4.9: SYNDEMICS AND THE ECOLOGICAL MODEL
It is important to recognize that disease risk is not spread evenly within or between populations. Diseases also combine and interact to create a syndemic, where the coexistence of two or more conditions exacerbates the effects of one or all conditions. One example is coinfection with HIV and Mycobacterium tuberculosis, which is associated with more rapid disease progression, worse symptoms, and a higher pathogenic load than during a single infection with either agent (Singer et al. 2017). Syndemic risk also includes social, political, economic, and environmental factors that increase risk for the clustering of two or more diseases (Singer et al. 2017; Singer and Clair 2003). One of the first syndemics identified involved substance abuse, violence, and AIDS (SAVA), in which the inner-city health crisis around HIV/AIDS was related to other conditions, including tuberculosis, sexually transmitted infections, hepatitis, cirrhosis, infant mortality, drug abuse, suicide, and homicide. These were, in turn, connected to poverty, homelessness, unemployment, poor nutrition, lack of social support, and social and ethnic inequality (Singer et al. 2017). Together, these factors and others, like health policy and unequal access to health care, form an ecological model of health and disease, a more holistic way of viewing health issues and their solutions than focusing solely on biology and medical intervention (Sallis et al. 2008).
A historical example will serve to illustrate these concepts. You will remember the discussion of the first epidemiological transition from earlier in this chapter. This involved a rise in infectious disease following human adoption of agriculture as a primary subsistence strategy. This transition took place in the Old World and was fueled by zoonotic pathogens that infected humankind following the domestication of cattle, pigs, horses, sheep, goats, chickens, and other species. During the thousands of years following that transition, epidemics repeatedly occurred among Old World populations resulting in periods of crisis mortality, when large numbers of people died. This was followed by population recovery as survivors, who often became immune to reinfection, produced new generations to be infected during the next epidemic (Omran 2005). This same set of interactions did not, however, occur in the New World, where species that might have developed into domesticated animals equivalent to horses and cattle were wiped out at the end of the last Ice Age, when humans are hypothesized to have migrated to the New World across an exposed land bridge in the Arctic (Diamond 1997). These extinctions may have been the result of hunting or climate change or a combination of both. What is important to note is that the land bridge disappeared as sea levels rose at the end of the Ice Age, isolating the Americas until European contact in the 15th century. This isolation was to have severe consequences for Native Americans.
When Columbus “discovered” the New World in 1492, he unleashed one of the first waves of infectious disease that decimated Native American populations in the centuries to follow (Crosby 2003), eventually killing 90% of the population, an estimated 20 million people (Diamond 1997). The devastation of native communities was the result of a combination of factors. One was the very different histories of Europe and the Americas. With no history of animal domestication beyond dogs, turkeys, ducks, guinea pigs, llamas, and alpacas, Native Americans did not fall prey to zoonotic pathogens that produced highly contagious infectious diseases, leaving them with no resistance. Also, in spite of their profound differences in culture, language, subsistence, and political and economic systems, Native Americans were genetically very much alike (Crosby 2003). This was due to the small number of individuals who crossed the land bridge, which then closed, leaving them in genetic isolation for 10,000 years or more. This meant there was not a high degree of variation for natural selection to act upon in the midst of the severe evolutionary pressure of smallpox and other infectious diseases introduced by Europeans. Native Americans had also not benefited from the technological developments associated with warfare in the Old World, including steel swords, guns, and fighting on horseback, that had been perfected over centuries of conflict (Diamond 1997). European conquest also toppled existing political and social systems already crippled by epidemics of disease, leading to social disorder and cultural and economic disruption. To compound the situation, European colonization included the enslavement and forced labor of native populations to serve European interests, resulting in injury, starvation, and other mistreatment and leading to further loss of life. This complex of epidemiological, technological, social, political, and economic factors (a syndemic) combined to nearly exterminate Native Americans in the centuries following European contact, but this need not have been the case. Alfred Crosby (2003) points out that although epidemics among immunologically unprepared populations produce high mortality rates, some individuals survive, and the population will recover if left alone. He reminds us that,
Europe, for instance, lost one-third of its population to the Black Death in the fourteenth century and recovered in time. If the Black Death had been accompanied by the arrival of Genghis Khan’s hordes, miraculously plague-proof, the story would have been very different. It might have been similar to what happened when European settlers followed on the heels of smallpox and other infections previously unknown to American Indians. [Crosby 2003:xxii]
Unfortunately, syndemics did not begin or end with European colonization of the New World. Interactions between disease and income inequality, education, discrimination, warfare, migration, climate change, and a host of other factors continue to affect humans today, causing health disparities that lead to differences in morbidity and mortality within and across nations (Singer and Baer 2012; see Figure 16.9).
|
United States |
Worldwide |
|
1. Heart disease |
1. Heart disease |
|
2. Cancer |
2. Stroke |
|
3. Accidents |
3. Chronic Obstructive Pulmonary Disease |
|
4. Chronic lower respiratory diseases |
4. Lower respiratory infections |
|
5. Stroke |
5. Alzheimer disease and dementia |
|
6. Alzheimer’s disease |
6. Lung cancer |
|
7. Diabetes |
7. Diabetes mellitus |
|
8. Influenza and pneumonia |
8. Road injury |
|
9. Kidney disease |
9. Diarrheal diseases |
|
10. Suicide |
10. Tuberculosis |
Figure 4.7 Top ten causes of death in the U.S. and worldwide.
Although a full discussion of global health disparities is beyond the scope of this chapter, a brief discussion of asthma in the United States can shed light on several common factors that contribute to inequalities in health today. Nearly 20 million people in the U.S. suffer from asthma, over a third of whom are children under 18 years of age (CDC 2017). Childhood-asthma prevalence doubled from 1980 to 1995, then increased slowly from 2001 to 2010, leveling off in 2013. Rates of asthma are highest among African American and Latino children (Akinbami et al. 2016). Among Latinos, Puerto Ricans have the highest lifetime asthma rate (16.9%), more than three times the rate for Mexican Americans (Singer and Baer 2012). Given that most adult asthma has its origins in early life, discovering the causes of childhood asthma and preventing it has become a major public health focus (Beasley et al. 2015).
A range of factors contribute to the development of asthma in childhood. These include genetics and family history, as well as exposure to stress and being born into a single-parent family. Other factors include being a low-birth-weight baby or being born prematurely. Living in an urban environment, being exposed to indoor and outdoor air pollution, including cigarette smoke, is also a contributor. Certain childhood infections (e.g., pertussis), antibiotics use, and exposure to environmental toxins like mold are also associated with asthma. Diets high in trans-fatty acids and salt, especially fast-food, also contribute to the development of asthma. Sedentarism, high BMI, overweight, and obesity are also factors, with incidence increased by 20% in overweight children and doubled for obese kids (Chen et al. 2012). There are also gender differences associated with the obesity-asthma connection, with boys experiencing higher rates until age 13 and asthma becoming more prevalent in girls post-puberty (Beasley et al. 2015). The mechanisms behind this are unknown but may include anatomical differences in lung capacity, sleep disorders, body fat distribution, and inflammation (Chen et al. 2012). In keeping with the hygiene hypothesis, children exposed to dogs or farm animals in early childhood, including before age one, are less likely to develop asthma (Fall et al. 2015), especially children in urban environments where they may have less frequent contact with the natural environment (Dunn 2018).
Differences in prevalence of childhood asthma between ethnic groups within a population are not mainly because of genetic differences but, rather, because of differences in exposure to environmental and lifestyle factors (Beasley et al. 2015). Given this, let us examine the case of African American and Latino children in light of the risk factors just described. Working-class people and people of color in the U.S. are more likely to live in close proximity to freeways and environmental threats like petrochemical plants and waste incinerators. They are also more likely to live in poverty and in areas with high rates of crime and violence, which elevate stress levels, as does racial discrimination (Singer and Baer 2012). African American children are also far more likely than other groups in the U.S. to grow up in female-headed households, with 72% now being born to single mothers (Washington 2010), many of whom live in poverty and lack access to health care (Pearl 2015). Accurate diagnosis and treatment are key to management of childhood asthma, yet many children of color remain undiagnosed, in part because of lack of regular check-ups. One study conducted among Puerto Ricans in Chicago found prevalence of asthma among Puerto Rican children jumped to 34% when counting cases of possible asthma based on reports of patient symptoms rather than a physician’s diagnosis (Joseph et al. 1996). Another study, conducted in New York City, demonstrated that Puerto Rican children were more likely to miss school because of asthma than other ethnic groups in the same neighborhoods, and that low-income Latino families with children with asthma were less likely to have training, education, and resources to manage their child’s asthma (Findley et al. 2003). A 2002 study of over 1,000 American children and their families found that Latino and African American children were less likely to be prescribed the standard treatment for asthma and that Latino children received fewer inhaled steroids than white children (Ortega et al. 2002). Clearly, there are multiple factors contributing to health disparities in asthma for American children of different ethnic backgrounds, suggesting an ecological approach is necessary for addressing the problem.
Currently, there is no cure for asthma and no vaccine against it. Instead, public health efforts have largely focused on diagnosis, treatment, and education in place of prevention (Beasley et al. 2015). Given the sheer number of risk factors involved, some scholars have begun to question whether prevention is even possible. Richard Beasley and colleagues (2015:1078) explain: “Public health efforts will need to focus on reducing environmental tobacco exposure, reducing indoor and outdoor air pollution and occupational exposures, reducing childhood obesity and encouraging a diet high in vegetables and fruit, improving fetal and maternal health, encouraging breastfeeding, promoting childhood vaccinations, and reducing social inequalities.” These challenges serve to remind us to take an ecological approach to health and disease. As humans, we all have our biology and genetics with which to contend, but we often do so in the midst of very different life circumstances.
ARE WE STILL EVOLVING?
Given the current global burden of non-communicable diseases like heart disease, cancer, and diabetes discussed in this chapter, many students ask why humans have not yet evolved in response. First, the health conditions highlighted here do not typically have repercussions on reproductive success, meaning natural selection cannot act to favor one genotype over another to protect against them. There also may not have been sufficient time for natural selection to act (Stearns et al. 2008). The cultural transformation of our food supply and lifestyle came about quickly. The transition from foraging to farming took place beginning 12,000 years ago, industrial food production came about in the last 200 years, and technologies like television, the internet, and social media that promote sedentarism are less than 75 years old—one human lifetime. Even under the strongest selective pressure, evolution takes many generations. For example, the mutation that led pastoral populations to be able to digest fresh milk likely took 8,000 years, or 325 generations, to reach a frequency of 90% (Crow and Kimura 1970). This does not mean, however, that humans have stopped evolving. As a species, we continue to respond to selective pressures biologically and culturally. This portion of the chapter will focus on contemporary examples of human evolution.
Before beginning, let’s remind ourselves of the modern definition of evolution, which is a change in allele frequencies across generations in a given population for a particular trait. We must also review the conditions necessary for natural selection to operate on a trait. First, the trait must be heritable, meaning it is transmitted genetically from generation to generation. Non-inherited traits are learned and include things like cultural preferences for certain types of foods or who we think it is best to marry. Not only must a trait be heritable, there must also be variation of the trait in human populations and the trait must influence reproductive success. Three examples of traits that meet these criteria are immunity to HIV, height, and wisdom teeth (Andrews et al. 2011).
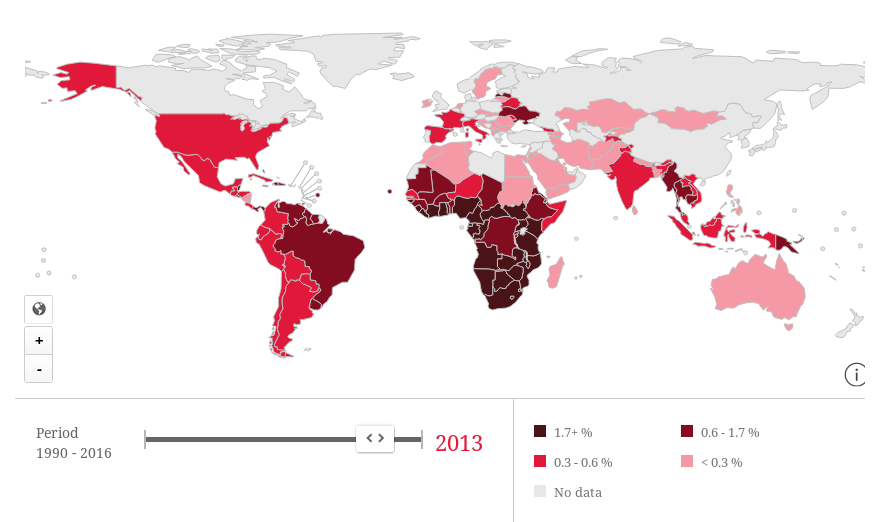
AIDS is a potentially fatal infectious disease caused by the Human Immunodeficiency Virus (HIV), a zoonosis believed to be derived from Simian Immunodeficiency Viruses (SIVs) found in chimpanzees and monkeys, most likely transmitted to humans through the butchering of infected animals (Sharp and Hahn 2011). In total, 35 million people have died from AIDS-related illnesses since the start of the global epidemic in the 1980s. There were 36.7 million people around the world living with AIDS as of 2016, including 1.8 million new cases and 1 million deaths in that year alone (UNAIDS 2018). A disease causing this level of morbidity and mortality represents a major selective pressure, especially given that infection can occur before birth (Goulder et al. 2016), having an affect on future reproductive success.
The majority of people in the world are highly susceptible to HIV infection, but some are not. There are individuals who are homozygous for a rare, recessive allele at the CCR5 locus who are immune. Heterozygotes who inherit a single copy of this allele are more resistant to infection and the disease takes longer to progress in the event they are infected. The mechanism by which the allele prevents infection involves a 32-base pair deletion in the DNA sequence of the CCR5 gene, creating a non-functioning receptor on the surface of the cell that prevents HIV from infecting the cell. The allele is inherited as a simple Mendelian trait, and there is variation in its prevalence, ranging as high as 14% of the population in northern Europe and Russia (Novembre et al. 2005; see Figure 16.8). What is interesting about the allele’s geographic distribution is that it does not map onto parts of the world with the highest rates of HIV infection (UNAIDS 2018), suggesting that AIDS was not the original selective pressure favoring this allele (Figure 16.10 and Figure 16.11).
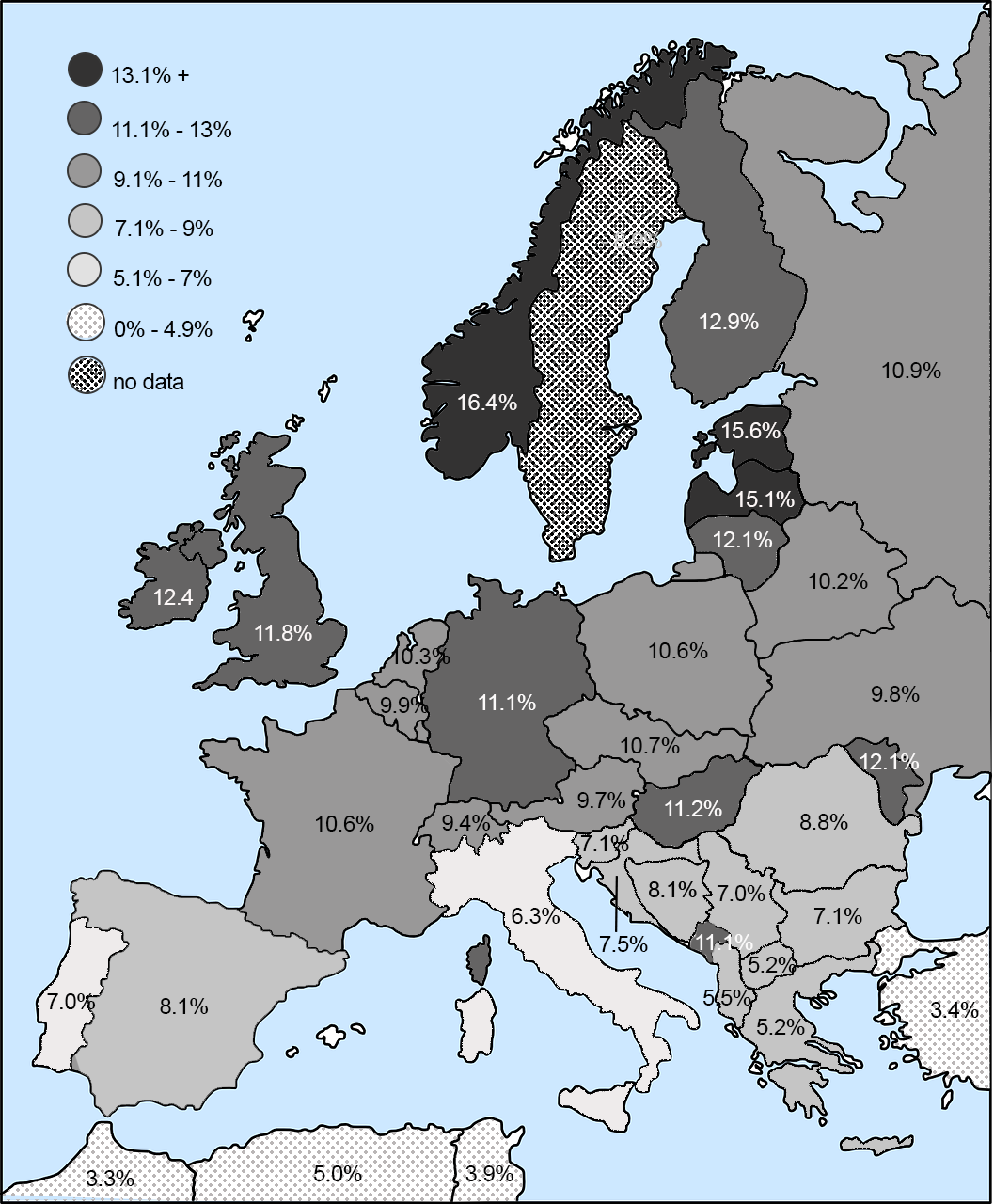
Given its current geographic distribution, the bubonic plague, which ravaged Europe repeatedly from the 14th to the 19th centuries (Pamuk 2007), was initially proposed as the selective agent. Subsequent research suggests smallpox, which killed up to 400,000 people annually in 18th-century Europe (Hays 2005), was more likely the selective pressure (Novembre et al. 2005). Given the mortality rates for smallpox and the selective pressure it has exhibited on humanity for centuries (Crosby 2003), an allele that conferred immunity was highly advantageous, as it is for those faced with the threat of HIV infection today. There are efforts to employ the natural immunity this mutation provides in the creation of an AIDS vaccine (Lopalco 2010).
Height is another example of a trait currently experiencing selective pressure. If you have ever toured a historical site, you have likely hit your head on a doorframe or become claustrophobic trying to squeeze down a narrow hallway under a lower-than-average ceiling. It is not your imagination. Humans have gotten taller in recent centuries. In fact, the average height of people in industrialized nations has increased approximately 10 centimeters (about four inches) in the past 150 years. This increase has been attributed to improvements in nutrition, sanitation, and access to medical care (Hatton 2014). But this is only part of the story.
Height is highly heritable. Studies indicate 80% of variation in height within populations is due to genetics, with 697 different genetic variances identified as having an effect on adult stature (Devuyst 2014). Multiple studies also demonstrate a positive relationship between height and reproductive success for men (Andrews et al. 2011). This is primarily due to sexual selection and nonrandom mating, namely women’s preferences for taller men, which may explain why height is one characteristic men often lie about on dating websites (Guadagno et al. 2012). Sexual selection also plays out with regard to economic success in Western cultures, with taller men more likely to be in higher-level positions that pay well. Research demonstrates an inch of height is worth an additional $789 per year in salary, meaning a man who is six feet tall will earn on average $5,525 more per year than an identical man who is five foot five (Gladwell 2007). Over the course of a thirty-year career, this adds up to hundreds of thousands of dollars, likely allowing the taller man to attract more potential mates and increase his reproductive success.
Wisdom teeth are also undergoing evolutionary pressure. Have you or anyone in your family had their wisdom teeth removed? It can be a painful and expensive process, and it is a common experience in Western nations. Conversely, do you know anyone whose wisdom teeth never came in? That is fairly common in other populations, suggesting evolutionary pressure favoring the absence of wisdom teeth has been culturally influenced. According to research by physical anthropologists, the oldest fossil evidence of skulls missing third molars was found in China and is 300,000 to 400,000 years old, suggesting the earliest mutation selecting against the eruption of wisdom teeth arose in Asia (Main 2013). Since that time, jaws have continued to decrease in size to the point they often cannot accommodate third molars, which can become impacted, painful, and even infected, a condition physical anthropologist Alan Main argues might have interfered with the ability to survive and reproduce in ancestral populations (Main 2013). As we have learned, a mutation that positively influences reproductive success—such as being born without the trait to develop wisdom teeth in an environment where food was cooked before eating—would likely be selected for over time. Evidence in modern humans suggests this is the case, with 40% of modern Asians and 45% of Native Alaskans and Greenlanders (populations descended from Asian populations) lacking wisdom teeth. The percentage among those of European descent ranges from 10 to 25% and for African Americans is 11% (Main 2013). Earlier chapters in this text emphasize that directional selection progresses along a particular path until the environment changes and a trait is no longer advantageous. In the case of wisdom teeth, the ability of modern dentistry to preempt impaction through surgery may, in fact, be what is preventing natural selection from doing away with wisdom teeth altogether.
FOOD FOR THOUGHT
This chapter focused on health conditions prevalent in contemporary, industrialized societies that are due, in part, to the mismatch between our evolved biology and modern cultural and physical environments. Obesity is at the root of it all. Claude Bouchard (2007) identified factors contributing to the global epidemic of obesity and the diseases associated with it. These are the built environment and the social environment, which together form the obesogenic environment in which unhealthy behaviors are encouraged. This chapter will close by examining each of these in a college context.

In terms of the built environment, consider your campus or neighborhood from an evolutionary perspective. To what degree does the construction of the space lend itself to physical activity as part of daily life? Is your campus constructed in such a way that it promotes the use of automobiles at the expense of walking or biking? If driving is necessary, is parking available close to the buildings or do you need to walk a fair distance from the parking lot to your destination? Do the buildings have stairs or ramps or is it necessary to take the elevator? Is it possible to negotiate safely around campus or the neighborhood on foot or by bike in all weather? After dark? How about the classrooms and computer labs? Do they have standing or treadmill desks as options? Does your class schedule encourage walking from building to building between classes, or are most courses in your major scheduled in the same location? I regularly have students who sit in the same room for hours, not even changing desks, while instructors rush from place to place. Most college majors also lack a physical activity requirement, leaving it up to students to incorporate exercise into already-busy schedules (See Figure 4.10).
Sociocultural factors that contribute to obesity include food advertising, ubiquitous fast-food and junk food options, and social pressure to consume, all of which are present on college campuses. Although nutritional options on campuses have improved in recent years, many students find eating healthy in the dining halls and dorms challenging (Plotnikoff et al. 2015), and students who live off campus fare even worse (Small et al. 2013). There are also parties and other social events, a normal part of college life, that often involve unhealthy food and encourage behaviors like alcohol consumption and smoking. Give some thought to the social atmosphere on your campus and the ways in which it may contribute to obesity. My own freshman orientation involved a succession of pizza parties, ice cream socials, and barbecues, followed by late-night runs to the nearest fast-food outlet. The purpose of these events was to encourage people to make friends and feel comfortable living away from home, but the foods served were not healthy, and there was social pressure to join in and be part of the group. Such activities set students up for the “freshman fifteen” and then some. They also reinforce the idea that being social involves eating (and sometimes drinking and/or smoking).
Sedentarism and inactivity are also built into the academics of college life. Digital technology is a significant contributor to obesity. Students use laptops and cell phones to take notes, complete their work outside of class, and access social media. There are also video games, virtual reality headsets, and streaming television and movies for entertainment. The built environment of college already necessitates that students sit in class for hours each day, then sit at computers to complete work outside of class. The social environment enabled by digital technology encourages sitting around for entertainment. It is telling that we call it “binge watching” when we spend hours watching our favorite shows. Doing so often involves eating, as well as multiple exposures to food advertising embedded in the shows themselves. In these many ways, college contributes to the development of obesogenic behaviors that can have negative health ramifications long after college is over (Small et al. 2013).
In the U.S., the greatest increase in obesity is among young adults aged 18–29 years, a significant percentage of whom are college students (Plotnikoff et al. 2015). Analyses of college students’ behavior across semesters shows consumption of fruits and vegetables drops over time, as does the amount of physical activity, while consumption of sugar-sweetened beverages and fast-food goes up, leading to weight gain at nearly six times the rate of the general public (Small et al. 2013). Realizing this, many colleges and universities have instituted programs to encourage healthier eating and more physical activity among students (Plotnikoff et al. 2015). Some schools have even done away with collegiate sports, which often serve a small percentage of students, in favor of campus-wide efforts at getting everyone active (Tierney 2013). Investigate the options on your campus and take advantage of opportunities. We cannot change our biology, but we can certainly change our habits.
Exercises
Review Questions
- Geographer, historian, and author Jared Diamond (1987) once referred to agriculture as “the worst mistake in the history of the human race.” Given what you have learned about the health consequences of the domestication of plants and animals for humans, how would you respond to his statement?
- Why do humans like foods that are “bad” for them? Describe the evolutionary underpinnings of our tastes for sugar, salt, and fat.
- How might understanding contemporary disease from an evolutionary perspective benefit medical practitioners in treating their patients?
- Given the size of the world population today, humanity could not return to foraging for subsistence. What can we do to promote healthier food consumption on a world scale? How might we build changes into our physical environments to counter the health risks associated with modern diet and activity patterns?
- Several risk factors for conditions like heart disease, diabetes, and cancer are referred to as “lifestyle factors,” implying these are behavioral choices people make that put them at risk. These include unhealthy eating, lack of physical activity, smoking, and alcohol consumption. To what degree is unhealthy behavior structured by environment? For example, how does being a college student influence your eating habits, physical activity patterns, smoking, and consumption of alcohol?
- Who benefits from the global obesity epidemic? Think about the following industries and institutions: How might the medical establishment profit from obesity? The fitness industry? The diet industry? Fashion? Pharmaceutical companies? Food manufacturers? Advertisers?
- Can you think of any human traits in addition to height, wisdom teeth, and immunity from HIV that might be undergoing selection? How would you go about investigating those traits to find out if this is true?
Key Terms
Autotrophic: Autotrophic organisms are capable of producing their own food using inorganic substances such as light, water, carbon dioxide or chemical energy.
Body Mass Index (BMI): A person’s weight in kilograms divided by the square of their height in meters. The most widely used measure for identifying obesity. The formula using kilograms and meters (or centimeters) is: weight (kg) / [height (m)]2 . The formula using pounds and inches is: 703 x weight (lbs) / [height (in)]2 .
Cancer: A collection of related diseases in which some of the body’s cells begin to divide without stopping and spread into surrounding tissues.
Cardiovascular Disease (CVD): A disease of the heart and blood vessels, often related to atherosclerosis, CVD is a condition in which a substance called plaque builds up in the walls of the arteries, blood vessels that carry blood away from the heart, compromising the flow of blood to the heart or brain.
Central Nervous System: The complex of nerve tissues stemming from the brain and spinal cord that controls the activities of the body.
Circulatory system: The biological system that circulates blood around the body via the heart, arteries, and veins, delivering oxygen and nutrients to organs and cells and carrying waste products away.
Diabetes Mellitus: An endocrine disorder in which high glucose (blood sugar) levels occur over a prolonged period of time. Blood glucose is your body’s main source of energy and comes from the food you eat. Insulin, a hormone made by the pancreas, helps glucose from food get into your cells to be used for energy. Sometimes your body does not make enough—or any—insulin (Type 1 diabetes) or does not take up insulin well (Type 2 diabetes). Glucose then stays in your blood and does not reach your cells.
“Double Burden”: Refers to parts of the world in which there is a prevalence of chronic disease (e.g.,. cancer, heart disease) while, at the same time, there are also high rates of infectious disease due to poverty, malnutrition, poor sanitation, and lack of access to health care, often accompanied by high rates of maternal and child mortality.
Ecological model: Ecological models of health and disease emphasize environmental and policy contexts of behavior, while incorporating social and psychological influences, rather than focusing on individual behaviors. These models encompass multiple levels of influence and can lend themselves to more comprehensive health interventions.
Emerging Infectious Diseases (EIDs): Infections that have recently appeared within a population or those whose incidence or geographic range is rapidly increasing or threatens to increase in the near future. Examples include Ebola, Zika, SARS, and avian (bird) flu.
Endocrine system: Those organs in the body whose primary function is the production of hormones.
Epidemiological transition: A transformation in patterns of disease (morbidity) and death (mortality) among a population.
Glucose metabolism: The body’s evolved mechanism by which we turn food into energy for bodily functions.
Glycemic Index (GI): A system that ranks foods on a scale from 1 to 100 based on their effect on blood-sugar levels. Carbohydrates with a low GI value (55 or less) are more slowly digested and metabolised causing a lower, slower rise in blood glucose and insulin levels.
Hypertension: High blood pressure. Blood pressure is the force exerted by the blood against the walls of the blood vessels. In a blood pressure reading, the top number (usually higher) refers to the systolic pressure, the amount of pressure in your arteries during the contraction of your heart muscle when your heart beats. The bottom number is the diastolic pressure when your heart muscle is resting between beats. Hypertension can lead to severe health complications and increases the risk of heart attack and stroke.
Incidence: The rate at which new cases of a disease occur in a population over a given period of time.
Insulin: A hormone produced in the pancreas that regulates the amount of glucose in the blood. Lack of insulin or the inability to absorb insulin causes diabetes.
Metabolic Syndrome: A cluster of conditions, including increased blood pressure, high blood sugar, excess body fat around the waist, and abnormal cholesterol levels that occur together, increasing the risk of heart disease, stroke, and diabetes. Lifestyle changes like losing weight, regularly exercising, and making dietary changes can help prevent or reverse metabolic syndrome.
Menarche: The first occurrence of menstruation.
Morbidity: The number of cases of disease per unit of population occurring over a unit of time.
Mortality: The number of deaths attributable to a particular cause per unit of population over a unit of time.
Noncommunicable Diseases (NCDs): Also known as chronic diseases, NCDs tend to be of long duration and are the result of a combination of genetic, physiological, environmental, and behavior factors. The main types of NCDs are cardiovascular diseases (like heart attacks and stroke), cancers, chronic respiratory diseases (such as chronic obstructive pulmonary disease and asthma), and diabetes.
Obesity: A medical condition in which excess body fat has accumulated to the point that it has adverse effects on health. The most widely used measure for identifying obesity is the Body Mass Index (BMI), a person’s weight in kilograms divided by the square of their height in meters. A measure of 30 kg/m2 is considered obese and 25—29 kg/m2 overweight. Distribution of body fat also matters. Fat in the abdominal region has a stronger association with Type 2 diabetes and cardiovascular disease, meaning waist to hip ratio and waist circumference are also important indicators of obesity-related health risk.
Obesogenic: Promoting excessive weight gain. For example, an environment in which tasty, cheap food filled with excess calories is abundant.
Omnivorous: Able to eat and digest foods of both plant and animal origins.
Osteoarthritis: Refers to the degeneration of joint cartilage and underlying bone, causing pain and stiffness. In the absence of previous injury, it is most common in modern populations from middle age onward.
Prevalence: The proportion of individuals in a population who have a particular disease or condition at a given point in time.
Sedentism: Living in groups settled permanently in one place.
Sedentarism: A way of life characterized by much sitting and little physical activity.
Stress response: A predictable response to any significant threat to homeostasis. The human stress response involves the central nervous system and the endocrine system acting together. Sudden and severe stress incites the “flight or flight” response from the autonomic nervous system in conjunction with hormones secreted by the adrenal and pituitary glands, increasing our heart rate and breathing and releasing glucose from the liver for quick energy.
Stroke: A stroke occurs when a blood vessel leading to the brain is blocked or bursts, preventing that part of the brain from receiving blood and oxygen, leading to the death of cells in that part of the brain.
Syndemic: The aggregation (grouping together) of two or more diseases or health conditions in a population in which there is some level of harmful biological or behavioral interface that exacerbates the negative health effects of any or all of the diseases involved. Syndemics involve the adverse interaction of diseases of all types, including infections, chronic non-communicable diseases, mental health problems, behavioral conditions, toxic exposure, and malnutrition.
Vector-borne diseases: Human illnesses caused by parasites, viruses, and bacteria that are transmitted by mosquitoes, flies, ticks, mites, snails, and lice.
Zoonoses: Diseases that can be transmitted from animals to humans.
For Further Exploration
Lents, Nathan H. 2018. Human Errors: A Panorama of Our Glitches, from Pointless Bones to Broken Genes. Boston: Houghton Mifflin Harcourt.
Stearns, Stephen C., and Jacob C. Koella, eds. 2008. Evolution in Health and Disease. Second Edition. United Kingdom: Oxford University Press.
Zuk, Marlene. 2013. Paleofantasy: What Evolution Really Tells Us About Sex, Diet, and How We Live. New York: W.W. Norton & Company.
CITATION/ATTRIBUTION
Namie, Joylin. “16 Contemporary Topics: Human Biology and Health.” In EXPLORATIONS: AN OPEN INVITATION TO BIOLOGICAL ANTHROPOLOGY, edited by Beth Shook, Katie Nelson, Kelsie Aguilera, and Lara Braff. American Anthropological Associationn.d. https://pressbooks-dev.oer.hawaii.edu/explorationsbioanth/chapter/__unknown__-11/.
References
Abid, Zaynah, Amanda J. Cross, and Rashmi Sinha. 2014. “Meat, Dairy, and Cancer.” The American Journal of Clinical Nutrition 100, Issue Supplement 1 (1): 386S–393S.
Akil, Luma, and H. Anwar Ahmad. 2011. “Relationships between Obesity and Cardiovascular Diseases in Four Southern States and Colorado.” Journal of Health Care for the Poor and Underserved 22 (Suppl. 4): 61–72.
Akinbami, Lara J., Alan E. Simon, and Lauren M. Rossen. 2016. “Changing Trends in Asthma Prevalence among Children.” Pediatrics 137 (1). doi:10.1542/peds.2015-2354.
Ali, Aus Tariq. 2014. “Reproductive Factors and the Risk of Endometrial Cancers.” International Journal of Gynecological Cancer 24 (3): 384–393.
American Heart Association. 2014. “Smoking & Cardiovascular Disease (Heart Disease).” Last modified February 17, 2014. https://docs.google.com/ document/d/1iMgccSz67i37839NhIAPGQlwsWA3VGtSKtejlrGN_LI/edit.
——— 2018. “Heart Disease and Stroke Statistics 2017 At-a-Glance.” Last modified January 31, 2018. https://healthmetrics.heart.org/wp-content/uploads/2018/02/At-A-Glance-Heart-Disease-and-Stroke-Statistics-2018.pdf.
American Psychiatric Association (APA). 2013. Diagnostic and Statistical Manual of Mental Disorder. Fifth Edition: DSM-5. Washington, DC: APA.
Andrews, Tessa M., Steven T. Kalinowski, and Mary J. Leonard. 2011. “Are Humans Evolving? A Classroom Discussion to Change Students’ Misconceptions Regarding Natural Selection.” Evolution: Education and Outreach 4 (3): 456–466.
Armelagos, George. 1990. “Health and Disease in Populations in Transition.” In Disease in Populations in Transition, edited by Alan C. Swedlund and George J. Armelagos, 127–144. New York: Bergin & Garvey.
Armelagos, George J., Peter J. Brown, and Bethany Turner. 2005. “Evolutionary, Historical and Political Economic Perspectives on Health and Disease.” Social Science and Medicine 61 (4): 755–765.
Asher, Claire. 2017. “Illegal Bushmeat Trade Threatens Human Health and Great Apes.” Mongabay, April 6. https://news.mongabay.com/2017/04/illegal-bushmeat-trade-threatens-human-health-and-great-apes/.
Baer, Hans, and Merrill Singer. 2009. Global Warming and the Political Ecology of Health: Emerging Crises and Systemic Solutions. Walnut Creek, CA: Left Coast Press.
Baker, W.A., G.A. Hitman, K. Hawrami, M.I. McCarthy et al. 1994. “Apolipoprotein D Gene Polymorphism: A New Genetic Marker for Type 2 Diabetic Subjects in Nauru and South India.” Diabetic Medicine 11 (10): 947–952.
Baltic, Milan Z., and Marija Boskovic. 2015. “When Man Met Meat: Meat in Human Nutrition from Ancient Times Till Today.” Procedia Food Science 5: 6–9.
Beasley, Richard, Alex Semprini, and Edwin A. Mitchell. 2015. “Risk Factors for Asthma: Is Prevention Possible?” The Lancet 386 (9998): 1075–1085.
Berenbaum, Francis. 2011. “Diabetes-induced Osteoarthritis: From a New Paradigm to a New Phenotype.” Annals of the Rheumatic Diseases 70 (8). doi:10.1136/ard.2010.146399.
Berna, Francesco, Paul Goldberg, Liora Kolska Horwitz, James Brink, Sharon Holt, Marion Bamford, and Michael Chazan. 2012. “Microstratigraphic Evidence of In Situ Fire in the Acheulean Strata of Wonderwerk Cave, Northern Cape Province, South Africa.” Proceedings of the National Academy of Sciences 109: E1215e-E1220.
Blue Cross Blue Shield Association (BCBSA). 2017. “Diabetes and the Commercially Insured U.S. Population.” The Health of America Report, August 1. https://www.bcbs.com/the-health-of-america/reports/diabetes-and-commercially-insured-us-population.
Bogin, Barry. 1991. “The Evolution of Human Nutrition.” In The Anthropology of Medicine: From Culture to Method, edited by Lola Romanucci-Ross, Daniel E. Moerman, and Laurence R. Tancredi, 158–195. New York: Bergin & Garvey.
Bouchard, Claude. 2007. “The Biological Predisposition to Obesity: Beyond the Thrifty Genotype Scenario.” International Journal of Obesity 31: 1337–1339.
Brown, Peter J. 1991. “Culture and the Evolution of Obesity.” Human Nature 2 (1): 31–57.
Bruni, L., L. Barrionuevo-Rosas, G. Albero, B. Serrano et al. 2017. “Human Papillomavirus and Related Diseases in the World.” Summary Report 27, July. ICO/IARC Information Centre on HPV and Cancer (HPV Information Centre). http://www.hpvcentre.net/statistics/reports/XWX.pdf.
Buchman, Aron S., Lei Yu, Robert S. Wilson, Andrew Lim, Robert J. Dawe, Chris Gaiteri, Sue E. Leurgans, Julie A. Schneider, and David A. Bennett. 2019. “Physical Activity, Common Brain Pathologies, and Cognition in Community-Dwelling Older Adults.” Neurology 98 (2). doi:10.1212/WNL.0000000000006954.
Center for Science in the Public Interest (CSPI). 2010. Food Dyes: A Rainbow of Risk. Washington, DC: Center for Science in the Public Interest.
Centers for Disease Control and Prevention (CDC). 2014. Breastfeeding Report Card: United States/2014. Atlanta, GA: Centers for Disease Control and Prevention.
———. 2016. “Leading Causes of Death.” National Center for Health Statistics. https://www.cdc.gov/nchs/fastats/leading-causes-of-death.htm.
——— 2017. “Human Papillomavirus.” Genital HPV Infection—Fact Sheet. Atlanta, GA: Centers for Disease Control and Prevention.
———. 2017. “Asthma.” National Center for Health Statistics. https://www.cdc.gov/nchs/fastats/asthma.htm.
Cerón, Ella. 2017. “Here’s Every Oreo Flavor Ever Created.” TeenVogue.com, June 19. https://www.teenvogue.com/story/every-oreo-flavor-ranked.
Chen, Yang, Yi-Lun Lee, and Guang-Hui Dong. 2012. “Gender Difference of Childhood Overweight and Obesity in Predicting the Risk of Incident Asthma: A Systematic Review and Meta-Analysis.” Obesity Reviews 14 (3): 222–231. doi:10.1111/j.1467-789X.2012.01055.x
Chin, Jessie, Brennan R. Payne, Wai-Tat Fu, Daniel G. Morrow, and Elizabeth A. L. Stine-Morrow. 2015. “Information Foraging across the Life Span: Search and Switch in Unknown Patches.” Topics in Cognitive Science 7 (3): 428–450.
Cooling, Laura. 2015. “Blood Groups in Infection and Host Susceptibility.” Clinical Microbiology Reviews 28 (3): 801–870.
Cordain, Loren. 2002. The Paleo Diet: Lose Weight and Get Healthy by Eating the Food You Were Designed to Eat. Hoboken, NJ: John Wiley & Sons.
Crosby, Alfred W., Jr. 2003. The Columbian Exchange: Biological and Cultural Consequences of 1492. 30th Anniversary Edition. Westport, CT: Praeger Publishers.
Croston, Glenn. 2012. “The Thing We Fear More Than Death: Why Predators Are Responsible for Our Fear of Public Speaking.” Psychology Today blog, November 29. https://www.psychologytoday.com/us/blog/the-real-story-risk/201211/the-thing-we-fear-more-death.
Crow, James F., and Motoo Kimura. 1970. An Introduction to Population Genetics Theory. New York: Harper and Row.
Currie, Candace, Naman Ahluwalia, Emmanuelle Godeau, Saoirse Nic Gabhainn, Pernille Due, and Dorothy B. Mille . 2012. “Is Obesity at Individual and National Level Associated with Lower Age at Menarche? Evidence from 34 Countries in the Health Behaviour in School-Aged Children Study.” Journal of Adolescent Health 50 (6): 621–626.
David, A. Rosalie, and Michael Zimmerman. 2010. “Cancer: An Old Disease, A New Disease or Something In Between?” Nature Reviews: Cancer 10 (10): 728–733.
Davis, Mike. 2005. The Monster at Our Door: The Global Threat of Avian Flu. New York: Owl Books.
de Silva, A. M., K. R. Walder, T. J. Aitman, T. Gotoda, A. P. Goldstone, A. M. Hodge, M. P. de Courten, P. Z. Zimmet, and G. R. Collier. 1999. “Combination of Polymophisms in OB-R and the OB Gene Associated with Insulin Resistance in Nauruan Males.” International Journal of Obesity 23 (8): 816–822.
Devuyst, Olivier. 2014. “High Time for Human Height.” Peritoneal Dialysis International 34 (7): 685–686.
Diamond, Jared. 1987. “The Worst Mistake in the History of the Human Race.” Discover, May: 64–66.
———. 1997. Guns, Germs, and Steel: The Fates of Human Societies. New York: W. W. Norton.
Dimsdale, Joel E. 2008. “Psychological Stress and Cardiovascular Disease.” Journal of the American College of Cardiology 51 (13): 1237–1246.
Dunn, Robb. 2018. Never Home Alone: From Microbes to Millipedes, Camel Crickets, and Honeybees, the Natural History of Where We Live. New York: Basic Books.
Dutton, Denis. 2009. The Art Instinct: Beauty, Pleasure, and Human Evolution. New York: Bloomsbury.
Eaton, S. Boyd, Melvin Konner, and Marjorie Shostak. 1988. “Stone Agers in the Fast Lane: Chronic Degenerative Diseases in Evolutionary Perspective.” American Journal of Medicine 84 (4): 739–749.
Eaton, S. Boyd, Malcolm C. Pike, Roger V. Short, Nancy C. Lee, James Trussell, Robert A. Hatcher, James W. Wood, et al. 1994. “Women’s Reproductive Cancers in Evolutionary Context.” The Quarterly Review of Biology 69 (3): 353–367.
Ewald, Paul W. 2018. “Ancient Cancers and Infection-Induced Oncogenesis.” International Journal of Paleopathology 21: 178–185. http://dx.doi.org/10.1016/J.ijpp.2017.08.007.
Fall, Tove, Cecilia Lundholm, Anne K. Orkqvist, Katja Fall et al. 2015. Early Exposure to Dogs and Farm Animals and the Risk of Childhood Asthma. JAMA Pediatrics 169 (11). doi: 10.1001/jamapediatrics.2015.3219.
Farb, Peter, and George Armelagos. 1980. Consuming Passions: The Anthropology of Eating. New York: Washington Square Press.
Findley, Sally, Katherine Lawler, Monisha Bindra, Linda Maggio, Madeline M. Penachio, and Christopher Maylahn. 2003. “Elevated Asthma and Indoor Environmental Exposures among Puerto Rican Children of East Harlem.” Journal of Asthma 40 (5): 557–569.
Flinn, Mark V., and Barry G. England. 2003. “Childhood Stress: Endocrine and Immune Responses to Psychosocial Events.” In Social and Cultural Lives of Immune Systems: Theory and Practice in Medical Anthropology and International Health, edited by James M. Wilce Jr., 105–146. London: Routledge.
Fumagalli, Matteo, Ida Moltke, Niels Grarup, Fernando Racimo, Peter Bjerregaard, Marit E. Jørgensen, Thorfinn S. Korneliussen, et al. 2015. “Greenlandic Inuit Show Genetic Signatures of Diet and Climate Adaptation.” Science349 (6254): 1343–1347.
Gao, George. 2015. “Americans’ Ideal Family Size Is Smaller Than It Used to Be.” Pew Research Center, May 8. http://www.pewresearch.org/fact-tank/2015/05/08/ideal-size-of-the-american-family/.
Gladwell, Malcolm. 2007. Blink: The Power of Thinking Without Thinking. New York: Back Bay Books.
Goulder, Philip J., Sharon R. Lewin, and Ellen M. Leitman. 2016. “Paediatric HIV Infection: The Potential for Cure.” Nature Reviews Immunology 16: 259–271.
Graber, Cynthia. 2014. “Michael Pollan Explains What’s Wrong with the Paleo Diet.” Mother Jones, January 17. https://www.motherjones.com/environment/2014/01/michael-pollan-paleo-diet-inquiring-minds/.
Greaves, Mel. 2015. “Evolutionary Determinants of Cancer.” Cancer Discovery 5 (8): 806–820.
Greenspan, Louise, and Julianna Deardorff. 2014. The New Puberty: How to Navigate Early Development in Today’s Girls. New York: Rodale.
Guadagno, Rosanna E., Bradley M. Okdie, and Sara A. Kruse. 2012. “Dating Deception: Gender, Online Dating, and Exaggerated Self-Presentation.” Computers in Human Behavior 28 (2): 642–647.
Guilak, Farshid. 2012. “Biomechanical Factors in Osteoarthritis.” Best Practice & Research: Clinical Rheumatology 25 (6): 815–823.
Gurven, Michael, and Hillard Kaplan. 2007. “Longevity among Hunter-Gatherers: A Cross-Cultural Examination.” Population and Development Review 33 (2): 321–365.
Hamilton, Cheryl. 2011. Communicating for Results, a Guide for Business and the Professions, Ninth Edition. Belmont, CA: Thomson Wadsworth.
Harper, Kristin, and George Armelagos. 2010. “The Changing Disease-Scape in the Third Epidemiological Transition.” International Journal of Environmental Research and Public Health 7 (2): 675–697.
Harris, Marvin. 1989. “Life Without Chiefs.” New Age Journal, November/December: 42–45, 205–209.
Hatton, Tim. 2014. “Why Did Humans Grow Four Inches in 100 Years? It Wasn’t Just Diet.” The Conversation, May 1. https://theconversation.com/why-did-humans-grow-four-inches-in-100-years-it-wasnt-just-diet-25919.
Hays, J. N. 2005. Epidemics and Pandemics: Their Impacts on Human History. Santa Barbara, CA: ABC-CLIO, Inc.
International Diabetes Federation (IDF). 2018. IDF Diabetes Atlas. Eighth Edition. http://www.diabetesatlas.org/key-messages.html.
Issa, Rital, and Timothy M. Griffin. 2012. “Pathobiology of Obesity and Osteoarthritis: Integrating Biomechanics and Inflammation.” Pathobiology of Aging and Age-Related Diseases 2 (1). https://doi.org/10.3402/pba.v2i0.17470.
Jain, H. K.. 2012. “Transition to Twenty-First Century Agriculture: Change of Direction.” Agricultural Research 1 (1): 12–17.
Jones, Kate E., Nikkita G. Patel, Mark A. Levy, Adam Storeygard, Deborah Balk, John L. Gittleman, and Peter Daszak. 2008. “Global Trends in Emerging Infectious Disease.” Nature 451 (7181): 990–993.
Jones, Rachel K., and Joerg Dreweke. 2011. Countering Conventional Wisdom: New Evidence on Religion and Contraceptive Use. Report, April 2011. New York: Guttmacher Institute.
Joseph, Christine L. M., Betsy Foxman, Frederick E. Leickly, Edward Peterson, and Dennis Ownby. 1996. “Prevalence of Possible Undiagnosed Asthma and Associated Morbidity among Urban Schoolchildren.” Journal of Pediatrics 129 (5): 735–742.
Kaczmarczyk, Melissa M., Michael J. Miller, and Gregory G. Freund. 2012. “The Health Benefits of Dietary Fiber: Beyond the Usual Suspects of Type 2 Diabetes Mellitus, Cardiovascular Disease and Colon Cancer.” Metabolism: Clinical and Experimental 61 (8): 1058–1066.
Larsen, Clark Spencer. 2014. “Foraging to Farming Transition: Global Health Impacts, Trends, and Variation.” In Encyclopedia of Global Archaeology, edited by Claire Smith, 2818–2824. New York: Springer.
Lattimer, James M., and Mark D. Haub. 2010. “Effects of Dietary Fiber and Its Components on Metabolic Health.” Nutrients 2 (12): 1266–1289.
Lee, Richard B. 2013. The Dobe Ju/’hoansi. Fourth Edition. Belmont, CA: Wadsworth/Cengage Learning.
Leontis, Lisa M. N.d. “Type 2 Diabetes and Exercise: Exercise Makes It Easier to Control Your Diabetes.” https://www.endocrineweb.com/conditions/type-2-diabetes/type-2-diabetes-exercise.
Lieberman, Daniel E. 2015. “Human Locomotion and Heat Loss: An Evolutionary Perspective.” Comprehensive Physiology 5(1): 99–117.
Lieberman, Leslie Sue. 2006. “Evolutionary and Anthropological Perspectives on Optimal Foraging in Obesogenic Environments.” Appetite 47 (1): 3–9.
Liu, Gang. 2018. “Abstract P184: Meat Cooking Methods and Risk of Hypertension: Results From Three Prospective Cohort Studies.” Circulation 137 (Suppl. 1): AP184.
Liu, Gang, Geng Zong, Kana Wu, Yang Hu, Yanping Li, Walter C. Willett, David M. Eisenberg, Frank B. Hu, and Qi Sun. 2018. “Meat Cooking Methods and Risk of Type 2 Diabetes: Results From Three Prospective Cohort Studies.” Diabetes Care 41 (5): 1049–1060.
Livingston, Gretchen. 2015. “Childlessness.” Pew Research Center, May 7. http://www.pewsocialtrends.org/2015/05/07/childlessness/.
Lopalco, Lucia. 2010. “CCR5: From Natural Resistance to a New Anti-HIV Strategy.” Viruses 2 (2): 574–600.
Lucock, Mark D., Charlotte E. Martin, Zoe R. Yates, and Martin Veysey. 2014. “Diet and Our Genetic Legacy in the Recent Anthropocene: A Darwinian Perspective to Nutritional Health.” Journal of Evidence-Based Complementary and Alternative Medicine 19 (1): 68–83.
Main, Douglas. 2013. “Ancient Mutation Explains Missing Wisdom Teeth.” Live Science, March 13. https://www.livescience.com/27529-missing-wisdom-teeth.html.
Malina, Robert M., and Bertis B. Little. 2008. “Physical Activity: The Present in the Context of the Past.” American Journal of Human Biology 20 (4): 373–391.
Mandsager, Kyle, Serge Harb, and Paul Cremer. 2018. “Association of Cardiorespiratory Fitness with Long-term Mortality among Adults Undergoing Exercise Treadmill Testing.” JAMA Network Open 1 (6): e183605. doi:10.1001/jamanetworkopen.2018.3605.
Marciniak, Stephanie, and George H. Perry. 2017. “Harnessing Ancient Genomes to Study the History of Human Adaptation.” Nature Reviews Genetics 18: 659–674.
Marlowe, Frank W. 2005. “Hunter-Gatherers and Human Evolution.” Evolutionary Anthropology 14 (2): 54–67.
Marmot, Michael. 2005. “Social Determinants of Health Inequality.” The Lancet 365 (9464): 1099–1104.
Martini, Frederic H., William C. Ober, Edwin F. Bartholomew, and Judi L. Nath. 2013. Visual Essentials of Anatomy & Physiology. Boston, MA: Pearson.
Mathews, T.J., and Brady E. Hamilton. 2016. “Mean Age of Mothers Is on the Rise: United States, 2000–2014.” National Center for Health Statistics (CHS) Data Brief. No. 232. https://www.cdc.gov/nchs/data/databriefs/db232.pdf.
McElroy, Ann, and Patricia Townsend. 2009. Medical Anthropology in Ecological Perspective. Fifth Edition. Boulder, CO: Westview Press.
McEvoy, Claire T., Norman Temple, and Jayne V. Woodside. 2012. “Vegetarian Diets, Low-Meat Diets and Health: A Review.” Public Health Nutrition 15 (12): 2287–2294.
McKee, Trudy, and James R. McKee. 2015. Biochemistry: The Molecular Basis of Life. Sixth Edition. Oxford, UK: Oxford University Press.
Moss, Michael. 2013. Salt, Sugar, Fat: How the Food Giants Hooked Us. New York: Random House.
National Geographic Society. N.d. Resource Library: Encyclopedic Entry (n.d.), s.v., “Autotroph.” National Geographic Society. https://www.nationalgeographic.org/encyclopedia/autotroph/.
National Institutes of Health (NIH). 2017. “Obesity and Cancer Fact Sheet.” Last modified January, 2017. https://www.cancer.gov/about-cancer/causes-prevention/risk/obesity/obesity-fact-sheet.
Neeha, V. S., and Priyamvadah Kinth. 2013. “Nutrigenomics Research: A Review.”Journal of Food Science and Technology, 50 (3): 415–428.
Neel, James V. 1962. “Diabetes Mellitus: A ‘Thrifty’ Genotype Rendered Detrimental by ‘Progress’?” American Journal of Human Genetics 14 (4): 353–362.
Novembre, John, Alison P. Galvani, and Montgomery Slatkin. 2005. “The Geographic Spread of the CCR5 Δ32 HIV-Resistance Allele.” PLoS Biology 3 (11): e339.
Odes, Edward J., Patrick S. Randolph-Quinney, Maryna Steyn, Zach Throckmorton, Jacqueline S. Smilg, Bernhard Zipfel, Tanya N. Augustine, et al. 2016. “Earliest Hominin Cancer: 1.7-Million-Year-Old Osteosarcoma from Swartkrans Cave, South Africa.” South African Journal of Science 112 (7–8): 1–5.
O’Keefe Osborn, Corinne. 2017. “Type 1 and Type 2 Diabetes: What’s the Difference?” Healthline Newsletter, August 24. https://www.healthline.com/health/Difference-between-type-1-and-type-2-diabetes.
Omran, Abdel R. 1971. “The Epidemiological Transition: A Theory of the Epidemiology of Population Change.” Milbank Memorial Fund Quarterly 49 (4): 509–538.
———. 2005. “The Epidemiological Transition: A Theory of the Epidemiology of Population Change.” The Milbank Quarterly 83 (4): 731–757.
Organ, Chris, Charles L. Nunn, Zarin Machanda, and Richard W. Wrangham. 2011. “Phylogenetic Rate Shifts in Feeding Time during the Evolution of Homo.” Proceedings of the National Academy of Sciences 108 (35): 14555–14559.
Ortega, Alexander Neil, Peter J. Gergen, A. David Paltiel, Howard Bauchner, Kathleen D. Belanger, and Brian P. Leaderer. 2002. “Impact of Site of Care, Race, and Hispanic Ethnicity on Medication Use for Childhood Asthma.” Pediatrics 109 (1): E1.
Palma-Gudiel, H., A. Córdova-Palomera, E. Eixarch, M. Deuschle, and L. Fañanás. 2015. “Maternal Psychosocial Stress during Pregnancy Alters the Epigenetic Signature of the Glucocorticoid Receptor Gene Promoter in Their Offspring: A Meta-Analysis.” Epigenetics 10 (10): 893–902.
Pamuk, Şevket. 2007. “The Black Death and the Origins of the ‘Great Divergence’ across Europe, 1300–1600.” European Review of Economic History 11 (3): 289–317.
Pearl, Robert. 2015. “Why Health Care Is Different if You’re Black, Latino, or Poor.” Forbes, March 5. https://www.forbes.com/sites/robertpearl/2015/03/05/healthcare-black-latino-poor/#1ab6e3807869.
Physical Activity Council. 2018. 2018 Participation Report. http://www.physicalactivitycouncil.com/pdfs/current.pdf.
Pickering, Travis Rayne, and Henry T. Bunn. 2007. “The Endurance Running Hypothesis and Hunting and Scavenging in Savanna-Woodlands.” Journal of Human Evolution 53 (4): 434–438.
Pierce, Mary, and Rebecca Hardy. 2012. “Commentary: The Decreasing Age of Puberty— As Much a Psychosocial as Biological Problem?” International Journal of Epidemiology 41 (1): 300–302.
Plotnikoff, Ronald C., Sarah A. Costigan, Rebecca L. Williams, Melinda J. Hutchesson, Sarah G. Kennedy, Sara L. Robards, Jennifer Allen, Clare E. Collins, Robin Callister, and John Germov. 2015. “Effectiveness of Interventions Targeting Physical Activity, Nutrition and Healthy Weight for University and College Students: A Systematic Review and Meta-analysis.” International Journal of Behavioral Nutrition and Physical Activity 12 (1): 1–10.
Poinar, George. 2018. “Vertebrate Pathogens Vectored by Ancient Hematophagous Arthropods.” Historical Biology, November 7. doi:10.1080/08912963.2018.1545018.
Pontzer, Herman, David A. Raichlen, Brian M. Wood, Audax Z. P. Mabulla, Susan B. Racette, and Frank W. Marlowe. 2012. “Hunter-Gatherer Energetics and Obesity.” PLoS ONE 7 (7): e40503. doi:10.1371/journal.pone.0040503.
Pritchard, Jonathan K. 2010. “How We Are Evolving.” Scientific American 303 (4): 4047.
Raichlen, David A., and Gene E. Alexander. 2014. “Exercise, APOE Genotype, and the Evolution of the Human Lifespan.” Trends in Neurosciences 37 (5): 247–255.
Raichlen, David A., Herman Pontzer, Jacob A. Harris, Audax Z. P. Mabulla, Frank W. Marlowe, J. Josh Snodgrass, Geeta Eick, J. Colette Berbesque, Amelia Sancilio, Brian M. Wood. 2016. “Physical Activity Patterns and Biomarkers of Cardiovascular Disease Risk in Hunter-Gatherers.” American Journal of Human Biology 29 (2): e22919. https://doi.org/10.1002/ajhb.22919.
Rankinen, Tuomo, Aamir Zuberi, Yvon C. Chagnon, S. John Weisnagel, George Argyropoulos, Brandon Walts, Louis Pérusse, and Claude Bouchard. 2006. “The Human Obesity Gene Map: The 2005 Update.” Obesity 14 (4): 529–644.
Richards, M. P. 2002. “A Brief Review of the Archaeological Evidence for Palaeolithic and Neolithic Subsistence.” European Journal of Clinical Nutrition 56 (12): 1270–1278.
Sallis, James F., Neville Owen, and Edwin B. Fisher. 2008. “Chapter 20: Ecological Models of Health Behavior.” In Health Behavior and Health Education: Theory, Research, and Practice, edited by Karen Glanz, Barbara K. Rimer, and K. Viswanath, 465–485. Fourth Edition. San Francisco, CA: Jossey-Bass.
Sharp, Paul M., and Beatrice H. Hahn. 2011. “Origins of HIV and the AIDS Pandemic.” Cold Springs Harbor Perspectives in Medicine 1 (1): a006841.
Shreiner, Andrew B., John Y. Kao, and Vincent B. Young. 2015. “The Gut Microbiome in Health and Disease.” Current Opinion in Gastroenterology 31 (1): 69–75.
Singer, Merrill, and Hans Baer. 2012. “Health Disparity, Health Inequality.” In Introducing Medical Anthropology: A Discipline in Action, Second edition, edited by Merrill Singer and Hans Baer, 175–205. Lanham, MD: AltaMira.
Singer, Merrill, and Scott Clair. 2003. “Syndemics and Public Health: Reconceptualizing Disease in Bio-Social Context.” Medical Anthropology Quarterly 17 (4): 423–441.
Singer, Merrill, Nicola Bulled, Bayla Ostrach, and Emily Mendenhall. 2017. “Syndemics and the Biosocial Conception of Health.” Lancet 389 (10072): 941–950.
Small, Meg, Lisa Bailey-Davis, Nicole Morgan, and Jennifer Maggs. 2013. “Changes in Eating and Physical Activity Behaviors across Seven Semesters of College: Living On or Off Campus Matters.” Health Education and Behavior 40 (4): 435–441.
Smith-Morris, Carolyn M. 2004. “Reducing Diabetes in Indian Country: Lessons from the Three Domains Influencing Pima Diabetes.” Human Organization 63 (1): 34–46.
Sonfield, Adam, Kinsey Hasstedt, Megan L. Cavanaugh, and Ragnar Anderson. 2013. The Social and Economic Benefits of Women’s Ability to Determine Whether and When to Have Children. New York: Guttmacher Institute. https://www.guttmacher.org/report/social-and-economic-benefits-womens-ability-determine-whether-and-when-have-children.
Stearns, Stephen C., Randolph M. Nesse, and David Haig. 2008. “Introducing Evolutionary Thinking into Medicine.” In Evolution in Health and Disease, edited by Stephen C. Stearns and Jacob C. Koella, 3–15. United Kingdom: Oxford University Press.
St. Pierre, Danielle. 2018. “The 15 Best Potato Chips for Every Flavor Craving.” Best, April 6. Retrieved June 13, 2018 from https://www.bestproducts.com/eats/food/g972/best-potato-chips/.
Strassmann, Beverly I. 1997. “The Biology of Menstruation in Homo Sapiens: Total Lifetime Menses, Fecundity, and Nonsynchrony in a Natural-Fertility Population.” Current Anthropology 38 (1): 123–129.
———. 1999. “Menstrual Cycling and Breast Cancer: An Evolutionary Perspective.” Journal of Women’s Health 8 (2): 193–202.
Tierney, Mike. 2013. “At Spelman, Dropping Sports in Favor of Fitness.” New York Times, April 13. https://www.nytimes.com/2013/04/14/sports/at-spelman-dropping-sports-in-favor-of-fitness.html.
Trafialek, Joanna, and Wojciech Kolanowski. 2014. “Dietary Exposure to Meat-Related Carcinogenic Substances: Is There a Way to Estimate the Risk?” International Journal of Food Sciences and Nutrition 65 (6): 774–780.
UNAIDS. 2018. “Fact Sheet: Latest Statistics on the AIDS Epidemic.” http://www.unaids.org/en/resources/fact-sheet.
Ventola, C. Lee. 2015. “The Antibiotic Resistance Crisis: Part I: Causes and Threats.” Pharmacy & Therapeutics 40 (4): 277–283.
Versini, M., Jeandel, P., Bashi, T., Bizzaro, G., Blank, M., and Shoenfeld, Y. 2015. “Unraveling the Hygiene Hypothesis of Helminthes and Autoimmunity: Origins, Pathophysiology, and Clinical Applications.” BMC Medicine, 13: 81. https://doi.org/10.1186/s12916-015-0306-7.
Vucenik, Ivana, and Joseph P. Stains. 2012. “Obesity and Cancer Risk: Evidence, Mechanisms, and Recommendations.” Special issue, “Nutrition and Physical Activity in Aging, Obesity, and Cancer,” Annals of the New York Academy of Sciences Volume 1271:: 37–43.
Walker, Polly, Pamela Rhubart-Berg, Shawn McKenzie, Kristin Kelling, and Robert S. Lawrence. 2005. “Public Health Implications of Meat Production and Consumption.” Public Health Nutrition 8 (4): 348–356.
Washington, Jesse. 2010. “Blacks Struggle with 72% Unwed Mothers Rate.” NBCNEWS.com, November 7. http://www.nbcnews.com/id/39993685/ns/health-womens_health/t/blacks-struggle-percent-unwed-mothers-rate/#.XEETH89KjBJ.
Willett, Walter, Johan Rockström, Brent Loken, Marco Springmann, Tim Lang, Sonja Vermeulen, Tara Garnett, et al. 2019. “Food in the Anthropocene: The EAT–Lancet Commission on Healthy Diets from Sustainable Food Systems.” The Lancet, January 16. http://dx.doi.org/10.1016/S0140-6736(18)31788-4.
Williams, David R., and Selina A. Mohammed. 2013. “Racism and Health I: Pathways and Scientific Evidence.” American Behavioral Scientist 57 (8). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3863357/.
Wolfe, Nathan, Claire P. Dunavan, and Jared Diamond. 2012. “Origins Of Major Human Infectious Diseases.” In Institute of Medicine: Improving Food Safety Through a One Health Approach: Workshop Summary. Washington, DC: National Academies Press. A16. https://www.ncbi.nlm.nih.gov/books/NBK114494/.
Woo, Kam S., Timothy C.Y. Kwok, and David S. Celermajer. 2014. “Vegan Diet, Subnormal Vitamin B-12 Status and Cardiovascular Health.” Nutrients 6 (8): 3259–3273.
World Health Organization (WHO). 2016. Global Report on Diabetes. http://apps.who.int/iris/bitstream/handle/10665/204871/9789241565257_eng.pdf.
———. 2017a. “Global Health Estimates 2016: Deaths by Cause, Age, Sex, by Country and by Region, 2000–2016.” Geneva: WHO.
———. 2017b. “Obesity and Overweight.” Fact Sheet. Last modified October 2017. http://www.who.int/mediacentre/factsheets/fs311/en/.
———. 2018a. Global Health Observatory (GHO) Data. “Life Expectancy.” http://www.who.int/gho/mortality_burden_disease/life_tables/situation_trends/en.
———. 2018b. “Cancer.” Fact Sheet. Last modified February 2018. http://www.who.int/news-room/fact-sheets/detail/cancer.
———. 2018c. “Healthy Diet.” Fact Sheet. Last modified October 2018. https://www.who.int/news-room/fact-sheets/detail/Healthy-diet.
———. n.d. “Influenza.” Accessed January 7, 2019 from https://www.who.int/influenza/human_animal_interface/avian_influenza/h5n1_research/faqs/en/.
Worthman, Carol M., and Jennifer Kuzara. 2005. “Life History and the Early Origins of Health Differentials.” American Journal of Human Biology 17 (1): 95–112.
Wrangham, Richard. 2009. Catching Fire: How Cooking Made Us Human. New York: Basic Books.
Yehuda, Rachel, and Joseph LeDoux. 2007. “Response Variation Following Trauma: A Translational Neuroscience Approach to Understanding PTSD.” Neuron 56 (1): 19–32.
Zuckerman, Molly K., and George J. Armelagos. 2014. “The Hygiene Hypothesis and the Second Epidemiologic Transition.” In Modern Environments and Human Health: Revisiting the Second Epidemiologic Transition, edited by Molly K. Zuckerman, 301-320. Hoboken, NJ: Wiley-Blackwell.
Zuckerman, Molly Kathleen, Kristin Nicole Harper, Ronald Barrett, and George John Armelagos. 2014. “The Evolution of Disease: Anthropological Perspectives on Epidemiologic Transitions.” Special issue, “Epidemiological Transitions: Beyond Omran’s Theory,” Global Health Action 7(1): 23303. doi:10.3402/gha.v7.23303.
Zuk, Marlene. 2013. Paleofantasy: What Evolution Really Tells Us About Sex, Diet, and How We Live. New York: W. W. Norton.
Figure Attributions
Figure 16.1 Carcinogenic Meats a derivative work original to Explorations: An Open Invitation to Biological Anthropology by Katie Nelson is under a CC BY-NC 4.0 License. [Includes Hot dog PNG image by unknown, CC BY-NC 4.0; Rasher of Bacon by unknown, public domain (CC0); Salami aka by André Karwath Aka, CC BY-SA 2.5; Cow PNG image by unknown, CC BY-NC 4.0; sheep PNG image by unknown, CC BY-NC 4.0; Pig on white background by unknown, public domain (CC0).]
Figure 16.2 Hadazbe returning from hunt by Andreas Lederer has been modified (cropped) and is used under a CC BY 2.0 License.
Figure 16.3 Obesity rates by country original to Explorations: An Open Invitation to Biological Anthropology by Katie Nelson is under a CC BY-NC 4.0 License. Based on data from Obesity Update. 2017. Organisation for Economic Co-operation and Development (OECD) Health Statistics.
Figure 16.4 The potato in three modern forms a derivative work original to Explorations: An Open Invitation to Biological Anthropology by Joylin Namie and Katie Nelson is under a CC BY-NC 4.0 License. [Includes Potato by unknown, public domain (CC0); McDonalds-French-Fries-Plate by Evan-Amos, public domain (CC0); Potato chips bowl by unknown, public domain (CC0).]
Figure 16.5 Participants of a walk against Diabetes and for general fitness around Nauru airport by Lorrie Graham, Department of Foreign Affairs and Trade is used under a CC BY 2.0 License.
Figure 16.6 Medical complications of obesity by the Centers for Disease Control and Prevention (CDC) is in the public domain.
Figure 16.7 Glucose metabolism original to Explorations: An Open Invitation to Biological Anthropology by Mary Nelson is under a CC BY-NC 4.0 License.
Figure 16.8 Type 1 and Type 2 Diabetes original to Explorations: An Open Invitation to Biological Anthropology by Mary Nelson is under a CC BY-NC 4.0 License.
Figure 16.9 Top ten causes of death in the U.S. and worldwide original to Explorations: An Open Invitation to Biological Anthropology by Joylin Namie is under a CC BY-NC 4.0 License. Based on data from Centers for Disease Control and Prevention (2016) and World Health Organization (2018).
Figure 16.10 Map of CCR5-delta32 allele distribution original to Explorations: An Open Invitation to Biological Anthropology by Katie Nelson is under a CC BY-NC 4.0 License. [Includes Europe Map Western Political 32847, unknown, Pixabay License; data from Solloch, Ute V., Kathrin Lang, Vinzenz Lange, and Irena Böhme. 2017. “Frequencies of gene variant CCR5-Δ32 in 87 countries based on next-generation sequencing of 1.3 million individuals sampled from 3 national DKMS donor centers.” Human Immonology, 78 (11-12).]
Figure 16.11 HIV-world-map-UNAIDS by UNAIDS has been designated to the public domain (CC0).
Figure 16.12 Row four man woman people walking together 3755342 by MaxPixel has been designated to the public domain (CC0).

