Reading: Regulation and Policy Making
Disparities within the US Healthcare System and Policy Making
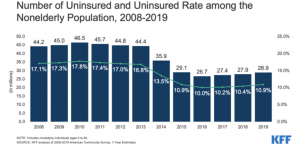
he rates of uninsured Americans reached a low in 2016 and has been increasing in the following years amid changes in the availability and affordability of coverage under the Patient Protection and Affordable Care Act (ACA), as shown in Figure 2.
Figure 2. Uninsured Rate Among the Nonelderly Population, 2008-2019 (Source: Key Facts About the Uninsured Population. Kaiser Family Foundation)
Regulation and Policymaking
Federal healthcare laws are enacted and amended through Congress, the legislative branch of government. Policy can also be changed through the regulatory process, whereby the federal branch of the government interprets how policies are to be implemented and enforced. In the United States, the Department of Health and Human Services (HHS) is responsible for the provision of medicine, public health services, and social services at the national level. The HHS is part of the federal branch of government and is the oversight agency for healthcare organizations in the country such as the Food and Drug Administration (FDA), Centers for Medicare and Medicaid Services (CMS), National Institutes of Health (NIH), Agency for Healthcare Research and Quality (AHRQ), and Centers for Disease Control and Prevention (CDC). For more information on these healthcare decision makers, see here. In addition to federal healthcare laws, states may pass additional laws, as long as federal law is not contradicted.
Recent National Legislation
The 21st Century Cures Act was signed into law on December 13, 2016 and laid out changes to the FDA’s drug and device approval processes, with the goal of incorporating patient perspective into drug and device development and expediting the development and review of novel medical products. This legislation calls for the incorporation of “data summaries” and real-world evidence into the drug approval process and laid the groundwork for preapproval communication of appropriate healthcare economic information (HCEI) to expedite the formulary decision-making process after FDA approval. Also, the Regenerative Medicine Advanced Therapy and Breakthrough Devices Program was established as a new expedited product development program.
On March 23, 2010 the ACA, often referred to as “Obamacare,” was passed by Congress. This sweeping overhaul of the healthcare system represents the largest change and expansion of coverage since the passing of Medicare and Medicaid in 1965.
The ACA, in its original format, was an attempt to increase healthcare coverage for American citizens and involved the expansion of coverage provisions related to access and quality of care, summarized below.13,14
- Expansion of Public Programs
- The ACA provides the expansion of Medicaid to individuals with incomes up to 138% of the federal poverty level and eliminates the limitations that prohibited most adults without dependent children from enrolling. Increased federal funding for state Medicaid programs was used as an incentive for states to expand their Medicaid access. As of November 2, 2020, 38 states and Washington, DC have expanded Medicaid access.
- Establishment of the American Health Benefit Exchanges
- A health insurance marketplace, also known as the “exchange” or “marketplace,” is where individuals and small employers are able to purchase private insurance. Consumers are provided information to enable them to choose among plans that meet their health and financial needs.
- These Health Insurance Marketplace plans are required to meet a minimum set of coverage standards, also known as “essential health benefits.”
- Essential health benefits include: ambulatory patient services; emergency services; hospitalization; pregnancy, maternity, and newborn care; mental health and substance use disorder services; prescription drugs; rehabilitative and habilitative services and devices; laboratory services; pediatric services (including oral and vision care); total birth control coverage; and breastfeeding coverage.
- Premium tax credits and cost-sharing reduction subsidies (CSR) are also available to make plans available on the exchanges more affordable for those who qualify.
- Changes to Private Insurance
- New regulations prevent health insurers from denying coverage to people for any reason, including pre-existing health conditions and charging people more based on health status and gender.
- Young adults can remain on their parents’ health insurance up to age 26.
- Health insurers are prohibited from imposing lifetime limits on coverage and are prohibited from rescinding coverage.
- $0 copayments are available on many preventative health services.
- The Individual Mandate
- All individuals were required to have health insurance, with few exceptions, beginning in 2014. Those who did not have coverage were required to pay a yearly financial penalty.
- In late 2017, the federal individual mandate was repealed in a tax bill passed by Congress and signed by the Trump administration.
- Employer Requirements for Health Coverage
- Employers with more than 50 employees are assessed a fee of $2000 per full-time employee if they do not offer coverage and they have at least one employee who receives a premium credit through an Exchange.

