4.2: HEALTH CONSEQUENCES OF THE TRANSITION TO AGRICULTURE AND ANIMAL DOMESTICATION
The shift from foraging to food production occurred relatively recently in our evolutionary history (Larsen 2014), and there are indications our biology has not yet caught up (Pritchard 2010). Beginning around 12,000 BCE in several parts of the globe, humans began to move to a diet based on domesticated plants and animals (Armelagos et al. 2005). This involved manipulating the natural landscape to facilitate intensive food production, including the clearing of forest and construction of wells, irrigation canals, and ditches, exposing humans to water-borne illnesses and parasites, and attracting mosquitos and other vectors of disease to human settlements. The heavy, repetitive physical labor of early agricultural production resulted in negative impacts on articular joints, including osteoarthritis (Larsen 2014). At the same time, nutritional diversity became restricted, focused on major cereal crops that continue to dominate agricultural production today, including corn, wheat, and rice (Jain 2012). This represented a major shift in diet from a wide variety of plant and animal foods to dependence on starchy carbohydrates, leading to increases in dental caries (cavities), reductions in stature and growth rates, and nutritional deficiencies (Larsen 2014). Domesticated animals added new foods to the human diet, including meat that was higher in fat and cholesterol than wild game as well as dairy products (Lucock et al. 2014). Agriculture provided the means to produce a storable surplus for the first time in human history, allowing some individuals to grow and consume more than others, leading to the beginnings of economic inequality (Harris 1989). Social hierarchies led to the unequal distribution of the basic resources for healthy living, concentrating infectious disease among the poor and malnourished (Zuckerman et al. 2014), a situation that continues to plague humanity today (Marmot 2005).
Sedentism and a rise in population density accompanied the move to agriculture, increasing the risk of infectious disease. Agriculture often provided enough calories, if not enough nutrition, to increase fertility. That is, although diets were worse and people unhealthier, populations continued to grow, even in the midst of high levels of child and maternal mortality and short life expectancies (Omran 2005). Hygiene became an issue as large settlements increased the already-difficult problem of removing human wastes and providing uncontaminated water (Armelagos et al. 2005). Domesticated animals, including cattle, sheep, goats, pigs, chickens, and horses, provided reservoirs of zoonotic pathogens, which affected farmers more than foragers, as farmers were in closer proximity to their animals on a daily basis (Marciniak and Perry 2017). Many of these diseases became major killers of humankind, including influenza, tuberculosis, malaria, plague, syphilis, and smallpox, functioning as selective pressures in and of themselves (Cooling 2015). As these diseases encountered large human populations, malnourished and concentrated in early settlements, they caused major epidemics that traveled along newly established routes for trade, warfare, and colonization.
EPIDEMIOLOGICAL TRANSITIONS
Changes in diet and physical-activity patterns associated with agriculture, in conjunction with increased population densities and exposure to zoonoses, resulted in what is known as an epidemiological transition, a shift in the causes of morbidity and mortality among humankind (Omran 1971). The first epidemiological transition from foraging to food production resulted in increases in dental caries, nutritional deficiencies, infectious disease, and skeletal conditions like osteoarthritis, as well as decreases in growth and height (Larsen 2014). A second epidemiological transition occurred following the Industrial Revolution in Western Europe and the United States when socioeconomic, political, and cultural conditions contributed to improved standards of living, hygiene, and nutrition that minimized the effects of infectious disease, after which people began to experience the Noncommunicable Diseases (NCDs) that are the focus of the remainder of this chapter (Omran 2005). With the addition of immunizations and other public health initiatives, modified forms of this transition remain ongoing in many low- and middle-income countries (Zuckerman et al. 2014), with several now facing a “double burden” of disease, with poor, often rural, populations falling prey to infectious diseases, while more affluent citizens are victims of chronic illnesses. A third epidemiological transition is now underway as infectious diseases, some of them novel, others re-emergent, and others even multi-drug resistant, have once again become major health concerns (Harper and Armelagos 2010; Zuckerman et al. 2014). These include Ebola, HIV/AIDS, tuberculosis, malaria, dengue, Lyme disease, and West Nile virus, all zoonoses that initially spread to humans through contact with animals. These diseases are increasing their geographic ranges due to climate change, economic development, and deforestation (Baer and Singer 2009).
Patterns of morbidity and mortality continue to shift across the globe. As with the first epidemiological transition resulting from the adoption of large-scale agriculture, such shifts can be the direct, if unintended, result of human interactions with the environment. For example, there has been a well-documented rise in chronic inflammatory diseases (CIDs) in recent decades in developed countries (Versini et al. 2015). This includes increased rates of allergic conditions like asthma, as well as autoimmune diseases like rheumatoid arthritis, multiple sclerosis, Crohn’s disease, and inflammatory bowel disease. This has coincided with the decrease in infectious disease associated with the second epidemiological transition, and the two are related. The “hygiene hypothesis” postulates the rise in CIDs is a result of limited exposure to nonlethal environmental pathogens in utero and early childhood (Zuckerman and Armelagos 2014). Modern human societies have become so sanitized that we are no longer exposed to microorganisms that stimulate the development of a healthy immune system (Versini et al. 2015). “In effect, the lifestyle changes—sanitary improvements, pasteurization, use of antibiotics, and improved hygiene—that contributed to the second transition may have produced a substantial trade-off in health and quality of life, with developed nations exchanging a high burden of infectious disease for a higher burden of CIDs” (Zuckerman et al. 2014).
Similarly, the re-emergence of infectious disease, the third epidemiological transition, reflects the continuing relationship between humans, animals, and pathogens. Over 60% of Emerging Infectious Diseases (EIDs) between 1940 and 2004 have been of zoonotic origin, with over 70% stemming from human contact with wildlife (Jones et al. 2008). The global bushmeat trade currently devastating Africa’s wildlife is a continuing source of Ebola infection (Asher 2017), as well as the original source of HIV and viruses related to leukemia and lymphoma among humans (Zuckerman et al. 2014). Further, new strains of avian (bird) flu, some with mortality rates as high as 60% among human victims (WHO n.d.), are transmitted to humans through poultry production and contact with wild birds; these pose a looming global threat of epidemic disease (Davis 2005). Lastly, the use of antibiotics in commercial meat production is directly related to the rise of drug-resistant strains of previously controlled infectious diseases. An estimated 80% of antibiotics in the U.S. are used to promote growth and prevent infection in livestock, and drug-resistant bacteria from these animals are transmitted to humans through meat consumption (Ventola 2015).
These examples illustrate continuing interaction between humans, our evolved biology, and the physical and cultural environments in which we live. The remainder of this chapter will focus on selected noncommunicable diseases and the social, cultural, and environmental factors that contribute to their prevalence in modern, industrialized economies. We begin with the health condition that affects all of the others—obesity.
OBESITY
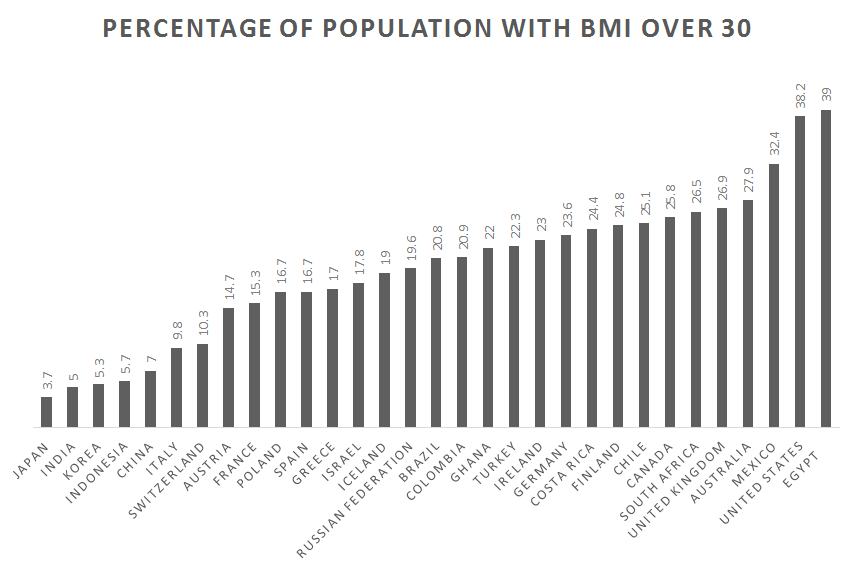
According to the World Health Organization (2017b), 1.9 billion of the world’s people are overweight and 650 million of these are obese. In the United States, 70% of Americans are overweight, and 40% of these meet the criteria for obesity. For the first time in human history, most of the world’s population lives in countries where overweight and obesity kill more people than hunger does (see Figure 16.3). Improvements in public health and food production have allowed a greater number of people to live past childhood and to have enough food to eat. This does not include everyone. Many people still struggle with poverty, hunger, and disease, even in the wealthiest of nations, including the United States. On a global scale, however, many people not only have enough food to survive but also to gain weight—and, notably, enough extra weight to cause significant health problems. Several aspects of life in modern, industrialized societies contribute to the obesity crisis.
Causes of Obesity
Although studies show differences in daily energy expenditure between modern foraging and farming populations in comparison with industrialized peoples, the major contributor to obesity in Western populations is energy intake (Pontzer et al. 2012). Many people not only eat too much but too much of the wrong things. Biological anthropologist Leslie Lieberman (2006) argues that contemporary humans continue to rely on cues from foraging strategies in our evolutionary past that are now counterproductive in the obesogenic environments in which we now live.
Examine your own eating habits in the context of how humans once hunted and gathered. We relied on visual cues to find food, often traveling long distances to obtain it, then transporting it back to our home base. There we may have had to process it, by hand, to render it edible. Think of how much less energy it takes to find food now. If we have the financial resources, we can acquire big energy payoffs by simply sitting at home and using an app on our mobile phone to place an order for delivery. And, voila! High-calorie (if not highly nutritious) food arrives at our door within minutes. Should we venture out for food, search time is reduced by signage and advertising directing us toward high-density “patches” where food is available 24 hours a day. These include vending machines, gas stations, and fast-food outlets. Travel time is minimal and little human energy is used in the process (Lieberman 2006).
Foods are also pre-packaged and prepared in ways that allow us to eat large quantities quickly. Think French fries or chicken nuggets, which we can easily eat with our hands while doing other things, like driving or watching television, rendering eating mindless and allowing us to take in food faster than our endocrine systems can let us know we are getting full. Modern “patches” offer low-fiber, calorie-dense resources, which allows us to eat larger quantities, a problem already encouraged by our larger portion sizes (Lieberman 2006). Processed foods are also engineered to appeal to hominin preferences for sweet tastes and fatty, creamy textures (Moss 2013). Remember from earlier chapters that natural selection favored depth perception, color vision, grasping hands, and coordinated eye-hand movements as general primate traits. Advertising and packaging now use our color vision against us, attracting us to products with little nutritional value and playing to our evolutionary predisposition toward variety. Remember those 50 different nutrients we require? That variety is now presented to us in the form of 55 different flavors of Oreo cookies (Cerón 2017), which we take out of the package and dip in milk using our hand-eye coordination and depth perception.
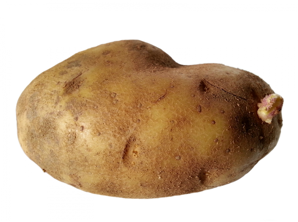
Even if we are ostensibly eating the same things our ancestors did, these foods may not be all that much alike. Take potatoes, for example. One medium-sized, plain, baked potato is a healthy food, especially if we eat the skin too. It contains 110 calories, 0 grams of fat, 26 grams of carbohydrates, and 3 grams of protein, plus 30% of the U.S. Recommended Daily Allowance (RDA) of vitamin C, 10% of vitamin B6, 15% of potassium, and no sodium. In contrast, a medium order of McDonald’s fries, which takes the potato and adds salt and fat, contains 340 calories, 16 grams of fat, 44 grams of carbohydrates, 4 grams of protein, and 230 mg of sodium. Potato chips take food processing to a whole new level, removing even more nutrition and adding a host of additional ingredients, including oils, preservatives, and artificial flavorings and colors (Moss 2013). Let us use Ruffles Loaded Bacon and Cheddar Potato Skins Potato Chips, one of the top new flavors of 2018, as an example (St. Pierre 2018). The number of ingredients increases from one to 11 to 35 as we move from the potato to the potato chip, moving further from nature with each step (Figure 16.4). It should be noted that the nutritional information for the potato chips is based on a serving size of 11 chips, an amount likely smaller than many people eat. Our bodies also do not react to fries and chips the same way they do to potatoes. Added fat and calories translate into overweight and obesity. Sodium contributes to hypertension. And, artificial flavorings and colorings, including the Yellow 5 and Yellow 6 in the chips, have been linked to cancer, as well as allergies and hyperactivity in children (CSPI 2010). Many sweet, fatty, salty foods like fries and chips are cheap and easily available, which is why many people choose to eat them (Moss 2013). The price of a medium-sized order of McDonald’s fries as of this writing is US$1.79, and the potato chips are $2.98 for an 8.5-ounce bag. A single potato pre-wrapped for microwaving is available in many supermarkets for US$1.99 but requires travel to a market and access to a microwave and eating utensils, making it less convenient.
|
|
Baked Potato [baked, skin on, plain] |
French Fries [medium order] |
Potato Chips [1 oz. serving of 11 chips] |
|
Calories |
110 |
340 |
160 |
|
Calories from fat |
0 |
144 |
90 |
|
Fat |
0 g |
16 g |
10 g |
|
Carbohydrates |
26 g |
44 g |
15 g |
|
Protein |
3 g |
4 g |
2 g |
|
Sodium |
0 g |
230 mg |
170 mg |
|
Dietary fiber |
2 g |
4 g |
1 g |
|
Sugars |
1 g |
0 g |
1 g |
|
Cholesterol |
0 g |
0 g |
0 g |
|
Ingredients |
Potato |
Potatoes, Vegetable Oil (Canola Oil, Soybean Oil, Hydrogenated Soybean Oil, Natural Beef Flavor [Wheat and Milk Derivatives]*, Citric Acid [Preservative]), Dextrose, Sodium Acid Pyrophosphate (Maintain Color), Salt. |
Potatoes, Vegetable Oil (Sunflower, Corn, and/or Canola oil), Bacon & Cheddar Loaded Potato Skins Seasoning (Maltodextrin [Made from Corn], Salt, Cheddar Cheese [Milk, Cheese Cultures, Salt, Enzymes], Sour Cream [Cultured Cream, Skim Milk], Whey, Dried Onion, Monosodium Glutamate, Natural Flavor [including Natural Smoke Flavor], Skim Milk, Corn Oil, Canola Oil, Sugar, Buttermilk, Yeast Extract, Romano Cheese [Part-Skim Cow’s Milk, Cheese Cultures, Salt Enzymes], Whey Protein Concentrate, Dextrose, Spice, Citric Acid, Lactic Acid, Artificial Color [Yellow 5 Lake, Yellow 5, Yellow 6, Yellow 6 Lake], Butter [Cream, Salt], Sodium Caseinate, Garlic Powder, Blue Cheese [Milk, Cheese Cultures, Salt, Enzymes], and Bacon Fat. |
Table 2 The potato in three modern forms
Not only have we transformed the food supply and our eating in ways that are detrimental to our health, but these changes have been accompanied by reductions in physical activity. Sedentarism is built into contemporary lifestyles. Think of how much time you spent sitting down today. Some of it may have been in class or at work, some may have been driving a car or perhaps binge-watching your favorite show, playing a video game, or checking in on social media. An inactive lifestyle is almost dictated by the digital age (Lucock et al. 2014). Levels of physical activity in many countries are now so low that large portions of the population are completely sedentary, including 28% of Americans (Physical Activity Council 2018). For a species whose biology evolved in an environment where walking, lifting, and carrying were part of daily life, this is unhealthy and often leads to weight gain.
Obesity varies by gender, age, geography, and, to some degree, ethnicity (Brown 1991). In general, women tend to gain weight easier than men, but fat distribution is different between them. Women tend to put on weight in the thighs and hips, while men gain weight around their abdomen. The latter is a much greater health risk (Akil and Ahmad 2011). Weight gain also varies across the lifespan, with infants and toddlers tending toward chubbiness then becoming slimmer until adolescence and the onset of puberty (Lucock et al. 2014). This pattern is the result of selective pressure to maintain energy for brain development in early life, then again later on for reproduction. There is also the “thrifty gene” hypothesis: the idea that natural selection favored genotypes that clung to every calorie available to protect against the constant threat of food shortages throughout our evolutionary history, and that this was a species-wide adaptation (Neel 1962).

More recent genetic research indicates there are multiple genetic variants that influence weight gain, and they are not spread evenly across or within human populations. Tuomo Rankinen and colleagues (2006) identified 127 genes associated with obesity, of which 22 were supported by research indicating that they contributed to positive energy balance and weight gain. Claude Bouchard (2007) went further, identifying five categories of obesity-promoting genotypes. These include genotypes that promote sedentarism, result in low metabolism, and lead to poor regulation of appetite and satiety and a propensity to overeat. An example of the impact such genotypes can have in an environment of plenty is found among the population of the Micronesian island of Nauru. Historically, the island was geographically isolated and the food supply was unpredictable. These conditions favored genotypes that promoted the ability to rapidly build up and store fat in times of food availability. In Nauruans, there are two genetic variations favoring weight gain and insulin resistance, and both are associated with obesity and Type 2 diabetes. One variant is also associated with higher diastolic blood pressure. One of these variants is also found in Pima Indians in the United States, where it is associated with a high Body Mass Index (BMI) and Type 2 diabetes, although it is not associated with the same outcomes in Japanese and British subjects (de Silva et al. 1999). The other variant was also analyzed in Finnish and South Indian populations, neither of whom experienced the same outcome as Nauruans. This suggests these alleles may act as modifying genes for Type 2 diabetes in some population groups (Baker et al. 1994). Unfortunately, Nauruans are one of those groups. Eventually, they became wealthy through phosphate mining on the island, gaining access to a calorie-rich Western diet of imported foods and developing a sedentary lifestyle. This resulted in rates of Type 2 diabetes as high as 30–40% of Nauruans over the age of 15, which became the leading cause of death (Lucock et al. 2014), something Nauruans are taking seriously (See Figure 16.5).
Factors other than biology influence which populations carry and express a genetic predisposition toward obesity and which populations carry but do not express it. The Pima Indians, for example, were seriously impacted by U.S. government policies that affected water rights, forcing the population away from subsistence farming to dependence on government commodities and convenience food. This resulted in a significant loss of physical activity and sedentarism, as well as malnutrition and obesity. Those living on the reservation continue to experience hardship due to high rates of unemployment and poverty, as well as depression, sometimes made worse by alcoholism. In the absence of these pressures, the Pima were diabetes free for centuries prior, even though they relied on agriculture for subsistence, suggesting genetics alone is not responsible for high rates of obesity and diabetes in current populations (Smith-Morris 2004).
Obesity also has an epigenetic component. You learned about epigenetics in Chapter 3. With regard to obesity, epigenetics is counterintuitive in that mothers who do not take in enough calories during pregnancy often give birth to babies who grow up to be fat. What takes place is that the fetus receives signals from the mother through the placenta and intrauterine environment about environmental conditions during pregnancy, in this case food insecurity. These signals encourage the turning on and off of genes related to metabolism, for example. This alters the phenotype of the fetus so that if the child is born into an environment where food is readily available, it will put on weight rapidly whenever possible, falling prey to obesity and related diseases later in life. What is worse is that if the child is a girl, her own eggs are formed in utero with the same genetic changes coded in, meaning she will pass along this same genetic predisposition to gain weight to her children. Hence, a biological propensity toward obesity can continue across generations (Worthman and Kuzara 2005). This same mechanism operates in populations born into poverty that are now growing into plenty. Epigenetic changes to genes that promote weight gain are argued to be partly responsible for the rapid rise in obesity and diabetes in recent years in developing countries gaining access to Western diets (Stearns et al. 2008).
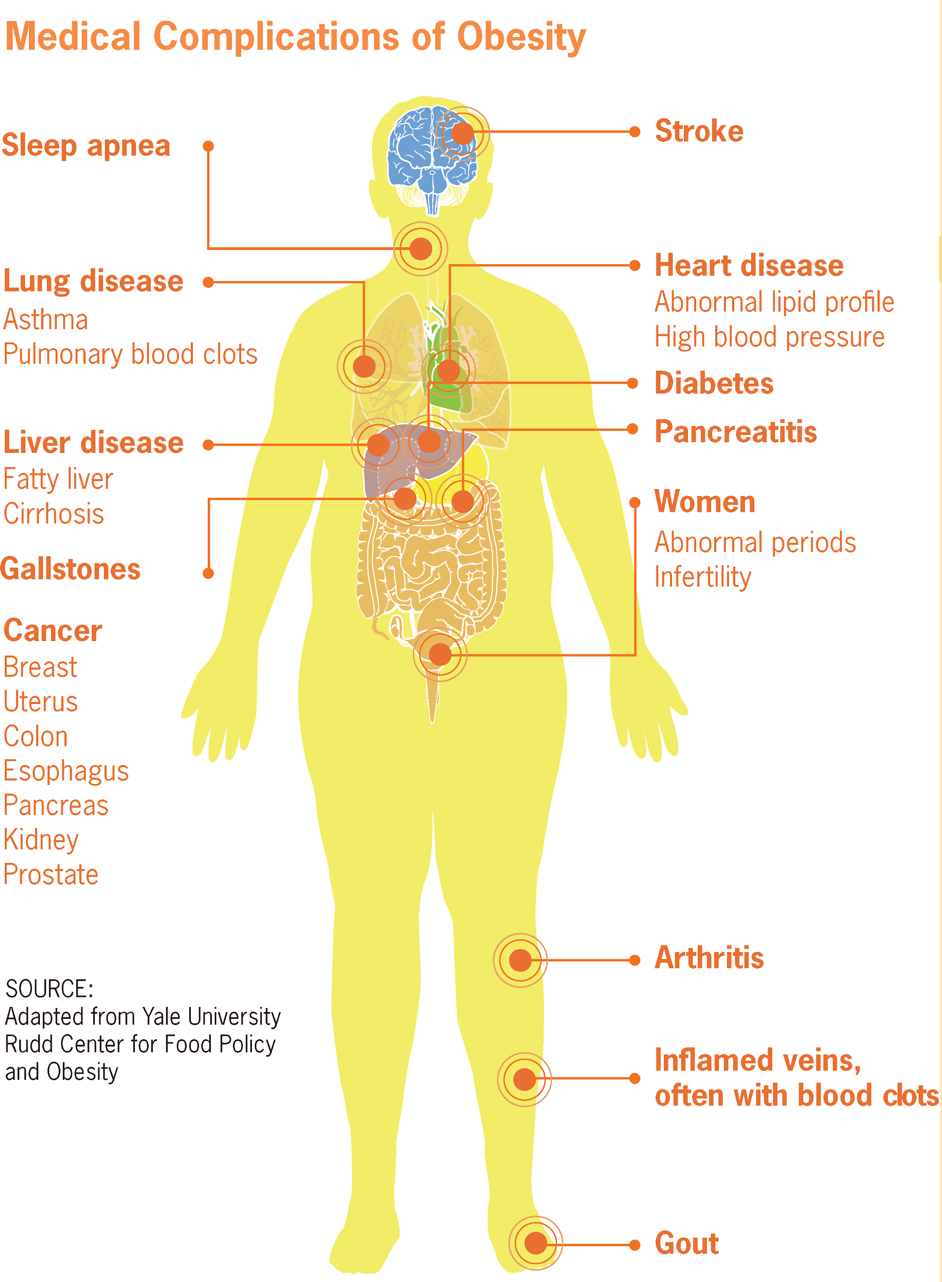
Obesity and overweight put a tremendous strain on several biological systems of the body, including the circulatory, endocrine, and skeletal systems, contributing to hypertension, heart disease, stroke, diabetes, and osteoarthritis (See Figure 16.6). Obesity also elevates the risk of cancers of the breast, endometrium, kidney, colon, esophagus, stomach, pancreas, and gallbladder (National Institutes of Health 2017; Vucenik and Stains 2012). Diabetes, one of the fastest growing health conditions around the globe (WHO 2016) and one tightly connected to obesity and overweight, is the focus of the following Special Topics feature.