Reading: HealthCare Costs in the US
Understanding HealthCare Statistics
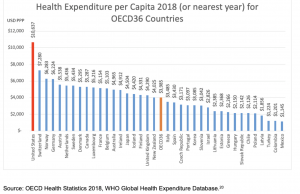
The United States is the third most populous country in the world, behind China and India, but has a population that is only about one-quarter of either of those 2 countries. Nevertheless, it spent $3.5 trillion on healthcare, or 16.9% of the gross domestic product (GDP), (more than any other country) in 2018.19,20 Comparable healthcare spending estimates include Switzerland (12.2%), the second-highest country, as well as Germany (11.2%) and the United Kingdom (UK) (9.8%).20 Figure 3, below, illustrates the per capita spend of the United States on healthcare relative to other developed nations.
Figure 3. Health Expenditure per Capita for 2017 in the Organization for Economic Cooperation and Development (OECD) 36 Countries
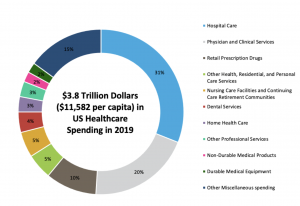
In the United States, hospital care is the main driver of overall healthcare spending, accounting for 33% of 2017 healthcare dollars, physician and clinical services are second at 20%, and prescription drugs are third at 10%. See Figure 4 below for a more complete breakdown of total healthcare spending in the United States.
Figure 4. 2017 Healthcare Spending by Type of Service or Product in the United States
Decision Makers and Influencers
Regulators and Policymakers
The US Department of Health and Human Services (HHS is responsible for protecting the health and providing essential human services for all Americans. Several agencies function under HHS, see below. HHS and state-level departments of health are responsible for developing and supervising the implementation of health policies, as well as managing a large part of healthcare expenditure via CMS. However, there is no strict target for federal- or state-wide healthcare expenditure.
Agency for Healthcare Research and Quality (AHRQ): The AHRQ’s mission is to produce evidence to make healthcare safer, of higher quality, more accessible, equitable, and affordable, and to work within HHS and with other partners to make sure that the evidence is understood and used.
Centers for Disease Control and Prevention (CDC): The CDC, part of the Public Health Service, protects the public health of the nation by providing leadership and direction for the prevention and control of diseases and other preventable conditions and responding to public health emergencies.
National Institutes of Health (NIH): The NIH, part of the Public Health Service, supports biomedical and behavioral research within the United States and abroad, conducts research in its own laboratories and clinics, trains promising young researchers, and promotes collecting and sharing medical knowledge.
Office of Inspector General (OIG): OIG protects the integrity of HHS programs as well as the health and welfare of the program participants.
The US Food and Drug Administration (FDA): The FDA, part of the Public Health Service, ensures that food is safe, pure, and wholesome; human and animal drugs, biological products, and medical devices are safe and effective; and electronic products that emit radiation are safe. In addition, FDA oversees regulatory approval of drugs, biologics, diagnostics, and devices in the United States.
Center for Drug Evaluation and Research (CDER): CDER performs an essential public health task by making sure that safe and effective drugs are available to improve the health of people in the United States. As part of the FDA, CDER regulates over-the-counter and prescription drugs, including generic drugs. This covers more than just pharmaceuticals. For example, fluoride toothpaste, antiperspirants, dandruff shampoos, and sunscreens are all considered “drugs.”
Center for Biologics Evaluation and Research (CBER): CBER is the center within FDA that regulates biological products for human use under applicable federal laws. CBER protects and advances the public health by ensuring that biological products are safe and effective and available to those who need them. CBER also provides the public with information to promote the safe and appropriate use of biological products.
Center for Devices and Radiological Health (CDRH): CDRH ensures that patients and providers have timely and continued access to safe, effective, and high-quality medical devices and safe radiation-emitting products. CDRH facilitates medical device innovation by advancing regulatory science, providing industry with predictable, consistent, transparent, and efficient regulatory pathways, and assuring consumer confidence in devices marketed in the United States. The CDRH also oversees the Office of In Vitro Diagnostics and Radiological Health (OIR).
Payers
Centers for Medicare & Medicaid Services (CMS): CMS represents the public health insurance provider for around 30% of Americans and combines the oversight of the Medicare program, the federal portion of the Medicaid program and CHIP, the Health Insurance Marketplace, and related quality assurance activities.
Medicare: Medicare is a single-payer national health insurance program that began in 1966. Funding for this program comes from payroll taxes, premiums and surtaxes from beneficiaries, and general federal revenue. It primarily provides health insurance to Americans aged 65 and older who have paid into the Social Security system through payroll taxes. (for more information see The Facts on Medicare Spending and Financing under Suggested Reading) Additional health insurance coverage through Medicare is provided to younger people with some disability, patients with amyotrophic lateral sclerosis, or patients with renal failure requiring dialysis or transplant. Coverage for Medicare is broken down into 4 parts, A through D. Traditional Medicare plans (A, B, and D) do not contain an out-of-pocket spending limit.
Part A: Medicare Part A coverage relates to inpatient hospital costs, skilled nursing, and hospice services.
Part B: Medicare Part B coverage relates to outpatient physician services. Durable medical equipment (DME), such as diabetic testing supplies, is covered under these plans. Some drugs also may be covered under Medicare Part B and are usually treatments that require the intervention of a physician to administer, such as chemotherapy, immunosuppressant drugs, and dialysis drugs.
Part C: Also known as a Medicare Advantage (MA) Plan, Medicare Supplement Plans, or Medigap, Part C coverage is an alternative to traditional Medicare that allows patients to choose private plans with at least the same benefits of Parts A and B, and often D (as a Medicare Advantage Prescription Drug [MAPD] plan). These plans provide an annual out-of-pocket spending limit, which traditional Parts A and B plans do not contain.
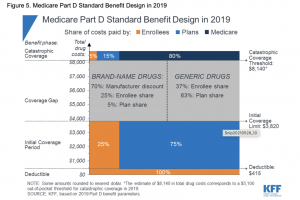
Part D: Medicare Part D coverage relates to prescription drug coverage. This coverage has a standard benefit design for all patients. See Figure 5 below for a breakdown of costs for Medicare Part D plans in 2019
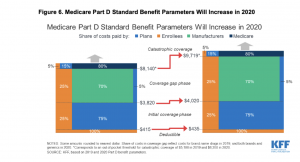
These benefits will increase in 2020 to:
Medicaid: Medicaid is a joint federal and state program that provides healthcare coverage for patients with limited income and resources. It is the largest source of funding for medical and health-related services for people with low income in the United States. It is jointly funded by the state and federal governments and managed by individual states, who determine eligibility. Recipients must be US citizens or legal permanent residents and may include low-income adults, their children, and people with certain disabilities. Poverty alone does not necessarily qualify a person for Medicaid.
State Children’s Health Insurance Program (CHIP): CHIP provides low-cost health coverage to children in families that earn too much to qualify for Medicaid. In some states, CHIP covers pregnant women as well. It is a jointly federal and state-funded program where individual states determine exact coverage rules; however, all states are required to provide basic comprehensive coverage including prescriptions and doctor visits. Routine visits are free under CHIP but there may be copayments for other services. Some states charge monthly premiums for CHIP coverage, but those will not be more than 5% of the family’s annual income
Veterans Health Administration (VHA): The VHA is a federal healthcare entity funded by the Department of Veterans Affairs (VA). Around 1700 hospitals, outpatient clinics, counseling centers, and long-term care facilities provide care to active and discharged individuals from the armed forces. Although many individuals are eligible, demand exceeds capacity, so a priority system has been developed to provide care to those most in need. The VA health system is owned and operated by the federal government. 23
Military Health System (MHS): The MHS is a federal healthcare entity funded by the Department of Defense. This integrated healthcare system provides medical care in combat situations, overseas bases, and in the United States to active military and dependents. MHS, unlike the VA, is not a completely federally funded system and relies on a government insurance plan, TRICARE, which is managed by the Defense Health Agency. 23
Managed Care Organizations (MCOs): MCOs operationalize health insurance for their enrollees by providing a complete healthcare delivery system consisting of affiliated and/or owned hospitals, physicians, and other providers that provide a wide range of coordinated health services. These health organizations contract with insurers, or self-insured employers, to deliver healthcare.
Health Maintenance Organizations (HMOs): In this healthcare plan model, patients tend to have lower monthly premiums and “in-network” restrictions on primary care physicians. Sometimes, patients are required to select a single primary care physician for treatment. Specialists require referrals from the primary care provider and out-of-network services are not covered. Premiums and deductibles are often lower when compared to preferred provider organizations.
Preferred Provider Organizations (PPO): These health plans have a preferred network of providers but will still cover out-of-network care. Patients can see specialists without a referral from a primary care physician visit. Because these plans are less restrictive, patients tend to have higher monthly premiums and cost-sharing. These plans have lost some popularity due to efforts to control costs. Premiums and deductibles are often higher when compared to HMOs.
Tiered-Network Plans (TNP): Tiered networks can be considered a hybrid plan that combines the physician networks of an HMO and the expanded network options of a PPO. With a tiered network, members pay lower out-of-pocket costs when they visit a preferred tier provider. Patients can visit nonpreferred physicians for healthcare but will pay more out of pocket. Even if a patient visits a nonpreferred physician, the incurred out-of-pocket costs go towards the out-of-pocket limits established by the ACA.
Integrated Delivery Networks (IDN): IDNs utilize vertical integration of healthcare to deliver the full range of healthcare services to its patients. The major distinction of an IDN is that the healthcare providers covered by the health plan are also employees of the health plan, rather than contracted physician networks. When patients receive care in the outpatient, specialist, and inpatient settings, they will utilize services owned and provided by the health plan executor. Kaiser Permanente, on the West Coast of the United States, is a good example of this type of healthcare delivery system. 24
Pharmacy Benefit Managers (PBM): PBMs design, implement, and manage pharmacy benefits and coverage. Health plans and self-insured employers often partner up with PBMs and let the latter manage pharmacy-related insurance responsibilities.
Self-Insured Employers: In addition to the private health plan organizations listed above, many employers will choose to self-insure and fund their own healthcare plans for their employees. In this scenario, employers will contract with healthcare providers to administer their health plans but have full control of coverage options and total responsibility for costs. These self-insured employers are able to offer health plans tailored to their insured population and can serve as a cost-containment method. There is the risk, however, of high-cost individuals driving up overall costs to the employer, who maintains full responsibility for payment.
Third-Party Organizations
Academy of Managed Care Pharmacy (AMCP): A leading professional association dedicated to increasing patient access for affordable medicines, improving health outcomes, and ensuring the wise use of healthcare dollars. Members include practitioners who manage medication therapies served by health plans, PBM firms, emerging care models, and government.
Institute of Clinical and Economic Review (ICER): Since 2006, ICER has been an independent research organization that objectively evaluates the clinical and economic value of prescription drugs, medical tests, and other healthcare delivery innovations. ICER is best known as an independent pricing watchdog for the United States. Each drug report contains an analysis of economic value to establish a “value-based price benchmark” and recommends how drugs should be priced to reflect long-term patient outcomes and short-term budget impact appropriately.
Healthcare Provider Groups
Accountable Care Organizations (ACO): Groups of healthcare providers that agree to coordinate care and to be held accountable for the quality and costs of the services they provide. This is a shared risk and shared savings program. Medicare and Medicaid ACOs’ goals are to make sure patients get the right care at the right time, in order to avoid unnecessary duplication of services and preventing medical errors.
Patient-Centered Medical Home (PCMH): A care delivery model whereby patients’ treatment is coordinated through their primary care physicians. The objective is to have a centralized setting that facilitates partnerships between individual patients and their personal physicians. Care is facilitated by registries, information technology, and health information exchange to ensure that patients get the indicated care when and where they need and want it in an appropriate manner.
Pharmacy and Therapeutics Committee (P&T): Develops and manages the formulary systems used in many different settings, ie, hospitals, long-term care facilities, Medicare, Medicaid, insurance companies, and managed care organizations. It acts as the liaison between pharmacy and medical staff in terms of coverage decisions for therapies that are effective, safe, and cost-effective for their particular facility or insurance plans.
Value Analysis Committee: Similar to a P&T Committee, these groups focus on the management of medical diagnostics and devices in a health system. Additionally, these groups also assess the value of certain clinical services to ensure the cost-effective provision of care.

