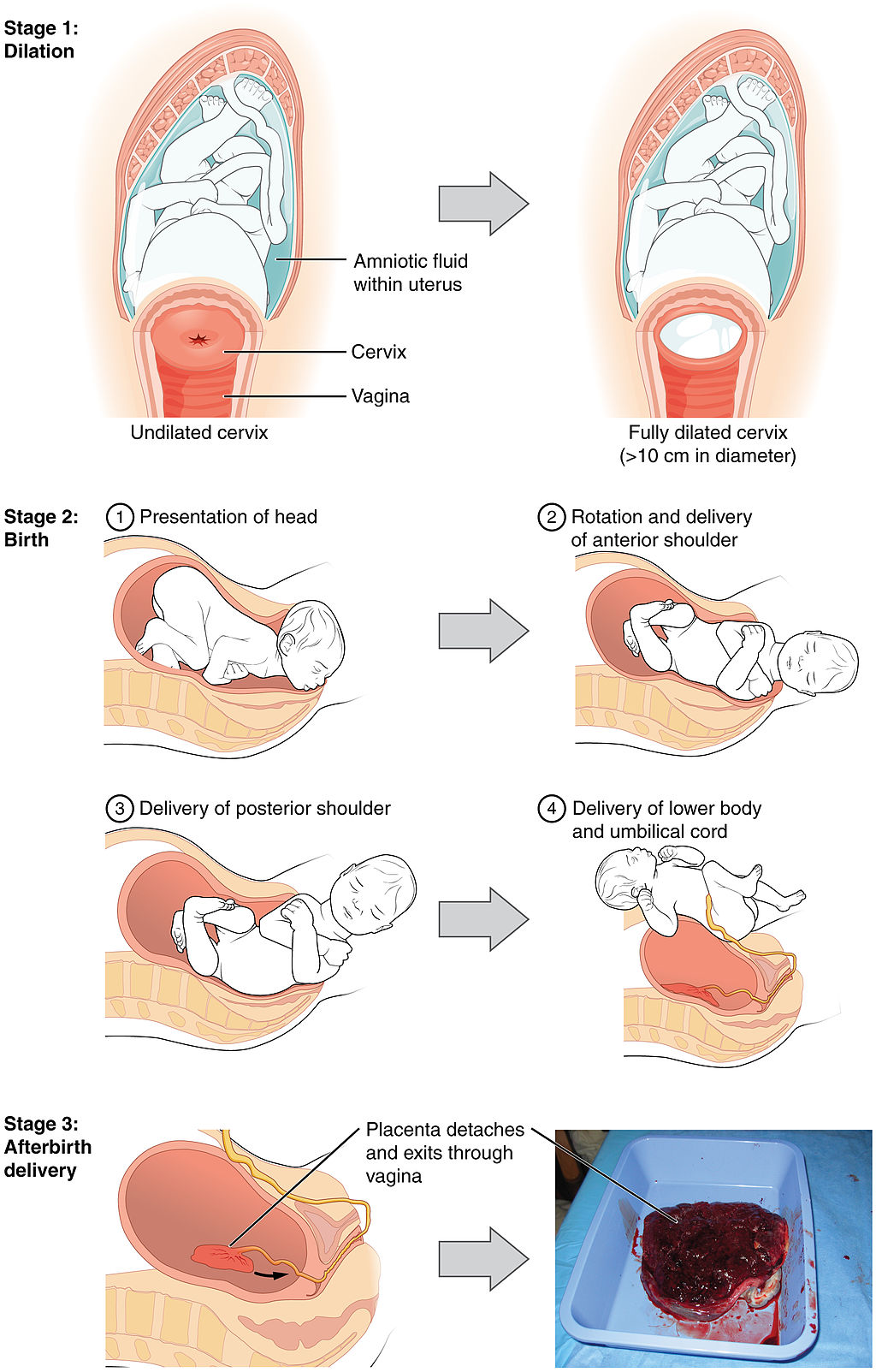
Breastfeeding
Although the breasts are not classified as organs of the reproductive system, they nonetheless may play an important role in reproduction. The physiological function of the female breast is lactation, or the production of breast milk to feed an infant. This function is illustrated in Figure 18.7.7. Besides nutrients, breast milk provides hormones, antibodies, and other substances that help ensure a healthy start after birth.

The Figure 18.7.7 (above) shows the correct way for an infant to suck the breast to stimulate the letdown of milk from the mammary glands (lips flanged, baby's mouth on the nipple symmetrically). The letdown of milk when an infant sucks at the breast is one of the few examples of a positive feedback loop in the human organism. Sucking causes a release from the posterior pituitary gland of the hypothalamic hormone oxytocin. Oxytocin, in turn, causes milk to flow from the alveoli in the breasts where milk is produced, through the milk ducts, and into the milk sacs behind the areola. You can trace this route of milk through the breast in Figure 18.7.8. The baby can suck the milk out of the sacs through the nipple, where they converge. The release of milk stimulates the baby to continue sucking, which in turn keeps the milk flowing. Oxytocin is also an important hormone for maternal-child attachment.
Female Sex Hormones
Female reproduction could not occur without sex hormones released by the ovaries. These hormones include estrogen and progesterone.
Estrogen
Before birth, estrogen is released by the gonads in female fetuses and leads to the development of female reproductive organs. At puberty, estrogen levels rise and are responsible for sexual maturation, and for the development of female secondary sex characteristics (such as breasts). Estrogen is also needed to help regulate the menstrual cycle and ovulation throughout a woman’s reproductive years. Estrogen is produced primarily by follicular cells in the ovaries. During pregnancy, estrogen is also produced by the placenta. There are actually three forms of estrogen in the human female: estradiol, estriol, and estrone.
- Estradiol is the predominant form of estrogen during the reproductive years. It is also the most potent form of estrogen.
- Estriol is the predominant form of estrogen during pregnancy. It is also the weakest form of estrogen.
- Estrone is the predominant form of estrogen in post-menopausal women. It is intermediate in strength between the other two forms of estrogen.
Progesterone
Progesterone stands for “pro-gestational hormone.” It is synthesized and secreted primarily by the corpus luteum in the ovary. Progesterone plays many physiological roles, but is best known for its role during pregnancy. In fact, it is sometimes called the “hormone of pregnancy.” Among other functions, progesterone prepares the uterus for pregnancy each month by building up the uterine lining. If a pregnancy occurs, progesterone helps maintain the pregnancy in a number of ways, such as decreasing the maternal immune response to the genetically different embryo, and decreasing the ability of uterine muscle tissue to contract. Progesterone also prepares the mammary glands for lactation during pregnancy, and withdrawal of progesterone after birth is one of the triggers of milk production.
Feature: Myth vs. Reality
There are many myths associated with pregnancy. Most are harmless, but some may put the pregnant woman or fetus at risk. As always, knowledge is power.
| Myth | Reality |
|---|---|
| "You should avoid petting your cat during pregnancy." | Cat feces may be contaminated with microscopic parasites that can cause a disease called toxoplasmosis. Pregnant women who contract this disease are at risk of stillbirth, miscarriage, or giving birth to an infant with serious health problems. Pregnant women should not have contact with a cat’s litter box or feces, but petting a cat poses no real risk of infection. |
| "You should not dye your hair during pregnancy, because the chemicals can harm the fetus." | Whereas some chemicals (such as certain pesticides) have been shown to be associated with birth defects, there is no evidence that using hair dye during pregnancy increases this risk. |
| "A pregnant woman needs to eat for two, so she should double her pre-pregnancy caloric intake." | Throughout a typical pregnancy, a woman needs only about 300 extra calories per day, on average, to support her growing fetus. Most of the extra calories are needed during the last trimester, when the fetus is growing most rapidly. Doubling her caloric intake during pregnancy is likely to cause too much weight gain, which can be detrimental to her baby. Babies that weigh much more than the average 7.5 pounds (3.4 kg) at birth are more likely to develop diabetes and obesity in later life. |
| "Women who are pregnant have strange food cravings, such as ice cream with pickles." | Some women do have food cravings during pregnancy, but they are not necessarily cravings for strange foods or unusual food combinations. For example, a pregnant woman might crave starchy foods for a few weeks, or she may be put off by certain foods that she loved before pregnancy. |
| "A pregnant woman has skin that glows." | Pregnancy can actually be hard on the skin and its appearance. Besides stretch marks on the abdomen and breasts, pregnancy may lead to spider veins, varicose veins, new freckles, darkening of moles, and acne flare-ups. In addition, as many as 75 per cent of pregnant women experience chloasma, which is the emergence of blotchy brown patches of skin on the face due to high estrogen levels. Chloasma is often referred to as the “mask of pregnancy.” |
18.7 Summary
- Oogenesis is the process of producing ova in the ovaries of a female fetus. Oogenesis begins when a diploid oogonium divides by mitosis to produce a diploid primary oocyte. The primary oocyte begins meiosis I and then remains at this stage in an immature ovarian follicle until after birth. By birth, a female’s ovaries contain all the eggs she will ever produce, numbering at least a million.
- After puberty, one follicle a month matures, and its primary oocyte completes meiosis I to produce a secondary oocyte, which begins meiosis II. During ovulation, the mature follicle bursts open, and the secondary oocyte leaves the ovary and enters an oviduct.
- While a follicle is maturing in an ovary each month, the endometrium in the uterus is building up to prepare for an embryo. Around the time of ovulation, cervical mucus becomes thinner and more alkaline to help sperm reach the secondary oocyte.
- If the secondary oocyte is fertilized by a sperm, it quickly completes meiosis II and forms a diploid zygote, which will continue through the oviduct. The zygote will go through multiple cell divisions before reaching and implanting in the uterus. If the secondary oocyte is not fertilized, it will not complete meiosis II, and it will soon disintegrate.
- Pregnancy is the carrying of one or more offspring from fertilization until birth. The maternal organism must provide all the nutrients and other substances needed by the developing offspring, and also remove its wastes. She should also avoid exposures that could potentially damage the offspring, especially early in the pregnancy when organ systems are developing.
- The average duration of pregnancy is 40 weeks (from the first day of the last menstrual period) and is divided into three trimesters of about three months each. Each trimester is associated with certain events and conditions that a pregnant woman may expect, such as morning sickness during the first trimester, feeling fetal movements for the first time during the second trimester, and rapid weight gain in both fetus and mother during the third trimester.
- Labour, which is the general term for the birth process, usually begins around the time the amniotic sac breaks and its fluid leaks out. Labour occurs in three stages: dilation of the cervix, birth of the baby, and delivery of the placenta (afterbirth).
- The physiological function of female breasts is lactation, or the production of breast milk to feed an infant. Sucking on the breast by the infant stimulates the release of the hypothalamic hormone oxytocin from the posterior pituitary, which causes the flow of milk. The release of milk stimulates the baby to continue sucking, which in turn keeps the milk flowing. This is one of the few examples of positive feedback in the human organism.
- The ovaries produce female sex hormones, including estrogen and progesterone. Estrogen is responsible for sexual differentiation before birth, as well as for sexual maturation and the development of secondary sex characteristics at puberty. It is also needed to help regulate the menstrual cycle and ovulation after puberty and until menopause. Progesterone prepares the uterus for pregnancy each month during the menstrual cycle, and helps maintain the pregnancy if fertilization occurs.
18.7 Review Questions
-
- What is pregnancy, and what is the role of the maternal organism in pregnancy?
- What is the average duration of pregnancy? Identify the trimesters of pregnancy.
- Define labour. What event is often a sign that labour will soon begin?
- Identify the stages of labour.
- Describe the physiological function of female breasts. How is this function controlled?
- Identify the functions of the female sex hormones estrogen and progesterone.
- Describe the roles of the cervix in fertilization and childbirth.
18.7 Explore More
https://youtu.be/XEfnq4Q4bfk
Pregnancy 101 | National Geographic, 2018.
https://youtu.be/aOfWTscU8YM
How do pregnancy tests work? - Tien Nguyen, TED-Ed, 2015.
https://youtu.be/_5OvgQW6FG4
Fertilization, Nucleus Medical Media, 2013.
https://youtu.be/xmNzUEmFZMg
The science of milk - Jonathan J. O'Sullivan, TED-Ed, 2017.
Attributions
Figure 18.7.1
Pregnant by Mustafa Omar on Unsplash is used under the Unsplash License (https://unsplash.com/license).
Figure 18.7.2
Oogenesis by Acedatrey2 on Wikimedia Commons is used under a CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0) license.
Figure 18.7.3
Blausen_0404_Fertilization by BruceBlaus on Wikimedia Commons is used under a CC BY 3.0 (https://creativecommons.org/licenses/by/3.0/deed.en) license.
Figure 18.7.4
Prenatal Diet/ Milch-Jogurt-Früchte by Peggy Greb, Agricultural Research Service (USDA) on Wikimedia Commons is in the public domain (https://commons.wikimedia.org/wiki/Public_domain).
Figure 18.7.5
Pregnancy_comparison by Maustrauser at English Wikipedia on Wikimedia Commons is in the public domain (https://commons.wikimedia.org/wiki/Public_domain).
Figure 18.7.6
Stages_of_Childbirth-02 by OpenStax on Wikimedia Commons is used under a CC BY 4.0 (https://creativecommons.org/licenses/by/4.0/) license.
Figure 18.7.7
Childhood: breast feeding [photo] by Jan Kopřiva on Unsplash is used under the Unsplash License (https://unsplash.com/license).
Figure 18.7.8
Breast-Diagram by Women's Health (NCI/ NIH) on Wikimedia Commons is in the public domain (https://commons.wikimedia.org/wiki/Public_domain).
References
Betts, J. G., Young, K.A., Wise, J.A., Johnson, E., Poe, B., Kruse, D.H., Korol, O., Johnson, J.E., Womble, M., DeSaix, P. (2013, June 19). Figure 28.21 Stages of childbirth [digital image]. In Anatomy and Physiology (Section 28.4). OpenStax. https://openstax.org/books/anatomy-and-physiology/pages/28-4-maternal-changes-during-pregnancy-labor-and-birth
Blausen.com Staff. (2014). Medical gallery of Blausen Medical 2014. WikiJournal of Medicine 1 (2). DOI:10.15347/wjm/2014.010. ISSN 2002-4436
National Geographic. (2018, December 20). Pregnancy 101 | National Geographic. YouTube. https://www.youtube.com/watch?v=XEfnq4Q4bfk&feature=youtu.be
Nucleus Medical Media. (2013, January 31). Fertilization. YouTube. https://www.youtube.com/watch?v=_5OvgQW6FG4&feature=youtu.be
TED-Ed, (2015, July 7). How do pregnancy tests work? - Tien Nguyen. YouTube. https://www.youtube.com/watch?v=aOfWTscU8YM&feature=youtu.be
TED-Ed. (2017, January 31). The science of milk - Jonathan J. O'Sullivan. YouTube. https://www.youtube.com/watch?v=xmNzUEmFZMg&feature=youtu.be
Created by CK-12 Foundation/Adapted by Christine Miller
Taboo Topic
The banner in Figure 18.8.1 was carried in a 2014 march in Uganda as part of the celebration of Menstrual Hygiene Day. Menstrual Hygiene Day is an awareness day on May 28 of each year that aims to raise awareness worldwide about menstruation and menstrual hygiene. Maintaining good menstrual hygiene is difficult in developing countries like Uganda because of taboos on discussing menstruation and lack of availability of menstrual hygiene products. Poor menstrual hygiene, in turn, can lead to embarrassment, degradation, and reproductive health problems in females. May 28 was chosen as Menstrual Hygiene Day because of its symbolism. May is the fifth month of the year, and most women average five days of menstrual bleeding each month. The 28th day was chosen because the menstrual cycle averages about 28 days.
What Is the Menstrual Cycle?
The menstrual cycle refers to natural changes that occur in the female reproductive system each month during the reproductive years. The cycle is necessary for the production of ova and the preparation of the uterus for pregnancy. It involves changes in both the ovaries and the uterus, and is controlled by pituitary and ovarian hormones. Day 1 of the cycle is the first day of the menstrual period, when bleeding from the uterus begins as the built-up endometrium lining the uterus is shed. The endometrium builds up again during the remainder of the cycle, only to be shed again during the beginning of the next cycle if pregnancy does not occur. In the ovaries, the menstrual cycle includes the development of a follicle, ovulation of a secondary oocyte, and then degeneration of the follicle if pregnancy does not occur. Both uterine and ovarian changes during the menstrual cycle are generally divided into three phases, although the phases are not the same in the two organs.
Menarche and Menopause
The female reproductive years are delineated by the start and stop of the menstrual cycle. The first menstrual period usually occurs around 12 or 13 years of age, an event that is known as menarche. There is considerable variation among individuals in the age at menarche. It may occasionally occur as early as eight years of age or as late as 16 years of age and still be considered normal. The average age is generally later in the developing world, and earlier in the developed world. This variation is thought to be largely attributable to nutritional differences.
The cessation of menstrual cycles at the end of a woman’s reproductive years is termed menopause. The average age of menopause is 52 years, but it may occur normally at any age between about 45 and 55 years of age. The age of menopause varies due to a variety of biological and environmental factors. It may occur earlier as a result of certain illnesses or medical treatments.
Variation in the Menstrual Cycle
The length of the menstrual cycle — as well as its phases — may vary considerably, not only among different women, but also from month to month for a given woman. The average length of time between the first day of one menstrual period and the first day of the next menstrual period is 28 days, but it may range from 21 days to 45 days. Cycles are considered regular when a woman’s longest and shortest cycles differ by less than eight days. The menstrual period itself is usually about five days long, but it may vary in length from about two days to seven days.
Ovarian Cycle
The events of the menstrual cycle that take place in the ovaries make up the ovarian cycle. It consists of changes that occur in the follicles of one of the ovaries. The ovarian cycle is divided into the following three phases: follicular phase, ovulation, and luteal phase. These phases are illustrated in Figure 18.8.2.
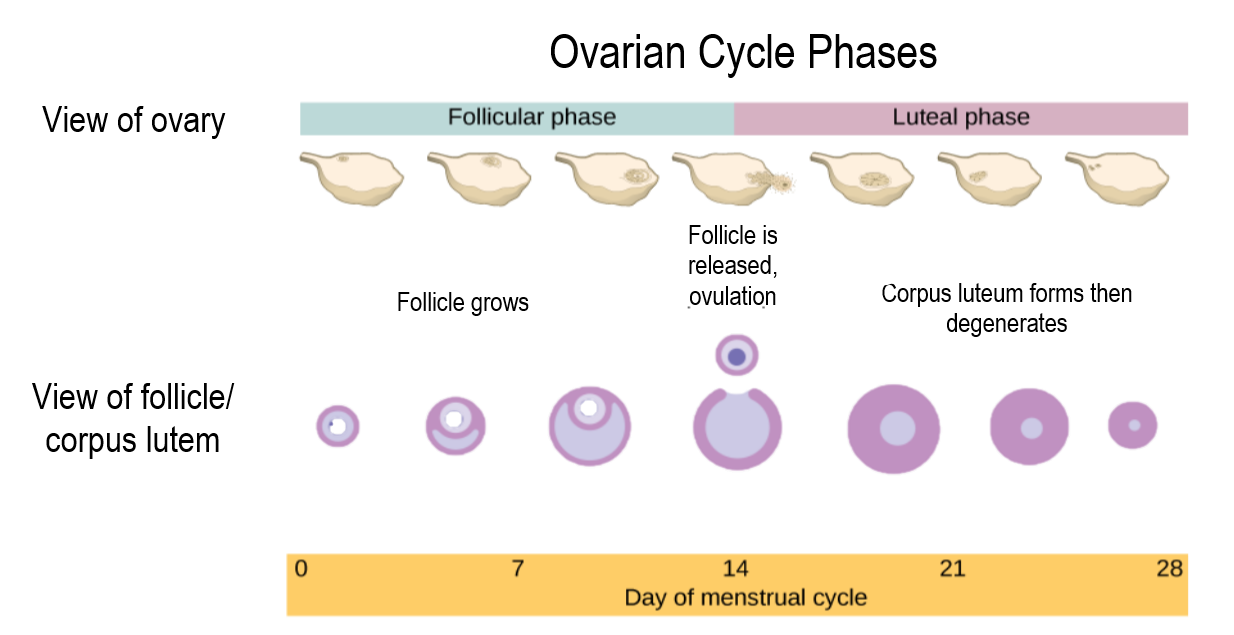
Follicular Phase
The follicular phase is the first phase of the ovarian cycle. It generally lasts about 12 to 14 days for a 28-day menstrual cycle. During this phase, several ovarian follicles are stimulated to begin maturing, but usually only one — called the Graafian follicle — matures completely so it is ready to release an egg. The other maturing follicles stop growing and disintegrate. Follicular development occurs because of a rise in the blood level of follicle stimulating hormone (FSH), which is secreted by the pituitary gland. The maturing follicle releases estrogen, the level of which rises throughout the follicular phase. You can see these and other changes in hormone levels that occur during the menstrual cycle in the following chart.
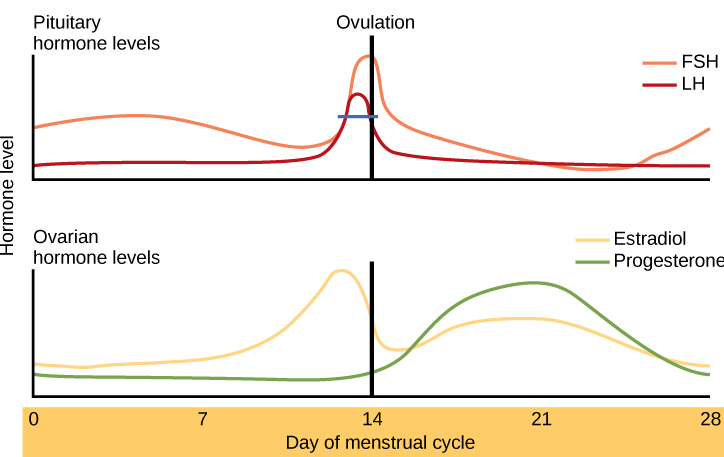
Ovulation
Ovulation is the second phase of the ovarian cycle. It usually occurs around day 14 of a 28-day menstrual cycle. During this phase, the Graafian follicle ruptures and releases its ovum. Ovulation is stimulated by a sudden rise in the blood level of luteinizing hormone (LH) from the pituitary gland. This is called the LH surge. You can see the LH surge in the top hormone graph in Figure 18.8.3. The LH surge generally starts around day 12 of the cycle and lasts for a day or two. The surge in LH is triggered by a continued rise in estrogen from the maturing follicle in the ovary. During the follicular phase, the rising estrogen level actually suppresses LH secretion by the pituitary gland. However, by the time the follicular phase is nearing its end, the level of estrogen reaches a threshold level above which this effect is reversed, and estrogen stimulates the release of a large amount of LH. The surge in LH matures the ovum and weakens the wall of the follicle, causing the fully developed follicle to release its secondary oocyte.
Luteal Phase
The luteal phase is the third and final phase of the ovarian cycle. It typically lasts about 14 days in a 28-day menstrual cycle. At the beginning of the luteal phase, FSH and LH cause the Graafian follicle that ovulated the egg to transform into a structure called a corpus luteum. The corpus luteum secretes progesterone, which in turn suppresses FSH and LH production by the pituitary gland and stimulates the continued buildup of the endometrium in the uterus. How this phase ends depends on whether or not the ovum has been fertilized.
- If fertilization has not occurred, the falling levels of FSH and LH during the luteal phase cause the corpus luteum to atrophy, so its production of progesterone declines. Without a high level of progesterone to maintain it, the endometrium starts to break down. By the end of the luteal phase, the endometrium can no longer be maintained, and the next menstrual cycle begins with the shedding of the endometrium (menses).
- If fertilization has occurred so a zygote forms and then divides to become a blastocyst, the outer layer of the blastocyst produces a hormone called human chorionic gonadotropin (HCG). This hormone is very similar to LH and preserves the corpus luteum. The corpus luteum can then continue to secrete progesterone to maintain the new pregnancy.
Uterine Cycle
The events of the menstrual cycle that take place in the uterus make up the uterine cycle. This cycle consists of changes that occur mainly in the endometrium, which is the layer of tissue that lines the uterus. The uterine cycle is divided into the following three phases: menstruation, proliferative phase, and secretory phase. These phases are illustrated in Figure 18.8.4.
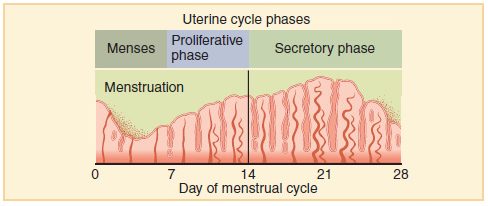
Menstruation
Menstruation (also called menstrual period or menses) is the first phase of the uterine cycle. It occurs if fertilization has not taken place during the preceding menstrual cycle. During menstruation, the endometrium of the uterus, which has built up during the preceding cycle, degenerates and is shed from the uterus, flowing through an opening in the cervix, and out through the external opening of the vagina. The average loss of blood during menstruation is about 35 mL (about 1 oz or 2 tablespoons). The flow of blood is often accompanied by uterine cramps, which may be severe in some women.
Proliferative Phase
The proliferative phase is the second phase of the uterine cycle. During this phase, estrogen secreted by cells of the maturing ovarian follicle causes the lining of the uterus to grow, or proliferate. Estrogen also stimulates the cervix of the uterus to secrete larger amounts of thinner mucus that can help sperm swim through the cervix and into the uterus, making fertilization more likely.
Secretory Phase
The secretory phase is the third and final phase of the uterine cycle. During this phase, progesterone produced by the corpus luteum in the ovary stimulates further changes in the endometrium so it is more receptive to implantation of a blastocyst. For example, progesterone increases blood flow to the uterus and promotes uterine secretions. It also decreases the contractility of smooth muscle tissue in the uterine wall.
Bringing it All Together
It is important to note that the pituitary gland, the ovaries and the uterus are all responsible for parts of the ovarian and uterine cycles. The pituitary hormones, LH and FSH affect the ovarian cycle and its hormones. The ovarian hormones, estrogen and progesterone affect the uterine cycle and also feedback on the pituitary gland. Look at Figure 18.8.5 and look at what is happening on different days of the cycle in each of the sets of hormones, the ovarian cycle and the uterine cycle.
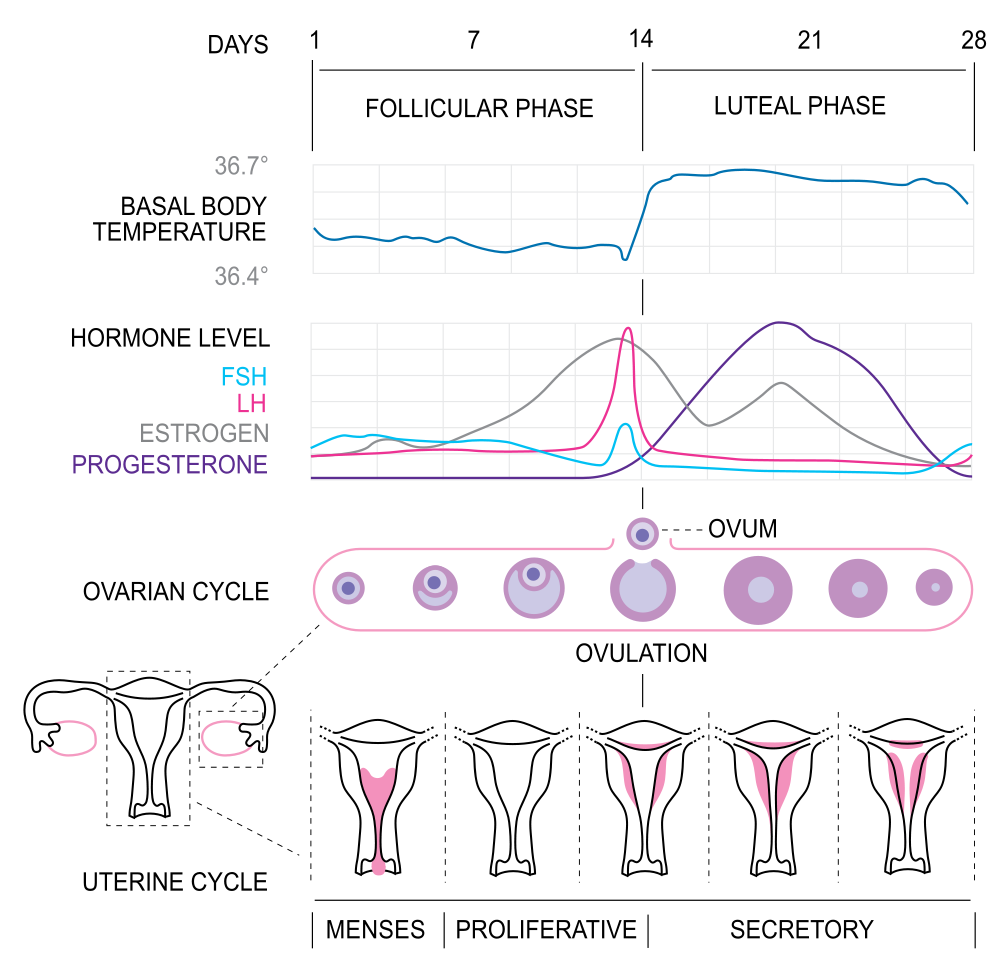
18.8 Summary
- The menstrual cycle refers to natural changes that occur in the female reproductive system each month during the reproductive years, except when a woman is pregnant. The cycle is necessary for the production of ova and the preparation of the uterus for pregnancy. It involves changes in both the ovaries and uterus, and is controlled by pituitary gland hormones (FSH and LH) and ovarian hormones (estrogen and progesterone).
- The female reproductive period is delineated by menarche, or the first menstrual period, which usually occurs around age 12 or 13; and by menopause, or the cessation of menstrual periods, which typically occurs around age 52. A typical menstrual cycle averages 28 days in length but may vary normally from 21 to 45 days. The average menstrual period is five days long, but may vary normally from two to seven days. These variations in the menstrual cycle may occur both between women and within individual women from month to month.
- The events of the menstrual cycle that take place in the ovaries make up the ovarian cycle. It includes the follicular phase (when a follicle and its ovum mature due to rising levels of FSH), ovulation (when the ovum is released from the ovary due to a rise in estrogen and a surge in LH), and the luteal phase (when the follicle is transformed into a structure called a corpus luteum that secretes progesterone). In a 28-day menstrual cycle, the follicular and luteal phases typically average about two weeks in length, with ovulation generally occurring around day 14 of the cycle.
- The events of the menstrual cycle that take place in the uterus make up the uterine cycle. It includes menstruation, which generally occurs on days 1 to 5 of the cycle and involves shedding of endometrial tissue that built up during the preceding cycle; the proliferative phase, during which the endometrium builds up again until ovulation occurs; and the secretory phase, which follows ovulation and during which the endometrium secretes substances and undergoes other changes that prepare it to receive an embryo.
18.8 Review Questions
-
- What is the menstrual cycle? Why is the menstrual cycle necessary in order for pregnancy to occur?
- What organs are involved in the menstrual cycle?
- Identify the two major events that mark the beginning and end of the reproductive period in females. When do these events typically occur?
- Discuss the average length of the menstrual cycle and menstruation, as well as variations that are considered normal.
- If the LH surge did not occur in a menstrual cycle, what do you think would happen? Explain your answer.
- Give one reason why FSH and LH levels drop in the luteal phase of the menstrual cycle.
18.8 Explore More
https://youtu.be/cjbgZwgdY7Q
Why do women have periods? TED-Ed, 2015.
https://youtu.be/5B3Abpv0ysM
Girl's Rite of Passage | National Geographic, 2007.
Attributions
Figure 18.8.1
WaterforPeople_Uganda by WaterforPeople_Uganda on Wikimedia Commons is used under a CC BY 2.0 (https://creativecommons.org/licenses/by/2.0) license.
Figure 18.8.2
Ovarian Cycle by CNX OpenStax on Wikimedia Commons is used and adapted under a CC BY 4.0 (https://creativecommons.org/licenses/by/4.0) license.
Figure 18.8.3
Figure_43_04_04 by CNX OpenStax on Wikimedia Commons is used under a CC BY 4.0 (https://creativecommons.org/licenses/by/4.0) license. (Original: modification of work by Mikael Häggström)
Figure 18.8.4
Ovarian and menstrual cycle by OpenStax College on Wikimedia Commons is used under a CC BY 3.0 (https://creativecommons.org/licenses/by/3.0) license.
Figure 18.8.5
1000px-MenstrualCycle2_en.svg by Isometrik on Wikimedia Common is used under a CC BY-SA 3.0 (https://creativecommons.org/licenses/by-sa/3.0) license.
References
Betts, J. G., Young, K.A., Wise, J.A., Johnson, E., Poe, B., Kruse, D.H., Korol, O., Johnson, J.E., Womble, M., DeSaix, P. (2013, June 19). Figure 27.15 Hormone levels in ovarian and menstrual cycles [digital image]. In Anatomy and Physiology (Section 27.2). OpenStax. https://openstax.org/books/anatomy-and-physiology/pages/27-2-anatomy-and-physiology-of-the-female-reproductive-system
National Geographic. (2007, May 31). Girl's rite of passage | National Geographic. YouTube. https://www.youtube.com/watch?v=5B3Abpv0ysM&feature=youtu.be
OpenStax. (2016, May 27) Figure 4 Rising and falling hormone levels result in progression of the ovarian and menstrual cycles [digital image]. In Open Stax, Biology (Section 43.4). OpenStax CNX. https://cnx.org/contents/GFy_h8cu@10.53:Ha3dnFEx@6/Hormonal-Control-of-Human-Reproduction
TED-Ed. (2015, October 19). Why do women have periods? YouTube. https://www.youtube.com/watch?v=cjbgZwgdY7Q&feature=youtu.be
Created by CK-12 Foundation/Adapted by Christine Miller

Vaccinating Against Cancer
Can a vaccine prevent cancer? In the case of cervical cancer, it can. Cervical cancer is one of three disorders of the female reproductive system described in detail in this concept. Of the three, only cervical cancer can be prevented with a vaccine.
Cervical Cancer
Cervical cancer occurs when cells of the cervix (neck of the uterus) grow abnormally and develop the ability to invade nearby tissues or spread to other parts of the body, such as the abdomen or lungs. Figure 18.9.2 shows the location of the cervix and the appearance of normal and abnormal cervical cells when examined with a microscope.
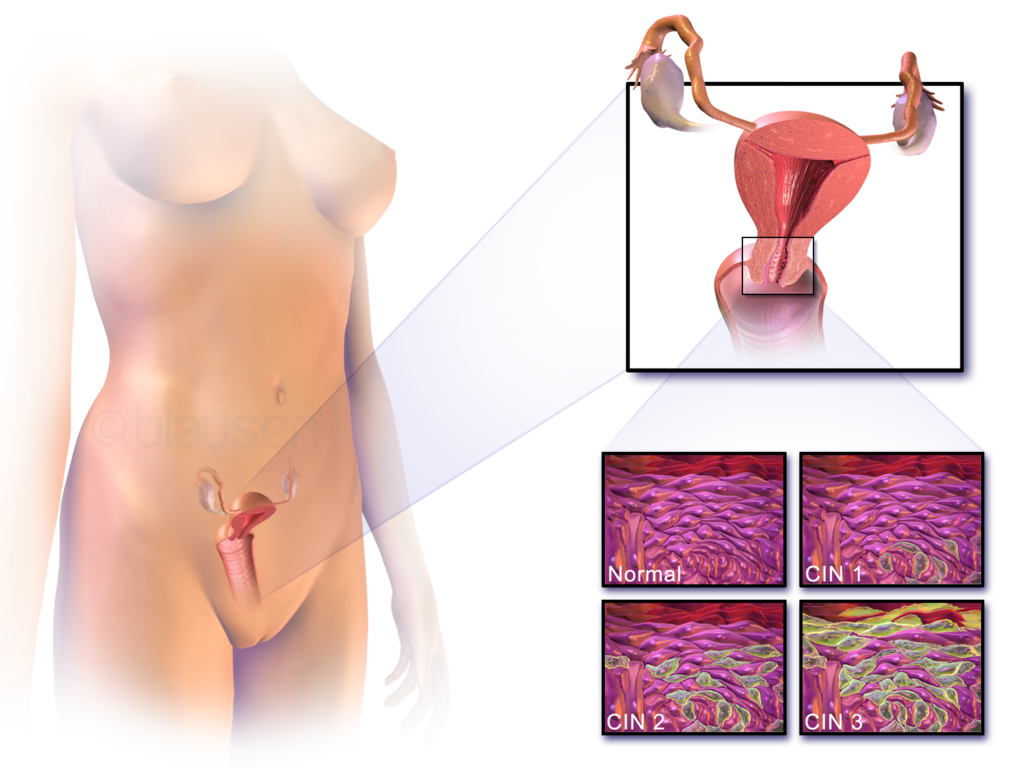
Cervical Cancer Prevalence and Death Rates
Worldwide, cervical cancer is the second most common type of cancer in females (after breast cancer) and the fourth-most common cause of cancer death in females. In Canada and other high-income nations, the widespread use of cervical cancer screening has detected many cases of precancerous cervical changes and has dramatically reduced rates of cervical cancer deaths. About 75% of cervical cancer cases occur in developing countries, where routine screening is less likely because of cost and other factors. Cervical cancer is also the most common cause of cancer death in low-income countries.
Symptoms of Cervical Cancer
Early in the development of cervical cancer, there are typically no symptoms. As the disease progresses, however, symptoms are likely to occur. The symptoms may include abnormal vaginal bleeding, pelvic pain, or pain during sexual intercourse. Unfortunately, by the time symptoms start to occur, cervical cancer has typically progressed to a stage at which treatment is less likely to be successful.
Cervical Cancer Causes and Risk Factors
More than 90 per cent of cases of cervical cancer are caused at least in part by human papillomavirus (HPV), which is a sexually transmitted virus that also causes genital warts. Figure 18.9.3 shows how HPV infection can cause cervical cancer by interfering with a normal cell division checkpoint. When HPV is not present, cervical cells containing mutations are not allowed to divide, so the cervix remains healthy. When HPV is present, however, cervical cells with mutations may be allowed to divide, leading to uncontrolled growth of mutated cells and the formation of a tumor.
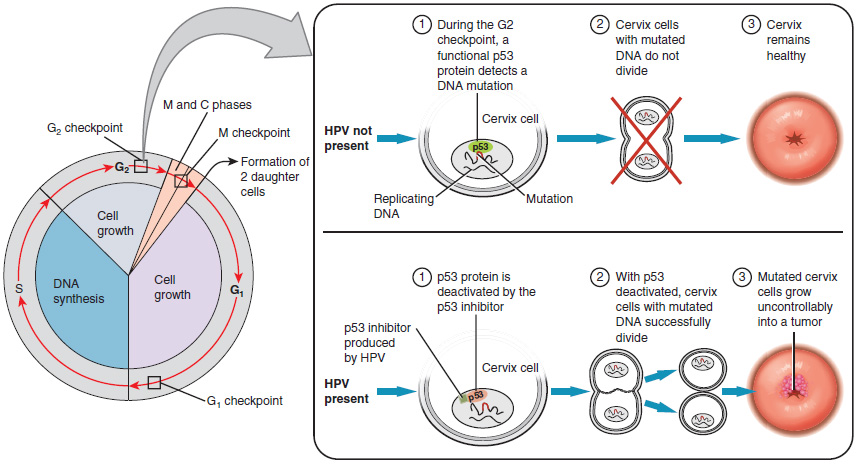
Other risk factors for cervical cancer include smoking, a weakened immune system (for example, due to HIV infection), use of birth control pills, becoming sexually active at a young age, and having many sexual partners. However, these risk factors are less important than HPV infection. Instead, the risk factors are more likely to increase the risk of cervical cancer in females who are already infected with HPV. For example, among HPV-infected women, current and former smokers have roughly two to three times the incidence of cervical cancer as non-smokers. Passive smoking, or secondhand smoke, is also associated with an increased risk of cervical cancer, but to a lesser extent.
Diagnosis of Cervical Cancer
Diagnosis of cervical cancer is typically made by looking for microscopic abnormal cervical cells in a smear of cells scraped off the cervix. This is called a Pap smear. If cancerous cells are detected or suspected in the smear, this test is usually followed up with a biopsy to confirm the Pap smear results. Medical imaging (by CT scan or MRI, for example) is also likely to be done to provide more information, such as whether the cancer has spread.
Prevention of Cervical Cancer
It is now possible to prevent HPV infection with a vaccine. The first HPV vaccine was approved by the U.S. Food and Drug Administration in 2006. The vaccine protects against the strains of HPV that have the greatest risk of causing cervical cancer. It is thought that widespread use of the vaccine will prevent up to 90% of cervical cancer cases. Current recommendations are for females to be given the vaccine between the ages of nine and 26. (Boys should be vaccinated against HPV, as well, because the virus may also cause cancer of the penis and certain other male cancers.) The vaccine is effective only if it is given before HPV infection has occurred. Using condoms during sexual intercourse can also help prevent HPV infection and cervical cancer, in addition to preventing pregnancy and sexually transmitted infections (such as HIV).
Even in women who have received the HPV vaccine, there is still a small risk of developing cervical cancer. Therefore, it is recommended that women continue to be examined with regular Pap smears.
Treatment of Cervical Cancer
Treatment of cervical cancer generally depends on the stage at which the cancer is diagnosed, but it is likely to include some combination of surgery, radiation therapy, and/or chemotherapy. Outcomes of treatment depend largely on how early the cancer is diagnosed and treated. For surgery to cure cervical cancer, the entire tumor must be removed with no cancerous cells found at the margins of the removed tissue on microscopic examination. If cancer is found and treated very early when it is still in the microscopic stage, the five-year survival rate is virtually 100%.
Vaginitis
Vaginitis is inflammation of the vagina — and sometimes the vulva, as well. Symptoms may include a discharge that is yellow, gray, or green; itching; pain; and a burning sensation. There may also be a foul vaginal odor and pain or irritation with sexual intercourse.
Causes of Vaginitis
About 90% of cases of vaginitis are caused by infection with microorganisms. Most commonly, vaginal infections are caused by the yeast Candida albicans (see Figure 18.9.4). Such infections are referred to as vaginal candidiasis or more commonly as a yeast infection. Candida albicans is one of the most common opportunistic infections in the world and can affect not only the vagina, but any of the mucus membranes and skin. Other possible causes of vaginal infections include bacteria, especially Gardnerella vaginalis, and some single-celled parasites, notably the protist parasite Trichomonas vaginalis, which is usually transmitted through vaginal intercourse. The risk of vaginal infections may be greater in women who wear tight clothing, are taking antibiotics for another condition, use birth control pills, or have improper hygiene. Poor hygiene allows organisms that are normally present in the stool (such as yeast) to contaminate the vagina.
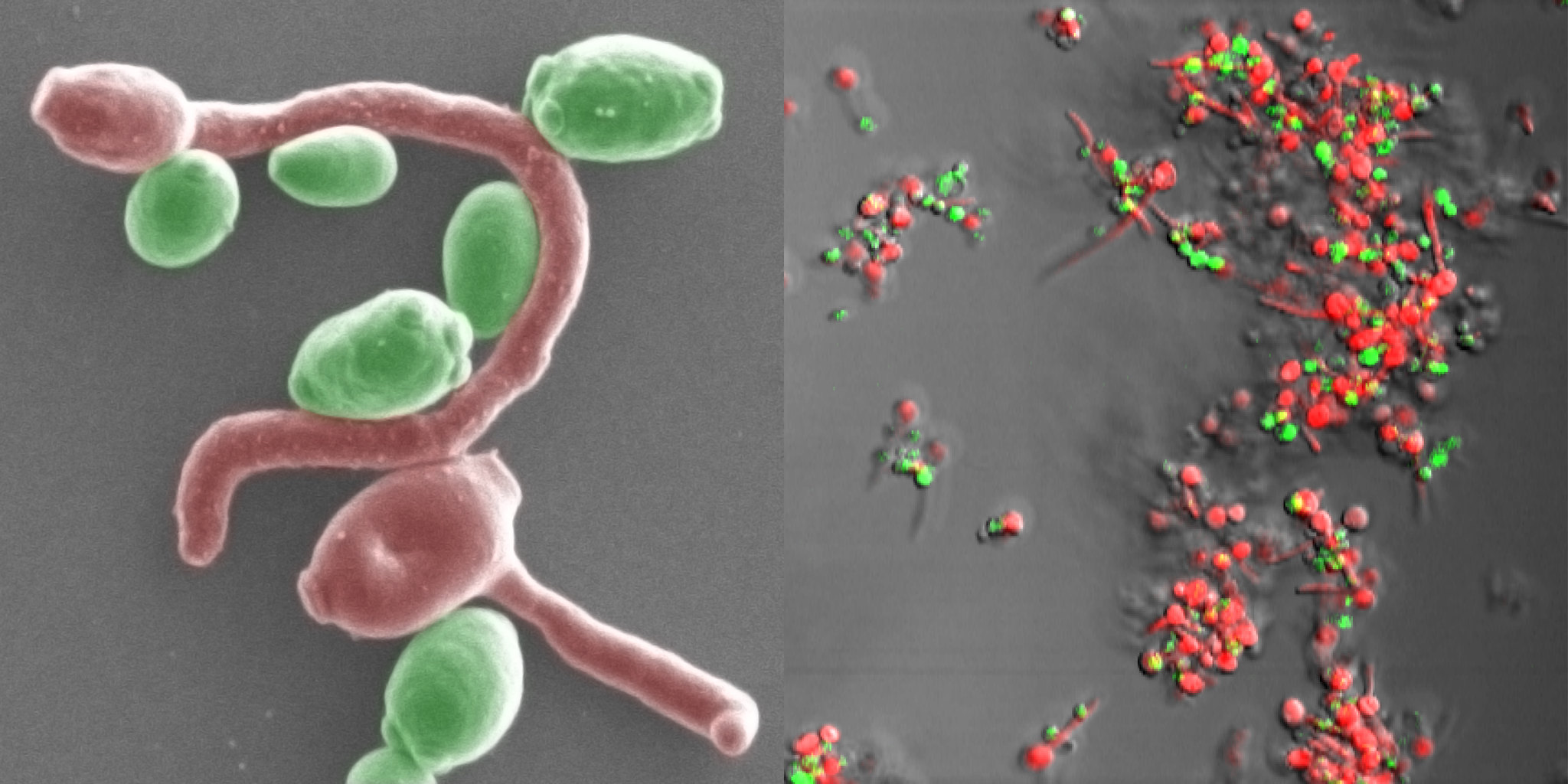
Most of the remaining cases of vaginitis are due to irritation by — or allergic reactions to — various products. These irritants may include condoms, spermicides, soaps, douches, lubricants, and even semen. Using tampons or soaking in hot tubs may be additional causes of this type of vaginitis.
Diagnosis of Vaginitis
Diagnosis of vaginitis typically begins with symptoms reported by the patient. This may be followed by a microscopic examination or culture of the vaginal discharge in order to identify the specific cause. The colour, consistency, acidity, and other characteristics of the discharge may be predictive of the causative agent. For example, infection with Candida albicans may cause a cottage cheese-like discharge with a low pH, whereas infection with Gardnerella vaginalis may cause a discharge with a fish-like odor and a high pH.
Prevention of Vaginitis
Prevention of vaginitis includes wearing loose cotton underwear that helps keep the vulva dry. Yeasts and bacteria that may cause vaginitis tend to grow best in a moist environment. It is also important to avoid the use of perfumed soaps, personal hygiene sprays, and douches, all of which may upset the normal pH and bacterial balance in the vagina. To help avoid vaginitis caused by infection with Trichomonas vaginalis, the use of condoms during sexual intercourse is advised.
Treatment of Vaginitis
The appropriate treatment of vaginitis depends on the cause. In many cases of vaginitis, there is more than one cause, and all of the causes must be treated to ensure a cure.
- Yeast infections of the vagina are typically treated with topical anti-fungal medications, which are available over the counter. The medications may be in the form of tablets or creams that are inserted into the vagina. Depending on the particular medication used, treatment may involve one, three, or seven days of applications.
- Bacterial infections of the vagina are usually treated with antibiotics. These may be taken orally as pills, or applied topically to the vagina in creams.
- Trichomonas vaginalis infections of the vagina are generally treated with a single dose of an oral antibiotic. Sexual partners should be treated at the same time, and intercourse should be avoided for at least a week until both partners have completed treatment, and have been followed-up by a physician.
Endometriosis
Endometriosis is a disease in which endometrial tissue, which normally grows inside the uterus, grows outside it, as shown in Figure 18.9.5. Most often, the endometrial tissue grows around the ovaries, Fallopian tubes, and uterus. In rare instances, the tissue may grow elsewhere in the body. The areas of endometriosis typically bleed each month during the menstrual period, and this often results in inflammation, pain, and scarring. An estimated six to ten per cent of women are believed to have endometriosis. It is most common in women during their thirties and forties, and only rarely occurs before menarche or after menopause.
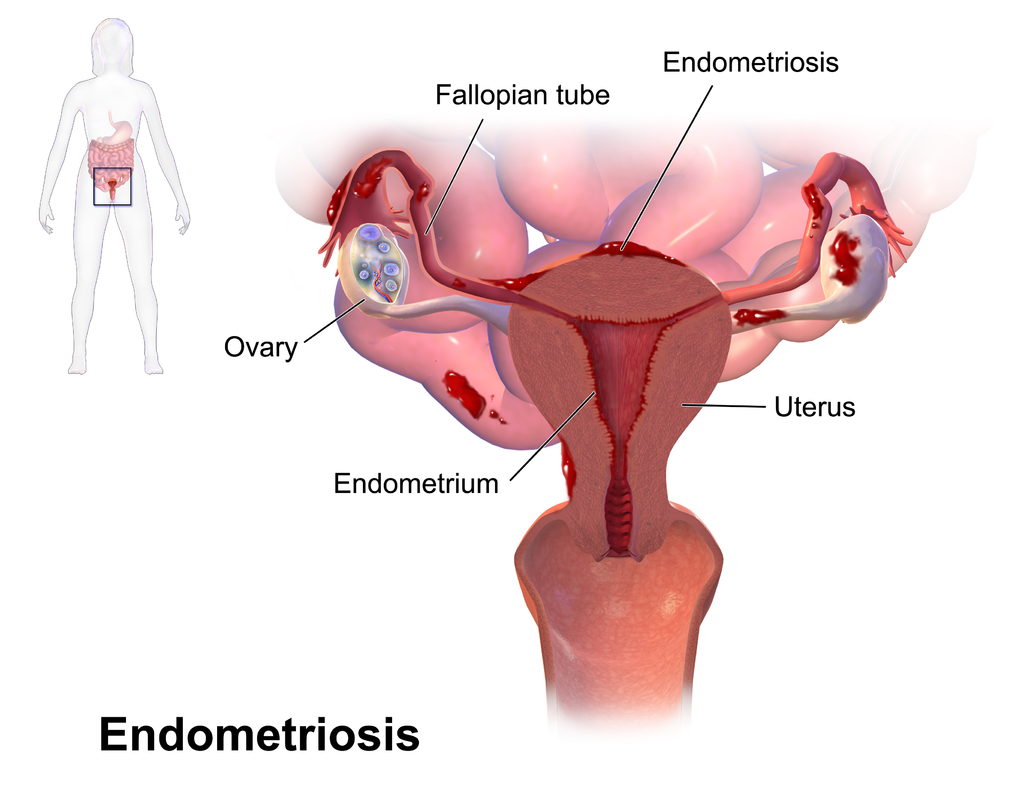
Signs and Symptoms of Endometriosis
The main symptom of endometriosis is pelvic pain, which may range from mild to severe. There appears to be little or no relationship between the amount of endometrial tissue growing outside the uterus and the severity of the pain. For many women with the disease, the pain occurs mainly during menstruation. However, nearly half of those affected have chronic pelvic pain. The pain of endometriosis may be caused by bleeding in the pelvis, which triggers inflammation. Pain can also occur from internal scar tissue that binds internal organs to each other.
Another problem often associated with endometriosis is infertility, or the inability to conceive or bear children. Among women with endometriosis, up to half may experience infertility. Infertility can be related to scar formation or to anatomical distortions due to the abnormal endometrial tissue. Other possible symptoms of endometriosis may include diarrhea or constipation, chronic fatigue, nausea and vomiting, headaches, and heavy or irregular menstrual bleeding.
Causes of Endometriosis
The causes of endometriosis are not known for certain, but several risk factors have been identified, including a family history of endometriosis. Daughters or sisters of women with endometriosis have about six times the normal risk of developing the disease themselves. It has been suggested that endometriosis results from mutations in several genes. It is likely that endometriosis is multifactorial, involving the interplay of several factors.
At the physiological level, the predominant idea for how endometriosis comes about is retrograde menstruation. This happens when some of the endometrial debris from a woman’s menstrual flow exits the uterus through the oviducts, rather than through the vagina. The debris then attaches itself to the outside of organs in the abdominal cavity, or to the lining of the abdominal cavity itself. Retrograde menstruation, however, does not explain all cases of endometriosis, so other factors are apparently involved. Suggestions include environmental toxins and autoimmune responses.
Diagnosis of Endometriosis
Diagnosis of endometriosis is usually based on self-reported symptoms and a physical examination by a doctor, often combined with medical imaging, such as ultrasonography. The only way to definitively diagnose endometriosis, however, is through visual inspection of the endometrial tissue. This can be done with a surgical procedure called laparoscopy, shown in Figure 18.9.6, in which a tiny camera is inserted into the abdomen through a small incision. The camera allows the physician to visually inspect the area where endometrial tissue is suspected.
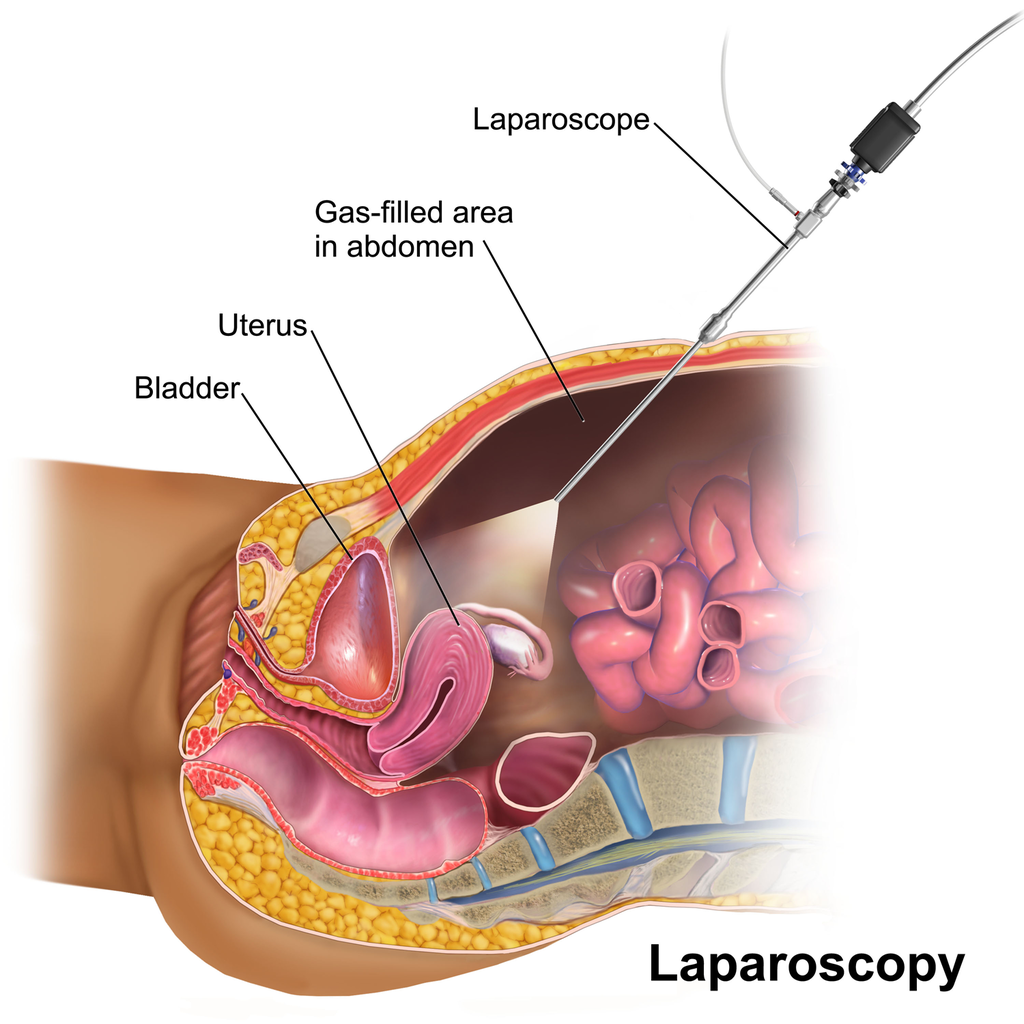
Treatment of Endometriosis
The most common treatments for endometriosis are medications to control the pain, and surgery to remove the abnormal tissue. Frequently used pain medications are non-steroidal inflammatory drugs (NSAIDS), such as naproxen. Opiates may be used in cases of severe pain. Laparoscopy can be used to surgically treat endometriosis, as well as to diagnose the condition. In this type of surgery, an additional small incision is made to insert instruments that the surgeon can manipulate externally in order to burn (cauterize) or cut away the endometrial growths. In younger women who want to have children, surgery is conservative to keep the reproductive organs intact and functional. However, with conservative surgery, endometriosis recurs in 20–40% of cases within five years of the surgery. In older women who have completed childbearing, hysterectomy may be undertaken to remove all or part of the internal reproductive organs. This is the only procedure that is likely to cure endometriosis and prevent relapses.
Feature: My Human Body
A Pap smear is a method of cervical cancer screening used to detect potentially pre-cancerous and cancerous cells in the cervix. It is the most widely used screening test for this type of cancer, and it is very effective. The test may also detect vaginal infections and abnormal endometrial cells, but it is not designed for these purposes.
According to HealthLink BC, females should start receiving routine Pap smears by age 25. Because most cases of cervical cancer are caused by infection with human papillomavirus (HPV), which is a sexually transmitted infection, there is little or no benefit to screening people who have not had sexual contact. Starting at age 25, general guidelines are for Pap smears to be repeated every three years until age 69. Screening may be discontinued after 69 years of age, if the last three Pap smears were normal. If a woman has a complete hysterectomy, she no longer has a cervix and there is no need for further Pap smears. On the other hand, if a woman has had a history of abnormal Pap smears or cancer, she will likely be screened more frequently. Pap smears can be done safely during the first several months of pregnancy, and resumed about three months after childbirth. Generally, better results are obtained if Pap smears are not done during menstruation.
If you’ve never had a Pap smear, knowing what to expect may help prepare you for the procedure. The patient lies on the examining table with her feet in “stirrups” to hold the legs up and apart. An instrument called a speculum is inserted into the vagina to hold back the vaginal walls and give access to the cervix. A tiny amount of tissue is brushed off the cervix and smeared onto a microscope slide. The speculum is then removed, and the procedure is over. The slide is later examined under a microscope for abnormal cells. Some women experience light spotting or mild diarrhea after a Pap smear, but most have no lasting effects.
Pap smears are uncomfortable and may be somewhat painful for some women. If you experience pain during a Pap smear, tell your health care provider. Many steps can be taken to minimize the pain, which might include using a smaller speculum, using warm instruments and a lubricant, and applying a topical anesthetic such as lidocaine to the cervix before obtaining the smear. Any pain is generally very brief, and the potential reward is worth it. Pap tests are estimated to reduce up to 80% of cervical cancer deaths. One of the lives saved could be your own.
18.9 Summary
- Cervical cancer occurs when cells of the cervix grow abnormally and develop the ability to invade nearby tissues or spread to other parts of the body. Worldwide, cervical cancer is the second-most common type of cancer in females and the fourth-most common cause of cancer death in females. Early on, cervical cancer often has no symptoms. Later, symptoms (such as abnormal vaginal bleeding and pain) are likely.
- Most cases of cervical cancer occur because of infection with human papillomavirus (HPV), so the HPV vaccine is expected to greatly reduce the incidence of the disease. Other risk factors include smoking and a weakened immune system. A Pap smear can diagnose cervical cancer at an early stage. Where Pap smears are done routinely, cervical cancer death rates have fallen dramatically. Treatment of cervical cancer generally includes surgery, which may be followed by radiation therapy or chemotherapy.
- Vaginitis is inflammation of the vagina. A discharge is likely, and there may be itching and pain. About 90% of cases of vaginitis are caused by infection with microorganisms, typically by the yeast Candida albicans. A minority of cases are caused by irritants or allergens in soaps, spermicides, or douches.
- Diagnosis of vaginitis may be based on characteristics of the discharge, which can be examined microscopically or cultured. Treatment of vaginitis depends on the cause and is usually an oral or topical anti-fungal or antibiotic medication.
- Endometriosis is a disease in which endometrial tissue grows outside the uterus. This tissue may bleed during the menstrual period and cause inflammation, pain, and scarring. The main symptom of endometriosis is pelvic pain, which may be severe. Endometriosis may also lead to infertility.
- Endometriosis is thought to have multiple causes, including genetic mutations. Retrograde menstruation may be the immediate cause of endometrial tissue escaping the uterus and entering the pelvic cavity. Endometriosis is usually treated with surgery to remove the abnormal tissue and medication for pain. If surgery is more conservative than hysterectomy, endometriosis may recur.
18.9 Review Questions
- What is cervical cancer? Worldwide, how prevalent is it, and how does it rank as a cause of cancer deaths?
- Identify symptoms of cervical cancer. What are causes of — and risk factors for — cervical cancer?
- What roles can Pap smears and HPV vaccines play in preventing cervical cancer cases and cervical cancer deaths?
- How is cervical cancer treated?
- Define vaginitis and identify its symptoms.
- What are some of the causes of vaginitis? Which cause is responsible for most of the cases?
- How is vaginitis diagnosed and treated?
- What is endometriosis, and what are its symptoms?
- Discuss possible causes of endometriosis.
- How is endometriosis treated? Which treatment is most likely to prevent recurrence of the disorder?
-
- In the case of infection with Trichomonas vaginalis, why is the woman’s sexual partner usually treated at the same time?
18.9 Explore More
https://youtu.be/KOz-bNhEHhQ
What is HPV and how can you protect yourself from it? - Emma Bryce, TED-Ed, 2019.
https://youtu.be/6HeQ4iEqAUk
Endometriosis - The Mystery Disease of Women | Cécile Real | TEDxBinnenhof, TEDx Talks, 2016.
https://youtu.be/ryNjSP5VVI8
The brain and ovarian hormones | Marwa Azab | TEDxMontrealWomen, TEDxTalks, 2015.
Attributions
Figure 18.9.1
a-nurse-giving-a-young-girl-a-vaccine-shot-or by CDC/ Judy Schmidt from Public Health Image Library (PHIL) #9424 is in the public domain (https://en.wikipedia.org/wiki/Public_domain).
Figure 18.9.2
1024px-Blausen_0221_CervicalDysplasia by Blausen Medical Communications, Inc. on Wikimedia Commons is used under a CC BY 3.0 (https://creativecommons.org/licenses/by/3.0) license.
Figure 18.9.3
HPV and Cervical Cancer by OpenStax by OpenStax College on Wikimedia Commons is used under a CC BY 3.0 (https://creativecommons.org/licenses/by/3.0) license.
Figure 18.9.4
Candida by NIH on Flickr from the NIH Image Gallery on Flickr is used under a CC BY NC 2.0 (https://creativecommons.org/licenses/by-nc/2.0/) license.
Figure 18.9.5
Blausen_0349_Endometriosis by BruceBlaus on Wikimedia Commons is used under a CC BY 3.0 (https://creativecommons.org/licenses/by/3.0) license.
Figure 18.9.6
1024px-Blausen_0602_Laparoscopy_02 by BruceBlaus on Wikimedia Commons is used under a CC BY 3.0 (https://creativecommons.org/licenses/by/3.0) license.
References
Betts, J. G., Young, K.A., Wise, J.A., Johnson, E., Poe, B., Kruse, D.H., Korol, O., Johnson, J.E., Womble, M., DeSaix, P. (2013, June 19). Figure 27.16 Development of cervical cancer [digital image]. In Anatomy and Physiology (Section 27.2). OpenStax. https://openstax.org/books/anatomy-and-physiology/pages/27-2-anatomy-and-physiology-of-the-female-reproductive-system
Blausen.com Staff. (2014). Medical gallery of Blausen Medical 2014. WikiJournal of Medicine 1 (2). DOI:10.15347/wjm/2014.010. ISSN 2002-4436.
HealthLink BC. (n.d.). Pap test: British Columbia specific information. https://www.healthlinkbc.ca/medical-tests/hw5266
TED-Ed. (2019, July 9). What is HPV and how can you protect yourself from it? - Emma Bryce. YouTube. https://www.youtube.com/watch?v=KOz-bNhEHhQ&feature=youtu.be
TEDx Talks. (2016, April 14). Endometriosis - The mystery disease of women | Cécile Real | TEDxBinnenhof. YouTube. https://www.youtube.com/watch?v=6HeQ4iEqAUk&feature=youtu.be
TEDx Talks. (2015, July 27). The brain and ovarian hormones | Marwa Azab | TEDxMontrealWomen. YouTube. https://www.youtube.com/watch?v=ryNjSP5VVI8&feature=youtu.be
Created by CK-12 Foundation/Adapted by Christine Miller

Communicating with Urine
Why do dogs pee on fire hydrants? Besides “having to go,” they are marking their territory with chemicals in their urine called pheromones. It’s a form of communication, in which they are “saying” with odors that the yard is theirs and other dogs should stay away. In addition to fire hydrants, dogs may urinate on fence posts, trees, car tires, and many other objects. Urination in dogs, as in people, is usually a voluntary process controlled by the brain. The process of forming urine — which occurs in the kidneys — occurs constantly, and is not under voluntary control. What happens to all the urine that forms in the kidneys? It passes from the kidneys through the other organs of the urinary system, starting with the ureters.
Ureters
As shown in Figure 16.5.2, ureters are tube-like structures that connect the kidneys with the urinary bladder. They are paired structures, with one ureter for each kidney. In adults, ureters are between 25 and 30 cm (about 10–12 in) long and about 3 to 4 mm in diameter.
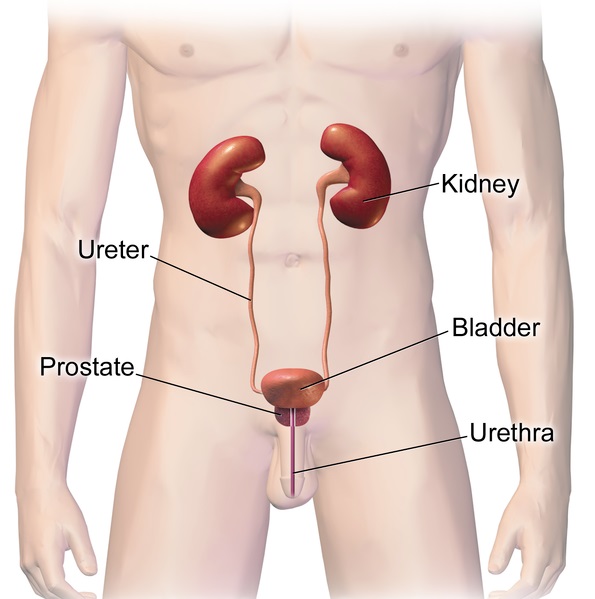
Each ureter arises in the pelvis of a kidney (the renal pelvis in Figure 16.5.3). It then passes down the side of the kidney, and finally enters the back of the bladder. At the entrance to the bladder, the ureters have sphincters that prevent the backflow of urine.
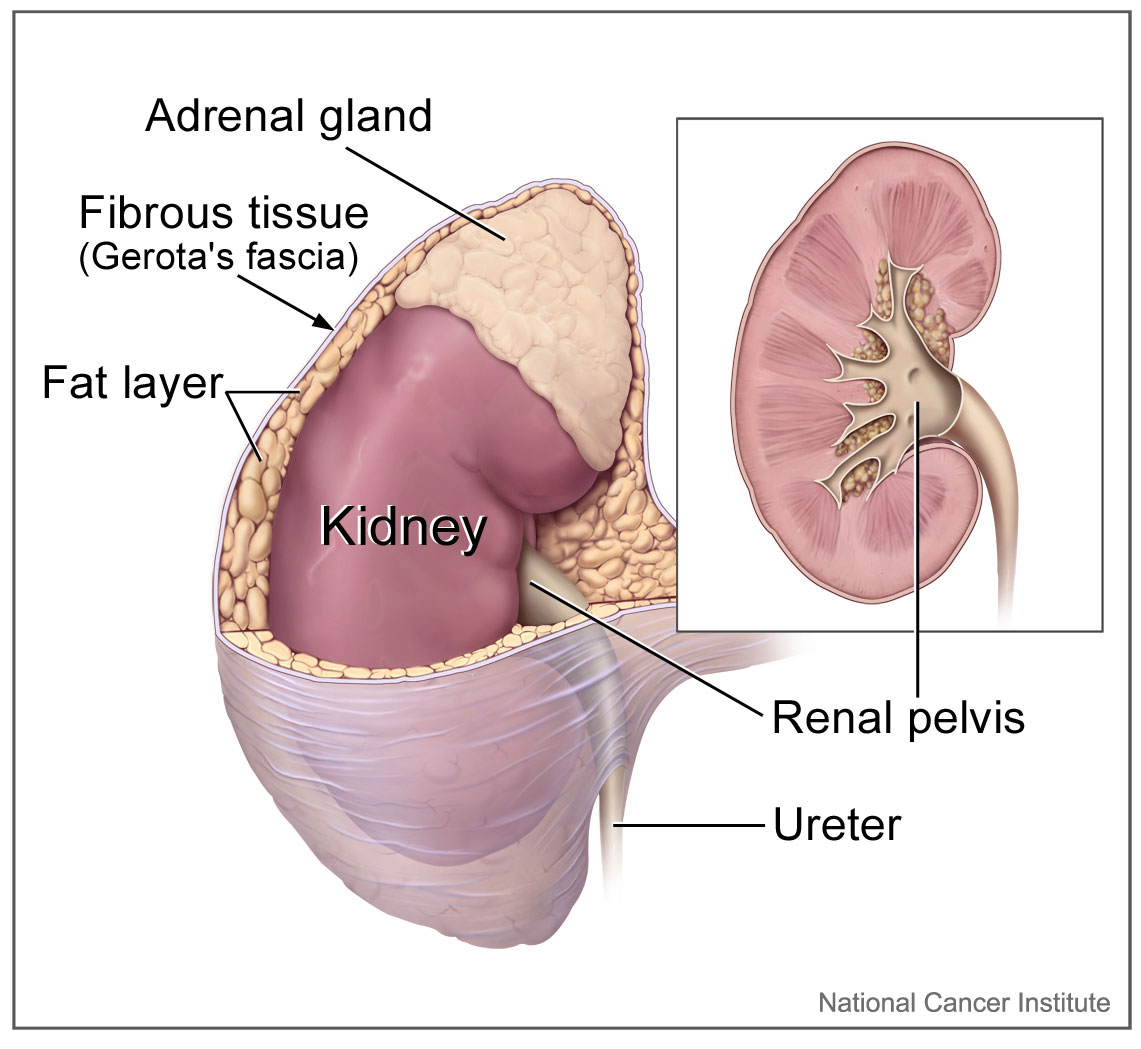
The walls of the ureters are composed of multiple layers of different types of tissues. The innermost layer is a special type of epithelium, called transitional epithelium. Unlike the epithelium lining most organs, transitional epithelium is capable of stretching and does not produce mucus. It lines much of the urinary system, including the renal pelvis, bladder, and much of the urethra, in addition to the ureters. Transitional epithelium allows these organs to stretch and expand as they fill with urine or allow urine to pass through. The next layer of the ureter walls is made up of loose connective tissue containing elastic fibres, nerves, and blood and lymphatic vessels. After this layer are two layers of smooth muscles, an inner circular layer, and an outer longitudinal layer. The smooth muscle layers can contract in waves of peristalsis to propel urine down the ureters from the kidneys to the urinary bladder. The outermost layer of the ureter walls consists of fibrous tissue.
Urinary Bladder
The urinary bladder is a hollow, muscular, and stretchy organ that rests on the pelvic floor. It collects and stores urine from the kidneys before the urine is eliminated through urination. As shown in Figure 16.5.4, urine enters the urinary bladder from the ureters through two ureteral openings on either side of the back wall of the bladder. Urine leaves the bladder through a sphincter called the internal urethral sphincter. When the sphincter relaxes and opens, it allows urine to flow out of the bladder and into the urethra.
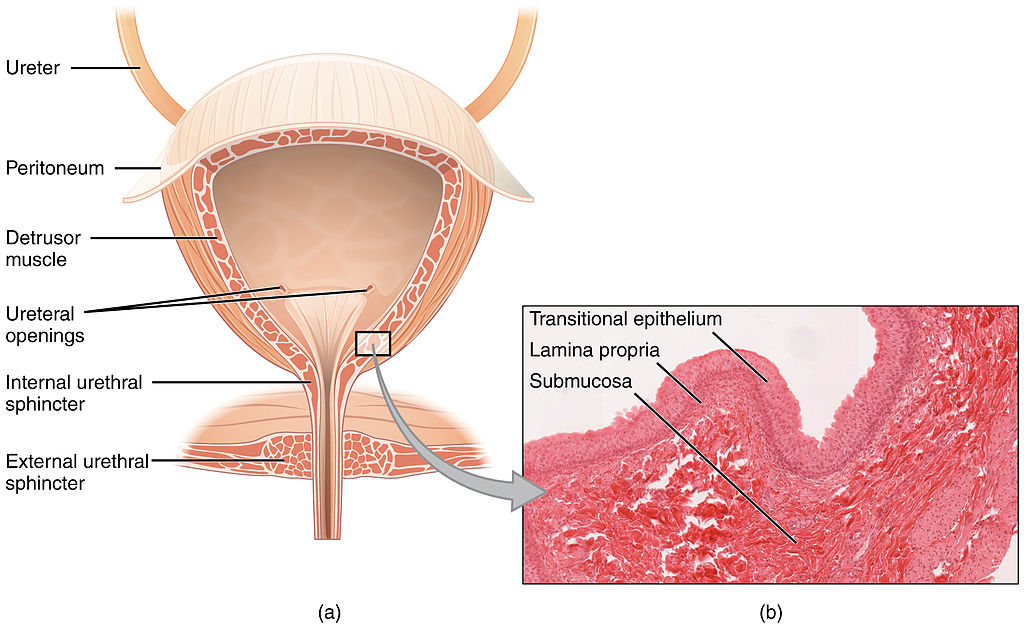
Like the ureters, the bladder is lined with transitional epithelium, which can flatten out and stretch as needed as the bladder fills with urine. The next layer (lamina propria) is a layer of loose connective tissue, nerves, and blood and lymphatic vessels. This is followed by a submucosa layer, which connects the lining of the bladder with the detrusor muscle in the walls of the bladder. The outer covering of the bladder is peritoneum, which is a smooth layer of epithelial cells that lines the abdominal cavity and covers most abdominal organs.
The detrusor muscle in the wall of the bladder is made of smooth muscle fibres controlled by both the autonomic and somatic nervous systems. As the bladder fills, the detrusor muscle automatically relaxes to allow it to hold more urine. When the bladder is about half full, the stretching of the walls triggers the sensation of needing to urinate. When the individual is ready to void, conscious nervous signals cause the detrusor muscle to contract, and the internal urethral sphincter to relax and open. As a result, urine is forcefully expelled out of the bladder and into the urethra.
Urethra
The urethra is a tube that connects the urinary bladder to the external urethral orifice, which is the opening of the urethra on the surface of the body. As shown in Figure 16.5.5, the urethra in males travels through the penis, so it is much longer than the urethra in females. In males, the urethra averages about 20 cm (about 7.8 in) long, whereas in females, it averages only about 4.8 cm (about 1.9 in) long. In males, the urethra carries semen (as well as urine), but in females, it carries only urine. In addition, in males, the urethra passes through the prostate gland (part of the reproductive system) which is absent in women.
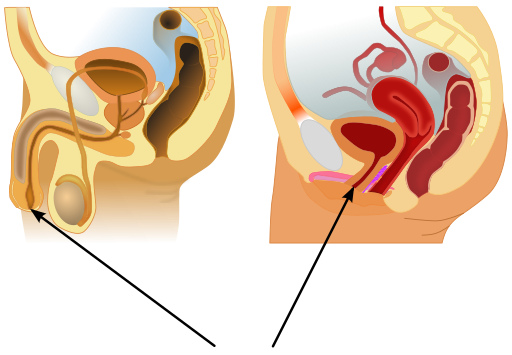
Like the ureters and bladder, the proximal (closer to the bladder) two-thirds of the urethra are lined with transitional epithelium. The distal (farther from the bladder) third of the urethra is lined with mucus-secreting epithelium. The mucus helps protect the epithelium from urine, which is corrosive. Below the epithelium is loose connective tissue, and below that are layers of smooth muscle that are continuous with the muscle layers of the urinary bladder. When the bladder contracts to forcefully expel urine, the smooth muscle of the urethra relaxes to allow the urine to pass through.
In order for urine to leave the body through the external urethral orifice, the external urethral sphincter must relax and open. This sphincter is a striated muscle that is controlled by the somatic nervous system, so it is under conscious, voluntary control in most people (exceptions are infants, some elderly people, and patients with certain injuries or disorders). The muscle can be held in a contracted state and hold in the urine until the person is ready to urinate. Following urination, the smooth muscle lining the urethra automatically contracts to re-establish muscle tone, and the individual consciously contracts the external urethral sphincter to close the external urethral opening.
16.5 Summary
- Ureters are tube-like structures that connect the kidneys with the urinary bladder. Each ureter arises at the renal pelvis of a kidney and travels down through the abdomen to the urinary bladder. The walls of the ureter contain smooth muscle that can contract to push urine through the ureter by peristalsis. The walls are lined with transitional epithelium that can expand and stretch.
- The urinary bladder is a hollow, muscular organ that rests on the pelvic floor. It is also lined with transitional epithelium. The function of the bladder is to collect and store urine from the kidneys before the urine is eliminated through urination. Filling of the bladder triggers the sensation of needing to urinate. When a conscious decision to urinate is made, the detrusor muscle in the bladder wall contracts and forces urine out of the bladder and into the urethra.
- The urethra is a tube that connects the urinary bladder to the external urethral orifice. Somatic nerves control the sphincter at the distal end of the urethra. This allows the opening of the sphincter for urination to be under voluntary control.
16.5 Review Questions
- What are ureters? Describe the location of the ureters relative to other urinary tract organs.
- Identify layers in the walls of a ureter. How do they contribute to the ureter’s function?
- Describe the urinary bladder. What is the function of the urinary bladder?
-
- How does the nervous system control the urinary bladder?
- What is the urethra?
- How does the nervous system control urination?
- Identify the sphincters that are located along the pathway from the ureters to the external urethral orifice.
- What are two differences between the male and female urethra?
- When the bladder muscle contracts, the smooth muscle in the walls of the urethra _________ .
16.5 Explore More
https://youtu.be/2Brajdazp1o
The taboo secret to better health | Molly Winter, TED. 2016.
https://youtu.be/dg4_deyHLvQ
What Happens When You Hold Your Pee? SciShow, 2016.
Attributions
Figure 16.5.1
Cliche by Jackie on Wikimedia Common s is used under a CC BY 2.0 (https://creativecommons.org/licenses/by/2.0) license.
Figure 16.5.2
Urinary System Male by BruceBlaus on Wikimedia Commons is used under a CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0) license.
Figure 16.5.3
Adrenal glands on Kidney by NCI Public Domain by Alan Hoofring (Illustrator) /National Cancer Institute (photo ID 4355) on Wikimedia Commons is in the public domain (https://en.wikipedia.org/wiki/Public_domain).
Figure 16.5.4
2605_The_Bladder by OpenStax College on Wikimedia Commons is used under a CC BY 3.0 (https://creativecommons.org/licenses/by/3.0) license. (Micrograph originally provided by the Regents of the University of Michigan Medical School © 2012.)
Figure 16.5.5
512px-Male_and_female_urethral_openings.svg by andrybak (derivative work) on Wikimedia Commons is used under a CC BY-SA 3.0 (https://creativecommons.org/licenses/by-sa/3.0) license. (Original: Male anatomy blank.svg: alt.sex FAQ, derivative work: Tsaitgaist Female anatomy with g-spot.svg: Tsaitgaist.)
References
Betts, J. G., Young, K.A., Wise, J.A., Johnson, E., Poe, B., Kruse, D.H., Korol, O., Johnson, J.E., Womble, M., DeSaix, P. (2013, June 19). Figure 25.4 Bladder (a) Anterior cross section of the bladder. (b) The detrusor muscle of the bladder (source: monkey tissue) LM × 448 [digital image]. In Anatomy and Physiology (Section 7.3). OpenStax. https://openstax.org/books/anatomy-and-physiology/pages/25-2-gross-anatomy-of-urine-transport
SciShow. (2016, January 22). What happens when you hold your pee? YouTube. https://www.youtube.com/watch?v=dg4_deyHLvQ&feature=youtu.be
TED. (2016, September 2). The taboo secret to better health | Molly Winter. YouTube. https://www.youtube.com/watch?v=2Brajdazp1o&feature=youtu.be
Created by CK-12 Foundation/Adapted by Christine Miller
Figure 16.3.1 The surprising uses of pee.
Surprising Uses
What do gun powder, leather, fabric dyes and laundry service have in common? This may be surprising, but they all historically involved urine. One of the main components in gun powder, potassium nitrate, was difficult to come by pre-1900s, so ingenious gun-owners would evaporate urine to concentrate the nitrates it contains. The ammonium in urine was excellent in breaking down tissues, making it a prime candidate for softening leathers and removing stains in laundry. Ammonia in urine also helps dyes penetrate fabrics, so it was used to make colours stay brighter for longer.
What is the Urinary System?
The actual human urinary system, also known as the renal system, is shown in Figure 16.3.2. The system consists of the kidneys, ureters, bladder, and urethra. The main function of the urinary system is to eliminate the waste products of metabolism from the body by forming and excreting urine. Typically, between one and two litres of urine are produced every day in a healthy individual.
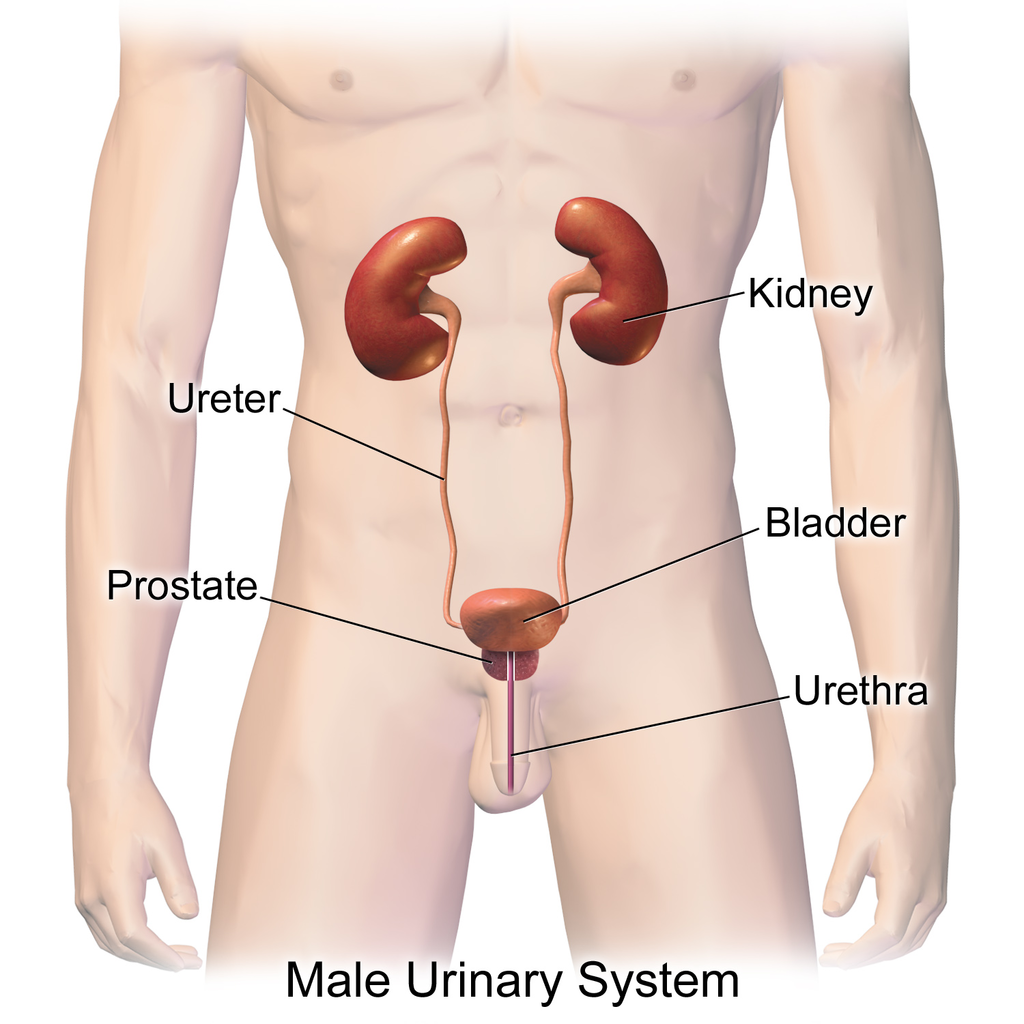
Organs of the Urinary System
The urinary system is all about urine. It includes organs that form urine, and also those that transport, store, or excrete urine.
Kidneys
Urine is formed by the kidneys, which filter many substances out of the blood, allow the blood to reabsorb needed materials, and use the remaining materials to form urine. The human body normally has two paired kidneys, although it is possible to get by quite well with just one. As you can see in Figure 16.3.3, each kidney is well supplied with blood vessels by a major artery and vein. Blood to be filtered enters the kidney through the renal artery, and the filtered blood leaves the kidney through the renal vein. The kidney itself is wrapped in a fibrous capsule, and consists of a thin outer layer called the cortex, and a thicker inner layer called the medulla.
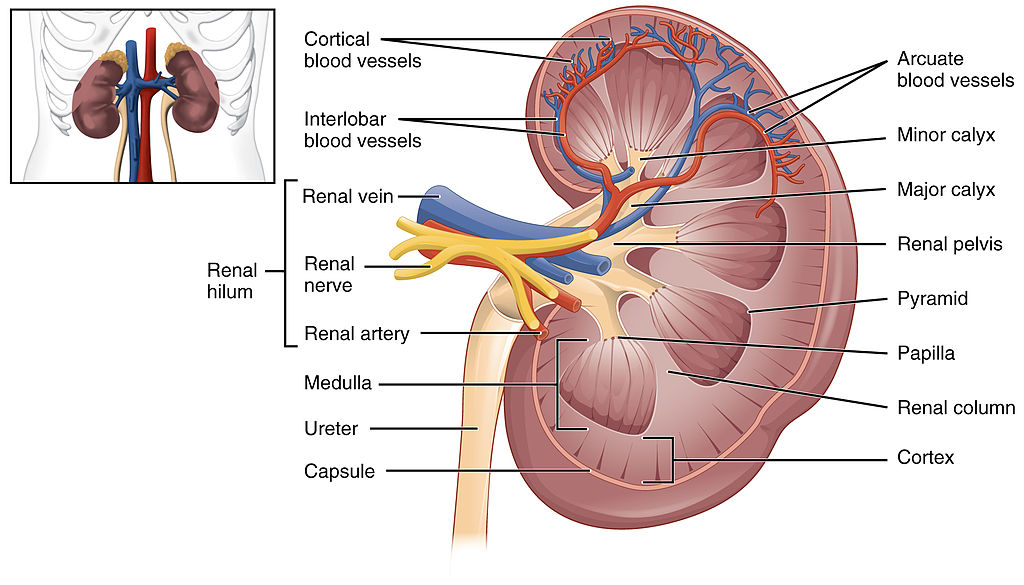
Blood is filtered and urine is formed by tiny filtering units called nephrons. Each kidney contains at least a million nephrons, and each nephron spans the cortex and medulla layers of the kidney. After urine forms in the nephrons, it flows through a system of converging collecting ducts. The collecting ducts join together to form minor calyces (or chambers) that join together to form major calyces (see Figure 16.3.3 above). Ultimately, the major calyces join the renal pelvis, which is the funnel-like end of the ureter where it enters the kidney.
Ureters, Bladder, Urethra
After urine forms in the kidneys, it is transported through the ureters (one per kidney) via peristalsis to the sac-like urinary bladder, which stores the urine until urination. During urination, the urine is released from the bladder and transported by the urethra to be excreted outside the body through the external urethral opening.
Functions of the Urinary System
Waste products removed from the body with the formation and elimination of urine include many water-soluble metabolic products. The main waste products are urea — a by-product of protein catabolism — and uric acid, a by-product of nucleic acid catabolism. Excess water and mineral ions are also eliminated in urine.
Besides the elimination of waste products such as these, the urinary system has several other vital functions. These include:
- Maintaining homeostasis of mineral ions in extracellular fluid: These ions are either excreted in urine or returned to the blood as needed to maintain the proper balance.
- Maintaining homeostasis of blood pH: When pH is too low (blood is too acidic), for example, the kidneys excrete less bicarbonate (which is basic) in urine. When pH is too high (blood is too basic), the opposite occurs, and more bicarbonate is excreted in urine.
- Maintaining homeostasis of extracellular fluids, including the blood volume, which helps maintain blood pressure: The kidneys control fluid volume and blood pressure by excreting more or less salt and water in urine.
Control of the Urinary System
The formation of urine must be closely regulated to maintain body-wide homeostasis. Several endocrine hormones help control this function of the urinary system, including antidiuretic hormone, parathyroid hormone, and aldosterone.
- Antidiuretic hormone (ADH), also called vasopressin, is secreted by the posterior pituitary gland. One of its main roles is conserving body water. It is released when the body is dehydrated, and it causes the kidneys to excrete less water in urine.
- Parathyroid hormone is secreted by the parathyroid glands. It works to regulate the balance of mineral ions in the body via its effects on several organs, including the kidneys. Parathyroid hormone stimulates the kidneys to excrete less calcium and more phosphorus in urine.
- Aldosterone is secreted by the cortex of the adrenal glands, which rest atop the kidneys, as shown in Figure 16.3.4. Through its effect on the kidneys, it plays a central role in regulating blood pressure. It causes the kidneys to excrete less sodium and water in urine.
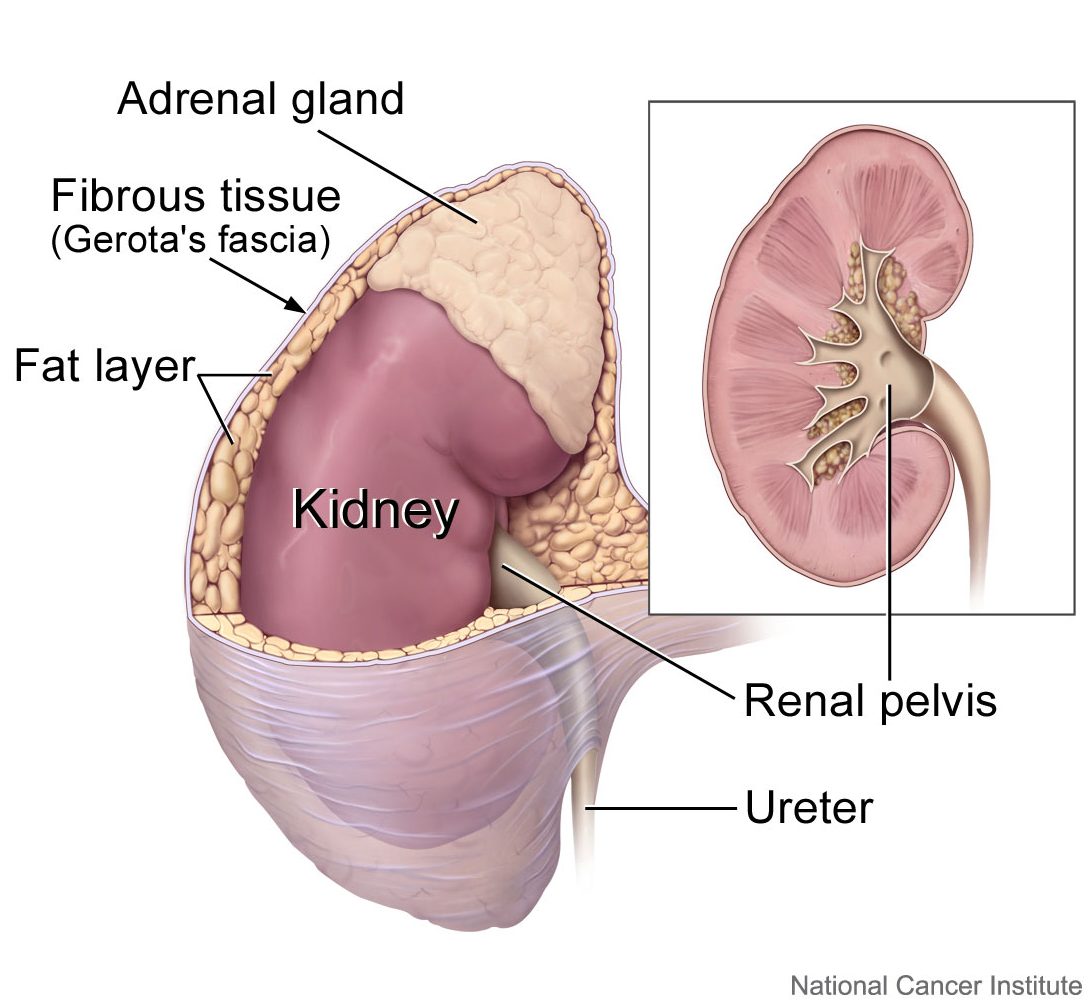
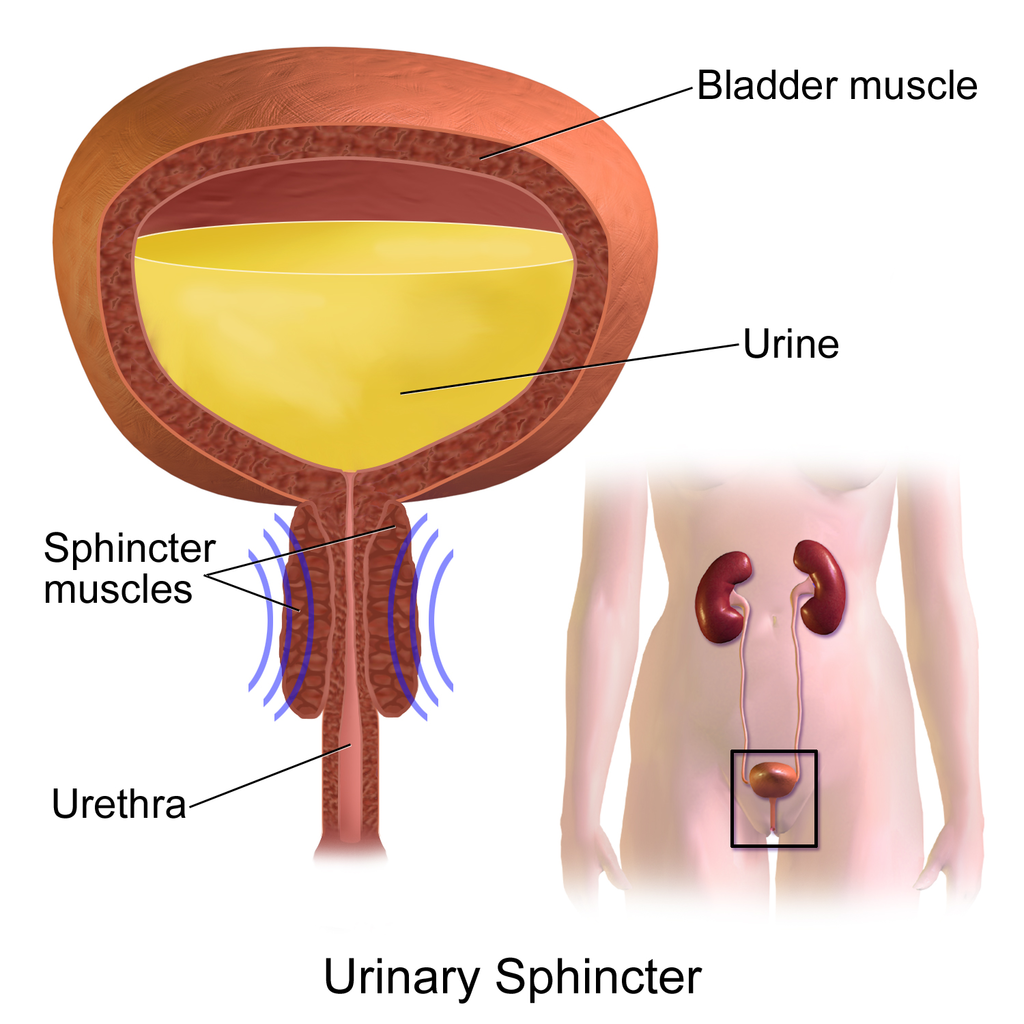
Once urine forms, it is excreted from the body in the process of urination, also sometimes referred to as micturition. This process is controlled by both the autonomic and the somatic nervous systems. As the bladder fills with urine, it causes the autonomic nervous system to signal smooth muscle in the bladder wall to contract (as shown in Figure 16.3.5), and the sphincter between the bladder and urethra to relax and open. This forces urine out of the bladder and through the urethra. Another sphincter at the distal end of the urethra is under voluntary control. When it relaxes under the influence of the somatic nervous system, it allows urine to leave the body through the external urethral opening.
16.3 Summary
- The urinary system consists of the kidneys, ureters, bladder, and urethra. The main function of the urinary system is to eliminate the waste products of metabolism from the body by forming and excreting urine.
- Urine is formed by the kidneys, which filter many substances out of blood, allow the blood to reabsorb needed materials, and use the remaining materials to form urine. Blood to be filtered enters the kidney through the renal artery, and filtered blood leaves the kidney through the renal vein.
- Within each kidney, blood is filtered and urine is formed by tiny filtering units called nephrons, of which there are at least a million in each kidney.
- After urine forms in the kidneys, it is transported through the ureters via peristalsis to the urinary bladder. The bladder stores the urine until urination, when urine is transported by the urethra to be excreted outside the body.
- Besides the elimination of waste products (such as urea, uric acid, excess water, and mineral ions), the urinary system has other vital functions. These include maintaining homeostasis of mineral ions in extracellular fluid, regulating acid-base balance in the blood, regulating the volume of extracellular fluids, and controlling blood pressure.
- The formation of urine must be closely regulated to maintain body-wide homeostasis. Several endocrine hormones help control this function of the urinary system, including antidiuretic hormone from the posterior pituitary gland, parathyroid hormone from the parathyroid glands, and aldosterone from the adrenal glands.
- The process of urination is controlled by both the autonomic and the somatic nervous systems. The autonomic system causes the bladder to empty, but conscious relaxation of the sphincter at the distal end of the urethra allows urine to leave the body.
16.3 Review Questions
-
- State the main function of the urinary system.
- What are nephrons?
- Other than the elimination of waste products, identify functions of the urinary system.
- How is the formation of urine regulated?
- Explain why it is important to have voluntary control over the sphincter at the end of the urethra.
- In terms of how they affect the kidneys, compare aldosterone to antidiuretic hormone.
- If your body needed to retain more calcium, which of the hormones described in this concept is most likely to increase? Explain your reasoning.
16.3 Explore More
https://youtu.be/dxecGD0m0Xc
The Urinary System - An Introduction | Physiology | Biology | FuseSchool, 2017.
https://youtu.be/pyMcTUQYMQw
Maple Syrup Urine Disease, Alexandria Doody, 2016.
https://youtu.be/3z-xjfdJWAI
How Accurate Are Drug Tests? Seeker, 2016.
https://youtu.be/xt1Tj5eeS0k
Three Ways Pee Could Change the World, Gross Science, 2015.
Attributions
Figure 16.3.1
- File:Pyrodex powder ffg.jpg by Hustvedt on Wikimedia Commons is used under a CC BY SA 3.0 (https://creativecommons.org/licenses/by-sa/3.0/deed.en).
- Brown leather satchel bag by Álvaro Serrano on Unsplash is used under the Unsplash Licence (https://unsplash.com/license).
- Laundry basket by Andy Fitzsimon on Unsplash is used under the Unsplash Licence (https://unsplash.com/license).
- Tags: Wool Skeins Natural Dyed Colorful Himalayan Weavers by on Pixabay is used under the Pixabay License (https://pixabay.com/service/license/).
Figure 16.3.2
Urinary_System_(Male) by BruceBlaus on Wikimedia Commons is used under a CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0) license.
Figure 16.3.3
2610_The_Kidney by OpenStax College on Wikimedia Commons is used under a CC BY 3.0 (https://creativecommons.org/licenses/by/3.0) license.
Figure 16.3.4
Adrenal glands on Kidney by Alan Hoofring (Illustrator)/ NCI Visuals Online is in the public domain (https://en.wikipedia.org/wiki/Public_domain).
Figure 16.3.5
Urinary_Sphincter by BruceBlaus on Wikimedia Commons is used under a CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0) license.
References
Alexandria Doody. (2016, March 29). Maple syrup urine disease. YouTube. https://www.youtube.com/watch?v=pyMcTUQYMQw&feature=youtu.be
Betts, J. G., Young, K.A., Wise, J.A., Johnson, E., Poe, B., Kruse, D.H., Korol, O., Johnson, J.E., Womble, M., DeSaix, P. (2013, June 19). Figure 25.8 Left kidney [digital image]. In Anatomy and Physiology (Section 25.3). OpenStax. https://openstax.org/books/anatomy-and-physiology/pages/25-3-gross-anatomy-of-the-kidney
FuseSchool. (2017, June 19). The urinary system - An introduction | Physiology | Biology | FuseSchool. YouTube. https://www.youtube.com/watch?v=dxecGD0m0Xc&feature=youtu.be
Gross Science. (2015, September 15). Three ways pee could change the world. YouTube. https://www.youtube.com/watch?v=xt1Tj5eeS0k&feature=youtu.be
Seeker. (2016, January 16). How accurate are drug tests? YouTube. https://www.youtube.com/watch?v=3z-xjfdJWAI&feature=youtu.be
A long extension of the cell body of a neuron that transmits nerve impulses to other cells.
Created by CK-12 Foundation/Adapted by Christine Miller

Family Planning Pioneer
Her name was Marie Stopes, and she was a British author and paleobotanist who lived from 1880 to 1958. She is pictured in Figure 18.11.1 in her lab next to her microscope. Stopes made significant contributions to science and was the first woman on the faculty of the University of Manchester in England. Her primary claim to fame was her work as a family planning pioneer.
Along with her husband, Stopes founded the first birth control clinic in Britain. She also edited a newsletter called Birth Control News, which gave explicit practical advice on how to avoid unwanted pregnancies. In 1918, she published a sex manual titled Married Love. The book was controversial and influential, bringing the subject of contraception into wide public discourse for the first time.
What Is Contraception?
About a century after Married Love, more than half of all fertile married couples worldwide use some form of contraception. Contraception, also known as birth control, is any method or device used to prevent pregnancy. Birth control methods have been used for centuries, but safe and effective methods only became available in the 20th century, in part because of the work of people like Marie Stopes.
Many different birth control methods are currently available, but they differ considerably in their effectiveness at preventing pregnancy. The effectiveness of contraception is generally expressed as the failure rate, which is the percentage of women who become pregnant using a given method during the first year of use. Virtually no one uses any method of birth control perfectly, so the failure rate with typical use is almost always higher — and often much higher — than the failure rate with perfect use. For example, with perfect use, a birth control method might have a failure rate of just 1%, whereas with typical use, the failure rate might be 25%. For comparison, there is an average one-year pregnancy rate of 85% if no contraception is used.
All methods of birth control have potential adverse effects, but their health risks are less than the health risks associated with pregnancy. Using contraception to space the children in a family is also good for the children’s health and development, as well as for the health of the mother.
Types of Contraception and Their Effectiveness
Types of birth control methods include barrier methods, hormonal methods, intrauterine devices, behavioural methods, and sterilization. With the exception of sterilization, all of these methods are reversible. Examples of each type of birth control method and their failure rates with typical use are described below. Much of the information is also summarized in Figure 18.11.2.
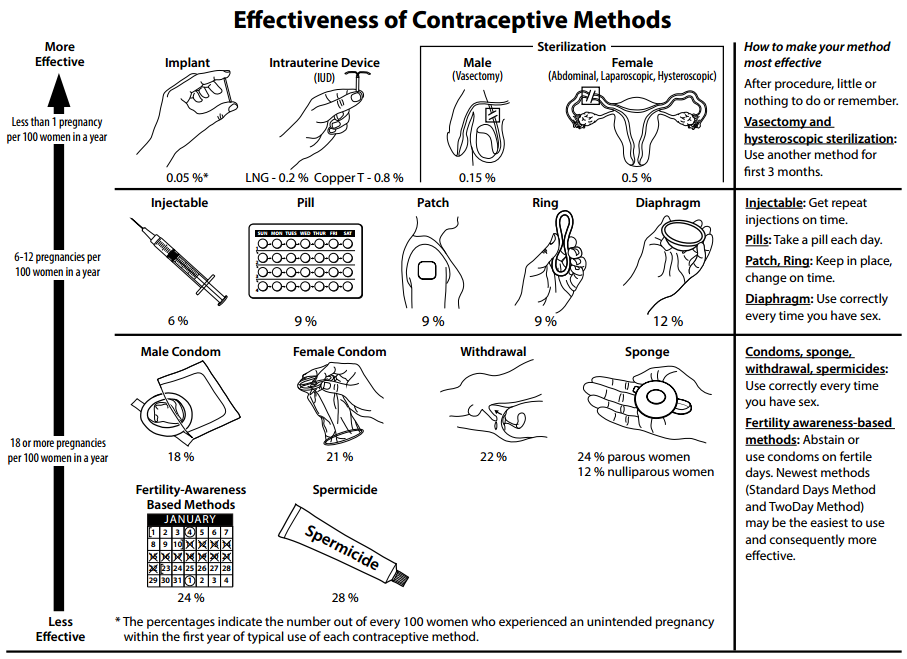
Barrier Methods
Barrier methods are devices that are used to physically block sperm from entering the uterus. They include condoms and diaphragms.

Condoms
Condoms are the most commonly used method of birth control globally. There are condoms for females and males, but male condoms are more widely used, less expensive, and more readily available. Both types of condoms are pictured in Figures 18.11.3 and 18.11.4. A male condom is placed on a man’s erect penis, and a female condom is placed inside a woman’s vagina. Whichever type of condom is used, it must be put in place before sexual intercourse occurs. Condoms work by physically blocking ejaculated sperm from entering the vagina of the sexual partner. With typical use, male condoms have an 18% failure rate, and female condoms have a 21% failure rate. Unlike virtually all other birth control methods, condoms also help prevent the spread of sexually transmitted infections (STIs), in addition to helping to prevent pregnancy.


Diaphragms
Diaphragms, like the one pictured in Figure 18.11.5, ideally prevent sperm from passing through the cervical canal and into the uterus. A diaphragm is inserted vaginally before sexual intercourse occurs and must be placed over the cervix to be effective. It is usually recommended that a diaphragm be covered with spermicide before insertion for extra protection. It is also recommended that the diaphragm be left in place for at least six hours after intercourse. The failure rate of diaphragms with typical use is about 12%, which is about half that of condoms. However, diaphragms do not help prevent the spread of STIs, and their use is also associated with an increased frequency of urinary tract infections in females.
Hormonal Methods
Hormonal contraception is the administration of hormones to prevent ovulation. Hormones can be taken orally in birth control pills, implanted under the skin, injected into a muscle, or received transdermally from a skin patch. Hormonal methods are currently available only for women, although hormonal contraceptives for men are being tested in clinical trials.
Birth control pills are the most common form of hormonal contraception. There are two types of pills: the combined pill (which contains both estrogen and progesterone) and the progesterone-only pill. Both types of pills inhibit ovulation and thicken cervical mucus. The failure rate of birth control pills is only about 1% or less, if used perfectly. However, the failure rate rises to about 10% with typical use, because women do not always remember to take the pill at the same time every day. The combined pill is associated with a slightly increased risk of blood clots, but a reduced risk of ovarian and endometrial cancers. The progesterone-only pill does not increase the risk of blood clots, but it may cause irregular menstrual periods. It may take a few weeks or even months for fertility to return to normal after long-term use of birth control pills.
Intrauterine Devices
An intrauterine device (IUD) is a T-shaped or coiled plastic structure that is inserted into the uterus via the vagina and cervix that contains either copper or a hormone. You can see an IUD in the uterus in the drawing of the female reproductive system in Figure 18.11.6. An IUD is inserted by a physician and may be left in place for months or even years. A physician also must remove an IUD, using the strings attached to the device. The copper in copper IUDs prevents pregnancy by interfering with the movement of sperm so they cannot reach and fertilize an egg. The copper may also prevent implantation in the unlikely circumstance of a sperm managing to reach and fertilize an ovum, in which case the blastocyst/zygote would be shed during menstruation. The hormones in hormonal IUDs prevent pregnancy by thickening cervical mucus and trapping sperm. The hormones may also interfere with ovulation, so there is no egg to fertilize.
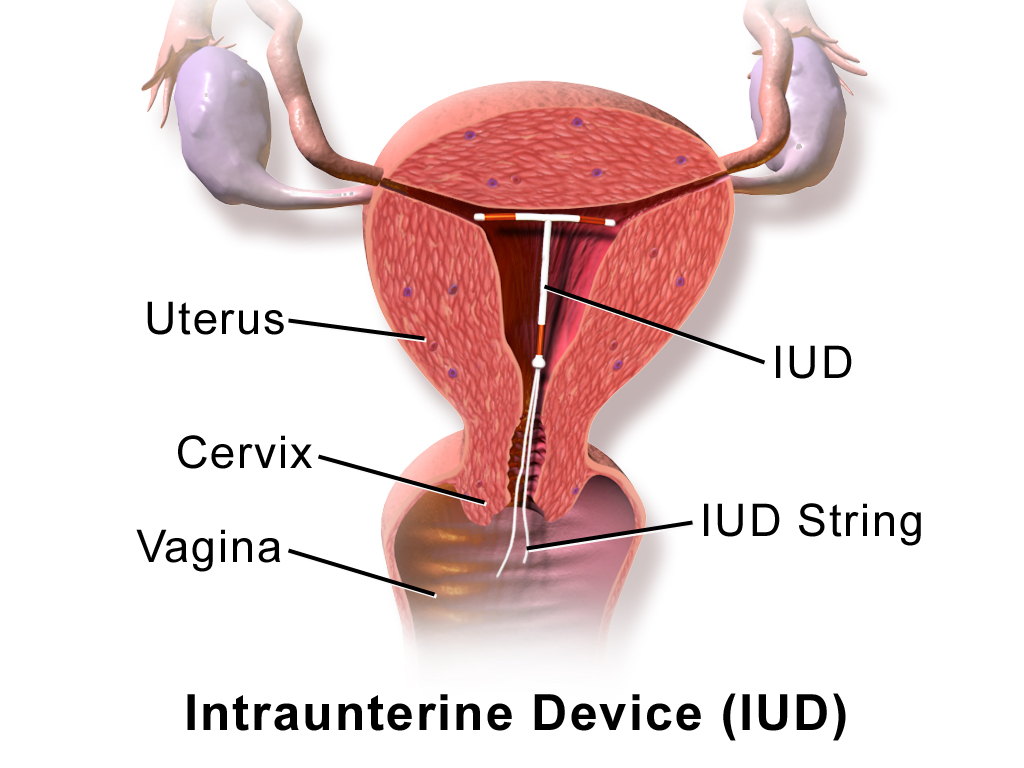
For both types of IUDs, the failure rates are <1%, and failure rates with typical use are virtually the same as failure rates with perfect use. Their effectiveness is one reason that IUDs are among the most widely used forms of reversible contraception. Once removed, even after long-term use, fertility returns to normal immediately. On the other hand, IUDs do have a risk of complications, including increased menstrual bleeding and more painful menstrual cramps. IUDs are also occasionally expelled from the uterus, and there is a slight risk of perforation of the uterus by the IUD.
Behavioural Methods
The least effective methods of contraception are behavioural methods. They involve regulating the timing or method of intercourse to prevent introduction of sperm into the female reproductive tract, either altogether or when an egg may be present. Behavioural methods include fertility awareness methods and withdrawal. Abstinence from sexual activity, or at least from vaginal intercourse, is sometimes considered a behavioural method, as well — but it is unlikely to be practiced consistently enough by most people to prevent pregnancy. Even teens who receive abstinence-only sex education do not have reduced rates of pregnancy. Abstinence is also ineffective in cases of non-consensual sex.
Fertility Awareness Methods
Fertility awareness methods involve estimating the most fertile days of the menstrual cycle and then avoiding unprotected vaginal intercourse on those days. The most fertile days are generally a few days before ovulation occurs, the day of ovulation, and another day or two after that. Unless unprotected sex occurs on those days, pregnancy is unlikely. Techniques for estimating the most fertile days include monitoring and detecting minor changes in basal body temperature or cervical secretions. This requires daily motivation and diligence, so it is not surprising that typical-use failure rates of these methods are at least 20–25%, and for some individuals may be as high as using no contraception at all (85%).
Basal body temperature is the lowest body temperature when the body is at rest (usually during sleep). It is most often estimated by a temperature measurement taken immediately upon awakening in the morning and before any physical activity has occurred. Basal body temperature normally rises after ovulation occurs, as shown in the graph below (Figure 18.11.7). The increase in temperature is small but consistent and may be used to determine when ovulation occurs, around which time unprotected intercourse should be avoided to prevent pregnancy. However, basal body temperature only shows when ovulation has already occurred, and it cannot predict in advance when ovulation will occur. Sperm can live for up to a week in the female reproductive tract, so determining the occurrence of ovulation only after ovulation has already happened is a major drawback of this method.
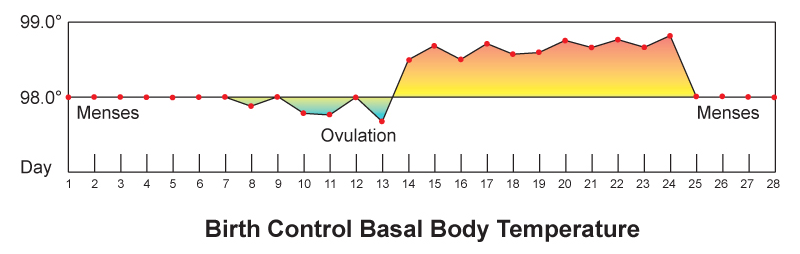
Monitoring cervical mucus has the potential for being more effective than monitoring basal body temperature, because it can predict ovulation ahead of time. As ovulation approaches, cervical secretions usually increase in amount and become thinner (which helps sperm swim through the cervical canal). By recognizing the changing characteristics of cervical mucus, a woman may be able to predict when she will ovulate. From this information, she can determine when she should avoid unprotected sex to prevent pregnancy.
Withdrawal
Withdrawal (also called coitus interruptus) is the practice of withdrawing the penis from the vagina before ejaculation ensues. The main risk of the withdrawal method is that the man may not perform the maneuver correctly or in a timely manner. Fluid typically released from the penis before ejaculation occurs may also contain some sperm. In addition, if sperm are ejaculated just outside of the vagina, there is a chance they will be able to enter the vagina and travel through the female reproductive tract to fertilize an egg. For all these reasons, the withdrawal method has a relatively high failure rate of about 22% with typical use.
Sterilization
The most effective contraceptive method is sterilization. In both sexes, sterilization generally involves surgical procedures that are considered irreversible. Additional surgery may be able to reverse a sterilization procedure, but there are no guarantees. Male sterilization is generally less invasive and less risky than female sterilization.
Male Sterilization
Male sterilization is usually achieved with a vasectomy. In this surgery, the vas deferens from each testis is clamped, cut, or otherwise sealed (see Figure 18.11.8). This prevents sperm from traveling from the epididymis to the ejaculatory ducts and being ejaculated from the penis. The same amount of semen will still be ejaculated, but it will not contain any sperm, making fertilization impossible. After a vasectomy, the testes continue to produce sperm, but the sperm are reabsorbed. It usually takes several months after a vasectomy for all remaining sperm to be ejaculated or reabsorbed. In the meantime, another method of birth control should be used.
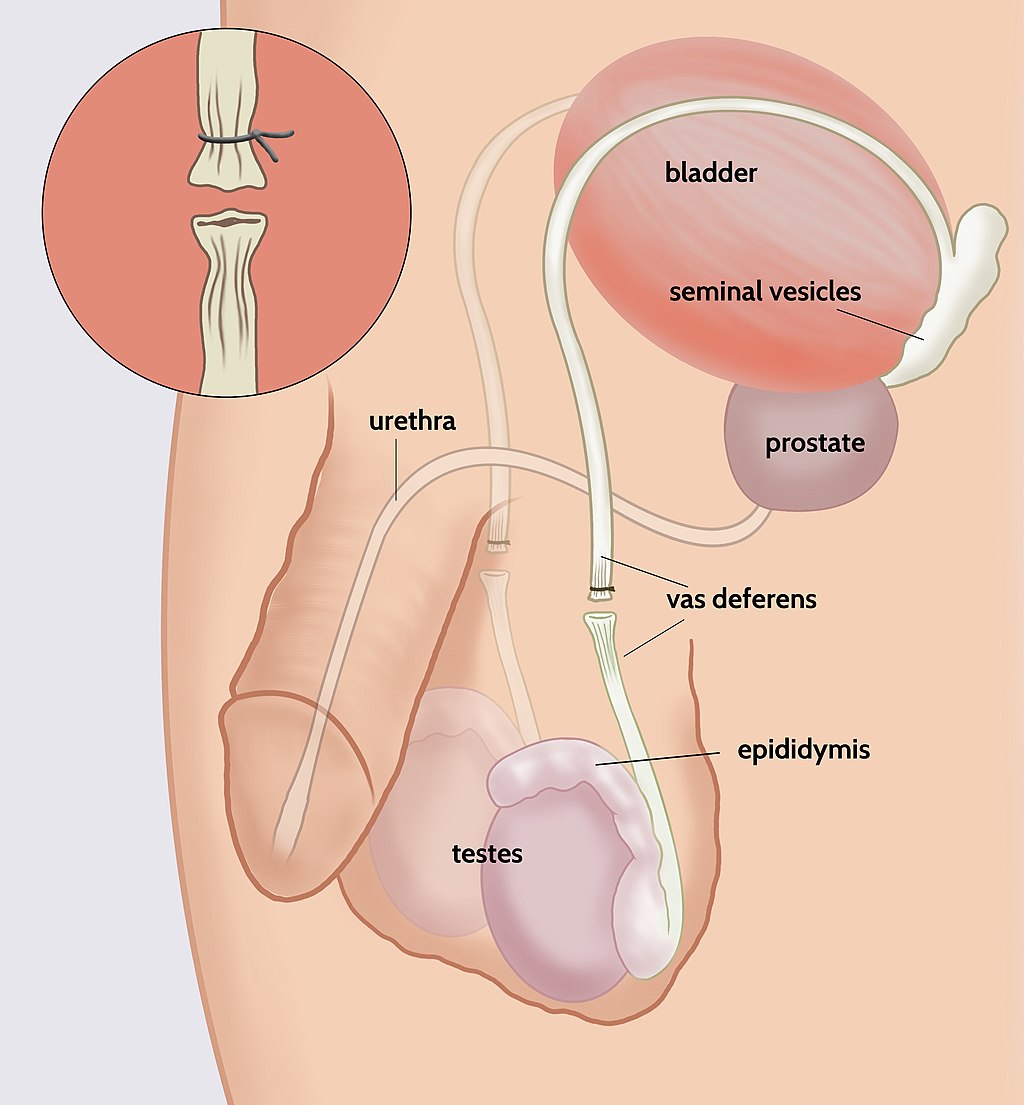
Female Sterilization
The procedure undertaken for female sterilization is usually tubal ligation. The oviducts may be tied or cut in a surgical procedure, which permanently blocks the tubes. Alternatively, tiny metal implants may be inserted into the oviducts in a nonsurgical procedure. Over time, scar tissue grows around the implants and permanently blocks the tubes. Either method stops eggs from traveling from the ovaries through the oviducts, where fertilization usually takes place.
Emergency Contraception
Emergency contraception is any form of contraception that is used after unprotected vaginal intercourse. One method is the so-called “morning-after” pill. This is essentially a high-dose birth control pill that helps prevent pregnancy by temporarily preventing ovulation. It works only if ovulation has not already occurred, and when taken within five days after unprotected sex. The sooner the pill is taken, the more likely it is to work. Another method of emergency contraception is the IUD. An IUD that is inserted up to five days after unprotected sex can prevent nearly 100% of pregnancies. It keeps sperm from reaching and fertilizing an egg, or inhibits implantation if an ovum has already been fertilized. The IUD can then be left in place to prevent future pregnancies.
18.11 Summary
- More than half of all fertile couples worldwide use contraception (birth control), which is any method or device used to prevent pregnancy. Different methods of contraception vary in their effectiveness, typically expressed as the failure rate, or the percentage of women who become pregnant using a given method during the first year of use. For most methods, the failure rate with typical use is much higher than the failure rate with perfect use.
- Types of birth control methods include barrier methods, hormonal methods, intrauterine devices, behavioural methods, and sterilization. Except for sterilization, all of the methods are reversible. All of the methods have health risks, but they are less than the risks of pregnancy.
- Barrier methods are devices that block sperm from entering the uterus. They include condoms and diaphragms. Of all birth control methods, only condoms can prevent the spread of sexually transmitted infections in addition to pregnancy.
- Hormonal methods involve the administration of hormones to prevent ovulation. Hormones can be administered in various ways, such as in an injection, through a skin patch, or — most commonly — in birth control pills. There are two types of birth control pills: those that contain estrogen and progesterone, and those that contain only progesterone. Both types are equally effective, but they have different potential side effects.
- An intrauterine device (IUD) is a small T-shaped plastic structure containing copper or a hormone that is inserted into the uterus by a physician and left in place for months or even years. It is highly effective even with typical use, but it does have some risks, such as increased menstrual bleeding and, rarely, perforation of the uterus.
- Behavioural methods involve regulating the timing or method of intercourse to prevent introduction of sperm into the female reproductive tract, either altogether or when an egg may be present. In fertility awareness methods, unprotected intercourse is avoided during the most fertile days of the cycle, as estimated by basal body temperature or the characteristics of cervical mucus. In withdrawal (coitus interruptus), the penis is withdrawn from the vagina before ejaculation occurs. Behavioural methods are the least effective methods of contraception.
- Sterilization is the most effective contraceptive method, but it requires a surgical procedure and may be irreversible. Male sterility is usually achieved with a vasectomy, in which the vas deferens are clamped or cut to prevent sperm from being ejaculated in semen. Female sterility is usually achieved with a tubal ligation, in which the oviducts are clamped or cut to prevent sperm from reaching and fertilizing eggs.
- Emergency contraception is any form of contraception used after unprotected vaginal intercourse. One method is the “morning after” pill, which is a high-dose birth control pill that can be taken up to five days after unprotected sex. Another method is an IUD, which can be inserted up to five days after unprotected sex.
18.11 Review Questions
-
- How is the effectiveness of contraceptive methods typically measured?
- What is an IUD?
- Discuss sterilization as a birth control method. Compare sterilization in males and females.
- What is emergency contraception? When is it used? What are two forms of emergency contraception?
- How does the thickness of cervical mucus relate to fertility? How do two methods of contraception take advantage of this relationship?
- If a newly developed method of contraception had a 35% failure rate, would you consider this to be an effective method? Explain your answer.
18.11 Explore More
https://youtu.be/Zx8zbTMTncs
How do contraceptives work? - NWHunter, TED-Ed, 2016.
https://youtu.be/jdr1yDO7MoY
The History Of Birth Control | TIME, 2015.
https://youtu.be/vIaL5QiKbWI
Finally, A Male Pill? SciShow, 2012.
Attributions
Figure 18.11.1
512px-Marie_Stopes [cropped] by AdamBMorgan on Wikimedia Commons is in the public domain (https://en.wikipedia.org/wiki/public_domain). (Original by Unknown author: File:Marie Stopes in her laboratory, 1904.jpg).
Figure 18.11.2
Effectivenessofcontraceptives by Center for Disease Control and Prevention on Wikimedia Commons is in the public domain (https://en.wikipedia.org/wiki/public_domain).
Figure 18.11.3
Condom by Reproductive Health Supplies Coalition on Unsplash is used under the Unsplash License (https://unsplash.com/license).
Figure 18.11.4
Female condom by Ceridwen on Wikimedia Commons is used under a CC BY-SA 2.0 FR (https://creativecommons.org/licenses/by-sa/2.0/fr/deed.en) license.
Figure 18.11.5
Contraceptive_diaphragm by Axefan2 on Wikimedia Commons is in the public domain (https://en.wikipedia.org/wiki/public_domain).
Figure 18.11.6
1024px-Blausen_0585_IUD by BruceBlaus on Wikimedia Commons is used under a CC BY 3.0 (https://creativecommons.org/licenses/by/3.0) license.
Figure 18.11.7
Basal_Body_Temperature by BruceBlaus on Wikimedia Commons is used under a CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0) license.
Figure 18.11.8
1024px-Open_Vasectomy_ by Timdwilliamson on Wikimedia Commons is used under a CC BY SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0) license.
References
Blausen.com Staff. (2014). Medical gallery of Blausen Medical 2014. WikiJournal of Medicine 1 (2). DOI:10.15347/wjm/2014.010. ISSN 2002-4436
SciShow. (2012, August 16). Finally, a male pill? YouTube. https://www.youtube.com/watch?v=vIaL5QiKbWI&feature=youtu.be
Stopes, M. (1918). Married love. Wikisource. https://en.wikisource.org/w/index.php?title=Married_Love&oldid=6230157 (Originally published with Preface and Notes by William J. Robinson, by The Critic and Guide Company. This book was banned in the United States until 1933.)
TED-Ed. (2016, September). How do contraceptives work? - NWHunter. YouTube. https://www.youtube.com/watch?v=Zx8zbTMTncs&feature=youtu.be
Time. (2015, January 30). The history of birth control | TIME. YouTube. https://www.youtube.com/watch?v=jdr1yDO7MoY&feature=youtu.be
Wikipedia contributors. (2020, August 9). Marie Stopes. In Wikipedia. https://en.wikipedia.org/w/index.php?title=Marie_Stopes&oldid=972063381
Created by CK-12 Foundation/Adapted by Christine Miller

Vampires
From Bram Stoker’s famous novel about Count Dracula, to films such as Van Helsing and the Twilight Saga, fantasies featuring vampires (like the one in Figure 14.5.1) have been popular for decades. Vampires, in fact, are found in centuries-old myths from many cultures. In such myths, vampires are generally described as creatures that drink blood — preferably of the human variety — for sustenance. Dracula, for example, is based on Eastern European folklore about a human who attains immortality (and eternal damnation) by drinking the blood of others.
What Is Blood?
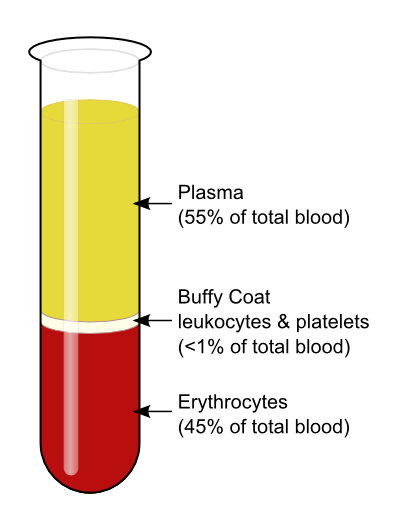
The average adult body contains between 4.7 and 5.7 litres of blood. More than half of that amount is fluid. Most of the rest of that amount consists of blood cells. The relative amounts of the various components in blood are illustrated in Figure 14.5.2. The components are also described in detail below.
Blood is a fluid connective tissue that circulates throughout the body through blood vessels of the cardiovascular system. What makes blood so special that it features in widespread myths? Although blood accounts for less than 10% of human body weight, it is quite literally the elixir of life. As blood travels through the vessels of the cardiovascular system, it delivers vital substances (such as nutrients and oxygen) to all of the cells, and carries away their metabolic wastes. It is no exaggeration to say that without blood, cells could not survive. Indeed, without the oxygen carried in blood, cells of the brain start to die within a matter of minutes.
Functions of Blood
Blood performs many important functions in the body. Major functions of blood include:
- Supplying tissues with oxygen, which is needed by all cells for aerobic cellular respiration.
- Supplying cells with nutrients, including glucose, amino acids, and fatty acids.
- Removing metabolic wastes from cells, including carbon dioxide, urea, and lactic acid.
- Helping to defend the body from pathogens and other foreign substances.
- Forming clots to seal broken blood vessels and stop bleeding.
- Transporting hormones and other messenger molecules.
- Regulating the pH of the body, which must be kept within a narrow range (7.35 to 7.45).
- Helping regulate body temperature (through vasoconstriction and vasodilation).
Blood Plasma
Plasma is the liquid component of human blood. It makes up about 55% of blood by volume. It is about 92% water, and contains many dissolved substances. Most of these substances are proteins, but plasma also contains trace amounts of glucose, mineral ions, hormones, carbon dioxide, and other substances. In addition, plasma contains blood cells. When the cells are removed from plasma, as in Figure 14.5.2 above, the remaining liquid is clear but yellow in colour.
Blood Cells
The cells in blood include erythrocytes, leukocytes, and thrombocytes. These different types of blood cells are shown in the photomicrograph (Figure 14.5.3) and described in the sections that follow.
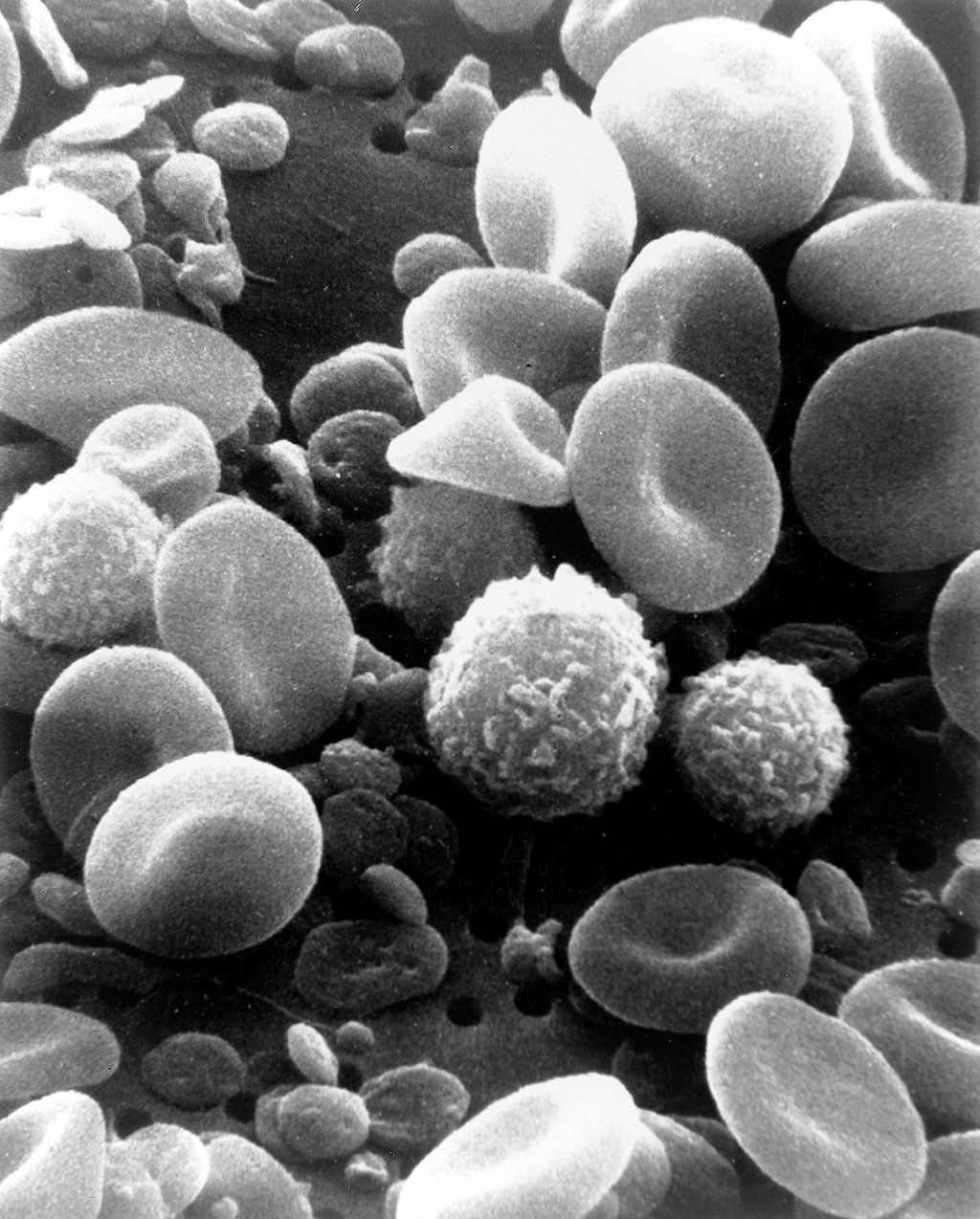
Erythrocytes
The most numerous cells in blood are red blood cells, also called erythrocytes. One microlitre of blood contains between 4.2 and 6.1 million red blood cells, and red blood cells make up about 25% of all the cells in the human body. The cytoplasm of a mature erythrocyte is almost completely filled with hemoglobin, the iron-containing protein that binds with oxygen and gives the cell its red colour. In order to provide maximum space for hemoglobin, mature erythrocytes lack a cell nucleus and most organelles. They are little more than sacks of hemoglobin.
Erythrocytes also carry proteins called antigens that determine blood type. Blood type is a genetic characteristic. The best known human blood type systems are the ABO and Rhesus systems.
- In the ABO system, there are two common antigens, called antigen A and antigen B. There are four ABO blood types, A (only A antigen), B (only B antigen), AB (both A and B antigens), and O (neither A nor B antigen). The ABO antigens are illustrated in Figure 14.5.4.
- In the Rhesus system, there is just one common antigen. A person may either have the antigen (Rh+) or lack the antigen (Rh-).
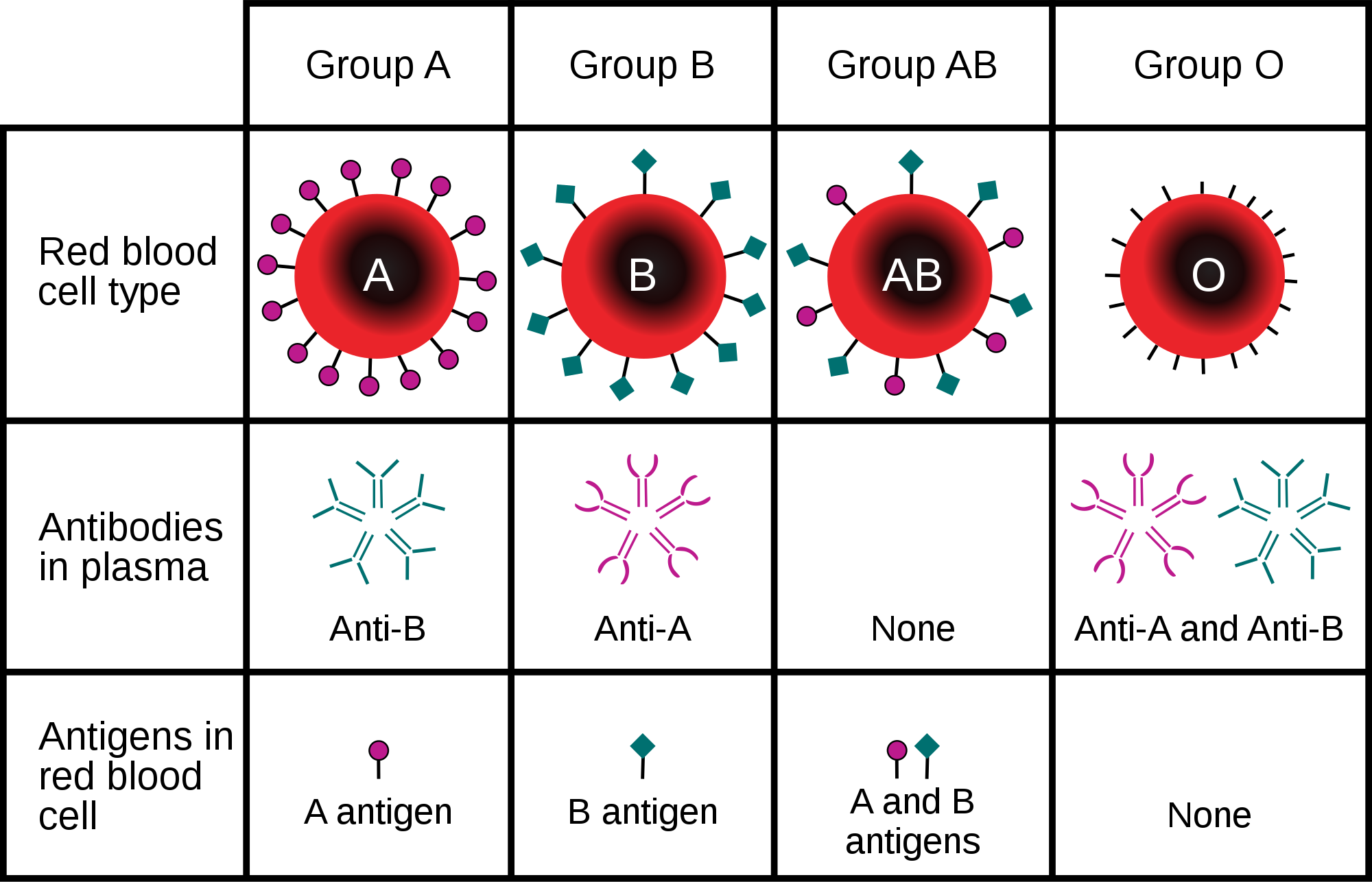
Blood type is important for medical reasons. A person who needs a blood transfusion must receive blood of a compatible type. Blood that is compatible lacks antigens that the patient's own blood also lacks. For example, for a person with type A blood (no B antigen), compatible types include any type of blood that lacks the B antigen. This would include type A blood or type O blood, but not type AB or type B blood. If incompatible blood is transfused, it may cause a potentially life-threatening reaction in the patient’s blood.
Leukocytes
Leukocytes (also called white blood cells) are cells in blood that defend the body against invading microorganisms and other threats. There are far fewer leukocytes than red blood cells in blood. There are normally only about 1,000 to 11,000 white blood cells per microlitre of blood. Unlike erythrocytes, leukocytes have a nucleus. White blood cells are part of the body’s immune system. They destroy and remove old or abnormal cells and cellular debris, as well as attack pathogens and foreign substances. There are five main types of white blood cells, which are described in Table 14.5.1: neutrophils, eosinophils, basophils, lymphocytes, and monocytes. The five types differ in their specific immune functions.
| Type of Leukocyte | Per cent of All Leukocytes | Main Function(s) |
|---|---|---|
| Neutrophil | 62% | Phagocytize (engulf and destroy) bacteria and fungi in blood. |
| Eosinophil | 2% | Attack and kill large parasites; carry out allergic responses. |
| Basophil | less than 1% | Release histamines in inflammatory responses. |
| Lymphocyte | 30% | Attack and destroy virus-infected and tumor cells; create lasting immunity to specific pathogens. |
| Monocyte | 5% | Phagocytize pathogens and debris in tissues. |
Thrombocytes
Thrombocytes, also called platelets, are actually cell fragments. Like erythrocytes, they lack a nucleus and are more numerous than white blood cells. There are about 150 thousand to 400 thousand thrombocytes per microlitre of blood.
The main function of thrombocytes is blood clotting, or coagulation. This is the process by which blood changes from a liquid to a gel, forming a plug in a damaged blood vessel. If blood clotting is successful, it results in hemostasis, which is the cessation of blood loss from the damaged vessel. A blood clot consists of both platelets and proteins, especially the protein fibrin. You can see a scanning electron microscope photomicrograph of a blood clot in Figure 14.5.5.
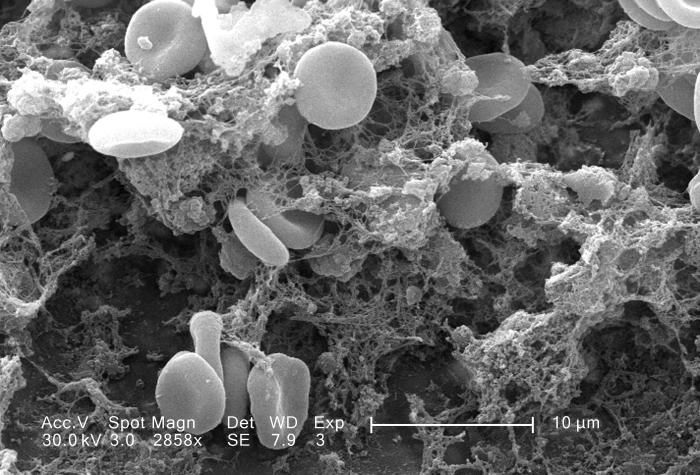
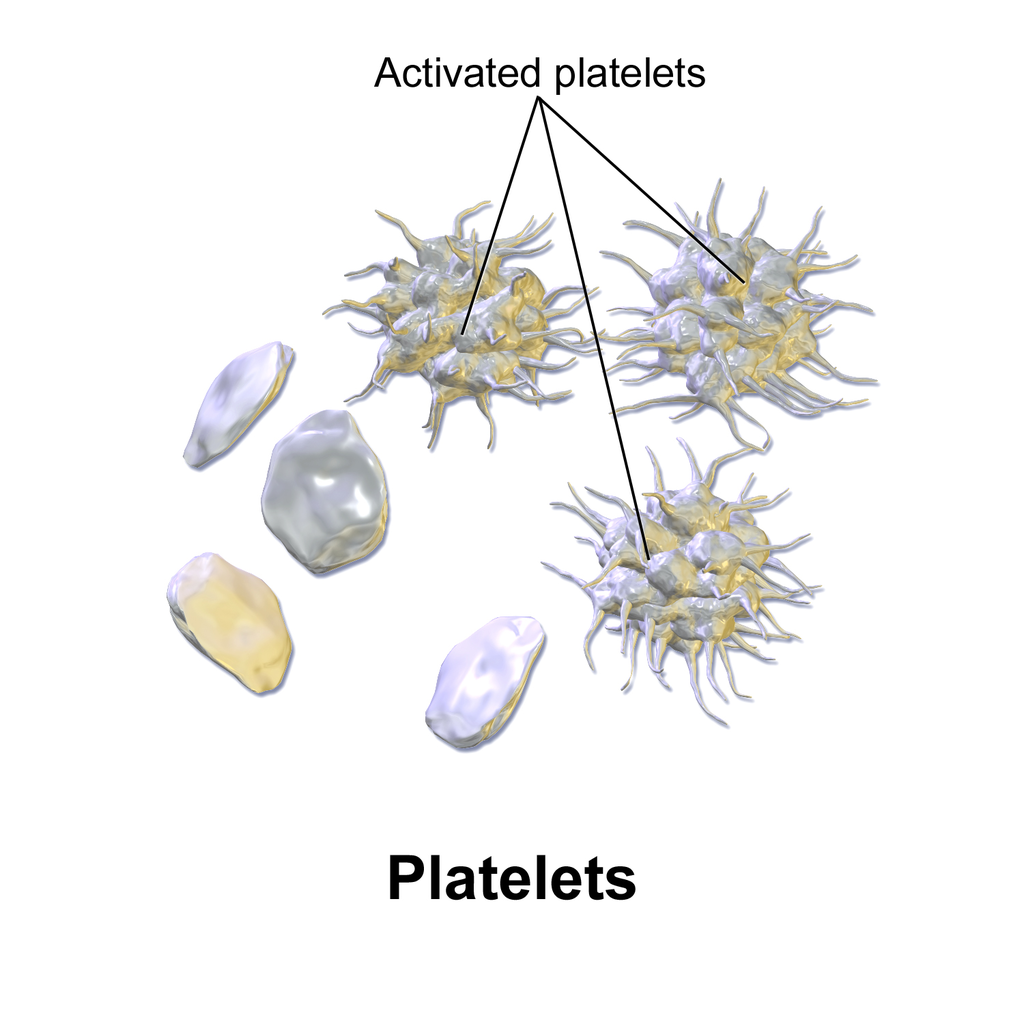
Coagulation begins almost instantly after an injury occurs to the endothelium of a blood vessel. Thrombocytes become activated and change their shape from spherical to star-shaped, as shown in Figure 14.5.6. This helps them aggregate with one another (stick together) at the site of injury to start forming a plug in the vessel wall. Activated thrombocytes also release substances into the blood that activate additional thrombocytes and start a sequence of reactions leading to fibrin formation. Strands of fibrin crisscross the platelet plug and strengthen it, much as rebar strengthens concrete.
Formation and Degradation of Blood Cells
Blood is considered a connective tissue, because blood cells form inside bones. All three types of blood cells are made in red marrow within the medullary cavity of bones in a process called hematopoiesis. Formation of blood cells occurs by the proliferation of stem cells in the marrow. These stem cells are self-renewing — when they divide, some of the daughter cells remain stem cells, so the pool of stem cells is not used up. Other daughter cells follow various pathways to differentiate into the variety of blood cell types. Once the cells have differentiated, they cannot divide to form copies of themselves.
Eventually, blood cells die and must be replaced through the formation of new blood cells from proliferating stem cells. After blood cells die, the dead cells are phagocytized (engulfed and destroyed) by white blood cells, and removed from the circulation. This process most often takes place in the spleen and liver.
Blood Disorders
Many human disorders primarily affect the blood. They include cancers, genetic disorders, poisoning by toxins, infections, and nutritional deficiencies.
- Leukemia is a group of cancers of the blood-forming tissues in the bone marrow. It is the most common type of cancer in children, although most cases occur in adults. Leukemia is generally characterized by large numbers of abnormal leukocytes. Symptoms may include excessive bleeding and bruising, fatigue, fever, and an increased risk of infections. Leukemia is thought to be caused by a combination of genetic and environmental factors.
- Hemophilia refers to any of several genetic disorders that cause dysfunction in the blood clotting process. People with hemophilia are prone to potentially uncontrollable bleeding, even with otherwise inconsequential injuries. They also commonly suffer bleeding into the spaces between joints, which can cause crippling.
- Carbon monoxide poisoning occurs when inhaled carbon monoxide (in fumes from a faulty home furnace or car exhaust, for example) binds irreversibly to the hemoglobin in erythrocytes. As a result, oxygen cannot bind to the red blood cells for transport throughout the body, and this can quickly lead to suffocation. Carbon monoxide is extremely dangerous, because it is colourless and odorless, so it cannot be detected in the air by human senses.
- HIV is a virus that infects certain types of leukocytes and interferes with the body’s ability to defend itself from pathogens and other causes of illness. HIV infection may eventually lead to AIDS (acquired immunodeficiency syndrome). AIDS is characterized by rare infections and cancers that people with a healthy immune system almost never acquire.
- Anemia is a disorder in which the blood has an inadequate volume of erythrocytes, reducing the amount of oxygen that the blood can carry, and potentially causing weakness and fatigue. These and other signs and symptoms of anemia are shown in Figure 14.5.8. Anemia has many possible causes, including excessive bleeding, inherited disorders (such as sickle cell hemoglobin), or nutritional deficiencies (iron, folate, or B12). Severe anemia may require transfusions of donated blood.
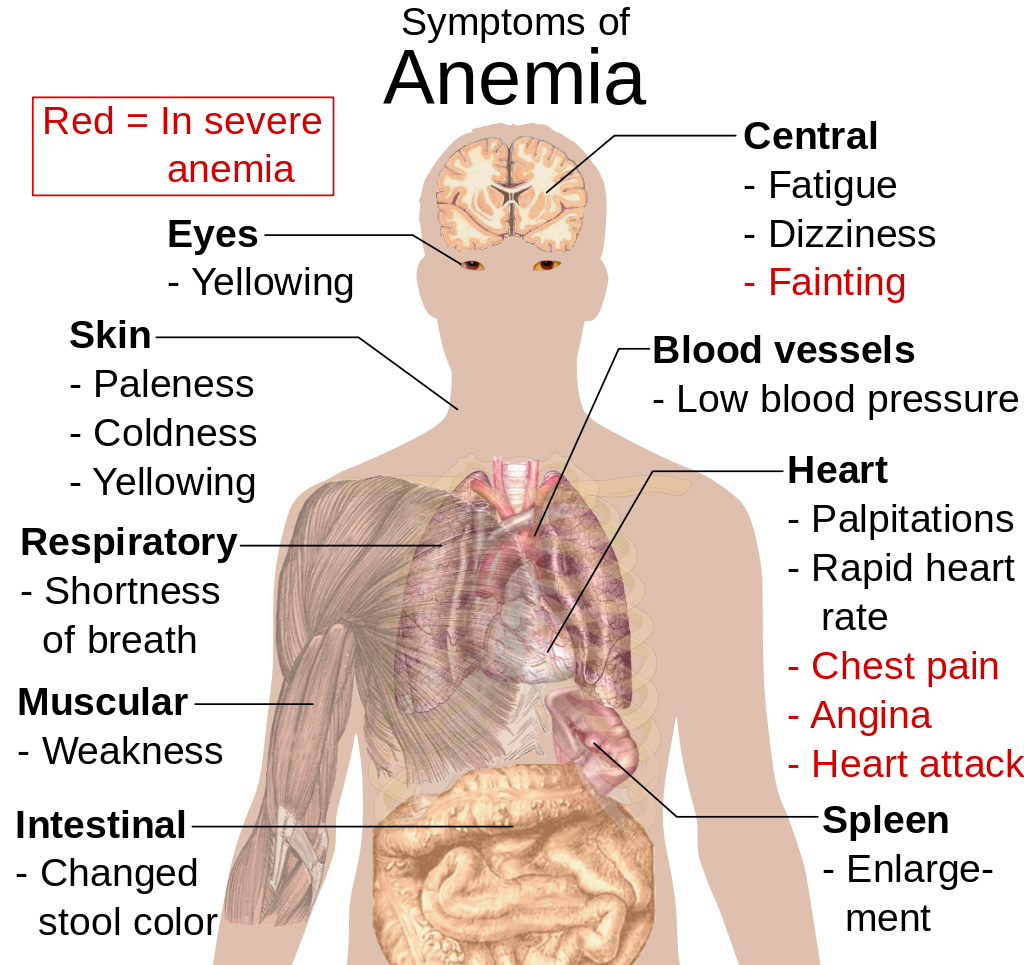
Feature: Myth vs. Reality
Donating blood saves lives. In fact, with each blood donation, as many as three lives may be saved. According to Government Canada, up to 52% of Canadians have reported that they or a family member have needed blood or blood products at some point in their lifetime. Many donors agree that the feeling that comes from knowing you have saved lives is well worth the short amount of time it takes to make a blood donation. Nonetheless, only a minority of potential donors actually donate blood. There are many myths about blood donation that may help explain the small percentage of donors. Knowing the facts may reaffirm your decision to donate if you are already a donor — and if you aren’t a donor already, getting the facts may help you decide to become one.
| Myth | Reality |
|---|---|
| "Your blood might become contaminated with an infection during the donation." | There is no risk of contamination because only single-use, disposable catheters, tubing, and other equipment are used to collect blood for a donation. |
| "You are too old (or too young) to donate blood." | There is no upper age limit on donating blood, as long as you are healthy. The minimum age is 16 years. |
| "You can’t donate blood if you have high blood pressure." | As long as your blood pressure is below 180/100 at the time of donation, you can give blood. Even if you take blood pressure medication to keep your blood pressure below this level, you can donate. |
| "You can’t give blood if you have high cholesterol." | Having high cholesterol does not affect your ability to donate blood. Taking cholesterol-lowering medication also does not disqualify you. |
| "You can’t donate blood if you have had a flu shot." | Having a flu shot has no effect on your ability to donate blood. You can even donate on the same day that you receive a flu shot. |
| "You can’t donate blood if you take medication." | As long as you are healthy, in most cases, taking medication does not preclude you from donating blood. |
| "Your blood isn’t needed if it’s a common blood type." | All types of blood are in constant demand. |
14.5 Summary
- Blood is a fluid connective tissue that circulates throughout the body in the cardiovascular system. Blood supplies tissues with oxygen and nutrients and removes their metabolic wastes. Blood helps defend the body from pathogens and other threats, transports hormones and other substances, and helps keep the body’s pH and temperature in homeostasis.
- Plasma is the liquid component of blood, and it makes up more than half of blood by volume. It consists of water and many dissolved substances. It also contains blood cells, including erythrocytes, leukocytes and thrombocytes.
- Erythrocytes, (also known as red blood cells) are the most numerous cells in blood. They consist mostly of hemoglobin, which carries oxygen. Erythrocytes also carry antigens that determine blood type.
- Leukocytes (also referred to as white blood cells) are less numerous than erythrocytes and are part of the body’s immune system. There are several different types of leukocytes that differ in their specific immune functions. They protect the body from abnormal cells, microorganisms, and other harmful substances.
- Thrombocytes (also called platelets) are cell fragments that play important roles in blood clotting, or coagulation. They stick together at breaks in blood vessels to form a clot and stimulate the production of fibrin, which strengthens the clot.
- All blood cells form by proliferation of stem cells in red bone marrow in a process called hematopoiesis. When blood cells die, they are phagocytized by leukocytes and removed from the circulation.
- Disorders of the blood include leukemia, which is cancer of the bone-forming cells; hemophilia, which is any of several genetic blood-clotting disorders; carbon monoxide poisoning, which prevents erythrocytes from binding with oxygen and causes suffocation; HIV infection, which destroys certain types of leukocytes and can cause AIDS; and anemia, in which there are not enough erythrocytes to carry adequate oxygen to body tissues.
14.5 Review Questions
- What is blood? Why is blood considered a connective tissue?
- Identify four physiological roles of blood in the body.
- Describe plasma and its components.
-
14.5 Explore More
https://youtu.be/e-5wqwp64MM
Joe Landolina: This gel can make you stop bleeding instantly, TED, 2014.
https://youtu.be/hgp8LtwFSBA
Can Synthetic Blood Help The World's Blood Shortage? Science Plus, 2016.
https://youtu.be/1Qfmkd6C8u8
How bones make blood - Melody Smith, TED-Ed, 2020.
Attributions
Figure 14.5.1
vampire_PNG32 from pngimg.com is used under a CC BY-NC 4.0 (https://creativecommons.org/licenses/by-nc/4.0/) license.
Figure 14.5.2
Blood-centrifugation-scheme by KnuteKnudsen at English Wikipedia on Wikimedia Commons is used under a CC BY 3.0 (https://creativecommons.org/licenses/by/3.0) license.
Figure 14.5.3
SEM_blood_cells by Bruce Wetzel and Harry Schaefer (Photographers)/ NCI AV-8202-3656 on Wikimedia Commons is in the public domain (https://en.wikipedia.org/wiki/en:Public_domain).
Figure 14.5.4
ABO_blood_type.svg by InvictaHOG on Wikimedia Commons is in the public domain (https://en.wikipedia.org/wiki/en:Public_domain).
Figure 14.5.5
Blood_clot_in_scanning_electron_microscopy by Janice Carr from CDC/ Public Health Image LIbrary (PHIL) ID #7308 on Wikimedia Commons is in the public domain (https://en.wikipedia.org/wiki/en:Public_domain).
Figure 14.5.6
Blausen_0740_Platelets by BruceBlaus on Wikimedia Commons is used under a CC BY 3.0 (https://creativecommons.org/licenses/by/3.0) license.
Figure 14.5.7
Platelet_Party_900x by Awkward Yeti (used with permission of the author) © All Rights Reserved
Figure 14.5.8
Symptoms_of_anemia.svg by Mikael Häggström on Wikimedia Commons is in the public domain (https://en.wikipedia.org/wiki/en:public_domain).
References
Blausen.com Staff. (2014). Medical gallery of Blausen Medical 2014. WikiJournal of Medicine 1 (2). DOI:10.15347/wjm/2014.010. ISSN 2002-4436.
Blood, organ and tissue donation. (2020, April 28). Government of Canada. https://www.canada.ca/en/public-health/services/healthy-living/blood-organ-tissue-donation.html#a3
Canadian Blood Services. (n.d.). There is an immediate need for blood as demand is rising. https://www.blood.ca
Science Plus. (2016, March 2). Can synthetic blood help the world's blood shortage? https://www.youtube.com/watch?v=hgp8LtwFSBA&feature=youtu.be
TED. (2014, November 20). Joe Landolina: This gel can make you stop bleeding instantly. YouTube. https://www.youtube.com/watch?v=e-5wqwp64MM&feature=youtu.be
TED-Ed. (2020, January 27). How bones make blood - Melody Smith. YouTube. https://www.youtube.com/watch?v=1Qfmkd6C8u8&feature=youtu.be
Created by CK-12 Foundation/Adapted by Christine Miller

One Piano, Four Hands
Did you ever see two people play the same piano? How do they coordinate all the movements of their own fingers — let alone synchronize them with those of their partner? The peripheral nervous system plays an important part in this challenge.
What Is the Peripheral Nervous System?
The peripheral nervous system (PNS) consists of all the nervous tissue that lies outside of the central nervous system (CNS). The main function of the PNS is to connect the CNS to the rest of the organism. It serves as a communication relay, going back and forth between the CNS and muscles, organs, and glands throughout the body.
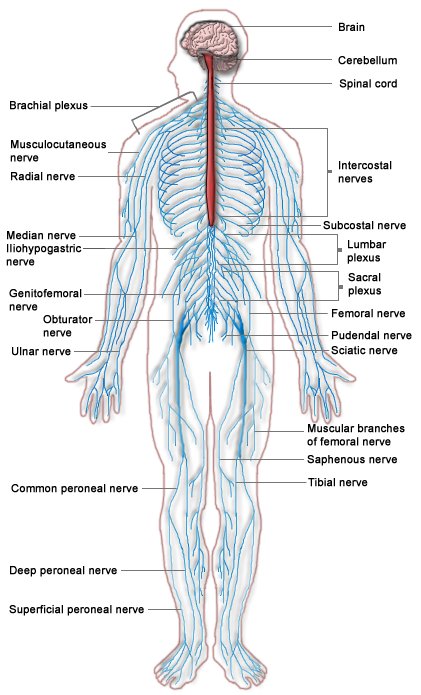
Tissues of the Peripheral Nervous System
The PNS is mostly made up of cable-like bundles of axons called nerves, as well as clusters of neuronal cell bodies called ganglia (singular, ganglion). Nerves are generally classified as sensory, motor, or mixed nerves based on the direction in which they carry nerve impulses.
- Sensory nerves transmit information from sensory receptors in the body to the CNS. Sensory nerves are also called afferent nerves. You can see an example in the figure below.
- Motor nerves transmit information from the CNS to muscles, organs, and glands. Motor nerves are also called efferent nerves. You can see one in the figure below.
- Mixed nerves contain both sensory and motor neurons, so they can transmit information in both directions. They have both afferent and efferent functions.
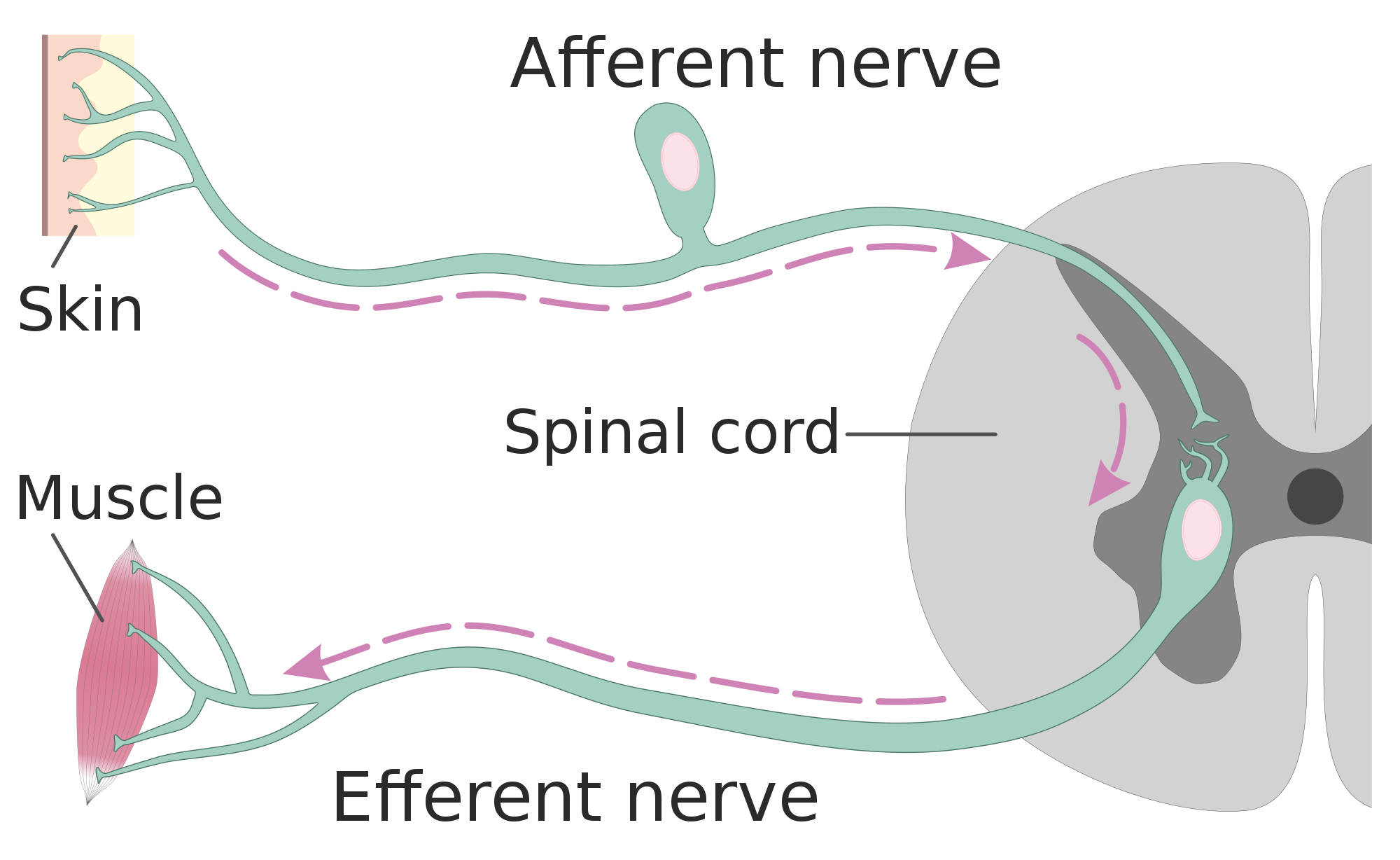
Divisions of the Peripheral Nervous System
The PNS is divided into two major systems, called the autonomic nervous system and the somatic nervous system. In the diagram below, the autonomic system is shown on the left, and the somatic system on the right. Both systems of the PNS interact with the CNS and include sensory and motor neurons, but they use different circuits of nerves and ganglia.
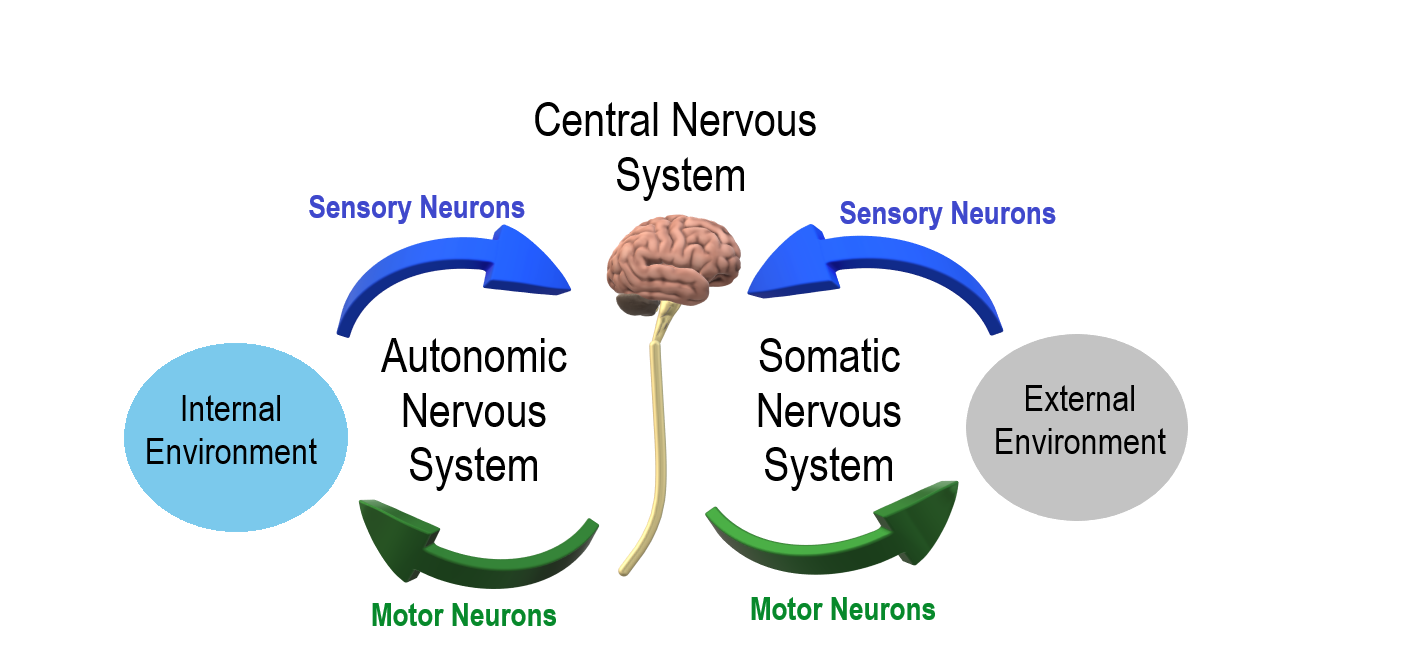
Somatic Nervous System
The somatic nervous system primarily senses the external environment and controls voluntary activities about which decisions and commands come from the cerebral cortex of the brain. When you feel too warm, for example, you decide to turn on the air conditioner. As you walk across the room to the thermostat, you are using your somatic nervous system. In general, the somatic nervous system is responsible for all of your conscious perceptions of the outside world, as well as all of the voluntary motor activities you perform in response. Whether it’s playing a piano, driving a car, or playing basketball, you can thank your somatic nervous system for making it possible.
Somatic sensory and motor information is transmitted through 12 pairs of cranial nerves and 31 pairs of spinal nerves. Cranial nerves are in the head and neck and connect directly to the brain. Sensory components of cranial nerves transmit information about smells, tastes, light, sounds, and body position. Motor components of cranial nerves control skeletal muscles of the face, tongue, eyeballs, throat, head, and shoulders. Motor components of cranial nerves also control the salivary glands and swallowing. Four of the 12 cranial nerves participate in both sensory and motor functions as mixed nerves, having both sensory and motor neurons.
Spinal nerves emanate from the spinal column between vertebrae. All of the spinal nerves are mixed nerves, containing both sensory and motor neurons. The areas of skin innervated by the 31 pairs of spinal nerves are shown in the figure below. These include sensory nerves in the skin that sense pressure, temperature, vibrations, and pain. Other sensory nerves are in the muscles, and they sense stretching and tension. Spinal nerves also include motor nerves that stimulate skeletal muscles to contract, allowing for voluntary body movements.
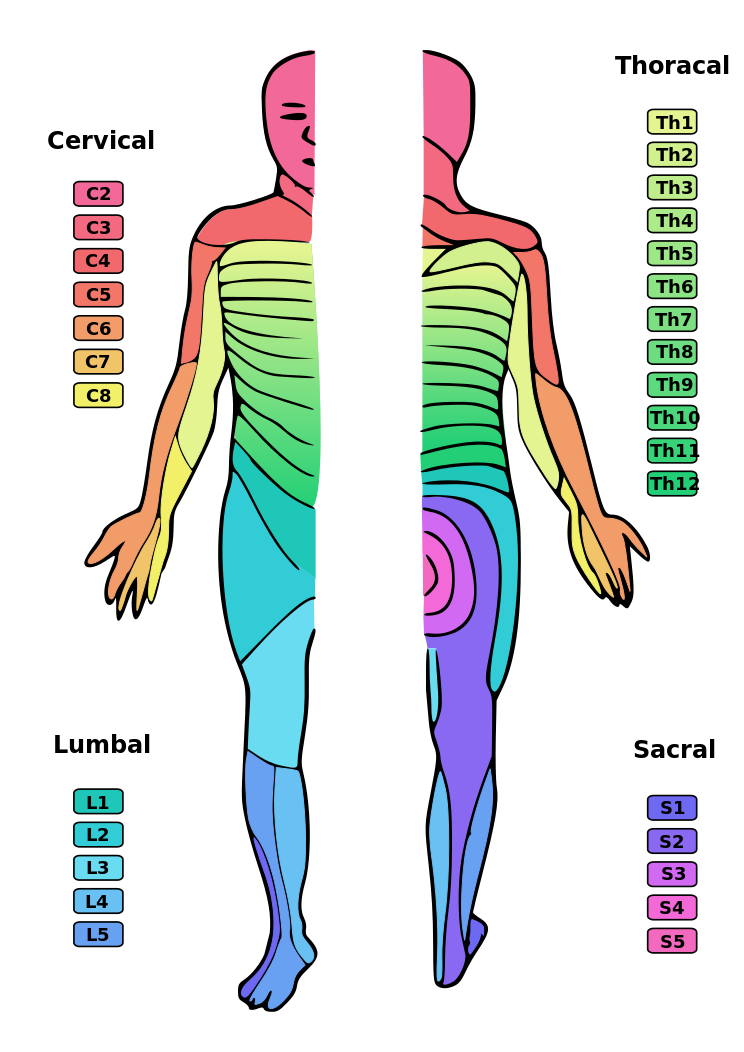
Autonomic Nervous System
The autonomic nervous system primarily senses the internal environment and controls involuntary activities. It is responsible for monitoring conditions in the internal environment and bringing about appropriate changes in them. In general, the autonomic nervous system is responsible for all the activities that go on inside your body without your conscious awareness or voluntary participation.
Structurally, the autonomic nervous system consists of sensory and motor nerves that run between the CNS (especially the hypothalamus in the brain), internal organs (such as the heart, lungs, and digestive organs), and glands (such as the pancreas and sweat glands). Sensory neurons in the autonomic system detect internal body conditions and send messages to the brain. Motor nerves in the autonomic system affect appropriate responses by controlling contractions of smooth or cardiac muscle, or glandular tissue. For example, when sensory nerves of the autonomic system detect a rise in body temperature, motor nerves signal smooth muscles in blood vessels near the body surface to undergo vasodilation, and the sweat glands in the skin to secrete more sweat to cool the body.
The autonomic nervous system, in turn, has three subdivisions: the sympathetic division, parasympathetic division, and enteric division. The first two subdivisions of the autonomic system are summarized in the figure below. Both affect the same organs and glands, but they generally do so in opposite ways.
- The sympathetic division controls the fight-or-flight response. Changes occur in organs and glands throughout the body that prepare the body to fight or flee in response to a perceived danger. For example, the heart rate speeds up, air passages in the lungs become wider, more blood flows to the skeletal muscles, and the digestive system temporarily shuts down.
- The parasympathetic division returns the body to normal after the fight-or-flight response has occurred. For example, it slows down the heart rate, narrows air passages in the lungs, reduces blood flow to the skeletal muscles, and stimulates the digestive system to start working again. The parasympathetic division also maintains internal homeostasis of the body at other times.
- The enteric division is made up of nerve fibres that supply the organs of the digestive system. This division allows for the local control of many digestive functions.
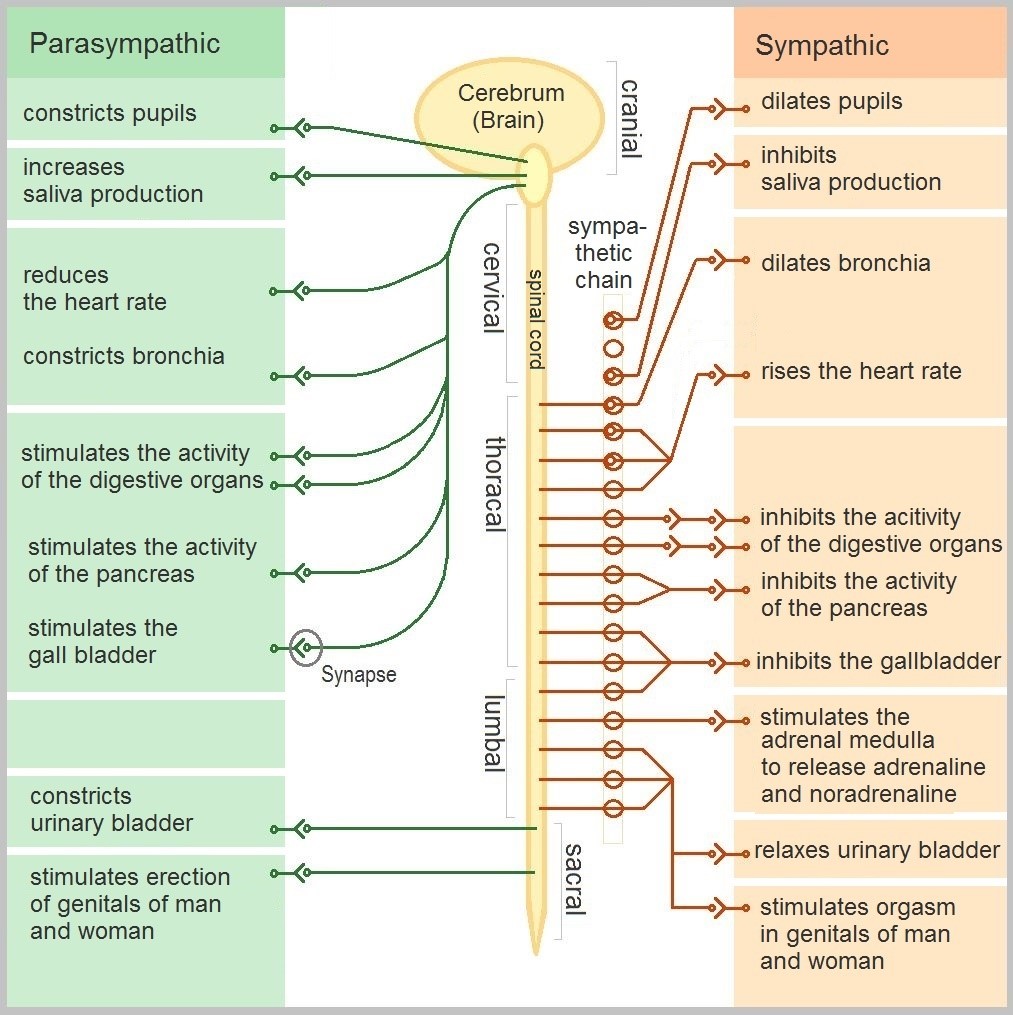
Disorders of the Peripheral Nervous System
Unlike the CNS — which is protected by bones, meninges, and cerebrospinal fluid — the PNS has no such protections. The PNS also has no blood-brain barrier to protect it from toxins and pathogens in the blood. Therefore, the PNS is more subject to injury and disease than is the CNS. Causes of nerve injury include diabetes, infectious diseases (such as shingles), and poisoning by toxins (such as heavy metals). PNS disorders often have symptoms like loss of feeling, tingling, burning sensations, or muscle weakness. If a traumatic injury results in a nerve being transected (cut all the way through), it may regenerate, but this is a very slow process and may take many months.
Two other diseases of the PNS are Guillain-Barre syndrome and Charcot-Marie-Tooth disease.
- Guillain-Barre syndrome is a rare disease in which the immune system attacks nerves of the PNS, leading to muscle weakness and even paralysis. The exact cause of Guillain-Barre syndrome is unknown, but it often occurs after a viral or bacterial infection. There is no known cure for the syndrome, but most people eventually make a full recovery. Recovery can be slow, however, lasting anywhere from several weeks to several years.
- Charcot-Marie-Tooth disease is a hereditary disorder of the nerves, and one of the most common inherited neurological disorders. It affects predominantly the nerves in the feet and legs, and often in the hands and arms, as well. The disease is characterized by loss of muscle tissue and sense of touch. It is presently incurable.
Feature: My Human Body
The autonomic nervous system is considered to be involuntary because it doesn't require conscious input. However, it is possible to exert some voluntary control over it. People who practice yoga or other so-called mind-body techniques, for example, can reduce their heart rate and certain other autonomic functions. Slowing down these otherwise involuntary responses is a good way to relieve stress and reduce the wear-and-tear that stress can place on the body. Such techniques may also be useful for controlling post-traumatic stress disorder and chronic pain. Three types of integrative practices for these purposes are breathing exercises, body-based tension modulation exercises, and mindfulness techniques.
Breathing exercises can help control the rapid, shallow breathing that often occurs when you are anxious or under stress. These exercises can be learned quickly, and they provide immediate feelings of relief. Specific breathing exercises include paced breath, diaphragmatic breathing, and Breathe2Relax or Chill Zone on MindShift™ CBT, which are downloadable breathing practice mobile applications, or "Apps". Try syncing your breathing with Eric Klassen's "Triangle breathing, 1 minute" video:
https://www.youtube.com/watch?v=u9Q8D6n-3qw
Triangle breathing, 1 minute, Erin Klassen, 2015.
Body-based tension modulation exercises include yoga postures (also known as “asanas”) and tension manipulation exercises. The latter include the Trauma/Tension Release Exercise (TRE) and the Trauma Resiliency Model (TRM). Watch this video for a brief — but informative — introduction to the TRE program:
https://www.youtube.com/watch?v=67R974D8swM&feature=youtu.be
TRE® : Tension and Trauma Releasing Exercises, an Introduction with Jessica Schaffer, Jessica Schaffer Nervous System RESET, 2015.
Mindfulness techniques have been shown to reduce symptoms of depression, as well as those of anxiety and stress. They have also been shown to be useful for pain management and performance enhancement. Specific mindfulness programs include Mindfulness Based Stress Reduction (MBSR) and Mindfulness Mind-Fitness Training (MMFT). You can learn more about MBSR by watching the video below.
https://www.youtube.com/watch?v=0TA7P-iCCcY&feature=youtu.be
Mindfulness-Based Stress Reduction (UMass Medical School, Center for Mindfulness), Palouse Mindfulness, 2017.
8.6 Summary
- The peripheral nervous system (PNS) consists of all the nervous tissue that lies outside the central nervous system (CNS). Its main function is to connect the CNS to the rest of the organism.
- The PNS is made up of nerves and ganglia. Nerves are bundles of axons, and ganglia are groups of cell bodies. Nerves are classified as sensory, motor, or a mix of the two.
- The PNS is divided into the somatic and autonomic nervous systems. The somatic system controls voluntary activities, whereas the autonomic system controls involuntary activities.
- The autonomic nervous system is further divided into sympathetic, parasympathetic, and enteric divisions. The sympathetic division controls fight-or-flight responses during emergencies, the parasympathetic system controls routine body functions the rest of the time, and the enteric division provides local control over the digestive system.
- The PNS is not as well protected physically or chemically as the CNS, so it is more prone to injury and disease. PNS problems include injury from diabetes, shingles, and heavy metal poisoning. Two disorders of the PNS are Guillain-Barre syndrome and Charcot-Marie-Tooth disease.
8.6 Review Questions
- Describe the general structure of the peripheral nervous system. State its primary function.
- What are ganglia?
- Identify three types of nerves based on the direction in which they carry nerve impulses.
- Outline all of the divisions of the peripheral nervous system.
- Compare and contrast the somatic and autonomic nervous systems.
- When and how does the sympathetic division of the autonomic nervous system affect the body?
- What is the function of the parasympathetic division of the autonomic nervous system? Specifically, how does it affect the body?
- Name and describe two peripheral nervous system disorders.
- Give one example of how the CNS interacts with the PNS to control a function in the body.
- For each of the following types of information, identify whether the neuron carrying it is sensory or motor, and whether it is most likely in the somatic or autonomic nervous system:
- Visual information
- Blood pressure information
- Information that causes muscle contraction in digestive organs after eating
- Information that causes muscle contraction in skeletal muscles based on the person’s decision to make a movement
-
8.6 Explore More
https://www.youtube.com/watch?v=ySIDMU2cy0Y&feature=emb_logo
Phantom Limbs Explained, Plethrons, 2015.
https://www.youtube.com/watch?time_continue=1&v=73yo5nJne6c&feature=emb_logo
Why Do Hot Peppers Cause Pain? Reactions, 2015.
Attributions
Figure 8.6.1
Kid’s piant duet by PJMixer on Flickr is used under a CC BY-NC-ND 2.0 (https://creativecommons.org/licenses/by-nc-nd/2.0/) license.
Figure 8.6.2
Nervous_system_diagram by ¤~Persian Poet Gal on Wikimedia Commons is released into the public domain (https://en.wikipedia.org/wiki/Public_domain).
Figure 8.6.3
Afferent_and_efferent_neurons_en.svg by Helixitta on Wikimedia Commons is used under a CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0) license.
Figure 8.6.4
Autonomic and Somatic Nervous System by Christinelmiller on Wikimedia Commons is used under a CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0) license.
Figure 8.6.5
Dermatoms.svg by Ralf Stephan (mailto:ralf@ark.in-berlin.de) on Wikimedia Commons is released into the public domain (https://en.wikipedia.org/wiki/Public_domain).
Figure 8.6.6
The_Autonomic_Nervous_System by Geo-Science-International on Wikimedia Commons is used and adapted by Christine Miller under a CC0 1.0 Universal
Public Domain Dedication license (https://creativecommons.org/publicdomain/zero/1.0/).
References
Erin Klassen. (2015, December 15). Triangle breathing, 1 minute. YouTube. https://www.youtube.com/watch?v=u9Q8D6n-3qw&feature=youtu.be
Jessica Schaffer Nervous System RESET. (2015, January 15). TRE® : Tension and trauma releasing exercises, an Introduction with Jessica Schaffer. YouTube. https://www.youtube.com/watch?v=67R974D8swM&feature=youtu.be
Mayo Clinic Staff. (n.d.). Charcot-Marie-Tooth disease [online article]. MayoClinic.org. https://www.mayoclinic.org/diseases-conditions/charcot-marie-tooth-disease/symptoms-causes/syc-20350517
Mayo Clinic Staff. (n.d.). Diabetes [online article]. MayoClinic.org. https://www.mayoclinic.org/diseases-conditions/diabetes/symptoms-causes/syc-20371444
Mayo Clinic Staff. (n.d.). Guillain-Barre syndrome [online article]. MayoClinic.org. https://www.mayoclinic.org/diseases-conditions/guillain-barre-syndrome/symptoms-causes/syc-20362793
Mayo Clinic Staff. (n.d.). Shingles [online article]. MayoClinic.org. https://www.mayoclinic.org/diseases-conditions/shingles/symptoms-causes/syc-20353054
Mayo Clinic Staff. (n.d.). Stroke [online article]. MayoClinic.org. https://www.mayoclinic.org/diseases-conditions/stroke/symptoms-causes/syc-20350113
Palouse Mindfulness. (2017, March 25). Mindfulness-based stress reduction (UMass Medical School, Center for Mindfulness), YouTube. https://www.youtube.com/watch?v=0TA7P-iCCcY&feature=youtu.be
Plethrons, (2015, March 23). Phantom limbs explained. YouTube. https://www.youtube.com/watch?v=ySIDMU2cy0Y&feature=youtu.be
Reactions. (2015, December 1). Why do hot peppers cause pain? YouTube. https://www.youtube.com/watch?v=73yo5nJne6c&feature=youtu.be
Created by CK-12 Foundation/Adapted by Christine Miller

Art in a Cup
Who knew that a cup of coffee could also be a work of art? A talented barista can make coffee look as good as it tastes. If you are a coffee drinker, you probably know that coffee can also affect your mental state. It can make you more alert, and it may improve your concentration. That’s because the caffeine in coffee is a psychoactive drug. In fact, caffeine is the most widely consumed psychoactive substance in the world. In North America, for example, 90 per cent of adults consume caffeine daily.
What Are Psychoactive Drugs?
Psychoactive drugs are substances that change the function of the brain and result in alterations of mood, thinking, perception, and/or behavior. Psychoactive drugs may be used for many purposes, including therapeutic, ritual, or recreational purposes. Besides caffeine, other examples of psychoactive drugs include cocaine, LSD, alcohol, tobacco, codeine, and morphine. Psychoactive drugs may be legal prescription medications (codeine and morphine), legal nonprescription drugs (alcohol and tobacco), or illegal drugs (cocaine and LSD).
Cannabis (or marijuana) is also a psychoactive drug that while illegal in many countries is legal for use in Canada by individuals over the age of 19 years. Legal prescription medications (such as opioids) are also used illegally by increasingly large numbers of people. Some legal drugs, such as alcohol and nicotine, are readily available almost everywhere, as illustrated by the images below.
Figure 8.8.2 These psychoactive drugs are legal and accessible almost anywhere.
Classes of Psychoactive Drugs
Psychoactive drugs are divided into different classes based on their pharmacological effects. Several classes are listed below, along with examples of commonly used drugs in each class.
- Stimulants are drugs that stimulate the brain and increase alertness and wakefulness. Examples of stimulants include caffeine, nicotine, cocaine, and amphetamines (such as Adderall).
- Depressants are drugs that calm the brain, reduce anxious feelings, and induce sleepiness. Examples of depressants include ethanol (in alcoholic beverages) and opioids, such as codeine and heroin.
- Anxiolytics are drugs that have a tranquilizing effect and inhibit anxiety. Examples of anxiolytic drugs include benzodiazepines (such as diazepam/Valium), barbiturates (such as phenobarbital), opioids, and antidepressant drugs (such as sertraline/Zoloft).
- Euphoriants are drugs that bring about a state of euphoria, or intense feelings of well-being and happiness. Examples of euphoriants include the so-called "club drug" MDMA (ecstasy), amphetamines, ethanol, and opioids (such as morphine).
- Hallucinogens are drugs that can cause hallucinations and other perceptual anomalies. They also cause subjective changes in thoughts, emotions, and consciousness. Examples of hallucinogens include LSD, mescaline, nitrous oxide, and psilocybin.
- Empathogens are drugs that produce feelings of empathy, or sympathy with other people. Examples of empathogens include amphetamines and MDMA.
Many psychoactive drugs have multiple effects, so they may be placed in more than one class. One example is MDMA, pictured below, which may act both as a euphoriant and as an empathogen. In some people, MDMA may also have stimulant or hallucinogenic effects. As of 2016, MDMA had no accepted medical uses, but it was undergoing testing for use in the treatment of post-traumatic stress disorder and certain other types of anxiety disorders.

Mechanisms of Action
Psychoactive drugs generally produce their effects by affecting brain chemistry, which in turn may cause changes in a person’s mood, thinking, perception, and behavior. Each drug tends to have a specific action on one or more neurotransmitters or neurotransmitter receptors in the brain. Generally, they act as either agonists or antagonists.
- Agonists are drugs that increase the activity of particular neurotransmitters. They might act by promoting the synthesis of the neurotransmitters, reducing their reuptake from synapses, or mimicking their action by binding to receptors for the neurotransmitters.
- Antagonists are drugs that decrease the activity of particular neurotransmitters. They might act by interfering with the synthesis of the neurotransmitters or by blocking their receptors so the neurotransmitters cannot bind to them.
Consider the example of the neurotransmitter GABA. This is one of the most common neurotransmitters in the brain, and it normally has an inhibitory effect on cells. GABA agonists — which increase its activity — include ethanol, barbiturates, and benzodiazepines, among other psychoactive drugs. All of these drugs work by promoting the activity of GABA receptors in the brain.
Uses of Psychoactive Drugs
You may have been prescribed psychoactive drugs by your doctor. For example, your doctor may have prescribed you an opioid drug, such as codeine for pain (most likely in the form of Tylenol with added codeine). Chances are you also use nonprescription psychoactive drugs (like caffeine) for mental alertness. These are just two of the many possible uses of psychoactive drugs.
Medical Uses

General anesthesia is one use of psychoactive drugs in medicine. With general anesthesia, pain is blocked and unconsciousness is induced. General anesthetics are most often used during surgical procedures and may be administered in gaseous form, as in Figure 8.8.4. General anesthetics include the drugs halothane and ketamine. Other psychoactive drugs are used to manage pain without affecting consciousness. They may be prescribed either for acute pain in cases of trauma (such as broken bones) or for chronic pain caused by arthritis, cancer, or fibromyalgia. Most often, the drugs used for pain control are opioids, such as morphine and codeine.
Many psychiatric disorders are also managed with psychoactive drugs. Antidepressants like sertraline, for example, are used to treat depression, anxiety, and eating disorders. Anxiety disorders may also be treated with anxiolytics, such as buspirone and diazepam. Stimulants (such as amphetamines) are used to treat attention deficit disorder. Antipsychotics (such as clozapine and risperidone) — as well as mood stabilizers, such as lithium — are used to treat schizophrenia and bipolar disorder.
Ritual Uses

Certain psychoactive drugs, particularly hallucinogens, have been used for ritual purposes since prehistoric times. For example, Native Americans have used the mescaline-containing peyote cactus (pictured in Figure 8.8.5) for religious ceremonies for as long as 5,700 years. In prehistoric Europe, the mushroom Amanita muscaria, which contains a hallucinogenic drug called muscimol, was used for similar purposes. Various other psychoactive drugs — including jimsonweed, psilocybin mushrooms, and cannabis — have also been used for millennia, by various peoples, for ritual purposes.
Recreational Uses
The recreational use of psychoactive drugs generally has the purpose of altering one’s consciousness and creating a feeling of euphoria commonly called a “high.” Some of the drugs used most commonly for recreational purposes are cannabis, ethanol (alcohol), opioids, and stimulants (such as nicotine). Hallucinogens are also used recreationally, primarily for the alterations they cause in thinking and perception.
Some investigators have suggested that the urge to alter one’s state of consciousness is a universal human drive, similar to the drive to satiate thirst, hunger, or sexual desire. They think that this instinct is even present in children, who may attain an altered state by repetitive motions, such as spinning or swinging. Some nonhuman animals also exhibit a drive to experience altered states. They may consume fermented berries or fruit and become intoxicated. The way cats respond to catnip (see Figure 8.8.6) is another example.

Addiction, Dependence, and Rehabilitation
Psychoactive substances often bring about subjective changes that the user may find pleasant (euphoria) or advantageous (increased alertness). These changes are rewarding and positively reinforcing, so they have the potential for misuse, addiction, and dependence. Addiction refers to the compulsive use of a drug, despite negative consequences that such use may entail. Sustained use of an addictive drug may produce dependence on the drug. Dependence may be physical and/or psychological. It occurs when cessation of drug use produces withdrawal symptoms. Physical dependence produces physical withdrawal symptoms, which may include tremors, pain, seizures, or insomnia. Psychological dependence produces psychological withdrawal symptoms, such as anxiety, depression, paranoia, or hallucinations.
Rehabilitation for drug dependence and addiction typically involves psychotherapy, which may include both individual and group therapy. Organizations such as Alcoholics Anonymous (AA) and Narcotics Anonymous (NA) may also be helpful for people trying to recover from addiction. These groups are self-described as international mutual aid fellowships, and their primary purpose is to help addicts achieve and maintain sobriety. In some cases, rehabilitation is aided by the temporary use of psychoactive substances that reduce cravings and withdrawal symptoms without creating addiction themselves. The drug methadone, for example, is commonly used to treat heroin addiction.
Feature: Human Biology in the News
In North America, a lot of media attention is currently given to a rising tide of opioid addiction and overdose deaths. Opioids are drugs derived from the opium poppy or synthetic versions of such drugs. They include the illegal drug heroin, as well as prescription painkillers such as codeine, morphine, hydrocodone, oxycodone, and fentanyl. In 2016, fentanyl received wide media attention when it was announced that an accidental fentanyl overdose was responsible for the death of music icon Prince. Fentanyl is an extremely strong and dangerous drug, said to be 50 to 100 times stronger than morphine, making risk of overdose death from fentanyl very high.
The dramatic increase in opioid addiction and overdose deaths has been called an opioid epidemic. It is considered to be the worst drug crisis in Canadian history. Consider the following facts:
- In 2016, there were almost 2,500 opioid-related deaths in Canada — almost 7 per day.
- The number of prescriptions written for opioids quadrupled between 1999 and 2010. If you have been prescribed codeine, fentanyl, morphine, oxycodone, hydromorphone or medical heroin, then you have been prescribed an opiate.
- There are many long-term health effects of using opioids, which include:
- Increased tolerance to the drug.
- Liver damage.
- Substance use disorder or addiction.
Doctors, public health professionals, and politicians have all called for new policies, funding, programs, and laws to address the opioid epidemic. Changes that have already been made include a shift from criminalizing to medicalizing the problem, more treatment programs, and more widespread distribution and use of the opioid-overdose antidote naloxone (Narcan). Opioids can slow or stop a person's breathing, which is what usually causes overdose deaths. Naloxone helps the person wake up and keeps them breathing until emergency medical treatment can be provided.
What, if anything, will work to stop the opioid epidemic in Canada and the United States? Keep watching the news to find out.
8.8 Summary
- Psychoactive drugs are substances that change the function of the brain and result in alterations of mood, thinking, perception, and behavior. They include prescription medications (such as opioid painkillers), legal substances (such as nicotine and alcohol), and illegal drugs (such as LSD and heroin).
- Psychoactive drugs are divided into different classes according to their pharmacological effects. They include stimulants, depressants, anxiolytics, euphoriants, hallucinogens, and empathogens. Many psychoactive drugs have multiple effects, so they may be placed in more than one class.
- Psychoactive drugs generally produce their effects by affecting brain chemistry. Generally, they act either as agonists — which enhance the activity of particular neurotransmitters — or as antagonists, which decrease the activity of particular neurotransmitters.
- Psychoactive drugs are used for various purposes, including medical, ritual, and recreational purposes.
- Misuse of psychoactive drugs may lead to addiction, which is the compulsive use of a drug despite the negative consequences such use may entail. Sustained use of an addictive drug may produce physical or psychological dependence on the drug. Rehabilitation typically involves psychotherapy, and sometimes the temporary use of other psychoactive drugs.
8.8 Review Questions
- What are psychoactive drugs?
- Identify six classes of psychoactive drugs, along with an example of a drug in each class.
- Compare and contrast psychoactive drugs that are agonists and psychoactive drugs that are antagonists.
- Describe two medical uses of psychoactive drugs.
- Give an example of a ritual use of a psychoactive drug.
- Generally speaking, why do people use psychoactive drugs recreationally?
- Define addiction.
- Identify possible withdrawal symptoms associated with physical dependence on a psychoactive drug.
- Why might a person with a heroin addiction be prescribed the psychoactive drug methadone?
- The prescription drug Prozac inhibits the reuptake of the neurotransmitter serotonin, causing more serotonin to be present in the synapse. Prozac can elevate mood, which is why it is sometimes used to treat depression. Answer the following questions about Prozac:
- Is Prozac an agonist or an antagonist for serotonin? Explain your answer.
- Is Prozac a psychoactive drug? Explain your answer.
- Name three classes of psychoactive drugs that include opioids.
- True or False: All psychoactive drugs are either illegal or available by prescription only.
- True or False: Anxiolytics might be prescribed by a physician.
- Name two drugs that activate receptors for the neurotransmitter GABA. Why do you think these drugs generally have a depressant effect?
8.8 Explore More
https://www.youtube.com/watch?v=foLf5Bi9qXs
How does caffeine keep us awake? - Hanan Qasim, TED-Ed, 2017.
https://www.youtube.com/watch?v=8qK0hxuXOC8
How do drugs affect the brain? - Sara Garofalo, TED-Ed, 2017.
https://www.youtube.com/watch?v=Nlcr1jd_Tok
Is marijuana bad for your brain? - Anees Bahji, TED-Ed, 2019.
Attributions
Figure 8.8.1
Cappucino Art by drew-coffman-tZKwLRO904E [photo] by Drew Coffman on Unsplash is used under the Unsplash License (https://unsplash.com/license).
Figure 8.8.2
- 3804, Saint-Laurent, Montreal - Cannabis Culture shop by Exile on Ontario St (Montreal, Canada) on Wikimedia Commons is used under a CC BY SA 2.0 (https://creativecommons.org/licenses/by-sa/2.0/deed.en) license.
- Drive Through Cigarette Store by Cosmo Spacely on Flickr is used under CC BY-NC-SA 2.0 (https://creativecommons.org/licenses/by-nc-sa/2.0/) license.
- Franklin-Nicollet Liquors by Max Sparber on Flickr is used under a CC BY 2.0 (https://creativecommons.org/licenses/by/2.0/deed.en) license.
Figure 8.8.3
Ecstasy_monogram by Drug Enforcement Administration on Wikimedia Commons is in the public domain (https://en.wikipedia.org/wiki/Public_domain).
Figure 8.8.4
US Navy 030513-N-1577S-001 Lt. Cmdr. Joe Casey, Ship's Anesthetist, trains on anesthetic procedures with Hospital Corpsman 3rd Class Eric Wichman aboard USS Nimitz (CVN 68) by U.S. Navy photo by Photographer’s Mate Airman Timothy F. Sosais on Wikimedia Commons is in the public domain (https://en.wikipedia.org/wiki/Public_domain).
Figure 8.8.5
Peyote Lophophora_williamsii_pm by Peter A. Mansfeld on Wikimedia Commons is used under a CC BY 3.0 (https://creativecommons.org/licenses/by/3.0/deed.en) license.
Figure 8.8.6
Cat under effects of catnip/Self Indulgence by Katieb50 on Flickr is used under a CC BY 2.0 (https://creativecommons.org/licenses/by/2.0/deed.en) license.
Alcoholics Anonymous World Services, Inc. (n.d.). Regional correspondent U.S. and Canada [website]. https://www.aa.org/pages/en_US/regional-correspondent-us-and-canada
Belzak, L., & Halverson, J. (2018). The opioid crisis in Canada: a national perspective. La crise des opioïdes au Canada : une perspective nationale. Health promotion and chronic disease prevention in Canada : research, policy and practice, 38(6), 224–233. https://doi.org/10.24095/hpcdp.38.6.02
British Columbia Regional Service Committee of Narcotics Anonymous. (n.d.). Welcome to the B.C. region of N.A. [website]. https://www.bcrna.ca/
Centers for Disease Control and Prevention (CDC). (2011 November 4). Vital signs: overdoses of prescription opioid pain relievers—United States, 1999–2008. Morbidity and Mortality Weekly Report (MMWR),60(43):1487-1492. https://www.cdc.gov/mmwr/preview/mmwrhtml/mm6043a4.htm
TED-Ed. (2017, June 29). How do drugs affect the brain? - Sara Garofalo. YouTube. https://www.youtube.com/watch?v=8qK0hxuXOC8&feature=youtu.be
TED-Ed. (2017, July 17). How does caffeine keep us awake? - Hanan Qasim. YouTube. https://www.youtube.com/watch?v=foLf5Bi9qXs&feature=youtu.be
TED-Ed. (2019, December 2). Is marijuana bad for your brain? - Anees Bahji. YouTube. https://www.youtube.com/watch?v=Nlcr1jd_Tok&feature=youtu.be
One of two main divisions of the nervous system that includes the brain and spinal cord.
Created by CK-12 Foundation/Adapted by Christine Miller

Case Study Conclusion: Trying to Conceive
The woman in Figure 18.12.1 is holding a home pregnancy test. The two pink lines in the middle are the type of result that Alicia and Victor are desperately hoping to see themselves one day — a positive pregnancy test. In the beginning of the chapter you learned that Alicia and Victor have been actively trying to get pregnant for a year, which, as you now know, is the time frame necessary for infertility to be diagnosed.
Alicia and Victor tried having sexual intercourse on day 14 of her menstrual cycle to optimize their chances of having his sperm meet her ovum. Why might this not be successful, even if they do not have fertility problems? Although the average menstrual cycle is 28 days, with ovulation occurring around day 14, many women vary widely from these averages (either consistently or variably) from month to month. Recall, for example, that menstrual cycles may vary from 21 to 45 days in length, and a woman’s cycle is considered to be regular if it varies within as many as eight days from shortest to longest cycle. This variability means that ovulation often does not occur on or around day 14, particularly if the woman has significantly shorter, longer, or irregular cycles — like Alicia does. Therefore, by aiming for day 14 without knowing when Alicia is actually ovulating, they may not be successful in helping Victor’s sperm encounter Alicia’s egg.
Lack of ovulation entirely can also cause variability in menstrual cycle length. As you have learned, the regulation of the menstrual cycle depends on an interplay of hormones from the pituitary gland and ovaries, including FSH and LH from the pituitary and estrogen and progesterone from the ovary — specifically from the follicle which surrounds the maturing egg and becomes the corpus luteum after ovulation. Shifts in these hormones and processes can affect ovulation and menstrual cycle length. This is why Alicia was concerned about her long and irregular menstrual cycles. If they are a sign that she is not ovulating, that could be the reason why she is having trouble getting pregnant.
In order to get a better idea of whether Alicia is ovulating, Dr. Bashir recommended that she take her basal body temperature (BBT) each morning before getting out of bed, and track it throughout her menstrual cycle. As you have learned, BBT typically rises slightly and stays high after ovulation. While tracking BBT is not a particularly effective form of contraception, since the temperature rise occurs only after ovulation, it can be a good way to see whether a woman is ovulating at all. Although not every woman will see a clear shift in BBT after ovulation, it is a relatively easy way to start assessing a woman’s fertility and is used as part of a more comprehensive fertility assessment by some physicians.
Dr. Bashir also recommended that Alicia use a home ovulation predictor kit. This is another relatively cheap and easy way to assess ovulation. Most ovulation predictor kits work by detecting the hormone LH in urine using test strips, like the ones shown in Figure 18.12.2. Why can this predict ovulation? Think about what you have learned about how ovulation is triggered. Rising levels of estrogen from the maturing follicle in the ovary causes a surge in the level of LH secreted from the pituitary gland, which triggers ovulation. This surge in LH can be detected by the home kit, which compares the level of LH in a woman’s urine to that of a control on the strip. After the LH surge is detected, ovulation will typically occur within one to two days.
By tracking her BBT and using the ovulation predictor kit, Alicia has learned that she is most likely ovulating, but not in every cycle, and sometimes she ovulates much later than day 14. Because frequent anovulatory cycles can be a sign of an underlying hormonal disorder, such as polycystic ovary syndrome (PCOS) or problems with the pituitary or other glands that regulate the reproductive system, Dr. Bashir orders blood tests for Alicia and sets up an appointment for a physical exam.
However, because Alicia is sometimes ovulating, the problem may not lie solely with her. Recall that infertility occurs in similar proportions in men and women, and can be due to problems in both partners. This is why it is generally recommended that both partners get assessed for fertility issues when they are having trouble getting pregnant after a year of trying.
Therefore, Victor proceeds with the semen analysis that Dr. Bashir recommended. In this process, the man provides a semen sample by ejaculating into a cup or special condom, and the semen is then examined under a microscope. The semen is then checked for sperm number, shape, and motility. Sperm with an abnormal shape or trouble moving will likely have trouble reaching and fertilizing an egg. A low number of sperm will also reduce the chances of conception. In this way, semen analysis can provide insight into the possible underlying causes of infertility. For instance, a low sperm count could indicate problems in sperm production or a blockage in the male reproductive tract that is preventing sperm from being emitted from the penis. Further testing would have to be done to distinguish between these two possible causes.
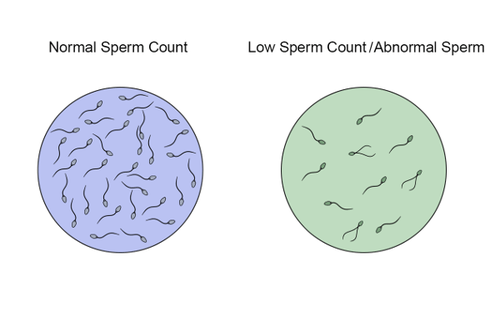
Victor had been worried that past injuries to his testes may have affected his fertility. You may remember the testes are where sperm are produced, and because they are external to the body, they are vulnerable to injury. In addition to physical damage to the testes and other parts of the male reproductive tract, a testicular injury could potentially cause the creation of antibodies against a man’s own sperm. As you have learned, Sertoli cells lining the seminiferous tubules are tightly packed so that the developing sperm are normally well-separated from the body’s immune system. However, in the case of an injury, this barrier can be breached, which can cause the creation of antisperm antibodies. These antibodies can hamper fertility by killing the sperm, or otherwise interfering with their ability to move or fertilize an egg. When infertility is due to such antibodies, it is called “immune infertility.”
Victor’s semen analysis shows that he has normal numbers of healthy sperm. Dr. Bashir recommends that while they investigate whether Alicia has an underlying medical issue, she continue to track her BBT and use ovulation predictor kits to try to pinpoint when she is ovulating. She recommends that once Alicia sees an LH surge, the couple try to have intercourse within three days to maximize their chances of conception. If Alicia is found to have a medical problem that is inhibiting ovulation, depending on what it is, they may either address the problem directly, or she can take medication that stimulates ovulation, such as clomiphene citrate (often sold under the brand name Clomid). This medication works by increasing the amount of FSH secreted by the pituitary.
Fortunately, tracking ovulation at home and timing intercourse appropriately was all Alicia and Victor needed to do to finally get pregnant! After their experience, they, like you, now have a much deeper understanding of the intricacies of the reproductive system and the complex biology that is involved in the making of a new human organism.
Chapter 18 Summary
In this chapter, you learned about the male and female reproductive systems. Specifically, you learned that:
- The reproductive system is the human organ system responsible for the production and fertilization of gametes and, in females, the carrying of a fetus.
- Both male and female reproductive systems have organs called gonads (testes in males, ovaries in females) that produce gametes (sperm or ova) and sex hormones (such as testosterone in males and estrogen in females). Sex hormones are endocrine hormones that control prenatal development of sex organs, sexual maturation at puberty, and reproduction after puberty.
- The reproductive system is the only organ system that is significantly different between males and females. A Y-chromosome gene called SRY is responsible for undifferentiated embryonic tissues developing into a male reproductive system. Without a Y chromosome, the undifferentiated embryonic tissues develop into a female reproductive system.
- Male and female reproductive systems are different at birth, but immature and nonfunctioning. Maturation of the reproductive system occurs during puberty when hormones from the hypothalamus and pituitary gland stimulate the gonads to produce sex hormones again. The sex hormones, in turn, cause the physical changes experienced during puberty.
- Male reproductive system organs include the testes, epididymis, penis, vas deferens, prostate gland, and seminal vesicles.
-
- The two testes are sperm- and testosterone-producing male gonads. They are contained within the scrotum, a pouch that hangs down behind the penis. The testes are filled with hundreds of tiny, tightly coiled seminiferous tubules, where sperm are produced. The tubules contain sperm in different stages of development, as well as Sertoli cells, which secrete substances needed for sperm production. Between the tubules are Leydig cells, which secrete testosterone.
- The two epididymides are contained within the scrotum. Each epididymis is a tightly coiled tubule where sperm mature and are stored until they leave the body during an ejaculation.
- The two vas deferens are long, thin tubes that run from the scrotum up into the pelvic cavity. During ejaculation, each vas deferens carries sperm from one of the epididymides to one of the pair of ejaculatory ducts.
- The two seminal vesicles are glands within the pelvis that secrete fluid through ducts into the junction of each vas deferens and ejaculatory duct. This alkaline fluid makes up about 70% of semen, the sperm-containing fluid that leaves the penis during ejaculation. Semen contains substances and nutrients that sperm need to survive and “swim” in the female reproductive tract.
- The prostate gland is located just below the seminal vesicles and surrounds the urethra and its junction with the ejaculatory ducts. The prostate secretes an alkaline fluid that makes up close to 30% of semen. Prostate fluid contains a high concentration of zinc, which sperm need to be healthy and motile.
- The ejaculatory ducts form where the vas deferens joins with the ducts of the seminal vesicles in the prostate gland. They connect the vas deferens with the urethra. The ejaculatory ducts carry sperm from the vas deferens, and secretions from the seminal vesicles and prostate gland that together form semen.
- The paired bulbourethral glands are located just below the prostate gland. They secrete a tiny amount of fluid into semen. The secretions help lubricate the urethra and neutralize any acidic urine it may contain.
- The penis is the external male organ that has the reproductive function of intromission, which is delivering sperm to the female reproductive tract. The penis also serves as the organ that excretes urine. The urethra passes through the penis and carries urine or semen out of the body. Internally, the penis consists largely of columns of spongy tissue that can fill with blood and make the penis stiff and erect. This is necessary for sexual intercourse so intromission can occur.
- Parts of a mature sperm include the head, acrosome, midpiece, and flagellum. The process of producing sperm is called spermatogenesis. This normally starts during puberty and continues uninterrupted until death.
-
- Spermatogenesis occurs in the seminiferous tubules in the testes, and requires high concentrations of testosterone. Sertoli cells in the testes play many roles in spermatogenesis, including concentrating testosterone under the influence of follicle stimulating hormone (FSH) from the pituitary gland.
- Spermatogenesis begins with a diploid stem cell called a spermatogonium, which undergoes mitosis to produce a primary spermatocyte. The primary spermatocyte undergoes meiosis I to produce haploid secondary spermatocytes, and these cells in turn, undergo meiosis II to produce spermatids. After the spermatids grow a tail and undergo other changes, they become sperm.
- Before sperm are able to “swim,” they must mature in the epididymis. The mature sperm are then stored in the epididymis until ejaculation occurs.
- Ejaculation is the process in which semen is propelled by peristalsis in the vas deferens and ejaculatory ducts from the urethra in the penis.
- Leydig cells in the testes secrete testosterone under the control of luteinizing hormone (LH) from the pituitary gland. Testosterone is needed for male sexual development at puberty and to maintain normal spermatogenesis after puberty. It also plays a role in prostate function and the ability of the penis to become erect.
- Disorders of the male reproductive system include erectile dysfunction (ED), epididymitis, prostate cancer, and testicular cancer.
-
- ED is a disorder characterized by the regular and repeated inability of a sexually mature male to obtain and maintain an erection. ED is a common disorder that occurs when normal blood flow to the penis is disturbed or there are problems with the nervous control of penile engorgement or arousal.
-
-
- Possible physiological causes of ED include aging, illness, drug use, tobacco smoking, and obesity, among others. Possible psychological causes of ED include stress, performance anxiety, and mental disorders.
- Treatments for ED may include lifestyle changes, such as stopping smoking and adopting a healthier diet and regular exercise. However, the first-line treatment is prescription drugs such as Viagra® or Cialis® that increase blood flow to the penis. Vacuum pumps or penile implants may be used to treat ED if other types of treatment fail.
- Epididymitis is inflammation of the epididymis. It is a common disorder, especially in young men. It may be acute or chronic and is often caused by a bacterial infection. Treatments may include antibiotics, anti-inflammatory drugs, and painkillers. Treatment is important to prevent the possible spread of infection, permanent damage to the epididymis or testes, and even infertility.
- Prostate cancer is the most common type of cancer in men and the second leading cause of cancer death in men. If there are symptoms, they typically involve urination, such as frequent or painful urination. Risk factors for prostate cancer include older age, family history, a high-meat diet, and sedentary lifestyle, among others.
-
-
-
- Prostate cancer may be detected by a physical exam or a high level of prostate-specific antigen (PSA) in the blood, but a biopsy is required for a definitive diagnosis. Prostate cancer is typically diagnosed relatively late in life, and is usually slow growing, so no treatment may be necessary. In younger patients or those with faster-growing tumors, treatment is likely to include surgery to remove the prostate, followed by chemotherapy and/or radiation therapy.
- Testicular cancer, or cancer of the testes, is the most common cancer in males between the ages of 20 and 39 years. It is more common in males of European than African ancestry. A lump or swelling in one testis, fluid in the scrotum, and testicular pain or tenderness are possible signs and symptoms of testicular cancer.
-
-
-
- Testicular cancer can be diagnosed by a physical exam and diagnostic tests, such as ultrasound or blood tests. Testicular cancer has one of the highest cure rates of all cancers. It is typically treated with surgery to remove the affected testis, and this may be followed by radiation therapy, and/or chemotherapy. Normal male reproductive functions are still possible after one testis is removed, if the remaining testis is healthy.
-
- The female reproductive system is made up of internal and external organs that function to produce haploid female gametes called ova, secrete female sex hormones (such as estrogen), and carry and give birth to a fetus.
- Female reproductive system organs include the ovaries, oviducts, uterus, vagina, clitoris, and labia.
-
- The vagina is an elastic, muscular canal that can accommodate the penis. It is where sperm are usually ejaculated during sexual intercourse. The vagina is also the birth canal, and it channels the flow of menstrual blood from the uterus. A healthy vagina has a balance of symbiotic bacteria and an acidic pH.
- The uterus is a muscular organ above the vagina where a fetus develops. Its muscular walls contract to push out the fetus during childbirth. The cervix is the neck of the uterus that extends down into the vagina. It contains a canal connecting the vagina and uterus for sperm or an infant to pass through. The innermost layer of the uterus, the endometrium, thickens each month in preparation for an embryo but is shed in the following menstrual period if fertilization does not occur.
- The oviducts extend from the uterus to the ovaries. Waving fimbriae at the ovary ends of the oviducts guide ovulated ova into the tubes where fertilization may occur as the ova travel to the uterus. Cilia and peristalsis help eggs move through the tubes. Tubular fluid helps nourish sperm as they swim up the tubes toward eggs.
- The ovaries are gonads that produce eggs and secrete sex hormones including estrogen. Nests of cells called follicles in the ovarian cortex are the functional units of ovaries. Each follicle surrounds an immature ovum. At birth, a baby girl’s ovaries contain at least a million eggs, and they will not produce any more during her lifetime. One egg matures and is typically ovulated each month during a woman’s reproductive years.
- The vulva is a general term for external female reproductive organs. The vulva includes the clitoris, two pairs of labia, and openings for the urethra and vagina. Secretions from Bartholin’s glands near the vaginal opening lubricate the vulva.
- The breasts are technically not reproductive organs, but their mammary glands produce milk to feed an infant after birth. Milk drains through ducts and sacs and out through the nipple when a baby sucks.
- Oogenesis is the process of producing eggs in the ovaries of a female fetus. Oogenesis begins when a diploid oogonium divides by mitosis to produce a diploid primary oocyte. The primary oocyte begins meiosis I and then remains at this stage in an immature ovarian follicle until after birth.
- After puberty, one follicle a month matures and its primary oocyte completes meiosis I to produce a secondary oocyte, which begins meiosis II. During ovulation, the mature follicle bursts open and the secondary oocyte leaves the ovary and enters a oviducts.
- While a follicle is maturing in an ovary each month, the endometrium in the uterus is building up to prepare for an embryo. Around the time of ovulation, cervical mucus becomes thinner and more alkaline to help sperm reach the secondary oocyte.
- If the secondary oocyte is fertilized by a sperm, it quickly completes meiosis II and forms a diploid zygote, which will continue through the oviducts. The zygote will go through multiple cell divisions before reaching and implanting in the uterus. If the secondary oocyte is not fertilized, it will not complete meiosis II, and will soon disintegrate.
- Pregnancy is the carrying of one or more offspring from fertilization until birth. The maternal organism must provide all the nutrients and other substances needed by the developing offspring, and also remove its wastes. She should also avoid exposures that could potentially damage the offspring, especially early in the pregnancy when organ systems are developing.
-
- The average duration of pregnancy is 40 weeks (from the first day of the last menstrual period) and is divided into three trimesters of about three months each. Each trimester is associated with certain events and conditions that a pregnant woman may expect, such as morning sickness during the first trimester, feeling fetal movements for the first time during the second trimester, and rapid weight gain in both fetus and mother during the third trimester.
- Labour, which is the general term for the birth process, usually begins around the time the amniotic sac breaks and its fluid leaks out. Labour occurs in three stages: dilation of the cervix, birth of the baby, and delivery of the placenta (afterbirth).
- The physiological function of female breasts is lactation, or the production of breast milk to feed an infant. Sucking on the breast by the infant stimulates the release of the hypothalamic hormone oxytocin from the posterior pituitary, which causes the flow of milk. The release of milk stimulates the baby to continue sucking, which in turn keeps the milk flowing. This is one of the few examples of positive feedback in the human organism.
- The ovaries produce female sex hormones, including estrogen and progesterone. Estrogen is responsible for sexual maturation and secondary sex characteristics at puberty. It is also needed to help regulate the menstrual cycle and ovulation after puberty until menopause. Progesterone prepares the uterus for pregnancy each month during the menstrual cycle, and helps maintain the pregnancy if fertilization occurs.
- The menstrual cycle refers to natural changes that occur in the female reproductive system each month during the reproductive years, except when a woman is pregnant. The cycle is necessary for the production of ova and the preparation of the uterus for pregnancy. It involves changes in both the ovaries and uterus and is controlled by pituitary hormones (FSH and LH) and ovarian hormones (estrogen and progesterone).
-
- The female reproductive period is delineated by menarche, or the first menstrual period, which usually occurs around age 12 or 13; and by menopause, or the cessation of menstrual periods, which typically occurs around age 52. A typical menstrual cycle averages 28 days in length but may vary normally from 21 to 45 days. The average menstrual period is five days long, but may vary normally from two to seven days. These variations in the menstrual cycle may occur both between women and within individual women from month to month.
- The events of the menstrual cycle that take place in the ovaries make up the ovarian cycle. It includes the follicular phase, when a follicle and its ovum mature due to rising levels of FSH; ovulation, when the ovum is released from the ovary due to a rise in estrogen and a surge in LH; and the luteal phase, when the follicle is transformed into a structure called a corpus luteum that secretes progesterone. In a 28-day menstrual cycle, the follicular and luteal phases typically average about two weeks in length, with ovulation generally occurring around day 14 of the cycle.
- The events of the menstrual cycle that take place in the uterus make up the uterine cycle. It includes menstruation, which generally occurs on days 1 to 5 of the cycle and involves shedding of endometrial tissue that built up during the preceding cycle; the proliferative phase, during which the endometrium builds up again until ovulation occurs; and the secretory phase, which follows ovulation and during which the endometrium secretes substances and undergoes other changes that prepare it to receive an embryo.
- Disorders of the female reproductive system include cervical cancer, vaginitis, and endometriosis.
-
- Cervical cancer occurs when cells of the cervix grow abnormally and develop the ability to invade nearby tissues, or spread to other parts of the body. Worldwide, cervical cancer is the second-most common type of cancer in females and the fourth-most common cause of cancer death in females. Early on, cervical cancer often has no symptoms; later, symptoms such as abnormal vaginal bleeding and pain are likely.
-
-
- Most cases of cervical cancer occur because of infection with human papillomavirus (HPV), so the HPV vaccine is expected to greatly reduce the incidence of the disease. Other risk factors include smoking and a weakened immune system. A Pap smear can diagnose cervical cancer at an early stage. Where Pap smears are done routinely, cervical cancer death rates have fallen dramatically. Treatment of cervical cancer generally includes surgery, which may be followed by radiation therapy or chemotherapy.
- Vaginitis is inflammation of the vagina. A discharge is likely, and there may be itching and pain. About 90% of cases of vaginitis are caused by infection with microorganisms, typically by the yeast Candida albicans. A minority of cases are caused by irritants or allergens in products such as soaps, spermicides, or douches.
-
-
-
- Diagnosis of vaginitis may be based on characteristics of the discharge, which can be examined microscopically or cultured. Treatment of vaginitis depends on the cause, and is usually an oral or topical anti-fungal or antibiotic medication.
- Endometriosis is a disease in which endometrial tissue grows outside the uterus. This tissue may bleed during the menstrual period and cause inflammation, pain, and scarring. The main symptom of endometriosis is pelvic pain, which may be severe. Endometriosis may also lead to infertility.
-
-
-
- Endometriosis is thought to have multiple causes, including genetic mutations. Retrograde menstruation may be the immediate cause of endometrial tissue escaping the uterus and entering the pelvic cavity. Endometriosis is usually treated with surgery to remove the abnormal tissue and medication for pain. If surgery is more conservative than hysterectomy, endometriosis may recur.
-
- Infertility is the inability of a sexually mature adult to reproduce by natural means. It is defined scientifically and medically as the failure to achieve a successful pregnancy after at least one year of regular, unprotected sexual intercourse.
- About 40% of infertility in couples is due to female infertility, and another 30% is due to male infertility. In the remaining cases, a couple’s infertility is due to problems in both partners or to unknown causes.
- Male infertility occurs when there are no or too few healthy, motile sperm. This may be caused by problems with spermatogenesis or by blockage of the male reproductive tract that prevents sperm from being ejaculated. Risk factors for male infertility include heavy alcohol use, smoking, certain medications, and advancing age, to name just a few.
- Female infertility occurs due to failure to produce viable ova by the ovaries or structural problems in the oviducts or uterus. Polycystic ovary syndrome is the most common cause of failure to produce viable eggs. Endometriosis and uterine fibroids are possible causes of structural problems in the oviducts and uterus. Risk factors for female infertility include smoking, stress, poor diet, and older age, among others.
- Diagnosing the cause(s) of a couple’s infertility generally requires testing both the man and the woman for potential problems. For men, semen is likely to be examined for adequate numbers of healthy, motile sperm. For women, signs of ovulation are monitored, for example, with an ovulation test kit or ultrasound of the ovaries. For both partners, the reproductive tract may be medically imaged to look for blockages or other abnormalities.
-
- Treatments for infertility depend on the cause. For example, if a medical problem is interfering with sperm production, medication may resolve the underlying problem so sperm production is restored. Blockages in either the male or the female reproductive tract can often be treated surgically. If there are problems with ovulation, hormonal treatments may stimulate ovulation.
- Some cases of infertility are treated with assisted reproductive technology (ART). This is a collection of medical procedures in which eggs and sperm are taken from the couple and manipulated in a lab to increase the chances of fertilization occurring and an embryo forming. Other approaches for certain causes of infertility include the use of a surrogate mother, gestational carrier, or sperm donation.
- Infertility can negatively impact a couple socially and psychologically, and it may be a major cause of marital friction or even divorce. Infertility treatments may raise ethical issues relating to the costs of the procedures and the status of embryos that are created in vitro but not used for pregnancy. Infertility is an under-appreciated problem in developing countries where birth rates are high and children have high economic as well as social value. In these countries, poor health care is likely to lead to more problems with infertility and fewer options for treatment.
- More than half of all fertile couples worldwide use contraception (birth control), which is any method or device used to prevent pregnancy. Different methods of contraception vary in their effectiveness, typically expressed as the failure rate, or the percentage of women who become pregnant using a given method during the first year of use. For most methods, the failure rate with typical use is much higher than the failure rate with perfect use.
- Types of birth control methods include barrier methods, hormonal methods, intrauterine devices, behavioural methods, and sterilization. Except for sterilization, all of the methods are reversible.
-
- Barrier methods are devices that block sperm from entering the uterus. They include condoms and diaphragms. Of all birth control methods, only condoms can also prevent the spread of sexually transmitted infections.
- Hormonal methods involve the administration of hormones to prevent ovulation. Hormones can be administered in various ways, such as in an injection, through a skin patch, or, most commonly, in birth control pills. There are two types of birth control pills: those that contain estrogen and progesterone, and those that contain only progesterone. Both types are equally effective, but they have different potential side effects.
- An intrauterine device (IUD) is a small T-shaped plastic structure containing copper or a hormone that is inserted into the uterus by a physician and left in place for months or even years. It is highly effective even with typical use, but it does have some risks, such as increased menstrual bleeding and, rarely, perforation of the uterus.
- Behavioural methods involve regulating the timing or method of intercourse to prevent introduction of sperm into the female reproductive tract, either altogether or when an egg may be present. In fertility awareness methods, unprotected intercourse is avoided during the most fertile days of the cycle as estimated by basal body temperature or the characteristics of cervical mucus. In withdrawal, the penis is withdrawn from the vagina before ejaculation occurs. Behavioural methods are the least effective methods of contraception.
- Sterilization is the most effective contraceptive method, but it requires a surgical procedure and may be irreversible. Male sterility is usually achieved with a vasectomy, in which the vas deferens are clamped or cut to prevent sperm from being ejaculated in semen. Female sterility is usually achieved with a tubal ligation, in which the oviducts are clamped or cut to prevent sperm from reaching and fertilizing eggs.
- Emergency contraception is any form of contraception that is used after unprotected vaginal intercourse. One method is the “morning after” pill, which is a high-dose birth control pill that can be taken up to five days after unprotected sex. Another method is an IUD, which can be inserted up to five days after unprotected sex.
In this chapter, you learned how the male and female reproductive systems work together to produce a zygote. In the next chapter, you will learn about how the human organism grows and develops throughout life — from a zygote all the way through old age.
Chapter 18 Review
-
- Which glands produce the non-sperm fluids that make up semen? What is the rough percentage of each fluid in semen?
- What is one reason why semen's alkalinity assists in reproduction?
- What are three things that pass through the cervical canal of females, going in either direction?
- Other than where the cancer originates, what is one difference between prostate and testicular cancer?
- If a woman is checking her basal body temperature each morning as a form of contraception, and today is day 12 of her menstrual cycle and her basal body temperature is still low, is it safe for her to have unprotected sexual intercourse today? Why or why not?
-
- Where is a diaphragm placed? How does it work to prevent pregnancy?
- Why are the testes located outside of the body?
- Why is it important to properly diagnose the causative agent when a woman has vaginitis?
- Describe two ways in which sperm can move through the male and/or female reproductive tracts.
Attributions
Figure 18.12.1
Pregnancy test/ Dos rayitas by Esparta Palma on Flickr is used under a CC BY 2.0 (https://creativecommons.org/licenses/by/2.0/) license.
Figure 18.12.2
1024px-Ovulatietest by Sapp on Wikimedia Commons is in the public domain (https://en.wikipedia.org/wiki/Public_domain).
Figure 18.12.3
Sperm Count by CK-12 Foundation is used under a CC BY-NC 3.0 (https://creativecommons.org/licenses/by-nc/3.0/) license.
References
Brainard, J/ CK-12 Foundation. (2016). Figure 3 Normal vs. low sperm count [digital image]. In CK-12 College Human Biology (Section 20.12) [online Flexbook]. CK12.org. https://www.ck12.org/book/ck-12-college-human-biology/section/20.12/
Image shows a burger, with the beef patty, an eff, slices of ham, and two slices of melted cheese. The burger is so packed with fillings and toppings that it needs a wooden stick in it to keep it from falling over.
A nervous system cell that provides support for neurons and helps them transmit nerve impulses.
As per caption
Image shows a diagram of the heart, with a blockage of one of the major coronary arteries. The blockage is cause by a plaque and a blood clot which was unable to pass through the artery narrowed by the plaque.
The central part of a neuron that contains the nucleus and other cell organelles.
An extension of the cell body of a neuron that receives nerve impulses from other neurons. A neuron will have several dendrites extending from the cell body.
A central organelle containing hereditary material.
Image shows a leg affect by PAD. Plaques in the leg arteries have caused reduced blood flow to the leg.
Image shows a blood pressure monitor meant to be worn on the wrist. It displays systolic and diastolic blood pressure, pulse and the date and time.


